Abstract
Background:
The average professional soccer team experiences 1 to 2 traumatic leg fractures per season, with unknown effects on player performance.
Purpose:
To (1) determine the rate and time to return to play (RTP) following leg fracture, (2) investigate the rate of reinjury following RTP, and (3) investigate long-term effects that lower extremity (LE) fracture may have on elite soccer player performance.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Using publicly available records, we identified athletes sustaining a traumatic leg fracture across the 5 major European soccer leagues (English Premier League, Bundesliga, La Liga, Ligue 1, and Serie A) between 2000 and 2016. Athletes with leg fracture (femur, tibia, and/or fibula) were matched 1:2 to controls by demographic characteristics and performance metrics 1 season before the index timepoint. Investigations included the RTP rate, reinjury rate, player characteristics associated with RTP within 2 seasons, long-term player retention, performance metrics during the 4 following seasons, and subgroup analysis by player position.
Results:
A total of 112 players with LE fracture and 224 controls were identified. Players with LE fractures were absent for a mean of 157 days (range, 24-601 days) and 21 games (range, 2-68 games). The rate of RTP within 1 season was 80%, with 4% experiencing subsequent refracture. Injured players remained active in the league at a higher rate than their uninjured counterparts. As compared with controls, injured athletes played 309 fewer total minutes (P < .05), scored 0.09 more assists per game (P < .01) 1 season after injury, and scored 0.12 more points per game 4 seasons after injury (P < .01). Defenders were most affected by an LE fracture, playing 5.24 fewer games (P < .05), 603 fewer total minutes (P < .01), and recording 0.19 more assists per 90 minutes of play as compared with controls 1 season after injury (P < .001). Attackers and midfielders demonstrated no significant difference in metrics after RTP when compared with controls.
Conclusion:
Most players sustaining an LE fracture returned to elite soccer at the same level after a significant loss of playing time, with a 4% rate of refracture. Player retention was higher for those sustaining an LE fracture versus uninjured controls. Overall, injured players did not experience a decline in performance after recovery from an LE fracture.
Keywords: football (soccer), general sports trauma, performance outcomes, lower extremity fracture, case-control
Soccer is the world’s most popular sport and is currently played by an estimated 270 million people, equivalent to 4% of the world’s population.9 Fractures constitute an estimated 3% to 4% of all injuries sustained among male professional soccer players.4,18 Most of these are in the lower extremity (LE) and range in acuity from acute traumatic fractures to chronic overuse stress fractures.18 Traumatic fractures are most commonly fractures of the tibia or the fibula and typically occur in game situations.4 Mechanisms of injury include contact made during a sliding tackle, collision with a goalkeeper, or collision between 2 players contesting a loose ball leading to high-energy injuries.3
Recent investigations on LE fractures in soccer athletes have been tailored toward development of protocols for optimized surgical and rehabilitative management.24,28,33 Both traumatic and chronic fractures pose the risk of loss of play time because of prolonged rehabilitation after injury.1,6,8,18,34 In elite soccer players, the recovery period following an LE fracture has been reported to be within a range of 2 to 9 months, depending on the site of fracture.1,8,34 Rates of return to play (RTP) following LE fractures have been reported to be 43% in National Basketball Association athletes but have not been established in professional soccer athletes.14 Considering that the average professional soccer team experiences an estimated 1 to 2 fractures per season and recovery from an LE fracture often requires significant rehabilitation, it is evident that LE fractures pose the potential for significant loss of time on the field, of productivity, and of value. This is further compounded by the potential for permanent changes in a player’s functional movement patterns and higher risk of subsequent injury.1,7,31
Previous investigations on LE fractures in professional soccer players have focused on epidemiology and rehabilitation, with limited sample sizes.28,30,31 There is a paucity of literature regarding the potential association between LE injury and possible effects on player performance after RTP. The purpose of this matched-cohort analysis was to (1) provide a comprehensive report of the rates of LE fractures within the 5 major European soccer leagues, (2) characterize rates of RTP and reinjury, and (3) investigate changes in performance metrics in players with LE fracture as compared with a matched cohort.
Methods
A retrospective review of male soccer players in any of the 5 major European soccer leagues (English Premier League, Bundesliga, Serie A, La Liga, and Ligue 1) was conducted from 2000 to 2016 via a publicly available database, as established in previous investigations.10,12,24,37–39 Players with traumatic fractures involving the femur, the tibia, and/or the fibula were identified for inclusion in the LE fracture cohort. Players with no recorded injury of the LE were identified for inclusion in the control cohort. Tibial and fibular fractures that would be considered “ankle fractures” were excluded. All player injury reports were cross-referenced with official league reports, official team websites, injury reports, official team press releases, personal websites, and professional statistical websites, as described in the aforementioned investigations.
Inclusion criteria consisted of the following: the player was on the team roster during a season the team qualified for participation in 1 of the 5 major leagues; participated in at least 1 game before injury; and had a minimum 1-year follow-up after injury. Players with ambiguous injury status were excluded from both injury and control cohorts to minimize potential confounders and skewing. Data collected for each individual player included demographic data (age, height, position, and playing experience), recovery time after injury (days and games missed), field time metrics (total time played in the season, games played, and average minutes played per game), and performance metrics (goals scored, assists, and points per game). Goals and assists were standardized to 90 minutes of play to account for differing total field time between players. Players with reinjury were defined as those with documentation of femoral, tibial, fibular, or both tibial and fibular fractures at a date more than 12 weeks from the primary injury. There were no players with duplicate documentation of LE fracture within 12 weeks of the primary injury.
