Abstract
Objective:
This study documents the adoption of telehealth by various types of primary healthcare (PHC) providers working in teaching PHC clinics in Quebec during the COVID-19 pandemic. It also identifies the perceived advantages and disadvantages of telehealth.
Method:
A cross-sectional study was conducted between May and August 2020. The e-survey was completed by 48/50 teaching primary care clinics representing 603/1,357 (44%) PHC providers.
Results:
Telephone use increased the most, becoming the principal virtual modality of consultation, during the pandemic. Video consultations increased, with variations by type of PHC provider: between 2% and 16% reported using it “sometimes.” The main perceived advantages of telehealth were minimizing the patient's need to travel, improved efficiency and reduction in infection transmission risk. The main disadvantages were the lack of physical exam and difficulties connecting with some patients.
Conclusion:
The variation in telehealth adoption by type of PHC provider may inform strategies to maximize the potential of telehealth and help create guidelines for its use in more normal times.
Abstract
Objectif:
Cette étude explore et documente l'adoption rapide des téléconsultations par différents types de de professionnels de première ligne travaillant dans des groupes de médecine familiale universitaires au Québec pendant la pandémie de COVID-19. Elle identifie également les avantages et les inconvénients perçus de la téléconsultation.
Méthode:
Une étude transversale a été menée entre mai et août 2020. Le sondage électronique a été complété dans 48/50 cliniques par 603/1,357 professionnels de première ligne (44 %).
Résultats:
L'utilisation du téléphone a le plus augmenté, devenant la principale modalité de consultation virtuelle pendant la pandémie. Les consultations par vidéo ont également augmenté, avec des variations selon le type de professionnel; entre 2 % et 16 % des répondants ont déclaré l'utiliser « parfois ». Les principaux avantages perçus de la téléconsultation étaient la réduction des déplacements des patients, l'amélioration de l'efficacité et la réduction du risque de transmission des infections. Les principaux inconvénients étaient l'absence d'examen physique et les difficultés de connexion avec certains patients.
Conclusion:
La variation de l'adoption des téléconsultations selon le type de professionnel de première ligne nous permet de prévoir des stratégies visant à maximiser le potentiel de la télésanté et d'élaborer des lignes directrices pour son utilisation en temps normal.
Introduction
Before the COVID-19 pandemic, telehealth implementation in most countries was very limited (Smith et al. 2020). Telehealth is defined as synchronous or asynchronous consultations at distance between healthcare providers and patients with the help of information and communication technologies (Deldar et al. 2016) such as telephone, video conference or secure messaging (CMA 2020). Canada lags behind other Organisation for Economic Co-operation and Development (OECD) countries in the adoption of telehealth (CMA 2020). In countries participating in a Commonwealth Fund survey in 2019, an average 65% of medical clinics reported interacting with patients online (via e-mail or secure website), compared to only 23% in Canada and 17% in Quebec (CIHI 2020). While an average 4.2% of healthcare professionals across Canada reported frequently using video consultations, in Quebec the average was around 0.6%. A recent survey conducted before the pandemic by the Canadian Medical Association found that only 8% of Canadians were able to consult their physicians remotely, though 69% would have liked to do so (CMA 2019).
Advantages of telehealth identified before and during the pandemic include improved access, remote triage of patients, routine follow-up care (especially for managing chronic conditions), remote diagnosis and remote patient care (Breton et al. 2021; Kichloo et al. 2020; Smith et al. 2020; Srinivasan et al. 2020; Wijesooriya et al. 2020). Disadvantages relate mainly to changes in the therapeutic relationship, which make it more difficult to establish trust and can depersonalize care (Bergman et al. 2020; Shankar et al. 2020; Srinivasan et al. 2020). These disadvantages suggest that certain professional activities may be less compatible with telehealth than others (Donnelly et al. 2021), especially when patients need psychosocial support (Bergman et al. 2020; Shankar et al. 2020; Srinivasan et al. 2020). Some studies report confidentiality issues and inequities based on access to or ability to use technology, which poses a risk of excluding certain groups, such as the elderly (Shankar et al. 2020; Srinivasan et al. 2020; Wijesooriya et al. 2020) and vulnerable populations (e.g., people living in rural areas or with low income, linguistic or ethnic minorities, etc.) (Crawford and Serhal 2020; Fujioka et al. 2020; Nouri et al. 2020). Establishing a reliable diagnosis is also challenging due to limitations on the information that can be gathered, including the lack of physical examination during a telehealth consultation (Srinivasan et al. 2020).
Before the COVID-19 pandemic, the use of telehealth varied widely between jurisdictions depending on healthcare policies, financial incentives, acceptance by healthcare workers and patients and integration with in-person healthcare services (Hashiguchi 2020). Governments around the world introduced temporary measures to remove barriers to telehealth during the pandemic. In Quebec's universal publicly funded healthcare system, family physicians (FPs) are remunerated predominantly on a fee-for-service basis, although some new modes of mixed remuneration are also available to encourage the follow-up of patients in the community (Breton et al. 2014). Because FPs were not remunerated for telehealth before March 16, 2020, the province authorized a temporary billing code for telephone or video consultations at the same rate as an in-person consultation. The Ministry of Health and Social Services also approved a list of platforms providers could use (e.g., Teams, Health Zoom, REACTS, EMR platforms) that ensured safety and confidentiality during telehealth consultation (Gouvernement du Québec 2020).
The COVID-19 pandemic revealed the critical importance of being able to provide telehealth effectively to meet patient's needs while reducing the risk of infection from SARS-CoV-2 (Bloem et al. 2020; McMahon et al. 2020; Smith et al. 2020; Srinivasan et al. 2020). Healthcare providers were compelled to adapt rapidly in a context where they and their patients had little prior experience with virtual consultations. The whirlwind speed of change provided a unique opportunity to find out how primary healthcare (PHC) providers adapted their practices to integrate regular telehealth use.
