Abstract
Background:
Occupational hand dermatitis (OHD) is a skin disease occurring on employees’ hands in certain jobs. Little is known about prevalence, incidence and characteristics of this adverse skin reaction and its associated risk factors during COVID-19 pandemic. To evaluate both prevalence and incidence of OHD and associated risk factors in Italian clinicians.
Methods:
A cross-sectional study was performed using a self-report questionnaire.
Results:
Two hundred and thirty clinicians responded to the survey and 82% of responders did not report previous OHD history before the COVID-19 pandemic. Daily use of gloves was reported by 80% of responders. OHD prevalence was 18%, while incidence was 80%. We found a protective effect on symptom occurrence for vinyl/nitrile gloves if the time with gloves was ≥ 6 hours per day.
Conclusions:
This survey reveals a high OHD incidence in an Italian population of clinicians. Furthermore, wearing vinyl/nitrile gloves for at least 6 hours a day had a protective effect on symptom onset.
Keywords: COVID-19, occupational hand dermatitis, healthcare workers, personal protective equipment, protective gloves, hand washing
Introduction
A novel coronavirus named 2019-nCoV was discovered in December 2019 in Wuhan, China causing coronavirus disease 2019 (COVID-19), which spread rapidly throughout the country and the world (1,2). In this emergency, the simple act of hand washing, regardless of other medical interventions, is a cornerstone of behaviours to prevent the transmission of respiratory viruses (3). Furthermore, hand washing with an adequate antimicrobial product for at least 20 seconds can reduce the risk of transmission of viruses including SARS-CoV-2 (4). However, hand protection measures (gloves, alcoholic-based sanitizers, cream/moisturizers) can cause adverse skin reaction; occupational hand dermatitis (OHD) is common in health-care workers (HCWs), because of frequent hand hygiene and prolonged glove wearing. The first signs of OHD are red and scaly patches in the finger webs and on the knuckle area of the hands. Itchy blisters, painful cracks, and possibly infection are common, and eventually the skin becomes thickened.
In the pre-COVID era the prevalence of OHD among HWCs was around 20-50% in the United States (5), 31.5% in China (6) and 13% in the Netherlands (7), which increased significantly during the COVID-19 pandemic. One multicentre study from Wuhan, China, reported an OHD prevalence of 74.5% (6). A further Chinese study showed that the prevalence of skin injury, caused by enhanced infection-prevention measures, increased up to 97% among physicians and nurses who worked in tertiary hospitals during the pandemic (8). In the rest of the world, the prevalence of OHD was estimated to be 46.4% in a group of Saudi Arabian HCWs (9), 50.4% in a group of Turkish HCWs treating COVID-19 patients (10), and 76% in an Irish study (11). In a German survey, comparing the onset of OHD and associated symptoms between HCWs directly involved in intensive care and HCWs without direct contact to this patient cohort, in a single surgical clinic during the COVID-19 pandemic, the total prevalence was 90.4% (12).
Beiu et al. (4) reviewed the potential dermatological adverse effects that may arise due to frequent hand washing, as well as practical tips to prevent these uncomfortable skin reactions, which were preventable and manageable using appropriate skin care products and found that regular skin hydration is essential to prevent skin injuries derived from frequent washing. To date, no data on both prevalence and incidence of OHD in Italy is available. We aimed to study both prevalence and incidence of OHD (primary outcomes) among clinicians employed in a tertiary Italian Hospital. Furthermore, we assessed associations among skin damages and demographic, occupational and behavioral variables.
Methods
Study design, setting, and participants
This cross-sectional survey was carried out from September 7 to November 7, 2020. The prevalence of OHD-defined as a skin disease occurring on employees’ hands in certain jobs-was evaluated at the beginning of the study (March 1, 2020). Incidence was estimated from data collected in the period from March 2, 2020 until the end of the study. All clinicians received an online survey via email to assess self-perceived adverse skin reactions. The e-mail contained a brief explanation of the study aims and an invitation to respond anonymously to a 10-item multiple choice questionnaire. After consenting to participate anonymously, the recipient answered the questionnaire.
The study was conducted and described according to the STROBE checklist. The local Ethics Committee approved the SHIELD Study.