Cases and Controls
A matched-cohort analysis was utilized to compare performance metrics between players with an LE fracture and those without LE injury. Players with an LE fracture were matched to the control cohort in a 1:2 ratio using an optimized matching frontier methodology, a technique with concepts derived from k–nearest neighbor imputation.15–17,20 Players were matched by both demographic characteristics and baseline performance metrics. Demographic characteristics consisted of age, height, playing experience (within 1 year), and position, while performance metrics consisted of total field time, goals scored per 90 minutes of play, and assists per 90 minutes of play recorded 1 season before the index timepoint (year of injury for LE fracture cohort).25–27 The acceptable ranges of matching for playing experience, goals, and assists were selected based on the calculated variability of these features before any data processing. Goalkeepers were included in the descriptive analysis but were subsequently excluded from the case-control analysis because the very low number of injured players was not conducive to reasonable analysis with long-term follow-up.24,25
Statistical Analysis
Player characteristics associated with RTP within 2 seasons of injury were investigated by use of a logistic multivariable regression. The log-rank test was utilized to compare player retention in the league between control and injured cohorts during the follow-up period. The seasonal field time and performance metrics were collected from 3 seasons prior to the index timepoint (year of injury for the LE fracture cohort) through 4 seasons after the index timepoint. Overall differences between control and injured cohorts were assessed for each metric and timepoint combination, with subsequent subgroup analysis by player position. Univariate 2-group comparisons were performed using independent 2-group t tests or independent Wilcoxon rank-sum tests when normality distributions were violated. Chi-square tests were utilized to compare categorical data. Statistical significance was set at P < .05; all analyses were performed using R Studio software Version 3.6.2 (R Foundation for Statistical Computing).
Results
Characteristics
A total of 112 elite soccer players who sustained a traumatic LE fracture between 2000 and 2016 were identified. The mean age of the injured cohort was 24.97 ± 3.72 years, with a mean 4.95 ± 3.72 years played in the league at the time of injury. The matching between cases and controls was satisfactory, with no significant differences in player characteristics or baseline metrics 1 season before the index timepoint (Table 1 ). The LE fracture cohort consisted of 40 fibular (36%), 31 femoral (28%), 22 tibial (20%), and 19 concomitant tibial and fibular fractures (17%) (Table 2).
Table 1.
Player Characteristics and Baseline Metricsa
| Control (n = 224) |
LE Fractureb
(n = 112) |
P Value | |
|---|---|---|---|
| Case-control match | |||
| Player position, n | .939 | ||
| Attacker | 62 | 31 | |
| Midfielder | 68 | 34 | |
| Defender | 84 | 42 | |
| Goalkeeper | 0 | 5 | |
| Season of play (calendar year) | 2013 ± 4.66 | 2010 ± 4.03 | .068 |
| Years played before index timepoint | 3.53 ± 3.06 | 4.95 ± 3.72 | ≥.999 |
| Height, m | 1.82 ± 0.06 | 1.82 ± 0.06 | .746 |
| Age during season, y | 24.33 ± 3.87 | 24.97 ± 3.72 | .139 |
| Baseline metricsb | |||
| Games played | 20.2 ± 11.37 | 21.51 ± 11.14 | .459 |
| Total time played | 1499.39 ± 1072.36 | 1634.35 ± 1051.16 | .422 |
| Goals scoredc | 0.15 ± 0.17 | 0.21 ± 0.21 | .220 |
| Assists recordedc | 0.24 ± 0.56 | 0.15 ± 0.12 | .342 |
aData are reported as mean ± SD unless otherwise indicated. LE, lower extremity.
bMetrics 1 season before the index timepoint.
cStandardized to 90 minutes of play.
Table 2.
Injury Characteristics (n = 112 players)a
| Characteristic | Value |
|---|---|
| Bone fractured | |
| Tibia | 22 (20) |
| Fibula | 40 (36) |
| Tibia and fibula | 19 (17) |
| Femur | 31 (28) |
| Primary injury | |
| Days missed | 156.56 ± 110.56 |
| Games missed | 20.96 ± 14.35 |
| RTP | |
| At any timepoint | 90 (80) |
| By 1 season after injury | 81 (72) |
| By 2 seasons after injury | 86 (77) |
| By 3 seasons after injury | 89 (79) |
| By 4 seasons after injury | 90 (80) |
| Secondary injury | |
| Number of LE refractures | 14 (12) |
| Time to LE refracture, y | 4.21 ± 3.04 |
| Days missedb | 124.07 ± 99.38 |
| Games missedc | 18.14 ± 11.02 |
aData are reported as mean ± SD or n (%). LE, lower extremity; RTP, return to play.
bNot significantly different compared with primary injury (P = .415).
cNot significantly different compared with primary injury (P = .587).
