Abstract
The incidence and prevalence rates of inflammatory bowel disease (IBD) have been increasing in East Asian countries over the past few decades. Accordingly, the general understanding and awareness of IBD among healthcare professionals has increased considerably in this region. This increase is ultimately associated with the evolving focus of IBD clinicians devoted to comprehensive patient care, especially in establishing IBD clinics/centers capable of providing multidisciplinary counseling. Comprehensive IBD care at IBD clinics/centers usually includes surgical and medication decision-making, transition from pediatric to adult clinics, care of extraintestinal manifestations, care of infectious diseases in patients undergoing immunomodulatory or biologic therapies, and nutritional, psychosocial, socioeconomic, and pharmacological care. Team members comprise specialists from various departments related to IBD and can be divided into core and ad hoc members. Usually, the scope of work in IBD clinics/centers involves patient care, patient outreach, and system management. Considering the environmental changes in IBD treatment, it is necessary to perform comprehensive IBD patient care in the form of a program based on competencies, rather than simply following the organization of previous IBD centers. The present review summarizes recent trends in IBD patient care and offers perspectives regarding IBD center management.
Keywords: Inflammatory bowel diseases, Interdisciplinary communication, Progressive patient care
INTRODUCTION
Inflammatory bowel diseases (IBDs), including Crohn’s disease (CD) and ulcerative colitis (UC), exhibit chronic, recurrent, complicated, and heterogeneous clinical characteristics. Although genetic, immunological, environmental, and microbial factors are believed to be associated with the development of IBD, the exact pathogenesis remains unclear [1,2]. Despite IBD not being as prevalent in East Asian compared with Western countries, its incidence has been increasing during the past few decades in East Asia, especially in Korea, Taiwan, Japan, India, and China [3]. The reasons for the rapid increase in incidence are not clear, but changes in dietary habits and the environment, advances in diagnostic technologies, and physician awareness have been proposed as contributing factors [4]. Additionally, therapeutic approaches have been developed based on in vivo and in vitro investigations targeting specific cytokine pathways and/or adhesion molecules [5].
Unfortunately, a considerable number of IBD patients ultimately require surgical intervention and experience diverse complications, including extraintestinal manifestations (EIMs) and complications of the disease itself, such as strictures, fistulas, and/or abscesses [6]. Psychological issues and socioeconomic burdens are also often associated with IBD [7]. Recently, patient quality of life has been recognized as an important issue in the treatment of IBD. Novel biologic agents introduced in recent decades have revolutionized IBD care by providing diverse therapeutic options [8]. These changes and the heterogeneity of the disease itself have prompted the development of personalized therapies, which can be administered most efficiently at IBD clinics/centers. Therefore, patient care for IBD involves more comprehensive and centralized demands than for any other disease due to the complexities of IBD and various clinical aspects, including new drugs, surgical interventions, EIMs, and nutritional and psychological issues.
The present review describes the current status of IBD treatment in Korea, proposes avenues to optimize and improve treatment strategies, and identifies important factors in IBD clinic/center management.
THE EPIDEMIOLOGY OF IBD IN KOREA
The incidence of a particular disease refers to the number of newly diagnosed patients in a population during a specific period [9]. Although several epidemiological studies have investigated IBD in East Asian countries, it is difficult to make direct comparisons among studies due to variation in screening criteria, diagnostic definitions, target populations, and data sources. Fortunately, population- and big data-based studies in Korea using nationwide population data have been recently published. During the 2011 to 2014 period, the average annual incidences of CD and UC in Korea were 2.8 and 5.0 per 100,000, respectively, based on national health insurance data [10]. Similar results have been reported in other studies [11]. Compared with other East Asian countries, the incidence and prevalence rates of IBD in Korea are the second highest after Japan. The overall crude annual incidences of CD and UC in Asia were estimated as 0.35 (95% confidence interval [CI], 0.31 to 0.40) and 0.76 (95% CI, 0.69 to 0.84) in 2011 to 2012 and 0.66 (95% CI, 0.60 to 0.73) and 1.20 (95% CI, 1.11 to 1.29) in 2012 to 2013, respectively [12]. The crude incidences of CD and UC in Taiwan specifically were 0.47 and 0.95 per 100,000 in 2015, respectively [13]. The crude incidence rate of IBD in 2011 to 2012 was 3.06 (95% CI, 2.49 to 3.73) in Hong Kong, 3.44 (95% CI, 2.47 to 4.42) in mainland China (Guangzhou), and 1.06 (95% CI, 0.76 to 1.45) in Singapore [14]. Previously, IBD was considered a disease that is predominantly prevalent in Western countries; however, the incidence rate has increased throughout East Asia over the past 20 years [15].
