Abstract
Background
Cut-points to define slow walking speed have largely been derived from expert opinion.
Methods
Study participants (13 589 men and 5043 women aged ≥65years) had walking speed (m/s) measured over 4–6 m (mean ± SD: 1.20 ± 0.27 m/s in men and 0.94 ± 0.24 m/s in women.) Mobility limitation was defined as any self-reported difficulty with walking approximately 1/4 mile (prevalence: 12.6% men, 26.4% women). Sex-stratified classification and regression tree (CART) models with 10-fold cross-validation identified walking speed cut-points that optimally discriminated those who reported mobility limitation from those who did not.
Results
Among 5043 women, CART analysis identified 2 cut-points, classifying 4144 (82.2%) with walking speed ≥0.75 m/s, which we labeled as “fast”; 478 (9.5%) as “intermediate” (walking speed ≥0.62 m/s but <0.75 m/s); and 421 (8.3%) as “slow” (walking speed <0.62 m/s). Among 13 589 men, CART analysis identified 3 cut-points, classifying 10 001 (73.6%) with walking speed ≥1.00 m/s (“very fast”); 2901 (21.3%) as “fast” (walking speed ≥0.74 m/s but <1.00 m/s); 497 (3.7%) as “intermediate” (walking speed ≥0.57 m/s but <0.74 m/s); and 190 (1.4%) as “slow” (walking speed <0.57 m/s). Prevalence of self-reported mobility limitation was lowest in the “fast” or “very fast” (11% for men and 19% for women) and highest in the “slow” (60.5% in men and 71.0% in women). Rounding the 2 slower cut-points to 0.60 m/s and 0.75 m/s reclassified very few participants.
Conclusions
Cut-points in walking speed of approximately 0.60 m/s and 0.75 m/s discriminate those with self-reported mobility limitation from those without.
Keywords: Classification and regression trees, Gait speed, Mobility limitation
Slow usual pace gait speed measured over a short distance is predictive of mortality and disability (1,2). Several cut-points to define slowness and dichotomize gait speed into “slow” and “not slow” categories have been proposed: 0.6 (3), 0.8 (4,5), and 1.0 m/s (6). However, these cut-points are largely based on expert opinion or consideration of the prevalence of slowness defined by the various cut-points by age. For example, in Health ABC, a cut-point of 1.0 m/s was selected based on visual inspection of a graph relating walking speed to incident lower extremity limitation in a random subset, and then positive and negative likelihood ratios were compared across a number of cut-points in a separate subset of participants (7). As noted by Cesari et al., the relation between walking speed and risk of functional imitation (and other conditions in aging) appears to be log linear with no clear inflection point that could be refined by splines or other methods (1,2,7–9). Few, if any, reports have used data-driven approaches to identify a cut-point in gait speed that classifies people as slow based on self-reported function, particularly in community-dwelling adults. How “slowness” is defined has important implications for incorporating slowness into composite definitions of conditions such as sarcopenia (4–6) and frailty (10) and for predicting the risk of distal outcomes based on slowness.
Therefore, using a subset of cross-sectional data from cohort studies of older adults included in the Sarcopenia Definitions and Outcomes Consortium (SDOC), we used a machine learning technique, classification and regression tree analysis (CART), to identify cut-points in gait speed that best discriminate those who self-report a mobility limitation (at least some difficulty walking a short distance) from those who do not report such limitation. Herein we aimed to use the prevalence of a common patient-reported outcome, mobility limitation, as the “anchor,” or the term the CART models aimed to make most different across subsets of participants as identified by the model-derived cut-points. Self-reported outcomes represent a person-centered approach and are in line with efforts by the Patient-Centers Outcomes Research Institute and the National Institute of Health. A patient-reported outcome was selected as our focus because our ultimate goal is to identify cut-points in walking speed that are most important to the day-to-day health of older adults.
Method
Study Population
We used data from 8 cohort studies that were assembled for the analyses of the SDOC (11–13) (Supplementary Table 1). These studies have been extensively described elsewhere and in the SDOC publications. Analyses were limited to community-dwelling older adults aged 65 years and older with dual-energy x-ray absorptiometry body composition, grip strength, walking speed, and mobility complaints data. Participants were included if they had complete data for self-rated mobility limitation, gait speed, and age and sex. Data from the baseline visit of each study were used, except for Health ABC where the Year 7 (Visit 8) and the Cardiovascular Health Study (CHS) where Year 6 data were used. Health ABC was a high-functioning cohort at baseline. We chose to use follow-up data to enrich our sample with lower-functioning older adults. Thus, for Health ABC, data from Year 7 were used from Health ABC in order to have a broader range of function (as all participants were nondisabled at enrollment). Data from Year 6 were used from CHS because that was the first visit in which gait speed and self-reported function were available.
