Abstract
Background:
It has been suggested that foot strike technique (FST) at initial contact is related to running-related injuries (RRIs).
Purpose:
To explore the relationship between FST and RRIs.
Study Design:
Systematic review; Level of evidence, 3.
Methods:
A systematic electronic search was performed using MEDLINE, PubMed, SPORTDiscus, Scopus, and Web of Science databases. Included were studies published in the English language that explored the relationship between FST and RRIs between January 1960 and November 2020. Results were extracted and collated. The Grading of Recommendations, Assessment, Development and Evaluation approach was applied to synthesize the quality of evidence.
Results:
We reviewed 13 studies exploring the relationship between FST and RRIs. Of these, 6 studies reported FST categorically (foot strike pattern [FSP]), and 7 reported continuous measures (foot contact angle, ankle flexion angle, and strike index). Three of the 6 studies looking at categorical FSP found rearfoot strikers have a significantly greater retrospective injury rate than do non– rearfoot strikers, with 1 other study noting a greater risk associated with midfoot and forefoot strike. Regarding the continuous measures of FST, only 1 of the 7 studies reported a significant relationship with RRIs.
Conclusion:
There was low evidence to suggest a relationship between FST (or its subcategories of categorical FSP and continuous measures) and RRIs. While two-thirds of the categorical studies found a relationship between FSP and RRIs, these studies were very low quality, with limitations such as retrospective study design, low participant numbers, and poor FSP assessment methods. More large-scale prospective studies are required.
Keywords: running, injury, foot strike, systematic review
Running is an extremely popular sport and physical activity13 with proven health benefits, such as cardiovascular, respiratory, and psychological improvements.59 However, prevalence rates of running-related injuries (RRIs) are as high as 79% in recreational runners42,64 and 85% in novice runners.5,34 Taking a biomechanical model approach to injury, RRIs are caused by high loading relative to tissue strength.33 Given that the foot is the first point of ground impact and has the potential to mediate the subsequent force applied to the body,25,38 the relationship between foot strike technique (FST) and RRI has received significant attention within the scientific11,25,53,66 and general running communities.46
It has been speculated that for the majority of human evolutionary history, runners would have run barefoot or would have run in minimalist footwear with little or no cushioning (eg, sandals).41 It is believed that this style of running would encourage a running technique where the forefoot strikes the ground first, or alternatively the runner might land with a flat foot, to manage the impact load.41 However, with the introduction of modern running shoes and increased cushioning properties within these shoes, shod runners are thought to be more likely to strike the ground with their heels (rearfoot strike [RFS]).41 It is unknown how or why runners develop a specific FST (ie, some runners land on their toes first, while others land on their heels), but it appears that evolution of both humans and running shoe properties may have played a role in the predominance of RFS pattern prevalence seen among the modern-day running community.11,39
Thus far, FST has been defined in 2 ways: (1) using nominal means via foot strike pattern (FSP) classification and (2) using continuous measures. Nominally, FSP classification has been categorized into various subgroups based on which part of the foot contacts the ground first: RFS, midfoot strike (MFS), and forefoot strike (FFS).10 RFS describes initial contact with the heel or posterior aspect of the foot, FFS involves contact with anterior aspects of the foot, and MFS involves simultaneous contact of both the posterior and the anterior parts.1 Some studies57,66 have also combined MFS and FFS patterns, grouping them together as non-RFS. Studies that have reported FSP classifications have used visual analysis of sagittal plane video recordings,11,21,32,61,66 categorization of continuous measures (foot and ankle contact angles and strike index [SI]),14,15,18,45,48,53 or self-reporting methods.25
Continuous measures of FST have been derived from 3 assessment techniques: (1) measuring the foot contact angle (FCA), (2) measuring the ankle flexion angle (AFA) at contact, and (3) calculating the center of pressure during impact relative to foot length (SI). FCA has been determined using 3-dimensional (3D) motion analysis.14,18,53 AFA has also been determined using 3D motion analysis and describes whether the ankle is in a dorsiflexed or plantarflexed position at initial contact.15 Last, SI has been examined using force plates37,48 and pressure-sensitive insoles43 and has been defined as the position of the center of pressure during landing relative to foot length.10 While FST measures may have been captured as a continuous measure (eg, FCA, AFA, or SI), these have subsequently been categorized into nominal FSPs by some authors. With respect to FCA, there have been variations in the values suggested to represent each FSP. Altman and Davis2 suggested FCAs >8.0° represent an RFS, <−1.6° represent an FFS, and −1.6° to 8.0° represent an MFS, following a comparative analysis between FCA and SI measures. Other authors have suggested that RFS is any positive FCA, FFS is any negative FCA, and MFS is 0°.41 The challenge with this classification is how infrequent a landing of exactly 0° may be, and this guideline may therefore be too stringent. With respect to AFA, it has been proposed that landing in dorsiflexion represents an RFS, planterflexion represents an FFS, and a neutral angle reflects an MFS.15 Last, according to Cavanagh and Lafortune,10 an SI of <33% represents an RFS, 34% to 66% represents an MFS, and >67% represents an FFS.
Interest in the relationship between FST and injury has, at least in part, been guided by the research examining the relationship between FSP and loading. Some research has found RFSs result in higher magnitudes38,47,62 and rates38,57,69 of whole-body loading (via vertical ground reaction forces) and higher knee loading25,38 in comparison with an FFS (or non-RFS). While loading forms a necessary component of training, resulting in homeostatic-positive responses and adaptations,9,65 excessive cumulative load and a poor work-recovery ratio may result in maladaptation to training and an increased risk of injury.17,56 Based on the excessive load that some FSPs may produce and the potential for this cumulative load to become injurious over time,8,12,33 some researchers have suggested that FST, especially an RFS pattern, may be causative of RRIs.11,25 While this may be intuitive, a direct relationship needs to be established.
To the best of our knowledge, only 1 systematic review3 has explored the relationship between FST and injury, and this was done as part of a much broader systematic review. That review,3 however, only identified 1 study, which was in the area of FSP and injury. The authors of that review neglected to include “injury” in their search terms and subsequently may have missed relevant studies. Our systematic review therefore collated all of the existing research on FST (FSP, FCA, AFA, and SI) and RRI, which may be valuable for clinicians, coaches, and athletes in the prevention and management of RRIs. The aim of this review was to investigate if FST (both categorical and continuous measures) relates to RRIs.
Methods
Protocol and Registration
This systematic review was registered with PROSPERO (Centre for Reviews and Dissemination) on July 17, 2019 (CRD42020142747). The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement provided structural guidelines for writing this review.51
Identification and Selection of Studies
A systematic review was undertaken by 2 authors (A.B., S.D.) between November 2 and 9, 2020. MEDLINE, PubMed, SPORTDiscus, Scopus, and Web of Science databases were searched to identify studies investigating FST and RRIs between January 1960 and November 2020. The search was restricted to clinical trials, case comparison, and cohort studies that were published in English including human participants. Reviews, commentaries, opinion articles, case studies, and conference proceedings were excluded. The search terms used are in Appendix Table A1 (available online as Supplemental Material) and were combined using Boolean terms.
