ABSTRACT
Human Papillomavirus (HPV) vaccination is recommended for adults aged 27–45 as a shared clinical decision with their healthcare provider. With the rise of social media as a vaccine information source, this study examined the extent of exposure to HPV vaccine content by social media platform and evaluated associations between HPV vaccine content on social media and HPV vaccine intent among both 27–45 year olds and their eligible children. U.S. participants (51% women, 9% Black, 8% Hispanic/Latinx), aged 27–45, were cross-sectionally surveyed online from April to May 2020 (n = 691). Outcomes included HPV vaccination intention (intend/do not intend) for themselves and, among participants with unvaccinated children aged 9–17 (n = 223), their eligible children. Adjusted odds ratios for HPV vaccine content and both outcomes were calculated. Extent of HPV vaccination exposure on social media was not associated with intention to vaccinate for HPV. Seeing mostly negative/mixed information about the HPV vaccine on social media was associated with lower odds of vaccination intention for adults (aOR = 0.34, 95% CI 0.15, 0.79) and adolescents (aOR = 0.34, 95% CI 0.21, 0.53). Viewing HPV vaccine information from social media as not credible was associated with lower odds of vaccine intent for adults (aOR = 0.17, 95% CI 0.07, 0.41) and adolescents (aOR = 0.16, 95% CI 0.10, 0.29). Although extent of HPV vaccine exposure on social media was not associated with vaccination outcomes, findings support developing quality social media strategies that increase the dissemination of positive and credible information in favor of HPV vaccination.
KEYWORDS: human papillomavirus, HPV vaccine, vaccination, social media, credibility, health information
Introduction
Human papillomavirus (HPV) is the most common sexually transmitted infection in the United States (U.S.).1 While low-risk strains of HPV are responsible for genital warts, high-risk strains of HPV can cause anogential and oropharyngeal cancers.2 Specifically, there are approximately 34,800 HPV-attributable cancers diagnosed annually in the U.S.2 To prevent some of these HPV-attributable cancers, a nonvalent HPV vaccine is recommended by the Advisory Committee on Immunization Practices (ACIP) for 11–12 year olds as routine vaccination.3 According to ACIP, previously unvaccinated persons can receive the vaccine until age 26 for catch-up vaccination.3 Most recently, due to the emerging evidence of efficacy in older populations, adults ages 27–45 years old can receive the HPV vaccine based on a shared clinical decision with their healthcare provider.4
Both global5 and national working groups6 have identified social media as a top priority to disseminate accurate information to strengthen parents’ confidence in the vaccine and combat non-credible misinformation presented across different social media platforms.7–9 Social media use is common among adults in the U.S., with recent research indicating that 78% of adults age 30–49 report using at least one social media platform.10 Social media users frequently learn about others’ interests, hobbies, social lives, and importantly, beliefs on important topics, such as HPV vaccination.11–13
When looking at specific platforms among U.S. adults, 69% reported using Facebook, 37% reported using Instagram, and 22% reported using Twitter.14 Facebook’s features include posting photos, status updates, and creating events and groups whereas Instagram is a platform where users share photos with their followers and Twitter is a ‘microblogging’ system that allows users to send and receive short, 280-character posts. Notably, women were more likely to report using Facebook and Instagram relative to men, whereas men were slightly more likely to report using Twitter.14 Although adults are less likely to use Instagram and Twitter than young adults,14 the largest group of active Facebook users is between ages 25–44.15 For parents, mothers were more likely to use Facebook (81%) and Instagram (30%), compared to fathers – 66% and 19%, respectively.16 For many users, social media is part of their daily routine; roughly three-quarters of Facebook users, around six-in-ten Instagram users, and four-in-ten Twitter users visited these sites at least once a day.10 While there is evidence that social media use and race/ethnicity are associated with awareness of HPV,17 understanding end-user perceptions of exposure, credibility, and content polarity remains to be directly tested. Thus, social media may be a particularly important and unique communication channel through which users can share and receive stories about HPV vaccines for themselves and their children.18