Walking Speed
Walking speed was assessed at the participant’s usual pace over 20 m in Health ABC; over 6 m in MrOS, Mr&MsOS Hong Kong, MrOS Sweden, SOF, CHAMP; and over 4.6 m (15 ft) in CHS. In the Johnston County Osteoarthritis Project, walking speed was assessed over 2.4 m (8 ft). Because walking speed is slower over shorter distances than over longer distances due to the acceleration phase when initiating movement, walking speed on the 8-foot course was harmonized to an equivalent speed that would have been observed over 4–6 m using equations previously published by Guralnik et al. (14).
Mobility Limitation
In Health ABC, MrOS, SOF, CHS, MrOS Sweden, and Mr&MsOS Hong Kong participants self-reported difficulty walking short distances outside, either 2–3 blocks or ½ mile. In the CHAMP, participants were queried “are you able to walk half a mile (approx. 1 km) without any help?” In the Johnston County Osteoarthritis Project, the participants were asked “During the past seven days … have you been able to walk outside on flat ground?” Participants with any difficulty or inability to walk these distances were classified as having a prevalent self-reported mobility limitation.
Statistical Analysis
Means ± SD and N (%) for selected characteristics are presented; characteristics across walking speed groups were tested by chi-square for categorical variables and analysis of variance for normally distributed continuous variables; and Kruskal–Wallis test for skewed continuous variables. To identify cut-points(s) in walking speed that most strongly discriminated self-reported mobility limitation, we developed CART models using the rpart package in R (version 3.1.2). Cross-validation was used to “prune” less important splits to prevent overfitting and produce a more parsimonious tree. Cross-validation was performed by randomly partitioning the pooled data into 10 equally sized mutually exclusive data sets (ie, each set excluded 10% of the original pooled data). The tree was then applied to 10 subsamples that contained 90% of the data (ie, 10% of the data was left out of each subsample), and the prediction error from each subsample was calculated. The 10 prediction errors (error sum of squares) were used to calculate the empirical standard error of the prediction error. Following published guidelines (15), the tree was pruned to the most parsimonious tree that was within 1 SE of the tree with the smallest prediction error. For utility in clinical settings, we also aimed to round cut-points to the nearest 0.05 m/s and compare classification against the CART-derived versions. We examined race and ethnicity as a sensitivity analysis in the final CART model. If CART did not select race or ethnicity as a variable of importance, it was subsequently dropped from the final models. We found that adding a variable for being Chinese did not change the nodes identified. We repeated this approach with Black race and found similar results. Race/ethnicity also did not show up in the variable importance list. As such, we did not stratify the results by being a citizen of China, race, or ethnicity.
To quantify the discriminative ability of the identified cut-points, we used logistic regression models to estimate relative odds of mobility limitation based on being classified according to the identified cut-points. No covariates were included in the logistic models as these models were used to quantify the risk represented by the different prevalence values at different walking speeds.
Results
The overall prevalence of self-reported mobility limitation in men was 12.6%; in women, the prevalence of self-reported mobility limitation was more than twice as high (26.4%). Mean ± SD walking speed was 1.17 ± 0.26 m/s in men and 0.94 ± 0.23 m/s in women.
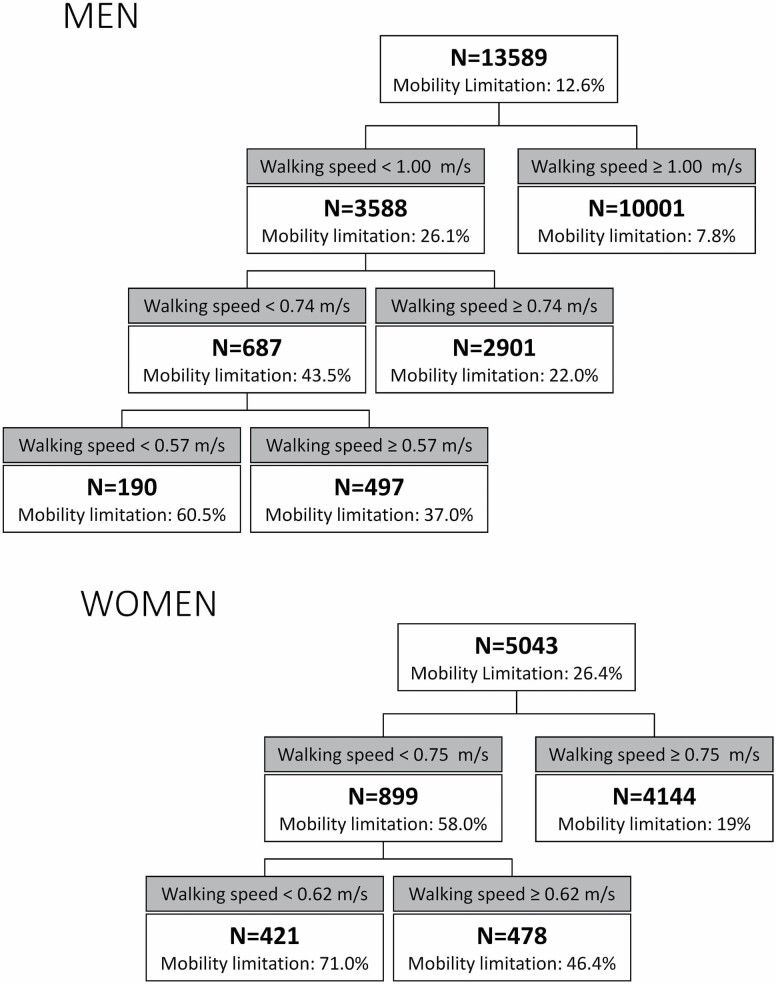
For women, 2 cut-points were identified: the first at 0.75 m/s and a second among those who walked more slowly at 0.62 m/s (Figure 1). We considered 4144 (82.2%) women who walked ≥0.75 m/s as “fast”; 478 women (9.5%) who walked ≥0.62 m/s but <0.75 m/s as “intermediate”; and 421 women (8.3%) who walked <0.62 m/s as “slow.” The prevalence of self-reported mobility limitation was higher in women classified as slow compared to classified as fast (71% vs 19%, p < .001).