Similar to the incidence rate, the prevalence rate of IBD has steadily increased over time due to the chronic nature and increasing incidence of the disease as well as global aging trends. Although still lower in East Asian compared with Western countries [15], the prevalence rates of CD and UC in Taiwan during the 2000s increased sharply from 0.6 and 2.1 per 100,000 in 2001 to 3.9 and 12.8 per 100,000 in 2015, respectively [13]. From 2009 to 2016, the prevalence of CD in Korea increased from 16.0 to 29.6 per 100,000, whereas that of UC increased from 41.4 to 66.0 per 100,000 [16], the incidence of CD in Korea increased from 2.4 to 2.9 per 100,000, whereas that of UC increased from 4.0 to 5.3 per 100,000 [16]. Research on local populations in Korea revealed similar results, with an adjusted prevalence rate of 76.66 per 100,000 for UC and 31.59 per 100,000 for CD in 2015 [17]. In Hong Kong, the adjusted prevalence rates of UC and CD were 24.5 and 18.6 per 100,000 in 2014, respectively [18]. Considering that IBD patients represent approximately 0.9% and 0.3% of the populations of the United States and Europe, respectively, the prevalence of IBD in East Asia remains relatively low, yet is steadily increasing. Specifically, incidence trends for pediatric IBD in Korea have increased markedly, especially within the past 5 years, and the incidence rate of perianal disease is higher in Korean than in Western children (43.9% vs. 9%–15%) [19]. Additionally, according to a nationwide registry, the number of anal surgeries conducted in IBD patients in Korea is large due to the high rate of anal involvement, and the rate of laparoscopic surgery increased dramatically from 11.6% in 2009 to 30% in 2015 [20]. Overall, it is expected that the number of IBD patients in Korea will increase further. Therefore, it is necessary to systematically construct a comprehensive IBD treatment environment comparable with that of Western countries.
IBD-RELATED CLINICAL TRIALS IN KOREA
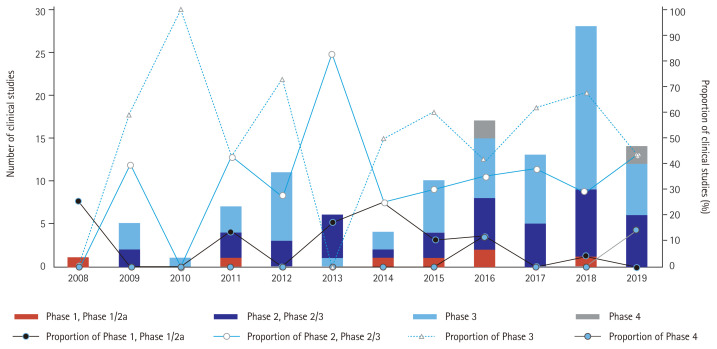
The developmental environment for IBD-related clinical trials in Korea is similar to that for IBD epidemiology. A search of the website for new investigational drug applications (http://nedrug.mfds.go.kr) from all clinical trials approved by the Korean Ministry of Food and Drug Safety was conducted in March 2020 using the keywords “CD,” “UC,” “IBD,” “intestinal Behçet’s disease,” and combinations thereof. As shown in Fig. 1, the number of new IBD clinical trials has increased considerably in Korea [21]. From 2008 to 2019, 37 (30.6%) phase II and 64 (52.9%) phase III clinical trials among all IBD clinical trials were conducted. Conversely, relatively fewer phase I clinical trials for IBD have been conducted in Korea.
Figure 1.
Number of protocols for assessing investigational drugs for inflammatory bowel disease approved annually by the Korean Ministry of Food and Drug Safety.