Return to Play
A total of 90 (80%) of players with an LE fracture returned to play at the same level. Of these, 81 (72%) returned within 1 season. Players missed a mean of 157 days (range, 24-601 days) and 21 games (range, 2-68 games). Four players experienced a subsequent LE fracture 8, 12, 13, and 20 months after the initial injury. Three players sustained refracture of the same bone (tibia and fibula, fibula, and tibia only) while 1 player initially sustained a fibular shaft fracture and subsequently a tibial fracture. There were no significant differences in days or games missed as compared with primary injury (Table 2).
Factors considered in the analysis of RTP included demographic characteristics (bone fractured, age, player experience in the league, position of play) and performance metrics 1 season before injury (games played, time played, total goals, and total assists). On the univariate analysis, correlations between player characteristics and time to RTP were minimal (r = 0.2), with no statistically significant associations (P > .05). Combined tibial and fibular fractures were associated with the longest time to RTP (median, 183; interquartile range [IQR], 145-290 days), followed by isolated tibial fracture (median, 150; IQR, 104-206 days). Femoral fractures (median, 97; IQR, 55-185 days) and isolated fibular fractures (median, 91; IQR, 70-131 days) had similar time to RTP. There were no statistically significant differences between the time to RTP and the bone fractured (P = .376).
There were no player characteristics associated with likelihood of RTP within 2 years on the multivariable regression (Table 3).
Table 3.
Multivariable Regression of RTP Within 2 Seasons of Injurya
| OR (95% CI) | P Value | |
|---|---|---|
| Bone fractured | ||
| Tibia | Reference | |
| Fibula | 1.17 (0.59-2.42) | .67 |
| Tibia and fibula | 1.01 (0.44-2.30) | .98 |
| Femur | 0.91 (0.43-2) | .81 |
| Age, y | ||
| <21 | Reference | |
| 21-25 | 1.02 (0.48-2.43) | .96 |
| 26-30 | 0.80 (0.35-2.02) | .62 |
| >30 | 0.90 (0.29-2.75) | .85 |
| Time in league, y | ||
| <3 | Reference | |
| 3-5 | 0.81 (0.41-1.57) | .53 |
| 6-8 | 1.06 (0.47-2.27) | .89 |
| >8 | 0.93 (0.39-2.16) | .86 |
| Player position | ||
| Goalkeeper | Reference | |
| Attacker | 0.96 (0.50-1.85) | .89 |
| Midfielder | 0.94 (0.45-1.95) | .86 |
| Defender | 0.94 (0.23-3.04) | .92 |
| Games playedb | ||
| <10 | Reference | |
| 10-19 | 1.55 (0.63-3.47) | .31 |
| 20-29 | 1.72 (0.43-6.11) | .42 |
| >30 | 1.56 (0.13-14.78) | .70 |
| Time played, minb | ||
| <1000 | Reference | |
| 1000-1999 | 0.90 (0.28-2.94) | .86 |
| 2000-2500 | 0.99 (0.20-4.51) | .99 |
| >2500 | 1.19 (0.12-14.28) | .89 |
| Goalsb | ||
| <3 | Reference | |
| 3-6 | 0.97 (0.39-2.20) | .95 |
| 7-9 | 1.04 (0.25-3.46) | .95 |
| >9 | 0.51 (0.02-3.52) | .55 |
| Assistsb | ||
| 0-3 | Reference | |
| >3 | 1.01 (0.28-3.24) | .99 |
aRTP at same league level. OR, odds ratio; RTP, return to play.
bOverall metrics for 1 season before the index timepoint.
Player Availability After RTP
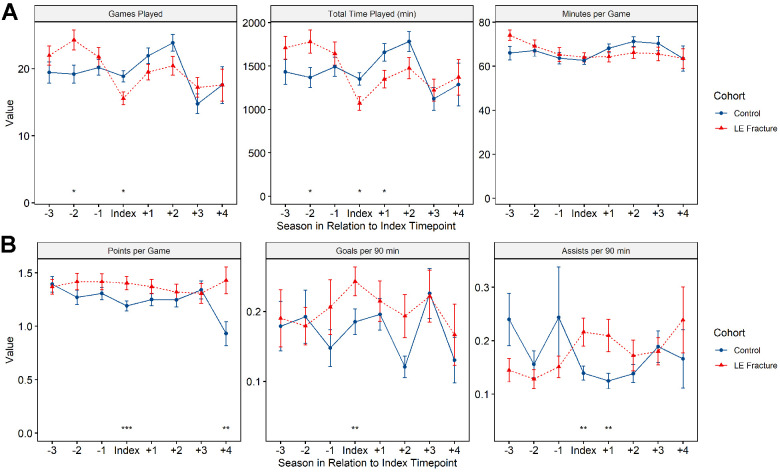
Players sustaining an LE fracture remained active in the league, playing >1 game per season, at a higher rate than controls up to 4 seasons after the index timepoint (P < .001) (Figure 1). Of the players who had retired before the endpoint of this study, there was no significant difference in total career length between controls (14.90 ± 4.07 years) and those sustaining an LE fracture (13.5 ± 4.24 years; P = .056). Within the injured cohort, players demonstrated similar long-term availability regardless of their fractured bone (P = .103).
Figure 1.