Figure 1.
CART results: Classification of men and women by walking speed cut-points that best discriminate the prevalence of self-ported mobility limitation.
For men, 3 cut-points were identified: the first at 1.0 m/s, the second at 0.74 m/s among those who walked more slowly, and the third at 0.57 m/s (Figure 1). The CART models identified 10 001 men (73.6%) who walked ≥1.00 m/s which we classified as “very fast”; 2901 men (21.3%) who walked ≥0.74 m/s but <1.00 m/s who we classified as “fast”; 497 (3.7%) who walked ≥0.57 m/s but <0.74 m/s who we classified as “intermediate”; and 190 (1.4%) who walked <0.57 m/s who we classified as “slow.” As seen with women, the prevalence of self-reported mobility limitation in men was the lowest in those with faster gait speed (7.8% in those considered “very fast”) and the highest in those considered “slow” (60.5%). For parsimony across sexes, we evaluated the effect of classifying men into 3 groups by collapsing the “very fast” and “fast” groups. The resulting group (“very fast or fast”) had 12 902 men (94.9% of men) with a prevalence of self-reported mobility limitation of 11.0%. Those in the slower walking categories were older, had lower grip strength and appendicular lean mass, and higher body mass index (BMI; although the BMI association only reached statistical significance for women, Table 1). Race and self-reported mobility limitation also varied by walking speed category.
Table 1.
Characteristics (N (%) or mean ± SD) of Participants by Walking Speed Categories
| Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | Fast or Very Fast (≥0.74 m/s) | Intermediate (<0.74 to ≥0.57 m/s) | Slow (<0.57 m/s) | p | Fast (≥0.75 m/s) | Intermediate (<0.75 to ≥0.62 m/s) | Slow (<0.62 m/s) | p |
| N (%) | 12 902 (94.9) | 497 (3.7) | 190 (1.4) | 4144 (82.2) | 478 (9.5) | 421 (8.3) | ||
| Age (years) | 74.4 ± 5.3 | 78.3 ± 6.0 | 80.0 ± 5.7 | <.001 | 74.9 ± 5.5 | 77.4 ± 5.4 | 78.7 ± 5.6 | <.001 |
| BMI (kg/m2) | 26.6 ± 3.9 | 26.8 ± 4.6 | 27.1 ± 4.4 | .080 | 25.9 ± 4.8 | 27.6 ± 6.0 | 28.0 ± 6.3 | <.001 |
| Maximum grip strength (kg) | 40.1 ± 8.6 | 32.0 ± 8.0 | 31.1 ± 8.6 | <.001 | 22.6 ± 5.3 | 20.5 ± 5.4 | 20.0 ± 5.6 | <.001 |
| Grip strength/BMI | 1.53 ± 0.35 | 1.21 ± 0.32 | 1.17 ± 0.32 | <.001 | 0.89 ± 0.24 | 0.76 ± 0.22 | 0.74 ± 0.25 | <.001 |
| Appendicular lean mass (ALM), kg | 23.3 ± 3.7 | 21.0 ± 3.6 | 20.9 ± 3.9 | <.001 | 15.3 ± 3.0 | 15.8 ± 3.7 | 16.1 ± 3.8 | <.001 |
| ALM/ht2, kg/m2 | 7.8 ± 1.0 | 7.5 ± 1.0 | 7.4 ± 1.1 | <.001 | 6.3 ± 1 | 6.6 ± 1.2 | 6.7 ± 1.3 | <.001 |
| Race | <.001 | <.001 | ||||||
| White | 10 151 (78.7) | 348 (70.0) | 140 (73.7) | 1594 (38.5) | 156 (32.6) | 140 (33.3) | ||
| Black | 510 (4.0) | 36 (7.2) | 24 (12.6) | 827 (20.0) | 163 (34.1) | 158 (37.5) | ||
| Asian | 2050 (15.9) | 110 (22.1) | 25 (13.2) | 1721 (41.5) | 159 (33.3) | 122 (29.0) | ||
| Other | 191 (1.5) | 3 (0.6) | 1 (0.5) | 2 (0) | 0 (0) | 1 (0.2) | ||
| Walking speed (m/s) | 1.20 ± 0.24 | 0.67 ± 0.04 | 0.49 ± 0.09 | <.001 | 1.02 ± 0.18 | 0.68 ± 0.03 | 0.49 ± 0.10 | N/A* |
| Self-reported mobility limitation | 1414 (11) | 184 (37) | 115 (60.5) | <.001 | 808 (19.5) | 222 (46.4) | 299 (71) | <.001 |
Note: BMI = body mass index.
