Abstract
Background: Total knee arthroplasty (TKA) demonstrates excellent durability using jig-based manual techniques (manual TKA [mTKA]), but significant rates of dissatisfaction remain. Modifications of mTKA techniques and TKA implant designs to improve outcomes have had minimal success. Studies comparing relative outcomes of mTKA and robotic-assisted TKA (raTKA) are limited. Purpose: This study sought to compare outcomes of mTKA and raTKA in patients at a single institution. Methods: We retrospectively reviewed all primary TKAs performed by 1 surgeon from 2015 to 2017. In all, 139 consecutive mTKAs (2015–2016) and 148 consecutive raTKAs (2016–2017) were included. No cases were excluded. Patient demographics, complications, readmission rates, and clinical and patient-reported outcomes were compared at a minimum of 1-year follow-up. A post hoc student t test and Pearson χ2 test were used for continuous and categorical data. Results: We found that mTKA patients compared with raTKA patients required significantly longer length of stay (LOS) (1.73 vs 1.18 days, respectively), greater morphine milligram equivalents consumption (89.6 vs 65.2, respectively), and increased physical therapy (PT) visits (13.0 vs 11.0, respectively) with increased 30-day readmission rates (4.3 vs 0.7%, respectively) that approached significance. Knee Injury and Osteoarthritis Outcome Score for Joint Replacement and the University of California at Los Angeles activity score did not differ significantly comparing raTKA with mTKA patients at 1 year. There were no differences in complication rates. Conclusion: Significant early clinical benefits were noted with raTKA, including lower opioid requirements, shorter LOS, and fewer PT visits when compared with mTKA. A reduction in 30-day readmission rates was noted with raTKA that was not significant. Excellent clinical results with similar patient-reported outcomes were noted in both groups at 1-year follow-up. Further prospective investigations at longer follow-up intervals comparing these techniques are warranted.
Keywords: robotics, navigation, knee arthroplasty, outcomes, Mako
Introduction
Total knee arthroplasty (TKA) has demonstrated excellent durability using traditional jig-based manual implantation techniques (manual TKA [mTKA]) with a variety of implant designs at intermediate-term and long-term follow-up intervals [3]. Low rates of revision after primary TKA have been consistently noted in large retrospective case series and based on international registry data [17]. Despite outstanding durability with primary TKA, 10% to 20% of patients remain dissatisfied with the outcome of the procedure even in the absence of complications [1,5,9].
Modification of surgical technique and implant design to address patient dissatisfaction and improve functional outcomes after traditional manual jig-based primary TKA has met with limited success. These efforts have included minimally invasive surgery, patient-specific instrumentation, custom implants, and gender-specific implants. No significant consistent functional advantage has been demonstrated based on bearing surface (cruciate retaining [CR], cruciate substituting, fixed bearing, or mobile-bearing designs), component design (single radius, J curve, medial pivot), or alignment rationale (kinematic or mechanical) [7,18,21,22]. Computer navigation alone has improved TKA coronal alignment and durability compared with non-navigated techniques [10] but has not consistently demonstrated improved patient satisfaction. Sensor-guided surgery has provided quantitative intraoperative data regarding intra-articular compartment pressures and knee kinematics, but data regarding improved patient satisfaction at long-term intervals are limited [4].
Robotic-assisted techniques that adopt enhanced preoperative planning using a computed tomography (CT)-based platform, quantitative intraoperative deformity assessment, and haptically guided robotic bone preparation have been introduced. This approach has demonstrated improved durability when comparing robotic-assisted unicompartmental knee arthroplasty (raUKA) with manual UKA techniques [14], reduced rates of complication and improved functional outcome when comparing robotic-assisted with manual total hip arthroplasty at minimum 2-year interval [8], and improved rate of recovery and functional outcomes when comparing robotic-assisted TKA (raTKA) with mTKA techniques at short-term follow-up interval [11,16]. These promising early results with raTKA suggested analysis at long-term intervals is warranted. The purpose of our study was to compare mTKA and raTKA functional outcomes and complication rates at a minimum 1-year follow-up interval.
