Abstract
Background
sarcopenia registries are a potential method to meet the challenge of recruitment to sarcopenia trials. We tested the feasibility of setting up a UK sarcopenia registry, the feasibility of recruitment methods and sought to characterise the pilot registry population.
Methods
six diverse UK sites took part, with potential participants aged 65 and over approached via mailshots from local primary care practices. Telephone pre-screening using the SARC-F score was followed by in-person screening and baseline visit. Co-morbidities, medications, grip strength, Short Physical Performance Battery, bioimpedance analysis, Geriatric Depression Score, Montreal Cognitive Assessment, Sarcopenia Quality of Life score were performed and permission sought for future recontact. Descriptive statistics for recruitment rates and baseline measures were generated; an embedded randomised trial examined the effect of a University logo on the primary care mailshot on recruitment rates.
Results
sixteen practices contributed a total of 3,508 letters. In total, 428 replies were received (12% response rate); 380 underwent telephone pre-screening of whom 215 (57%) were eligible to attend a screening visit; 150 participants were recruited (40% of those pre-screened) with 147 contributing baseline data. No significant difference was seen in response rates between mailshots with and without the logo (between-group difference 1.1% [95% confidence interval −1.0% to 3.4%], P = 0.31). The mean age of enrollees was 78 years; 72 (49%) were women. In total, 138/147 (94%) had probable sarcopenia on European Working Group on Sarcopenia 2019 criteria and 145/147 (98%) agreed to be recontacted about future studies.
Conclusion
recruitment to a multisite UK sarcopenia registry is feasible, with high levels of consent for recontact.
Keywords: sarcopenia, older people, recruitment, registry
Key Points
Recruiting to sarcopenia studies is challenging; registries have proved to be useful for other underserved patient groups.
We successfully piloted a UK sarcopenia registry and recruitment network with efficient recruitment from primary care.
Over 90% of registrants fulfilled the EWGSOP 2019 criteria for probable sarcopenia.
In total, 98% of participants agreed to be recontacted for future clinical studies.
Introduction
Sarcopenia, the loss of muscle strength and mass [1], is an important health problem for many older people. It is a major underlying cause of falls, impairment in activities of daily living and the need for care and is a significant contributor to hospitalisation, increased length of stay and earlier death [2, 3]. Resistance training is the only intervention with good evidence for the treatment of sarcopenia [4], but not all older people are able to or willing to undertake resistance training. Our understanding of the pathophysiology of sarcopenia is advancing rapidly, with multiple lines of therapeutic enquiry [5], and there is therefore a pressing need to conduct clinical trials to test potential interventions to prevent and treat sarcopenia [6].
Undertaking clinical trials for sarcopenia presents multiple challenges. The diagnosis is not commonly made in clinical practice in part due to the need to measure muscle mass and muscle strength [7, 8]. Many clinical sites do not have easy access to equipment (for instance bioimpedance or whole-body dual-energy X-ray absorptiometry) within the clinical environment to enable the diagnosis to be made. Even when the diagnosis is made it is often not systematically recorded in searchable electronic health records or databases. Finding participants with sarcopenia for clinical trials is therefore challenging and often requires screening large numbers of potential participants in order to identify those with sarcopenia. Previous trials have found recruitment of patients with sarcopenia to be difficult and have often either used a more relaxed definition of sarcopenia than that stipulated in current guidelines [9, 10] or have failed to reach their recruitment targets [11]. While many hospital inpatients have sarcopenia, many are too unwell or too frail to take part in trials.
Disease registries provide one solution to this challenge. Registries have been used successfully in other long-term conditions such as bronchiectasis and rare neuromuscular conditions [12, 13]. They allow a pool of eligible participants to be recruited and identified over an extended period across multiple sites even when a trial is not active. Signing up to a registry can include consent to recontact participants when a suitable trial becomes available. Because participants are pre-screened with phenotypic data already collected, the process of selecting participants for a given clinical trial can be much more rapid and efficient. Although plans have been established for a sarcopenia registry in Europe [14], no registry currently exists in the United Kingdom. The aim of this project was therefore to test recruitment processes for a UK sarcopenia registry and to characterise those willing to participate in such a registry.
Methods
Study population
The SarcNet registry pilot study was designed as an observational study with longitudinal follow-up. The target population was people aged 65 and over with self-reported impairment in physical function. The study Sponsor was Newcastle University, and the study was approved by the North East—Tyne and Wear South NHS Research Ethics Committee (reference 18/NE/0314). Written informed consent was obtained from all participants.