More approved clinical research trials will lead to a greater rate of approved medications on the market, ultimately providing more therapeutic options for IBD patients. Consequently, IBD patients in Korea would benefit from an expanded range of new therapeutic options; however, the number of clinical trials is not always consistent with the number of approved drugs. Collectively, the statuses of these clinical trials and newly approved medications provide evidence illustrating the increasing complexity of IBD treatment. Moreover, health professionals, especially IBD specialists, should aim to gain a more accurate understanding of disease mechanisms and their impact on therapeutic decisions to optimize the initiation, selection, and sequencing of biologics [22]. Such changes will be among the components driving the development of the IBD treatment environment in Korea, with more biological and small-molecule therapies and advanced drug-response monitoring, including therapeutic drug monitoring [23].
IBD CLINICS/CENTERS AND MULTIDISCIPLINARY TREATMENT
The disease complexity, heterogeneity, and EIMs of IBD require a coordinated and collaborative therapeutic approach involving gastroenterologists, colorectal surgeons, pediatric gastroenterologists, radiologists, IBD nurses, dieticians, and pharmacists. Thus, multidisciplinary and team-based patient care is strongly recommended for the optimal treatment of IBD [24,25]. Because clinical treatment decisions and opinions regarding IBD often differ among various types of clinicians, a multidisciplinary team approach is very important for achieving consensus and standardization of IBD care services. This is a prominent trend in the recent medical environment and has originated from the treatment of cancers and chronic diseases other than IBD [26,27]. Moreover, IBD care has evolved from physician superiority to a shared decision-making process involving patients and/or patient empowerment, which can lead to greater treatment adherence in patients [28]. In the presence of effective multidisciplinary communication, while ensuring patient safety considering the characteristics of IBD, team-based approaches have gained popularity. Such an approach may involve the following components: surgery-related decisions, such as the optimal timing, necessity of surgery, and/or postoperative care; determining the appropriate timing or selection of medications; special care for patients experiencing EIMs; care for patients receiving immunomodulatory or biologic therapies, who are at high risk of infection; nutritional, psychosocial, obstetrical, pharmacological, and socioeconomic care; and the transition from pediatric to adult clinical care. Focused services could lead to more appropriate clinical decisions by increasing the efficiency of the professionals delivering IBD services. All of these activities can be integrated in an IBD clinic/center. Worldwide, the major leading hospitals are now operating multidisciplinary treatment programs and systems based on IBD clinics/centers.
In Korea until the early 2010s, most university or tertiary hospitals provided multidisciplinary care centered on gastroenterologists, without establishing official clinics/centers. Most hospitals focused on IBD patient treatment are now establishing and operating official IBD clinics/centers, which generally integrate staff members from various departments. Based on the experience of Severance Hospital (Seoul, Korea), these staff members can be divided into core and ad hoc members (Table 1). Core members participate mainly in routine multidisciplinary treatment, patient outreach, and annual/regular IBD patient seminars. Thus, the core members participate in regular conferences or meetings to discuss routine tasks ranging from patient issues to clinical and administrative issues. The ad hoc members facilitate collaboration regarding specific patients and situations. For example, the care of patients transitioning from a pediatric clinic/center to an adult facility and those requiring minor procedures necessitates collaboration between IBD nurses, gastroenterologists, and pediatricians. For patients initiating biologic agents, infectious disease physicians and gastroenterologists discuss and screen for the risk of tuberculosis and any other infections, while IBD nurses and infusion nurses work together to design infusion schedules. Accordingly, most IBD clinics/centers have subdivisions. The most typical system involves a CD, UC, or intestinal Behçet’s disease clinic within the IBD center depending on the focal disease entity. Alternatively, the clinics can be organized according to field, such as transition, fertility, and/or ostomy clinics. The clinic composition may vary depending on the characteristics of each hospital or the areas of focus of the participating members.
Table 1.
Core and ad hoc member groups at the Severance Hospital IBD Clinic (Seoul, Korea)
| Core member | Gastroenterologist | Colorectal surgeon | Pediatric gastroenterologist | Radiologist |
|---|---|---|---|---|
| IBD nurse | Dietician | Pharmacist | Social service worker | |
| Ad hoc member | Dermatologista | Psychiatrist | Rheumatologista | |
| Histopathologistb | Infectious disease physicianc | Obstetrician | ||
| Wound, ostomy, continence nurseb | Clinical research coordinator | Infusion nursec | ||
IBD, inflammatory bowel disease.
Treatment for intestinal Behçet’s disease.
In case of surgery.
In case of biologics initiation.