Materials and Methods
Institutional review board approval (IRB) was obtained, and a retrospective review of our departmental database was performed to identify all raTKA or mTKA procedures performed at our institution by 1 fellowship-trained surgeon using a cemented CR design (Triathlon; Stryker, Mahwah, New Jersey) from April 2015 to September 2017. No patients were excluded. Informed consent was not obtained as this was a retrospective, minimum risk study. A consecutive series of 139 mTKAs (132 patients) and 148 raTKAs (140 patients) were identified during this period. All TKAs performed prior to October 2016 were performed with jig-based mTKA technique. The raTKA platform was introduced at our institution in October 2016, and all TKAs performed after this date were performed with the raTKA technique. No other changes occurred during the study period regarding patient selection, preoperative assessment, surgical technique, anesthetic technique, intraoperative periarticular injection protocols, implant system, or postoperative therapy protocols. Demographics including age, sex, body mass index (BMI), preoperative diagnosis, laterality, medical comorbidities, and smoking history were recorded for both cohorts. Data used for this study are stored in a manner that is Health Insurance Portability and Accountability Act–compliant and IRB-approved.
Assessments included tourniquet time, intraoperative and postoperative complications, 30- and 90-day readmission rates, and discharge disposition (home vs skilled nursing facility or acute rehabilitation). Discharge criteria remained the same throughout the study period and included clinician and physical therapist (PT) assessments so that the patient was safe to be discharged home or to a skilled nursing facility. The time from admission to discharge was retrieved from the electronic medical record. All patients were prescribed postoperative physical therapy according to a standardized rehabilitation protocol that did not change during the study interval. The total number of PT visits was recorded for each group. All patients (in the absence of complication) were seen postoperatively at 2-week, 6-week, and 1-year intervals. Outcomes compared after a minimum of 1-year follow-up included rates of revision, surgical site infection (SSI), and manipulation under anesthesia.
Patient-reported outcome measures (PROMs) were recorded preoperatively and at 1-year follow-up visits. Patient-reported outcome measures included the Short Form 12 mental component (SF-12 MCS) and Short Form 12 physical component scores (SF-12 PCS), Veterans RAND 12 physical component (VR-12 PCS) and mental component scores (VR-12 MCS), the Knee Injury and Osteoarthritis Outcome Score for Joint Replacement (KOOS-JR), and the University of California at Los Angeles (UCLA) Activity Score. Comparison analyses were performed by a departmental statistician using the post hoc student t test for comparing PROMs between groups and the Pearson χ2 test for categorical variables.
Inpatient postoperative opioid use was compared between groups. The medication administration record (MAR) was used to capture opioid use from arrival to the general care floor through discharge. Medications included tramadol, hydrocodone-acetaminophen, oxycodone, oral and intravenous hydromorphone, and oral and intravenous morphine. These doses were converted to morphine milligram equivalents (MME) as defined by both the Centers for Medicare and Medicaid Services and the Centers for Disease Control and Prevention [19].
All TKAs were performed by the senior author using a medial parapatellar approach and the CR Triathlon system (Stryker). The decision to resurface the patella was made intraoperatively in both cohorts. All patients were screened for methicillin-sensitive and methicillin-resistant Staphylococcus aureus preoperatively to guide perioperative antibiotic therapy. Both groups received regional anesthesia (98% mTKA and 99% raTKA cases) consisting of a single-shot spinal injection in conjunction with an adductor canal block unless regional anesthesia was contraindicated. A proximal thigh tourniquet was inflated in all cases until wound closure. Prior to closure, a periarticular injection was performed with 0.25% Marcaine, 30 mg of Toradol, and 1.5 g of cefuroxime (total volume of 60 mL).
Manual TKAs were performed using the measured resection technique and a goal of neutral mechanical alignment with symmetric balance in extension and flexion. Preoperative imaging included plain radiographs of the knee (standing anteroposterior, lateral, Rosenberg, and sunrise patellofemoral views). Standard Triathlon manual instrument sets were used with conventional extramedullary tibial and intramedullary femoral cutting guides. Trial femoral and tibial components were used in all cases, and soft tissue releases were performed as needed to achieve deformity correction and optimize balance. All components were fixed with cement. Patella resurfacing was not performed unless significant patellar arthritis or maltracking was noted.