Recruitment strategy
Six hospital sites were selected to give geographical and demographic contrast in coverage. Sites were selected to cover major cities versus smaller population centres, areas with high versus low ethnic diversity and north versus south of England. Participants were recruited from primary care organisations (General Practices) located near to each recruiting centre. Primary care practices willing to take part screened their practice lists to identify potentially eligible participants aged 65 and over, supported by the National Institute for Healthcare Research Primary Care Research Network. A clinical member of staff at the primary care practice then screened the generated lists to remove the name of any individual who they deemed it inappropriate to approach; criteria suggested by the study team for this were patients approaching the end of life and those who had previously stated a wish not to engage with research. Invitations were mailed to potential participants on behalf of participating primary care practices using the DocMail mailshot system (CFH Docmail, Radstock UK). DocMail allows documents to be uploaded by the research team to a secure website, combined with names and addresses uploaded by primary care practices, with automated printing, packaging and postage of the information packs to recipients. Reply slips were returned via a business reply mail service to the central research team in Newcastle.
Screening and eligibility
Positive responses were sent to the relevant local research team, who then contacted participants via telephone. At this initial telephone pre-screening call, a brief series of questions including date of birth, the presence of a pacemaker or defibrillator (a contraindication to bioimpedance measurement) and the five-question SARC-F sarcopenia screening score [15] were asked to assess eligibility. Participants had to score 3 or more (out of 10) on the SARC-F questionnaire at pre-screening; this threshold was selected to ensure that the enrolled population had a substantial degree of functional impairment. Eligible participants who still expressed interest were then sent the full-study information sheet by the research team and were invited to a combined in-person screening/baseline visit. This took place in a secondary care clinic, research facility or, if the participant chose, in their own home. Exclusion criteria assessed at the screening visit were life expectancy of <6 months in the judgement of the local investigator, participation in an interventional study within the last 30 days, presence of a permanent pacemaker with an atrial sensing lead or presence of an implantable cardioverter–defibrillator (both contraindications to bioimpedance testing), peripheral oedema present above knee level or body temperature >38°C at the baseline visit (both likely to affect bioimpedance accuracy).
Measures collected
Hand grip strength was measured using a Jamar hydraulic dynamometer (Lafayette Instrument Company, USA); three measurements were recorded on each hand and the maximum used for analysis [16]. Appendicular lean muscle mass was assessed using the Akern 101 bioimpedance system (Akern SRL, Pontassieve, Italy); the Sergi equation was used to derive appendicular lean mass [17]. The Short Physical Performance Battery (SPPB) was conducted, comprising tandem and semi-tandem balance, five times sit to stand and gait speed measured over a 4-m course [18]. Reasons for not completing physical performance measures and bioimpedance were collected (unable, declined or technical problem). The Sarcopenia Quality of Life (SarQoL) questionnaire was administered to assess quality of life [19]. Cognition was assessed using the Montreal Cognitive Assessment (MoCA) [20] and depressive symptoms using the 15-point geriatric depression score [21]. Height, weight, medication use, medical history and the most recent blood results from routine clinical practice in the last 12 months were recorded.
Embedded trial of intervention to boost mailshot response rate
As part of SarcNet, we conducted an embedded randomised controlled trial of a simple intervention that aimed to boost mailshot response rates. Although mailshots provide a cost-effective way to reach large numbers of potentially eligible participants, response rates are often low, with many recipients not even opening the letter. Previous studies have tested whether envelope colour or inclusion of a pen increases response rates to trial invitations, but the effect of including the logo of a trusted provider (e.g. a primary care practice, hospital or University) on the mailshot envelope (to signal that the envelope is unlikely to be junk mail) has not previously been tested in a randomised trial [22, 23]. The intervention we chose was the addition of the Newcastle University logo (as study Sponsor) to the outside envelope containing study information that was mailed to potential participants. The control arm received the same envelope but without any logo on the front. The internal content of all envelopes was identical. Randomisation was performed at the level of individual mail shots (i.e. all letters in a single mailshot either had or did not have the logo added) and was stratified by centre and by primary care practice. Randomisation codes were generated by an individual not otherwise associated with the trial; participants and investigators were, however, not blinded to intervention allocation.
Statistical analysis
All statistical analyses were conducted using SPSS v24 (IBM, New York). A two-sided P-value of <0.05 was taken as significant for all analyses. Descriptive statistics were generated for baseline characteristics of the enrolled population, along with descriptive characteristics for each stage of the recruitment process. For the embedded randomised controlled trial, the primary outcome (the proportion of letters generating a positive reply [mail slip or telephone contact] was compared using Pearson’s chi-squared test with 95% confidence intervals (CIs). Baseline measures of physical performance were correlated with baseline age, quality of life, selected blood test results, medication number and number of conditions, SARC-F score and muscle mass. Pearson’s correlations were used where both variables were normally distributed; Spearman’s correlation was used where one or both variables were not normally distributed.