Questionnaire and Data Collection
The study used the commercially available online survey platform Microsoft Forms, which is included in the Hospital’s Microsoft Office 365 package. Survey data were analyzed with the analytic tools within Microsoft Forms respectively Microsoft Excel. The questionnaire was firstly validated through the following procedure: 1) use of a structured Delphi Method to achieve mutual agreement among panel experts to identify questions, and 2) validation phase on the first 25 responders to analyze applicability and generalizability.
A reminder mail was sent after two weeks of the first communication. In addition to demographic information, self-perceived adverse skin reactions were recorded. Furthermore, the following variables were collected: known exposure to COVID-19 patients, duration with and types of gloves, frequency of hand washing, topical hand cream application after washing, previously allergological history and pre-existing hand dermatitis (HD). No incentives were offered to complete the survey.
Sample size
For the calculation of the sample size (i.e. the number of completed responses the research team receives) 1) a population size of 1465 clinicians, 2) a margin of error of 5%, 3) a chosen sampling confidence level of 95% and 4) a response rate (i.e. the percentage of clinicians who actually complete the survey) of 50% was considered; a sample size of 305 subjects was estimated.
Statistical analysis
The effect of candidate predictors on the outcome of interest (having at least one symptom) was tested individually with Chi-squared test or Fisher’s exact test, when appropriate. Covariates, resulting statistically significant at the univariate analysis, were used to estimate a logistic regression model through Akaike Information Criterion (AIC)-based stepwise model selection. Two versions of the model have been foreseen. In a first version of the model, all the covariates were considered as non-interacting. In the second version of the model, an interaction term was added between “time with gloves” and “type of gloves”.
The receiver operating characteristic (ROC) curve was used to evaluate the performance of the model. A threshold of 0.05 on p-values was considered significant for statistical test. All statistical analysis was performed using R (version 3.4.4).
Results
Two hundred thirty clinicians responded to this survey. Table 1 summarizes the results of the questionnaire. Twenty (8.7%) clinicians were under 29 years old, 136 (59.1%) between 30 and 49 years, and the remaining 74 (32.2%) were at least 50 years old. No gender predominance was found: 123 (53.5%) clinicians were female.
Table 1.
Results of survey. HE~: hand eczema. CD*: contact dermatitis
| Items | N° of subjects | % | |
| N° ofresponders | 230 | ||
| Sex (Female) | 123 | 53 | |
| Age groups (years) |
≤29 | 20 | 9 |
| 30-49 | 136 | 59 | |
| ≥50 | 74 | 32 | |
| Pre-existing HE~ | No | 188 | 82 |
| Yes | 42 | 18 | |
| Irritative CD * | 17 | 7 | |
| AllergicCD * | 4 | 2 | |
| Atopic dermatitis | 13 | 6 | |
| Unclassified eczema | 8 | 3 | |
| History of other allergie disease | No | 173 | 75 |
| Yes | 57 | 25 | |
| Time with gloves | <6 hours/day | 121 | 53 |
| ≥6 hours/day | 63 | 27 | |
| Type of used gloves | I.atex gloves | 93 | 40 |
| Vinyl/ nitrile gloves | 109 | 47 | |
| Frequency of hand washing |
<10 times/ day | 56 | 24 |
| ≥10 times/ day | 173 | 75 | |
| Topical hand emollient cream use after washing | No | 213 | 93 |
| Yes | 16 | 7 |
The majority of responders (188, 82%) did not report a history of HD before the COVID-19 pandemic. Among the remaining responders, 17 (7%) suffered from irritative contact dermatitis, 4 (2%) reported a history of allergic contact dermatitis, 13 (6%) reported previous atopic dermatitis. Finally, 8 (3%) responders reported a history of unclassified eczema.
One hundred and seventy-three (75%) clinicians did not suffer from other allergic diseases. Daily use of gloves was reported by most responders: 121 (53%) clinicians reported wearing gloves for less than 6 hours per day, while, 63 (27%) clinicians wore gloves for at least 6 hours per day. There was no predominance of a specific glove type: 93 (40%) clinicians reported wearing latex gloves, while, 109 (47%) responders preferred vinyl/nitrile gloves. As expected, most clinicians (173, 75%) reported frequent daily hand washing at least 10 times a day. Very rare was the use of emollient cream applied after hand washing. In fact, only 16 (7%) responders reported the use of emollients.