To our knowledge, this is among the first studies to explore the adoption of telehealth by PHC providers in Canada since the beginning of the pandemic (Glazier et al. 2021). It documents the transition – achieved over a few months – to telehealth across the province of Quebec (603 respondents) by various types of PHC providers working in university-affiliated (teaching) family medicine groups (U-FMGs). It also identifies the perceived advantages and disadvantages of telehealth in the Quebec context.
Method
Design and Setting
A cross-sectional study was conducted based on an open e-survey hosted on a web platform and distributed between May and August 2020 to all U-FMGs in Quebec (n = 50). The U-FMG model involves interdisciplinary teams with a teaching mission for family medicine residents (Breton et al. 2020). An FMG is a group of physicians working closely with nurses, social workers, pharmacists and other professionals in the provision of services to enrolled patients on a non-geographic basis (Breton et al. 2011). The number of accredited FMG practices has steadily increased since the FMG model was inaugurated in 2002, and the FMG is now the predominant model of PHC in Quebec (Breton et al. 2013). There are more than 330 accredited FMGs, of which 50 are U-FMGs. Located in both urban and rural settings, each U-FMG is linked to one of the province's four faculties of medicine.
The self-administered e-survey included 20 open-ended and closed questions, which took about 10 minutes to complete. The survey (Appendix 1, available online at here) was inspired by a “Together for Better Telehealth” pilot survey developed by the Massachusetts Health Quality Partners (2020) and was adapted to the Quebec context. The survey was pre-tested with four PHC providers using cognitive testing (Levine et al. 2005).
Participants
All healthcare providers working in U-FMGs were invited to complete the anonymous online survey on a voluntary basis.
Recruitment Process and Survey Administration
The research team worked in close collaboration with the province's four practice-based research networks (PBRNs). Each PBRN includes a network of U-FMGs, is linked to a faculty of medicine and has an organizational structure that enables rapid communication with U-FMG members. A personalized approach was developed with the research facilitators of each PBRN to encourage participation in the study. Information sessions were organized to present the research project (the research team and the purpose of the study) to U-FMG directors and explain the involvement required from participants (i.e., length of survey, confidentiality, opportunity to withdraw, etc.).
The research team prepared an e-mail message, which included a hyperlink to the e-survey, inviting PHC providers to participate. This was forwarded to the facilitators in each U-FMG. The Dillman method (Dillman et al. 2014), based on three reminders, was used to maximize the response rate. Participation rates of U-FMGs were communicated to the designated PBRN representative following each reminder.
Analysis
Statistical Analysis
Descriptive analyses by type of provider, along with Wilcoxon tests, were conducted with IBM SPSS, Version 26. Descriptive statistics were used to summarize socio-demographic variables (gender and years in practice) and response frequencies (percentage, valid percent) by type of provider. Wilcoxon tests were used to detect significant differences between telehealth use before and during the first few months of the pandemic. Incomplete responses were excluded from the analyses. To clarify the presentation of results on use of telephone, video, e-mail or text message consultations, the categories “never” and “rarely” were merged, as were categories “often” and “most of the time.”
Qualitative Data Analysis
Inductive thematic analysis (Miles et al. 2014) using the NVivo software explored responses to open-ended questions about advantages and disadvantages of using telehealth along with general comments. Key themes were identified and coded. To ensure the quality of the analysis, two researchers regularly reviewed their coding and discussed emerging themes with a third researcher on the team. The Results section presents the main sub-themes that emerged from this exploratory analysis.
Ethics Approval
This study was approved by the Research Ethics Committee of Centre de recherche – Hôpital Charles-Le Moyne of the CISSS de la Montérégie-Centre (MP-04-2019-368). Participants were provided with information on the study, and they consented to participate before completing the survey.
Results
Across the province, 48 of 50 U-FMGs participated in the study. A total of 603 out of a potential 1,357 PHC providers responded to the survey, including 405 FPs, 81 nurses, 34 nurse practitioners (NPs), 27 social workers, 13 psychologists and 43 other professionals including pharmacists, nutritionists, physiotherapists and respiratory therapists. The overall response rate was above 44%, with the denominator (1,357) based on the number of PHC provider positions assigned in the administrative database of the Ministry of Health and Social Services to the 48 U-FMGs participating in the study. This denominator included PHC providers on sick or maternity leave, unfilled positions and providers reallocated to other settings during the pandemic. Among those who participated, the completion rate was 87%.
Respondents were mostly women. FPs had been in practice an average of 10 years, while the range for NPs, nurses, psychologists and social workers was between 11 and 14 years. Between 83% and 100% of providers in each U-FMG rated their computer skills as above average (Table 1).
Table 1.