Results
Recruitment strategy
Six recruitment sites were activated during the pilot project—Gateshead, Lewisham, Exeter, Bradford, Leeds and Solent. In total, 20 mailshots were sent out from 16 primary care practices; the size of mailshot varied from 35 to 313. A total of 3,508 letters were mailed out. In total, 428 replies were received (12% response rate); 380 underwent telephone prescreening of whom 215 (57%) were eligible to attend a screening visit; 150 participants were recruited (40% of those undergoing telephone prescreen). Details of response rates, telephone pre-screening pass rates and enrolment rates at each of the six sites are given in Table 1. Recruitment took place between July 2019 and March 2020, when activity was stopped due to restrictions on research activity imposed as part of the COVID-19 pandemic response in the United Kingdom. To minimise practice workload and to preserve confidentiality, practices did not collect, share or report information on the age or sex of patients included in the mailshots.
Table 1 .
Recruitment numbers by site
| Gateshead (3 practices) | Lewisham (1 practice) | Exeter (3 practices) | Bradford (3 practices) | Leeds (3 practices) | Solent (3 practices) | Total | |
|---|---|---|---|---|---|---|---|
| Letters sent | 526 | 48 | 700 | 859 | 560 | 815 | 3,508 |
| Positive responses (% of total letters sent) | 93 (17.7) | 11 (22.9) | 153 (21.9) | 39 (4.5) | 50 (8.9) | 82 (10.1) | 428 (12.2) |
| Telephone screened | 92 (1 unable to contact) | 6 (unable to contact 5) | 149 (unable to contact 4) | 22 (3 unable to contact; 14 not contacted due to COVID) | 38 (2 declined after finding out more about study; 10 not contacted due to COVID) | 73 (4 unable to contact; 2 unable to communicate by phone; 2 declined prior to phone screen; 1 due to COVID) | 380 |
| Eligible to progress to baseline visit (% of those undergoing telephone screen) | 66 (71.7) (26 failed screen) | 3 (50.0) (3 failed screen) | 66 (44.3) (83 failed screen) | 20 (90.9) (2 failed screen) | 26 (68.4) (12 failed screen) | 34 (46.6) (39 failed screen) | 215 (56.6) |
| Consented to enter the study (% of those undergoing telephone screen) | 46 (52.9) (15 declined to progress; 5 unable to progress due to COVID) | 0 (0) (3 declined to progress) | 49 (32.9) (17 declined) | 18 (81.8) (2 declined) | 15 (39.5) (11 unable to progress due to COVID) | 22 (30.1) (5 unable to progress due to COVID; 7 declined due to illness) | 150 (39.5) |
Embedded trial
The CONsolidated Standards Of Reporting Trials (CONSORT) diagram for the embedded randomised controlled trial of using the Newcastle University logo on the mailshot envelope is shown in Figure 1. No significant difference was seen in positive response rates between mailshots with the logo (180/1399 [12.9%]) and those without the logo (248/2109 [11.8%]). The between group difference in response rates was 1.1% (95%CI −1.0 to 3.4%, P = 0.31).
Figure 1 .
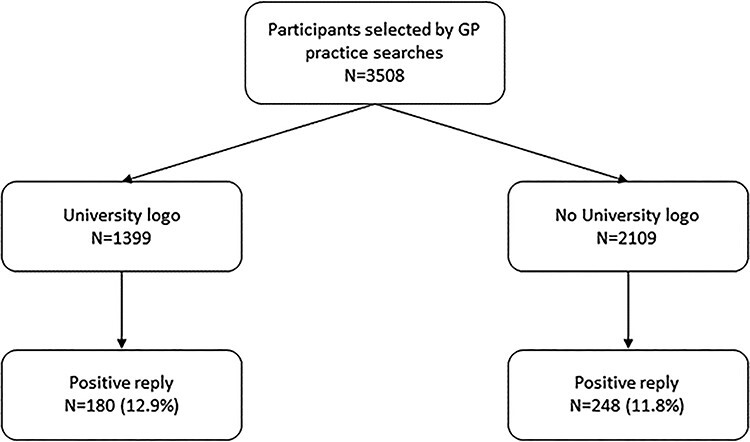
CONSORT flow diagram for recruitment into embedded trial.
