Abstract
Background
older people with cancer are at risk of complex and fluctuating health problems, but little is known about the extent to which their well-being changes in the last years of life.
Objective
to examine changes in physical, psychological and social well-being in the last 5 years of life of older people with cancer.
Design
prospective cohort study.
Setting
Belgium, the Netherlands.
Participants
people with a new primary diagnosis of breast, prostate, lung or gastrointestinal cancer, aged ≥70 years, life expectancy >6 months, were recruited from nine hospitals. We analysed data of deceased patients.
Methods
data were collected from participants around diagnosis, and after 6 months, 1, 3 and 5 years through structured questionnaires administered through interviews or as self-report. Outcomes were physical, emotional, social, role functioning (EORTC QLQ-C30), depressive symptoms (GDS-15), emotional and social loneliness (Loneliness Scale). We conducted linear mixed model analyses.
Results
analysing 225 assessments from 107 deceased participants (assessments took place between 1,813 and 5 days before death), mean age at baseline 77 years (standard deviation: 5.2), we found statistically significant deterioration in physical functioning (b = 0,016 [95%confidence interval 0.009–0.023]), depressive symptoms (b = −0,001 [−0.002 to 0.000]) and role functioning (b = 0.014 [0.004–0.024]). Changes over time in emotional and social functioning and in social and emotional loneliness were smaller and statistically non-significant.
Conclusions
care towards the end of life for older people with cancer needs to put their social and psychological well-being at the centre, alongside physical needs. Future research should focus on understanding inter-individual variation in trajectories.
Keywords: longitudinal study, prospective cohort study, older people with cancer, well-being, end of life
Key points
Physical functioning, role functioning and depressive symptoms deteriorate over the last 5 years of life of older people with cancer.
End-of-life care needs to put their social and psychological well-being at the centre, alongside physical needs.
Future research should focus on understanding inter-individual variation in trajectories.
Introduction
Global annual cancer-related deaths are projected to reach 11.5 million in 2030 [1], with the increase disproportionately affecting older people [2]. As they near the end of life, many older people with cancer experience important fluctuations in their health that can affect their physical, psychological and social well-being. These problems are often caused by the cumulative effects of cancer, cancer treatment and other chronic conditions as well as social problems for which age is a risk factor [3–5]. As there are very few longitudinal studies on the end of life, little is known about changes in the well-being of older people with cancer as they near death. The available longitudinal data mostly concern physical decline [6–8] but largely neglect psychological and social well-being, even though these are key domains of well-being towards the end of life that also interact with physical health [9–11]. Better knowledge of these changes could inform anticipatory care for individual patients [12] as well as support public health policy-making and resource planning for health and social care [6]. We studied to what extent physical, psychological and social well-being change in the last 5 years of life of older people with cancer.
Method
Study design and population
We analysed data of an existing prospective cohort study in Belgium and the Netherlands that was set up to study the well-being of older people with cancer (KLIMOP study) [13]. We selected participants aged 70 years and over at baseline, who had died by October 2019 and whose date of death we were able to ascertain (communicated by the family to the researchers or identified in public obituaries). We included assessments that had taken place within the last 5 years of the patient’s life. The KLIMOP study included patients who had a new primary diagnosis of breast, prostate, lung or gastrointestinal cancer (i.e. most frequently occurring types); a life expectancy of >6 months as judged by the attending physician; a thorough command of the Dutch language and if the first interview could take place within 3 months after diagnosis. The KLIMOP study excluded patients with a formal diagnosis of dementia, a previous diagnosis of invasive cancer and people too ill to participate in data collection. Recruitment took place at nine hospitals in Belgium and the Netherlands from June 2010 until October 2014, with the last follow-up completed in 2019. The KLIMOP study protocol has been approved by the Ethics Committee of UZ/KU Leuven and by the Medical Ethics Committee of Maastricht University Medical Centre. All data were collected anonymously following informed consent, and participation was voluntary.
