Abstract
Background
Evidence from previous public health emergencies indicates that adults with disabilities have higher risk for morbidity (physical and mental) and mortality than adults without disabilities.
Objective
To provide estimates of mental health indicators and stressors for US adults by disability status during April and May 2020, shortly following the emergence of the COVID-19 pandemic.
Methods
We analyzed data from Porter Novelli View 360 opt-in Internet panel survey conducted during the weeks of April 20th and May 18th, 2020 among 1004 English-speaking adults aged ≥18 years without and with disabilities (serious difficulty with hearing, vision, cognition, or mobility; any difficulty with self-care or independent living). Weighted logistic regression was used to test for significant differences between calculated prevalence estimates at the P ≤ .05 level.
Results
One in four adults reported any disability. Adults with any disability were significantly more likely than adults without disability to report current depressive symptoms, frequent mental distress, suicidal ideation, and COVID-19-related initiated or increased substance use (all p values < .0001). Adults with disabilities also reported significantly higher levels of stressors, such as access to health care services (p < .0001), difficulty caring for their own (or another’s) chronic condition (p < .0001), emotional or physical abuse from others (p < .001), and not having enough food (p < .01).
Conclusions
The disproportionately high levels of poor mental health indicators among adults with disabilities as compared to those without highlight the importance of delivering timely mental health screening and treatment/intervention during and after the COVID-19 pandemic to persons with disabilities.
Keywords: Disabilities, Coronavirus, Mental health, Stress, Health disparities
Introduction
More than 61 million adults in the United States report living with a disability.1 Among these, 11.1 million have a vision disability; 14.0 million have a hearing disability; 25.8 million have a cognitive disability; 32.8 million have a mobility disability; 8.9 million have a self-care disability; and 16.2 million have an independent living disability (i.e., doing errands alone).1 Adults with disabilities have been found to be at increased risk for morbidity (physical and mental) and mortality during previous emergency responses due to pre-existing health disparities and social vulnerabilities, such as poverty.2 , 3 The disproportionate morbidity and mortality from public health emergencies, including the COVID-19 pandemic, experienced by persons with disabilities can also create a negative or synergistic impact on their mental health when exacerbated by psychosocial stressors.4
Mental health disorders are disproportionately prevalent among adults with disabilities, and may be either the underlying cause of disability or a comorbid condition.5 , 6 In fact, depression has been identified as one of the most common secondary conditions associated with disability.7 Similar to the general population,8 depression among adults living with a disability may contribute to poor self-care practices, increased social isolation, adverse health behaviors, poorer quality of life, and higher health care utilization and costs.9, 10, 11, 12
Stressors, such as worry over the care of existing health conditions, access to needed treatments, supplies, or medications, or supports and services may contribute to worsening mental health and adverse health outcomes.13 While disability alone may not increase the risk for severe COVID-19, some adults with disabilities may have underlying medical conditions (e.g., diabetes, heart disease, stroke, cancer, obesity, lung disease [not an exhaustive list]) that potentially increase the risk for severe illness from COVID-19.13, 14, 15, 16 Adults requiring caregiver assistance, including those living in congregate care settings and those with limited mobility, may have increased risk of exposure to SARS-CoV-2, the virus that causes COVID-19, because they need the assistance of caregivers to complete activities of daily living, such as bathing, dressing, and eating, and thus, might be unable to consistently implement the practice of physical distancing.17 , 18 Adults with cognitive and intellectual and developmental disabilities may be at increased risk of exposure to SARS-CoV-2 because of difficulty accurately understanding or adhering to guidance to reduce the risk for exposure to SARS-CoV-2 (e.g., handwashing, physical distancing, wearing a mask).19 , 20 Finally, adults with disabilities who have a reduced ability to communicate may have concerns about being denied reasonable access to support persons in the hospital during COVID-19 and, as a consequence, delay needed health care.13 , 21
Concerns over medical rationing or access to needed support persons during the COVID-19 pandemic are not unfounded for many adults with disabilities and may increase the risk of stress and poor mental and physical health.13 , 22 , 23 The Office of Civil Rights (OCR) continues to investigate complaints from national and state disability groups on the discriminatory practices of covered entities (i.e., Department of Health and Human Services funded health programs or activities) during the COVID-19 public health emergency.21 , 23, 24, 25 The OCR has enforced federal civil rights laws in several states to ensure, for example, that people with dementia, intellectual disabilities, and other disabilities would not be denied a ventilator and other care simply because of those conditions.23, 24, 25 Other stressors exacerbated by the COVID-19 pandemic, such as social isolation, food insecurities (e.g., lack of financial resources), family stressors (e.g., caregiving responsibilities for children or another adult in the household), substance misuse, or physical or emotional abuse, may cause further stress and exacerbate existing, often complex medical conditions.2 , 7 , 13
There is limited research on the impact of public health emergencies such as the COVID-19 pandemic on the mental health of adults with disabilities.13 Moreover, psychosocial and social determinants of health (SDOH) stressors, e.g., stress or worry about obtaining adequate food or housing, related to the COVID-19 pandemic among adults with disabilities in the United States have yet to be fully explored. This type of exploration may inform current and future disability inclusive emergency response and recovery efforts. Thus, the objective of this study is to provide estimates of mental health indicators and stressors for US adults by disability status during April and May 2020 of the COVID-19 pandemic.
Methods
Data came from the Porter Novelli (PN) View 360, a nationwide, weekly opt-in Internet panel survey of US adults ≥18 years (http://styles.porternovelli.com/pn-view-panels). The PN View 360 survey has been used to provide insights into the behaviors and physical and mental health status of the public during the COVID-19 pandemic.26 , 27 For this study, we utilized two independent weeks of data, collected a week each in April and May 2020 (total n = 1004). The survey was administered by ENGINE Insights, a market research company, in English using the Lucid platform which provides access to a compilation of opt-in sample sources.28 Panel members who had not taken a survey in the 20 waves prior to survey administration were eligible to participate (i.e., to prevent “serial or professional” panel participants from qualifying for back to back studies).
Respondents were informed that their answers were being used for market research and they could refuse to answer any question. Data quality filters designed to prevent multiple responses from the same panelist and to improve accuracy (e.g., prevent speeding) are embedded in every survey. Demographic caps (quota sampling) were set to prevent unbalanced participation, and statistical weighting was used during the analysis to match the December 2019 Current Population Survey proportions, so the sample represented the US population by sex, age, region, race/ethnicity, and education. The Centers for Disease Control and Prevention (CDC) obtained the PN View 360 survey data from PN through a subscription license. No personal identifiers were included in the data file provided to CDC. While PN and its vendors are not subject to CDC Institutional Review Board review, they do adhere to all professional standards and codes of conduct set forth by the Council of American Survey Research Organizations. This activity was reviewed by CDC and was conducted consistent with applicable federal law (i.e., 45 C.F R. part 4601 [b][2]) and CDC policy.