Three authors (A.B., S.D., and K.A.M.) determined the inclusion and exclusion criteria before the search commenced (Appendix Table A2, available online). All studies investigating FST and RRIs were included. RRIs were identified using guidance from a consensus definition and were defined as any pain attributed to running, involving muscles, joints, tendons, ligaments, and/or bones of the lower extremities (hip, groin, thigh, knee, lower leg, ankle, foot, and toe) that caused a restriction or stoppage of running (distance, speed, duration of training) or that required the runner to consult a physician or other health care professional.68 Titles and abstracts were reviewed independently by 2 authors (A.B., S.D.) using predetermined selection criteria. A full manuscript review was performed if selection was unclear. Disagreements were resolved via discussion or third-party mediation (K.A.M.).
Risk-of-Bias Assessment
Each study’s methodological quality was assessed independently by 2 authors (A.B., S.D.) using a modified Downs and Black Quality Index (Appendix Table A3, available online).16 Index items that did not pertain to the nature of the selected studies were excluded from the assessment. The modified index comprised 19 items within 4 categories: information reporting, external validity, internal validity, and selection bias. Items representing a high and low risk of bias were scored 0 and 1, respectively. Total scores of 0 to 5 were classified as high risk; 6 to 12, as moderate risk; and 13 to 19, as low risk. The index has good test-retest reliability (r = 0.88), good inter-rater reliability (r = 0.75), and high internal consistency (α = .89).16
Data Extraction
Data extraction of the selected articles was performed by 1 author (A.B.). The study design, population, sample size, participant characteristics (age, sex, body mass index), FSP prevalence, definition of injury, testing characteristics (testing surface, testing speed, FST classification), and other outcome variables were recorded. To evaluate the association between FST and RRIs, P values, hazard ratios, odds ratios (ORs), and relative risks (means and 95% confidence intervals) were extracted where possible. Study authors were contacted via email to request full data sets where missing or incomplete.
Assessment of Evidence
Given the wide heterogeneity of methods and outcome measures, a meta-analysis was not possible. The quality of the body of evidence was therefore determined via the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach that analyzes the following areas: study design, study limitations (risk of bias), inconsistency of results, indirectness of studies, imprecision of study results, and publication bias.27 The quality of evidence for each outcome measure was presented using a 4-level rating system (high, moderate, low, and very low).27 Details of the GRADE approach and scoring criteria are provided in the Supplemental Material (Appendix Table A4).
Results
Overview of Findings
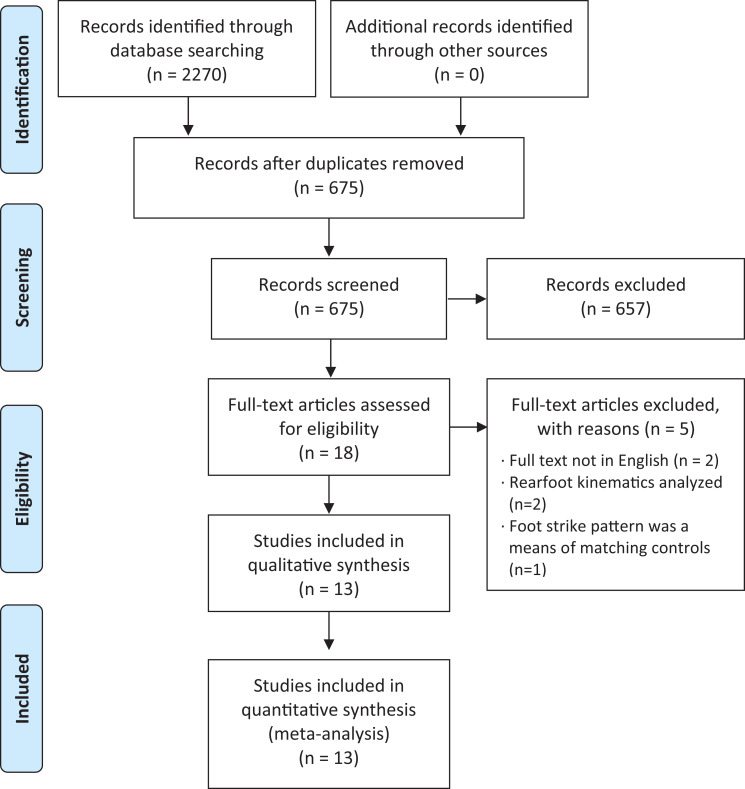
A total of 2270 articles were identified. After duplicate articles were removed, 675 titles and abstracts were reviewed. Eighteen articles were assessed for eligibility, of which 5 were excluded (full text was not in English [n = 2], rearfoot motion was the only kinematic variable assessed [n = 2], and FSP was a means of matching injured runners with controls [n = 1]). The remaining 13 papers were included for review.∥ Reviewing their bibliographies did not reveal any additional includable studies. A PRISMA flow diagram of study selection is shown in Figure 1.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram.
Risk of Bias
Scoring of the quality assessment is detailed in Appendix Table A5 (available online). The mean score for the 19-item risk of bias assessment was 11.1 (range, 11-17). Two studies had a moderate risk of bias,15,23 and 11 studies had a low risk.¶ The most common risk items were participants not being representative of the population, no blinding of the examiners to the outcome, and a lack of power calculations.
Synthesis of Study Characteristics
A summary of the 13 studies’ designs, inclusive of participant, injury, and testing characteristics, can be viewed in Appendix Table A6 (available online). Three of the 13 studies included were prospective cohort studies,18,37,48 and 10 were retrospective cohort studies.# Analysis of participant characteristics revealed a total of 2564 participants, with a range of study sample sizes from 19 to 881 participants (median, 70 participants [interquartile range: 36-320 participants]), with recreational (n = 6), military (n = 1), collegiate cross-country running (n = 3), and mixed (recreational, collegiate, and military, n = 1; recreational and competitive, n = 1) groups being investigated.** One study61 did not report the population of runners that was studied. Twelve studies†† had a mixed-sex population, and 1 study looked exclusively at male runners.66 BMI did not differ greatly among studies that reported it (20.5-24.9 reported across 9 studies).‡‡ The proportion of participants analyzed ranged from 79% to 100%. Reasons given for analyzing <100% of participants included barefoot runners being excluded because of small sample size25; runners sustaining non-RRIs37; poor image quality14; and injuries to the nondominant limb, where only the dominant limb had been tested.18
With respect to injury characteristics, the time frame for injury surveillance ranged between 4 months and 7 years (median, 18 months [interquartile range, 12-60 months]). However, 1 study66 did complete an additional analysis of injuries sustained within a lifetime, which has not been included in the former interquartile range calculation. The definition of injury varied across many studies, with only 7 studies demonstrating a similar time-loss definition ranging from 1 session18 to 1 week,14,25,45,66 2 weeks,48 and 3 months of interrupted training.21 One study53 neglected to define injury.