Beginning in October 2016, the senior author exclusively used raTKA using the Mako Robotic Arm–Assisted Surgery platform (Stryker) for all TKAs. Computed tomographic scans were performed according to the manufacturer’s specifications and used supported preoperative planning software. Intraoperative registration of the femur and tibia was completed in all cases. Pose captures were then obtained in extension and flexion with passive deformity correction to determine the estimated gaps in these positions prior to bone resections. Modifications were then made to component position, and soft tissue releases were performed as needed to achieve target alignment and symmetric gaps of appropriate size in flexion and extension. The target coronal alignment for all cases was within 3° of mechanical neutral position. Tibial slope was set at 3° posterior slope according to manufacturers’ recommendations for the Triathlon CR design. Tibial and femoral bone preparation was completed using the Stryker Mako Robotic–assisted technique. Trial components were placed after bone preparation, and all knees were assessed to determine that the target alignment, balance, and knee kinematics had been achieved. Additional adjustments were made as needed to implant position, and soft tissue releases were performed, if required, to achieve the surgical goals prior to final component implantation. All components were cemented. Patella resurfacing was not performed unless significant patella arthritis or maltracking was noted.
Statistical Analysis
Comparison analyses were performed by a departmental statistician using the post hoc Student t test for comparing PROMs between groups and the Pearson χ2 test for categorical variables. Significance was defined as P < .05.
Results
There were no significant differences noted in patient characteristics between mTKA and raTKA groups (Table 1). Two intraoperative tibia fractures occurred within the manual group, and none were noted in the raTKA group (P = .17). Two deep SSIs requiring reoperation with irrigation, debridement, and implant retention occurred in the mTKA cohort compared with none in the raTKA group (P = .17). Mean tourniquet time was significantly longer in the raTKA group compared with mTKA (96.8 vs 91.6, P < .001; Figure 1). There were no statistically significant differences in mean tourniquet time of the last 20 raTKA compared with the mTKA cohort (93.8 vs 91.6, P = .505) (Fig. 1).
Table 1.
Patient Demographics.
| Manual techniques (139) | Robotic-assisted total knee arthroplasty (148) | P value | |
|---|---|---|---|
| Age | 66.1 (8.0a) | 65.9 (8.2a) | .913 |
| Body mass index | 31.5 (5.0a) | 30.6 (5.3a) | .149 |
| Sex, male | 63 (45.3%) | 72 (48.6%) | .656 |
| Side, right | 68 (48.9%) | 83 (56.1%) | .273 |
| Depression | 24 (17.3%) | 24 (16.2%) | .936 |
| Diabetes | 17 (12.2%) | 22 (14.8%) | .632 |
| Hypertension | 78 (56.1%) | 80 (54.1%) | .816 |
| Obstructive sleep apnea | 35 (25.2%) | 31 (20.9%) | .477 |
| Chronic kidney disease | 8 (5.8%) | 13 (8.8%) | .449 |
| Hypothyroidism | 19 (13.7%) | 20 (13.5%) | .999 |
| Coronary artery disease | 14 (10.1%) | 23 (15.5%) | .228 |
| Ever smoked | 51 (36.7%) | 52 (35.1%) | .880 |
Reported as standard deviation.
Fig. 1.
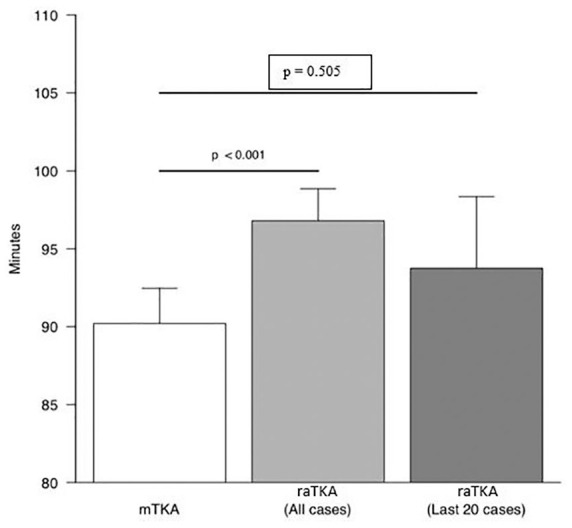
Tourniquet time was significantly longer within the raTKA cohort versus manual when anticipated learning curve was not accounted for (96.8 vs 91.6, respectively; P < .001). This difference was not observed when comparing times of the last 20 raTKA cases with mTKA (93.8 vs 91.6 p = 0.505). mTKA manual total knee arthroplasty; raTKA robotic-assisted total knee arthroplasty .