Measures
Disability status and types
The PN View 360 included six survey items to measure disability from a functional perspective consistent with the International Classification of Functioning, Disability, and Health.29 Disability status and types were assessed with a positive response in ≥1 of the six response categories following the question: “Which, if any of the following apply to you?” (response categories: I am deaf or have serious difficulty hearing (hearing); I am blind or have serious difficulty seeing, even when wearing glasses (vision); Because of a physical, mental, or emotional condition, I have serious difficulty concentrating, remembering, or making decisions (cognition); I have serious difficulty walking or climbing stairs (mobility); I have difficulty dressing or bathing (self-care); and Because of a physical, mental, or emotional condition, I have difficulty doing errands alone such as visiting a doctor’s office or shopping (independent living)).
Outcomes
Survey questions asked about indicators of mental health conditions and sources of stress and worry.
Indicators of mental health conditions included current depressive symptoms, frequent mental distress (FMD), suicidal ideation, and initiated or increased substance use to cope with stress or emotions related to COVID-19. Current depressive symptoms were assessed with the Patient Health Questionnaire 8 (PHQ-8) screener.30 The PHQ-8 is adapted from the 9-item scale (i.e. PHQ-9), which is based on nine criteria aligned with the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition31 diagnosis of depressive disorders. The PHQ-8 survey question was standardized to be similar to how other national surveys32 have included the stem question “Over the last 2 weeks, how often have you been bothered by any of the following problems?” followed by the eight symptoms of depression30 “Little interest or pleasure in doing things; Feeling down, depressed, or hopeless; Trouble falling or staying asleep, or sleeping too much; Feeling tired or having little energy; Poor appetite or overeating; Feeling bad about yourself--or that you are a failure or have let yourself or your family down; Trouble concentrating on things, such as reading the newspaper or watching television; and Moving or speaking so slowly that other people have noticed. Or the opposite—"being so fidgety or restless that you have been moving around a lot more than usual.” The response categories were ‘nearly every day’, ‘more than half the days’, ‘several days’, and ‘not at all’. The modified response set was converted back to the original PHQ-8 response set: 0–1 day = ‘not at all’; 2–6 days = ‘several days’; 7–11 days = ‘more than half the days‘; and 12–14 days = ‘nearly every day’, with points (0–3) assigned to each category, respectively. The scores for each item were summed to produce a total score between 0 and 24 points. Respondents were considered to have current depressive symptoms (i.e., past 2 weeks) if their total score was ≥10, which has an 88% sensitivity and 88% specificity for major depression.30
Mental distress was assessed with the survey question “Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?” Respondents were considered to have FMD if they reported their mental health was not good for ≥14 days. Suicidal ideation was assessed with the survey question “At any time in the past 30 days, did you seriously think about trying to kill yourself?” Initiated or increased substance use was assessed with the survey question “Have you started or increased using substances to help you cope with stress or emotions during the COVID-19 pandemic? Substance use includes alcohol, legal or illegal drugs, or prescription drugs that are taken in a way not recommended by your doctor.”
The question used to assess stress and worry related to psychosocial stressors, SDOH stressors, and interpersonal violence or household stress was “Which of any of the items below are a source of stress and worry?” Responses categorized as psychosocial stressors were: Getting sick from coronavirus/infecting others; Health of my family and loved ones; Being exposed to COVID-19 through my work or workplace; Feeling isolated or lonely; Death of a loved one/people dying; Difficulty caring for a chronic condition (yours or others); and Stigma or discrimination (from being blamed for spreading COVID-19). Responses categorized as SDOH stressors were: Loss of job or income; Getting the health care services I need (i.e., doctor, dentist); Not enough food; Unstable housing or unable to pay rent; and Childcare challenges/Dealing with schooling kids at home. Responses categorized as interpersonal violence or household stress were: Emotional or physical abuse from others and Conflict or stress within the household.
Covariates
Standard demographic questions were included to examine sex, age (18–34, 35–64, ≥65 years), race/ethnicity (non-Hispanic White, non-Hispanic Black or African American, Hispanic or Latino, and other non-Hispanic race/multirace), educational attainment (≤high school, some college/technical school, ≥ college), employment status (yes/no), marital status (married/living with a partner, divorced/separated/widowed, never married), total household income before taxes in 2019 (<$30 K, $30 K-<$60 K, $60 K-<$100 K, ≥$100 K), US Census region (Northeast, Midwest, South, West), type of community (urban, suburban, rural), and underlying medical conditions that increase the risk of severe illness associated with COVID-19 (lung condition [like moderate to severe asthma]; heart disease; diabetes; weakened immune system; chronic kidney or liver disease; obesity).14
Statistical analyses
We used SAS software (Version 9.4; SAS Institute) to calculate weighted prevalence estimates with 95% confidence intervals for sociodemographic characteristics, medical conditions, mental health indicators, and stressors for adults without and with any disability (≥1 type); and for mental health indicators, by non-mutually exclusive disability type. We used SAS-callable SUDAAN (Version 11.0.3; RTI International) to calculate weighted adjusted prevalence estimates and to test for differences between calculated prevalence estimates. Statistical inferences were based on a P ≤ .05. Because there was little difference between the unadjusted and adjusted estimates we chose to present the unadjusted models (see Appendices A and B for adjusted model estimates).
Results
One in four (26.6%) US adults in the survey reported any disability (Table 1 ). Mobility was the most common disability type (11.0%), followed by cognition (10.4%), independent living (9.6%), self-care (4.8%), hearing (3.1%), and vision (2.6%). Men reported a higher prevalence of any disability compared to women (p < .05), as did Hispanic adults compared to other non-Hispanic racial/ethnic groups (p < .01 for all), adults who were not employed compared to adults who were employed (p < .05), adults with a total household income <$30 K compared to adults with higher incomes (<$30 K vs $30 K-<$60 K, $60 K-<$100 K, and ≥$100 K, respectively; p < .05, p < .01, and p < .05, respectively), and adults who lived in an urban community compared to those who reported living in rural or suburban communities (p < .01 and p < .0001, respectively). No differences were found in the prevalence of any disability by age group, educational attainment, marital status, or US Census region. Table 2 compares the prevalence of selected underlying medical conditions associated with severe illness from COVID-19 among adults with and without any disability. Adults with any disability were more likely to report each condition (p < .0001 for all). Diabetes and obesity were the most common chronic medical conditions reported by both adults with and without disabilities, followed generally by lung condition, weakened immune system, heart disease, and chronic kidney or liver disease.
Table 1.