Baseline data
Three participants of the 150 enrolled did not complete baseline assessment; two due to illness and one due to the onset of the COVID-19 pandemic stopping non-COVID research. Baseline details for the population contributing baseline data (n = 147) are given in Table 2. In total, 73 (49%) elected to have the baseline visit conducted in their own home. The majority of participants had significantly impaired physical function, with low walk speed, low SPPB scores, impaired sit to stand scores and weak grip strength. The proportion of participants with low muscle mass according to the European Working Group on Sarcopenia in Older People (EWGSOP) 2019 cut-offs differed greatly depending on body mass index (BMI); for those with BMI <18.5 kg/m2, 1 of 1 (100%) had low muscle mass; 16/23 (70%) of those with BMI 18.5–24.9 kg/m2 had low muscle mass, as did 15/52 (29%) of those with BMI 25.0–29.9 kg/m2. The largest group was of those with BMI >30 kg/m2), of whom 0/71 (0%) had a low muscle mass.
Table 2 .
Details for participants undergoing baseline assessment (n = 147)
| Mean age (years) (SD) | 77.6 (7.3) | |
| Female sex (%) | 72 (49) | |
| Max handgrip strength (kg) (SD) | Men | 27.2 (9.4) |
| Women | 15.7 (6.1) | |
| Mean BMI (kg/m2) (SD) | 30.2 (6.2) | |
| Mean BIA muscle massa (kg/m2) (SD) | Men (n = 70) | 7.84 (1.21) |
| Women (n = 69) | 6.65 (1.13) | |
| Mean SPPB (SD) | 5.5 (2.3) | |
| Mean walk speed (m/s) (SD) n = 142b | 0.61 (0.24) | |
| Median chair stand time (s) (IQR) n = 106c | 24.0 (17.4–32.0) | |
| Mean SARC-F score (SD) | 5.3 (1.8) | |
| Conditions (%) | Ischaemic heart disease | 40 (27) |
| Stroke | 25 (17) | |
| Chronic heart failure | 17 (11) | |
| Diabetes mellitus | 35 (24) | |
| Atrial fibrillation | 25 (17) | |
| Thyroid disease | 25 (17) | |
| Dementia | 0 (0) | |
| Anxiety | 13 (9) | |
| Depression | 22 (15) | |
| Parkinsonian syndromes | 3 (2) | |
| Chronic obstructive pulmonary disease | 24 (16) | |
| Asthma | 25 (17) | |
| Other lung disease | 22 (15) | |
| Osteoarthritis | 66 (45) | |
| Inflammatory arthropathy | 8 (5) | |
| Proportion with multimorbidity (2 or more long-term conditions) (%) | 100 (68) | |
| Median (IQR) number of medications | 8 (6–11) | |
| Fried frailty category (%) | Non-frail | 27 (18) |
| Pre-frail | 94 (64) | |
| Frail | 26 (18) | |
| Median MoCA score (IQR) n = 133 | 23 (20.5–26) | |
| Geriatric Depression Score (SD) | 4.2 (3.2) | |
| SarQoL score (SD) (best = 100) | 51 (12) | |
| Haemoglobin (g/l) (SD) n = 122 | 133 (13) | |
| eGFR (ml/min/1.73 m2) (SD) n = 131 | 68 (18) | |
| Albumin (g/l) n = 106 | 41 (4) |
BIA, bioimpedance assessment; eGFR: estimated glomerular filtration rate; IQR, interquartile range; SD, standard deviation.
aAppendicular skeletal muscle mass index by Sergi equation
bReasons for non-completion: wheelchair use (n = 1); no reason given (n = 4)
cUnable to complete five stands (n = 39); unable to stand without human assistance (n = 2)
Proportion with sarcopenia in the enrolled population
The proportions of enrolled individuals meeting the criteria for sarcopenia, probable sarcopenia under a series of different definitions, and different physical performance cutoffs are shown in Table 3. EWGSOP 2019 guidelines suggest a diagnosis of ‘probable sarcopenia’ can be made according to muscle strength cut-offs (low grip strength or prolonged chair stand time). Using this definition, 94% of enrolled participants had a diagnosis of probable sarcopenia. For a diagnosis of ‘confirmed’ sarcopenia, demonstration of low muscle mass is also required. Consistent with the proportions of participants with low muscle mass reported above, fewer than a fifth of participants met the criteria for ‘definite’ sarcopenia.
Table 3 .