There were no statistically significant differences noted comparing raTKA and mTKA revision rates (0% vs 0.63%, respectively; P = .484), manipulation rates (0.7% vs 2.9%, respectively; P = .202), rates of patellar resurfacing (22% vs 25.9%, respectively; P = .91), or rates of home discharge (90.5% vs 91.4%, respectively; P = .970) (Figs 2 and 3). Longer length of stay (LOS) was noted comparing mTKA with raTKA (1.73 vs 1.18 days, respectively; P < .001). A reduction in raTKA compared with mTKA 30-day readmission rate did not reach significance (0.7% vs 4.3%, P = .060). Fewer PT visits were required postoperatively for the raTKA group compared with the mTKA group (11.0 vs 13.3, respective;, P < .004) (Fig. 4); 30-day readmissions occurred within the manual group due to elevated international normalized ratio, deep venous thrombosis, pulmonary embolism, acute congestive heart failure, and renal failure. The only raTKA readmission was following a vasovagal episode 3 days postoperatively. No pin site wound complications or postoperative pin site–related fractures were noted. The 90-day readmission rates between the mTKA and raTKA groups were statistically indistinct (7.9 and 8.8%, respectively) (Fig. 2).
Fig. 2.
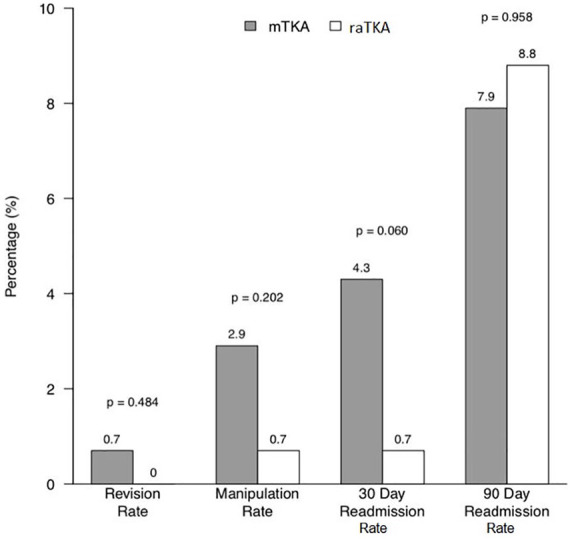
Comparison of revision rates, manipulation rates, and 30- and 90-day readmission between cohorts. mTKA manual total knee arthroplasty; raTKA robotic-assisted total knee arthroplasty.
Fig. 3.
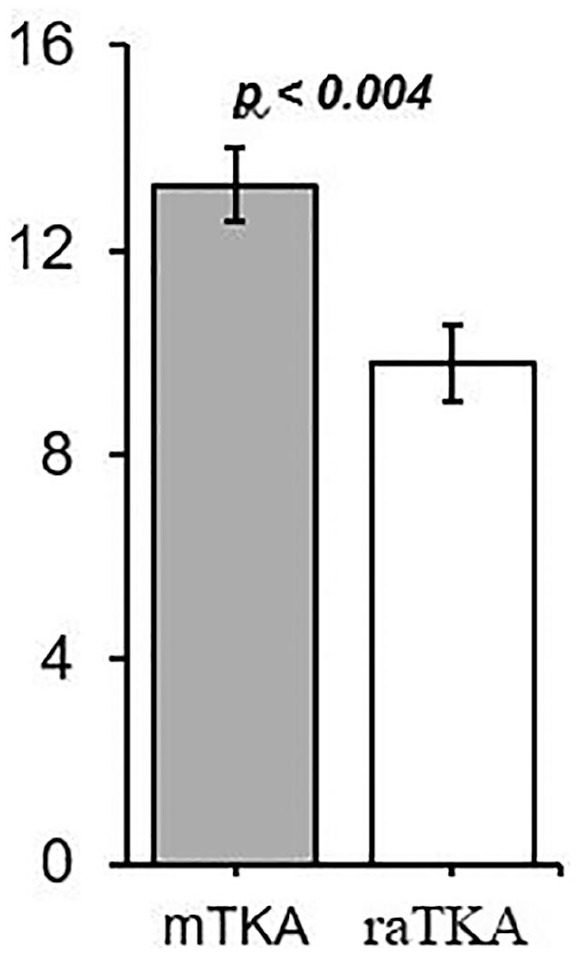
Comparison of the average number of postoperative physical therapy appointments between cohorts following hospital discharge (11.0 vs 13.3, P < .004). mTKA manual total knee arthroplasty; raTKA robotic-assisted total knee arthroplasty.