Data collection and measurements
Data were collected upon inclusion (baseline) and 6-month, 1-, 3- and 5-year follow-up periods through structured questionnaires administered in personal interviews or as self-report. Physical well-being was assessed through the ‘physical functioning’ subscale of the quality of life questionnaire of the European Organisation for Research and Treatment of Cancer (EORTC QLQ-C30; five items) [14]. Psychological well-being was assessed through three outcomes: emotional functioning, measured using EORTC QLQ-C30 (four items, feeling tense, worrying, feeling irritable, feeling depressed); depressive symptoms, measured using the 15-item Geriatric Depression Scale (GDS-15; higher scores indicating higher symptom burden) [15] and social and emotional loneliness assessed using the Loneliness Scale (11 items, higher scores indicating higher levels of loneliness) [16]. Social well-being was assessed through two outcomes: the social functioning (i.e. physical condition or medical treatment interfering with individual’s family life and social activities) and role functioning (i.e. being limited in doing work or other daily activities or in pursuing hobbies or other leisure time activities) subscales of the EORTC QLQ-C30 (two items per subscale). Higher scores on the EORTC QLQ-C30 subscales indicated better functioning [17]. Sociodemographic data and co-morbidities were assessed at baseline, through medical records and patient interviews.
Analysis
To determine changes in physical, psychological and social well-being, we conducted one linear mixed model analysis per dependent variable, with number of days before death as independent variable. All models were estimated with random intercepts and, if model convergence allowed, also with random slopes for days before death. Linear mixed models handle missing data through maximum likelihood estimation. Plots were created in R; linear mixed model analyses were conducted in SPSS v26.
Results
Sample
We identified 110 deceased people with cancer whose date of death we could establish. We excluded three patients whose five assessments all occurred >5 years before death. The remaining 107 participants provided a total of 225 assessments, ranging from 1,813 to 5 days before death (Supplementary Figure S1).
Mean age at baseline was 77 (standard deviation 5.2), and half (49.5%) of participants were female. Of the 107 patients, 68.2% lived with family, 25.2% lived alone, 5.6% in a nursing/care home and 0.9% in another location. Fifty-nine percent lived together with the person who provided most care to them. In total, 11 and 14% had co-morbid heart failure and chronic lung disease, respectively. Missing data did not exceed 6.5% on any variable.
Changes in physical, psychological and social well-being towards the end of life
Among older people with cancer, physical functioning (regression coefficient b for change per day: 0.016 [95% confidence interval, CI, 0.009–0.023]; P < 0.001) and role functioning (b = 0.014 [95%CI 0.004–0,024]; P = 0.009) significantly declined towards death and depressive symptoms increased (b = −0.001 [95%CI −0.002 to 0.000]; P = 0.017) (Table 1). There were small and statistically non-significant changes over time in emotional and social functioning and in social and emotional loneliness. Figure 1 visualises the trajectories of physical and role functioning and depressive symptoms. Statistically significant random effects in the linear mixed model analysis for social functioning indicated inter-individual variation in the extent to which social functioning changed towards the end of life (slope variance: b = 0.000 [95%CI 0.000–0.001], P = 0.01; intercept–slope covariance: b = −0.53 [95%CI −0.89 to −0.16]; P = 0.004) (Supplementary Table S1). The slope variance indicates variation in trajectories between individuals; the negative intercept–slope covariance indicates that a higher initial score is associated with a more rapid decrease.
Table 1 .
Changes per day before death in physical, psychological and social well-being in older people with cancer (N = 107; 225 assessments)a
| Well-being constructs | Coefficient b (95% CI) for change per day before deathb | P-value |
|---|---|---|
| Physical well-being | ||
| Physical functioning (scale 0–100) | 0.016 (0.009–0.023) | <0.001 |
| Psychological well-being | ||
| Emotional functioning (scale 0–100) | −0.002 (−0.007 to 0.004) | 0.523 |
| Depressive symptoms (scale 0–15) | −0.001 (−0.002 to 0.000) | 0.017 |
| Social lonelinessc (scale 0–11) | 0.00 (0.00–0,00) | 0.261 |
| Emotional lonelinessc (scale–11) | 0.00 (0.00–0.00) | 0.233 |
| Social well-being | ||
| Role functioning (scale 0–100) | 0.014 (0.004–0.024) | 0.009 |
| Social functioning (scale 0–100) | 0.005 (−0.003 to 0.013) | 0.210 |
aLinear mixed models with days before death as independent variable and random effects for individual. Full model estimates, including intercepts and random variance, are presented in Supplementary Table S1.