Weighted prevalence estimates of disability by selected demographic characteristics among adults aged ≥18 years — Porter Novelli View 360 Internet survey, United States, April and May 2020.
|
Characteristic |
Total |
Adults with no disability |
Adults with any disabilitya |
|||
|---|---|---|---|---|---|---|
| Unweighted n | Weighted % (95% CI) | Unweighted n | Weighted % (95% CI) | Unweighted n | Weighted % (95% CI) | |
| Total | 1004 | 100% | 748 | 73.4 (70.5–76.4) | 256 | 26.6 (23.6–29.5) |
| Sex | ||||||
| Male | 502 | 48.3 (45.0–51.6) | 358 | 70.1 (65.7–74.5) | 144 | 29.9 (25.5–34.3) |
| Female | 502 | 51.7 (48.4–55.0) | 390 | 76.6 (72.6–80.5) | 112 | 23.4 (19.5–27.4) |
| Age group | ||||||
| 18–34 years | 316 | 29.7 (26.7–32.6) | 237 | 72.8 (67.5–78.1) | 79 | 27.2 (21.9–32.5) |
| 35–64 years | 534 | 49.8 (46.5–53.1) | 389 | 71.8 (67.6–75.9) | 145 | 28.2 (24.1–32.4) |
| ≥65 years | 154 | 20.6 (17.7–23.5) | 122 | 78.5 (71.7–85.2) | 32 | 21.5 (14.8–28.3) |
| Race | ||||||
| Hispanic | 118 | 16.3 (13.6–18.9) | 72 | 60.3 (51.2–69.4) | 46 | 39.7 (30.6–48.8) |
| White, non-Hispanic | 657 | 63.5 (60.2–66.7) | 497 | 75.4 (71.9–78.9) | 160 | 24.6 (21.1–28.1) |
| Black, non-Hispanic | 100 | 11.9 (9.6–14.1) | 77 | 78.1 (69.9–86.3) | 23 | 21.9 (13.7–30.1) |
| Other, non-Hispanicb | 129 | 8.4 (6.9–9.9) | 102 | 77.4 (69.4–85.4) | 27 | 22.6 (14.6–30.6) |
| Education | ||||||
| ≤ High school | 321 | 39.5 (36.2–42.8) | 236 | 72.5 (67.3–77.6) | 85 | 27.5 (22.4–32.7) |
| Some college/technical school | 262 | 26.8 (23.9–29.7) | 186 | 70.5 (64.7–76.3) | 76 | 29.5 (23.7–35.3) |
| ≥ College | 421 | 33.7 (30.7–36.7) | 326 | 76.9 (72.5–81.3) | 95 | 23.1 (18.7–27.5) |
| Employment status | ||||||
| Not employedc | 417 | 45.6 (42.2–48.9) | 296 | 69.8 (65.1–74.5) | 121 | 30.2 (25.5–34.9) |
| Employedd | 587 | 54.4 (51.1–57.8) | 452 | 76.5 (72.7–80.3) | 135 | 23.5 (19.7–27.3) |
| Total household incomee | ||||||
| < $30,000 | 255 | 28.4 (25.3–31.4) | 171 | 66.2 (60.0–72.3) | 84 | 33.8 (27.7–40.0) |
| $30,000-< $59,999 | 254 | 27.2 (24.2–30.2) | 194 | 75.5 (69.8–81.3) | 60 | 24.5 (18.7–30.2) |
| $60,000- $99,999 | 245 | 23.7 (20.9–26.4) | 191 | 77.6 (72.0–83.2) | 54 | 22.4 (16.8–28.0) |
| ≥ $100,000 | 250 | 20.8 (18.3–23.3) | 192 | 76.0 (70.1–81.8) | 58 | 24.0 (18.2–29.9) |
| Marital status | ||||||
| Divorced/separated/widowed | 133 | 15.6 (13.1–18.2) | 95 | 70.3 (62.1–78.6) | 38 | 29.7 (21.4–37.9) |
| Married/member of unmarried couple | 558 | 53.8 (50.4–57.1) | 415 | 74.0 (70.0–77.9) | 143 | 26.0 (22.1–30.0) |
| Never married | 313 | 30.6 (27.6–33.6) | 238 | 74.2 (68.8–79.5) | 75 | 25.8 (20.5–31.2) |
| US Census regionf | ||||||
| South | 374 | 37.6 (34.4–40.9) | 266 | 70.4 (65.4–75.4) | 108 | 29.6 (24.6–34.6) |
| Northeast | 185 | 17.8 (15.3–20.3) | 135 | 71.9 (64.9–78.9) | 50 | 28.1 (21.1–35.1) |
| West | 240 | 23.7 (20.9–26.6) | 189 | 76.2 (70.3–82.2) | 51 | 23.8 (17.8–29.7) |
| Midwest | 205 | 20.8 (18.1–23.5) | 158 | 77.1 (71.0–83.2) | 47 | 22.9 (16.8–29.0) |
| Type of community | ||||||
| Urban | 316 | 30.4 (27.4–33.4) | 206 | 62.5 (56.6–68.3) | 110 | 37.5 (31.7–43.4) |
| Rural | 206 | 21.3 (18.6–24.0) | 156 | 74.7 (68.4–81.1) | 50 | 25.3 (18.9–31.6) |
| Suburban | 482 | 48.3 (45.0–51.6) | 386 | 79.8 (75.9–83.7) | 96 | 20.2 (16.3–24.1) |
Abbreviation: CI = confidence interval.
Disability was assessed with a positive response in ≥1 of the six response categories following the question “Which, if any of the following apply to you?” (response categories: I am deaf or have serious difficulty hearing (hearing); I am blind or have serious difficulty seeing, even when wearing glasses (vision); Because of a physical, mental, or emotional condition, I have serious difficulty concentrating, remembering, or making decisions (cognition); I have serious difficulty walking or climbing stairs (mobility); I have difficulty dressing or bathing (self-care); and Because of a physical, mental, or emotional condition, I have difficulty doing errands alone such as visiting a doctor’s office or shopping (independent living).
Other non-Hispanic race includes Native American or Alaska Native persons, Asian persons, and persons of another race or more than one race; these were combined because of small sample size.
Student, homemaker, retired, or not currently employed.
Working full-time, part-time, or self-employed.
Total household income before taxes in 2019.
U.S. Census region: South - Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia; Northeast - Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont; West – Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Wyoming, and Washington; Midwest - Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin.
Table 2.
Weighted prevalence estimates of chronic medical conditionsa that increase the risk of severe illness associated with COVID-19 among adults aged ≥18 years by disability status — Porter Novelli View 360 Internet survey, United States, April and May 2020.
| Diabetes | Obesityb | Lung conditionc | Weakened immune system | Heart disease | Chronic kidney or liver disease | |
|---|---|---|---|---|---|---|
| Total | ||||||
| Unweighted n | 115 | 124 | 85 | 56 | 41 | 31 |
| Weighted % (95% CI) | 12.0 (9.8–14.2) | 12.4 (10.2–14.6) | 8.7 (6.8–10.6) | 5.5 (4.0–7.0) | 4.1 (2.8–5.4) | 3.6 (2.3–5.0) |
| Any disabilityd | ||||||
| Unweighted n | 58 | 54 | 47 | 41 | 25 | 22 |
| Weighted % (95% CI) | 22.6 (17.1–28.2)∗ | 20.8 (15.4–26.2)∗ | 19.1 (14.0–24.3)∗ | 15.6 (10.9–20.4)∗ | 9.6 (5.8–13.4)∗ | 9.5 (5.5–13.6)∗ |
| No disability | ||||||
| Unweighted n | 57 | 70 | 38 | 15 | 16 | 9 |
| Weighted % (95% CI) | 8.2 (6.0–10.4) | 9.4 (7.1–11.6) | 4.9 (3.3–6.6) | 1.8 (0.8–2.8) | 2.2 (1.1–3.3) | 1.5 (0.5–2.6) |
Abbreviation: CI = confidence interval.