Although we are beginning to understand the role social media may play on HPV vaccination attitudes and behaviors, there may also be differential associations with different social media platforms and HPV-related information exposure, credibility, and polarity of content (e.g., having been exposed to mostly positive or negative HPV vaccine information on social media), given the specific features of different social media platforms. A comparison of social media platforms found Twitter users to be more likely to connect with individuals with whom they have shared interests but not necessarily off-line relationships as compared to other sites including Facebook and Instagram.19 Since anywhere from one-quarter to one-half of Twitter posts are negative against the HPV vaccine,20 it is possible that most of these negative Tweets are coming from unknown individuals. In contrast, on Facebook, where nearly half of HPV vaccination posts are considered negative,21 anti-vaccine content may be more likely to be posted by peers since individuals are the most likely to interact with friends or known others. When examining different reasons for using individual platforms, people report being the most likely to use Facebook to share content with known others whereas they are most likely to use Twitter to get news and Instagram to view photos.22 As such, it is possible that exposure to HPV content on Instagram may not be as prevalent as it is on other platforms and that exposure to HPV vaccination content also varies across other platforms.
Because health information communicated in interactive platforms like social media is of questionable accuracy, as it is often exchanged without the participation of health professionals or health organizations,23,24 understanding the type and credibility of HPV vaccination content on social media remains an important avenue of research. Given that 72% of U.S. adults reported having searched for health information online25 coupled with the potential for exposure to health information on social media to shape knowledge, attitudes, and beliefs, it is of utmost importance to examine specific social media factors that may improve the likelihood of self-vaccination and parents vaccinating their children against HPV.
To better understand exposure to HPV vaccination content across different social media platforms and potential associations between perceived polarity and credibility of HPV vaccine information on social media and vaccination likelihood and behaviors, this current study describes perceived exposure of HPV vaccine posts on commonly utilized social media, and examines likelihood to get HPV vaccination for (1) adults aged 27–45 and (2) currently unvaccinated children aged 9–17, eligible for vaccination. It is hypothesized that, when adjusting for demographic variables, social media factors such as polarity of HPV vaccine content and perceived social media information credibility will be associated with uptake for both adults aged 27–45 and their adolescent children.
Methods and materials
Sample
Data from the present study were drawn from a cross-sectional survey conducted among adults 27–45 years of age who had not received HPV vaccination previously, using Qualtrics Online Panel. Qualtrics provides small compensation for their participation. Participant recruitment was conducted between April-May 2020, and the study received prior approval from the local Institutional Review Board. Non-Hispanic Black and Hispanic/Latinx groups were oversampled due to higher HPV-related disparities among those populations.26,27
Black people make up 13.4% of the population but account for a higher rate of cervical cancer deaths when compared to White women.28 Hispanic people constitute almost one-fifth (18.3%) of the U.S. population,28 but reported the highest incidence (8.9 per 100,000 women) of cervical cancer rates in 2017 in the U.S.29 Furthermore, disparities in HPV vaccination rates exist among Black and Hispanic adolescents: Black and Hispanic adolescents were 52% and 25% (respectively) less likely to complete HPV vaccination three-shot series when compared to non-Hispanic White adolescents.30 Moreover, disparities in HPV vaccination rates among Black and Hispanic populations may also be associated with several underlying socioeconomic disparities in education, poverty,31 HPV awareness,17 and access to care32 compared to non-Hispanic White populations.