Proportion of participants reaching threshold for diagnosis of sarcopenia (n = 147)
| EWGSOP 2010a | Low grip strengthb | Walk speed ≤0.8 m/s | Sit to stand >15 s | EWGSOP 2019 probablec | EWGSOP 2019 confirmedd | EWGSOP 2019 severee | FNIHf | |
|---|---|---|---|---|---|---|---|---|
| Men | 13 (17%) | 33 (44%) | 56 (75%) | 67 (89%) | 71 (95%) | 18 (24%) | 11 (15%) | 15 (20%) |
| Women | 8 (11%) | 35 (49%) | 60 (83%) | 65 (90%) | 67 (93%) | 9 (13%) | 7 (10%) | 14 (19%) |
| All | 21 (14%) | 68 (46%) | 116 (79%) | 132 (90%) | 138 (94%) | 27 (18%) | 18 (12%) | 29 (20%) |
FNIH, Foundation for the National Institutes of Health.
aLow grip strength (<30 kg men or <20 kg women) OR walk speed ≤0.8 m/s AND low appendicular muscle mass index (<7.26 kg/m2 men or < 5.5 kg/m2 women)
bLow grip strength (<27 kg men or <16 kg women)
cLow grip strength (<27 kg men or <16 kg women) OR sit to stand test >15 s/unable to complete
dLow grip strength (<27 kg men or <16 kg women) OR sit to stand test >15 s/unable to complete, AND low appendicular muscle mass index (<7.0 kg/m2 men or <5.5 kg/m2 women)
eAs for (c) but with walk speed ≤0.8 m/s
fLow grip strength (<26 kg men or <16 kg women) AND low appendicular lean mass (lean mass in kg divided by BMI in kg/m2 <0.789 for men or <0.512 for women)
Relationship of baseline physical performance to other baseline measures
The SARC-F score showed a moderate correlation with grip strength, walk speed and the SPPB score as shown in Table 4. The relationship between physical function and sarcopenia-specific quality of life was weak but reached significance for male grip strength and the SPPB score. Baseline biochemical and haematological indices were not significantly associated with baseline physical performance, but higher burden of multimorbidity was associated with lower physical performance.
Table 4 .
Association between baseline measures of muscle function and selected baseline variables (n = 147)
| Walk speed | SPPB | Grip strength (men) | Grip strength (women) | |||||
|---|---|---|---|---|---|---|---|---|
| r | P | r | P | r | P | r | P | |
| Age | -0.11 | 0.21 | -0.12 | 0.16 | -0.17 | 0.14 | 0.02 | 0.89 |
| SARC-F | −0.33 | <0.001 | −0.40 | <0.001 | −0.41 | <0.001 | −0.25 | 0.02 |
| SarQoL | 0.15 | 0.08 | 0.23 | 0.006 | 0.35 | 0.002 | 0.23 | 0.09 |
| Haemoglobin | 0.04 | 0.67 | 0.09 | 0.33 | 0.20 | 0.11 | 0.07 | 0.62 |
| Albumin | 0.86 | 0.38 | 0.03 | 0.73 | 0.19 | 0.14 | 0.01 | 0.94 |
| eGFR | 0.92 | 0.31 | 0.14 | 0.12 | 0.03 | 0.79 | -0.25 | 0.05 |
| Appendicular muscle mass | -0.94 | 0.31 | -0.05 | 0.54 | 0.13 | 0.30 | 0.26 | 0.03 |
| Number of conditions* | −0.20 | 0.02 | −0.19 | 0.03 | -0.08 | 0.51 | −0.27 | 0.02 |
| Number of medications* | −0.29 | <0.001 | −0.17 | 0.04 | -0.04 | 0.74 | -0.19 | 0.10 |
Pearson’s correlation coefficient except for *Spearman’s rho. The bold results are where p<0.05.
Proportion agreeing to enter registry
In total, 145/147 (98%) of participants completing the baseline assessment consented to be held on the registry to be contactable for future studies. Of these, 125 (85%) were happy to be contacted by letter, 21 (14%) by email, 59 (40%) by telephone and 10 (7%) by text messaging.
Discussion
We describe the first sarcopenia registry to be set up in the United Kingdom and show that such a registry is feasible and acceptable to participants who enrolled. Rates of consent for recontacting for future studies were very high suggesting that such a registry can perform its primary purpose of providing a pool of participants who are phenotyped and contactable for future clinical trial enrolment. Although we did not limit recruitment to those with sarcopenia, our recruitment strategy succeeded in enrolling a high proportion of participants with probable sarcopenia according to EWGSOP 2019 guidelines. Confirmed sarcopenia including low muscle mass as a criterion was, however, less common, in line with previous population-based cohort studies [24].