*p values are not appropriate for this row, as the walking speed values are known to be different by definition.
In logistic models, men and women classified as slow were at least 10 times more likely to report a mobility limitation than those who were classified as fast or very fast (Table 2); and those classified as intermediate were at least 3 times more likely to report a mobility limitation than those who were fast or very fast.
Table 2.
Likelihood (odds ratio, 95% CI) of Mobility Limitation by Category of Walking Speed in Men and Women
| Women | Men | |||
|---|---|---|---|---|
| Group | With derived cut-points* | With rounded cut-points* | With derived cut-points* | With rounded cut-points* |
| Fast or very fast | 1.0 (referent) | 1.0 (referent) | 1.0 (referent) | 1.0 (referent) |
| Intermediate | 3.6 (2.9, 4.4) | 3.9 (3.2, 4.7) | 4.8 (3.9, 5.8) | 4.4 (3.7, 5.3) |
| Slow | 10.1 (8.1, 12.7) | 9.8 (7.8, 12.4) | 12.5 (9.3, 16.8) | 11.2 (8.6, 14.7) |
*Derived cut-points are 0.57 and 0.74 m/s in men and 0.62 and 0.75 m/s in women; rounded cut-points are 0.6 and 0.75 m/s in men and women, respectively.
The prevalence of self-reported mobility limitation was somewhat higher among women than men classified as “slow” or when classified as “intermediate.” Among men and women classified as slow, 71.0% of women and 60.5% of men reported a mobility limitation, while among those classified as intermediate, 46.4% of women and 37.0% of men reported a mobility limitation. Among those classified as “fast” or “very fast,” more women (19.5%) than men (11.0%) reported a mobility limitation.
If the cut-points to define 3 groups in both men and women are rounded to 0.75 and 0.60 m/s, some participants would be differentially classified. For women, no change would be made to the “fast” group, and 36 would be classified as “intermediate” rather than “slow” with the rounded numbers for the cut-points. For men, 69 would be classified as “intermediate” rather than “fast or very fast”; 40 would be classified as “slow” rather than “intermediate” with the rounded numbers for the cut-points. If 2 groups were defined based on a cut-point of 0.8 m/s as suggested by others (13,16), rather than 0.75 m/s as identified herein to define “fast” and “slow,” a number of men and women would be differentially classified. For men, 12 833 (94.4%) walk faster than 0.75 m/s while 12 427 (91.5%) walk faster than 0.80 m/s. For women, 4144 (82.2%) walk faster than 0.75 m/s while 3758 (74.5%) walk faster than 0.80 m/s.
Discussion
Our data-driven approach found that 2 cut-points of approximately 0.60 and 0.75 m/s stratify men and women into groups with vastly different prevalence of self-reported mobility limitation. An additional cut-point of 1.0 m/s was found for men, but not for women. Although the precise cut-point for the lower value of walking speed was slightly different for men and women (0.62 and 0.57, respectively), the rounded cut-points of 0.6 and 0.75 m/s reclassified relatively few participants (about 0.01% of the population or less). The cut-point of 0.75 is fairly different from 0.8 m/s as previously proposed by other groups (4,5). The difference of 0.05 m/s represents a difference of 0.19 SD in men and 0.22 SD in women. Using 0.8 instead of 0.75 would reclassify a fair number of individuals (>5%), especially women.
The utility of walk speed cut-points is multifold. First, it is a standardized and objective measure that is free of environmental and psychosocial factors known to influence self-reported function. Second, evidence-based cut-points help practitioners by categorizing individuals into risk groups for further evaluation and/or to target interventions. CART identified a different number of cut-points in men (3 cut-points) and women (2 cut-points). Highlighting features of the CART method may clarify the reason for this apparent sex discordant finding. CART is not based on a prespecified number of cut-points, and its objective is to optimize discrimination (not to identify a given number of cut-points). We intentionally set these analyses up as a classification problem whereby the algorithm minimizes node “impurity” (ie, makes the nodes as homogenous as possible with regard to the prevalence of the outcome, mobility limitation). The best solution for this problem in men was to identify 3 cut-points but for women, it was to identify 2 cut-points. In other words, for men, the algorithm found that it could improve its objective function (reduce node “impurity”) beyond noise (the cross-validation) by creating another node, but another node was not helpful in this regard for women.