With regard to FSP classification and testing, 6 studies classified FSP into distinct FSPs (RFS, MFS, FFS, and non-RFS [MFS or FFS pattern combined]) via visual analysis of sagittal plane video recordings of FCAs11,21,32,61,66 or self-reporting.25 In contrast, 7 studies14,15,18,37,45,48,53 examined FST on 2 continuous scales: (1) initial ground contact angles (FCA, AFA) via 3D motion analysis14,15,18,53 and (2) location of initial point of contact relative to foot length (SI) using pressure-sensitive insoles45 and force plate analysis.37,48 There were also differences in testing conditions, with 3 studies18,37,48 analyzing running on an overground surface within a laboratory; 6, on a treadmill14,15,32,45,53,61; and 2, on an outdoor runway.21,66 One study analyzed running on both an outdoor track and a treadmill,11 reporting identical FSP categorization across surfaces. One study asked participants to self-report their FSP through an online survey.25 There was also variation in the number of foot strikes analyzed (median, 5 [interquartile range, 3-7]; range, 2-161). With regard to running speed, 9 studies directed participants to run at a self-selected pace that was reflective of their typical training14,15,18,21,32,45,48 or running event pace.53,66 Kuhman et al37 and Sugimoto et al61 tested participants at a predetermined speed (4.0-4.5 and 1.8-2.3 m/s, respectively), while Daoud et al11 examined running at self-selected and predetermined speeds of 3.0 to 5.0 m/s. For the 9 of 52 runners who changed their FSP with increasing speed,11 the FSP at which the participant ran the majority of his or her miles was used in the FSP classification of that runner. Of the 10 studies analyzing self-selected speeds,§§ 6 studies14,15,18,21,32,45 reported the actual test speed, which ranged between 2.1 and 3.0 m/s.
Regarding the evidence of a relationship between FST and RRIs, there was very low evidence to confidently say that a relationship existed (Table 1). Less than 40% (5/13) of studies found a significant relationship between FST and RRI, which included 1595 of the total 2564 participants.11,14,25,32,61 When FST was analyzed via FSP classification, 67% (4/6) of the studies, which included 1553 of 2016 participants, reported RRI prevalence25,32,61 and rate11 to be related to FSP. Two of these studies11,25 found general overuse RRI rates, and 1 study61 found hamstring injury rates to be greater in RFS runners compared with MFS or FFS runners, with 1 of these studies25 having a moderate risk of bias and the other 2 having a low risk of bias11,61 (Table 2). In contrast, Hollander et al32 found Achilles tendon injuries to be significantly greater in MFS runners compared with both RFS and FFS runners and posterior shank injuries to be significantly greater in FFS runners compared with both RFS and MFS runners. It should be noted that all of the studies examining the relationship between categorical measures of FST and RRI were retrospective cohort studies.
TABLE 1.
Scoring of Studies Through the GRADE Approacha
| Outcome | Initial Rating of Study Design | Study Limitations | Inconsistency | Indirectness | Imprecision | Publication Bias | Grading Up | GRADE Quality of Evidence |
|---|---|---|---|---|---|---|---|---|
| Studies using nominal measures | ||||||||
| Foot strike pattern (6 studies, 2016 participants) | Low | –1 | N/A | 0 | –1 | 0 | 0 | Very low |
| Studies using continuous measures | ||||||||
| Foot contact angle (3 studies, 117 participants) | Low | 0 | N/A | –1 | –1 | –1 | 0 | Very low |
| Ankle flexion angle (1 study, 22 participants) | Low | –1 | N/A | –1 | –1 | –1 | 0 | Very low |
| Strike index (3 studies, 409 participants) | Low | 0 | N/A | –1 | –1 | 0 | 0 | Very low |
aSee the Supplemental Material for scoring criteria. GRADE, Grading of Recommendations, Assessment, Development and Evaluation; N/A, not applicable.
TABLE 2.
Results of Studies Exploring Categorical Measures of Foot Strike Technique and Running-Related Injuriesa
| Running-Related Injuries | |||||||
|---|---|---|---|---|---|---|---|
| Lead Author | Injury Measure | RFS | MFS | FFS | NRFS | P | Outcome |
| Retrospective Studies | |||||||
| Daoud11 | Injury rate per 10,000 mi (mean ± SEM) | Repetitive RRI Mild: 3.19 ± 0.55b Moderate: 4.96 ± 0.84b Severe: 3.70 ± 0.64 Moderate/severe: 8.66 ± 1.02b Traumatic RRI Mild: 2.61 ± 0.81 Moderate: 1.18 ± 0.58 Severe: 0.59 ± 0.21 Moderate/severe: 1.77 ± 0.58 RFS-basedc Mild: 1.93 ± 0.44b Moderate: 3.36 ± 0.68b Severe: 2.44 ± 0.53 Moderate/severe: 5.80 ± 0.84b FFS-basedc Mild: 0.42 ± 0.15 Moderate: 0.67 ± 0.26 Severe: 0.76 ± 0.32 Moderate/severe: 1.43 ± 0.41 |
N/A | Repetitive RRI Mild: 1.25 ± 0.67b Moderate: 2.03 ± 0.66b Severe: 2.97 ± 1.01 Moderate/severe: 5.00 ± 1.43b Traumatic RRI Mild: 0.78 ± 0.56 Moderate: 1.25 ± 0.35 Severe: 0.31 ± 0.18 Moderate/severe: 1.56 ± 0.42 RFS-basedc Mild: 0.47 ± 0.39b Moderate: 0.78 ± 0.43b Severe: 1.41 ± 0.75 Moderate/severe: 2.19 ± 1.00b FFS-basedc Mild: 0.47 ± 0.22 Moderate: 0.94 ± 0.39 Severe: 0.94 ± 0.44 Moderate/severe: 1.88 ± 0.65 |
N/A | Repetitive RRI .025b .006b .54 .037b Traumatic RRI .06 .91 .32 .78 RFS-based .012b .001b .26 .006b FFS-based .86 .57 .74 .56 |
Repetitive RRI: Mild and moderate repetitive stress injury rates were ∼2.5 times higher in RFS vs FFSb
Traumatic RRI NS RFS-based RRI: Injury rates 2.7 times higher for RFS vs FFSb FFS-based RRI: NS |
| Goss25 | Injury prevalence | 52.4% | 34.7% | 22.8% | N/A | <.001b | Injury rates greater (18-30%) in RFS vs MFS and FFSb |
| Warr66 | Injury prevalence | Acute, ≤5 y: 14% Overuse, ≤5 y: 32% In a lifetime: 50% |
N/A | N/A | Acute, ≤5 y: 7% Overuse, ≤5 y: 31% In a lifetime: 56% |
.51 | NS |
| Hollander32 | Injury prevalence | Location Lower back: ∼73% Hip/groin: ∼71% Thigh: ∼75% Knee: ∼73% Achilles tendon: ∼60% Ankle: ∼65% Foot/toes: ∼68% Sublocation Posterior thigh: ∼75% Anterior knee: ∼76% Lateral knee: ∼70% Anterior shank: ∼77% Posterior shank: ∼66% |
Location Lower back: ∼10% Hip/groin: ∼10% Thigh: ∼6% Knee: ∼8% Achilles tendon: ∼20%b Ankle: ∼4% Foot/toes: ∼12% Sublocation Posterior thigh: ∼10% Anterior knee: ∼8% Lateral knee: ∼9% Anterior shank: ∼6% Posterior shank: ∼16% |
Location Lower back: ∼17% Hip/groin: ∼19% Thigh: ∼19% Knee: ∼19% Achilles tendon: ∼20% Ankle: ∼31% Foot/toes: ∼20% Sublocation Posterior thigh: ∼15% Anterior knee: ∼16% Lateral knee: ∼21% Anterior shank: ∼17% Posterior shank: ∼18%b |
N/A | Location >.05 >.05 >.05 >.05 .04b >.05 >.05 Sublocation >.05 >.05 >.05 >.05 .004b |
Location: Runners with an MFS pattern were at 2.27 times greater odds of sustaining an Achilles tendon injury Sublocation: Runners with an FFS pattern were at 2.6 times greater odds of sustaining a posterior shank injury |
| Fukusawa21 | Injury prevalence | Anterior knee pain: 97% Uninjured: 93% |
N/A | N/A | Anterior knee pain: 3% Uninjured: 7% |
>.05 | NS |
| Sugimoto61 | Injury prevalence | Hamstring injury: 74%b
Uninjured: 43% |
Hamstring injuries: 20% Uninjured: 20% |
Hamstring injury: 6% Uninjured: 37% |
N/A | .004b | 74% of the runners with hamstring injuries demonstrated an RFS pattern vs 43% RFS in healthy controls |
aFFS, forefoot strike; MFS, midfoot strike; N/A, not applicable; NRFS, non-rearfoot strike; NS, no significant difference; RFS, rearfoot strike; RRI, running-related injury.
bSignificant P value at P < .05.
cRearfoot strike-based RRIs: RRIs predicted by the authors to be more common in rearfoot strike runners; FFS-based RRIs: RRIs predicted by the authors to be more common in forefoot strike runners.