bPositive b coefficients indicate lower values in the well-being construct as death approaches (fewer days); negative values indicate higher values as death approaches (fewer days).
cb coefficient is very small because the Loneliness Scales have a relatively small range, from 0 to 11, and the coefficient captures the change per day.
Figure 1 .
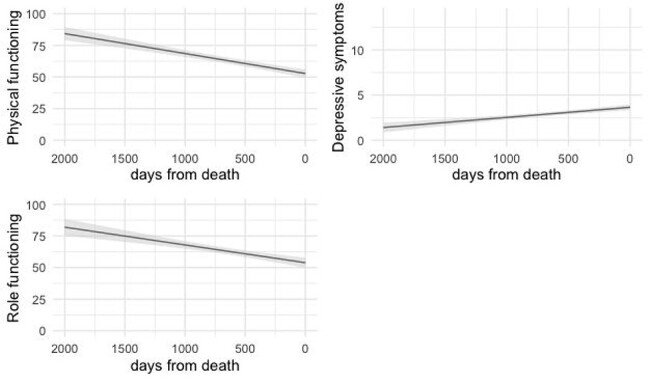
Changes over the last 5 years of life in physical functioning, role functioning and depressive symptoms among older people with cancer (N = 107; 225 assessments), based on predictions of unconditional linear mixed model analyses with number of days before death as independent variable and random intercept for individual.
Discussion
This longitudinal study of the last 5 years of life of older people with cancer found statistically significant deterioration in the physical, psychological and social domains. Specifically, physical functioning and role functioning decreased and depressive symptoms increased. While there were no statistically significant changes in social functioning towards the end of life, we found that social functioning trajectories varied significantly between individuals.
Concluding from these data, care towards the end of life for older people with cancer needs to put social and psychological well-being at the centre, alongside physical needs. Importantly, within the social domain, attention should be paid to deteriorations in role functioning and differing social functioning trajectories between individuals. This finding is an important addition to existing research on the social domain towards the end of life, which has focused mainly on social support, including structural and functional indicators thereof, such as marital status and hours of family care received [18, 19] and on caregiver burden [20, 21], but has largely neglected people’s perceptions of their social connections and activities. Yet such ‘qualitative’ aspects of social connection were found to be important determinants of health outcomes [9, 22]. Several outcomes, all in the psychological well-being domain (i.e. emotional functioning, social and emotional loneliness), did not show large changes over time. This partly corresponds to findings from other populations showing that loneliness, on average, does not change to a great extent over time [23, 24]. However, it is also possible that individual patients experience fluctuations in these outcomes that are not visible in assessments that are 2 years apart. This highlights the need for longitudinal studies on the end of life with larger samples and shorter assessment intervals that balance a higher temporal resolution with limited patient burden and that can examine variation in trajectories between individuals. So far, such work has been limited to the physical domain [6].
This study has several limitations, related to the KLIMOP study having a different primary aim [13]. It excluded patients with a life expectancy below 6 months at diagnosis (baseline) and those with a formal dementia diagnosis. Our findings may therefore not be generalisable to patients whose health deteriorates very quickly and may not capture the possibly unique changes in psychological and social well-being of older people with cancer who additionally face deterioration in cognitive abilities due to dementia. The prevalence of co-morbid cancer and dementia is not clear, which makes it difficult to estimate the impact of this exclusion on our findings [25]. Future longitudinal studies should seek to develop data collection methods that allow involving people with dementia for as long as possible. Our sample size was not very large as we included the subset of KLIMOP participants who had died. Nevertheless, we obtained a good distribution of measurements over the last 5 years of life (Supplementary Figure S1) and captured important changes in well-being. As is common in longitudinal ageing studies, there were losses to follow-up, most likely due to participants’ poor health [26, 27]. While we still included assessments of participants who died after dropping out of the study, measurements close to death from those who were in very poor health may be underrepresented.
