To the Editor: Connections between diet and skin disease have long piqued the interest of patients and physicians.1,2 While traditionally, acne has been the focus, there has been a recent turn toward psoriasis,3 connected to multiple comorbidities, including diabetes mellitus, atherosclerosis, and obesity.2,4 As a result, patients with psoriasis may express interest in dietary interventions to improve their skin and associated diseases.3,5 This study aimed to assess which dietary interventions and supplements are popular among patients with psoriasis and may lead to improved psoriasis.
An Institutional Review Board-approved 30-question survey was offered voluntarily to patients with psoriasis at the University of Iowa Dermatology Clinic and Saint Louis University Dermatology Clinic from July 2019 to January 2021. The inclusion criteria included patients over 18 years of age with clinically defined psoriasis. Table I demonstrates patient perceptions of psoriasis subtype, severity, and demographics.
Table I.
Demographics and characteristics of patients with psoriasis responding to the survey
| Variable | (N = 270) |
|---|---|
| n (%) | |
| Age | |
| 18-25 y | 16 (5.97) |
| 25-35 y | 37 (13.81) |
| 35-45 y | 40 (14.93) |
| 45-55 y | 55 (20.52) |
| 55 y or greater | 120 (44.78) |
| Gender | |
| Male | 92 (34.20) |
| Female | 177 (65.80) |
| Psoriasis severity | |
| Mild | 116 (43.94) |
| Moderate | 87 (32.95) |
| Severe | 61 (23.11) |
| Psoriasis subtype | |
| Plaque psoriasis | 141 (54.86) |
| Guttate psoriasis | 9 (3.50) |
| Flexural/inverse psoriasis | 6 (2.33) |
| Scalp/nail psoriasis | 23 (8.95) |
| Two or more | 78 (30.35) |
| Race | |
| Caucasian (White) | 240 (89.55) |
| African American (Black) | 20 (7.46) |
| Asian/Pacific Islander | 1 (0.37) |
| American Indian/Alaskan | 2 (0.75) |
| Other | 5 (1.87) |
| Body mass index | |
| Underweight | 5 (1.94) |
| Normal | 58 (22.48) |
| Overweight | 67 (25.97) |
| Obese (class 1-3) | 128 (49.61) |
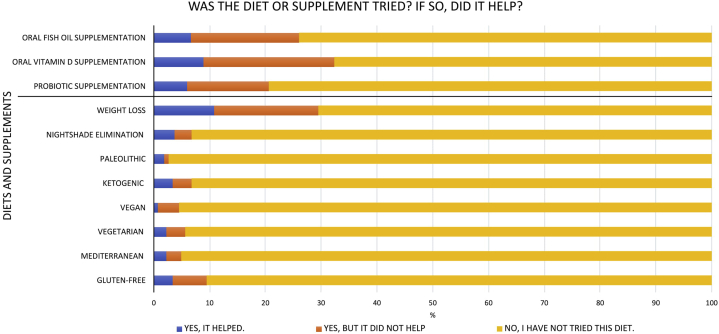
Of the 430 individuals that were offered the survey, 270 completed it with a 62.8% response rate. A total of 79 of 268 (29.5%) participants attempted weight loss as a dietary intervention, with 29 of 79 (36.7%) participants indicating that this helped their psoriasis severity (Fig 1). Participants endorsing dietary experimentation noted improvement in psoriasis with ketogenic (9 of 18 participants [50%]), Mediterranean (6 of 13 [46%]), vegetarian (6 of 15 [40%]), and gluten-free (9 of 25 [36%]) diets. The most tried supplement was oral vitamin D (87 of 269 [32%]), followed by oral fish oil (70 of 269 [26%]) and oral probiotics (55 of 267 [21%]). Of these supplements, probiotic use produced the greatest positive skin response (16 of 55 [29%]) with vitamin D (24 of 87 [27.6%]) and fish oil (18 of 70 [25.7%]) following closely.
Fig 1.
Distribution of diets and supplements attempted by patients with psoriasis responding to the survey.
Out of all participants, 41.85% did not try any of the diets or supplements surveyed, while 52.2% attempted between 1 and 4 interventions and only 5.9% tried 5 or more. Wilcoxon tests showed that participants with 2 or more subtypes of psoriasis (plaque, guttate, flexural, scalp/nail) tried more diets or supplements than those without (P = .03). Additionally, participants younger than 55 years sought to try more diets or supplements than those aged 55 years or older (P = .02). χ2 testing between body mass index and psoriasis severity indicated that participants who were categorized as obese (body mass index > 30.0), had a higher rate of moderate to severe psoriasis than those who were not obese (P < .01). Patients with obesity also increasingly reported having 2 or more subtypes of psoriasis than nonobese counterparts (P < .05).
Diet remains an important therapeutic intervention that patients with psoriasis attempt alongside medical management. This study suggests that younger patients may be more likely to attempt dietary interventions with relevant supplements being probiotics, vitamin D, and fish oil. Weight loss helped in roughly a third of those who attempted it. The limitations of this study include low generalizability as the majority of the participants were Caucasian and female as well as the possibility of response bias. Thus, further investigation on a larger scale expanding to other geographical regions is recommended to improve the understanding of how particular dietary modifications can help patients with psoriasis manage their condition.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: This study was supported in part by The University of Iowa Clinical and Translational Science Award granted with funds from the NIH (UL1TR002537).
IRB approval status: This study was reviewed and approved by the University of Iowa Institutional Review Board, approval #201906847 and determined to qualify for exempt status on July 2, 2019. This study was also reviewed and approved by Saint Louis University Institutional Review Board, approval #30968 and determined to qualify for exempt status on May 4, 2020.
References
- 1.Murzaku E.C., Bronsnick T., Rao B.K. Diet in dermatology: part II. Melanoma, chronic urticaria, and psoriasis. J Am Acad Dermatol. 2014;71(6):1053.e1–1053.e16. doi: 10.1016/j.jaad.2014.06.016. [DOI] [PubMed] [Google Scholar]
- 2.Duarte G., Barbosa Rosa. The management of psoriasis through diet. Psoriasis (Auckl) 2012;2012:45–53. [Google Scholar]
- 3.Ford A., Siegel M., Bagel J. Dietary recommendations for adults with psoriasis or psoriatic arthritis from the Medical Board of the National Psoriasis Foundation: a systematic review. JAMA Dermatol. 2018;154(8):934–950. doi: 10.1001/jamadermatol.2018.1412. [DOI] [PubMed] [Google Scholar]
- 4.Debbaneh M., Millsop J.W., Bhatia B.K., Koo J., Liao W. Diet and psoriasis, part I: impact of weight loss interventions. J Am Acad Dermatol. 2014;71(1):133–140. doi: 10.1016/j.jaad.2014.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Afifi L., Danesh M.J., Lee K.M. Dietary behaviors in psoriasis: patient-reported outcomes from a US national survey. Dermatol Ther (Heidelb) 2017;7(2):227–242. doi: 10.1007/s13555-017-0183-4. [DOI] [PMC free article] [PubMed] [Google Scholar]