When FST was analyzed via continuous measures (FCA, AFA, and SI), only 1 of the 7 studies referred to in Table 3 reported a significant relationship between FST and RRI, with Dingenen et al14 (n = 506 participants) reporting a significantly lower FCA (injured: 6.8° vs uninjured: 9.7°) in runners who had current running-related knee injuries compared with uninjured controls (Table 3).
TABLE 3.
Results of Studies Exploring Continuous Measures of Foot Strike Technique and Running-Related Injuries
| Foot Strike Technique Assessment | Injured (Mean ± SD) | Uninjured (Mean ± SD) | Mean Difference | P |
|---|---|---|---|---|
| Foot contact angle, deg | ||||
| Dudley18 prospective) | 11.2 | 11 | –0.2 | .94 |
| Paquette53 (retrospective) | 5.0 ± 5.9 | 4.7 ± 6.5 | –0.3 | .88 |
| Dingenen14 (retrospective) | 6.8 ± 5.1 | 9.7 ± 6.0 | 2.9 | .03b |
| Ankle flexion angle, deg | ||||
| Donoghue15 (retrospective) | 3.3 ± 5.5 | 2.9 ± 4.9 | –0.4 | >.05 |
| Strike index, %a | ||||
| Kuhman37 (prospective) | 44.8 ± 50.0 | 55.8 ± 48.7 | 10.0 | .64 |
| Messier48 (prospective) | 12.0 ± 18.0 | 14.0 ± 0.0 | 2.0 | .44 |
| Mann45 (retrospective) | 25.1 ± 9.4 | 23.7 ± 10.3 | –1.4 | .58 |
aKuhman et al37 used the ratio of center of pressure location at foot strike relative to modified foot length (%) measured using 3-dimensional (3D) motion analysis. Messier et al48 used the percentage distance from the heel measured using 3D motion analysis. Mann et al45 used the percentage of total sole length of pressure-sensitive insole.
bStatistically significant difference between groups (P < .05).
Discussion
The overall finding is that there is very low evidence to suggest a relationship between FST and RRI. While two-thirds of categorical studies found a relationship between FSP and RRI, the quality of these studies was very low. This became particularly evident in the GRADE assessment, with moderate risk of bias and imprecision of study methodologies featuring in the downgrading of FSP as an outcome measure.
One potential reason for the majority of categorical studies finding a relationship between FSP and RRI but no such trends being noted for continuous measures may be because of the dichotomization or trichotomization of data in FSP studies. Categorizing FST data into RFS, MFS, FFS, or non-RFS (MFS and FFS combined) allows the identification of defined groups that may produce distinct loading patterns. The lack of findings for continuous measures of FST suggests that as FCA changes from RFS (with maximum dorsiflexion) to FFS (with maximum plantarflexion), there is not a continuous linear change in the associated loading on the body (eg, peak or rate of vertical ground reaction force.60 While both FFS and RFS involve impact with the ground, the RFS pattern appears to demonstrate a higher magnitude and earlier timing of the vertical impact peak compared with FFS running,41 which has been proposed to be related to overuse RRIs.50,54,63 Although there may be a vertical impact with FFS, it might not be evident as a peak in the time domain.7,58 Additionally, loading at the knee (greater patellofemoral joint reaction forces,67 tibiofemoral average loading rate,6 and knee extensor moments38) can be greater in RFS patterns compared with FFS patterns. It should be acknowledged, however, that loading of the Achilles tendon (Achilles tendon peak force29 and ankle plantarflexor moments29,30,38) is greater with a non-RFS pattern compared with an RFS pattern. Because of this potential influence of high loading on overuse RRIs19,54 and the demonstration of greater loading with various FSPs, several authors have speculated that there may be a relationship between FSP and RRI.23,36,38,57,69
This speculation has been further encouraged through the findings of Daoud et al,11 Goss and Gross,25 and Sugimoto et al,61 as reported in this review, whereby injury rates were significantly greater in RFS running compared with non-RFS running. Daoud et al noted repetitive injury rates to be significantly greater in RFS compared with FFS runners. In agreement with Daoud et al, Goss and Gross,25 and Sugimoto et al, we found overuse injury and hamstring injury rates were significantly greater in RFS runners in comparison with FFS runners. Interestingly, a recent study by Hollander et al32 reported that no relationship exists between RFS and RRI, but they did find strong associations between non-RFS patterns and injury, with MFS runners more than twice as likely to have sustained an Achilles tendon injury (OR, 2.3) and FFS runners more than twice as likely to have sustained a posterior lower leg injury (OR, 2.6) in comparison with RFS runners. In contrast to the findings of the aforementioned studies,11,25,32,61 Warr et al66 and Fukusawa et al21 did not find a relationship between FSP and RRI. Warr et al solely examined military personnel, whose injuries may be attributable to high training volume, additional load carriage, and obstacle course and land navigations,35,43 suggesting that this group may not be ideal for examination and generalization of the possible relationship between FST and RRIs. While Goss and Gross25 included military personnel, the authors did not describe their prevalence (recreational, military, and collegiate cross-country), so it is unclear if their inclusion was large enough to affect the results. Fukusawa et al examined the relationship between FSP and running-related knee injuries in recreational runners, but the injured runners in this study had been training with knee pain for an average of 12 months.
Despite the FSP prevalence being similar between injured (RFS, 97%; non-RFS, 3%) and uninjured groups (RFS, 93%; non-RFS, 7%), it would appear that the uninjured group may have been more habituated to the loading associated with an RFS pattern. Perhaps the runners with knee pain sustained injury because of their inability to withstand this loading and a subsequent inability to adapt their mechanics to dissipate these loads appropriately. In addition, it appears that only 155 of 2 intervention studies52,55 found a beneficial effect of FST modification (changing from RFS to non-RFS) in RRI reduction, and both of these studies had poor study design, very low level of evidence (as measured using the GRADE assessment approach), and low participant numbers, further supporting the main findings of this systematic review.
For continuous measures of FST, it does not appear that FCA, AFA, or SI is related to RRIs in recreational14,15,45,48,53 and collegiate cross-country runners.18,37 Only 114 of 3 studies14,18,53 found a relationship between FCA and RRI, with lower FCA observed in recreational runners who had a current knee injury compared with healthy controls.14 A lower FCA (6.8°) would be suggestive of an MFS landing pattern.4 Authors of the study speculated that the lower FCA values observed in the injured group were indicative of a potential compensatory pattern adapted by the runners in efforts to reduce knee loading.14 Given the retrospective case-control nature of this study, it is difficult to know how accurate this speculation may be.