Supplementary Material
Acknowledgements
We thank all patients, physicians and nurses for their participation in this study.
Contributor Information
Lara Pivodic, Vrije Universiteit Brussel (VUB) & Ghent University, End-of-Life Care Research Group, Brussels, Belgium; Vrije Universiteit Brussel (VUB), Department of Family Medicine and Chronic Care, Brussels, Belgium.
Tine De Burghgraeve, Department of Public Health and Primary Care, Academic Center of General Practice, KU Leuven, Leuven, Belgium.
Jos Twisk, Department of Epidemiology and Data Science, Amsterdam University Medical Center, Amsterdam, The Netherlands.
Marjan van den Akker, Department of Public Health and Primary Care, Academic Center of General Practice, KU Leuven, Leuven, Belgium; Institute of General Practice, Goethe University, Frankfurt am Main, Germany; Department of Family Medicine, Care and Public Health Research Institute, Maastricht University, Maastricht, The Netherlands.
Frank Buntinx, Department of Public Health and Primary Care, Academic Center of General Practice, KU Leuven, Leuven, Belgium; Department of Family Medicine, Care and Public Health Research Institute, Maastricht University, Maastricht, The Netherlands.
Lieve Van den Block, Vrije Universiteit Brussel (VUB) & Ghent University, End-of-Life Care Research Group, Brussels, Belgium; Vrije Universiteit Brussel (VUB), Department of Family Medicine and Chronic Care, Brussels, Belgium.
Declaration of Conflicts of Interest
None.
Funding
The KLIMOP study was supported by Kom Op Tegen Kanker (10482); European Union/Interreg IV Grensregio Vlaanderen—Nederland (IVA-VLANED-3.46). The present work was supported by a Postdoctoral Fellowship of the Research Foundation-Flanders (FWO) to L.P.
References
- 1.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006; 3: e442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lichtman SM, Sloan M, Cancer K, Jacobsen PB. Geriatric oncology: an overview. J Clin Oncol 2014; 32: 28–30. [PubMed] [Google Scholar]
- 3.Handforth C, Clegg A, Young Cet al. The prevalence and outcomes of frailty in older cancer patients: a systematic review. Ann Oncol 2015; 26: 1091–101. [DOI] [PubMed] [Google Scholar]
- 4.Naeim A, Aapro M, Subbarao R, Balducci L. Supportive care considerations for older adults with cancer. J Clin Oncol 2014; 32: 2627–34. [DOI] [PubMed] [Google Scholar]
- 5.Puts M, Strohschein F, Oldenmenger Wet al. Position statement on oncology and cancer nursing care for older adults with cancer and their caregivers of the International Society of Geriatric Oncology Nursing and Allied Health Interest Group, the Canadian Association of Nurses in Oncology & Aging Sp. J Geriatr Oncol 2021. doi: 10.1016/j.jgo.2021.03.010. [DOI] [PubMed] [Google Scholar]
- 6.Gill TM, Gahbauer EA, Han L, Allore HG. Trajectories of disability in the last year of life. N Engl J Med 2010; 362: 1173–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lunney JR, Lynn J, Foley DJ, Lipson S, Guralnik JM. Patters of functional decline at the end of life. JAMA 2003; 289: 2387–92. [DOI] [PubMed] [Google Scholar]
- 8.Tang ST, Liu LN, Lin KCet al. Trajectories of the multidimensional dying experience for terminally ill cancer patients. J Pain Symptom Manage 2014; 48: 863–74. [DOI] [PubMed] [Google Scholar]
- 9.Holt-Lunstad J. Why social relationships are important for physical health: a systems approach to understanding and modifying risk. Annu Rev Psychol 2018; 69: 437–58. [DOI] [PubMed] [Google Scholar]
- 10.Gerstorf D, Hoppmann CA, Löckenhoff CEet al. Terminal decline in well-being: the role of social orientation. Psychol Aging 2016; 31: 149–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Siddall PJ, Physical MLRD. Psychological/psychiatric, social, and spiritual problems and symptoms. In: Mac Leod RD, Block L, eds. Textbook of Palliative Care. Cham, Switzerland: Springer, 2019; 133–48. [Google Scholar]
