Abstract
Female patient, suffering from nephrolithiasis, at the age of 32 was admitted for renal colic caused by a stone obstructing UP junction with left hydronephrosis. Nephrostomy was placed, resulting in brisk diuresis. Severe metabolic acidosis with normal anion gap and urine pH of 6.5 was noted. Potassium level dropped to extremely low level (1.6 mEq/L), causing muscle paralysis and respiratory failure, necessitating mechanical ventilation. The patient was treated by potassium chloride infusion, followed by correction of severe metabolic acidosis by sodium bicarbonate. Diagnosis of distal type renal tubular acidosis type I (dRTA) was made based on normal anion gap metabolic acidosis, alkaline urine, hypokalemia, and nephrolithiasis. Five years later, the patient presented with severe hypoxia, lung opacities, and bronchiolitis obliterans organizing pneumonia which was confirmed by bronchoscopy with lung tissue biopsy. Concurrently, the patient presented with dry mouth, pruritus, skin rash with hypocomplementemia, elevated anti-DNA, anti-Ro, and anti-SmAb. Diagnosis of overlap Sjögren's/systemic lupus erythematosus disease was done and treatment by hydroxychloroquine, prednisone, and azathioprine was started. Possible presence of Sjögren's syndrome should be considered in adult patients with unexplained dRTA.
Keywords: Renal tubular acidosis type I, Sjögren's syndrome, Bronchiolitis obliterans
Introduction
Sjögren's syndrome (SS) is an autoimmune disorder with lymphocytic infiltration of secretory glands with sicca syndrome (dryness of eyes and mouth) and extra glandular involvement (renal, hepatic, neurologic, and skin). Renal involvement in Sjogren's disease includes interstitial nephritis, renal tubular acidosis (commonly distal type RTA [dRTA]), and glomerular disease, which usually appear several years after the initial presentation of SS.
dRTA is a tubular disorder with a primary defect of urinary acidification and acid excretion in the collecting duct. These patients suffer from hyperchloremic metabolic acidosis with nephrolithiasis, necessitating correction of metabolic and electrolyte defects.
RTA in adults may be associated with SS and other autoimmune diseases, on the contrary in children mutations of SCL4A1, ATP6V1B1, and ATP6VOA4 are the cause of inherited forms of RTA.
Case Presentation
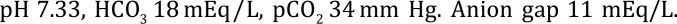
The 32-year-old patient (married with 1 child), with history of 3 spontaneous abortions, was suffering for years from nephrolithiasis, ureterolithiasis, and vesicolithiasis. The patient was admitted for renal colic caused by a stone obstructing UP junction with left hydronephrosis. Left nephrostomy was performed, causing brisk diuresis. Clinical picture was complicated by muscle paralysis, ECG changes with QT prolongation, U waves, and respiratory failure due to severe hypokalemia (potassium level dropped as low as 1.6 mEq/L). The patient required mechanical ventilation, admitted to the intensive care unit, and treated by fluids with potassium chloride infusion (9 g of potassium chloride infused during 6 h, 30 mEq/h). She was also treated orally by potassium chloride 12 tablets per day. After improvement of potassium level, sodium bicarbonate was given for correction of severe metabolic acidosis. Hypocalcemia and hypophosphatemia were treated appropriately. Diagnosis of dRTA made based on normal anion gap metabolic acidosis, alkaline urine, hypokalemia, and nephrolithiasis.
Blood Tests on Admission
Blood test on admission showed urea 20 mg/dL, creatinine 1.04 mg/dL, chloride 114 mEq/L, sodium 140 mEq/L, K 1.6 mEq/L, calcium 5.7 mg/dL, phosphate 2.2 mg/dL, pH 7.26, PCO2 18, and HCO3 8.1.
Medical Prescription
- The following is the medical prescription:
- Tablets of potassium chloride 2,400 mg 4 times a day (QID).
- Tablets of sodium bicarbonate 2 g 4 times a day (QID).
- Tablets of dibasic sodium phosphate/monobasic potassium phosphate 285 mg/602 mg 4 tablets 4 times a day (QID).
- Tablets of potassium citrate twice a day (BID).