Respondents' identification
| Characteristics | Profession (number of respondents – n) | |||||
|---|---|---|---|---|---|---|
| FPs(n = 405) | NPs(n = 34) | Nurses(n = 81) | Social Workers(n = 27) | Psychologists(n = 13) | Otherprofessionals(n = 43) | |
| Women % (n) | 71% (256) | 93% (26) | 94% (63) | 83% (20) | 92% (11) | 84% (26) |
| Computer skills above average % (n) | 92% (334) | 100% (29) | 93% (62) | 88% (21) | 83% (10) | 94% (30) |
| Years of practice Mean [min., max.] | 8.9 [1, 15] | 10.5 [3, 15] | 13.4 [3, 15] | 10.7 [3, 15] | 14 [7, 15] | 8.1 [3, 15] |
Quantitative Results
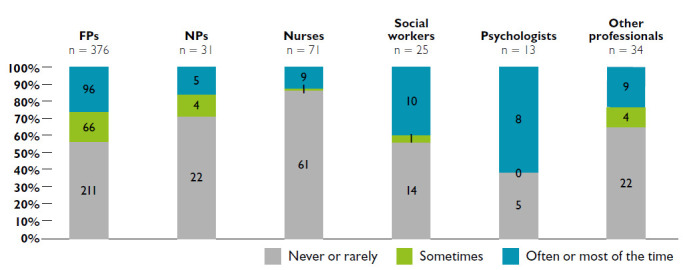
Results show a clear increase in use of telephone consultations during the COVID-19 pandemic. Telephone use went from “never” or “rarely” being used before the pandemic to becoming the principal consultation modality during the pandemic. The percentage of PHC providers using telephone consultations “often” or “most of the time” was 80% for FPs, 87% for NPs, 76% for nurses, 88% for social workers, 69% for psychologists and 80% for other professionals. Use of telephone consultations by all PHC providers during the first three months of the pandemic was statistically significantly higher than before the pandemic (z = −19.729, p < 0.001) (Figure 1).
Figure 1.
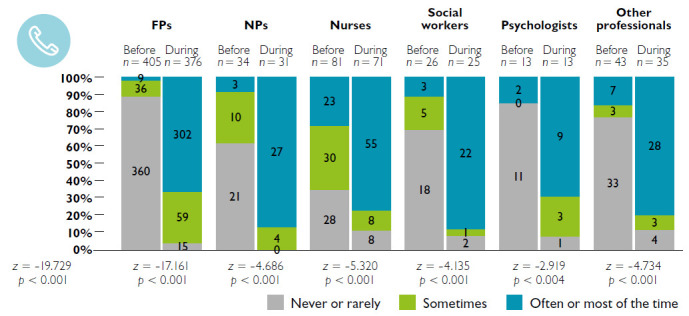
Proportion of respondents using the telephone for patient consultations before and during the pandemic, by type of PHC provider
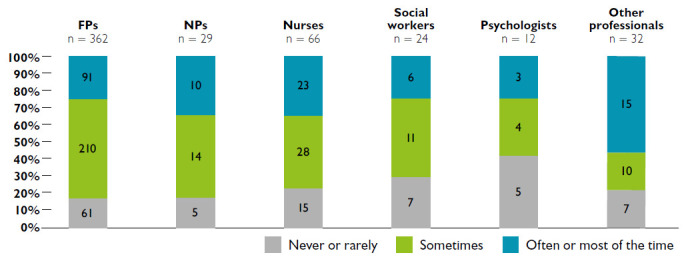
The use of video consultations (Figure 2) also slightly increased, but these were used by fewer providers and less frequently than the telephone. Before the COVID-19 pandemic, providers rarely used video consultations. During the pandemic, between 2% and 15% of professionals used video “sometimes” (p < 0.001), except for over half of psychologists who used video “often” or “most of the time” (z = −2,762, p = 0.006).
Figure 2.
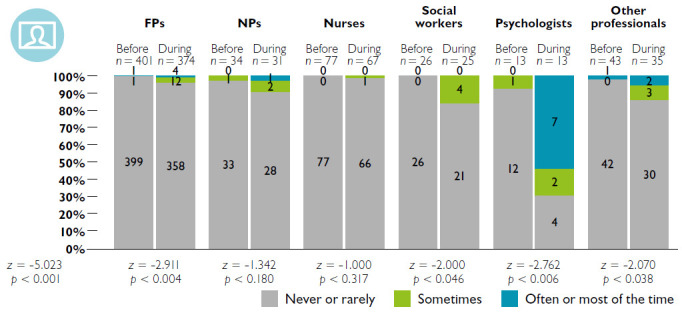
Proportion of respondents using video consultations before and during the pandemic, by type of PHC provider
The use of e-mail (Figure 3) with patients before the pandemic varied among PHC providers – 65% of FPs, 32% of NPs, 30% of nurses, 4% of social workers, 31% of psychologists and 46% of other providers “never” or “rarely” used e-mail before the pandemic. During the first three months of the pandemic, use of e-mail by all PHC providers was statistically significantly higher than before (z = −8.876, p < 0.001).
Figure 3.
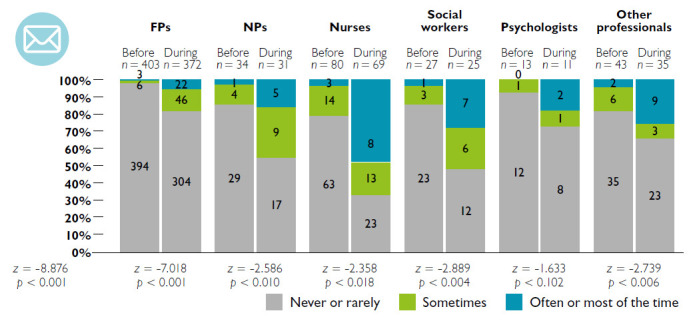
Proportion of respondents using e-mail before and during the pandemic, by type of PHC provider
During the pandemic, use of text messages increased between 3% and 10% for FPs, NPs, nurses, social workers and psychologists. No increase was observed among the other providers, including pharmacists, nutritionists, physiotherapists and respiratory therapists (z < 0.001, p = 1.000) (Figure 4).
Figure 4.