Player retention in the leagues by injury status during the study follow-up period. LE, lower extremity.
Player Performance
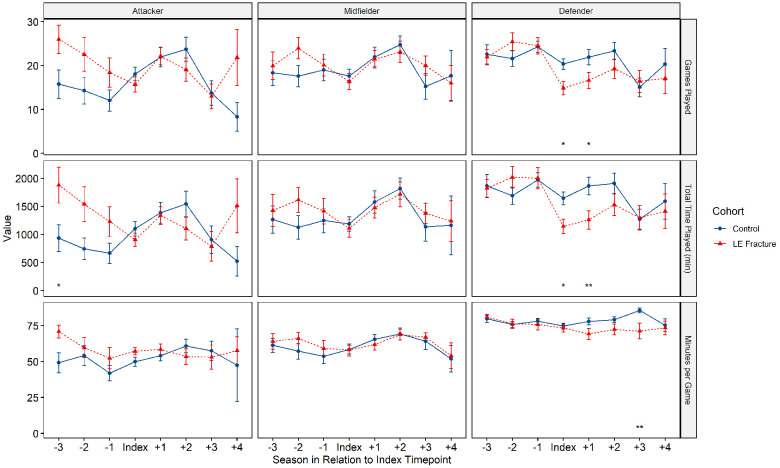
After RTP, players who sustained an LE fracture played 309 fewer minutes 1 season after injury (P < .05) but otherwise had no significant differences in field time as compared with controls (Figure 2). On the other hand, players who sustained an LE fracture scored 0.09 more assists per 90 minutes of play 1 season after injury (P < .01) and 0.12 more points per game 4 seasons after injury (P < .01) (Figure 2).
Figure 2.
Player performance and field time: (A) games played, total time played in minutes, and minutes per game, and (B) points per game, goals per 90 minutes, and assists per 90 minutes. Statistically significant differences between study groups: *P < .05, **P < .01, ***P < .001. LE, lower extremity.
Of note, injured athletes had played significantly more games (P < .05) and total minutes (P < .05) as compared with controls 2 seasons before injury (Figure 2 ). During the season of injury, athletes with an LE fracture demonstrated significantly less field time (games and total minutes player per season; P < .05), yet recorded more assists and goals per 90 minutes of play (P < .01) as well as more points per game (P < .001) as compared with the control cohort.
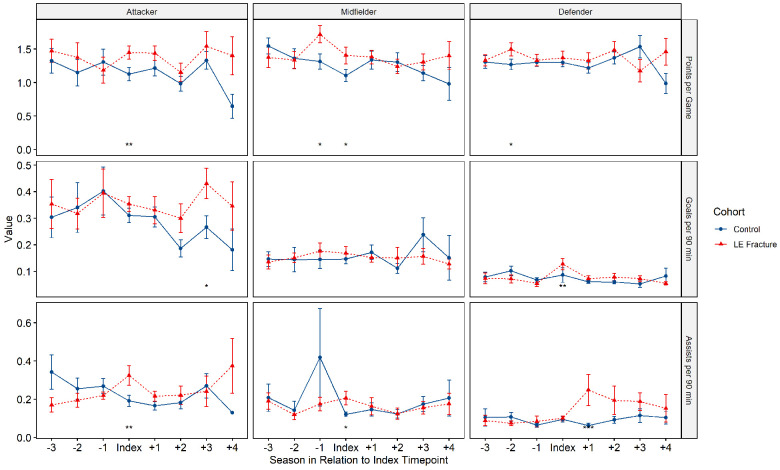
Field Time by Position
Defenders with an LE fracture demonstrated significant differences in field time, playing 5.24 fewer games (P < .05) and 603 fewer total minutes (P < .01) as compared with controls 1 season after injury. This trend persisted 3 seasons after injury, with defenders logging 14.24 fewer minutes per game as compared with controls (P < .01). On the other hand, defenders in both cohorts played an equivalent number of minutes per game up to 3 seasons after injury, at which point the injured cohort played approximately 14 fewer minutes per game (P < .01) as compared with controls (Figure 3). Attackers and midfielders had no significant changes in games played, total time played, or minutes per game as compared with controls at any timepoint (Figure 3).
Figure 3.
Field time metrics by player position. Statistically significant differences between study groups: *P < .05, **P < .01. LE, lower extremity.
Compared with players who sustained an isolated tibial or fibular fracture, femoral or combined tibial and fibular fractures demonstrated significantly diminished field time 2 and 4 seasons after injury. Specifically, players sustaining combined tibial and fibular fractures demonstrated the most significant difference in field time 2 seasons after injury, playing approximately 7 fewer games (P < .05), approximately 800 fewer total minutes (P < .01), and 15 fewer minutes per game (P < .01) as compared with players with isolated fractures. Players sustaining femoral fractures demonstrated a significant decline in field time 4 seasons after injury, playing fewer total minutes (P < .05) and minutes per game (P < .01) as compared with players sustaining isolated tibial or isolated fibular fractures.