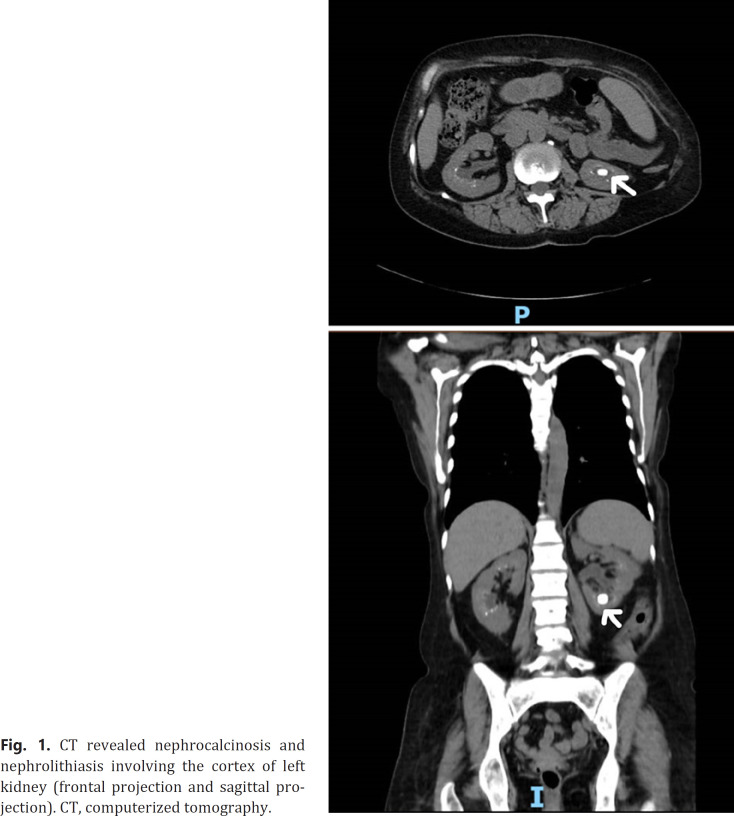
Repetitive computerized tomography (CT) and ultrasound examination revealed big stone (1.7 cm) and nephrocalcinosis involving the cortex of left kidney (shown in Fig. 1). Five years later, the patient complained of dryness of mouth and eyes and skin rash.
Fig. 1.
CT revealed nephrocalcinosis and nephrolithiasis involving the cortex of left kidney (frontal projection and sagittal projection). CT, computerized tomography.
On physical examination, salivary glands were normal. Laboratories disclosed hypocomplementemia with low C3 level −33 mg% (reference value 90–180 mg%), positive antinuclear antibody, anti-Ro, anti-SM (anti-Smith Ab) and elevated anti-double-stranded DNA 133 IU/mL (reference value 0–6 IU/mL). Salivary gland biopsy was not done since our patient had the immune tests consistent with SS and due to comorbidities preventing additional interventions.
Based on clinical and laboratory data, diagnosis of overlap systemic lupus erythematosus (SLE)/Sjögren's disease was made with acidification defect due to RTA type I secondary to autoimmune disease. In addition, the patient complained of sensory disturbances of legs that were most probably attributed to nervous system involvement by vasculitis.
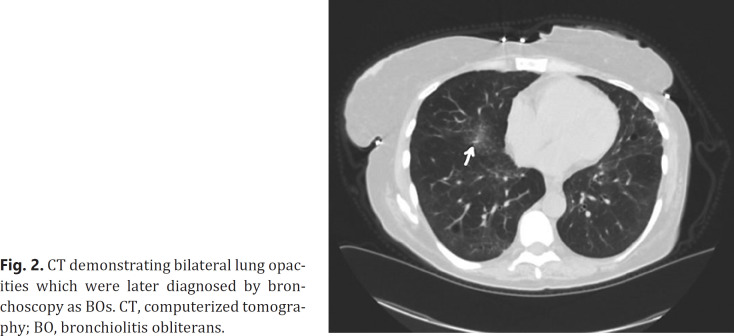
At the same time, she developed shortness of breath, severe hypoxia, necessitating 24-h oxygen supply and ground-glass opacities of lungs demonstrated by the CT scan (shown in Fig. 2). Bronchoscopy with bronchial biopsy confirmed the diagnosis of bronchiolitis obliterans (BOs).