Fig. 4.
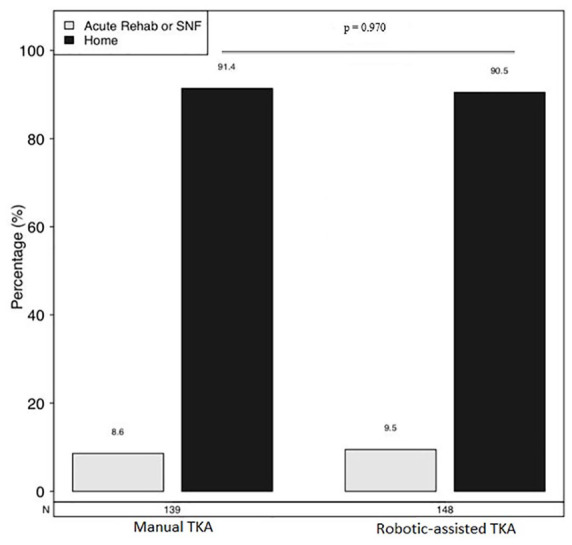
Comparison of the percentage of patients discharged to home versus acute rehabilitation or skilled nursing facility following mTKA and raTKA (91.4% vs 90.5%, P = .970). mTKA manual total knee arthroplasty; raTKA robotic-assisted total knee arthroplasty.
Postoperative PROM data were available in 79% SF-12/VR-12, 74.2% UCLA, and 66.2% KOOS-JR. The overall survey response rate for preoperative PROMs was 25.2% in the manual group compared with 73.6% in the robotic group (P < .001), whereas the response rate for postoperative PROMs was 73.6% in the manual group compared with 81.8% in the robotic group (P = .095). No differences in preoperative SF-12 or VR-12 scores were noted between groups (combined MCS, P = .360; combined PCS, P = .998) (Table 2). There were no differences in mean preoperative UCLA activity scores between groups (P = .735) (Table 2). No statistically significant differences were noted comparing mTKA and raTKA postoperative UCLA activity and KOOS-JR scores at 1 year (5.6 vs 6.12, respectively; P = .059 and 72.2 vs 75.7, respectively; P = .072) (Table 2). No differences were noted comparing mTKA and raTKA postoperative scores in VR-12 MCS (55.9 vs 55.4, P = .668) and VR-12 PCS (42.9 vs 41.6, P = .336) (Table 2).
Table 2.
PROMs Reported Preoperatively and at 1 Year Postoperatively.
| N | Manual total knee arthroplasty | N | Robotic-assisted total knee arthroplasty | P value | |
|---|---|---|---|---|---|
| Preoperative PROMs | |||||
| SF-12 MCS | 18 | 52.5 (10.9) | 17 | 55.4 (7.8) | .361 |
| SF-12 PCS | 18 | 32.4 (10.1) | 17 | 42.3 (10.3) | .007 |
| VR-12 MCS | 0 | N/A | 105 | 55.0 (10.4) | |
| VR-12 PCS | 0 | N/A | 105 | 31.8 (9.3) | |
| Combined MCSa | 18 | 52.5 (10.9) | 109 | 55.0 (10.2) | .360 |
| Combined PCSa | 18 | 32.4 (10.1) | 109 | 32.4 (9.7) | .998 |
| KOOS-JR | 0 | N/A | 72 | 52.90 (13.2) | |
| UCLA | 17 | 5.5 (2.2) | 98 | 5.34 (2.0) | .735 |
| Overall response rate | 35 | 25.2% | 109 | 73.6% | <.001 |
| Postoperative PROMs at 1-year follow-up | |||||
| VR-12 MCS | 104 | 55.4 (9.2) | 121 | 55.9 (9.0) | .668 |
| VR-12 PCS | 105 | 41.6 (10.6) | 121 | 42.9 (9.7) | .336 |
| KOOS, JR | 88 | 72.2 (13.7) | 102 | 75.767 (12.5) | .072 |
| UCLA | 102 | 5.6 (2.3) | 111 | 6.12 (1.7) | .059 |
| Overall response rate | 107 | 73.6% | 121 | 81.8% | .095 |
PROMs patient-reported outcome measures, SF-12 MCS/PCS Short-Form 12 Health Survey–Mental Component/Physical Component Scores, VR-12 MCS/PCS Veterans RAND 12-Item Health Survey–Mental Component/Physical Component Scores, KOOS-JR, Knee Injury and Osteoarthritis Outcome Score for Joint Replacement; UCLA University of California at Los Angeles Activity Score.