∗p < .0001.
The question used to assess chronic medical conditions was “Have you EVER been told by a doctor, nurse, or other health professional that you have any of the following?” These conditions were not mutually exclusive; one respondent might have two or more chronic medical conditions.
Obesity was listed as a chronic medical condition (i.e., not a calculated variable as height and weight were not reported by respondents).
Like moderate to severe asthma.
Disability was assessed with a positive response in ≥1 of the six response categories following the question “Which, if any of the following apply to you?” (response categories: I am deaf or have serious difficulty hearing (hearing); I am blind or have serious difficulty seeing, even when wearing glasses (vision); Because of a physical, mental, or emotional condition, I have serious difficulty concentrating, remembering, or making decisions (cognition); I have serious difficulty walking or climbing stairs (mobility); I have difficulty dressing or bathing (self-care); and Because of a physical, mental, or emotional condition, I have difficulty doing errands alone such as visiting a doctor’s office or shopping (independent living).
Mental health indicators
Table 3 compares the prevalence of current depressive symptoms, FMD, suicidal ideation, and initiated or increased substance use related to COVID-19 among adults with and without any disability and by disability type. Adults with any disability were more likely to report each mental health condition (p < .0001 for all). When examined by disability type, the prevalence of current depression was significantly higher for all six disability types; the prevalence of FMD was significantly higher for adults reporting four of the six disability types (i.e., cognitive disability, mobility disability, self-care disability, and independent living disability); and the prevalence of suicidal ideation and initiated or increased substance use related to COVID-19 was significantly higher for five of the six disability types (with the exception of mobility disability).
Table 3.
Weighted prevalence estimates of indicators of poor mental health indicatorsa among adults aged ≥18 years by disability status and typeb — Porter Novelli View 360 Internet survey, United States, April and May 2020.
| Current Depressive symptoms | Frequent mental distress | Suicidal ideation | Initiated or increased substance use | |
|---|---|---|---|---|
| Total | ||||
| Unweighted n | 306 | 119 | 86 | 193 |
| Weighted % (95% CI) | 28.6 (25.6–31.5) | 12.2 (10.0–14.4) | 8.4 (6.6–10.2) | 18.2 (15.7–20.7) |
| Disability status | ||||
| Any disability | ||||
| Unweighted n | 154 | 62 | 53 | 89 |
| Weighted % (95% CI) | 56.8 (50.3–63.4)∗∗∗∗ | 24.8 (18.9–30.6)∗∗∗∗ | 20.7 (15.3–26.0)∗∗∗∗ | 31.5 (25.5–37.4)∗∗∗∗ |
| No disability | ||||
| Unweighted n | 152 | 57 | 33 | 104 |
| Weighted % (95% CI) | 18.4 (15.5–21.2) | 7.8 (5.7–9.9) | 4.1 (2.6–5.5) | 13.4 (10.8–16.0) |
| Disability type | ||||
| Hearing disability | ||||
| Unweighted n | 16 | 5 | 9 | 13 |
| Weighted % (95% CI) | 51.6 (31.5–71.7)∗ | 14.4 (0.9–28.0) | 31.0 (12.4–49.6)∗∗∗ | 38.2 (19.3–57.2)∗ |
| No hearing disability | ||||
| Unweighted n | 290 | 114 | 77 | 180 |
| Weighted % (95% CI) | 27.8 (24.9–30.8) | 12.1 (9.9–14.4) | 7.7 (5.9–9.5) | 17.6 (15.0–20.1) |
| Vision disability | ||||
| Unweighted n | 17 | 6 | 13 | 16 |
| Weighted % (95% CI) | 66.8 (44.4–89.3)∗∗ | 28.1 (5.9–50.3) | 49.8 (26.7–72.9)∗∗∗∗ | 61.3 (38.4–84.2)∗∗∗∗ |
| No vision disability | ||||
| Unweighted n | 289 | 113 | 73 | 177 |
| Weighted % (95% CI) | 27.5 (24.6–30.5) | 11.8 (9.6–14.0) | 7.3 (5.6–9.0) | 17.0 (14.6–19.5) |
| Cognitive disability | ||||
| Unweighted n | 83 | 36 | 31 | 43 |
| Weighted % (95% CI) | 76.4 (67.6–85.3)∗∗∗∗ | 39.4 (28.5–50.3)∗∗∗∗ | 31.0 (21.2–40.9)∗∗∗∗ | 36.1 (26.5–45.7)∗∗∗∗ |
| No cognitive disability | ||||
| Unweighted n | 223 | 83 | 55 | 150 |
| Weighted % (95% CI) | 23.0 (20.2–25.9) | 9.3 (7.2–11.3) | 6.0 (4.3–7.6) | 16.1 (13.6–18.7) |
| Mobility disability | ||||
| Unweighted n | 47 | 20 | 15 | 19 |
| Weighted % (95% CI) | 46.0 (35.8–56.3)∗∗∗ | 20.0 (11.6–28.4)∗ | 13.0 (6.5–19.5) | 16.6 (9.4–23.8) |
| No mobility disability | ||||
| Unweighted n | 259 | 99 | 71 | 174 |
| Weighted % (95% CI) | 26.4 (23.4–29.4) | 11.2 (9.0–13.5) | 7.8 (5.9–9.7) | 18.4 (15.7–21.1) |
| Self-care disability | ||||
| Unweighted n | 35 | 16 | 18 | 23 |
| Weighted % (95% CI) | 65.8 (51.7–79.9)∗∗∗∗ | 33.3 (18.5–48.0)∗∗∗ | 32.9 (19.2–46.7)∗∗∗∗ | 38.6 (24.5–52.8)∗∗∗ |
| No self-care disability | ||||
| Unweighted n | 271 | 103 | 68 | 170 |
| Weighted % (95% CI) | 26.7 (23.7–29.6) | 11.1 (8.9–13.3) | 7.2 (5.4–8.9) | 17.2 (14.6–19.7) |
| Independent living disability | ||||
| Unweighted n | 69 | 32 | 25 | 38 |
| Weighted % (95% CI) | 71.2 (61.6–80.7)∗∗∗∗ | 34.7 (24.0–45.4)∗∗∗∗ | 28.7 (18.6–38.8)∗∗∗∗ | 37.7 (27.4–48.0)∗∗∗∗ |
| No independent living disability | ||||
| Unweighted n | 237 | 87 | 61 | 155 |
| Weighted % (95% CI) | 24.1 (21.2–27.0) | 9.9 (7.8–12.0) | 6.3 (4.7–8.0) | 16.1 (13.6–18.7) |
Abbreviation: CI = confidence interval.