TASKS OF IBD CLINICS/CENTERS: THREE MAJOR CATEGORIES
Using Severance Hospital as an example, the work of an IBD clinic is divided into three major categories: patient care, patient outreach, and system management (Table 2). Multidisciplinary conferences, as part of the patient care category, can be conducted by core and ad hoc members, whereas patient participation is not always necessary. When deciding whether to perform surgery, a conference between the patients, colorectal surgeon, and gastroenterologist is most effective. Conversely, when considering a differential diagnosis or designing a therapeutic strategy, it may be more efficient to conduct a conference between the physician and the corresponding IBD clinic staff members, including the radiologist and pathologist, to discuss radiological imaging and pathology results. Thus, the organization can differ depending on the situation. A multidisciplinary approach to cancer management with organizational support is usually applied in real-world clinical settings to improve the effectiveness of clinical decision-making. In Korea, the fee for multidisciplinary consultation has officially been covered by national insurance since 2014, although such coverage was applicable to only some cancer patients. However, since 2017, insurance coverage has expanded to include other cancers, tuberculosis, and rare incurable diseases, including CD, UC, and intestinal bowel disease. Therefore, multidisciplinary consultation with such patients and their families can be performed systematically and officially in tertiary hospitals in Korea. A multidisciplinary approach is the most important feature of the IBD center. To optimize management and time efficiency, in cases involving colorectal cancer, it may make sense to conduct the patient consultation in parallel with the cancer multidisciplinary team, especially if the same members are involved in both teams.
Table 2.
Scope of the work conducted at the Severance Hospital IBD Clinic (Seoul, Korea)
| Patient care | Patient outreach | System management |
|---|---|---|
|
|
|
IBD, inflammatory bowel disease; SNS, social network services.
Among the activities of IBD centers/clinics, in terms of patient care, the assessment of IBD severity is another key factor. The CD activity index [29,30], Mayo score [31], and disease activity index for intestinal bowel disease [32] are simple and adequate measures used for personalized risk stratification and should be adapted according to the therapeutic plan. Radiological or endoscopic evaluation is also a tool for risk stratification. Furthermore, the use of tablets to create diaries and simultaneously share/archive these diaries in electronic medical records is also recommended. High-risk patient groups requiring special management, short bowel syndrome patients, and those likely requiring surgery or at high risk of infection can be easily referred to sub-clinics such as those specializing in transitional care, fertility, or ostomy, as mentioned earlier. In particular, patients treated with immunomodulators or biologics require considerably more monitoring. Drug trough levels, complete blood counts, signs or symptoms of infection, and infusion reactions should be monitored frequently. Therefore, special management of high-risk patient groups is required for these situations. Dietitians can play an important role within the multidisciplinary team by assessing nutritional status, measuring dietary intake, and suggesting tailored oral or parenteral nutritional support in inpatients or outpatients. To increase patient adherence, the Severance Hospital IBD Clinic operates a follow-up telephone call system known as “Happy Call” for patients who miss outpatient clinic appointments and an additional telephone call service to provide pharmaceutical consultation for patients experiencing difficulty taking, or adhering to, prescribed medications. Various other activities can be conducted under the umbrella of patient care, and these methodologies integrated within the scope of the IBD center/clinic can improve approaches to standardizing patient management.
The patient outreach category is also based on collaboration among IBD center/clinic team members. IBD seminars, small group lectures, and other activities involving patient education or public relations should cover the diverse aspects of IBD treatment and the disease itself. Therefore, the assignment of activities is based on the needs and requirements of the IBD center/clinic team. Because IBD occurs mainly in younger individuals and due to rapidly evolving information technologies, it may be better to conduct patient outreach activities via online communication, such as social network services (SNS), rather than off-line lectures [33,34]. Moreover, the importance of electronic consultation via SNS or other internet platforms is even greater during the current coronavirus disease 2019 pandemic to ensure patient protection using the appropriate information. A practical example is uploading lecture clips on YouTube (http://www.youtube.com) and posting information sheets in online blogs. This may compensate for the lack of sufficient communication between doctors and patients in centers/clinics, playing a role in the dissemination of scientifically accurate information. IBD patients often experience emergency situations, such as acute abdominal pain, bleeding, and cramping, during which it can be difficult to decide whether to visit the emergency department [35]. For these situations, the Severance Hospital IBD Clinic provides medical staff contact information and emergency counseling via SNS as a patient outreach activity.
