Abstract
Rationale: The role of and needs for extracorporeal membrane oxygenation (ECMO) at a population level during the coronavirus disease (COVID-19) pandemic have not been completely established.
Objectives: To identify the cumulative incidence of ECMO use in the first pandemic wave and to describe the Nationwide Chilean cohort of ECMO-supported patients with COVID-19.
Methods: We conducted a population-based study from March 3 to August 31, 2020, using linked data from national agencies. The cumulative incidence of ECMO use and mortality risk of ECMO-supported patients were calculated and age standardized. In addition, a retrospective cohort analysis was performed. Outcomes were 90-day mortality after ECMO initiation, ECMO-associated complications, and hospital length of stay. Cox regression models were used to explore risk factors for mortality in a time-to-event analysis.
Measurements and Main Results: Ninety-four patients with COVID-19 were supported with ECMO (0.42 per population of 100,000, 14.89 per 100,000 positive cases, and 1.2% of intubated patients with COVID-19); 85 were included in the cohort analysis, and the median age was 48 (interquartile range [IQR], 41–55) years, 83.5% were men, and 42.4% had obesity. The median number of pre-ECMO intubation days was 4 (IQR, 2–7), the median PaO2/FiO2 ratio was 86.8 (IQR, 64–99) mm Hg, 91.8% of patients were prone positioned, and 14 patients had refractory respiratory acidosis. Main complications were infections (70.6%), bleeding (38.8%), and thromboembolism (22.4%); 52 patients were discharged home, and 33 died. The hospital length of stay was a median of 50 (IQR, 24–69) days. Lower respiratory system compliance and higher driving pressure before ECMO initiation were associated with increased mortality. A duration of pre-ECMO intubation ≥10 days was not associated with mortality.
Conclusions: Documenting nationwide ECMO needs may help in planning ECMO provision for future COVID-19 pandemic waves. The 90-day mortality of the Chilean cohort of ECMO-supported patients with COVID-19 (38.8%) is comparable to that of previous reports.
Keywords: extracorporeal membrane oxygenation, COVID-19, severe acute respiratory distress syndrome, pandemic
At a Glance Commentary
Scientific Knowledge on the Subject
Extracorporeal membrane oxygenation (ECMO) has been incorporated in the World Health Organization recommendations for the management of coronavirus disease (COVID-19)–associated severe acute respiratory distress syndrome. However, the incidence of ECMO use, its time course, and its outcomes are unknown at a nationwide level under the COVID-19 pandemic scenario.
What This Study Adds to the Field
In this nationwide study, all patients who received ECMO for severe acute respiratory distress syndrome during the first wave of the COVID-19 pandemic in Chile were identified. The incidence and time course of ECMO use was similar to those observed in the 2009 influenza A (H1N1) pandemic in Australia/New Zealand. The mortality rate was comparable with that reported for other indications of extracorporeal respiratory support. The operation of the National Advisory Commission for Adult ECMO was key in its assistance with patient eligibility, transportation, and allocation in tertiary centers in a resource-limited and logistically complex pandemic scenario. These findings might be useful for future COVID-19 pandemic waves worldwide.
Most patients with coronavirus disease (COVID-19) have mild disease, approximately 14% develop respiratory failure, and 5% require invasive mechanical ventilation (MV) (1). The vast majority of COVID-19–associated severe acute respiratory distress syndrome (ARDS) cases can be adequately supported by conventional critical care including protective MV, prone positioning, and neuromuscular blockade. Conventional critical care is unable to support a minority of patients, and extracorporeal membrane oxygenation (ECMO) has been used in such patients as a salvage therapy (2–4).
ECMO is a potentially lifesaving strategy in severe ARDS (5, 6) that has shown to be cost-effective in the United Kingdom (7). During the respiratory virus outbreaks caused by 2009 influenza A (H1N1) and Middle East respiratory syndrome coronavirus, the use of ECMO was included as part of intensive care support for severely ill patients (8–13). The benefits of ECMO use in patients with COVID-19 and the real need for ECMO in a population during this pandemic have not been well established; although initial reports of ECMO use in COVID-19–associated ARDS were discouraging (14), more recent larger cohorts suggest that results are equivalent to other ECMO indications for respiratory support (2–4). However, the “need” for ECMO in a population during the COVID-19 pandemic remains unknown.
ECMO has been incorporated in the World Health Organization (WHO) recommendations for the support of COVID-19–associated severe ARDS (15). However, ECMO is not available in many middle- and low-income countries. The complexities of this therapy require appropriate supplies and trained healthcare providers. In fact, it has been emphasized that institutions without a well-established ECMO program should not attempt to initiate it during a pandemic (16–18). At the same time, the priorities during this pandemic have been public health logistics to control the outbreak, including the provision of personal protective equipment and the coordination of clinical resources. In this scenario, ECMO may be too complicated to implement and too expensive to afford for the national health system of a small, middle-income country with challenging geographical peculiarities, like Chile. However, the application of a rationalization process based on the definition of tertiary referral centers, peer selection of patients, a program for transportation of ECMO candidates or mobile ECMO, strict follow-up, and public–private cooperation under the auspices of the ministry of health, may ensure cost-effective ECMO allocation and eventually improve patients’ outcomes. In Chile, these tasks were undertaken by the National Advisory Commission for Adult ECMO with global coverage over the entire country and population.
Crossing the national COVID-19 epidemiological database with the national ECMO database, we aimed to identify the cumulative incidence of ECMO use and mortality risk of ECMO-supported patients per population, per the number of positive cases, and per the number of ventilated patients with COVID-19 during the first wave of the COVID-19 pandemic. In addition, we describe the clinical characteristics and outcomes of ECMO-supported patients with COVID-19–associated severe ARDS in our country.
Methods
Study Design and Population
We conducted a population-based study during the first wave of COVID-19 pandemic in Chile (March 3 through August 31, 2020). The daily number and age of confirmed COVID-19 cases and mechanically ventilated patients with COVID-19 were obtained from the Ministry of Health records (19). Population size estimations for the year of 2020 were obtained from the National Institute of Statistics (20). Daily RT-PCR–confirmed severe acute respiratory syndrome coronavirus (SARS-CoV-2)–infected patients, aged 15 years or older, who received ECMO for severe ARDS in any of the 13 ECMO centers in Chile in the period were provided by the National Advisory Commission for Adult ECMO. Members of the commission technically evaluated and authorized the procedure and the referral to ECMO centers, including those using mobile ECMO (21). Patient selection criteria and ECMO management was based on the Extracorporeal Life Support Organization (ELSO) COVID-19 guidelines (22). In the selection process, critical care capacity was considered (see the online supplement). Patients were followed up until March 3, 2021; their vital status was checked in the National Civil Registry. The primary outcome was the cumulative incidence of ECMO use per population, per the number of positive cases, and per the number of ventilated patients with COVID-19. Respective rates of death in ECMO-supported patients were also calculated.