Fig. 2.
CT demonstrating bilateral lung opacities which were later diagnosed by bronchoscopy as BOs. CT, computerized tomography; BO, bronchiolitis obliterans.
CT scan also demonstrated dilatation of distal esophagus probably due to achalasia/esophageal involvement. The patient refused gastrointestinal tract investigation.
Treatment by Prednisone and Azathioprine was started, with subsequent improvement of hypoxia. Cardiac echocardiogram (ECHO) revealed severe pulmonary hypertension of 68 mm Hg. The patient was referred to right-sided heart catheterization and treatment by Sildenafil was recommended.
Diagnosis of overlap SS/SLE syndrome with RTA type I with nephrolithiasis and lung involvement (BOs) due to SS was confirmed. Positivity of antinuclear antibody and anti-DNA and anti-Ro, anti-SM (anti-Smith Ab) suggested that our patent is suffering from secondary SS due to overlap Sjögren's disease/SLE. Overlap Sjögren's/SLE disease was treated by prednisone and azathioprine. Later azathioprine had been stopped for pancytopenia and renewed for relapse with diffuse skin rash related to SLE. Immunosuppression treatment in our patient did not improve acidification defect. Recurrent urinary tract infections, related to obstructive uropathy, were treated by antibiotics. Recurrent nephrolithiasis was treated for years by shock wave lithotripsy, ureteric stents, and percutaneous nephrolithotomy.
Investigations
The presence of severe metabolic acidosis in our patent which passed alkaline urine (PH 6.7–8.0) raised suspicion of urine acidification defect. This case urged distinction between types of RTA. Bicarbonaturia is compatible with proximal type RTA. Decrease H + ATPase pump function compromises tubular proton H+ excretion with alkaline urine is compatible with distal type RTA, which may be confirmed by low PCO2 excretion in urine. Additionally, hypocitraturia is observed, since enhanced reabsorption of citrate in proximal tubule stimulated by academia.
The bicarbonate load test was performed with infusion of IV sodium bicarbonate 150 mEq diluted in 5% dextrose solution, blood, and urine samples were taken according to the time schedule: 0′ (zero), 30, and 60 min after the infusion of bicarbonate. Bicarbonate load test was performed in order to exclude proximal type of RTA and disclosed low fractional excretion of bicarbonate, confirming the diagnosis of RTA type I (shown in Table 1).
Table 1.
Bicarbonate load test
| PH | PCO2, mm Hg | HCO3, mEq/L | Time, min |
|---|---|---|---|
| Blood plasma | |||
| 7.22 | 32 | 12.8 | 0 |
| 7.26 | 41.4 | 18.4 | 30 |
| 7.26 | 46.8 | 19.6 | 60 |
| Urine | |||
| 6.7 | 0 | ||
| 6.9 | 26.8 | 5.7 | 30 |
| 7.07 | 24.6 | 7.3 | 60 |
HCO3 × Urinary Cr × 100 (%) Fe HCO3 = Urine HCO3 × Plasma Cr/Plasma.
Fe HCO3 + 7 × 1.0/19.6 × 18 × 100 = 1.9%.
Fractional excretion of bicarbonate had been calculated using the next equation
Ammonium test was not available at that time.
Laboratory Examination
Hemoglobin 7.4 g/dL, white blood cell count 2,950, platelets 94,000, urea 40 mg/dL, creatinine 1.64 mg/dL, sodium 139 mEq/L, potassium 3.8 mEq/L, chloride 110 mEq/L, calcium 5.9 mg/dL, phosphate 2.2 mg/dL, albumin 2.8 g/dL.
Urine sodium level was 50 mEq/L, urine potassium level 16 mEq/L, and chloride 52 mEq/L. Urine anion gap was +14 mEq/L, and pH in urine was 8.0. Protein was 1,500 mg in 24-h urine collection.
Outcome
Gradually, she lost weight (17 kg) with severe cachexia. Anemia necessitated erythropoietin treatment. The patient refused gastrointestinal tract investigation. Bone marrow investigation performed to investigate pancytopenia revealed myelofibrosis probably related to secondary hyperparathyroidism with parathyroid hormone level 470 pg/mL (normal value 14–72 pg/mL).