Finally, the system management category is closely aligned with patient care and outreach. Clinical staff members work in close collaboration to ensure that all aspects of the IBD center meet the needs of the patients and the clinic itself, including strategic directions, financial decisions, and educational and/or research programs. Thus, the typical IBD clinic conference addresses various issues pertaining to the continuous management of clinics. Additionally, to provide scholarly up-to-date education to IBD clinic staff members, residents, and fellows, conferences, journal reviews, and research meetings are conducted regularly as a component of the system management category
THE ROLE OF IBD NURSES
The most important resource for IBD clinic/center management is the IBD coordinator, more commonly known as the IBD nurse. Previous research has demonstrated that IBD nurses can even influence patient quality of life. Most clinic/center activities are usually initiated by IBD nurses, who are frequently affiliated with the department of gastroenterology because IBD patient care is generally provided by gastrointestinal physicians/specialists. IBD nurses offer patients consistent support by arranging clinical appointments and providing education, as well as organizing consultation schedules with other departments as needed. This is often described as a gatekeeper role, available under one roof—or “one time shopping”—at some hospitals. Therefore, IBD nurses must exhibit competence and expertise. Despite the need for professionalism, IBD nurses have access only to educational programs provided at the academic level (the Advanced Practice Provider Preceptor program of the Crohn’s & Colitis Foundation [https://site.crohnscolitisfoundation.org] and the European Crohn’s and Colitis Organisation IBD Nurse Education Program [https://ecco-ibd.eu/education/nurse-education-programme.html]); however, there is no official or national certification program. Most of these nurses rely solely on educational programs provided by academic gastroenterology congresses or patient seminars. Moreover, the division of duties among IBD nurses is not always clear. In Korea, the Korea Nurses Association has the authority to certify nurses and advanced practice nurses, but there is no certification available for gastrointestinal or IBD specialties. Generally, advanced practice nurses, registered nurses, and nurse practitioners in the gastrointestinal department play concurrent roles in IBD care. However, it is important to note that the certification and/or licensing of IBD nurses is anticipated to be formalized in the near future.
EFFECTIVE MANAGEMENT OF AN IBD CLINIC/CENTER
IBD is a complex and systematic disease that often requires multidisciplinary treatment. Therefore, an organized and controlled therapeutic approach is required [36]. Treatment schedules for IBD patients are generally managed by IBD nurses, who provide patients with consistent support, arrange clinic appointments and educational opportunities, and plan consultation schedules with other departments, as needed [37]. However, for several hospitals overseeing multiple IBD patients, it may be difficult for a single IBD nurse to handle all of these aspects. Hence, it is more effective to establish an IBD clinic/center in hospitals where IBD patients have feasible contact with IBD clinicians. Hashash et al. [38] suggested eight steps for developing an IBD treatment program for hospitalized patients, including the appointment of leadership, establishing staff support, archiving educational materials, and developing a training manual for volunteers. To design such a clinic/center within a hospital, organizational support, including the provision of staff members, budget, and space, is essential and requires the cooperation of many other departments within the hospital.
Adopting the systems of well-known IBD centers is not easy in general hospitals or in hospitals without available institutional support. Therefore, to improve the quality of care for IBD patients and effectively provide integrated treatment, efforts to organize these steps or integrate IBD clinic/center activities into the program require internal rather than external infrastructure. It is important to have flexibility so that IBD care programs can be executed according to each hospital’s situation and/or capabilities. For example, some hospitals can only run transition clinics based on cooperation between the gastroenterology and pediatric departments, whereas others can only prepare patient survey systems and educational materials focusing on patient outreach. All activities can be gathered and distributed according to the situation, as mentioned in Table 2. The key factor is that the programs are focused on ensuring patient safety and convenience based on the integration of leading department physicians and IBD nurses.
To develop a sustainable IBD patient care program, the following strategic elements should be considered: the number of patients; service staff sustainability and resiliency; scope of the activities, responsibilities of, and communication and coordination with staff members; clinical care space; and administrative processes [39]. Practically, the clinic’s own guidelines or standardized processes should be based on the consensus of all affiliated members. The simulation of program activities is an effective method for training team members in the management of any difficult situations and improving team performance in terms of communication, especially in resuscitation care or emergency situations [40]. The IBD clinic/center does not need to make decisions pertaining to patient care services. However, establishing a procedural flow to alleviate trial-and-error scenarios may be helpful.