In addition, a retrospective cohort study of these ECMO-supported patients was performed, excluding patients from centers that refused to participate. The study was approved by an institutional review board that waived informed consent (No. 063/2020, Hospital Clínico Universidad de Chile). Prespecified data were collected in an anonymized standard form for each patient, which included demographics, comorbidities, the PaO2/FiO2 ratio, prone positioning, blood lactate, and severity scores (Sequential Organ Failure Assessment score [23], Respiratory ECMO Survival Prediction [RESP] score [24], and Murray Lung Injury Score [25]) as well as pre-ECMO intubation days. Ventilatory settings and respiratory mechanics before ECMO and at ECMO initiation were also collected. The primary outcome was 90-day mortality after ECMO initiation. Secondary outcomes included the frequency of ECMO-associated complications, ICU length of stay (LOS), hospital LOS, and factors associated with survival.
Statistical Analysis
In the population-based study, the age-standardized cumulative incidence of ECMO cases and deaths of ECMO-supported patients were calculated per population of 100,000, per 100,000 positive cases, and per 1,000 ventilated patients with COVID-19. The cumulative incidence of ECMO was calculated as the ratio of the sum of the incident cases of ECMO-supported patients and the population at risk in the same period. The mortality risk of ECMO-supported patients was calculated as the ratio of ECMO-supported patients who died and the population at risk in the period. Age-specific rates were calculated and then directly standardized according to the WHO standard population (26).
In the cohort study, variables are reported as the mean (±SD), median (interquartile range [IQR]), or absolute frequency and percentage. In the case of missing data, an available-case strategy was used, and the number of missing data was reported (see the online supplement). Comparisons between survivors and nonsurvivors were made using the Mann-Whitney U, Student’s t, and Fisher exact tests. Cox regression models were performed to explore risk factors associated with mortality in a time-to-event survival analysis. These factors were selected on the basis of previous studies (24, 27, 28) and tested in unadjusted models to achieve more than 10 events per variable. Time was considered as days to event from ECMO initiation, and the proportional hazard assumption was tested by using Schoenfeld residuals. The variables related to mortality with a P value ≤0.1 were categorized by using the concordance probability method (29). In addition, Kaplan-Meier curves were constructed to group patients according to duration of pre-ECMO intubation using 10 days as threshold and compared using a log rank test. Analyses were performed in Stata version 12.0 (StataCorp LP), and graphs were plotted in Prism version 8.0 (GraphPad).
Results
Epidemiology of ECMO during the COVID-19 Pandemic
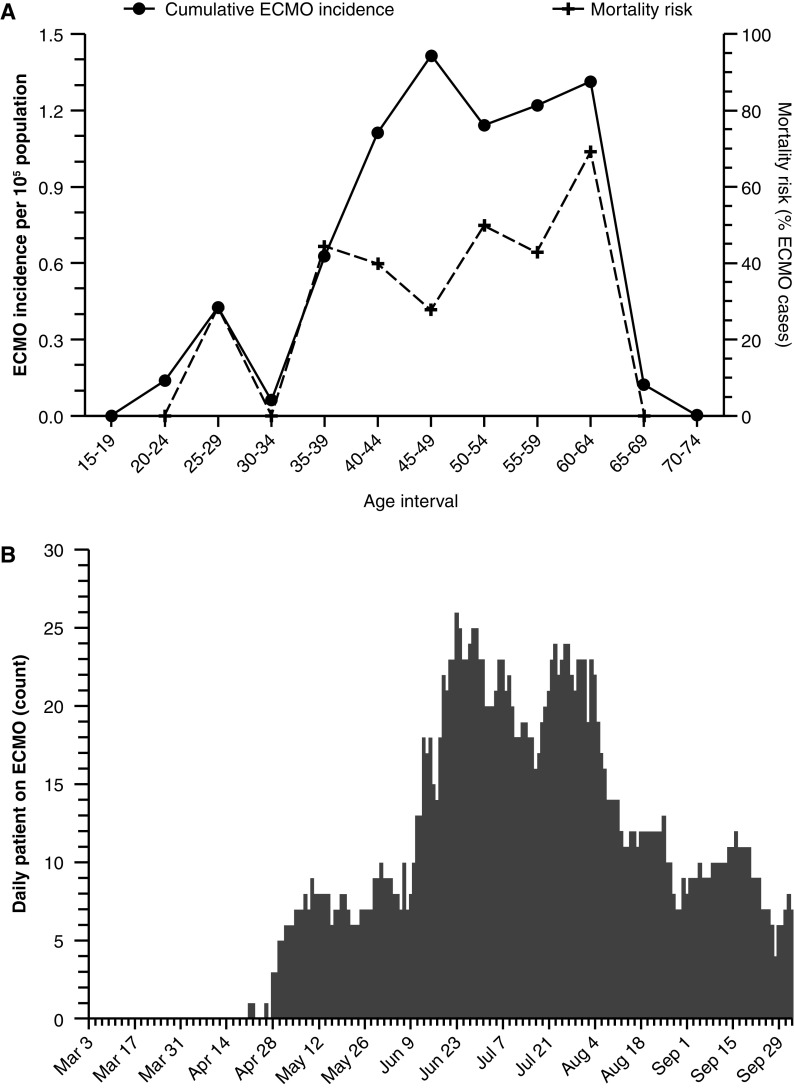
Between March 3 (the first case of COVID-19) and August 31, 2020, there were 444,921 COVID-19–positive cases in adults and 7,792 mechanically ventilated patients with COVID-19 in Chile; 94 of the patients with COVID-19–associated severe ARDS were supported with ECMO. The overall age-adjusted cumulative incidence of ECMO use was 0.42 per population of 100,000, 14.89 per 100,000 COVID-19–positive cases, and 1.2% of the ventilated patients with COVID-19. The age-standardized cumulative incidence of ECMO use and death among ECMO-supported patients for Chile and the WHO standard population are reported in Table 1. The majority of ECMO use occurred in people aged 40–60 years, and over half of deaths occurred in those aged 50–64 years; in addition, the mortality rate had a trend of increasing with age until the age interval of 60–64 years (Figure 1A). The number of peak ECMO-supported patients was higher than 25 simultaneous cases per day (Figure 1B). Time intervals between the first case of the pandemic and the first ECMO cannulation, the first ECMO cannulation and the peak number of ECMO-supported patients, and the peak number of ECMO-supported patients and halving of this peak were 49, 63, and 46 days, respectively.
Table 1.