Concerning the primary outcomes, OHD prevalence among clinicians was 18% and incidence was 80%. Figure 1 describes the frequency of OHD symptoms reported by clinicians. Dryness, erythema, desquamation, fissuring and itching were the symptoms most commonly described by responders.
Figure 1.
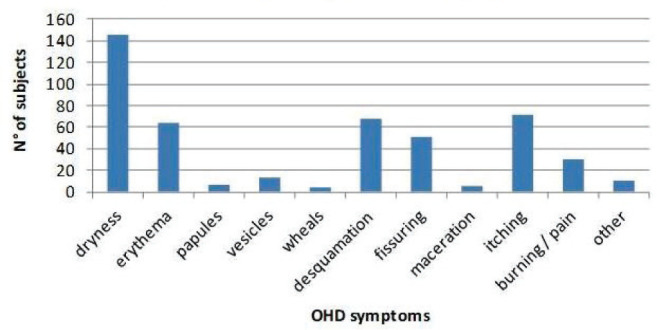
Frequency of OHD symptoms.
Table 2 shows the individual effect of candidate predictors on the outcome of interest “incidence”. Age (p=0.029), sex (p=0.047), time with gloves (p=0.042) and pre-existing hand eczema (HE) (p<0.001) was individually associated to OHD incidence.
Table 2.
Effect of candidate predictors on the outcome of interest “OHD incidence”. *: The effect of candidate predictors on the outcome of interest “OHD incidence” (having at least 1 symptom among those shown in Figure 1) was tested individually with Fisher’s exact test. HEɫ: hand eczema
| Covariate | No OHD symptoms | OHD symptoms | p-value • | |
| Age | ≤ 29 years | 6 | 14 | 0.029 |
| 30-49 years | 19 | 117 | ||
| ≥ 50 years | 20 | 54 | ||
| Sex | Male | 27 | 80 | 0.047 |
| Female | 18 | 105 | ||
| Time with gloves | < 6 hours/day | 20 | 101 | 0.042 |
| ≥ 6 hours/day | 9 | 54 | ||
| No gloves | 16 | 30 | ||
| Type of gloves | Latex | 15 | 64 | NS |
| Vinyl / nitrile | 10 | 81 | ||
| Frequency of hand washing | < 10 times/day | 15 | 41 | NS |
| ≥ 10 times/day | 30 | 143 | ||
| Topical band cream appliance after washing | No | 43 | 170 | NS |
| Yes | 2 | 14 | ||
| Other pre-existing allergic diseases | No | 34 | 138 | NS |
| Yes | 10 | 47 | ||
| Pre-existing HE1 | No | 46 | 143 | < 0.001 |
| Yes | 0 | 42 |
After the AIC-based selection, the logistic regression model included the following variables: age, sex, time with gloves and pre-existing HE (Figure 2). Overall classification performance of the model was: AUC = 0.79 (95% CI: 0.63-0.75), sensitivity = 0.6811, specificity = 0.7556, positive predictive value (PPV) = 0.9197 and negative predictive value (NPV) = 0.3656 (Figure 2).
Figure 2.
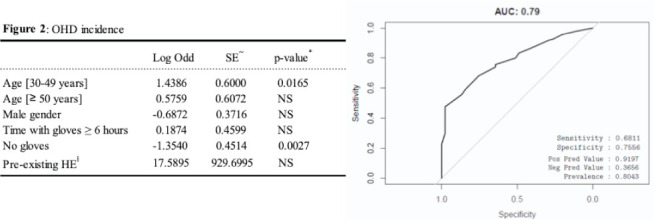
OHD incidence: logistic regression model through AIC-based stepwise model selection with covariates which resulted statistically significant at the univariate analysis. All covariates were considered as non-interacting. *: A threshold of 0.05 on p-values was considered significant for statistical test. SE~: Standard Error. HEɫ: hand eczema
The second version of the model, after the AIC-based selection, included the following variables: age, sex, time with gloves, type of gloves, pre-existing HE, interaction term between time with gloves and type of gloves (Figure 3). The effect of the last interaction term had a protective effect on symptom occurrence for type of gloves equal to vinyl/nitrile if the time with gloves is ≥ 6 hours per day, showing a log odd of -2.21 and a p-value of 0.0339. The overall classification performance of the second model was: AUC = 0.79 (95% CI: 0.64-0.77), sensitivity = 0.6968, specificity = 0.7586, PPV = 0.9391 and NPV = 0.3188 (Figure 3).