Finally, for effective management, several metrics for clinics/centers should be determined to assess the quality of the care service and patient satisfaction [41]. These metrics may include the number of multidisciplinary care teams, number of dedicated clinic members, number of patient lectures, patient participation rate in seminars/lectures, rate of follow-up loss, adverse event metrics, IBD clinical trial/research metrics, and patient satisfaction measures. Any set of metrics is permitted according to the scope of the IBD care program activities. The analysis of these metrics should highlight any weak aspect of clinical management and guide the next steps in the operation of the center.
CONCLUSIONS
The prevalence and incidence rates of IBD in East Asian countries, including Korea, Taiwan, Japan, and China, have nearly reached those reported in Western countries. Accordingly, the number of clinical trials on, and level of physician interest in, the systematic care of IBD patients have increased and are expected to continue in the future. Most tertiary hospitals in Korea established IBD centers during the 2010s, and such centers are the most effective tools for resource integration. However, for greater flexibility, tailored programs should be established, rather than following the structure of larger centers according to the competencies and size of each hospital. Short-term goals to integrate resources related to patient care, patient outreach, and system management should be set (Table 2). Furthermore, a long-term goal is to modify and develop previous settings to ensure the quality of expert-based standard care. Thus, IBD treatment and patient care do not always require the formal establishment of a center; however, they must be incorporated into the general setting of each hospital as an adaptable program that can be adjusted to meet a wide range of outcomes.
Footnotes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Podolsky DK. Inflammatory bowel disease. N Engl J Med. 2002;347:417–429. doi: 10.1056/NEJMra020831. [DOI] [PubMed] [Google Scholar]
- 2.de Souza HS, Fiocchi C, Iliopoulos D. The IBD interactome: an integrated view of aetiology, pathogenesis and therapy. Nat Rev Gastroenterol Hepatol. 2017;14:739–749. doi: 10.1038/nrgastro.2017.110. [DOI] [PubMed] [Google Scholar]
- 3.Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142:46–54. doi: 10.1053/j.gastro.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 4.King D, Reulen RC, Thomas T, et al. Changing patterns in the epidemiology and outcomes of inflammatory bowel disease in the United Kingdom: 2000–2018. Aliment Pharmacol Ther. 2020;51:922–934. doi: 10.1111/apt.15701. [DOI] [PubMed] [Google Scholar]
- 5.Chang S, Hudesman D. First-line biologics or small molecules in inflammatory bowel disease: a practical guide for the clinician. Curr Gastroenterol Rep. 2020;22:7. doi: 10.1007/s11894-020-0745-y. [DOI] [PubMed] [Google Scholar]
- 6.Shen B. Interventional IBD: the role of endoscopist in the multidisciplinary team management of IBD. Inflamm Bowel Dis. 2018;24:298–309. doi: 10.1093/ibd/izx058. [DOI] [PubMed] [Google Scholar]
- 7.Knowles SR, Graff LA, Wilding H, Hewitt C, Keefer L, Mikocka-Walus A. Quality of life in inflammatory bowel disease: a systematic review and meta-analyses: part I. Inflamm Bowel Dis. 2018;24:742–751. doi: 10.1093/ibd/izx100. [DOI] [PubMed] [Google Scholar]
- 8.Mao R, Hu PJ. The future of IBD therapy: where are we and where should we go next? Dig Dis. 2016;34:175–179. doi: 10.1159/000443135. [DOI] [PubMed] [Google Scholar]
- 9.Kaplan GG, Windsor JW. The four epidemiological stages in the global evolution of inflammatory bowel disease. Nat Rev Gastroenterol Hepatol. 2021;18:56–66. doi: 10.1038/s41575-020-00360-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jung YS, Han M, Kim WH, Park S, Cheon JH. Incidence and clinical outcomes of inflammatory bowel disease in South Korea, 2011–2014: a nationwide population-based study. Dig Dis Sci. 2017;62:2102–2112. doi: 10.1007/s10620-017-4640-9. [DOI] [PubMed] [Google Scholar]