National Estimates for ECMO Use during Chilean First Wave of the COVID-19 Pandemic
| ECMO Support, frequency measures* | Chile | WHO Standard Population† |
|---|---|---|
| ECMO cases per 105 population | 0.48 | 0.42 |
| ECMO cases per 105 COVID-19–positive cases | 17.08 | 14.89 |
| ECMO cases per 103 ventilated patients with COVID-19 | 12.06 | N/A |
| Mortality risk of ECMO-supported patients per 105 population | 0.20 | 0.17 |
| Mortality risk of ECMO-supported patients per 105 COVID-19–positive cases | 7.18 | 6.09 |
| Mortality risk of ECMO-supported patients per 103 ventilated patients with COVID-19 | 5.01 | N/A |
Definition of abbreviations: COVID-19 = coronavirus disease; ECMO = extracorporeal membrane oxygenation; N/A = not applicable; WHO = World Health Organization.
Frequency measures were estimated for the first wave of COVID-19 in Chile (March 3 to August 31, 2020).
WHO standard population for 2000–2025.
Figure 1.
Age-specific cumulative incidence of extracorporeal membrane oxygenation (ECMO) use per population of 100,000 and 90-day mortality for (A) patients receiving ECMO support and (B) daily patients on ECMO during the first wave of the coronavirus disease (COVID-19) pandemic in Chile. The incidence (black dots), cumulative incidence of ECMO use (solid line), mortality risk (black crosses), and age-specific 90-day mortality risk (dashed line) for patients receiving ECMO support are shown.
Chilean Cohort of ECMO-supported Patients
In this cohort report, we present data obtained from 85 of 94 ECMO patients (90%); 1 of 13 ECMO centers did not include its 9 patients because of an institutional decision. Patients who required ECMO support were mainly male (83.5%) and a median of 48 (IQR, 41–55) years of age, 42.4% had obesity, and the median Sequential Organ Failure Assessment score was 10 (IQR, 7–12) points. The duration of pre-ECMO intubation was a median of 4 (IQR, 2–7) days, the median PaO2/FiO2 ratio was lower than 87 mm Hg, and 91.8% of patients presented with persistent refractory hypoxemia, even with prone positioning; 16.5% of patients were connected to ECMO primarily because of refractory respiratory acidosis. One woman was pregnant, and all but three patients received venovenous (VV) ECMO support (Table 2). Ventilatory settings, respiratory mechanics, and oxygenation before ECMO initiation are displayed in Table 3; most patients were receiving ECMO in a volume-controlled mode (90.6%), the median Vt was 5 (IQR, 4.2–5.9) mL/kg of predicted body weight, the mean positive end-expiratory pressure (PEEP) was 10.3 (SD, 4.1) cm H2O, and the median static respiratory system compliance was 23.0 (IQR, 19.0–29.0) mL/cm H2O (Table 3). The duration of the ECMO run was a median of 16 (IQR, 10–27) days.
Table 2.
Patient Characteristics before ECMO Onset
| Characteristic | Total (N = 85) | Survivors (N = 52) | Nonsurvivors (N = 33) | P Value |
|---|---|---|---|---|
| Age, yr | 48 (41–55) | 47 (40–53) | 51 (42–57) | 0.087 |
| Sex, M | 71 (83.5%) | 43 (82.7%) | 28 (84.8%) | 1.000 |
| Comorbidities | 1 (1–2) | 1.0 (1.0–2.0) | 1.0 (1.0–2.0) | 0.421 |
| Hypertension | 26 (30.6%) | 14 (26.9%) | 12 (36.4%) | 0.469 |
| Diabetes | 18 (21.2%) | 10 (19.2%) | 8 (24.2%) | 0.597 |
| Obesity | 36 (42.4%) | 24 (46.2%) | 12 (36.4%) | 0.500 |
| COPD/asthma | 6 (7.1%) | 5 (9.6%) | 1 (3.0%) | 0.397 |
| Others | 19 (22.4%) | 14 (26.9%) | 5 (15.2%) | 0.287 |
| Days from COVID-19 diagnosis to MV | 4.0 (0.0–7.0) | 2.5 (0.0–6.0) | 5.0 (0.0–11.0) | 0.032 |
| Pre-ECMO intubation days | 4.0 (2.0–7.0) | 4.5 (2.0–8.0) | 4.0 (2.0–6.0) | 0.975 |
| SOFA score | 10 (7–12) | 9.0 (7.0–11.0) | 11.0 (8.0–13.0) | 0.094 |
| RESP score | 3.0 (1.0–5.0) | 4.0 (1.0–5.0) | 2.0 (1.0–4.0) | 0.032 |
| LIS | 3.3 (3.0–3.7) | 3.3 (3.0–3.5) | 3.3 (3.0–3.8) | 0.430 |
| Blood lactate, mmol/L | 1.6 (1.1–2.4) | 1.5 (1.0–2.2) | 2.0 (1.4–2.8) | 0.045 |
| Prone positioning | 78 (91.8%) | 47 (90.4%) | 31 (93.9%) | 0.701 |
| Neuromuscular blockade | 80 (94.1%) | 50 (96.2%) | 30 (90.9%) | 0.372 |
| VV ECMO | 82 (96.5%) | 51 (98.1%) | 31 (93.9%) | 0.557 |
| Mobile ECMO | 29 (34.1%) | 18 (34.6%) | 11 (33.3) | 1.000 |
Definition of abbreviations: COPD = chronic obstructive pulmonary disease; COVID-19 = coronavirus disease; ECMO = extracorporeal membrane oxygenation; IQR = interquartile range; LIS = Lung Injury Score; MV = mechanical ventilation; RESP = Respiratory ECMO Survival Prediction; SOFA = Sequential Organ Failure Assessment; VV = venovenous.
Data shown are the median (IQR), or n (%).
Table 3.
Ventilatory Settings, Respiratory Mechanics, and Gas Exchange before ECMO Initiation
| Parameter | Total | Survivors | Nonsurvivors | P Value |
|---|---|---|---|---|
| VT (mL/kg PBW) | 5.4 (4.7–6.0) | 5.5 (4.6–6.0) | 5.0 (4.9–5.9) | 0.390 |
| PEEP, cm H2O | 10.4 (4.1) | 10.7 (4.1) | 9.8 (4.1) | 0.350 |
| Plateau pressure, cm H2O | 26.2 (5.2) | 25.5 (5.6) | 27.3 (4.3) | 0.120 |
| Driving pressure, cm H2O | 15.0 (14.0–18.0) | 15.0 (14.0–16.0) | 16.0 (15.0–20.0) | 0.008 |
| Static compliance, mL/cm H2O | 22.0 (18.0–28.0) | 23.5 (19.0–29.0) | 19.5 (14.5–24.0) | 0.002 |
| FiO2, % | 90 (70–100) | 80 (70–100) | 100 (80–100) | 0.043 |
| PaO2, mm Hg | 71.8 (18.3) | 70.8 (18.2) | 73.3 (18.7) | 0.550 |
| PaO2/FiO2 ratio | 86.8 (63.7–99.2) | 80 (64.0–98.3) | 87.8 (62.0–100.0) | 0.990 |
| PaCO2, mm Hg | 58.2 (46.7–71.0) | 58.0 (44.5–69.0) | 64.0 (55.0–82.0) | 0.066 |
| pH | 7.30 (0.1) | 7.31 (0.1) | 7.25 (0.1) | 0.009 |
Definition of abbreviations: ECMO = extracorporeal membrane oxygenation; IQR = interquartile range; PBW = predicted body weight; PEEP = positive end-expiratory pressure.