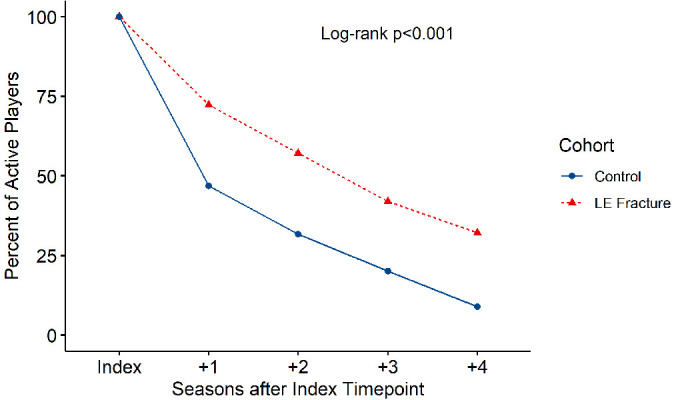
Player Performance by Position
There were no player position subgroups that demonstrated decreased performance after an LE fracture. Attackers sustaining an LE fracture scored 0.16 more goals per 90 minutes played as compared with controls 3 seasons after injury (P < .05). Similarly, defenders recorded 0.19 more assists per 90 minutes of play as compared with controls 1 season after injury (P < .001). Midfielders did not demonstrate significant differences in any performance metric after the index timepoint. However, attackers and midfielders both scored more points per game (0.32 [P < .01] and 0.30 [P < .05], respectively) and assists per 90 minutes of play (0.19 [P < .01] and 0.09 [P < .05], respectively) during the season of injury (Figure 4).
Figure 4.
Performance metrics by player position. Statistically significant differences between study groups: *P < .05, **P < .01, ***P < .001. LE, lower extremity.
Discussion
Although our understanding of the epidemiology of LE fractures within soccer continues to improve, the impact of these injuries on RTP and player performance remains unknown. In this retrospective study of elite soccer players who sustained traumatic LE fractures, an encouraging rate of RTP (80%) was observed. However, LE fracture was associated with prolonged recovery—a mean of 5 months and 20 missed games. In addition, a high risk of refracture (12%) was observed. Despite the duration and risks of recovery, injured players had greater league retention, remaining active in the league at a higher rate than their uninjured counterparts. Furthermore, injured players recorded higher points per game, despite reduced playing time the season following injury. Although defenders were most affected by LE fractures, with decline in games and total minutes the season following injury, their performance metrics improved, with more assists recorded than their uninjured teammates. Taken together, these results suggest that although LE fracture results in significant missed time and elevated risk of reinjury in elite soccer players, career longevity and performance is not compromised.
A prospective study of 41 teams in the Union of European Football Association (UEFA) Champions League from 2001 to 2012 reported that fractures, including both stress and traumatic, accounted for 3.5% of all injuries during the study period, corresponding to an overall traumatic fracture incidence rate of 0.25 per 1000 hours of soccer exposure.18 The current investigation identified 112 elite-level soccer players sustaining an LE fracture between the 1999-2000 and 2015-2016 seasons of the 5 major European soccer leagues. Taking into account the mean number of games per season in each league, this corresponds to a similar rate of 1.9 traumatic LE fractures per 1000 hours of soccer per player. Isolated fibular shaft fractures are reported to be the most common bone fractured, with reported proportions of all fractures ranging from 6.3% to 9%.18,36 This is consistent with the current series, where isolated fibular fractures accounted for over one-third of all LE fractures. Furthermore, the incidence of traumatic LE fracture is reported to be highest in defenders, followed by midfielders and attackers.18 The injured cohort in our study demonstrated significantly higher field time and superior performance during the season of injury as compared with controls. This suggests that while defenders may be at higher risk for LE fracture, an aggressive style of play in midfielders or attackers may enhance performance metrics at the cost of higher injury risk. While player absence because of injury negatively affects value, athletes at higher risk of injury may tend toward engagement in more risky maneuvers with potentially high reward, leading to higher player valuation and long-term retention.
Although overall RTP rates were encouraging, 1 in 5 players did not make it back onto the field. In an effort to identify players at higher risk of failure, it would be helpful to isolate factors associated with successful RTP. Unfortunately, the present study was unable to find any baseline demographic, injury, or performance characteristics associated with RTP within 2 seasons of injury. While higher joint hyperlaxity, lower skill level, and low hamstring-to-quadriceps ratio have been associated with increased risk of traumatic LE reinjury in soccer, there have been no reports on factors associated with higher likelihood of RTP following a traumatic LE fracture.6,23 Of note, age >30 years and secondary injury have been associated with lower odds of RTP at the same league level in the context of Achilles tendon ruptures.12 Fracture management was not investigated in the present study, but it may have affected outcomes and RTP. Surgical intervention has been reported to result in higher rates of RTP, possibly because of a combination of extended recovery and definitive fracture fixation.29 However, the risk of surgical complications may not lead to an overall net benefit when compared with nonoperative management and cautious radiographic confirmation of the union before RTP.2,22,29 Further investigations may continue to clarify the multitude of factors likely affecting RTP at the same league level for individual players.
