Abstract
Fish pedicures and/or fish manicures are treatments performed in spas involving the use of the living fish Garra rufa. In the last decade, the use of G. rufa for cosmetic and therapeutic reasons has become increasingly popular. The patients are placed into a bath to control psoriasis, eczema, or other skin conditions, but there is no scientific proof of their effectiveness. Most of the infections described in association with fish spas result from minor skin injury and contact with fish carrying such bacteria as Staphylococcus aureus, Aeromonas sobria, and Mycobacterium marinum. Therefore, fish spas in general should not be recommended, particularly for diabetic patients, immunocompromised patients, or patients treated with biological agents.
Keywords: Psoriasis, Garra rufa, Fish manicure, Fish pedicure, Fish spas, Mycobacteriosis, Infection, Aquarium granuloma, Swimming pool granuloma, Fish tank granuloma
Established Facts
Already known fact 1: use of Garra rufa fish in fish spas for cosmetic and therapeutic reasons.
Already known fact 2: fish spas are used to control psoriasis, eczema, or other skin conditions
Already known fact 3: without any scientific proof.
Already known fact 4: infections are described in association with fish spas.
Novel Insights
New information 1: first infection with fish manicures.
Introduction
The use of Garra rufa fish for cosmetic reasons has become popular. Fish pedicures and/or fish manicures involve the use of living fish. Conventional methods of sterilization and/or disinfection of the water and equipment cannot be used, as they would kill the fish. Both tank water and fish have been shown to contain a wide variety of microorganisms and can act as reservoirs for drug-resistant bacterial strains. This has raised questions about the potential transmission of infections in fish spas.
Case Report
A 41-year-old patient was admitted to the dermatology department because of a hardened, rough, brownish erythematous periungual plaque of the left thumb. The lesion, which extended radially, had developed 4 weeks after a fish manicure when he went on vacation in Thailand. During his vacation, the patient did not dive or eat seafood and did not hurt himself. The lesion had been slowly evolving for months (Fig. 1, 2). Pruritus was not present. The patient did not have any other disease and did not own an aquarium. He did not work in a garden. When he returned home to Belgium, the GP gave the patient some medication, topical fusidic acid, antimycotic cream, oral flucloxacillin, oral lymecycline, oral itraconazole, and oral fluconazole, but the lesion did not improve. The suspected mycobacterial infection was confirmed as a non-necrotizing granuloma made up of sheets of epithelioid histiocytes in the deep part of the dermis (Fig. 3, 4). Mycobacterium marinum infection was confirmed by molecular methods (PCR). The patient was treated with oral doxycycline 200 mg/day. After 4 months of treatment, the clinical infection regressed, leaving scars without regrowth after 10 months.
Fig. 1.
Hardened and rough-brownish erythematous periungual plaque of the left thumb − face view.
Fig. 2.
Lateral view of the left thumb.
Fig. 3.
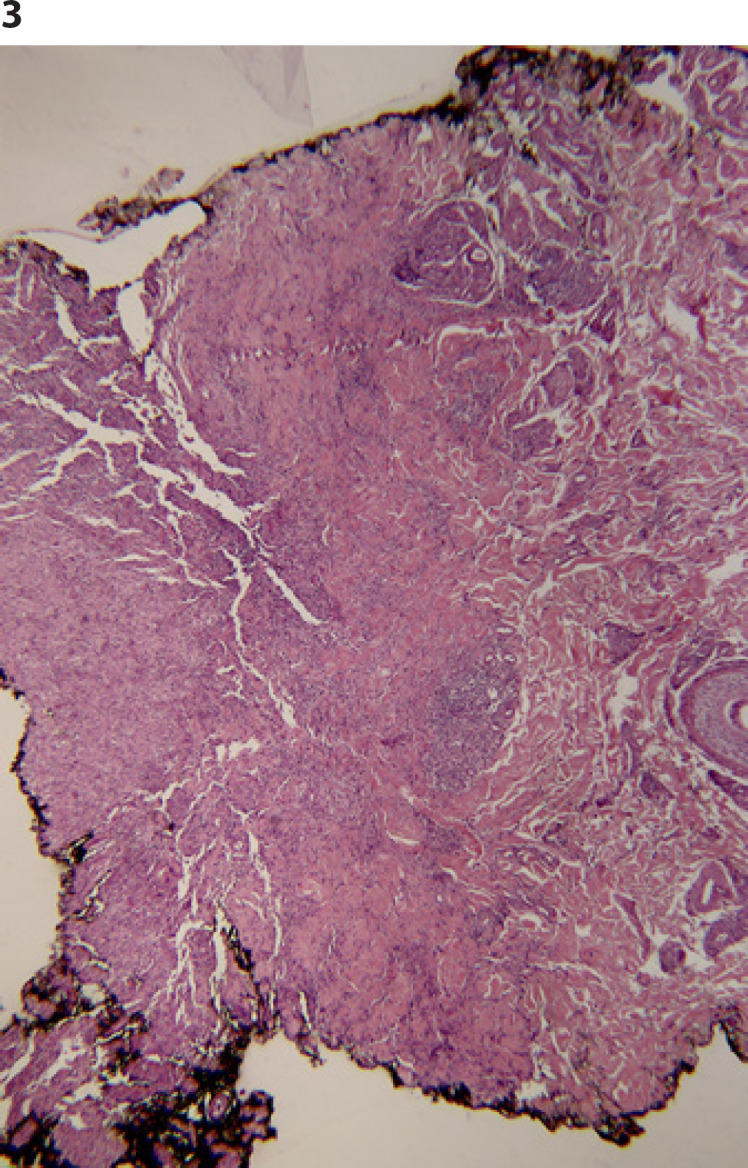
Inflammation in the deep part of the dermis (HE. ×50).