Figure 3.
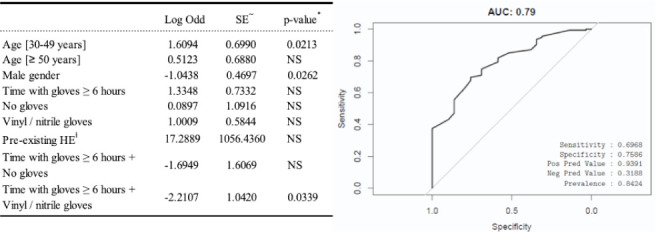
OHD incidence. Logistic regression model through AIC-based stepwise model selection with covariates which resulted statistically significant at the univariate analysis with the addition of an interaction term between “time with gloves” and “type of gloves”. *: A threshold of 0.05 on p-values was considered significant for statistical test. SE~: Standard Error. HEɫ: hand eczema
Discussion
To our knowledge, this is the first study that explores both prevalence and incidence of OHD among clinicians in an Italian tertiary hospital during the COVID-19 pandemic. We found a high incidence of OHD among clinicians (80%). Furthermore, a not negligible prevalence was observed (18%).
In literature, growing evidence demonstrate the impact of PPEs on the health of the skin, particularly on hands of frontline HCWs. In fact, after the first evidence of a very high prevalence of skin damages by Lan et al. in March 2020 (8), the subsequent reports, from different countries around the world, have confirmed a high prevalence of OHD ranging from 46.4% in a Saudi Arabia experience to 97% in a Chinese group of HCWs (6,8-13). Curiously, our data showed a prevalence (18%) lower than before mentioned published reports (6,8-13). On the other hand, we highlighted, for the first time, a high incidence of OHD (80%) in Italian clinicians during the COVID-19 pandemic. Studies reporting incidence data are limited (14-23) and results differed by study design, type of skin disease, and occupationally exposed populations.
Recently, Larese et al. systematically reviewed studies on incidence of contact dermatitis in HCWs highlighting the dearth of high-quality data and the possible underestimation of disease burden in the pre-COVID-19 era (24). In our study, age, sex, time with gloves and pre-existing HE were individually associated to OHD incidence. Therefore, we focused on these covariates in order to define a logistic regression model through AIC-based stepwise model selection. If all the covariates were considered as non-interacting, age between 30 and 49 years and wearing gloves could be considered risk factors for OHD with a prediction model characterized by a good performance (AUC = 0.79, PPV = 0.9197).
Since type of gloves and time with gloves are closely related from a clinical point of view, we eviscerated the impact of this interaction on OHD incidence through the before detailed second prediction model. Hence, we showed, for the first time, a protective effect on symptom occurrence for vinyl/nitrile gloves if the time with gloves was ≥ 6 hours per day (log odd of -2.21, p-value = 0.0339).
Our study has some limitations. First, only clinicians were invited to respond to the survey. Furthermore, the number of responders was limited. Out of 1465 clinicians invited, only 230 agreed to answer the questionnaire. Finally, this was a survey not supported by medical evaluation with allergological diagnostics of the new self-reported cases.
Conclusions
In conclusion, our study shows, for the first time, a high incidence of OHD in a population of Italian clinicians. Importantly, wearing vinyl/nitrile gloves for at least 6 hours a day has a protective effect on the onset of symptoms. Future studies are needed to investigate optimal strategies to reduce the risk of occupational hand dermatitis in all frontline healthcare workers.
Funding:
This research received no external funding.
Institutional Review Board Statement:
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of Fondazione Policlinico Universitario A. Gemelli IRCCS in Rome, Italy (ID 3274; Prot. N. 0025420/20).
Informed Consent Statement:
Patient consent was waived due to data were collected anonymously.