The overall RTP rate to the same league level was 80% in the present cohort, with a mean time to RTP of 136 days and 18 games missed. Previous studies have reported similar RTP rates of 86% at any level within 2 years of injury and 83% at the same league level or higher in professional soccer.30 In the ongoing UEFA injury study,18 prospectively tracking a subset of the players included in the present investigation, the mean time to RTP was reported to be 140 days for tibial and fibular fractures and 77 days for isolated fibular fractures. Of note, the UEFA study did not further categorize bone fractures of the tibia, the fibula, and the femur based on injury mechanism, and it included both stress and traumatic fractures.18 The results of the present study lie within the range of these previous findings, and regardless of minor differences in absolute numbers of days missed, all reports support a significant loss of field time following an LE fracture.
A high rate of reinjury and a 4% refracture rate after RTP was observed in the study cohort. However, this finding is echoed in prior studies, including athletes with fractures across other professional leagues and sports. Similar frequencies have been described in English soccer as well as other major American sports leagues.18,23,33 The surgical treatment of LE stress fractures in basketball players is associated with a 10% rate of reoperation, similar to rates of refracture currently reported in the literature.14 The mean time to RTP following any primary fracture in UEFA athletes has been reported to be lower than recommended guidelines and was accompanied by a 35-day increase in time to RTP after a refracture.18 Nonunion is a commonly reported risk factor for refracture, elevating the importance of time-appropriate RTP regardless of nonoperative or operative management. Return to full contact sport after a tibial shaft fracture is generally recommended at around 24 weeks, suggesting that many of the injured players in the present study returned prematurely based on current guidelines.28 Previous literature on LE refracture in UEFA athletes had reported a 35-day delay in time to RTP as compared with primary injury.6 On the other hand, the present cohort of athletes sustaining refracture demonstrated a time to RTP 24 days shorter than that of primary injury. These results are more similar to differences in time to RTP between primary and reinjury observed for other common types of injuries in UEFA players.18 Another proposed risk factor for refracture has been the percentage of games started during the season of RTP, highlighting the importance of continued efforts in the development of rehabilitation protocols and responsible long-term monitoring of athletes after injury.19,21,33
Finally, players sustaining an LE fracture were found to play 309 fewer minutes, yet score 0.09 more assists per 90 minutes of play as compared with controls 1 season after injury. To our knowledge, there have been no previous reports of player performance following RTP after an LE fracture in elite-level soccer players. However, several investigations within different sports have reported on player performance following RTP after other LE injuries, with conflicting results.14,33,35 Players in major American sports leagues sustaining metatarsal fracture have been reported to return to the same level of play and performance 1 year following injury, whereas basketball players sustaining stress fractures have been reported to play fewer games and record fewer steals 1 season after injury.14,33 While type of injury may certainly affect player performance, there are an abundance of other biopsychosocial factors that likely affect player performance following RTP, including management of the injury, coach and player goals of time to RTP, rehabilitation methods, player adherence to rehabilitation plans, and baseline performance before injury.
The subgroup analysis of field time and performance metrics by player position revealed that defenders experienced a significant decrease in total time and games played and a significant increase in goals and assists per 90 minutes of play as compared with controls 1 season after injury. Defenders have been reported to have the highest incidence of LE fracture among playing positions.18 Additionally, defenders have been noted to be, on average, 1 year older than their midfielder and attacker teammates.13 While this difference may be negligible in a practice providing care for all ages across adulthood, a mean age difference of 1 year is a substantially larger proportion of the typical age range of professional soccer athletes. Older age has been associated with subsequent risk of refracture in professional athletes, with a proposed mechanism being the age-dependent decrease bone in mineral density.3,23,36 With regard to risk of refracture, it is unknown whether the repetitive mechanical loading exposure during soccer training is protective, due to increased bone density under mechanical loading, or a risk factor, due to repetitive motion exposure.11 Nonetheless, coaches limiting field time for their older defenders to protect them from refracture may be contributing to the observed decrease in field time for defenders. On the other hand, attackers and midfielders demonstrated no significant differences in field time after RTP. It is interesting to note that athletes playing in both of these positions scored significantly more points and assists per game during the year of injury, suggesting that these players sustained a traumatic LE fracture secondary to more aggressive playing tactics as compared with the control cohort.
Limitations
There were a number of strengths and weaknesses to the present study. Publicly accessible data sources were utilized in generating the LE fracture and control cohorts. As such, selection bias may have occurred because of underreporting of LE fractures to the public. However, this limitation was likely minimal, as traumatic fractures are evident to the public during games and subsequently lead to prolonged absence for postinjury rehabilitation, thus rendering the likelihood of omitted LE fracture documentation very low. In addition, the incidence of LE fractures in this population is consistent with that reported within the prospective UEFA injury study.18 Second, manual selection of players and propensity score matching are 2 popular ways of creating cohorts for studies. However, both present serious issues when employed in limited sample sizes because of their higher risk of selection bias and imbalance in characteristics between cohorts. This may lead to significant skewing of data and potentially masking effects of statistical models.16,17,20 Third, decisions on time of RTP may also be affected by nonmedical factors (eg, roster limits, time in season). A significant strength of this study was the use of frontier matching for the selection of the control cohort. Frontier matching is a methodology with concepts derived from k–nearest neighbor clustering, and it thus minimizes the imbalances between groups and reduces potential risks of selection bias.15
Finally, because of the nature of publicly sourced data, it was not possible to obtain each player’s specific treatment radiographic diagnosis (including diaphyseal vs metaphyseal vs intra-articular fracture subtypes) or regimen (including surgical vs nonsurgical management) without access to official medical record documentation. It is important to note that the only existing study that had the capability of reporting on elite soccer athlete injuries within the context of specific management regimens all involved the same authors, with disclosures of direct funding and supervision from the UEFA.37 Publications with these data have been limited to epidemiologic investigations of incidence, RTP, and reinjury rates rather than changes in performance following injury.4–6,32,39 To our knowledge, there is no established infrastructure to process applications of study proposals utilizing these official data. Development of an application process for project-specific access to official prospectively collected European soccer league data, similar to those used in the National Football League, Major League Baseball, and the National Basketball Association, would encourage further high-quality and objective investigations aimed at optimizing orthopaedic care of high-level athletes.