Across men and women, 2 similar cut-points were found (0.6 and 0.75 m/s). The utility of each cut-point depends on its intended use. The cut-point of 0.6 m/s is emerging as one that distinguishes those with poor function. It is rare for community-dwelling older adults to be below this cut-point, as only 1.3% of men and only 8.3% of women were below this level and classified as slow by our analysis. Thus, in situations where the aim is to maximize the sensitivity of walking speed to identify those with poor function then the lower cut-point is likely most appropriate. On the other hand, previously suggested cut-points of 0.8 or 1.0 m/s3 result in a very high prevalence of slowness, particularly in the oldest old. For example, data from the National Health and Nutrition Examination Survey suggest that slowness defined by gait speed <1.0 m/s would be nearly universal in the oldest old, with a prevalence in the United States of 88% in men and 94% in women aged 85 and older (3). This high prevalence suggests that these higher cut-points for slowness would have little impact on risk stratification for adverse events in the oldest old (as everyone would be classified as “high risk”). On the other hand, if the intended use of the cut-point is to discriminate those with excellent function from those with good to poor function, then the higher cut-point of 0.75 m/s (or 1.0 m/s for men) may be useful. In this case, the goal would be to maximize the sensitivity of walking speed to identify those without any functional limitations. We note that the CART model found cut-points that are somewhat arbitrary in that they relate only to the features included in the model—walking speed and mobility limitation—and do not necessarily represent an underlying biological relationship, especially considering the clear log-linear relationship between walking speed and risk of limitation and disability. Thus, while categorization of walking speed will be useful in many situations, investigators should also consider the analysis of walking speed as a continuous variable especially when aiming to elucidate biological or other factors associated with walking speed.
The medical community often categorizes patients into risk groups despite a linear association between a health predictor and outcome. As an example, the association between systolic blood pressure and risk of stroke is extremely linear—yet, the treatment recommendations are based on cut-points. A similar phenomenon exists for glucose, low-density lipoprotein cholesterol, BMI, and bone density on their respective adverse health outcomes. Interestingly, cut-points for these commonly used measures are often not based on an empirical approach as we have performed. Instead, because of their linear associations with health outcomes, such cut-points are generated from consensus agreement among experts in the field. In clinical situations, the utility of these cut-points is not entirely clear, in part because there are no clear treatment pathways for those who walk slowly. However, patients with walking speeds below a lower cut-point of 0.6 m/s might be considered for treatment that carries higher costs and/or side effects (eg, for a yet-to-be-approved pharmacological treatment), whereas patients above the higher cut-point of 0.75 m/s may not have to be counseled about activities to improve fitness. Future work should further establish the clinical utility of these cut-points.
The CART models did not perfectly group individuals into high- versus low-functioning groups—while the prevalence of mobility limitation was much higher in the “slow” group than the “fast” or “very fast” groups, it was not negligible in the “fast”/“very fast” groups: about 11% in men and 19% in women. The reason for the apparent discrepancy for those who walk fast but still report limitation is not entirely clear, but this could be due to pain, endurance, or other factors that affect function over longer distances (~1/4 mile distance for self-reported limitation) versus <20 m distance (for objectively measured walking speed).
These data also reinforce differences between men and women in terms of walking speed and are consistent with previous results from normative databases that consistently demonstrate that women walk more slowly than men (17,18). Also consistent with our results, women are more likely to report mobility limitation than men (19–28), despite having better self-rated health and less multimorbidity than men (28). These differences are unlikely to be due to reporting differences as studies have found that men and women generally report disability accurately (19,22,29,30). Future studies should aim to elucidate the reasons for this consistent sex difference. Categorization of men and women as “slow,” “intermediate,” and “fast or very fast” classifies more women than men as slow; at every level of walking speed, more women than men report mobility limitation. We believe that this approach is correct, as it correctly reflects the additional burden of limitation that women carry when compared with men. However, an alternative approach could have been used to identify different cut-points in walking speed by sex: For example, we could have used other regression techniques to determine the level of walking speed at which the prevalence of mobility limitation reached some prespecified threshold (eg, 10%) for each sex. However, such an approach would have fixed the prevalence of mobility limitation across sexes as equal: If women have more limitations, then cut-points that identify more women as having such limitations will reflect the underlying burden of disease across the whole population.