Bone density T-score of femur was −3SD (standard deviations). At the age of 40, the patient lost all her teeth.
Renal functions test gradually deteriorated. An attempt to treat the patient by hemodialysis failed due to infection of tunneled central catheter that was removed and subsequently central line related bacteremia treated by antibiotics. Currently, she does not need renal replacement therapy. She continues medication to correct electrolyte disorders and erythropoietin to treat anemia.
Differential Diagnosis of SS
Renal involvement in SS includes interstitial nephritis, rarely with granuloma formation, and there may be a concurrent uveitis with differential diagnosis of sarcoidosis or tubulointerstitial nephritis and uveitis (TINU syndrome). Prominent enlargement of parotid and lacrimal glands, called Mikulicz syndrome is a benign disorder but may be associated with lymphoma associated with SS and IgG4-related disease.
Salivary gland biopsy remains an important diagnostic test in patients who lack evidence for systemic autoimmunity since our patient had the immune tests consistent with SS and other clinical signs that support the diagnosis of SS salivary gland biopsy was not necessary. Salivary gland biopsy was not done due to comorbidities precluding additional interventions.
Discussion
SS is an autoimmune condition with lymphocytic infiltration of the exocrine glands with sicca syndrome, dryness of the eyes (xerophthalmia), oral cavity (xerostomia), pharynx, and larynx, and occasionally involvement of visceral organs. The Swedish ophthalmologist Henrik Sjögren described a disease characterized by oral and conjunctival dryness (the “sicca syndrome”) in 1933. SS may present as a primary disease without other accompanying symptoms (primary SS) or may present as a secondary disease with other autoimmune disorders such as SLE, rheumatoid arthritis, and systemic sclerosis, called secondary SS. Classification criteria were published by the American College of Rheumatology/European League Against Rheumatism in 2016.
Estimated prevalence of SS in the general population ranges from 0.01 to 0.1%, usually after the age of 50 and predilection 9/1 toward females. Prevalence of renal involvement in SS varies greatly but may be up to 30% [1].
The most common renal involvement in SS is tubulointerstitial nephritis, dRTA, proximal tubule dysfunction (Fanconi syndrome), or nephrogenic diabetes insipidus. Glomerular involvement had also been reported including membranoproliferative glomerulonephritis and cryoglobulinemia induced by polyclonal B-cell activation. Prevalence of tubulointerstitial nephritis in SS with renal involvement can be as high as 65–71%, distal acidification defect occurs in up to 25% of patients.
dRTA is a tubular disorder with a primary defect of urinary acidification and acid excretion in the collecting duct. These patients suffer from hyperchloremic metabolic acidosis with nephrolithiasis, necessitating correction of metabolic and electrolyte defects. It can result in severe hypokalemia due to proximal leak of potassium, reduced distal H+ excretion with increased potassium secretion, and increased distal flow, causing additional urine potassium loss. Extreme hypokalemia may cause muscle paralysis, with respiratory arrest and cardiac arrhythmias. Metabolic acidosis is usually mild, but some patients present with a plasma bicarbonate concentration below 10 mEq/L and plasma potassium concentration below 1.5–2 mEq/L.
RTA may be associated with SS and other autoimmune diseases in adults or in childhood with mutations of SLC4A1, ATP6V1B1, and ATP6VOA4 in inherited forms of RTA due genetic defects in anion exchangers within intercalated cells. Alpha intercalated cells excrete protons with H+/K+-ATPase and H+-ATPase on the luminal membrane with retention of bicarbonate via BAND3 on the basolateral membrane. Mutations in the SLC4A1 gene encoding BAND3 lead to dRTA inherited in dominant fashion. Mutations of ATP6V1B1 or ATP6VOA4 genes encode H+-ATPase, resulting in recessively transmitted dRTA [2]. Patients with RTA due to hereditary mutations were usually under 10 years old, whereas adult (later than 16 years of age) onset of RTA and sex distribution (predominantly females) suggests RTA complicating autoimmune disorders, especially SS.