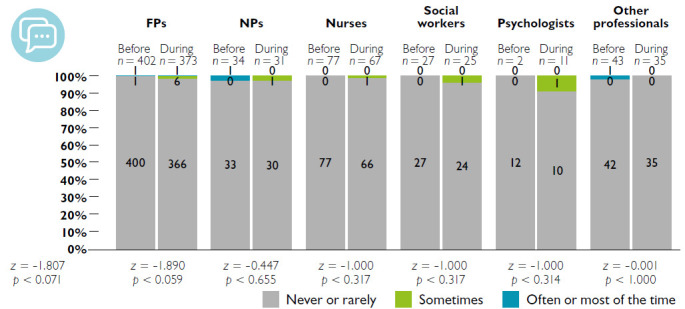
Proportion of respondents using text messages before and during the pandemic, by type of PHC provider
Telehealth consultations were conducted from home by 44% of FPs, 29% of NPs, 44% of social workers, 62% of psychologists, 37% of other professionals and just 15% of nurses (Figure 5).
Figure 5.
Proportion of respondents conducting telehealth from home, by type of PHC provider
Regarding intent to use telehealth in future practice, between 90% and 100% of PHC providers intended to continue using telehealth post-pandemic. As shown in Figure 6, 83% of FPs and NPs, 77% of nurses, 71% of social workers and 58% of psychologists thought they would use it “sometimes,” “often” or “most of the time” after the pandemic.
Figure 6.
Intent to use telehealth in post-pandemic practice
Qualitative Results
Table 2 presents the most frequently mentioned advantages and limitations of telehealth, as reported in participants' responses to open-ended questions.
Table 2.
Most frequently reported advantages and limitations of telehealth over in-person visits
| Advantages | Limitations |
|---|---|
|
|
Advantages
Responses from 400 participants pointed to advantages, including eliminating the need for patients to travel to appointments; this was mentioned especially with regard to vulnerable patients, patients with mobility issues and patients living in remote areas.
Now it seems to benefit mostly patients with limited mobility and may eventually provide a more patient-centred model of care for certain situations. (FP)
It makes life easier for patients who are vulnerable or lack means of transportation. (Nurse)
Along with reducing the risk of COVID-19, telehealth was also seen as an efficient means of conducting follow-up visits for prescription renewals and requests for tests or specialist consultations for patients with chronic illnesses.
Very useful for certain mental health and chronic disease follow-up visits that do not require a physical examination. (FP)
Limitations
Responses from 396 participants mentioned a number of limitations with telehealth consultations including limited ability to collect clinical information.
Telemedicine visits decrease the amount of information available to make clinical decisions. (FP)
Responses also mentioned that telehealth consultations did not allow for physical examinations, which could lead to additional in-person consultations and risk of errors.
The physical examination remains an essential element to evaluate a more complex problem. (FP).
[There is d]uplication of consultation when the teleconsultation reveals that a physical examination is needed and a second in-person appointment must be scheduled. (FP)
Complaints are more difficult to assess especially when you don't know the patient, increasing the risk of making diagnostic errors. (FP)
Several providers also reported challenges in establishing trust with new patients, particularly through telephone consultation, including the missing human contact and the non-verbal communication that is essential to building a therapeutic relationship and establishing an appropriate diagnosis.
[I have d]ifficulty connecting, especially [on] sensitive topics or [with] patients less known to me. (FP)
[There is d]ecreased human contact [crucial in psychotherapy or psychosocial support]. (FP)
[We d]o not see the non-verbal … [We d]o not see the physical signs [gait, general state, face] … (FP)
Technological limitations on both patient and provider ends were also mentioned, and some participants reported not having video conferencing capabilities (e.g., lack of equipment, insufficient bandwidth, etc.).
Video [is] not suitable for use in institutions with slow internet networks. (FP)
Certain clienteles have limited access to or understanding of technology. (Nurse)
Many PHC providers were concerned that the lack of visual contact with phone consultation limited the possibility of collecting physical and non-verbal information and risked affecting the quality of diagnosis.
Consultations on the phone do not allow us to see the person and [the] signs that guide us to a diagnosis or the cause of a problem. Video also limits what we can get as information. (NP)
Discussion
First and foremost, this study shows a dramatic shift toward telehealth in primary care settings in the early months of the COVID-19 pandemic when physical distancing directives required changing the way healthcare was delivered. The rapid implementation of telehealth early in the pandemic echoes results of other recent studies in Canada (Bhatia et al. 2021; CMA 2020; Glazier et al. 2021). Results also concur with findings that for most PHC providers the main modality for delivering care during the pandemic was the telephone (CMA 2020). Compared with studies conducted across Canada and in other countries (Bhatia et al. 2021; CMA 2020; Jaklevic 2020), adoption of video consultation by PHC providers in Quebec was limited before the pandemic. While it increased slightly during the pandemic, respondents reported technical barriers such as access to secure online platforms (including equipment and bandwidth) in their U-FMG as well as patients' barriers to video consultation, which could explain this difference. This was also reported in another Canadian study (Bhatia et al. 2021).
Results indicate that a large proportion of PHC providers conducted telehealth consultations from their homes with nurses being the least likely to do so and psychologists the most. Use of the telephone requires no bandwidth or special skills, it is inexpensive and was already common in virtual care practice before the pandemic (Bhatia et al. 2021). In addition, the fact that fees for telephone consultations were the same as for video visits (Gouvernement du Québec 2020) may have influenced their widespread use in Quebec during the pandemic; this was also reported in Ontario (Bhatia et al. 2021).
Variation in the use of video consultations between PHC providers suggests differences in the compatibility of certain professional activities with telehealth as recently highlighted by Donnelly et al. (2021). Psychologists are the PHC providers who used video the most for consultations. Several studies have found telehealth less suitable for psychosocial support (Bergman et al. 2020; Shankar et al. 2020; Srinivasan et al. 2020), but the pandemic context may have made it more relevant as a way to meet psychosocial needs in a crisis (Bhatia et al. 2021).