Fig. 4.

Non-necrotizing granuloma, constituted by sheets of epithelioid histiocytes (HE. ×200).
Discussion
Fish pedicures or manicures are treatments performed in spas. The patients put their hands or feet in small baths containing 25–30°C water and many fish that nibble off dead skin. G. rufa fish manicures and pedicures have been done for decades in Turkey and the Middle East, where patients are placed into a bath to control psoriasis, eczema, or other skin conditions, but there is no scientific proof of their effectiveness [1]. In the last decade, the use of G. rufa fish for cosmetic reasons has become increasingly popular, and establishments offering fish pedicures and/or manicures worldwide are visited because they claim that the fish only eat dead skin. The species G. rufa is known under the commercial name of doctor fish but is also referred to as Discognathus crenulatus, D. obtusus, D. rufus, G. rufa crenulata, G. rufa gymnothorax, and G. rufus. The health risks associated with fish manicures or pedicures are mainly infectious. Recently, case reports of Staphylococcus aureus infection [2] and methicillin-resistant S. aureus infection were reported [3] after fish pedicures. A case of Aeromonas sobria superficial necrotic bullous erysipelas in an unknown, latent non-insulin-dependent diabetic patient after a fish pedicure has also been described [1]. There have been reports of lower extremity furunculosis caused by M. fortuitum, M. mageritense, M. bolletii, M. massiliense, and M. chelonae/abscessus [4, 5, 6]. Recently, we reported an M. marinum infection of the foot following a fish pedicure [7]. There have been no reports of blood-borne disease transmission, such as HIV or hepatitis, but theoretically there exists a minor risk of these. Finally, onychomadesis of the toenails has been reported [8]. Given the lack of evidence, fish manicure has no proven cosmetic benefit and may cause significant infections. Since fish manicures or pedicures involve the use of living fish, conventional methods of sterilization and/or disinfection of the water and equipment, except chloramine T and peracetic acid, cannot be used, as they would kill the fish [9]. Both tank water and fish have been shown to contain a wide variety of microorganisms and can act as reservoirs for drug-resistant bacterial strains [10]. Indeed, the baths cannot be adequately disinfected between patients, and the fish also bring a risk of zoonotic infection transmission. The visitor must be aware of the risks of such procedures.
Conclusion
Fish manicures are probably less common than fish pedicures, but as illustrated by this case report, they have the same associated risks. Most of the infections described today in association with fish spas are infections transmitted from person to person through the water, including S. aureus. This S. aureus infection resulted from minor skin injury and contact with contaminated aquarium fish. The infection is also known as aquarium granuloma, swimming pool granuloma or fish tank granuloma. Fish tank granuloma is an uncommon and underreported disease, and few cases of pedicure footbaths have been reported [11, 12]. Disseminated infection is rare and almost always occurs in immunosuppressed individuals or patients with psoriasis treated with biological agents [13, 14, 15]. Therefore, fish spas in general should not be recommended, particularly for diabetic patients, immunocompromised patients, or patients treated with biological agents.
Statement of Ethics
The patient gave written informed consent to publish the case, including clinical images.
Conflict of Interest Statement
All authors certified that they have no conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject of this manuscript.
Funding Sources
No funding was obtained for this work.
Author Contributions
The content of the paper has not been published or submitted for publication elsewhere. All authors have contributed significantly, and are in agreement with the content of the manuscript. In keeping with the latest guidelines of the International Committee of Medical Journal Editors, each author's contribution to the paper is to be quantified.