While these analyses included a very large number of participants, limitations should be noted. Other reports have noted differences in walking speed or mobility complaints by race and ethnicity (9,31–33). Some race and ethnic groups are underrepresented, precluding our ability to perform analysis stratified by these factors. In addition, while some non-US cohorts were included in these analyses, too few international cohorts were available to stratify analyses by geographical location, so we are unable to determine whether race, geography, or local customs influence the associations reported here, and this should be a topic for future analyses. The data were harmonized, but some differences in the wording of the questions about mobility limitation may have influenced reporting of this condition differentially across studies. This study is cross-sectional and longitudinal models (for predicting incident mobility limitation) may define other cut-points. In addition, we used descriptive terms of “very fast,” “fast,” “intermediate,” and “slow” to describe the groups of participants. We note that these terms are relative to one another in the context of older adults participating in our studies. Further gradations in walking speed may exist in extremes of the population, such as master’s athletes who may be a faster group than the “very fast” or disabled but ambulatory individuals living in care facilities who may be much slower than the “slow.” Indeed, a recent analysis suggested that cut-points of 0.35 m/s may optionally differentiate in-hospital walking independence among surgical patients (8). However, other terms, such as “normal,” did not seem appropriate as our population was ambulatory, community-dwelling older adults who were not necessarily representative of underlying populations. Finally, CART is a useful tool to identify cut-points; however, CART only picks one optimum model comprising a cut-point or set of cut-points; other models that were not identified (that could have included more cut-points or cut-points at different levels) may have performed nearly as well as those reported in this article.
In conclusion, in both men and women, the data-driven models identified cut-points in walking speed of approximately 0.60 and 0.75 m/s that best discriminated individuals based on prevalent mobility limitation. These cut-points should be considered when categorized values of walking speed are required, for example, in research for determining eligibility for clinical trials and in clinical settings for determining those in need of follow-up or treatment.
Supplementary Material
Funding
The Sarcopenia Definitions and Outcomes Consortium (SDOC) is supported by the National Institute on Aging (NIA, grant number AG51421), the Foundation for the National Institutes of Health (FNIH, grant numbers CAWT16SARC2 and BHAS16SARC2), and the California Pacific Medical Center Foundation. This research was supported in part by the intramural research program at the NIA.
Conflict of Interest
P.M.C. serves as a consultant for Bioage and had grants to her institution from Abbott and Nestle. S.B. has received grant support for investigator-initiated research from NIA, NINR, NICHD, FNIH, PCORI, Abbvie, Transition Therapeutics, Abbott, Metro International Biotechnology, LLC, and Alivegen. These grants and contracts are managed by the Brigham and Women’s Hospital. He reports receiving consulting fees from AbbVie and OPKO and holding equity interest in FPT, LLC. R.A.F. reports grants from the NIH (NIA) and the USDA, during the conduct of the study; grants, personal fees and others from Axcella Health, other from Inside Tracker, grants and personal fees from Biophytis, grants and personal fees from Astellas, personal fees from Cytokinetics, personal fees from Amazentis, grants and personal fees from Nestle’, personal fees from Glaxo Smith Kline, outside the submitted work. S.B.K is a site PI on a trial of a sarcopenia drug (Biopytis is the company). D.P.K. royalty payments from Wolters Kluwer for contributions to UpToDate chapter on Falls. He has received a stipend from Springer for editor roles on the book, Osteoporosis in Older Persons. He has received consultant payments for serving on a scientific advisory board for Solarea Bio. He has received grant support to his institution from the Dairy Council, Policy Analysis, Inc, and Radius Health. J.M. consulted or served on advisory boards for American Orthopedic Association, Novartis, Pluristem, and Viking. None of these entities provided funding for the current project. A.S. was supported by a career development award from the NIH/NIA (K01 AG057726). All other authors report no conflicts.
Funding support for the individual studies that comprise the pooled data set is gratefully acknowledged:
MrOS (US): The Osteoporotic Fractures in Men (MrOS) Study is supported by National Institutes of Health funding. The following institutes provide support: the National Institute on Aging (NIA), the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Center for Advancing Translational Sciences (NCATS), and NIH Roadmap for Medical Research under the following grant numbers: U01 AG027810, U01 AG042124, U01 AG042139, U01 AG042140, U01 AG042143, U01 AG042145, U01 AG042168, U01 AR066160, and UL1 TR000128. MrOS data are available online: http://mrosdata.sfcc-cpmc.net.
MrOS Hong Kong: MrOS in Hong Kong was supported by a US National Institute of Health R01 Grant AR049439-01A1, the Research Grants Council Earmarked Grant CUHK 4101/02M, and a direct grant for research of The Chinese University of Hong Kong (No. 2041657).
MrOS Sweden: Financial support was received from the Swedish Research Council (2006-3832), the Swedish Foundation for Strategic Research, the ALF/LUA research grant in Gothenburg, the Lundberg Foundation, the Torsten and Ragnar Söderberg’s Foundation, Petrus and Augusta Hedlunds Foundation, the Västra Götaland Foundation, the Göteborg Medical Society and the Novo Nordisk Foundation, the ALF research grant in Lund, Regional foundations in Skane and Österlunds Foundation.