Results reveal an increase in the use of e-mail to communicate with patients, especially among NPs, nurses, social workers and other professionals. They also indicate that these types of providers already used this modality before the pandemic. E-mail appeared as an obvious asynchronous communication tool in 2020, and the appearance of the pandemic accelerated its use by all PHC providers.
Some of the advantages of telehealth reported by providers in this study may influence post-pandemic practice and improve the quality of healthcare services. These include facilitating access for patients who are vulnerable, have limited mobility, are at risk of infection or live in remote areas. This survey found that most PHC providers appreciated the efficiency and possibilities offered by virtual consultations especially for addressing relatively minor problems, reducing wait times and providing follow-up for patients with chronic health problems, such as prescription renewals, monitoring adherence to therapy or providing mental health/psychosocial support. Similar results about telehealth benefits for access and follow-up care have been reported in other studies (Kichloo et al. 2020; Smith et al. 2020; Srinivasan et al. 2020; Wijesooriya et al. 2020).
Participants expressed concerns about the limited possibilities for vulnerable populations to access some digital divide tools (e.g., video conferences, pictures, prescriptions by e-mail, etc.). Post-pandemic, barriers to equitable access will need to be considered to preserve the universality of the healthcare system. Research on health informatics and digital health have documented risks to health equity associated with virtual care initiatives (Anderson-Lewis et al. 2018; SPOR PIHCI Canada n.d.; Veinot et al. 2018, 2019). It is essential that the pandemic response and any subsequent reorganization of PHC do not exacerbate already significant health disparities between privileged and underserved patients. Telehealth has the potential to improve effectiveness and efficiency, but it can also introduce new risks and amplify existing inequalities (SPOR PIHCI Canada n.d.; Crawford and Serhal 2020; Fujioka et al. 2020; Hashiguchi 2020; Nouri et al. 2020; Srinivasan et al. 2020; Wijesooriya et al. 2020). Since the beginning of the pandemic, follow-up protocols for patients with chronic diseases, such as diabetes, and hypertension, have been developed by experts to secure telecare practices (Kiran et al. 2020; Omboni et al. 2020).
Many of the limitations reported in the present study relate to difficulties in establishing a reliable diagnosis using telehealth due to limited information gathered during the telehealth consultation, risk of errors and difficulty establishing trust relationships; these have also been reported in other studies (Bergman et al. 2020; Shankar et al. 2020; Srinivasan et al. 2020). Telehealth mainly involved using the telephone during the early months of the pandemic. Widespread use of telephone consultations may reflect ease of access to this technology, which makes it a practical choice for most patients. Although a telephone conversation may be appropriate for some consultations, additional visual cues or physical information are necessary for others (Hollander and Carr 2020; Nangalia et al. 2010). While video consultations can provide important additional information, providers and patients may require support to use them efficiently and effectively (Shankar et al. 2020). Recommendations are needed about what conditions can be addressed using virtual versus in-person visits and about practices to make video consultations more accessible.
Telehealth has changed PHC providers' use of their senses to gather the information needed to assess a patient's health status (Kelly and Gormley 2020). New knowledge and skills have to be developed to deliver quality telehealth. Before the pandemic, there was no mandatory academic training in the use of information and communication technologies in medical practice in Quebec (Bourassa Forcier et al. 2021). Since the beginning of the pandemic, the Collège des médecins du Québec (CMQ) has offered elective training (Bourassa Forcier et al. 2021; Collège des médecins du Québec 2021) focused on rules to be respected during telehealth consultations. The European Association for Communication in Healthcare (EACH n.d.) as well as the Academy of Communication in Healthcare (ACH 2021) have developed resources, e-learning courses, webinars and documents to help healthcare professionals provide quality telehealth consultations. Beyond the pandemic context, guidelines for prescribing telehealth are needed to standardize practices and achieve complementarity with in-person consultations (McMahon et al. 2020; Richard and Lussier 2015).
Finally, the use of telehealth modalities is greatly affected by the policies, regulations and funding models in place in a given jurisdiction (Hashiguchi 2020). It also hinges on factors such as technical capabilities, legitimacy as a new consultation practice (which suffers from concerns around safety or clinician training and preparation), remuneration and organization of the health system to enable appropriate staffing and support (Kho et al. 2020; Smith et al. 2020). After the outbreak of the pandemic in Quebec, several barriers to telehealth adoption were quickly removed; a new policy to facilitate sharing clinical information and a new fee code to allow physicians to bill for telehealth activities were established. A list of acceptable platforms as well as guides to safe and confidential use of these platforms were produced by the CMQ and Ministry of Health and Social Services (Collège des médecins du Québec 2020; Gouvernement du Québec 2020). While these key measures facilitated the rapid adoption of telehealth during the pandemic, technical, financial, human and organizational challenges still need to be addressed to ensure optimal use of video consultation in the future (Kho et al. 2020).
The rapid deployment of telehealth allowed little time to plan implementation strategies. However, it creates an enormous opportunity to share lessons learned across disparate settings, with the collective goal of improving the use of telehealth and identifying promising practices that can be scaled up for widespread use. Almost all PHC providers intend to continue using telehealth after the pandemic. This presents a unique opportunity to facilitate the spread of local and emergent best practices, and create a policy environment to support knowledge transfer and dissemination (Hashiguchi 2020). We will also need to pay special attention to train patients in the use of these new modalities and the appropriateness of the reason for telehealth consultations.