Data shown are the median (IQR) or mean (SD).
Outcomes of ECMO-supported patients are shown in Table 4. As of March 3, 2021, 52 patients had been discharged home and 33 patients had died. The 90-day mortality after ECMO initiation was 38.8% and remained without changes after at least 180 days of observation. The pregnant woman and her fetus were discharged alive. Two patients received a double-lung transplant and were discharged home after being on ECMO for 59 and 81 days, respectively. Ventilatory settings were ultraprotective after ECMO initiation (see the online supplement).
Table 4.
Outcomes of ECMO-supported Patients with COVID-19
| Outcome | Median (IQR) or n (%) |
|---|---|
| Mortality at study ending | 33 (38.8) |
| 30-d mortality | 25 (29.4) |
| 60-d mortality | 32 (37.7) |
| 90-d mortality | 33 (38.8) |
| 180-d mortality | 33 (38.8) |
| In-hospital mortality | 33 (38.8) |
| Out-of-hospital mortality | 0 (0.00) |
| Hospital discharge | 85 (100) |
| Hospital LOS, d | 50 (24–69) |
| ICU LOS, d | 40 (21–57) |
Definition of abbreviations: COVID-19 = coronavirus disease; ECMO = extracorporeal membrane oxygenation; LOS = length of stay.
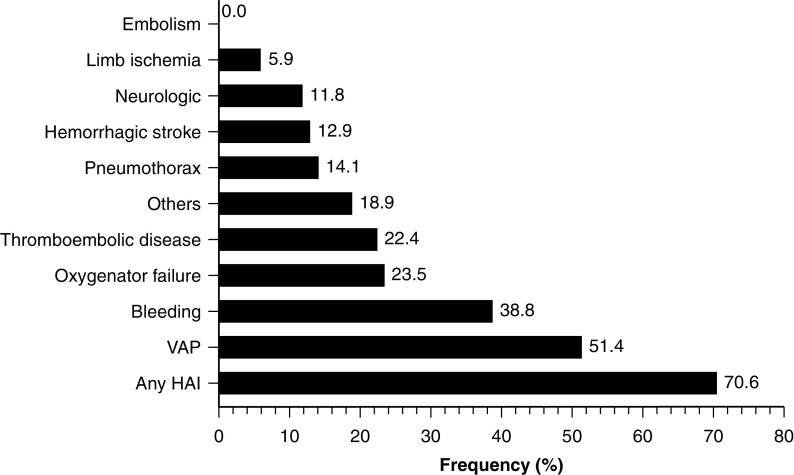
The absolute frequency of ECMO-associated complications was high (Figure 2). Most complications were infectious, including ventilator-associated pneumonia (VAP) in half of the patients, followed in prevalence by bleeding, oxygenator failure, and thromboembolic events. Hemorrhagic stroke, the most feared complication, was present in 12.9% of the patients. After normalizing by person-days on ECMO, the rate of infectious complications decreased but the rate of hemorrhagic complications remained high (see the online supplement). ICU and hospital stays were prolonged (medians of 40 and 50 d, respectively).
Figure 2.
Complications during ECMO support. ECMO = extracorporeal membrane oxygenation; HAI = healthcare-associated infections; VAP = ventilator-associated pneumonia.
Over 85% of patients started ECMO support before Day 10 of MV; however, delayed initiation of ECMO support in 11 patients was not associated with increased mortality (log rank test P value = 0.135; Figure 3). Patients who died had more time between the COVID-19 diagnosis and the connection to MV, a lower RESP score, a higher FiO2 requirement, lower respiratory system compliance, higher driving pressure, higher PaCO2, and a lower pH before ECMO initiation (Tables 2 and 3). A time between the COVID-19 diagnosis and the connection to MV >6 days, blood lactate >2.45 mmol/L, a RESP score <3, a static compliance of the respiratory system <18 ml/cm H2O, a pH <7.25 and PaCO2 >80 mm Hg before ECMO onset were all risk factors for mortality (Table 4). Neither mobile ECMO nor ICU-acquired infections were associated with increased mortality.
Figure 3.
Survival according to days on mechanical ventilation before ECMO initiation. ECMO = extracorporeal membrane oxygenation.
Discussion
Our population-based study provides valuable information about ECMO needs during the first wave of the COVID-19 pandemic. By having global coverage of an entire country and an entire population under the National Advisory Commission for Adult ECMO, we could obtain and coordinate the total number of ECMO-supported patients with COVID-19. ECMO in a middle-income economy like Chile was feasible, and the outcomes obtained in ECMO-rescued patients were similar to those of other studies of patients with severe ARDS with or without COVID-19 (3–5, 30).
ECMO use in COVID-19 worldwide has been variable, ranging from use in 1% of critically ill patients to use in 8% of critically ill patients (31–33). However, this is the only study that provides a nationwide incidence of ECMO use during the first wave of the COVID-19 pandemic. In our experience, 0.48 ECMO-supported patients per population of 100,000 were observed in a 6-month period, which is nearly twice the incidence observed in 3 months by the ANZ ECMO (Australia and New Zealand ECMO) investigators during the 2009 influenza A (H1N1) pandemic (0.26 per population of 100,000), with a similar number of concurrent patients receiving ECMO during the peak period (8). Interestingly, the number of ECMO-supported patients with COVID-19 reported here corresponds to nearly half of the historical annual ECMO cases in Chile, including all ECMO indications, which represents one-sixth of the annual incidence of VV ECMO reported in Germany in 2014 (34).