SOF: The Study of Osteoporotic Fractures (SOF) is supported by National Institutes of Health funding. The NIA provides support under the following grant numbers: R01 AG005407, R01 AR35582, R01 AR35583, R01 AR35584, R01 AG005394, R01 AG027574, and R01 AG027576.
Health Aging and Body Composition Study (Health ABC): This study was funded by the National Institutes of Aging. This research was supported by NIA contracts N01AG62101, N01AG62103, and N01AG62106.
Cardiovascular Health Study (CHS): This research was supported by contracts HHSN268201200036C, HHSN268200800007C, HHSN268201800001C, N01HC55222, N01HC85079, N01HC85080, N01HC85081, N01HC85082, N01HC85083, N01HC85086, and grants U01HL080295 and U01HL130114 from the National Heart, Lung, and Blood Institute (NHLBI), with additional contribution from the National Institute of Neurological Disorders and Stroke (NINDS). Additional support was provided by R01AG023629 from the NIA. A full list of principal CHS investigators and institutions can be found at CHS-NHLBI.org.
The Johnston County Osteoarthritis Project is supported in part by cooperative agreements S043, S1734, and S3486 from the Centers for Disease Control and Prevention/Association of Schools of Public Health; the NIAMS Multipurpose Arthritis and Musculoskeletal Disease Center grant 5-P60-AR30701; and the NIAMS Multidisciplinary Clinical Research Center grant 5 P60 AR49465-03.
Concord Health and Ageing in Men Project: CHAMP is funded by the National Health and Medical Research Council (project grant number 301916) and the Ageing and Alzheimer’s Institute.
References
- 1.Studenski S, Perera S, Patel K, et al. . Gait speed and survival in older adults. JAMA. 2011;305(1):50–58. doi: 10.1001/jama.2010.1923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Perera S, Patel KV, Rosano C, et al. . Gait speed predicts incident disability: a pooled analysis. J Gerontol A Biol Sci Med Sci. 2016;71(1):63–71. doi: 10.1093/gerona/glv126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cummings SR, Studenski S, Ferrucci L. A diagnosis of dismobility—giving mobility clinical visibility: a mobility working group recommendation. JAMA. 2014;311(20):2061–2062. doi: 10.1001/jama.2014.3033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Studenski SA, Peters KW, Alley DE, et al. . The FNIH Sarcopenia Project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci. 2014;69(5):547–558. doi: 10.1093/gerona/glu010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. . Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing. 2010;39(4):412–423. doi: 10.1093/ageing/afq034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fielding RA, Vellas B, Evans WJ, et al. . Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. 2011;12(4):249–256. doi: 10.1016/j.jamda.2011.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cesari M, Kritchevsky SB, Penninx BW, et al. . Prognostic value of usual gait speed in well-functioning older people—results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53(10):1675–1680. doi: 10.1111/j.1532-5415.2005.53501.x [DOI] [PubMed] [Google Scholar]
- 8.Graham JE, Fisher SR, Bergés IM, Kuo YF, Ostir GV. Walking speed threshold for classifying walking independence in hospitalized older adults. Phys Ther. 2010;90(11):1591–1597. doi: 10.2522/ptj.20100018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miller ME, Magaziner J, Marsh AP, et al. . Gait speed and mobility disability: revisiting meaningful levels in diverse clinical populations. J Am Geriatr Soc. 2018;66(5):954–961. doi: 10.1111/jgs.15331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fried LP, Tangen CM, Walston J, et al. . Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M156. doi: 10.1093/gerona/56.3.m146 [DOI] [PubMed] [Google Scholar]
- 11.Cawthon PM, Travison TG, Manini TM, et al. . Establishing the link between lean mass and grip strength cut-points with mobility disability and other health outcomes: proceedings of the sarcopenia definition and outcomes consortium conference. J Gerontol A Biol Sci Med Sci. 2020;75:1317–1323. doi: 10.1093/gerona/glz081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cawthon PM, Manini T, Patel SM, et al. . Putative cut-points in sarcopenia components and incident adverse health outcomes: an SDOC analysis. J Am Geriatr Soc. 2020;68(7):1429–1437. doi: 10.1111/jgs.16517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bhasin S, Travison TG, Manini TM, et al. . Sarcopenia definition: the position statements of the sarcopenia definition and outcomes consortium. J Am Geriatr Soc. 2020;68(7):1410–1418. doi: 10.1111/jgs.16372 [DOI] [PubMed] [Google Scholar]