Limitations of The Study
Almost 45% of PHC provider responses to the e-survey were received in the summer of 2020, when rates of COVID-19 infection were especially high (Audibert et al. 2020). Particular aspects of this study may limit the generalizability of findings. Firstly, it was conducted in teaching PHC clinics in Quebec that have certain characteristics – notably their teaching mission and the broad range of PHC providers working alongside physicians – that distinguish them from other clinical settings (Abou Malham et al. 2018). Secondly, the participating U-FMGs were located in both rural and urban areas, but information was not collected to enable analysis of the differences between these settings. Although these were teaching settings, no information was collected from family medicine residents or other students in these U-FMGs, and no information was available on the challenges of supervising residents conducting virtual consultations.
Conclusion
This study shows significant differences in the use of telehealth by all PHC providers before and during the first few months of the COVID-19 pandemic. The pandemic poses an enormous challenge for health services, but it also represents an opportunity to thoroughly integrate telehealth into teaching and other primary healthcare clinics. This study describes the swift implementation of telehealth in U-FMGs at the beginning of the pandemic, providing a baseline that will facilitate the transformation to be tracked over time. This rapid deployment has enabled providers to assess ways in which virtual consultations can make their everyday practice safer and better, and has led to an increased awareness of their limitations. It now seems clear that telehealth has a place in U-FMGs in Quebec and beyond and that much can be done to maximize its potential.
Acknowledgement
This study was supported by a grant from the Canadian Institutes of Health Research (CIHR, #399757) and Réseau-1 Quebec. The authors are grateful to the CIHR for funding Mylaine Breton's Canada Research Chair in Clinical Governance on Primary Health Care.
Contributor Information
Mylaine Breton, Associate Professor, Department of Community Health Sciences, Université de Sherbrooke Longueuil, QC.
Nadia Deville-Stoetzel, Research Professional, Université de Sherbrooke, Longueuil, QC; Doctoral Student, Department of Sociology, Université du Québec à Montréal, Montréal, QC.
Isabelle Gaboury, Professor, Department of Family and Emergency Medicine, Université de Sherbrooke, Longueuil, QC.
Mélanie Ann Smithman, Doctoral Student, Department of Community Health Sciences, Université de Sherbrooke, Sherbrooke, QC.
Janusz Kaczorowski, Professor, Department of Family and Emergency Medicine, Université de Montréal, Montréal, QC.
Marie-Thérèse Lussier, Director, Réseau de recherche en soins primaires de l'Université de Montréal (RRSPUM); Professor, Department of Family and Emergency Medicine, Université de Montréal, Montréal, QC.
Jeannie Haggerty, Professor, Department of Family Medicine, McGill University, Montreal, QC.
Aude Motulsky, Adjunct Professor, Department of Management Evaluation and Health Policy, School of Public Health of the Université de Montréal, Montréal, QC.
Peter Nugus, Associate Professor, Department of Family Medicine, McGill University, Montreal, QC.
Géraldine Layani, Clinical Adjunct Professor, Department of Family and Emergency Medicine, Université de Montréal, Montréal, QC.
Guy Paré, Professor, Department of Information Technologies, HEC Montréal, Montréal, QC.
Gabrielle Evoy, Student of Medicine, Université de Sherbrooke, Sherbrooke, QC.
Mylène Arsenault, Family Physician, UFM-G Herzl Family Practice Centre; Assistant Professor, Department of Family Medicine, McGill University, Montreal, QC.
Jean-Sébastien Paquette, Co-Director, Réseau de recherche axé sur les pratiques de première ligne de l'Université Laval; Associate Clinical Professor, Département médecine familiale et de médecine d'urgence (DMFMU), Université Laval, Québec City, QC.
Julien Quinty, Adjunct Professor, Department of Family Medicine and Emergency Medicine, Université Laval, Québec City, QC.
Marie Authier, Research Facilitator, Réseau de recherche en soins primaires de l'Université de Montréal (RRSPUM), Montreal, QC.
Nadjib Mokraoui, Research Facilitator and Coordinator, McGill Practice-Based Research Network (PBRN), Montreal, QC.
Mireille Luc, Deputy Director, Department of Family and Emergency Medicine, Practice-Based Research Network, Université de Sherbrooke, Sherbrooke, QC.
Marie-Eve Lavoie, Scientific Coordinator and Research Facilitator, Réseau de recherche en soins primaires de l'Université de Montréal (RRSPUM), Montreal, QC.
References
- Abou Malham S., Touati N., Maillet L., Breton M.. 2018. The Challenges of Implementing Advanced Access for Residents in Family Medicine in Quebec. Do Promising Strategies Exist? Medical Education Online 23(1). 10.1080/10872981.2018.1438719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Academy of Communication in Healthcare (ACH). 2021. Better Communication. Better Relationships. Better Care. Retrieved May 14, 2021. <https://achonline.org/COVID-19>.
- Anderson-Lewis C., Darville G., Mercado R.E., Howell S., Di Maggio S.. 2018. mHealth Technology Use and Implications in Historically Underserved and Minority Populations in the United States: Systematic Literature Review. JMIR MHealth and UHealth 6(6): e128. 10.2196/mhealth.8383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Audibert C., Glass D., Johnson T.P.2020. Method and Transparency of Online Physician Surveys: An Overview. Survey Methods: Insights from the Field. 10.13094/SMIF-2020-00001.