Our cohort includes some patients older than 60 years, some with more than 10 pre-ECMO intubation days, with more than 25 simultaneous ECMO cases per day during the peak COVID-19 pandemic period (Figure 1). Our results in ECMO-supported patients with COVID-19 are comparable with those from the COVID-19 ELSO registry that showed an estimated in-hospital mortality of 37.4% at 90 days (4). Mortality in COVID-19 has been related to male sex, advanced age, the presence of comorbidities, extrapulmonary organ failures, hyperinflammation, lymphopenia, and myocardial injury (35, 36). Most of these risk factors were also associated with mortality during ECMO in COVID-19, with the addition of venoarterial support, pre-ECMO cardiopulmonary resuscitation, and severity of pre-ECMO gas exchange impairment (4). In our cohort, patients who died had a longer time between diagnosis and the connection to MV, lower respiratory system compliance, higher driving pressure despite low Vt, and a lower pH, possibly indicating that delayed intubation (without excluding the progressive course of the disease itself) contributed to severe lung loss of aeration and/or fibrotic organization that led to dismal outcomes, notwithstanding ECMO support. In fact, it has been suggested that respiratory system compliance could be an important element for respiratory ECMO outcome assessment (27, 37). Further/larger studies are required to confirm this observation, as compliance has not been directly included in any score. On the other hand, higher blood lactate levels were also associated with increased mortality in our cohort, likely indicating that underlying severe systemic inflammation–associated hyperlactatemia is a turning point that may be difficult to reverse, even with ECMO support. In fact, blood lactate has been included in RESP models (27, 38).
Like in other COVID-19 ECMO reports, most of our patients were male, many had obesity, and most received VV ECMO support (2–4). The relatively high PaO2/FiO2 ratio, lower PEEP levels, and lower driving pressures as compared with previous reports (2–4), rather than corresponding to a lesser severity among our patients, may correspond to the inclusion of a significant group of patients presenting with refractory respiratory acidosis. In these patients, low levels of PEEP were used because high PEEP usually increases dead space, lowering the median value of PEEP used in the whole cohort before ECMO connection. As in the Paris-Sorbonne ECMO-COVID cohort (3), more than 90% of our cohort received neuromuscular blockade and underwent prone positioning before ECMO (Table 1); in contrast, the use of these adjunctive strategies was less common in the COVID-19 ELSO registry (4). Prone positioning can recruit collapsed lung even at low PEEP levels (e.g., 5 cm H2O) (39). Therefore, prone positioning can be also viewed as a PEEP-sparing maneuver in these severely hypoxemic patients, such that only moderate PEEP levels (e.g., 10 cm H2O) are required to balance its positive and detrimental effects. In fact, in the PROSEVA (Effect of Prone Positioning on Mortality in Patients with Severe and Persistent ARDS) trial, PEEP levels were lower in the prone group than in the supine group (40). Moreover, as recently observed by Ball and colleagues (41), severe COVID-19 pneumonia may have a low potential for recruitment; in 42 patients with this condition, these authors showed that increasing PEEP from 8 to 16 cm H2O leads to limited alveolar recruitment, as estimated by using computed tomography, at the expense of decreased respiratory system compliance. Even so, a high-PEEP trial was requested in all patients before considering transfer to an ECMO center in our cohort; thus, 28% of our patients were on PEEP levels ≥14 cm H2O before ECMO connection.
As in the COVID-19 ELSO registry, the duration of pre-ECMO intubation was not associated with 90-day mortality after ECMO initiation in our cohort; moreover, patients cannulated after 10 days of MV had a relatively low mortality rate. Because our study, with a relatively small sample size, was not designed to address this specific issue, the aforementioned observation should be considered with caution (the study had 80% power to detect a 2.02-fold difference in survival between patients with early [n = 74] and late [n = 11] ECMO initiation). However, it raises the plausible importance of differentiating between the length of pre-ECMO MV and that of pre-ECMO injurious MV in future studies, as protective ventilation strategies are likely easier to comply with during the first days of ventilation of a slowly deteriorating patient with ARDS (42).
The length of the ECMO run was in between that of the COVID-19 ELSO registry (4) and that of the Paris-Sorbonne ECMO-COVID cohort (3) (medians of 16, 13.9, and 20 days, respectively). Although the median hospital LOS was almost 2 weeks longer in our patients than in the COVID-19 ELSO registry (50 vs. 26.9 d), all of our surviving patients were discharged home, whereas a substantial number of patients in the ELSO registry were discharged to other healthcare facilities (4).
Regarding ECMO complications, oxygenator failure occurred in 23.5% of the patients in our cohort, which is almost three times that reported in the COVID-19 ELSO registry (8%) and nearly doubles the median rate reported by Vaquer and colleagues (12.8%) in non-COVID-19 VV ECMO patients (43). Bleeding occurred in 38.8% of our patients, whereas noncerebral bleeding occurred in 19% of the patients in the COVID-19 ELSO registry (4), 42% of the Paris-Sorbonne ECMO-COVID cohort (3), and 29.3% in Vaquer and colleagues’ meta-analysis (43). Hemorrhagic stroke occurred in 12.9% of our patients, which is more than double that reported in the COVID-19 ELSO registry (4) and 1.7 times that reported by Luyt and colleagues VV ECMO patients without COVID-19 (44). Even after normalizing the rates of hemorrhagic complications by time on ECMO, a significant excess persists (see the online supplement). In fact, Luyt and colleagues showed that hemorrhagic stroke is an early, relatively time-independent VV ECMO complication (44). Despite no substantial deviations from routine anticoagulation practice across centers, the rate of hemorrhagic stroke was also more than two times our own pre-COVID-19 pandemic experience. Potential factors associated with this major complication are lower pH before ECMO, lack of a specific protocol to avoid a large relative decrease in PaCO2 in the first 24 hours after ECMO initiation (45), the use of empiric intermediate or high-dose anticoagulation before ECMO (46), and the use of conventional initial heparin boluses regardless of previous anticoagulation and higher-end anticoagulation targets once on ECMO (22).
Among infectious complications, 51% of our patients had VAP, representing 19.5 per 1,000 person-days of ECMO. In the Paris-Sorbonne ECMO-COVID cohort, 87% of the patients had VAP (3). A subsequent report of the same group shows that this is a late-onset complication (median [IQR] MV duration before VAP, 10 [8–16] d) (44). In venoarterial ECMO patients without COVID-19, Bouglé and colleagues report VAP in 55.9%, with an incidence of 60.6 per 1,000 ECMO days (47), and in (mostly VV ECMO) patients without COVID-19, Grasselli and colleagues report VAP in 35%, with an incidence of 31 per 1,000 ECMO days (48). Overall, more than 70% of our cohort had a hospital-acquired infection, representing an incidence of 30.8 per 1,000 person-days of ECMO. This is in line with the Paris-Sorbonne ECMO-COVID cohort study, which reported that cannula infections and bacteremia episodes represented 23% and 48% of infections, respectively, apart from VAP cases (3). In ECMO patients without COVID-19, Grasselli and colleagues report nosocomial infection in 55% of patients, with an incidence of 50.4 infections per 1,000 person-days of ECMO (48). The comparison of rates and incidences of infectious complications between our cohort and that of Grasselli and colleagues reveals the time-sensitive nature of this kind of complication (our rates are higher, but our incidences are lower for both VAP and nosocomial infections). Furthermore, in contrast to Grasselli and colleagues’ cohort, ICU-acquired infections were not associated with mortality risk in our patients (Table 5). Nevertheless, considering the exploratory nature of our descriptive study, these observations should be considered with caution; unmeasured confounding remains possible. The low ICU capacity per population in Chile at the beginning 2020 and the massive mechanical ventilator demand for patients with severe COVID-19 forced the country’s healthcare system to triple its ICU capacity in a few months, increasing the number of ICU beds from 969 to 2,848 between January 30 and July 10, 2020 (see the online supplement). This major pressure on the critical care team and the sudden incorporation of lower-skilled healthcare workers may have had an impact on usual care, increasing the number of ECMO complications.