Differences among study methodologies may be somewhat responsible for the lack of consistency among results, some of which included differences in FST assessment, testing conditions, and definition of injury. Regarding continuous measurements of FST assessment, FCA, AFA, and SI have been analyzed using force plate and 3D motion analysis14,15,18,37,48,53 and pressure-sensitive insoles.45 Meanwhile, categorically, FSP was determined using sagittal plane video camera recordings,11,21,32,61,66 and through self-reported FSP methods via an online survey.25 However, accuracy of self-reporting is limited, with only 44% to 69% of runners able to accurately report their FSP,4,26 which may explain differences in reported prevalence between Goss and Gross25 (RFS, 31%; MFS, 43%; FFS, 20%) and other studies (RFS, 69-97%; MFS, 3-24%; FFS, 2-31%).11,21,29,32,39,45 In consequence, the findings of Goss and Gross25 may be somewhat erroneous. In contrast to self-reporting methods, there is high correlation among all other measures of FST assessment with R values of 0.92 to 0.942,44 and an intraclass correlation coefficient of 0.97 between SI (as determined via pressure-sensitive insoles44 and force plate analysis2) and FCA (as determined via 3D motion analysis2,44). Moreover, it has been demonstrated that sagittal plane video recording, which is the most inexpensive method, has excellent accuracy (91%) in determining FSP when compared with both 3D motion analysis and pressure-sensitive insoles.49
Regarding testing conditions, most studies11,15,18,21,37,48,53,66 analyzed ≤5 foot strikes. Given that within-participant FCA variation can be up to 21º throughout a run and 56% of runners may demonstrate a combination of RFS, MFS, and FFS patterns during the same run,40 analyzing ≤5 foot strikes may result in atypical FSTs being selected as representative.
Other testing conditions that varied across studies included surface and running speed. It has been reported that surface stiffness can affect FST, with harder surfaces encouraging a non-RFS technique.40 Additionally, speed may influence FST, with RFS more commonly associated with slower speeds.20,45 With some studies using self-selected speeds and others using predetermined speeds, comparison of results across studies is challenging. While there are too few studies to discuss whether surface conditions and running speed have an effect on the relationship between FST and RRI, there is clearly a need for consensus on FST analysis. This is especially pertinent for determining the best methods for assessing (1) FST, (2) the minimum number of foot strikes needed to best reflect the runners’ most representative FST, and (3) whether the reporting of FST should be categorical (ie, FSP) or in its absolute continuous form (ie, FCA, AFA, and SI). Unfortunately, no studies have directly compared the aforementioned approaches on the same data set.
Another methodological difference among studies was the definition of injury. While some RRIs were reflective of a restriction in performance for 1 full session,18 other RRIs required this restriction in performance to last at least 1 week.14,25,45,66 This variance in injury definition poses a challenge when cross-comparing or pooling study results. In addition, given the evidence that loading on specific tissues and structures varies with FSP (ie, RFS: greater tibiofemoral load and patellofemoral compression force67; FFS: greater load on plantarflexor muscles and Achilles tendon24,28,38), it may not be optimal to investigate RRIs collectively, but rather investigations should be based on pathology. Comparison of FST with a general binominal overuse injury outcome (ie, injured or uninjured) does not account for the implications of injury severity of specific pathologies. While the analysis of specific injury sites (eg, knee, calf, shin) assists in our understanding of where the body was overloaded, consideration of the exact pathology may be more insightful in determining the clinical relevance of a potential relationship between FST and RRI. For example, common pathologies affecting runners at the shin might include medial tibial stress syndrome or a tibial stress fracture.22 Both of these pathologies have resulted from excessive load at the site of the tibia but would have significantly different severities in terms of time loss and health care provisions.22 Although some recent research has demonstrated analysis of FST and specific sites of injury,14,21,32,61 only 1 study in this review explored how FST may relate to specific pathologies11 but may not have had sufficient power to find significant relationships.
These findings are in agreement with the conclusions of a nonsystematic narrative review regarding the concepts, classifications, and implications for FST and RRIs by Hoenig et al,31 who suggested that relationships between FST and RRIs are mostly unclear at present and thus should be considered critically. Although the review by Hoenig et al was descriptive as opposed to the systematic approach taken in this review, the authors identify similar limitations from scoping the literature such as the lack of standardized methodologies and definitions relating to FST. Despite taking a more narrative approach, the authors note that FSP may increase the risk of some RRIs (RFS runners might experience more knee injuries, while MFS/FFS runners might experience ankle and foot injuries),31 but the basis of this evidence is indirect, as it stems from studies comparing the kinetics and kinematics of various FSPs rather than directly comparing injuries among RFS, MFS, and FFS runners. Similar to the conclusion of our review, this highlights the need for more research looking at the relationship between FST and specific injury pathologies.
Limitations of the Studies
Limitations of the reviewed studies, which were initially identified in the risk of bias assessment, include the following: examiners not being blinded to the outcome, a lack of power calculation in determining the required sample size for a clinical effect, and poor reporting or control of potential confounding factors (eg, years of running experience, workload ratios, other physical training stress experienced in military groups) for RRIs (Appendix Table A4, available online). The majority of studies also had small sample sizes and may not have been sufficiently powered for detection of significance. In addition, studies did not always explore interaction effects between FST and other potential injury-causing factors. Given that RRIs are multifactorial in nature18,48 and these etiological factors can be interdependent, exploration of all potential confounding factors should be undertaken, especially in groups such as military and collegiate runners who may have significant interdependent RRI risk factors (eg, training volume, training frequency, training load/additional weight carriage). Another limitation of the studies is the diversity of methodologies and outcome measures utilized, impeding cross-comparison of studies and synthesis of findings, particularly with respect to the definition of injury and FST analysis. Additionally, there appears to be a lack of analysis of specific RRIs and their relationship with FST, potentially limiting our understanding of how FST and specific injury pathologies relate. Imprecision of study results and indirectness of study methodologies featured as common pitfalls in the GRADE assessment, highlighting the need for more rigorous and sophisticated methods, with better standards of analysis required (eg, reporting confidence intervals and relative effects). With respect to FST assessment, while 3D motion and force plate analysis, sagittal plane video recordings, and pressure-sensitive insoles all demonstrate valid and reliable FST assessments, direct comparison of categorical and continuous measures of FST is impossible. Additionally, the number of foot strikes assessed was quite low.
Finally, a very significant limitation was the predominance of retrospective case-control study designs. It cannot be determined whether or not the retrospective findings relating FST to RRI are actually a cause or an effect of the injury. In particular, it is worth noting that none of the FSP studies11,21,25,32,61,66 were prospective; thus, the necessity for more large-scale prospective analysis on FST and its relationship with RRIs is warranted.
Limitations of This Review
This study was limited to a narrative analysis given the wide heterogeneity of study methodologies and outcome measures reported. While all included studies investigated a form of FST and RRIs, this exploration may not have been the intended aim of all studies, and thus there were difficulties with extracting and synthesising the results, preventing the completion of a meta-analysis.
Conclusion
There is a very low level of evidence to suggest a relationship between FST and RRIs. While two-thirds of categorical studies did find a relationship between FSP and RRI, these studies were limited by very low quality such as retrospective case-control study design, low sample sizes, and the use of potentially inaccurate self-reporting methodologies.