- Bergman D., Bethell C., Gombojav N., Hassink S., Stange K.C.. 2020. Physical Distancing with Social Connectedness. Annals of Family Medicine 18(3): 272–77. 10.1370/afm.2538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatia R.S., Chu C., Pang A., Tadrous M., Stamenova V., Cram P.. 2021. Virtual Care Use before and during the COVID-19 Pandemic: A Repeated Cross-Sectional Study. CMAJ Open 9(1): E107–14. 10.9778/cmajo.20200311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloem B.R., Dorsey E.R., Okun M.S.. 2020. The Coronavirus Disease 2019 Crisis as Catalyst for Telemedicine for Chronic Neurological Disorders. JAMA Neurology 77(8): 927–28. 10.1001/jamaneurol.2020.1452. [DOI] [PubMed] [Google Scholar]
- Bourassa Forcier M., Laberge M., Adisso L., Attisso E., Bourdeau-Chabot M., Cardenas Benoit C. et al. 2021. Encadrement normatif et contractuel des pratiques de téléconsultation en clinique de première ligne. CIRANO. Retrieved May 14, 2021. <https://cirano.qc.ca/files/publications/2021RP-02.pdf>. [Google Scholar]
- Breton M., Lévesque J.-F., Pineault R., Hogg W.. 2011. Primary Care Reform: Can Quebec's Family Medicine Group Model Benefit from the Experience of Ontario's Family Health Teams? Healthcare Policy 7(2): e122–35. [PMC free article] [PubMed] [Google Scholar]
- Breton M., Maillet L., Duhoux A., Malham S.A., Gaboury I., Manceau L.M. et al. 2020. Evaluation of the Implementation and Associated Effects of Advanced Access in University Family Medicine Groups: A Study Protocol. BMC Family Practice 21: 41. 10.1186/s12875-020-01109-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breton M., Maillet L., Haggerty J., Vedel I.. 2014. Mandated Local Health Networks across the Province of Québec: A Better Collaboration with Primary Care Working in the Communities? London Journal of Primary Care 6(4): 71–78. 10.1080/17571472.2014.11493420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breton M., Pineault R., Levesque J.-F., Roberge D., Da Silva R.B., Prud'homme A.. 2013. Reforming Healthcare Systems on a Locally Integrated Basis: Is There a Potential for Increasing Collaborations in Primary Healthcare? BMC Health Services Research 13: 262. 10.1186/1472-6963-13-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breton M., Sullivan E.E., Deville-Stoetzel N., McKinstry D., DePuccio M., Sriharan A. et al. 2021. Telehealth Challenges during COVID-19 as Reported by Primary Healthcare Physicians in Quebec and Massachusetts [Under review]. BMC Family Practice 1–16. 10.21203/rs.3.rs-505725/v1. [DOI] [PMC free article] [PubMed]
- Canadian Medical Association (CMA). 2019. CMA Health Summit. Virtual Care in Canada: Discussion Paper. Retrieved August 13, 2020. <https://www.cma.ca/sites/default/files/pdf/News/Virtual_Care_discussionpaper_v2EN.pdf>.
- Canadian Medical Association (CMA). 2020, FebruaryVirtual Care: Recommendations for Scaling Up Virtual Medical Services. Retrieved August 13, 2020. <https://policybase.cma.ca/en/viewer?file=%2fdocuments%2fPolicyPDF%2fPD20-07.pdf#phrase=false>.
- Canadian Institute of Health Information. (CIHI). 2020, January30. Commonwealth Fund Survey 2019. Retrieved September 3, 2020. <https://www.cihi.ca/en/commonwealth-fund-survey-2019>.
- Collège des médecins du Québec. 2020, March31. Les téléconsultations réalisées par les médecins durant la pandémie de COVID-19. Guide à l'intention des médecins. Collège des médecins du Québec. Retrieved March 31, 2020. <http://www.cmq.org/publications-pdf/p-1-2020-03-31-fr-les-teleconsultations-realisees-par-les-medecins-durant-la-pandemie-de-covid-19.pdf>. [Google Scholar]
- Collège des médecins du Québec. 2021. Le médecin et les technologies de l'information. Retrieved May 14, 2021. <http://www.cmq.org/pdf/ateliers-dpc/atelier-medecin-technologies-information.pdf?t=1594400563071>.
- Crawford A., Serhal E.. 2020. Digital Health Equity and COVID-19: The Innovation Curve Cannot Reinforce the Social Gradient of Health. Journal of Medical Internet Research 22(6): e19361. 10.2196/19361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deldar K., Bahaadinbeigy K., Tara S.M.. 2016. Teleconsultation and Clinical Decision Making: A Systematic Review. Acta Informatica Medica 24(4): 286–92. 10.5455/aim.2016.24.286-292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillman D.A., Smyth J.D., Christian L.M.. 2014. Internet, Phone, Mail, and Mixed-Mode Surveys: The Tailored Design Method, 4th Edition. John Wiley & Sons, Inc. [Google Scholar]
- Donnelly C., Ashcroft R., Bobbette N., Mills C., Mofina A., Tran T. et al. 2021. Interprofessional Primary Care during COVID-19: A Survey of the Provider Perspective. BMC Family Practice 22: 31. 10.1186/s12875-020-01366-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EACH. n.d. COVID-19. Retrieved from May 14, 2021. <https://each.international/resources/covid-19/>.
- Fujioka J.K., Budhwani S., Thomas-Jacques T., De Vera K., Challa P., Fuller K. et al. 2020. Challenges and Strategies for Promoting Health Equity in Virtual Care: Protocol for a Scoping Review of Reviews. JMIR Research Protocols 9(12): e22847. 10.2196/22847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glazier R.H., Green M.E., Wu F.C., Frymire E., Kopp A., Kiran T.. 2021. Shifts in Office and Virtual Primary Care during the Early COVID-19 Pandemic in Ontario, Canada. CMAJ 193(6): E200–10. 10.1503/cmaj.202303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gouvernement du Québec. 2020, November19. Coronavirus (COVID-19 Guide de soutien pour la mise en œuvre des éléconsultations dans les établissements de santé du Québec dans le contexte de pandémie). Retrieved May 14, 2021. <https://telesantequebec.ca/wp-content/uploads/2020/12/20_210_133W_Guide_mise_en_oeuvre_teleconsultations_pandemie_MSSS_V2_VF.pdf>.