Table 5.
Risk Factors for Mortality in ECMO-supported Patients with COVID-19
| Risk Factor | Hazard Ratio (95% CI) | P Value |
|---|---|---|
| Age | 1.03 (0.98–1.06) | 0.111 |
| Obesity | 0.74 (0.36–1.51) | 0.408 |
| Blood lactate | 1.16 (0.98–1.36) | 0.080 |
| Blood lactate > 2.45 mmol/L | 2.17 (1.06–4.41) | 0.033 |
| SOFA score | 1.09 (0.98–1.22) | 0.126 |
| RESP score | 0.91 (0.81–1.02) | 0.098 |
| RESP score < 3 | 2.86 (1.38–5.91) | 0.005 |
| LIS | 1.08 (0.96–1.21) | 0.182 |
| PaO2/FiO2 ratio | 0.99 (0.99–1.01) | 0.663 |
| PaCO2 | 1.03 (1.01–1.05) | 0.001 |
| PaCO2 > 80 mm Hg | 4.83 (2.20–10.61) | <0.001 |
| pH | 0.00 (0.00–0.11) | 0.001 |
| pH < 7.25 | 3.66 (1.84–7.29) | <0.001 |
| Time from COVID-19 diagnosis to MV, d | 1.03 (0.99–1.07) | 0.105 |
| Time from COVID-19 diagnosis to MV >6 d, d | 2.37 (1.20–4.69) | 0.013 |
| Pre-ECMO intubation duration, d | 0.96 (0.90–1.02) | 0.173 |
| Ventilatory settings and respiratory mechanics before ECMO onset | ||
| VT (mL/kg PBW) | 0.93 (0.67–1.30) | 0.674 |
| PEEP | 0.96 (0.88–1.04) | 0.350 |
| Driving pressure | 1.09 (1.02–1.16) | 0.010 |
| Driving pressure > 16 | 2.88 (1.43–5.79) | 0.003 |
| Static compliance | 0.92 (0.87–0.97) | 0.004 |
| Static compliance < 25 | 3.61 (1.39–9.40) | 0.008 |
| Variables after ECMO onset | ||
| Oxygen saturation | 0.98 (0.96–0.99) | 0.015 |
| Oxygen saturation < 92% | 3.55 (1.55–8.14) | 0.003 |
| ICU-acquired infection | 0.63 (0.31–1.31) | 0.215 |
Definition of abbreviations: CI = confidence interval; COVID-19 = coronavirus disease; ECMO = extracorporeal membrane oxygenation; LIS = Lung Injury Score; MV = mechanical ventilation; PBW = predicted body weight; PEEP = positive end-expiratory pressure; RESP = Respiratory ECMO Survival Prediction; SOFA = Sequential Organ Failure Assessment.
Chile is located at the southwestern tip of South America and has a length of 4.270 km; its complex geography makes tertiary healthcare coverage difficult. Although WHO ranked Chile’s health system 33rd out of 190 countries, its mixed public–private healthcare system is fragmented with respect to delivery of services, and there is an unequal availability of resources (15). The national experience with ECMO in the 2009 influenza A (H1N1) pandemic and in hantavirus cardiopulmonary syndrome (also coordinated by the National Advisory Commission for Adult ECMO) served as an incentive to improve the logistics capacity in some regions, and four new ECMO centers in the public health system were implemented after 2016 (three of them out of Santiago, the biggest city).
Initiatives such as the National Advisory Commission for Adult ECMO service, with public/private cooperation and the possibility of mobile ECMO, have led to widespread availability of ECMO support. At the same time, the concentration of ECMO in a few expert centers, with a 24-h/d–7-d/wk mobile ECMO team coverage, improves the efficiency of the system.
In this nationwide study, the ECMO incidence in COVID-19 was similar to that observed in other pandemics. The reasonable mortality risk observed in these profoundly ill patients could be related to staff training and central organization. The existence of the National Advisory Commission for Adult ECMO was a key point for clinical decision-making, transportation, and logistics. These findings might be useful for subsequent COVID-19 pandemic waves worldwide.
Acknowledgments
Acknowledgment
The authors thank all the teams that work in the ICUs of Chile, especially the ECMO teams and members of the National Advisory Commission for Adult ECMO. The authors also thank Dr. Marcelo Villalón, M.D., Ph.D., (School of Public Health, Faculty of Medicine, University of Chile, Santiago, Chile) for the statistical advice in the present article.
Footnotes
Author Contributions: Authorship credit was based on substantial contributions to conception and design (R.A.D., J.G., A.I.J.G., and R.A.C.), acquisition of data (R.A.D., J.G., J.M.Z., C.R., J.A.E., S.I.B., P.A.S., J.C.B., L.B.C., A.I.J.G., A.K., L.L.F., J.V., R.E.C., R.A.P.-A., M.B., A.F.A., M.G.G., R.P., L.O., C.S., P.A.F., V.C., and R.A.C.), analysis and interpretation of data (R.A.D., J.G., J.M.Z., C.R., J.A.E., S.I.B., P.A.S., J.C.B., L.B.C., A.I.J.G., A.K., L.L.F., J.V., R.E.C., R.A.P.-A., M.B., A.F.A., M.G.G., R.P., L.O., C.S., P.A.F., V.C., and R.A.C.), drafting the article or revising it critically for important intellectual content (R.A.D., J.G., J.M.Z., C.R., J.A.E., S.I.B., P.A.S., J.C.B., L.B.C., A.I.J.G., A.K., L.L.F., J.V., R.E.C., R.A.P.-A., M.B., A.F.A., M.G.G., R.P., L.O., C.S., P.A.F., V.C., and R.A.C.), and final approval of the version to be published (R.A.D., J.G., J.M.Z., C.R., J.A.E., S.I.B., P.A.S., J.C.B., L.B.C., A.I.J.G., A.K., L.L.F., J.V., R.E.C., R.A.P.-A., M.B., A.F.A., M.G.G., R.P., L.O., C.S., P.A.F., V.C., and R.A.C.).
This article has an online supplement, which is accessible from this issue’s table of content online at www.atsjournals.org.