Possible mechanism of dRTA in these autoimmune disorders is not completely understood. Antibodies anti-SSA/Ro may be involved in the pathogenesis of dRTA and implicated in the pathogenesis of Sjögren's/SLE disease. Absence of H+-ATPase in renal biopsy by immunohistochemistry using a rabbit polyclonal antibody against the 70 kDa catalytic subunit of H (+)-ATPase was demonstrated in patients with SS and idiopathic dRTA. Evans et al. [3] demonstrated lymphocytic infiltrate with CD4T cell predominance on kidney biopsies.
Hypokalemic paralysis may precede sicca syndrome from 3 months to 4 years in the patient with final diagnosis of primary SS. Such cases have been initially diagnosed as RTA; some of these patients with hyperglobulinemia complained of dryness of the mouth and were later diagnosed as SS, while SS without hyperglobulinemia is rarely complicated by RTA [4, 5]. In our patient, RTA appeared 5 years before the presentation of Sjögren's disease.
Treatment of SS includes glucocorticoids, disease-modifying anti-rheumatic drugs, and biological drugs that may affect B-cells depletion (rituximab) or anti-B-cell activating factor therapy (belimumab), protein suppressing B-cell activating factor required for B-cell proliferation.
Steroid treatment only rarely corrects the acidification defect, as described by el-Mallakh et al. [6]. It was reported that RTA and interstitial nephritis remitted after long-standing glucocorticoid therapy in a patient with Sjögren's/SLE disease. In our patient despite treatment by immunosuppressive medication (steroids and Azathioprine), RTA persisted. Long delay from the first episode of nephrolithiasis and the final diagnosis of SS/SLE overlap syndrome may also explain failure of immunosuppressive therapy to correct acidification defect in our patient.
Take-Home Message
High index of suspicion for likelihood of SS is essential in adult patients, suffering from metabolic acidosis and hypokalemia with RTA.
Patients with RTA need strict laboratory control and replacement therapy for electrolyte and acid-base disorders.
RTA with hypokalemic paralysis in adult patients may precede sicca syndrome for several years until final diagnosis of SS is done.
Treatment of by immunosuppressive drugs may only rarely correct the acidification defect.
Statement of Ethics
The patient has given her written informed consent to publish her case including publication of images. The research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
We have no funding sources.
Author Contributions
Anna B. Basok, MD: follow-up and treatment of the patient and writing the article. Prof. Yosef-S. Haviv: treatment of the patient and writing the article. Boris Rogachev, MD: initial diagnosis of RTA of the patient. Marina Voroviov, MD: writing the article and contributed to further assessment of the patient.
References
- 1.Francois H, Mariette X. Renal involvement in primary Sjogren syndrome. Nat Rev Nephrol. 2016;12((2)):82–93. doi: 10.1038/nrneph.2015.174. [DOI] [PubMed] [Google Scholar]
- 2.Mohebbi N, Wagner CA. Pathophysiology, diagnosis and treatment of inherited distal renal tubular acidosis. J Nephrol. 2018;31((4)):511–22. doi: 10.1007/s40620-017-0447-1. [DOI] [PubMed] [Google Scholar]
- 3.Evans RD, Laing CM, Ciurtin C, Walsh SB. Tubulointerstitial nephritis in primary Sjogren syndrome: clinical manifestations and response to treatment. BMC Musculoskelet Disord. 2016;17:2. doi: 10.1186/s12891-015-0858-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.An J, Braam B. Complete hypokalemic quadriparesis as a first presentation of sjogren syndrome. Can J Kidney Health Dis. 2018;5:2054358118774536. doi: 10.1177/2054358118774536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lim AK, Choi MJ. Distal renal tubular acidosis associated with Sjogren syndrome. Intern Med J. 2013;43((12)):1330–4. doi: 10.1111/imj.12300. [DOI] [PubMed] [Google Scholar]
- 6.el-Mallakh RS, Bryan RK, Masi AT, Kelly CE, Rakowski KJ. Long-term low-dose glucocorticoid therapy associated with remission of overt renal tubular acidosis in Sjogren's syndrome. Am J Med. 1985;79((4)):509–14. doi: 10.1016/0002-9343(85)90040-3. [DOI] [PubMed] [Google Scholar]