MCS and PCS are combined from corresponding VR-12 and SF-12 components. If VR-12 data are missing but SF-12 data are present, then SF-12 data are used to impute the missing data; otherwise, VR-12 data take precedence. No patients had SF-12 data at postoperative PROM time point.
Postoperative inpatient opioid consumption was significantly lower in the raTKA group compared with the mTKA group (65.2 MME vs 89.6 MME, respectively; P = .02).
Discussion
The purpose of this study was to compare directly clinical outcomes and complication rates of mTKA and raTKA at a minimum 1-year follow-up interval. Our study demonstrated significant early clinical benefits with reduced LOS, lower opioid requirements, and fewer PT visits in raTKA patients compared with mTKA patients. A reduction in 30-day readmission rates was noted with raTKA that did not reach significance. At 1-year follow-up, there were no significant differences in complication rates or postoperative PROMs between groups.
Our study has several limitations. We had incomplete preoperative and postoperative PROM data (Table 2). Further study is needed with more complete PROM data capture to determine whether the patterns noted in our study will be supported or refuted. We also included a limited set of PROMs for analysis. Further study using a wider variety of PROMs would be beneficial to determine whether any clinical differences exist comparing raTKA and mTKA that were not identified in this study. Our study is a retrospective review of sequential cases performed by 1 fellowship-trained surgeon at a single institution, using 1 CR TKA design with selective patellar resurfacing and cemented technique. Patients were not blinded to the use of robotics, and it is possible that this introduced bias regarding patients’ perceived superiority of robotic-assisted technique. The senior surgeon also had significant previous robotic experience of over 10 years with partial knee replacement and total hip platforms and has a detailed understanding of the raTKA software used for this application; this expertise may have affected outcomes of robotic-assisted TKAs in this study. Further study is needed to determine whether similar findings will be noted in other centers with surgeons lacking the same degree of previous robotic experience. Prospective, randomized, multicenter studies in larger patient cohorts at longer follow-up intervals are warranted to confirm these promising early findings.
Traditional jig-based mTKA has a well-established record of restoring function and reducing pain in 80%–90% of patients with end-stage knee arthritis [2]. Previous efforts to improve patient satisfaction with modified surgical technique, navigation, and altered implant design have been met with limited or unproven benefit [7,18,21,22]. Robotic-assisted technique was introduced to improve accuracy, reproducibility, and patient outcomes following joint replacement. Previous studies have demonstrated that such robotic techniques have benefit compared with traditional manual technique regarding reduced rates of revision with raUKA at 5 years [14], reduced rates of dislocation and improved PROM at 2 years with raTHA [8], and improved short-term outcomes (3–6 months) comparing raTKA with mTKA [11,16]. Kayani et al found superior early clinical results with raTKA compared with mTKA during the initial hospitalization [11]. Although this study included only 40 patients in each cohort, findings included reduced levels of postoperative analgesic requirements, decreased blood loss, shorter time to straight leg raise, and improved knee flexion with raTKA. Marchand et al compared results of raTKA with mTKA at 6-month follow-up interval, demonstrating improvements in pain, function, and overall satisfaction [16]. Our study similarly demonstrated statistically significant and clinically relevant early benefits with raTKA compared with mTKA technique, but no differences in complication rates or PROMs (UCLA and KOOS-JR) at 1-year follow-up. Similar findings were noted by Liow regarding PROMs using a different robotic platform (ROBODOC) and a different TKA implant (Zimmer NexGen PS) with no significant differences in joint-specific PROMs or patient satisfaction comparing raTKA with mTKA at 2-year follow-up [15]. Opportunities exist to better define the preoperative patient clinical phenotype and the intraoperative quantified limb deformity and soft tissue laxity to better inform optimal patient-specific targeting. Further studies are needed to determine whether such patient-specific raTKA targeting efforts will improve clinical outcomes compared with mTKA at long-term follow-up intervals.