Originally Published in Press as DOI: 10.1164/rccm.202011-4166OC on April 6, 2021
Author disclosures are available with the text of this article at www.atsjournals.org.
Contributor Information
Collaborators: on behalf of the National Advisory Commission for Adult ECMO
References
- 1. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2. Mustafa AK, Alexander PJ, Joshi DJ, Tabachnick DR, Cross CA, Pappas PS, et al. Extracorporeal membrane oxygenation for patients with COVID-19 in severe respiratory failure. JAMA Surg. 2020;155:990. doi: 10.1001/jamasurg.2020.3950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Schmidt M, Hajage D, Lebreton G, Monsel A, Voiriot G, Levy D, et al. Groupe de Recherche Clinique en Reanimation et Soins Intensifs du Patient en Insuffisance Respiratoire Aigue (GRC-RESPIRE) Sorbonne Université; Paris-Sorbonne ECMO-COVID Investigators. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome associated with COVID-19: a retrospective cohort study. Lancet Respir Med. 2020;8:1121–1131. doi: 10.1016/S2213-2600(20)30328-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Barbaro RP, MacLaren G, Boonstra PS, Iwashyna TJ, Slutsky AS, Fan E, et al. Extracorporeal Life Support Organization. Extracorporeal membrane oxygenation support in COVID-19: an international cohort study of the Extracorporeal Life Support Organization registry. Lancet. 2020;396:1071–1078. doi: 10.1016/S0140-6736(20)32008-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Combes A, Hajage D, Capellier G, Demoule A, Lavoué S, Guervilly C, et al. EOLIA Trial Group; REVA; ECMONet. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378:1965–1975. doi: 10.1056/NEJMoa1800385. [DOI] [PubMed] [Google Scholar]
- 6. Combes A, Peek GJ, Hajage D, Hardy P, Abrams D, Schmidt M, et al. ECMO for severe ARDS: systematic review and individual patient data meta-analysis. Intensive Care Med. 2020;46:2048–2057. doi: 10.1007/s00134-020-06248-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Peek GJ, Clemens F, Elbourne D, Firmin R, Hardy P, Hibbert C, et al. CESAR: conventional ventilatory support vs extracorporeal membrane oxygenation for severe adult respiratory failure. BMC Health Serv Res. 2006;6:163. doi: 10.1186/1472-6963-6-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Davies A, Jones D, Bailey M, Beca J, Bellomo R, Blackwell N, et al. Australia and New Zealand Extracorporeal Membrane Oxygenation (ANZ ECMO) Influenza Investigators. Extracorporeal membrane oxygenation for 2009 influenza A (H1N1) acute respiratory distress syndrome. JAMA. 2009;302:1888–1895. doi: 10.1001/jama.2009.1535. [DOI] [PubMed] [Google Scholar]
- 9. Noah MA, Peek GJ, Finney SJ, Griffiths MJ, Harrison DA, Grieve R, et al. Referral to an extracorporeal membrane oxygenation center and mortality among patients with severe 2009 influenza A (H1N1) JAMA. 2011;306:1659–1668. doi: 10.1001/jama.2011.1471. [DOI] [PubMed] [Google Scholar]
- 10. Patroniti N, Zangrillo A, Pappalardo F, Peris A, Cianchi G, Braschi A, et al. The Italian ECMO network experience during the 2009 influenza A (H1N1) pandemic: preparation for severe respiratory emergency outbreaks. Intensive Care Med. 2011;37:1447–1457. doi: 10.1007/s00134-011-2301-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Alshahrani MS, Sindi A, Alshamsi F, Al-Omari A, El Tahan M, Alahmadi B, et al. Extracorporeal membrane oxygenation for severe Middle East respiratory syndrome coronavirus. Ann Intensive Care. 2018;8:3. doi: 10.1186/s13613-017-0350-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Al Gazwi HA, Ibrahim EE, Al Hammad ZA, Al Robeh ZA. Extracorporeal membrane oxygenation in severe ARDS secondary to Middle East respiratory syndrome coronavirus. Respir Care. 2019;64:3223338. [Google Scholar]
- 13. Cho HJ, Heinsar S, Jeong IS, Shekar K, Li Bassi G, Jung JS, et al. ECMO use in COVID-19: lessons from past respiratory virus outbreaks: a narrative review. Crit Care. 2020;24:301. doi: 10.1186/s13054-020-02979-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Henry BM, Lippi G. Poor survival with extracorporeal membrane oxygenation in acute respiratory distress syndrome (ARDS) due to coronavirus disease 2019 (COVID-19): pooled analysis of early reports. J Crit Care. 2020;58:27–28. doi: 10.1016/j.jcrc.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: interim guidance. 2020 May 27 [accessed 2020 Dec 15]. Available from: https://www.who.int/publications/i/item/clinical-management-of-covid-19.