Our recruitment strategy using primary care mailshots was successful, and we were able to reach large numbers of potential participants with relatively low cost and effort despite the relatively low response rate. The use of telephone prescreening reduced the number of face-to-face visits that participants needed to attend with a consequent reduction in study burden, and this also contributed to low failure rates at the face-to-face screening visits. Such an approach increases the efficiency of recruitment process. The choice of visits at home rather than at a study centre was popular, with half of participants taking up this option; this flexibility may have encouraged some people to take part who otherwise would have declined. Although we used the SARC-F questionnaire with a cut-off of 3 or more to ensure that all participants had a degree of impairment of daily activities, it may be possible to use a lower cut-off than we used in this study; recent population studies have suggested that a score of one or above might be equally effective in identifying those with sarcopenia [25]. Despite the success of the recruitment strategy in the current study, other strategies for additional potential registry recruitment could include direct response to adverts by potential participants, recruitment from secondary care clinics including geriatric medicine clinics or opt-out recruitment strategies [26].
We noted considerable variability between sites in their ability to engage local primary care practices to help with recruitment as well as in response rates from mailshots. We deliberately chose a range of sites including urban and rural sites, sites in affluent and deprived areas, sites with predominantly white populations and sites serving populations with a high proportion of people from ethnic minority communities. It was noteworthy that sites with a high proportion of people from ethnic minority communities had a low response rate to mailshots, although we were not able to break down the individual response rate or final recruitment numbers by ethnicity in this study. Our findings highlight the fact that more tailored approaches are necessary to effectively reach members of ethnic minority communities. We did not provide translations of information sheets in this pilot study, although recruitment staff belonging to local ethnic minority communities were used in two of the sites [27], and this may have helped to improve rates of progression from pre-screening through to enrolment. Even when translated written materials are available, alternatives to written information may be more effective for some groups [28]. We did not collect data on deprivation or other lifestyle factors such as diet and activity in order to keep the amount of data collected to a manageable level. The registry, however, provides an ideal platform for more detailed enquiry into the relationship between these factors and sarcopenia in future studies.
Our embedded randomised controlled trial of the inclusion of the Newcastle University logo on the mailshot envelope did not show a significant effect on return rates for expressions of interest. Our hypothesis that a University logo would differentiate the mailshot from junk mail (i.e. it would act as a badge of trust) did not translate into a meaningful difference in return rates. This may be because the logo was not viewed as a badge of trust by potential participants, or it may be that potential participants opened all of their mail regardless of whether they thought it was junk and that the presence of a logo did not influence the decision to open the envelope. No previous randomised controlled trials have studied this issue in a clinical research context; these findings, however, add to the growing body of evidence from other studies within a trial of what interventions are effective at improving recruitment rates to clinical research studies [22]. Further studies could usefully examine whether logos from healthcare providers, or local rather than remote academic institutions, might be more effective at encouraging recruitment.
For sarcopenia trials to be representative of the population seen in clinical practice, the trial population needs not only to fulfil the criteria for sarcopenia but also needs to reflect the age and capability of people seen in clinical practice. Our registry population has high levels of co-morbid disease with over two-thirds of participants having multimorbidity; the mean age of 78 years, and significantly impaired physical performance measures are reflective of the population of older people seen in primary care and in geriatric medicine practice in secondary care. Although sarcopenia is relatively common in selected populations such as those in care homes and those admitted to hospital, recruitment of these populations for trials is extremely difficult as this group of patients are often very unwell, have severe cognitive impairment, or have very limited life expectancy. In the current study, participants at some centres were offered the option of having their screening/baseline visit at home but not all centres were able to offer this as an option. It is quite possible that the logistics of attending a clinical research facility was a factor in actual recruitment rates after telephone screening, and hence, additional recruitment methods such as recruiting during other interactions (for example at clinical appointments or at community visits) may also be important for a more inclusive registry.
Sarcopenia is considerably less common in the general population at between 5 and 10% [29], and our findings reinforce that identifying participants with sarcopenia remains challenging, in part because muscle mass and strength are not measured as part of routine clinical practice in either primary or secondary care in most healthcare systems. Our findings also reinforce that current definitions of sarcopenia [8] may not make sufficient allowance for obesity—absolute muscle mass is often preserved in people with obesity (and patients do not therefore meet the muscle mass criteria for sarcopenia), but muscle mass relative to body size is low with consequent impairment of function.
To be of most use to academic and commercial partners seeking to conduct clinical trials and other studies, registries need to be of sufficient size and to have a presence in multiple recruiting centres. Scale up of this UK sarcopenia registry is therefore a priority and the use of a large registry would be of great value in enhancing the UK’s clinical research delivery infrastructure, augmenting the work of the National Institute for Health Research (NIHR) Clinical Research Network. Scale up is likely to require simplification of the data collected, perhaps not only by linking to routinely collected clinical records but also by expansion of recruitment streams to incorporate recruitment directly from secondary care clinics (particularly those already measuring muscle strength and/or muscle mass), via advertising and via pop-up recruitment clinics in community settings. Maintenance of the registry, including replacement of registrants who die, also requires ongoing funding for recruitment and follow-up. In addition to providing a way to recruit to future trials, the registry also provides an opportunity to conduct studies to better understand sarcopenia and to test and validate new diagnostic tools for sarcopenia.