Conclusion
Most players sustaining an LE fracture returned to elite soccer at the same league level after a significant loss of playing time, with a 4% rate of refracture. Player retention was higher for those sustaining LE fracture when compared with uninjured controls. Overall, injured players did not experience a decline in performance following recovery from an LE fracture.
Footnotes
Final revision submitted January 31, 2021; accepted February 28, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: M.R.C. has received hospitality payments from Medical Device Business Services. K.C.P. has received grant support from Arthrex and Acumed and educational support from Smith & Nephew. B.F. has received research support from Arthrex, Stryker, and Smith & Nephew; consulting fees from Stryker; education payments from Medwest; and personal fees from Elsevier; and has stock/stock options in Jace Medical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1.Boden BP, Lohnes JH, Nunley JA, Garrett WE, Jr. Tibia and fibula fractures in soccer players. Knee Surg Sports Traumatol Arthrosc. 1999;7(4):262–266. [DOI] [PubMed] [Google Scholar]
- 2.Chang WR, Kapasi Z, Daisley S, Leach WJ. Tibial shaft fractures in football players. J Orthop Surg Res. 2007;2:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chomiak J, Junge A, Peterson L, Dvorak J. Severe injuries in football players. Influencing factors. Am J Sports Med. 2000;28(5_suppl):S58–S68. [DOI] [PubMed] [Google Scholar]
- 4.Ekstrand J, Hägglund M, Waldén M. Injury incidence and injury patterns in professional football: the UEFA injury study. Br J Sports Med. 2011;45(7):553–558. [DOI] [PubMed] [Google Scholar]
- 5.Ekstrand J, Hägglund M, Waldén M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med. 2011;39(6):1226–1232. [DOI] [PubMed] [Google Scholar]
- 6.Ekstrand J, Krutsch W, Spreco A, et al. Time before return to play for the most common injuries in professional football: a 16-year follow-up of the UEFA Elite Club Injury Study. Br J Sports Med. 2020;54(7):421–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ekstrand J, Torstveit MK. Stress fractures in elite male football players. Scand J Med Sci Sports. 2012;22(3):341–346. [DOI] [PubMed] [Google Scholar]
- 8.Fankhauser F, Seibert FJ, Boldin C, Schatz B, Lamm B. The unreamed intramedullary tibial nail in tibial shaft fractures of soccer players: a prospective study. Knee Surg Sports Traumatol Arthrosc. 2004;12(3):254–258. [DOI] [PubMed] [Google Scholar]
- 9.Fédération Internationale de Football Association. FIFA Big Count 2006: 270 million people active in football. Accessed March 28, 2020. https://www.fifa.com/mm/document/fifafacts/bcoffsurv/bigcount.statspackage_7024.pdf
- 10.Gajhede-Knudsen M, Ekstrand J, Magnusson H, Maffulli N. Recurrence of Achilles tendon injuries in elite male football players is more common after early return to play: an 11-year follow-up of the UEFA Champions League injury study. Br J Sports Med. 2013;47(12):763–768. [DOI] [PubMed] [Google Scholar]
- 11.Gerhardt MN, Villarinho EA, Rockenbach MIB, et al. Radiographic changes of trabecular bone density after loading of implant-supported complete dentures: a 3-year prospective study. Clin Implant Dent Relat Res. 2019;21(5):1041–1047. [DOI] [PubMed] [Google Scholar]
- 12.Grassi A, Rossi G, D’Hooghe P, et al. Eighty-two per cent of male professional football (soccer) players return to play at the previous level two seasons after Achilles tendon rupture treated with surgical repair. Br J Sports Med. 2020;54(8):480–486. [DOI] [PubMed] [Google Scholar]
- 13.Kalen A, Rey E, de Rellan-Guerra AS, Lago-Penas C. Are soccer players older now than before? Aging trends and market value in the last three decades of the UEFA Champions League. Front Psychol. 2019;10:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khan M, Madden K, Burrus MT, et al. Epidemiology and impact on performance of lower extremity stress injuries in professional basketball players. Sports Health. 2018;10(2):169–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.King G, Lucas C, Nielsen RA. The balance-sample size frontier in matching methods for causal inference. Am J Pol Sci. 2017;61(2):473–489. [Google Scholar]
- 16.King G, Nielsen R. Why propensity scores should not be used for matching. Polit Anal. 2018;27(4):435–454. [Google Scholar]
- 17.King G, Zeng L. The dangers of extreme counterfactuals. Polit Anal. 2017;14(2):131–159. [Google Scholar]
- 18.Larsson D, Ekstrand J, Karlsson MK. Fracture epidemiology in male elite football players from 2001 to 2013: “How long will this fracture keep me out?” Br J Sports Med. 2016;50(12):759–763. [DOI] [PubMed] [Google Scholar]