- 11.Kim HJ, Hann HJ, Hong SN, et al. Incidence and natural course of inflammatory bowel disease in Korea, 2006–2012: a nationwide population-based study. Inflamm Bowel Dis. 2015;21:623–630. doi: 10.1097/MIB.0000000000000313. [DOI] [PubMed] [Google Scholar]
- 12.Ng SC, Kaplan GG, Tang W, et al. Population density and risk of inflammatory bowel disease: a prospective population-based study in 13 countries or regions in Asia-Pacific. Am J Gastroenterol. 2019;114:107–115. doi: 10.1038/s41395-018-0233-2. [DOI] [PubMed] [Google Scholar]
- 13.Yen HH, Weng MT, Tung CC, et al. Epidemiological trend in inflammatory bowel disease in Taiwan from 2001 to 2015: a nationwide populationbased study. Intest Res. 2019;17:54–62. doi: 10.5217/ir.2018.00096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ng SC, Tang W, Ching JY, et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asia-pacific Crohn’s and colitis epidemiology study. Gastroenterology. 2013;145:158–165. doi: 10.1053/j.gastro.2013.04.007. [DOI] [PubMed] [Google Scholar]
- 15.Mak WY, Zhao M, Ng SC, Burisch J. The epidemiology of inflammatory bowel disease: East meets West. J Gastroenterol Hepatol. 2020;35:380–389. doi: 10.1111/jgh.14872. [DOI] [PubMed] [Google Scholar]
- 16.Kwak MS, Cha JM, Lee HH, et al. Emerging trends of inflammatory bowel disease in South Korea: a nationwide population-based study. J Gastroenterol Hepatol. 2019;34:1018–1026. doi: 10.1111/jgh.14542. [DOI] [PubMed] [Google Scholar]
- 17.Park SH, Kim YJ, Rhee KH, et al. A 30-year trend analysis in the epidemiology of inflammatory bowel disease in the Songpa-Kangdong district of Seoul, Korea in 1986–2015. J Crohns Colitis. 2019;13:1410–1417. doi: 10.1093/ecco-jcc/jjz081. [DOI] [PubMed] [Google Scholar]
- 18.Ng SC, Leung WK, Shi HY, et al. Epidemiology of inflammatory bowel disease from 1981 to 2014: results from a territory-wide population-based registry in Hong Kong. Inflamm Bowel Dis. 2016;22:1954–1960. doi: 10.1097/MIB.0000000000000846. [DOI] [PubMed] [Google Scholar]
- 19.Hong SJ, Cho SM, Choe BH, et al. Characteristics and incidence trends for pediatric inflammatory bowel disease in Daegu-Kyungpook province in Korea: a multi-center study. J Korean Med Sci. 2018;33:e132. doi: 10.3346/jkms.2018.33.e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baek SJ, Lee KY, Song KH, Yu CS. Current status and trends in inflammatory bowel disease surgery in Korea: analysis of data in a nationwide registry. Ann Coloproctol. 2018;34:299–305. doi: 10.3393/ac.2018.07.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park S, Noh YH, Rha SY, Kim WH, Cheon JH. Institutional board review for clinical investigations on inflammatory bowel diseases: a single-center study. Intest Res. 2015;13:274–281. doi: 10.5217/ir.2015.13.3.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Verstockt B, Ferrante M, Vermeire S, Van Assche G. New treatment options for inflammatory bowel diseases. J Gastroenterol. 2018;53:585–590. doi: 10.1007/s00535-018-1449-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ma C, Battat R, Jairath V, Vande Casteele N. Advances in therapeutic drug monitoring for small-molecule and biologic therapies in inflammatory bowel disease. Curr Treat Options Gastroenterol. 2019;17:127–145. doi: 10.1007/s11938-019-00222-9. [DOI] [PubMed] [Google Scholar]
- 24.Ferman M, Lim AH, Hossain M, Siow GW, Andrews JM. Multidisciplinary team meetings appear to be effective in inflammatory bowel disease management: an audit of process and outcomes. Intern Med J. 2018;48:1102–1108. doi: 10.1111/imj.13965. [DOI] [PubMed] [Google Scholar]
- 25.Morar P, Read J, Arora S, et al. Defining the optimal design of the inflammatory bowel disease multidisciplinary team: results from a multicentre qualitative expert-based study. Frontline Gastroenterol. 2015;6:290–297. doi: 10.1136/flgastro-2014-100549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fader DJ, Wise CG, Normolle DP, Johnson TM. The multidisciplinary melanoma clinic: a cost outcomes analysis of specialty care. J Am Acad Dermatol. 1998;38(5 Pt 1):742–751. doi: 10.1016/s0190-9622(98)70203-8. [DOI] [PubMed] [Google Scholar]