References
- 1.Vanhooteghem O, Anseeuw D, Michel C, Penninckx M, Pironnet A-M, Simon A, et al. Fish pedicure-induced Aeromonas sobria superficial necrotic bullous dermatitis in a previously undiagnosed diabetes patient. What are the risks of fish pedicure for public health? Br J Med Med Res. 2015;10((12)):1–10. [Google Scholar]
- 2.Veraldi S, Nazzaro G, Çuka E. Staphylococcus aureus infection of the feet following fish pedicure. Infection. 2014;42((5)):925–6. doi: 10.1007/s15010-014-0622-4. [DOI] [PubMed] [Google Scholar]
- 3.Sugimoto K, Frei R, Graber P. Methicillin-resistant Staphylococcus aureus foot infection after fish pedicure. Infection. 2013;41((5)):1013–5. doi: 10.1007/s15010-013-0437-8. [DOI] [PubMed] [Google Scholar]
- 4.Wertman R, Miller M, Groben P, Morrell DS, Culton DA. Mycobacterium bolletti/Mycobacterium massiliense furunculosis associated with pedicure footbaths: a report of 3 cases. Arch Dermatol. 2011;147((4)):454–8. doi: 10.1001/archdermatol.2011.58. [DOI] [PubMed] [Google Scholar]
- 5.Gira AK, Reisenauer AH, Hammock L, Nadiminti U, Macy JT, Reeves A, et al. Furunculosis due to Mycobacterium mageritense associated with footbaths at a nail salon. J Clin Microbiol. 2004;42((4)):1813–7. doi: 10.1128/JCM.42.4.1813-1817.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Redbord KP, Shearer DA, Gloster H, Younger B, Connelly BL, Kindel SE, et al. Atypical Mycobacterium furunculosis occurring after pedicures. J Am Acad Dermatol. 2006;54((3)):520–4. doi: 10.1016/j.jaad.2005.10.018. [DOI] [PubMed] [Google Scholar]
- 7.Vanhooteghem O, Theate I. Fish pedicure-induced foot mycobacteriosis infection due to Mycobacterium marinum: a first case report. Eur J Dermatol. 2017;27((3)):299–300. doi: 10.1684/ejd.2017.2976. [DOI] [PubMed] [Google Scholar]
- 8.Lipner SR. Onychomadesis following a fish pedicure. JAMA Dermatol. 2018;154((9)):1091–2. doi: 10.1001/jamadermatol.2018.1827. [DOI] [PubMed] [Google Scholar]
- 9.Sirri R, Zaccaroni A, Di Biase A, Mordenti O, Stancampiano L, Sarli G, et al. Effects of two water disinfectants (chloramine T and peracetic acid) on the epidermis and gills of Garra rufa used in human ichthyotherapy. Pol J Vet Sci. 2013;16((3)):453–61. doi: 10.2478/pjvs-2013-0063. [DOI] [PubMed] [Google Scholar]
- 10.Volpe E, Mandrioli L, Errani F, Serratore P, Zavatta E, Rigillo A, et al. Evidence of fish and human pathogens associated with doctor fish (Garra rufa, Heckel, 1843) used for cometic treatment. J Fish Dis. 2019;42((12)):1637–44. doi: 10.1111/jfd.13087. [DOI] [PubMed] [Google Scholar]
- 11.Stout JE, Gadkowski LB, Rath S, Alspaugh JA, Miller MB, Cox GM. Pedicure-associated rapidly growing mycobacterial infection: an endemic disease. Clin Infect Dis. 2011;53((8)):787–92. doi: 10.1093/cid/cir539. [DOI] [PubMed] [Google Scholar]
- 12.Ang P, Rattana-Apiromyakij N, Goh CL. Retrospective study of Mycobacterium marinum skin infections. Int J Dermatol. 2000;39((5)):343–7. doi: 10.1046/j.1365-4362.2000.00916.x. [DOI] [PubMed] [Google Scholar]
- 13.Morales P, Gil A, Santos M. Mycobacterium abscessus infection in transplant recipients. Transplant Proc. 2010;42((8)):3058–60. doi: 10.1016/j.transproceed.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 14.Ribot E, Poisnel E, De Biasi C, Roudier J, Balandraud N. Atypical Mycobacterium marinum infection (Aquarium granuloma) in a patient on TNFα antagonist therapy for psoriatic arthritis. Joint Bone Spine. 2014;81((3)):272–3. doi: 10.1016/j.jbspin.2013.11.011. [DOI] [PubMed] [Google Scholar]
- 15.Caron J, Michot C, Fabre S, Godreuil S, Guillot B, Dereure O. Aggressive cutaneous infection with Mycobacterium marinum in two patients receiving anti-tumor necrosis factor-alfa agents. J Am Acad Dermatol. 2011;65((5)):1060–2. doi: 10.1016/j.jaad.2008.12.041. [DOI] [PubMed] [Google Scholar]