Conflict of interest:
No potential conflict of interest relevant to this article was reported by the authors
References
- 1.Epidemiology Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention. (The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China) Zhonghua Liu Xing Bing Xue Za Zhi Zhonghua Liuxingbingxue Zazhi. 2020;41(2):145–151. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003. Doi: 10.3760/cma.j.issn.0254-6450.2020.02.003. [DOI] [PubMed] [Google Scholar]
- 2.Wu Y-C, Chen C-S, Chan Y-J. The outbreak of COVID-19: An overview. J Chin Med Assoc (JCMA) 2020;83(3):217–220. doi: 10.1097/JCMA.0000000000000270. Doi: 10.1097/JCMA.0000000000000270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ma Q, Shan H, Zhang H, Li G, Yang R, Chen J. Potential utilities of mask‐wearing and instant hand hygiene for fighting SARS‐CoV‐2. J Med Virol. 2020 doi: 10.1002/jmv.25805. doi: 10.1002/jmv.25805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beiu C, Mihai M, Popa L, Cima L. Popescu MN. Frequent Hand Washing for COVID-19 Prevention Can Cause Hand Dermatitis: Management Tips. Cureus. 2020;12(4):e7506. doi: 10.7759/cureus.7506. Doi: 10.7759/cureus.7506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lampel HP, Patel N, Boyse K, O’Brien SH, Zirwas MJ. Prevalence of hand dermatitis in inpatient nurses at a United States hospital. Dermat Contact Atopic Occup Drug. 2007;18(3):140–142. doi: 10.2310/6620.2007.06024. Doi: 10.2310/6620.2007.06024. [DOI] [PubMed] [Google Scholar]
- 6.Lin P, Zhu S, Huang Y, et al. Adverse skin reactions among healthcare workers during the coronavirus disease 2019 outbreak: a survey in Wuhan and its surrounding regions. Br J Dermatol. 2020;183(1):190–192. doi: 10.1111/bjd.19089. Doi: 10.1111/bjd.19089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van der Meer EWC, Boot CRL, van der Gulden JWJ, Jungbauer FHW, Coenraads PJ, Anema JR. Hand eczema among healthcare professionals in the Netherlands: prevalence, absenteeism, and presenteeism. Contact Dermatitis. 2013;69(3):164–171. doi: 10.1111/cod.12099. Doi: 10.1111/cod.12099. [DOI] [PubMed] [Google Scholar]
- 8.Lan J, Song Z, Miao X, et al. Skin damage among health care workers managing coronavirus disease-2019. J Am Acad Dermatol. 2020;82(5):1215–1216. doi: 10.1016/j.jaad.2020.03.014. Doi: 10.1016/j.jaad.2020.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alluhayyan OB, Alshahri BK, Farhat AM, et al. Occupational-Related Contact Dermatitis: Prevalence and Risk Factors Among Healthcare Workers in the Al’Qassim Region, Saudi Arabia During the COVID-19 Pandemic. Cureus. 2020;12(10):e10975. doi: 10.7759/cureus.10975. Doi:10.7759/cureus.10975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Erdem Y, Altunay IK, Aksu Çerman A, et al. The risk of hand eczema in healthcare workers during the COVID-19 pandemic: Do we need specific attention or prevention strategies? Contact Dermatitis. 2020;83(5):422–423. doi: 10.1111/cod.13632. Doi: 10.1111/cod.13632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kiely LF, Moloney E, O’Sullivan G, Eustace JA, Gallagher J, Bourke JF. Irritant contact dermatitis in healthcare workers as a result of the COVID-19 pandemic: a cross-sectional study. Clin Exp Dermatol. 2020;46(1):142–144. doi: 10.1111/ced.14397. Doi: 10.1111/ced.14397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guertler A, Moellhoff N, Schenck TL, et al. Onset of occupational hand eczema among healthcare workers during the SARS-CoV-2 pandemic: Comparing a single surgical site with a COVID-19 intensive care unit. Contact Dermatitis. 