∗p ≤ .05; ∗∗p ≤ .01; ∗∗∗p ≤ .001; ∗∗∗∗p ≤ .0001.
Current depressive symptoms were determined with a score of ≥10 on the Patient Health Questionnaire 8 (PHQ-8). The PHQ-8 is adapted from the 9-item scale (i.e., PHQ-9), which is based on nine criteria aligned with the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition diagnosis of depressive disorders. Mental distress was assessed with the survey question “Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?” Respondents were considered to have frequent mental distress if they reported their mental health was not good for ≥14 days. Suicidal ideation was assessed with the question “At any time in the past 30 days, did you seriously think about trying to kill yourself?” Having started or increased substance use related to COVID-19 was assessed with the question “Have you started or increased using substances to help you cope with stress or emotions during the COVID-19 pandemic? Substance use includes alcohol, legal or illegal drugs, or prescriptions drugs that are taken in a way not recommended by your doctor.”
Disability type and any disability were assessed with a positive response to each of the disability response categories and ≥1 of the six response categories, respectively, following the question “Which, if any of the following apply to you?” (response categories: I am deaf or have serious difficulty hearing (hearing); I am blind or have serious difficulty seeing, even when wearing glasses (vision); Because of a physical, mental, or emotional condition, I have serious difficulty concentrating, remembering, or making decisions (cognition); I have serious difficulty walking or climbing stairs (mobility); I have difficulty dressing or bathing (self-care); and Because of a physical, mental, or emotional condition, I have difficulty doing errands alone such as visiting a doctor’s office or shopping (independent living). Each disability type might not be independent; one respondent might have two or more disability types.
Psychosocial stressors
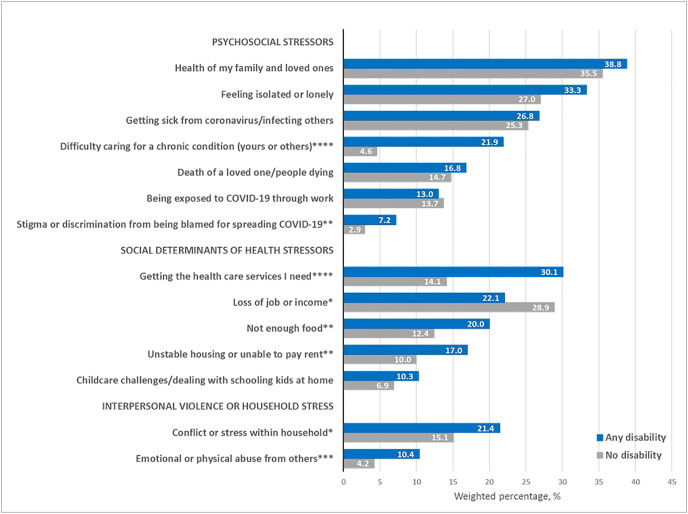
Fig. 1 compares the prevalence of self-reported psychosocial stressors, social determinants of health (SDOH) stressors, and interpersonal violence or household stress for adults with and without any disability. Adults with any disability reported nearly 5 times the level of stress and worry over difficulty caring for a chronic condition (self or others) than adults without disability (p < .0001) and a higher percentage of stress and worry about stigma or discrimination from being blamed for spreading COVID-19 than adults without disability (p < .01).
Fig. 1.
Weighted percentages of self-reported psychosocial stressors, social determinants of health stressors, and interpersonal violence or household stressa among adults aged ≥18 years by disability statusb — Porter Novelli View 360 Internet survey, United States, April and May 2020
∗ p ≤ .05; ∗∗p ≤ .01; ∗∗∗p ≤ .001; ∗∗∗∗p ≤ .0001
a The question used to assess self-reported stress and worry related to psychosocial stressors, social determinants of health stressors, and interpersonal violence or household stress was “Which of any of the items below are a source of stress and worry?”
b Disability was assessed with a positive response in ≥1 of the six response categories following the question “Which, if any of the following apply to you?” (response categories: I am deaf or have serious difficulty hearing (hearing); I am blind or have serious difficulty seeing, even when wearing glasses (vision); Because of a physical, mental, or emotional condition, I have serious difficulty concentrating, remembering, or making decisions (cognition); I have serious difficulty walking or climbing stairs (mobility); I have difficulty dressing or bathing (self-care); and Because of a physical, mental, or emotional condition, I have difficulty doing errands alone such as visiting a doctor’s office or shopping (independent living).
SDOH stressors
In comparison to adults without disability, adults with any disability reported significantly higher prevalences of stress and worry regarding getting the health care services they need (p < .0001), not having enough food (p < .01), and housing instability (p < .01); and a significantly lower prevalence of stress and worry about possible job loss (p = .05).
Interpersonal violence or household stress
Stress and worry over conflict or stress within the household and emotional or physical abuse from others were significantly higher among adults with any disability (p < .05 and p < .001, respectively).
Discussion
In April and May 2020 of the COVID-19 pandemic, as compared to adults without disabilities, adults with disabilities reported disproportionately higher levels of poor mental health (i.e., current depressive symptoms, FMD, suicidal ideation, initiated or increased substance use) and stressors, such as access to health care services, difficulty caring for their own (or another’s) chronic condition, conflict or stress within the household, and not having enough food. This study had several novel mental and behavioral health findings in the context of the COVID-19 pandemic.
In the current study, among adults with and without disabilities, the estimated prevalence of current depressive symptoms was 56.8% and 18.4%, respectively. Comparatively, these estimates were nearly three to four times higher than estimates of current depressive symptoms derived from two population-based surveys representative of non-institutionalized US adults with and without disabilities (24.3% vs 8.5%, respectively, from the 2006 Behavioral Risk Factor Surveillance System and 19.9% vs 5.3%, respectively from the 2005–2006 National Health and Nutrition Examination Survey, respectively).33 Among a 2011 nationally representative sample of US Medicare beneficiaries, based on the PHQ-2, current depressive symptoms were more prevalent among older adults with hearing (21.1%) and vision (28.4%) impairment than in older adults with no hearing or vision impairment (12.6%).34 Our study also found a higher prevalence of current depressive symptoms among adults with hearing (51.6%) or vision (66.8%) disability. While we did not have more recent comparative estimates, this information provides evidence of pre-COVID-19 pandemic disparities in current depressive symptoms by disability status and type.