- 12.Vliet L, Antunes B, Higginson IJ. Symptoms and trajectories experienced by older people approaching and at the end of life: implications for care. In: Block L, Albers G, Martins Pereira S, Onwuteaka-Philipsen B, Pasman R, Deliens L, eds. Palliative Care for Older People: A Public Health Perspective. Oxford: Oxford University Press, 2015. [Google Scholar]
- 13.Deckx L, Abbema D, Nelissen Ket al. Study protocol of KLIMOP: a cohort study on the wellbeing of older cancer patients in Belgium and the Netherlands. BMC Public Health 2011; 11: 825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aaronson NK, Ahmedzai S, Bergman Bet al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 1993; 85: 365–76. [DOI] [PubMed] [Google Scholar]
- 15.Yesavage JA, Brink TL, Rose TLet al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 1982; 17: 37–49. [DOI] [PubMed] [Google Scholar]
- 16.De Jong Gierveld J, Van Tilburg T. The De Jong Gierveld short scales for emotional and social loneliness: tested on data from 7 countries in the UN generations and gender surveys. Eur J Ageing 2010; 7: 121–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fayers P, Aaronson NK, Bjordal K, Groenvold M, Curran D, Bottomley AEORTC. QLQ-C30 Scoring Manual. European Organisation for Research and Treatment of. Cancer 2001. [Google Scholar]
- 18.Valtorta N, Hanratty B. Loneliness, isolation and the health of older adults: do we need a new research agenda? J R Soc Med Suppl 2012; 105: 518–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mohd TAMT, Yunus RM, Hairi F, Hairi NN, Choo WY. Social support and depression among community dwelling older adults in Asia: a systematic review. BMJ Open 2019; 9. https://pubmed.ncbi.nlm.nih.gov/31320348/(24 July 2020, date last accessed). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.DiGiacomo M, Kochovska S, Cahill P, Virdun C, Philips J. Family-focused care span. In: Mac Leod R, Van den Block L, eds. Textbook of Palliative Care. Cham, Switzerland: Springer, 2019. [Google Scholar]
- 21.Grande G, Ewing G. Informal/family caregivers. In: Mac Leod R, Block L, eds. Textbook of Palliative Care. Cham, Switzerland: Springer, 2019; 1–19. [Google Scholar]
- 22.Jetten J, Haslam SA, Cruwys T, Greenaway KH, Haslam C, Steffens NK. Advancing the social identity approach to health and well-being: progressing the social cure research agenda. Eur J Soc Psychol 2017; 47: 789–802. [Google Scholar]
- 23.Smith TO, Dainty JR, Macgregor A. Trajectory of social isolation following hip fracture: an analysis of the English Longitudinal Study of Ageing (ELSA) cohort. Age Ageing 2018; 47: 107–12. [DOI] [PubMed] [Google Scholar]
- 24.Mund M, Freuding MM, Möbius K, Horn N, Neyer FJ. The stability and change of loneliness across the life span: a meta-analysis of longitudinal studies. Pers Soc Psychol Rev 2020; 24: 24–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McWilliams L, Farrell C, Grande G, Keady J, Swarbrick C, Yorke J. A systematic review of the prevalence of comorbid cancer and dementia and its implications for cancer-related care. Aging Ment Health 2018; 22: 1254–71. [DOI] [PubMed] [Google Scholar]
- 26.Deckx L, Van Abbema DL, Van Den Akker Met al. A cohort study on the evolution of psychosocial problems in older patients with breast or colorectal cancer: comparison with younger cancer patients and older primary care patients without cancer. BMC Geriatr 2015; 15: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jacobsen E, Ran X, Liu A, Chang CCH, Ganguli M. Predictors of attrition in a longitudinal population-based study of aging. Int Psychogeriatr 2020; 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