2020;83(2):108–114. doi: 10.1111/cod.13618. Doi: 10.1111/cod.13618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pei S, Xue Y, Zhao S, et al. Occupational skin conditions on the front line: a survey among 484 Chinese healthcare professionals caring for Covid-19 patients. J Eur Acad Dermatol Venereol. 2020;34(8):e354–e357. doi: 10.1111/jdv.16570. Doi: 10.1111/jdv.16570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smit HA, Coenraads PJ. A retrospective cohort study on the incidence of hand dermatitis in nurses. Int Arch Occup Environ Health. 1993;64(8):541–544. doi: 10.1007/BF00517697. Doi: 10.1007/BF00517697. [DOI] [PubMed] [Google Scholar]
- 15.Smit HA, van Rijssen A, Vandenbroucke JP, Coenraads PJ. Susceptibility to and incidence of hand dermatitis in a cohort of apprentice hairdressers and nurses. Scand J Work Environ Health. 1994;20(2):113–121. doi: 10.5271/sjweh.1423. Doi: 10.5271/sjweh.1423. [DOI] [PubMed] [Google Scholar]
- 16.Schmid K, Broding HC, Uter W, Drexler H. Transepidermal water loss and incidence of hand dermatitis in a prospectively followed cohort of apprentice nurses. Contact Dermatitis. 2005;52(5):247–253. doi: 10.1111/j.0105-1873.2005.00557.x. Doi: 10.1111/j.0105-1873.2005.00557.x. [DOI] [PubMed] [Google Scholar]
- 17.Visser MJ, Verberk MM, van Dijk FJ, Bakker JG, Bos JD, Kezic S. Wet work and hand eczema in apprentice nurses; part I of a prospective cohort study. Contact Dermatitis. 2014;70(1):44–55. doi: 10.1111/cod.12131. Doi: 10.1111/cod.12131. [DOI] [PubMed] [Google Scholar]
- 18.Larese Filon F, Bochdanovits L, Capuzzo C, Cerchi R, Rui F. Ten years incidence of natural rubber latex sensitization and symptoms in a prospective cohort of health care workers using non-powdered latex gloves 2000-2009. Int Arch Occup Environ Health. 2014;87(5):463–469. doi: 10.1007/s00420-013-0885-6. Doi: 10.1007/s00420-013-0885-6. [DOI] [PubMed] [Google Scholar]
- 19.Larese Filon F, Plazzotta S, Rui F, Mauro M, De Michieli P, Negro C. Ten-year incidence of contact dermatitis in a prospective cohort of healthcare workers in Trieste hospitals (North East of Italy) 2004-2013. Br J Dermatol. 2017;177(2):560–561. doi: 10.1111/bjd.15118. Doi: 10.1111/bjd.15118. [DOI] [PubMed] [Google Scholar]
- 20.Diepgen TL, Coenraads PJ. The epidemiology of occupational contact dermatitis. Int Arch Occup Environ Health. 1999;72(8):496–506. doi: 10.1007/s004200050407. Doi: 10.1007/s004200050407. [DOI] [PubMed] [Google Scholar]
- 21.Dickel H, Kuss O, Blesius CR, Schmidt A. Diepgen TL. Occupational skin diseases in Northern Bavaria between 1990 and 1999: a population-based study. Br J Dermatol. 2001;145(3):453–462. doi: 10.1046/j.1365-2133.2001.04377.x. Doi: 10.1046/j.1365-2133.2001.04377.x. [DOI] [PubMed] [Google Scholar]
- 22.Larese F, Mattia CF, De Toni A. Incidence of occupational contact dermatitis in the province of Pordenone in the period of 1995-2000. G Ital Med Lav Ergon. 2003;25(3):252–253. [PubMed] [Google Scholar]
- 23.Machovcová A, Fenclová Z, Pelclová D. Occupational skin diseases in Czech healthcare workers from 1997 to 2009. Int Arch Occup Environ Health. 2013;86(3):289–294. doi: 10.1007/s00420-012-0764-6. Doi: 10.1007/s00420-012-0764-6. [DOI] [PubMed] [Google Scholar]
- 24.Larese Filon F, Pesce M, Paulo MS, et al. Incidence of occupational contact dermatitis in health care workers: A systematic review. J. Eur. Acad. Dermatol. Venereol. 2020;35(6):1285–1289. doi: 10.1111/jdv.17096. Doi: 10.1111/jdv.17096. [DOI] [PMC free article] [PubMed] [Google Scholar]