We believe these are the first estimates to show a marked disparity in suicidal ideation during the COVID-19 pandemic between adults with and without disabilities (5 times higher: 20.7% vs 4.1%). While we lacked comparable baseline estimates for suicidal ideation among persons with disability overall, estimates were available for adults with specific disabling conditions, ranging from 4.3% for autism spectrum disorder to 20.1% for epilepsy.35, 36, 37, 38 Researchers35 have assessed the independent and joint explanatory significance of physical disability, sociodemographics, and elements of the stress process model for risk of suicidal ideation: physical disabilities were predictive of suicidal ideation after controlling for psychiatric comorbidity and sociodemographics and stress exposure was predictive of an elevated risk of suicidal ideation.35 Most saliently, the increased risk of suicidal ideation associated with stress exposure (e.g., perceptions of burdensomeness; isolation) may be relevant in the context of the COVID-19 pandemic.35
To our knowledge, these are also the first estimates to demonstrate a significantly higher prevalence of initiated or increased substance use to cope with the COVID-19 pandemic comparing US adults with and without disabilities (2.4 times higher: 31.5% vs 13.4%). Substance use may result in impaired self-care activities, increased medical complications, and poorer health.39 Previous estimates derived from the 2002–2010 National Survey on Drug Use and Health,40 among adults aged 18–64 years, found that adults with disabilities were significantly more likely to report substance misuse than their peers without disabilities (40% vs 34% in each of the nine years); however, unlike our study, cigarette smoking was included as a substance. Our study found a higher disproportionate burden of substance use, with nearly one in three adults with disabilities reported having initiated or increased substance use to cope with stress or emotions during the COVID-19 pandemic.
In addition to poor mental health, adults with disability were significantly more likely than those without to report psychosocial stressors (e.g., difficulty caring for chronic conditions (self or others)), SDOH stressors (e.g., accessing needed health care services; having enough food), conflict or stress within the household, and emotional or physical abuse. Concern over access to needed health care services among adults with disabilities were two times that of adults without disabilities. This finding is replicated by a June 2020 report41 that found adults with disabilities were significantly more likely to report delayed or avoidance of medical care because of COVID-19–related concerns compared to adults without disabilities. The researchers hypothesized that adults with disabilities may have more challenges in accessing medical services because of disruptions in essential support services or lack of availability of accessible transportation, communication in accessible formats, perceived or actual increased risk of exposure to SARS-CoV-2, and medical needs that are hard to address through telehealth.41 Notably, the chronic medical conditions associated with an increased risk for severe COVID-1914 , 15 are more prevalent among adults with disabilities,13 , 16 underscoring their need for accessible health care services. The subsequent impact of delayed medical care on health, functioning, and well-being is unknown and requires elucidation.
It is well established that adults with disabilities are at increased risk of becoming victims of violence and abuse.42 , 43 We found adults with disabilities reported significantly higher levels of stress and worry over emotional or physical abuse from others than those without disabilities. This may be because of increased social isolation, disruption to daily routines, diminished support and services, and reliance on caregivers for assistance — who themselves, may be at increased risk for worse mental health.42, 43, 44, 45 These mitigation activities may also contribute to difficulties maintaining positive cycles of behavior such as exercising and eating well and may exacerbate negative cycles of behavior such as poor sleep hygiene and substance use.46
Another noteworthy study finding was that Hispanic or Latino adults reported the highest prevalence of disability in comparison to the other racial and ethnic groups examined, with cognitive disability being the most prevalent (two times higher than non-Hispanic White and Black adults: 18.2% vs 8.9% and 8.1%, respectively) followed by independent living disability (17.2%). The prevalence of disability varies among Hispanic subgroups, with non-US-born Hispanic adults having a lower prevalence of disability compared to non-Hispanic White adults and US-born Hispanic adults having a higher prevalence.47 US-born Hispanic adults may be more likely representative of the population we studied as they are more likely to be English-speaking adults. We were unable to explore this further with these data.
Our study has several limitations. First, we did not have baseline estimates for sources of stress and worry to benchmark against estimates obtained in April and May 2020. Nonetheless, adults with disabilities are disproportionately burdened by poor mental health and specific stressors in the context of the COVID-19 pandemic and, as a result, are at increased risk for adverse health outcomes. Second, the data were self-reported and might be subject to associated biases (e.g., social desirability, recall). Third, respondents could reside in a variety of housing types, such as single-family dwellings, congregate care settings, and group homes as none were specifically excluded. As a result, our findings might not be comparable to survey results conducted among non-institutionalized populations. Fourth, the survey was administered to English-speaking adults; therefore, limiting the generalizability beyond the US English-speaking adult population. Fifth, because adults without internet access are unable to participate in the survey, the results may not be generalizable to the overall US population of adults; and some adults with disabilities may experience other access barriers. Notably, while these data mirror the overall US adult population by sex, age, region, race/ethnicity, and education, when stratified by disability status, these data do not completely mirror the population of US adults with disability given the higher prevalence of males with disability and no difference by age group or education. Finally, responses were recorded in April and May 2020 of the COVID-19 pandemic, and thus, may not reflect the temporal trends in mental health and sources of stress and worry as the pandemic progresses.
Conclusion
The markedly disproportionate prevalence of indicators of poor mental health reported by adults with disabilities compared to those without disabilities, along with disparate reports of stress and worry about access to needed health care services, difficulty caring for chronic conditions of self or others, and emotional/physical abuse, highlights the need for immediate and on-going mental health promotion efforts48 and evidence-based substance use prevention (e.g., alcohol screening and brief intervention)49 to mitigate the impact of COVID-19 on adults with disabilities. These targeted efforts may include building resiliency through social connectedness,46 , 50 while maintaining physical distancing and other recommended prevention strategies (e.g., handwashing, wearing a mask).19 , 20 Further, health care providers might consider screening for mental health symptoms during the provision of health care; as well as strategies to address emotional and physical abuse at both the client-level and systems-level.45 , 51
Further public health efforts are needed to ensure availability of services and supports via telehealth or other modalities that allow adults with disabilities to reduce the risk of severe illness from COVID-19 while addressing their medical and mental health needs. Opportunities for extensive use of telemedicine (i.e., telepsychology) for mental and behavioral health care have been highlighted during the COVID-19 pandemic, and research to date has demonstrated its effectiveness.52 However, the utility of telehealth and telepsychology in effectively serving persons with disabilities needs further examination, including identification of its risks, benefits, and barriers to provision.53
Existing health disparities and the additive impact of stress and worry call for targeted and sustainable disability inclusive emergency response efforts and risk reduction in preparedness and response policies and plans at the local, state, and federal level. For example, resources developed by CDC funded State Disability and Health Programs54 may be used by public health professionals, emergency personnel, and communities to create emergency preparedness and response plans at the state and local level that are inclusive of people with disabilities. Other targeted strategies, such as the National Center on Birth Defects and Developmental Disabilities’ project Addressing the Needs of People with Disabilities in COVID-19 Preparedness, Planning, Mitigation, and Recovery Efforts in the United States, can be used to ensure that the needs of people with disabilities are addressed during pandemic response and recovery efforts.