Acknowledgements
With thanks to all the participants, participating primary care surgeries and the NIHR Primary Care Research Network. We would like to thank Maggie Rice, Haja Tholley, Lindsay Wilkes, Abigail Jones, Farhat Mahmood and Ikhlaq Jacob for their efforts in recruiting participants.
Contributor Information
Miles D Witham, AGE Research Group, NIHR Newcastle Biomedical Research Centre, Newcastle University and Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle, UK.
Philip Heslop, AGE Research Group, NIHR Newcastle Biomedical Research Centre, Newcastle University and Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle, UK.
Richard M Dodds, AGE Research Group, NIHR Newcastle Biomedical Research Centre, Newcastle University and Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle, UK.
Andrew P Clegg, Academic Unit for Ageing and Stroke Research, University of Leeds, Bradford Teaching Hospitals NHS Foundation Trust, Bradford, UK.
Suzy V Hope, College of Medicine and Health, University of Exeter, and Royal Devon & Exeter NHS Foundation Trust, Exeter, UK.
Claire McDonald, Department of Geriatrics, Gateshead Health NHS Foundation Trust, Gateshead, UK.
David Smithard, Queen Elizabeth Hospital, Lewisham and Greenwich NHS Trust and University of Greenwich, London, UK.
Bryony Storey, Department of Geriatrics, Gateshead Health NHS Foundation Trust, Gateshead, UK.
Ai Lyn Tan, NIHR Leeds Biomedical Research Centre, Chapel Allerton Hospital, and Leeds Institute of Rheumatic and Musculoskeletal Medicine, University of Leeds, Leeds, UK.
Anna Thornhill, Academy of Research and Improvement, Solent NHS Trust, Portsmouth, UK.
Avan A Sayer, AGE Research Group, NIHR Newcastle Biomedical Research Centre, Newcastle University and Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle, UK.
Declaration of Conflicts of Interest
None.
Declaration of Sources of Funding
The NIHR Newcastle Biomedical Research Centre. A.C. is part-funded by the National Institute for Health Research Applied Research Collaboration Yorkshire & Humber and Health Data Research UK, an initiative funded by UK Research and Innovation Councils, NIHR and the UK devolved administrations and leading medical research charities.
References
- 1.Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet 2019; 393: 2636–46. [DOI] [PubMed] [Google Scholar]
- 2.Lunt E, Ong T, Gordon AL, Greenhaff PL, Gladman JRF. The clinical usefulness of muscle mass and strength measures in older people: a systematic review. Age Ageing 2021; 50: 88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu P, Hao Q, Hai S, Wang H, Cao L, Dong B. Sarcopenia as a predictor of all-cause mortality among community-dwelling older people: a systematic review and meta-analysis. Maturitas 2017; 103: 16–22. [DOI] [PubMed] [Google Scholar]
- 4.Yeung SSY, Reijnierse EM, Pham VKet al. Sarcopenia and its association with falls and fractures in older adults: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle 2019; 10: 485–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cruz-Jentoft AJ, Landi F, Schneider SMet al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing 2014; 43: 748–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hardee JP, Lynch GS. Current pharmacotherapies for sarcopenia. Expert Opin Pharmacother 2019; 20: 1645–57. [DOI] [PubMed] [Google Scholar]
- 7.Witham MD. Bridging the gap between the laboratory and the clinic for patients with sarcopenia. Biogerontology 2019; 20: 241–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Offord NJ, Clegg A, Turner G, Dodds RM, Sayer AA, Witham MD. Current practice in the diagnosis and management of sarcopenia and frailty-results from a UK-wide survey. J Frailty Sarcopenia Falls 2019; 4: 71–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cruz-Jentoft AJ, Bahat G, Bauer Jet al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 2019; 48: 16–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bauer JM, Verlaan S, Bautmans Iet al. Effects of a vitamin D and leucine-enriched whey protein nutritional supplement on measures of sarcopenia in older adults, the PROVIDE study: a randomized, double-blind, placebo-controlled trial. J Am Med Dir Assoc 2015; 16: 740–7. [DOI] [PubMed] [Google Scholar]