Therefore, more large-scale prospective studies with sufficient power are required. Studies looking at the relationship between FST and RRIs should consider other known confounding factors that relate to injury (eg, training load, years’ experience, previous injury history) and conduct adequate statistical analysis allowing for multifactorial analyses where necessary. Standardization of FST is required, and both categorical and continuous measures should be reported where possible, along with determining the number of foot strikes necessary to represent the FST of a runner. Moreover, additional statistical analysis should be undertaken to investigate the effect of FST and specific RRI pathologies (eg, patellofemoral pain syndrome, tibial stress fractures, Achilles tendinopathy) rather than solely exploring RRIs collectively.
Supplemental material for this article is available at http://journals.sagepub.com/doi/suppl/10.1177/23259671211020283.
Supplemental Material
Supplemental Material, sj-docx-1-ojs-10.1177_23259671211020283 for Risk Factors for Injuries in Runners: A Systematic Review of Foot Strike Technique and Its Classification at Impact by Aoife Burke, Sarah Dillon, Siobhán O’Connor, Enda F. Whyte, Shane Gore and Kieran A. Moran in Orthopaedic Journal of Sports Medicine
Supplemental Material, sj-docx-2-ojs-10.1177_23259671211020283 for Risk Factors for Injuries in Runners: A Systematic Review of Foot Strike Technique and Its Classification at Impact by Aoife Burke, Sarah Dillon, Siobhán O’Connor, Enda F. Whyte, Shane Gore and Kieran A. Moran in Orthopaedic Journal of Sports Medicine
Supplemental Material, sj-docx-3-ojs-10.1177_23259671211020283 for Risk Factors for Injuries in Runners: A Systematic Review of Foot Strike Technique and Its Classification at Impact by Aoife Burke, Sarah Dillon, Siobhán O’Connor, Enda F. Whyte, Shane Gore and Kieran A. Moran in Orthopaedic Journal of Sports Medicine
Supplemental Material, sj-docx-4-ojs-10.1177_23259671211020283 for Risk Factors for Injuries in Runners: A Systematic Review of Foot Strike Technique and Its Classification at Impact by Aoife Burke, Sarah Dillon, Siobhán O’Connor, Enda F. Whyte, Shane Gore and Kieran A. Moran in Orthopaedic Journal of Sports Medicine
Supplemental Material, sj-docx-5-ojs-10.1177_23259671211020283 for Risk Factors for Injuries in Runners: A Systematic Review of Foot Strike Technique and Its Classification at Impact by Aoife Burke, Sarah Dillon, Siobhán O’Connor, Enda F. Whyte, Shane Gore and Kieran A. Moran in Orthopaedic Journal of Sports Medicine
Supplemental Material, sj-docx-6-ojs-10.1177_23259671211020283 for Risk Factors for Injuries in Runners: A Systematic Review of Foot Strike Technique and Its Classification at Impact by Aoife Burke, Sarah Dillon, Siobhán O’Connor, Enda F. Whyte, Shane Gore and Kieran A. Moran in Orthopaedic Journal of Sports Medicine
Supplemental Material, sj-pdf-1-ojs-10.1177_23259671211020283 for Risk Factors for Injuries in Runners: A Systematic Review of Foot Strike Technique and Its Classification at Impact by Aoife Burke, Sarah Dillon, Siobhán O’Connor, Enda F. Whyte, Shane Gore and Kieran A. Moran in Orthopaedic Journal of Sports Medicine
Acknowledgment
The authors thank the participants for their time in partaking in this study.
Footnotes
Final revision submitted January 4, 2021; accepted February 22, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was supported by a grant from Science Foundation Ireland (No. SFI/12/RC/2289), cofunded by the European Regional Development Fund. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1.Almeida MO, Davis IS, Lopes AD. Biomechanical differences of foot-strike patterns during running: a systematic review with meta-analysis. J Orthop Sports Phys Ther. 2015;45(10):738–755. [DOI] [PubMed] [Google Scholar]
- 2.Altman AR, Davis IS. A kinematic method for footstrike pattern detection in barefoot and shod runners. Gait Posture. 2012;35(2):298–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anderson LM, Bonanno DR, Hart HF, Barton CJ. What are the benefits and risks associated with changing foot strike pattern during running? A systematic review and meta-analysis of injury, running economy, and biomechanics. Sports Med. 2020;50(5):885–917. [DOI] [PubMed] [Google Scholar]
- 4.Bade MB, Aaron K, McPoil TG. Accuracy of self-reported foot strike pattern in intercollegiate and recreational runners during shod running. Int J Sports Phys Ther. 2016;11(3):350–355. [PMC free article] [PubMed] [Google Scholar]
- 5.Bovens AMP, Janssen GME, Vermeer HGW, Hoeberigs JH, Janssen MPE, Verstappen FTJ. Occurrence of running injuries in adults following a supervised training program. Int J Sports Med. 1989;10(suppl 3):S186–S190. [DOI] [PubMed] [Google Scholar]
- 6.Bowersock CD, Willy RW, DeVita P, Willson JD. Independent effects of step length and foot strike pattern on tibiofemoral joint forces during running. J Sports Sci. 2017;35(20):2005–2013. [DOI] [PubMed] [Google Scholar]
- 7.Boyer ER, Rooney BD, Derrick TR. Rearfoot and midfoot or forefoot impacts in habitually shod runners. Med Sci Sports Exerc. 2014;46(7):1384–1391. [DOI] [PubMed] [Google Scholar]
- 8.Bredeweg SW, Kluitenberg B, Bessem B, Buist I. Differences in kinetic variables between injured and noninjured novice runners: a prospective cohort study. J Sci Med Sport. 2013;16(3):205–210. [DOI] [PubMed] [Google Scholar]
- 9.Brooks G, Fahey T, Baldwin K. Exercise Physiology: Human Bioenergetics and Its Application. 4th ed. McGraw-Hill Education; 2004. [Google Scholar]
- 10.Cavanagh PR, Lafortune MA. Ground reaction forces in distance running. J Biomech. 1980;13(5):397–406. [DOI] [PubMed] [Google Scholar]
- 11.Daoud AI, Geissler GJ, Wang F, Saretsky J, Daoud YA, Lieberman DE. Foot strike and injury rates in endurance runners: a retrospective study. Med Sci Sports Exerc. 2012;44(7):1325–1334. [DOI] [PubMed] [Google Scholar]
- 12.Davis I, Bowser B, Mullineaux D. Greater vertical impact loading in female runners with medically diagnosed injuries: a prospective investigation. Br J Sports Med. 2016;50(4):887–892. [DOI] [PubMed] [Google Scholar]
- 13.Deelen I, Janssen M, Vos S, Kamphuis CBM, Ettema D. Attractive running environments for all? A cross-sectional study on physical environmental characteristics and runners’ motives and attitudes, in relation to the experience of the running environment. BMC Public Health. 2019;19(1):366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dingenen B, Malliaras P, Janssen T, Ceyssens L, Vanelderen R, Barton CJ. Two-dimensional video analysis can discriminate differences in running kinematics between recreational runners with and without running-related knee injury. Phys Ther Sport. 2019;38:184–191. [DOI] [PubMed] [Google Scholar]