The observed reduction in pain associated with the raTKA technique in our study may be due to multiple factors including improved soft tissue protection provided by robotic haptics [6,12,13] and reduced need for soft tissue releases associated with the raTKA technique. The raTKA “pre-resection balancing workflow” involves surgeon-generated pose captures that determine what degree of passive correction of limb deformity is possible, and then modifications of component positions are made within acceptable limits prior to bone resections to achieve optimal balancing. This pre-resection balancing raTKA workflow frequently avoids the need for significant soft tissue releases; mTKA using traditional measured resection techniques generally involves attempting to prepare the femur and tibia with neutral mechanical alignment and then performing soft tissue releases to balance the knee. The reduced soft tissue damage associated with robotic haptic bone preparation and modified surgical technique involving pre-resection balancing in appropriate patients may account for the observed improvement in narcotic requirements, shorter LOS, and reduced need for PT visits. The differences noted in manipulation rates comparing raTKA and mTKA (0.7% vs 2.9%, respectively) (Fig. 2) were not statistically significant, but further study in larger patient cohorts is warranted.
There was a demonstrated learning curve for adoption of the raTKA technique. After the initial learning curve period, mTKA and raTKA procedures were time-neutral (Fig. 1). Similar learning curves have been noted with the raTKA technique in other studies [20]. Despite differences in operative times during the learning curve, no difference in complication rates or SSIs was noted in our study.
In conclusion, this retrospective single-surgeon series demonstrated early postoperative clinical benefits associated with the raTKA technique, with lower opioid requirements, shorter LOS, and fewer postoperative PT sessions compared with mTKA. No differences in complication rates or PROMs were noted comparing raTKA and mTKA techniques at minimum 1-year follow-up. These data suggest further study is needed to determine whether the raTKA technique can be further refined with patient-specific targeting to achieve significant improvements in PROMs that exceed minimal clinically important difference thresholds compared with conventional mTKA techniques at long-term follow-up intervals. Further multicenter prospective investigations comparing these techniques are warranted.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: R.I. reports relationships with Stryker, the manufacturer of the robotics platform and implant used in this study; Orthosensor; and the American Academy of Orthopaedic Surgeons American Joint Replacement Registry. The other authors declare no potential conflicts of interest.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Human/Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent: Informed consent was waived from all patients included in this retrospective study.
Level of Evidence: Level III: Retrospective Therapeutic Study
Required Author Forms: Disclosure forms provided by the authors are available with the online version of this article as supplemental material.
References
- 1.Bullens PH, van Loon CJ, de Waal Malefijt MC, Laan RF, Veth RP: Patient satisfaction after total knee arthroplasty: a comparison between subjective and objective outcome assessments. J Arthroplasty. 2001;16(6):740–747. 10.1054/arth.2001.23922. [DOI] [PubMed] [Google Scholar]
- 2.Carr AJ, Robertsson O, Graves S, et al. : Knee replacement. Lancet. April72012;379(9823):1331–1340. 10.1016/s0140-6736(11)60752-6. [DOI] [PubMed] [Google Scholar]
- 3.Civinini R, Carulli C, Matassi F, Lepri AC, Sirleo L, Innocenti M: The survival of total knee arthroplasty: current data from registries on tribology: review article. HSS Journal. 2017;13(1):28–31. 10.1007/s11420-016-9513-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Delanois RE, Mistry JB, Chughtai M, et al. : Novel sensor tibial inserts in total knee arthroplasty: a review. Surg Technol Int. 2016;29:255–260. [PubMed] [Google Scholar]