- 19.Larsson S. Treatment of osteoporotic fractures. Scand J Surg. 2002;91(2):140–146. [DOI] [PubMed] [Google Scholar]
- 20.LeBrun DG, Tran T, Wypij D, Kocher MS. How often do orthopaedic matched case-control studies use matched methods? A review of methodological quality. Clin Orthop Relat Res. 2019;477(3):655–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lundblad M, Hägglund M, Thomeé C, et al. Medial collateral ligament injuries of the knee in male professional football players: a prospective three-season study of 130 cases from the UEFA Elite Club Injury Study. Knee Surg Sports Traumatol Arthrosc. 2019;27(11):3692–3698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mallee WH, Weel H, van Dijk CN, et al. Surgical versus conservative treatment for high-risk stress fractures of the lower leg (anterior tibial cortex, navicular and fifth metatarsal base): a systematic review. Br J Sports Med. 2015;49(6):370–376. [DOI] [PubMed] [Google Scholar]
- 23.Murphy DF, Connolly DA, Beynnon BD. Risk factors for lower extremity injury: a review of the literature. Br J Sports Med. 2003;37(1):13–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nilsson M, Hägglund M, Ekstrand J, Waldén M. Head and neck injuries in professional soccer. Clin J Sport Med. 2013;23(4):255–260. [DOI] [PubMed] [Google Scholar]
- 25.Okoroha KR, Fidai MS, Tramer JS, et al. Length of time between anterior cruciate ligament reconstruction and return to sport does not predict need for revision surgery in National Football League players. Arthroscopy. 2019;35(1):158–162. [DOI] [PubMed] [Google Scholar]
- 26.Okoroha KR, Kadri O, Keller RA, et al. Return to play after revision anterior cruciate ligament reconstruction in National Football League players. Orthop J Sports Med. 2017;5(4):2325967117698788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Okoroha KR, Taylor KA, Marshall NE, et al. Return to play after shoulder instability in National Football League athletes. J Shoulder Elbow Surg. 2018;27(1):17–22. [DOI] [PubMed] [Google Scholar]
- 28.Robertson GA, Wood AM. Fractures in sport: optimising their management and outcome. World J Orthop. 2015;6(11):850–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Robertson GA, Wood AM. Return to sport after tibial shaft fractures: a systematic review. Sports Health. 2016;8(4):324–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Robertson GA, Wood AM, Bakker-Dyos J, et al. The epidemiology, morbidity, and outcome of soccer-related fractures in a standard population. Am J Sports Med. 2012;40(8):1851–1857. [DOI] [PubMed] [Google Scholar]
- 31.Schiffner E, Latz D, Grassmann JP, et al. Fractures in German elite male soccer players. J Sports Med Phys Fitness. 2019;59(1):110–115. [DOI] [PubMed] [Google Scholar]
- 32.Serner A, Weir A, Tol JL, et al. Characteristics of acute groin injuries in the adductor muscles: a detailed MRI study in athletes. Scand J Med Sci Sports. 2018;28(2):667–676. [DOI] [PubMed] [Google Scholar]
- 33.Singh SK, Larkin KE, Kadakia AR, Hsu WK. Risk factors for reoperation and performance-based outcomes after operative fixation of foot fractures in the professional athlete: a cross-sport analysis. Sports Health. 2018;10(1):70–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Slauterbeck JR, Shapiro MS, Liu S, Finerman GA. Traumatic fibular shaft fractures in athletes. Am J Sports Med. 1995;23(6):751–754. [DOI] [PubMed] [Google Scholar]
- 35.Trofa DP, Noback PC, Caldwell JE, et al. Professional soccer players’ return to play and performance after operative repair of Achilles tendon rupture. Orthop J Sports Med. 2018;6(11):2325967118810772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vanlommel L, Vanlommel J, Bollars P, et al. Incidence and risk factors of lower leg fractures in Belgian soccer players. Injury. 2013;44(12):1847–1850. [DOI] [PubMed] [Google Scholar]
- 37.Waldén M, Hägglund M, Bengtsson H, Ekstrand J. Perspectives in football medicine. Unfallchirurg. 2018;121(6):470–474. [DOI] [PubMed] [Google Scholar]
- 38.Waldén M, Hägglund M, Magnusson H, Ekstrand J. ACL injuries in men’s professional football: a 15-year prospective study on time trends and return-to-play rates reveals only 65% of players still play at the top level 3 years after ACL rupture. Br J Sports Med. 2016;50(12):744–750. [DOI] [PubMed] [Google Scholar]
- 39.Werner J, Hägglund M, Ekstrand J, Waldén M. Hip and groin time-loss injuries decreased slightly but injury burden remained constant in men’s professional football: the 15-year prospective UEFA Elite Club Injury Study. Br J Sports Med. 2019;53(9):539–546. [DOI] [PubMed] [Google Scholar]