- 15.Donoghue OA, Harrison AJ, Laxton P, Jones RK. Lower limb kinematics of subjects with chronic Achilles tendon injury during running. Res Sports Med. 2008;16(1):23–38. [DOI] [PubMed] [Google Scholar]
- 16.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Heal. 1998;52:377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Drew MK, Finch CF. The relationship between training load and injury, illness and soreness: a systematic and literature review. Sports Med. 2016;46(6):861–883. [DOI] [PubMed] [Google Scholar]
- 18.Dudley RI, Pamukoff DN, Lynn SK, Kersey RD, Noffal GJ. A prospective comparison of lower extremity kinematics and kinetics between injured and non-injured collegiate cross country runners. Hum Mov Sci. 2017;52:197–202. [DOI] [PubMed] [Google Scholar]
- 19.Ferber R, Davis IM, Hamill J, Pollard CD, McKeown KA. Kinetic variables in subjects with previous lower extremity stress fractures. Med Sci Sports Exerc. 2002;34(5):S5. [Google Scholar]
- 20.Forrester SE, Townend J. The effect of running velocity on footstrike angle—a curve-clustering approach. Gait Posture. 2015;41(1):26–32. [DOI] [PubMed] [Google Scholar]
- 21.Fukusawa L, Stoddard R, Lopes AD. There is no difference in footstrike pattern distribution in recreational runners with or without anterior knee pain. Gait Posture. 2020;79:16–20. [DOI] [PubMed] [Google Scholar]
- 22.Gallo RA, Plakke M, Silvis ML. Common leg injuries of long-distance runners: anatomical and biomechanical approach. Sports Health. 2012;4(6):485–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goss DL, Gross MT. A comparison of negative joint work and vertical ground reaction force loading rates in Chi runners and rearfoot-striking runners. J Orthop Sport Phys Ther. 2013;43(10):685–692. [DOI] [PubMed] [Google Scholar]
- 24.Goss DL, Gross MT. A review of mechanics and injury trends among various running styles. US Army Med Dep J. 2012;62–71. [PubMed] [Google Scholar]
- 25.Goss DL, Gross MT. Relationships among self-reported shoe type, footstrike pattern, and injury incidence. US Army Med Dep J. 2012:25–30. [PubMed] [Google Scholar]
- 26.Goss DL, Lewek M, Yu B, Ware WB, Teyhen DS, Gross MT. Lower extremity biomechanics and self-reported foot-strike patterns among runners in traditional and minimalist shoes. J Athl Train. 2015;50(6):603–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guyatt G, Oxman A, Akl E, et al. GRADE guidelines, 1: introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–394. [DOI] [PubMed] [Google Scholar]
- 28.Hamill J, Gruber AAH. Is changing footstrike pattern beneficial to runners? J Sport Heal Sci. 2017;6(2):146–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hasegawa H, Yamauchi T, Kraemer W. Foot strike patterns of runners at the 15-km point during an elite-level half marathon. J Strength Cond Res. 2007;21(3):888. [DOI] [PubMed] [Google Scholar]
- 30.Hashizume S, Yanagiya T. A forefoot strike requires the highest forces applied to the foot among foot strike patterns. Sport Med Int Open. 2017;1(2):e37–e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoenig T, Rolvien T, Hollander K. Footstrike patterns in runners: concepts, classifications, techniques, and implications for running-related injuries. Dtsch Z Sportmed. 2020;71(3):55–61. [Google Scholar]
- 32.Hollander K, Johnson CD, Outerleys J, Davis IS. Multifactorial determinants of running injury locations in 550 injured recreational runners. Med Sci Sports Exerc. 2021;53(1):102–107. [DOI] [PubMed] [Google Scholar]
- 33.Hreljac A, Marshall RN, Hume PA. Evaluation of lower extremity overuse injury potential in runners. Med Sci Sports Exerc. 2000;32(9):1635–1641. [DOI] [PubMed] [Google Scholar]
- 34.Kluitenberg B, van Middelkoop M, Smits D, et al. The NLstart2run study: incidence and risk factors of running-related injuries in novice runners. Scand J Med Sci Sports. 2015;25(5):e515–e523. [DOI] [PubMed] [Google Scholar]
- 35.Knapik JJ, Graham B, Cobbs J, Thompson D, Steelman R, Jones BH. A prospective investigation of injury incidence and injury risk factors among army recruits in military police training. BMC Musculoskelet Disord. 2013;14(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kuhman D, Melcher D, Paquette M. Ankle and knee kinetics between strike patterns at common training speeds in competitive male runners. Eur J Sport Sci. 2016;16(4):433–440. [DOI] [PubMed] [Google Scholar]
- 37.Kuhman D, Paquette M, Peel S, Melcher D. Comparison of ankle kinematics and ground reaction forces between prospectively injured and uninjured collegiate cross country runners. Hum Mov Sci. 2016;47(47):9–15. [DOI] [PubMed] [Google Scholar]
- 38.Kulmala J, Avela J, Pasanen K, Parkkari J. Forefoot strikers exhibit lower running-induced knee loading than rearfoot strikers. Med Sci Sports Exerc. 2013;45(12):2306–2313. [DOI] [PubMed] [Google Scholar]
- 39.Larson P, Higgins E, Kaminski J, et al. Foot strike patterns of recreational and sub-elite runners in a long-distance road race. J Sports Sci. 2011;29(15):1665–1673. [DOI] [PubMed] [Google Scholar]
- 40.Lieberman DE, Castillo ER, Otarola-Castillo E, et al. Variation in foot strike patterns among habitually barefoot and shod runners in Kenya. PLoS One. 2015;10(7):e0131354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lieberman DE, Venkadesan M, Werbel WA, et al. Foot strike patterns and collision forces in habitually barefoot versus shod runners. Nature. 2010;463:531–535. [DOI] [PubMed] [Google Scholar]
- 42.Lun V, Meeuwisse WH, Stergiou P, Stefanyshyn D. Relation between running injury and static lower limb alignment in recreational runners. Br J Sports Med. 2004;38(5):576–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Majumdar D, Pal MS, Majumdar D. Effects of military load carriage on kinematics of gait. Ergonomics. 2010;53(6):782–791. [DOI] [PubMed] [Google Scholar]
- 44.Mann R, Malisoux L, Brunner R, et al. Reliability and validity of pressure and temporal parameters recorded using a pressure-sensitive insole during running. Gait Posture. 2014;39(1):455–459. [DOI] [PubMed] [Google Scholar]
- 45.Mann R, Malisoux L, Nührenbörger C, Urhausen A, Meijer K, Theisen D. Association of previous injury and speed with running style and stride-to-stride fluctuations. Scand J Med Sci Sports. 2015;25(6):e638–e645. [DOI] [PubMed] [Google Scholar]
- 46.McDougall C. Born to Run: A Hidden Tribe, Superathletes, and the Greatest Race the World Has Never Seen. Alfred A. Knopf; 2009. [Google Scholar]
- 47.Mercer JA, Horsch S. Heel-toe running: a new look at the influence of foot strike pattern on impact force. J Exerc Sci Fit. 2015;13(1):29–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Messier SP, Martin DF, Mihalko SL, et al. A 2-year prospective cohort study of overuse running injuries: The Runners And Injury Longitudinal Study (TRAILS). Am J Sports Med. 2018;46(9):2211–2221. [DOI] [PubMed] [Google Scholar]