- 27.Burton S, Brown G, Daniels IR, et al. MRI directed multidisciplinary team preoperative treatment strategy: the way to eliminate positive circumferential margins? Br J Cancer. 2006;94:351–357. doi: 10.1038/sj.bjc.6602947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eveleigh RM, Muskens E, van Ravesteijn H, van Dijk I, van Rijswijk E, Lucassen P. An overview of 19 instruments assessing the doctor-patient relationship: different models or concepts are used. J Clin Epidemiol. 2012;65:10–15. doi: 10.1016/j.jclinepi.2011.05.011. [DOI] [PubMed] [Google Scholar]
- 29.Best WR, Becktel JM, Singleton JW, Kern F., Jr Development of a Crohn’s disease activity index: National Cooperative Crohn’s Disease Study. Gastroenterology. 1976;70:439–444. [PubMed] [Google Scholar]
- 30.Thia KT, Sandborn WJ, Lewis JD, et al. Defining the optimal response criteria for the Crohn’s disease activity index for induction studies in patients with mildly to moderately active Crohn’s disease. Am J Gastroenterol. 2008;103:3123–3131. doi: 10.1111/j.1572-0241.2008.02176.x. [DOI] [PubMed] [Google Scholar]
- 31.Lewis JD, Chuai S, Nessel L, Lichtenstein GR, Aberra FN, Ellenberg JH. Use of the noninvasive components of the Mayo score to assess clinical response in ulcerative colitis. Inflamm Bowel Dis. 2008;14:1660–1666. doi: 10.1002/ibd.20520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cheon JH, Han DS, Park JY, et al. Development, validation, and responsiveness of a novel disease activity index for intestinal Behcet’s disease. Inflamm Bowel Dis. 2011;17:605–613. doi: 10.1002/ibd.21313. [DOI] [PubMed] [Google Scholar]
- 33.Chan WS, Leung AY. Use of social network sites for communication among health professionals: systematic review. J Med Internet Res. 2018;20:e117. doi: 10.2196/jmir.8382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Farag M, Bolton D, Lawrentschuk N. Use of YouTube as a resource for surgical education: clarity or confusion. Eur Urol Focus. 2020;6:445–449. doi: 10.1016/j.euf.2019.09.017. [DOI] [PubMed] [Google Scholar]
- 35.Burg MD, Riccoboni ST, Nusbaum J, Gupta N. Management of inflammatory bowel disease flares in the emergency department [digest] Emerg Med Pract. 2017;19(11 Suppl Points & Pearls):S1–S2. [PubMed] [Google Scholar]
- 36.Ye BD, Travis S. Improving the quality of care for inflammatory bowel disease. Intest Res. 2019;17:45–53. doi: 10.5217/ir.2018.00113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hernandez-Sampelayo P, Seoane M, Oltra L, et al. Contribution of nurses to the quality of care in management of inflammatory bowel disease: a synthesis of the evidence. J Crohns Colitis. 2010;4:611–622. doi: 10.1016/j.crohns.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 38.Hashash JG, Sigal R, Wein-Levy P, Szigethy EM, Merusi JJ, Regueiro MD. Inflammatory bowel disease (IBD) connect: a novel volunteer program for hospitalized patients with IBD and their families. Inflamm Bowel Dis. 2016;22:2748–2753. doi: 10.1097/MIB.0000000000000952. [DOI] [PubMed] [Google Scholar]
- 39.Finlay E, Rabow MW, Buss MK. Filling the gap: creating an outpatient palliative care program in your institution. Am Soc Clin Oncol Educ Book. 2018;38:111–121. doi: 10.1200/EDBK_200775. [DOI] [PubMed] [Google Scholar]
- 40.Murphy M, Curtis K, McCloughen A. What is the impact of multidisciplinary team simulation training on team performance and efficiency of patient care?: an integrative review. Australas Emerg Nurs J. 2016;19:44–53. doi: 10.1016/j.aenj.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 41.Anderson JB, Chowdhury D, Connor JA, et al. Optimizing patient care and outcomes through the congenital heart center of the 21st century. Congenit Heart Dis. 2018;13:167–180. doi: 10.1111/chd.12575. [DOI] [PubMed] [Google Scholar]