- Oliveira Hashiguchi T.2020. Bringing Health Care to the Patient: An Overview of the Use of Telemedicine in OECD Countries. OECD Health Working Papers, No. 116. OECD Publishing, 10.1787/8e56ede7-en. [Google Scholar]
- Hollander J.E., Carr B.G.. 2020. Virtually Perfect? Telemedicine for Covid-19. The New England Journal of Medicine 382: 1679–81. 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- Jaklevic M.C.2020. Telephone Visits Surge during the Pandemic, But Will They Last? JAMA 324(16): 1593–95. 10.1001/jama.2020.17201. [DOI] [PubMed] [Google Scholar]
- Kelly M.A., Gormley G.J.. 2020. In, But Out of Touch: Connecting with Patients during the Virtual Visit. Annals of Family Medicine 18(5): 461–62. 10.1370/afm.2568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kho J., Gillespie N., Martin-Khan M.. 2020. A Systematic Scoping Review of Change Management Practices Used for Telemedicine Service Implementations. BMC Health Services Research 20: 815. 10.1186/s12913-020-05657-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kichloo A., Albosta M., Dettloff K., Wani F., El-Amir Z., Singh J. et al. 2020. Telemedicine, the Current COVID-19 Pandemic and the Future: A Narrative Review and Perspectives Moving Forward in the USA. Family Medicine and Community Health 8(3): e000530. 10.1136/fmch-2020-000530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiran T., Moonen G., Bhattacharyya O.K., Agarwal P., Bajaj H.S., Kim J. et al. 2020. Managing Type 2 Diabetes in Primary Care during COVID-19. Canadian Family Physician 66(10): 745–47. [PMC free article] [PubMed] [Google Scholar]
- Levine R.E., Fowler F.J., Jr., Brown J.A.. 2005. Role of Cognitive Testing in the Development of the CAHPS® Hospital Survey. Health Services Research 40(6p2): 2037–56. 10.1111/j.1475-6773.2005.00472.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massachusetts Health Quality Partners. 2020. Together for Better Telehealth. Retrieved April 26, 2021. <http://bettertelehealth.mhqp.org/>.
- McMahon M., Nadigel J., Thompson E., Glazier R.H.. 2020. Informing Canada's Health System Response to COVID-19: Priorities for Health Services and Policy Research. Healthcare Policy 16(1): 112–24. 10.12927/hcpol.2020.26249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles M.B., Huberman A., Saldaña J.. 2014. Qualitative Data Analysis: A Methods Sourcebook (3rd ed.). SAGE Publications. [Google Scholar]
- Nangalia V., Prytherch D.R., Smith G.B.. 2010. Health Technology Assessment Review: Remote Monitoring of Vital Signs – Current Status and Future Challenges. Critical Care 14: 233. 10.1186/cc9208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nouri S., Khoong E.C., Lyles C.R., Karliner L.. 2020, May4. Addressing Equity in Telemedicine for Chronic Disease Management during the Covid-19 Pandemic. NEJM Catalyst Innovations in Care Delivery. Retrieved from May 14, 2021. <https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0123>.
- Omboni S., McManus R.J., Bosworth H.B., Chappell L.C., Green B.B., Kario K. et al. 2020. Evidence and Recommendations on the Use of Telemedicine for the Management of Arterial Hypertension. Hypertension 76(5): 1368–83. 10.1161/HYPERTENSIONAHA.120.15873. [DOI] [PubMed] [Google Scholar]
- Richard C., Lussier M.-T.. 2015. La communication professionnelle en santé, 2e Éd. Pearson. [Google Scholar]
- Shankar M., Fischer M., Brown-Johnson C.G., Safaeinili N., Haverfield M.C., Shaw J.G. et al. 2020. Humanism in Telemedicine: Connecting through Virtual Visits during the COVID-19 Pandemic. Annals of Family Medicine. Retrieved August 13, 2020. <http://hdl.handle.net/2027.42/154738>.
- Smith A.C., Thomas E., Snoswell C.L., Haydon H., Mehrotra A., Clemensen J. et al. 2020. Telehealth for Global Emergencies: Implications for Coronavirus Disease 2019 (COVID-19). Journal of Telemedicine and Telecare 26(5): 309–13. 10.1177/1357633X20916567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srinivasan M., Asch S., Vilendrer S., Thomas S.C., Bajra R., Barman L. et al. 2020. Qualitative Assessment of Rapid System Transformation to Primary Care Video Visits at an Academic Medical Center [Epub ahead of print 6 July 2020]. Annals of Internal Medicine 173: 527–35. 10.7326/M20-1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strategy for Patient-Oriented Research (SPOR) PIHCI Canada. n.d. COVID-19 Resources. Retrieved August 13, 2020. <http://spor-pihci.com/resources/covid-19/>.
- Veinot T.C., Ancker J.S., Bakken S.. 2019. Health Informatics and Health Equity: Improving Our Reach and Impact. Journal of the American Medical Informatics Association 26(8–9): 689–95. 10.1093/jamia/ocz132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veinot T.C., Mitchell H., Ancker J.S.. 2018. Good Intentions Are Not Enough: How Informatics Interventions Can Worsen Inequality. Journal of the American Medical Informatics Association 25(8): 1080–88. 10.1093/jamia/ocy052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wijesooriya N.R., Mishra V., Brand P.L.P., Rubin B.K.. 2020. COVID-19 and Telehealth, Education, and Research Adaptations. Paediatric Respiratory Reviews 35: 38–42. 10.1016/j.prrv.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]