- 14.Guralnik JM, Ferrucci L, Pieper CF, et al. . Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–M231. doi: 10.1093/gerona/55.4.m221 [DOI] [PubMed] [Google Scholar]
- 15.Maindonald J, Braun WJ.. Data Analysis and Graphics Using R: An Example-Based Approach (Cambridge Series in Statistical and Probabilistic Mathematics). 3rd ed. Cambridge University Press; 2010. [Google Scholar]
- 16.Cruz-Jentoft AJ, Bahat G, Bauer J, et al. . Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16–31. doi: 10.1093/ageing/afy169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oberg T, Karsznia A, Oberg K. Basic gait parameters: reference data for normal subjects, 10–79 years of age. J Rehabil Res Dev. 1993;30(2):210–223. doi: 10.1682/jrrd.2003.07.0361 [DOI] [PubMed] [Google Scholar]
- 18.Hollman JH, McDade EM, Petersen RC. Normative spatiotemporal gait parameters in older adults. Gait Posture. 2011;34(1):111–118. doi: 10.1016/j.gaitpost.2011.03.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Merrill SS, Seeman TE, Kasl SV, Berkman LF. Gender differences in the comparison of self-reported disability and performance measures. J Gerontol A Biol Sci Med Sci. 1997;52(1):M19–M26. doi: 10.1093/gerona/52a.1.m19 [DOI] [PubMed] [Google Scholar]
- 20.Strawbridge WJ, Kaplan GA, Camacho T, Cohen RD. The dynamics of disability and functional change in an elderly cohort: results from the Alameda County Study. J Am Geriatr Soc. 1992;40(8):799–806. doi: 10.1111/j.1532-5415.1992.tb01852.x [DOI] [PubMed] [Google Scholar]
- 21.Wheaton FV, Crimmins EM. Female disability disadvantage: a global perspective on sex differences in physical function and disability. Ageing Soc. 2016;36(6):1136–1156. doi: 10.1017/S0144686X15000227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leveille SG, Penninx BW, Melzer D, Izmirlian G, Guralnik JM. Sex differences in the prevalence of mobility disability in old age: the dynamics of incidence, recovery, and mortality. J Gerontol B Psychol Sci Soc Sci. 2000;55(1):S41–S50. doi: 10.1093/geronb/55.1.s41 [DOI] [PubMed] [Google Scholar]
- 23.Zunzunegui MV, Alvarado BE, Guerra R, Gómez JF, Ylli A, Guralnik JM. The mobility gap between older men and women: the embodiment of gender. Arch Gerontol Geriatr. 2015;61(2):140–148. doi: 10.1016/j.archger.2015.06.005 [DOI] [PubMed] [Google Scholar]
- 24.Gill TM, Gahbauer EA, Lin H, Han L, Allore HG. Comparisons between older men and women in the trajectory and burden of disability over the course of nearly 14 years. J Am Med Dir Assoc. 2013;14(4):280–286. doi: 10.1016/j.jamda.2012.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oman D, Reed D, Ferrara A. Do elderly women have more physical disability than men do? Am J Epidemiol. 1999;150(8):834–842. doi: 10.1093/oxfordjournals.aje.a010088 [DOI] [PubMed] [Google Scholar]
- 26.Clark DO, Stump TE, Wolinsky FD. Predictors of onset of and recovery from mobility difficulty among adults aged 51–61 years. Am J Epidemiol. 1998;148(1):63–71. doi: 10.1093/oxfordjournals.aje.a009561 [DOI] [PubMed] [Google Scholar]
- 27.Hardy SE, Allore HG, Guo Z, Gill TM. Explaining the effect of gender on functional transitions in older persons. Gerontology. 2008;54(2):79–86. doi: 10.1159/000115004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arber S, Cooper H. Gender differences in health in later life: the new paradox? Soc Sci Med. 1999;48(1):61–76. doi: 10.1016/s0277-9536(98)00289-5 [DOI] [PubMed] [Google Scholar]
- 29.Leveille SG, Resnick HE, Balfour J. Gender differences in disability: evidence and underlying reasons. Aging (Milano). 2000;12(2):106–112. doi: 10.1007/BF03339897 [DOI] [PubMed] [Google Scholar]
- 30.Daltroy LH, Larson MG, Eaton HM, Phillips CB, Liang MH. Discrepancies between self-reported and observed physical function in the elderly: the influence of response shift and other factors. Soc Sci Med. 1999;48(11):1549–1561. doi: 10.1016/s0277-9536(99)00048-9 [DOI] [PubMed] [Google Scholar]
- 31.Capistrant BD, Glymour MM, Berkman LF. Assessing mobility difficulties for cross-national comparisons: results from the World Health Organization Study on Global AGEing and Adult Health. J Am Geriatr Soc. 2014;62(2):329–335. doi: 10.1111/jgs.12633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boulifard DA, Ayers E, Verghese J. Home-based gait speed assessment: normative data and racial/ethnic correlates among older adults. J Am Med Dir Assoc. 2019;20(10):1224–1229. doi: 10.1016/j.jamda.2019.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Blanco I, Verghese J, Lipton RB, Putterman C, Derby CA. Racial differences in gait velocity in an urban elderly cohort. J Am Geriatr Soc. 2012;60(5):922–926. doi: 10.1111/j.1532-5415.2012.03927.x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.