- 5.Gunaratne R, Pratt DN, Banda J, Fick DP, Khan RJK, Robertson BW: Patient dissatisfaction following total knee arthroplasty: a systematic review of the literature. J Arthroplasty. 2017;32(12):3854–3860. 10.101/j.arth.2017.07.021. [DOI] [PubMed] [Google Scholar]
- 6.Hampp EL, Chughtai M, Scholl LY, et al. : Robotic-arm assisted total knee arthroplasty demonstrated greater accuracy and precision to plan compared with manual techniques. J Knee Surg. 2019;32(3):239–250. 10.1055/s-0038-1641729. [DOI] [PubMed] [Google Scholar]
- 7.Howell SM, Shelton TJ, Hull ML: Implant survival and function ten years after kinematically aligned total knee arthroplasty. J Arthroplasty. 2018;33(12):3678–3684. 10.1016/j.arth.2018.07.020. [DOI] [PubMed] [Google Scholar]
- 8.Illgen RL, Bukowski BR, Abiola R, et al. : Robotic-assisted total hip arthroplasty: outcomes at minimum two-year follow-up. Surg Technol Int. 2017;30:365–372. [PubMed] [Google Scholar]
- 9.Jacobs CA, Christensen CP, Karthikeyan T: Patient and intraoperative factors influencing satisfaction two to five years after primary total knee arthroplasty. J Arthroplasty. 2014;29(8):1576–1579. 10.1016/j.arth.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 10.Jones CW, Jerabek SA: Current role of computer navigation in total knee arthroplasty. J Arthroplasty. 2018;33(7):1989–1993. 10.1016/j.arth.2018.01.027. [DOI] [PubMed] [Google Scholar]
- 11.Kayani B, Konan S, Tahmassebi J, Pietrzak JRT, Haddad FS: Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: a prospective cohort study. Bone Joint J. 2018;100-b(7):930–937. 10.1302/0301-620x.100b7.bjj-2017-1449.r1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khlopas A, Chughtai M, Hampp EL, et al. : Robotic-arm assisted total knee arthroplasty demonstrated soft tissue protection. Surg Technol Int. 2017;30:441–446. [PubMed] [Google Scholar]
- 13.Khlopas A, Sodhi N, Sultan AA, Chughtai M, Molloy RM, Mont MA: Robotic arm-assisted total knee arthroplasty. J Arthroplasty. 2018;33(7):2002–2006. 10.1016/j.arth.2018.01.060. [DOI] [PubMed] [Google Scholar]
- 14.Kleeblad LJ, Borus TA, Coon TM, Dounchis J, Nguyen JT, Pearle AD: Midterm survivorship and patient satisfaction of robotic-arm-assisted medial unicompartmental knee arthroplasty: a multicenter study. J Arthroplasty. 2018;33(6):1719–1726. 10.1016/j.arth.2018.01.036. [DOI] [PubMed] [Google Scholar]
- 15.Liow MHL, Goh GS, Wong MK, Chin PL, Tay DK, Yeo SJ: Robotic-assisted total knee arthroplasty may lead to improvement in quality-of-life measures: a 2-year follow-up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc. 2017;25(9):2942–2951. 10.1007/s00167-016-4076-3. [DOI] [PubMed] [Google Scholar]
- 16.Marchand RC, Sodhi N, Khlopas A, et al. : Patient satisfaction outcomes after robotic arm-assisted total knee arthroplasty: a short-term evaluation. J Knee Surg. 2017;30(9):849–853. 10.1055/s-0037-1607450. [DOI] [PubMed] [Google Scholar]
- 17.Registry AOANJR: Annual Report. Australian National Joint Replacement Registry; 2016. [Google Scholar]
- 18.Serna-Berna R, Lizaur-Utrilla A, Vizcaya-Moreno MF, Miralles Muñoz FA, Gonzalez-Navarro B, Lopez-Prats FA: Cruciate-retaining vs posterior-stabilized primary total arthroplasty. Clinical outcome comparison with a minimum follow-up of 10 years. J Arthroplasty. 2018;33(8):2491–2495. 10.1016/j.arth.2018.02.094. [DOI] [PubMed] [Google Scholar]
- 19.Services, Centers for Medicare and Medicaid: Opioid Oral Morphine Milligram Equivalent (MME) Conversion Factors. 2018. https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/Oral-MME-CFs-vFeb-2018.pdf [Google Scholar]
- 20.Sodhi N, Khlopas A, Piuzzi NS, et al. : The learning curve associated with robotic total knee arthroplasty. J Knee Surg. 2018;31(1):17–21. 10.1055/s-0037-1608809. [DOI] [PubMed] [Google Scholar]
- 21.Warth LC, Ishmael MK, Deckard ER, Ziemba-Davis M, Meneghini RM: Do medial pivot kinematics correlate with patient-reported outcomes after total knee arthroplasty? J Arthroplasty. 2017;32(8):2411–2416. 10.1016/j.arth.2017.03.019. [DOI] [PubMed] [Google Scholar]
- 22.Young SW, Walker ML, Bayan A, Briant-Evans T, Pavlou P, Farrington B: The Chitranjan S. Ranawat award: no difference in 2-year functional outcomes using kinematic versus mechanical alignment in TKA: a randomized controlled clinical trial. Clin Orthop Relat Res. 2017;475(1):9-20. 10.1007/s11999-016-4844-x. [DOI] [PMC free article] [PubMed] [Google Scholar]