- 16. MacLaren G, Fisher D, Brodie D. Preparing for the most critically ill patients with COVID-19: the potential role of extracorporeal membrane oxygenation. JAMA. 2020;323:1245–1246. doi: 10.1001/jama.2020.2342. [DOI] [PubMed] [Google Scholar]
- 17. Abrams D, Lorusso R, Vincent J-L, Brodie D. ECMO during the COVID-19 pandemic: when is it unjustified? Crit Care. 2020;24:507. doi: 10.1186/s13054-020-03230-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bartlett RH, Ogino MT, Brodie D, McMullan DM, Lorusso R, MacLaren G, et al. Initial ELSO guidance document: ECMO for COVID-19 patients with severe cardiopulmonary failure. ASAIO J. 2020;66:472–474. doi: 10.1097/MAT.0000000000001173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Informe epidemiológico COVID-19. Santiago, Chile: Ministerio de Salud Chile; 2020. https://www.minsal.cl/nuevo-coronavirus-2019-ncov/informe-epidemiologico-covid-19/ [Google Scholar]
- 20.Informe de proyecciones de población. Santiago, Chile: Instituto Nacional de Estadísticas; 2020. https://www.ine.cl/docs/default-source/proyecciones-de-poblacion/publicaciones-y-anuarios/base-2017/ine_estimaciones-y-proyecciones-de-población-1992-2050_base-2017_síntesis.pdf?sfvrsn=c623983e_6 [Google Scholar]
- 21. Daniela M, Felipe S, Van Nicolette SJ, Tomás R, Eli V, Jorge R, et al. Mobile ECMO in COVID-19 patient: case report. J Artif Organs. doi: 10.1007/s10047-020-01209-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Shekar K, Badulak J, Peek G, Boeken U, Dalton HJ, Arora L, et al. ELSO Guideline Working Group. Extracorporeal Life Support Organization coronavirus disease 2019 interim guidelines: a consensus document from an international group of interdisciplinary extracorporeal membrane oxygenation providers. ASAIO J. 2020;66:707–721. doi: 10.1097/MAT.0000000000001193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. Working Group on Sepsis-related Problems, European Society of Intensive Care Medicine. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996;22:707–710. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 24. Schmidt M, Bailey M, Sheldrake J, Hodgson C, Aubron C, Rycus PT, et al. Predicting survival after extracorporeal membrane oxygenation for severe acute respiratory failure: the Respiratory Extracorporeal Membrane Oxygenation Survival Prediction (RESP) score. Am J Respir Crit Care Med. 2014;189:1374–1382. doi: 10.1164/rccm.201311-2023OC. [DOI] [PubMed] [Google Scholar]
- 25. Murray JF, Matthay MA, Luce JM, Flick MR. An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis. 1988;138:720–723. doi: 10.1164/ajrccm/138.3.720. [DOI] [PubMed] [Google Scholar]
- 26.Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJL, Lozano R, Inoue M.Age standardization of rates: a new WHO standard. Geneva, Switzerland: World Health Organization; 2001. GPE Discussion Paper Series No. 31 [accessed 2020 Dec 15]. Available from: https://www.who.int/healthinfo/paper31.pdf [Google Scholar]
- 27. Rozencwajg S, Pilcher D, Combes A, Schmidt M. Outcomes and survival prediction models for severe adult acute respiratory distress syndrome treated with extracorporeal membrane oxygenation. Crit Care. 2016;20:392. doi: 10.1186/s13054-016-1568-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hilder M, Herbstreit F, Adamzik M, Beiderlinden M, Bürschen M, Peters J, et al. Comparison of mortality prediction models in acute respiratory distress syndrome undergoing extracorporeal membrane oxygenation and development of a novel prediction score: the Prediction of Survival on ECMO Therapy-Score (PRESET-Score) Crit Care. 2017;21:301. doi: 10.1186/s13054-017-1888-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Liu X. Classification accuracy and cut point selection. Stat Med. 2012;31:2676–2686. doi: 10.1002/sim.4509. [DOI] [PubMed] [Google Scholar]
- 30. Schmidt M, Pham T, Arcadipane A, Agerstrand C, Ohshimo S, Pellegrino V, et al. Mechanical ventilation management during extracorporeal membrane oxygenation for acute respiratory distress syndrome: an international multicenter prospective cohort. Am J Respir Crit Care Med. 2019;200:1002–1012. doi: 10.1164/rccm.201806-1094OC. [DOI] [PubMed] [Google Scholar]
- 31. Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. COVID-19 Lombardy ICU Network. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Xie J, Wu W, Li S, Hu Y, Hu M, Li J, et al. Clinical characteristics and outcomes of critically ill patients with novel coronavirus infectious disease (COVID-19) in China: a retrospective multicenter study. Intensive Care Med. 2020;46:1863–1872. doi: 10.1007/s00134-020-06211-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Schmidt M, Hajage D, Demoule A, Pham T, Combes A, Dres M, et al. COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators. Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. Intensive Care Med. 2021;47:60–73. doi: 10.1007/s00134-020-06294-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Karagiannidis C, Brodie D, Strassmann S, Stoelben E, Philipp A, Bein T, et al. Extracorporeal membrane oxygenation: evolving epidemiology and mortality. Intensive Care Med. 2016;42:889–896. doi: 10.1007/s00134-016-4273-z. [DOI] [PubMed] [Google Scholar]
- 35. Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Schmidt M, Combes A, Pilcher D. What’s new with survival prediction models in acute respiratory failure patients requiring extracorporeal membrane oxygenation. Intensive Care Med. 2014;40:1155–1158. doi: 10.1007/s00134-014-3342-4. [DOI] [PubMed] [Google Scholar]
- 38. Enger T, Philipp A, Videm V, Lubnow M, Wahba A, Fischer M, et al. Prediction of mortality in adult patients with severe acute lung failure receiving veno-venous extracorporeal membrane oxygenation: a prospective observational study. Crit Care. 2014;18:R67. doi: 10.1186/cc13824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Cornejo RA, Díaz JC, Tobar EA, Bruhn AR, Ramos CA, González RA, et al. Effects of prone positioning on lung protection in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2013;188:440–448. doi: 10.1164/rccm.201207-1279OC. [DOI] [PubMed] [Google Scholar]
- 40. Guérin C, Reignier J, Richard J-C, Beuret P, Gacouin A, Boulain T, et al. PROSEVA Study Group. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 41. Ball L, Robba C, Maiello L, Herrmann J, Gerard SE, Xin Y, et al. GECOVID (GEnoa COVID-19) Group. Computed tomography assessment of PEEP-induced alveolar recruitment in patients with severe COVID-19 pneumonia. Crit Care. 2021;25:81. doi: 10.1186/s13054-021-03477-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Marini JJ, Gattinoni L. Time course of evolving ventilator-induced lung injury: the “shrinking baby lung.”. Crit Care Med. 2020;48:1203–1209. doi: 10.1097/CCM.0000000000004416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Vaquer S, de Haro C, Peruga P, Oliva JC, Artigas A. Systematic review and meta-analysis of complications and mortality of veno-venous extracorporeal membrane oxygenation for refractory acute respiratory distress syndrome. Ann Intensive Care. 2017;7:51. doi: 10.1186/s13613-017-0275-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Luyt C-E, Bréchot N, Demondion P, Jovanovic T, Hékimian G, Lebreton G, et al. Brain injury during venovenous extracorporeal membrane oxygenation. Intensive Care Med. 2016;42:897–907. doi: 10.1007/s00134-016-4318-3. [DOI] [PubMed] [Google Scholar]
- 45. Cavayas YA, Munshi L, Del Sorbo L, Fan E. The early change in PaCO2 after Extracorporeal membrane oxygenation initiation is associated with neurological complications. Am J Respir Crit Care Med. 2020;201:1525–1535. doi: 10.1164/rccm.202001-0023OC. [DOI] [PubMed] [Google Scholar]
- 46. Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135:2033–2040. doi: 10.1182/blood.2020006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Bouglé A, Bombled C, Margetis D, Lebreton G, Vidal C, Coroir M, et al. Ventilator-associated pneumonia in patients assisted by veno-arterial extracorporeal membrane oxygenation support: epidemiology and risk factors of treatment failure. PLoS One. 2018;13:e0194976. doi: 10.1371/journal.pone.0194976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Grasselli G, Scaravilli V, Di Bella S, Biffi S, Bombino M, Patroniti N, et al. Nosocomial infections during extracorporeal membrane oxygenation: incidence, etiology, and impact on patients’ outcome. Crit Care Med. 2017;45:1726–1733. doi: 10.1097/CCM.0000000000002652. [DOI] [PubMed] [Google Scholar]