Funding
No funding was received for this study.
Disclaimer
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Conflicts of interest
The authors have no conflicts of interest to report for this study.
Acknowledgments
Survey respondents; Fred Fridinger, Office of the Associate Director for Communication, CDC; Deanne Weber, Porter Novelli Public Services; Robyn Cree, National Center on Birth Defects and Developmental Disabilities; CDC COVID-19 Response Team.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.dhjo.2021.101110.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Okoro C.A., Hollis N.D., Cyrus A.C., Griffin-Blake S. Prevalence of disabilities and health care access by disability status and type Among adults - United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67:882–887. doi: 10.15585/mmwr.mm6732a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fox M.H., White G.W., Rooney C., Cahill A. The psychosocial impact of Hurricane Katrina on persons with disabilities and independent living center staff living on the American Gulf Coast. Rehabil Psychol. 2010;55:231–240. doi: 10.1037/a0020321. [DOI] [PubMed] [Google Scholar]
- 3.Malik S., Lee D.C., Doran K.M., et al. Vulnerability of older adults in disasters: emergency department utilization by geriatric patients after hurricane sandy. Disaster Med Public Health Prep. 2018;12:184–193. doi: 10.1017/dmp.2017.44. [DOI] [PubMed] [Google Scholar]
- 4.Necho M., Birkie M., Gelaye H., Beyene A., Belete A., Tsehay M. Depression, anxiety symptoms, Insomnia, and coping during the COVID-19 pandemic period among individuals living with disabilities in Ethiopia, 2020. PloS One. 2020;15 doi: 10.1371/journal.pone.0244530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cree R.A., Okoro C.A., Zack M.M., Carbone E. Frequent mental distress among adults by disability status, disability type, and selected characteristics — United States, 2018. MMWR Morb Mortal Wkly Rep. 2020;69:1238–1243. doi: 10.15585/mmwr.mm6936a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okoro C.A., Strine T.W., Balluz L.S., Crews J.E., Mokdad A.H. Prevalence and correlates of depressive symptoms among United States adults with disabilities using assistive technology. Prev Med. 2010;50:204–209. doi: 10.1016/j.ypmed.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 7.Kinne S., Patrick D.L., Doyle D.L. Prevalence of secondary conditions among people with disabilities. Am J Publ Health. 2004;94:443–445. doi: 10.2105/ajph.94.3.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Strine T.W., Mokdad A.H., Balluz L.S., et al. Depression and anxiety in the United States: findings from the 2006 Behavioral Risk Factor Surveillance System. Psychiatr Serv. 2008;59:1383–1390. doi: 10.1176/ps.2008.59.12.1383. [DOI] [PubMed] [Google Scholar]
- 9.Okoro C.A., Strine T.W., Eke P.I., Dhingra S.S., Balluz L.S. The association between depression and anxiety and use of oral health services and tooth loss. Community Dent Oral Epidemiol. 2012;40:134–144. doi: 10.1111/j.1600-0528.2011.00637.x. [DOI] [PubMed] [Google Scholar]
- 10.Gonzalez J.S., Safren S.A., Cagliero E., et al. Depression, self-care, and medication adherence in type 2 diabetes: relationships across the full range of symptom severity. Diabetes Care. 2007;30:2222–2227. doi: 10.2337/dc07-0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morgan R.O., Byrne M.M., Hughes R.B., et al. Do secondary conditions explain the relationship between depression and health care cost in women with physical disabilities? Arch Phys Med Rehabil. 2008;89:1880–1886. doi: 10.1016/j.apmr.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 12.Brenes G.A. Anxiety, depression, and quality of life in primary care patients. Prim Care Companion J Clin Psychiatry. 2007;9:437–443. doi: 10.4088/pcc.v09n0606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boyle C.A., Fox M.H., Havercamp S.M., Zubler J. The public health response to the COVID-19 pandemic for people with disabilities. Disabil Health J. 2020:100943. doi: 10.1016/j.dhjo.2020.100943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.CDC COVID-19 Response Team Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019 - United States, February 12-March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:382–386. doi: 10.15585/mmwr.mm6913e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stokes E.K., Zambrano L.D., Anderson K.N., et al. Coronavirus disease 2019 case surveillance - United States, January 22-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:759–765. doi: 10.15585/mmwr.mm6924e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dixon-Ibarra A., Horner-Johnson W. Disability status as an antecedent to chronic conditions: National Health Interview Survey, 2006-2012. Prev Chronic Dis. 2014;11:130251. doi: 10.5888/pcd11.130251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.CDC . Centers for Disease Control and Prevention; Atlanta, GA: 2020. Disability and Health Data System (DHDS)https://www.cdc.gov/ncbddd/disabilityandhealth/dhds/ [Google Scholar]
- 18.Kimball A., Hatfield K.M., Arons M., et al. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility - King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:377–381. doi: 10.15585/mmwr.mm6913e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grier E., Lunsky Y., Sullivan W.F., Casson I. The College of Family Physicians of Canada; 2020. Health Care of Adults with Intellectual and Developmental Disabilities in a Time of COVID-19. [Google Scholar]
- 20.CDC . US Department of Health and Human Services; Atlanta, GA: 2021. Coronavirus Disease 2019 (COVID-19). Preventing Getting Sick.https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/ [Google Scholar]
- 21.HHS.gov . US Department of Health and Human Services; Washington, D.C.: 2020. (OCR Resolves Complaints after State of Connecticut and Private Hospital Safeguard the Rights of Persons with Disabilities to Have Reasonable Access to Support Persons in Hospital Settings during COVID-19). [Google Scholar]
- 22.Drum C.E., Ditsch J., Oberg A., Cooper K., Carlin R. American Association on Health and Disability; Rockville, MD: 2020. COVID-19 & Adults with Disabilities: Health and Health Care Access- Comparative Analysis of Online Survey Results by Type of Disability. [Google Scholar]
- 23.Ne’eman A. The Hastings Center; 2020. When it comes to rationing, disability rights law prohibits more than prejudice.https://www.thehastingscenter.org/when-it-comes-to-rationing-disability-rights-law-prohibits-more-than-prejudice/ [Google Scholar]
- 24.HHS Office for Civil Rights in Action . US Department of Health and Human Services; Washington, D.C.: 2020. Bulletin: Civil Rights, HIPAA, and the Coronavirus Disease 2019 (COVID-19) [Google Scholar]
- 25.HHS.gov . US Department of Health and Human Services; Washington, D.C.: 2020. OCR Reaches Early Case Resolution with Alabama after it Removes Discriminatory Ventilator Triaging Guidelines. [Google Scholar]