- 49.Meyer F, Falbriard M, Aminian K, Millet GP. How accurate is visual determination of foot strike pattern and pronation assessment. Gait Posture. 2018;60:200–202. [DOI] [PubMed] [Google Scholar]
- 50.Milner CE, Ferber R, Pollard CD, Hamill J, Davis IS. Biomechanical factors associated with tibial stress fracture in female runners. Med Sci Sports Exerc. 2006;38(2):323–328. [DOI] [PubMed] [Google Scholar]
- 51.Moher D, Liberati A, Tetzlaff J, Altman DG; the PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. [DOI] [PubMed] [Google Scholar]
- 52.Morris JB, Goss DL, Miller EM, Davis IS. Using real-time biofeedback to alter running biomechanics: a randomized controlled trial. Transl Sport Med. 2019;3(1):63–71. [Google Scholar]
- 53.Paquette M, Milner C, Melcher D. Foot contact angle variability during a prolonged run with relation to injury history and habitual foot strike pattern. Scand J Med Sci Sports. 2017;27(2):217–222. [DOI] [PubMed] [Google Scholar]
- 54.Pohl MB, Hamill J, Davis IS. Biomechanical and anatomic factors associated with a history of plantar fasciitis in female runners. Clin J Sport Med. 2009;19(5):372–376. [DOI] [PubMed] [Google Scholar]
- 55.Roper JL, Harding EM, Doerfler D, et al. The effects of gait retraining in runners with patellofemoral pain: a randomized trial. Clin Biomech (Bristol, Avon). 2016;35:14–22. [DOI] [PubMed] [Google Scholar]
- 56.Schwellnus M, Soligard T, Alonso JM, et al. How much is too much? (Part 2) International Olympic Committee consensus statement on load in sport and risk of illness. Br J Sports Med. 2016;50(17):1043–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Shih Y, Lin KL, Shiang TY. Is the foot striking pattern more important than barefoot or shod conditions in running? Gait Posture. 2013;38(3):490–494. [DOI] [PubMed] [Google Scholar]
- 58.Shorten M, Mientjes MIV. The “heel impact” force peak during running is neither “heel” nor “impact” and does not quantify shoe cushioning effects. Footwear Sci. 2011;3(1):41–58. [Google Scholar]
- 59.Smits D, Huisstede B, Verhagen E, et al. Short-term absenteeism and health care utilization due to lower extremity injuries among novice runners: a prospective cohort study. Clin J Sport Med. 2016;26(6):502–509. [DOI] [PubMed] [Google Scholar]
- 60.Stiffler-Joachim MR, Wille CM, Kliethermes SA, Johnston W, Heiderscheit BC. Foot angle and loading rate during running demonstrate a nonlinear relationship. Med Sci Sports Exerc. 2019;51(10):2067–2072. [DOI] [PubMed] [Google Scholar]
- 61.Sugimoto D, Kelly BD, Mandel DL, et al. Running propensities of athletes with hamstring injuries. Sports. 2019;7(9):210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Thompson MA, Lee SS, Seegmiller J, McGowan CP. Kinematic and kinetic comparison of barefoot and shod running in mid/forefoot and rearfoot strike runners. Gait Posture. 2015;41(4):957–959. [DOI] [PubMed] [Google Scholar]
- 63.Van Gent RN, Siem D, van Middelkoop M, van Os AG, Bierma-Zeinstra SM, Koes BW. Incidence and determinants of lower extremity running injuries in long distance runners: a systematic review. Br J Sports Med. 2007;41(8):469–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Van Mechelen W, Hlobil H, Kemper HCG, Voorn WJ, De Jongh HR. Prevention of running injuries by warm-up, cool-down, and stretching exercises. Am J Sports Med. 1993;21(5):711–719. [DOI] [PubMed] [Google Scholar]
- 65.Viru A, Viru M. Nature of training effects. Exerc Sport Sci. 2000;6(7):67–95. [Google Scholar]
- 66.Warr B, Fellin R, Sauer S, Goss D. Characterization of foot-strike patterns: lack of an association with injuries or performance in soldiers. Mil Med. 2015;180(7):830–834. [DOI] [PubMed] [Google Scholar]
- 67.Willson JD, Ratcliff OM, Meardon SA, Willy RW. Influence of step length and landing pattern on patellofemoral joint kinetics during running. Scand J Med Sci Sports. 2015;25(6):736–743. [DOI] [PubMed] [Google Scholar]
- 68.Yamato TP, Saragiotto BT, Lopes AD. A consensus definition of running-related injury in recreational runners: a modified Delphi approach. J Orthop Sports Phys Ther. 2015;45(5):375–380. [DOI] [PubMed] [Google Scholar]
- 69.Yong J, Silder A, Montgomery K, Fredericson M, Delp S. Acute changes in foot strike pattern and cadence affect running parameters associated with tibial stress fractures. J Biomech. 2018;76:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-docx-1-ojs-10.1177_23259671211020283 for Risk Factors for Injuries in Runners: A Systematic Review of Foot Strike Technique and Its Classification at Impact by Aoife Burke, Sarah Dillon, Siobhán O’Connor, Enda F. Whyte, Shane Gore and Kieran A. Moran in Orthopaedic Journal of Sports Medicine
Supplemental Material, sj-docx-2-ojs-10.1177_23259671211020283 for Risk Factors for Injuries in Runners: A Systematic Review of Foot Strike Technique and Its Classification at Impact by Aoife Burke, Sarah Dillon, Siobhán O’Connor, Enda F. Whyte, Shane Gore and Kieran A. Moran in Orthopaedic Journal of Sports Medicine
Supplemental Material, sj-docx-3-ojs-10.1177_23259671211020283 for Risk Factors for Injuries in Runners: A Systematic Review of Foot Strike Technique and Its Classification at Impact by Aoife Burke, Sarah Dillon, Siobhán O’Connor, Enda F. Whyte, Shane Gore and Kieran A. Moran in Orthopaedic Journal of Sports Medicine
Supplemental Material, sj-docx-4-ojs-10.1177_23259671211020283 for Risk Factors for Injuries in Runners: A Systematic Review of Foot Strike Technique and Its Classification at Impact by Aoife Burke, Sarah Dillon, Siobhán O’Connor, Enda F. Whyte, Shane Gore and Kieran A. Moran in Orthopaedic Journal of Sports Medicine
Supplemental Material, sj-docx-5-ojs-10.1177_23259671211020283 for Risk Factors for Injuries in Runners: A Systematic Review of Foot Strike Technique and Its Classification at Impact by Aoife Burke, Sarah Dillon, Siobhán O’Connor, Enda F. Whyte, Shane Gore and Kieran A. Moran in Orthopaedic Journal of Sports Medicine
Supplemental Material, sj-docx-6-ojs-10.1177_23259671211020283 for Risk Factors for Injuries in Runners: A Systematic Review of Foot Strike Technique and Its Classification at Impact by Aoife Burke, Sarah Dillon, Siobhán O’Connor, Enda F. Whyte, Shane Gore and Kieran A. Moran in Orthopaedic Journal of Sports Medicine
Supplemental Material, sj-pdf-1-ojs-10.1177_23259671211020283 for Risk Factors for Injuries in Runners: A Systematic Review of Foot Strike Technique and Its Classification at Impact by Aoife Burke, Sarah Dillon, Siobhán O’Connor, Enda F. Whyte, Shane Gore and Kieran A. Moran in Orthopaedic Journal of Sports Medicine