- 11.Marzetti E, Cesari M, Calvani Ret al. The “Sarcopenia and Physical fRailty IN older people: multi-componenT Treatment strategies” (SPRINTT) randomized controlled trial: case finding, screening and characteristics of eligible participants. Exp Gerontol 2018; 113: 48–57. [DOI] [PubMed] [Google Scholar]
- 12.Band MM, Sumukadas D, Struthers ADet al. Leucine and ACE inhibitors as therapies for sarcopenia (LACE trial): study protocol for a randomised controlled trial. Trials 2018; 19: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chalmers JD, Aliberti S, Polverino Eet al. The EMBARC European Bronchiectasis Registry: protocol for an international observational study. ERJ Open Res 2016; 2: 00081–2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thompson R, Robertson A, Lochmüller H. Natural history, trial readiness and gene discovery: advances in patient registries for neuromuscular disease. Adv Exp Med Biol 2017; 1031: 97–124. [DOI] [PubMed] [Google Scholar]
- 15.Sanchez-Rodriguez D, Bruyere O. The International Registry of patients with sarcopenia: applying research in sarcopenia to clinical practice. Eur Geriatr Med 2018; 9: 735–8. [DOI] [PubMed] [Google Scholar]
- 16.Malmstrom TK, Morley JE. Sarcopenia: the target population. J Frailty Aging 2013; 2: 55–6. [DOI] [PubMed] [Google Scholar]
- 17.Roberts HC, Denison HJ, Martin HJet al. A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing 2011; 40: 423–9. [DOI] [PubMed] [Google Scholar]
- 18.Sergi G, De Rui M, Veronese Net al. Assessing appendicular skeletal muscle mass with bioelectrical impedance analysis in free-living Caucasian older adults. Clin Nutr 2015; 34: 667–73. [DOI] [PubMed] [Google Scholar]
- 19.Guralnik JM, Simonsick EM, Ferrucci Let al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 1994; 49: M85–94. [DOI] [PubMed] [Google Scholar]
- 20.Beaudart C, Edwards M, Moss Cet al. English translation and validation of the SarQoL®, a quality of life questionnaire specific for sarcopenia. Age Ageing 2017; 46: 271–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nasreddine ZS, Phillips NA, Bédirian Vet al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005; 53: 695–9. [DOI] [PubMed] [Google Scholar]
- 22.Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clin Gerontol 1986; 5: 165–73. [Google Scholar]
- 23.Treweek S, Pitkethly M, Cook Jet al. Strategies to improve recruitment to randomised trials. Cochrane Database Syst Rev 2018; 2: MR000013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.SWAT Repository Store . The Northern Ireland Hub for Trials Methodology Research. https://www.qub.ac.uk/sites/TheNorthernIrelandNetworkforTrialsMethodologyResearch/SWATSWARInformation/Repositories/SWATStore/(accessed 8 September 2020)
- 25.Costanzo L, De Vincentis A, Di Iorio Aet al. Impact of low muscle mass and low muscle strength according to EWGSOP2 and EWGSOP1 in community-dwelling older people. J Gerontol A Biol Sci Med Sci 2020; 75: 1324–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dodds RM, Murray JC, Robinson SM, Sayer AA. The identification of probable sarcopenia in early old age based on the SARC-F tool and clinical suspicion: findings from the 1946 British birth cohort. Eur Geriatr Med 2020; 11: 433–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gliklich RE, Dreyer NA, Leavy MB, eds. Chapter 8. Informed Consent for Registries. In: Registries for Evaluating Patient Outcomes, A User’s Guide, 3rd edition. Rockville, USA: Agency for Healthcare Research and Quality (US), 2014. [PubMed] [Google Scholar]
- 28.Jacob I, Mahmood F, Brown L, Heaven A, Mahmood S, Clegg A. Recruiting older people from the Pakistani community in community ageing research 75. Br J Community Nurs 2020; 25: 110–3. [DOI] [PubMed] [Google Scholar]
- 29.NIHR Collaboration for Leadership in Applied Health Research and Care East Midlands . Increasing participation of Black Asian and Minority Ethnic (BAME) groups in health and social care research. Available at: http://arc-em.nihr.ac.uk/clahrcs-store/increasing-participation-black-asian-and-minority-ethnic-bame-groups-health-and-social(accessed 14 October 2020).
- 30.Patel HP, Syddall HE, Jameson Ket al. Prevalence of sarcopenia in community-dwelling older people in the UK using the European Working Group on Sarcopenia in Older People (EWGSOP) definition: findings from the Hertfordshire Cohort Study (HCS). Age Ageing 2013; 42: 378–84. [DOI] [PMC free article] [PubMed] [Google Scholar]