- 26.Fisher K.A., Barile J.P., Guerin R.J., et al. Factors associated with cloth face covering use among adults during the COVID-19 pandemic — United States, April and May 2020. MMWR Morb Mortal Wkly Rep. 2020;69:933–937. doi: 10.15585/mmwr.mm6928e3. [DOI] [PubMed] [Google Scholar]
- 27.McKnight-Eily L.R., Okoro C.A., Strine T.W., et al. Racial and ethnic disparities in the prevalence of stress and worry, mental health conditions, and increased substance use among adults during the COVID-19 pandemic — United States, April and May 2020. MMWR Morb Mortal Wkly Rep. 2021;70:162–166. doi: 10.15585/mmwr.mm7005a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Coppock A., McClellan O.A. Validating the demographic, political, psychological, and experimental results obtained from a new source of online survey respondents. Research & Politics. 2019;6:1–14. [Google Scholar]
- 29.International World. World Health Organization; Geneva, Switzerland: 2001. Classification of Functioning, Disability, and Health (ICF) [Google Scholar]
- 30.Kroenke K., Strine T.W., Spitzer R.L., Williams J.B., Berry J.T., Mokdad A.H. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114:163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 31.American Psychiatric Association . 4th ed. American Psychiatric Publishing, Inc.; Washington, D.C.: 2000. Diagnostic and Statistical Manual – Text Revision (DSM-IV-TR) [Google Scholar]
- 32.CDC . US Department of Health and Human Services; Atlanta, GA: 2020. Behavioral Risk Factor Surveillance System. (Annual Survey Data). [Google Scholar]
- 33.Li C., Ford E.S., Zhao G., Tsai J., Balluz L.S. A comparison of depression prevalence estimates measured by the Patient Health Questionnaire with two administration modes: computer-assisted telephone interviewing versus computer-assisted personal interviewing. Int J Publ Health. 2012;57:225–233. doi: 10.1007/s00038-011-0253-9. [DOI] [PubMed] [Google Scholar]
- 34.Simning A., Fox M.L., Barnett S.L., Sorensen S., Conwell Y. Depressive and anxiety symptoms in older adults with auditory, vision, and dual sensory impairment. J Aging Health. 2019;31:1353–1375. doi: 10.1177/0898264318781123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Russell D., Turner R.J., Joiner T.E. Physical disability and suicidal ideation: a community-based study of risk/protective factors for suicidal thoughts. Suicide Life-Threatening Behav. 2009;39:440–451. doi: 10.1521/suli.2009.39.4.440. [DOI] [PubMed] [Google Scholar]
- 36.Giannini M.J., Bergmark B., Kreshover S., Elias E., Plummer C., O’Keefe E. Understanding suicide and disability through three major disabling conditions: intellectual disability, spinal cord injury, and multiple sclerosis. Disabil Health J. 2010;3:74–78. doi: 10.1016/j.dhjo.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 37.Friedman D., Spruill T.M., Liu H., et al. Depressive symptoms and suicidality among individuals with epilepsy enrolled in self-management studies: results from the US Centers for Disease Control and Prevention Managing Epilepsy Well (MEW) Network. Epilepsy Behav. 2018;87:235–240. doi: 10.1016/j.yebeh.2018.06.024. [DOI] [PubMed] [Google Scholar]
- 38.Hand B.N., Benevides T.W., Carretta H.J. Suicidal ideation and self-inflicted injury in Medicare enrolled autistic adults with and without co-occurring intellectual disability. J Autism Dev Disord. 2019;50(10):3489–3495. doi: 10.1007/s10803-019-04345-x. [DOI] [PubMed] [Google Scholar]
- 39.Smedema S.M., Ebener D. Substance abuse and psychosocial adaptation to physical disability: analysis of the literature and future directions. Disabil Rehabil. 2010;32:1311–1319. doi: 10.3109/09638280903514721. [DOI] [PubMed] [Google Scholar]
- 40.Glazier R.E., Kling R.N. Recent trends in substance abuse among persons with disabilities compared to that of persons without disabilities. Disabil Health J. 2013;6:107–115. doi: 10.1016/j.dhjo.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 41.Czeisler M.E., Marynak K., Clarke K.E.N., et al. Delay or avoidance of medical care because of COVID-19–related concerns — United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1250–1257. doi: 10.15585/mmwr.mm6936a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Breiding M.J., Armour B.S. The association between disability and intimate partner violence in the United States. Ann Epidemiol. 2015;25:455–457. doi: 10.1016/j.annepidem.2015.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Basile K.C., Breiding M.J., Smith S.G. Disability and risk of recent sexual violence in the United States. Am J Publ Health. 2016;106:928–933. doi: 10.2105/AJPH.2015.303004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Czeisler M.É., Lane R.I., Petrosky E., et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lund E.M. Interpersonal violence against people with disabilities: additional concerns and considerations in the COVID-19 pandemic. Rehabil Psychol. 2020;65:199–205. doi: 10.1037/rep0000347. [DOI] [PubMed] [Google Scholar]
- 46.Prime H., Wade M., Browne D.T. Risk and resilience in family well-being during the COVID-19 pandemic. Am Psychol. 2020;75:631–643. doi: 10.1037/amp0000660. [DOI] [PubMed] [Google Scholar]
- 47.Garcia M.A., Downer B., Crowe M., Markides K.S. Aging and disability among Hispanics in the United States: current knowledge and future directions. Innov Aging. 2017;1(2):1–11. doi: 10.1093/geroni/igx020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.CDC . US Department of Health and Human Services; Atlanta, GA: 2020. Mental Health. https://www.cdc.gov/mentalhealth/. Accessed April 28, 2021. [Google Scholar]
- 49.Curry S.J., Krist A.H., Owens D.K., et al. Vol. 320. JAMA; 2018. US Preventive Services Task Force. Screening and behavioral counseling interventions to reduce unhealthy alcohol use in adolescents and adults; pp. 1899–1909. [DOI] [PubMed] [Google Scholar]
- 50.Tough H., Siegrist J., Fekete C. Social relationships, mental health and wellbeing in physical disability: a systematic review. BMC Publ Health. 2017;17:414. doi: 10.1186/s12889-017-4308-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.CDC . US Department of Health and Human Services; Atlanta, GA: 2020. Coronavirus Disease 2019 (COVID-19): Support for People Experiencing Abuse. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/stress-coping/abuse.html. Accessed April 28, 2021. [Google Scholar]
- 52.Varker T., Brand R.M., Ward J., Terhaag S., Phelps A. Efficacy of synchronous telepsychology interventions for people with anxiety, depression, posttraumatic stress disorder, and adjustment disorder: a rapid evidence assessment. Psychol Serv. 2019;16:621–635. doi: 10.1037/ser0000239. [DOI] [PubMed] [Google Scholar]
- 53.Annaswamy T.M., Verduzco-Gutierrez M., Frieden L. Telemedicine barriers and challenges for persons with disabilities: COVID-19 and beyond. Disabil Health J. 2020;13(4):100973. doi: 10.1016/j.dhjo.2020.100973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Disability and Health Emergency Preparedness. US Department of Health and Human Services; Atlanta, GA: 2020. National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/disabilityandhealth/emergencypreparedness.html. Accessed April 28, 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.