To clarify the specific target population regarding ethnicity, this study survey asked whether people identified as Hispanic or Latinx. Terminology such as “Hispanic” and “Latinx” are sometimes used interchangeably, but it is important to acknowledge each’s distinct definitions.33 The term “Hispanic” was derived by the U.S. Census Bureau and frequently utilized in scientific research and national survey data: this population includes people from Spain and Latin America, excluding countries not colonized by Spain (e.g., Brazil), regardless of race. “Latinx” (formerly, Latino/Latina) is a terminology applying to Latin American countries only, thus not including Spain, regardless of race.33
Measures
There were two outcomes of interest: likelihood of vaccinating themselves based on recent guideline changes and likelihood of vaccinating their eligible adolescent child for the subset of participants with children eligible for HPV vaccination. The first outcome variable asked, “Based on what you know about HPV vaccination right now, how likely is it that you will get vaccinated against HPV in the next six months?” The second outcome asked, “How likely is it your child will receive the HPV shot in the next 12 months?” The five response options for both outcomes ranged from “very likely” to “very unlikely.” Both the outcomes were dichotomized based on bimodal distribution of the data, with “very likely” and “likely” categorized as “likely” and “neither likely nor unlikely,” “unlikely,” and “very unlikely” categorized as “unlikely.”
To assess exposure to HPV vaccination content on social media, participants were asked to select which social media platforms they have used in the last week, and for each selected social media platform, participants were asked how often they saw information about HPV vaccines with the response options ranging from “more than once a day” to “never.” Frequencies for each social media platform were calculated using the following categories: “one or more times a day,” “less than once a day or at least once a week,” “less than once a week or at least once ever,” and “never.” Cell sizes were limited when assessing exposure to HPV vaccine content on social media on the top three social media platforms, so a single dichotomous variable (exposure to posts on Facebook, Instagram, and/or Twitter; no exposure on Facebook, Instagram, and/or Twitter) was utilized as a proxy in the final model to account for HPV vaccination content exposure on social media.
To assess polarity of HPV vaccination information on social media, participants were asked, “The HPV vaccine content that I see on social media is … ” (dichotomized to “mostly positive” or “mostly negative/mixed” to account for bimodal distribution). Perceived credibility was assessed using the question, “Please rate how much you agree with … HPV vaccine information I see on social media is credible,” with responses on a 5-category Likert scale, dichotomized to “agree” or “disagree”. To assess whether the internet in general was used as a source of information for HPV vaccination, participants were asked, “Where would you like to get more information on HPV vaccination … internet” (“yes”/”no”). Participants were also asked about whether they were aware of recent guideline changes for adults aged 27–45: “There is an HPV vaccine that is currently approved by the Food and Drug Administration for men and women ages 27 to 45 years old” (responses operationalized into “yes” or “no/don’t know”).
The demographic covariates included age in years, sex assigned at birth (“female,” “male”), race (“White,” “Black,” “Other, Bi-multiracial”), ethnicity (“Hispanic/Latinx,” “non-Hispanic/Latinx”), insurance (“public,” “private,” “uninsured/don’t know”), education (“high school or less,” “some college,” “college,” “graduate degree”), and marital status (“single,” “married,” “other”). Due to response distributions and small cell sizes with outcomes, some demographic variables were further recategorized dichotomously: race (“White,” “non-White”), education (“less than a 4-year degree,” “4-year degree or higher”), and marital status (“married,” “not married”).
Data analysis
All data analysis was conducted using SAS 9.4.34 General descriptive statistics calculated for the entire sample (n = 691) include frequency and percentages of HPV vaccine exposure across the 10 included social media platforms and “Other” category. Participant demographics were cross tabulated for the entire sample of adults and a subsample of participants with children aged 9–17 eligible for HPV vaccination (n = 230). Based on frequencies of social media use in the last two weeks, model building was performed, incorporating the most frequently utilized social media platforms (i.e., Facebook, Instagram, and Twitter). Due to issues regarding cell sizes accounting for both outcomes, the sample was restricted to reporting either Facebook, Instagram, or Twitter use (n = 636, 92% of the original adult sample; and n = 223, 97% of the original subset parent sample, respectively) in adjusted analyses. Furthermore, cell sizes were limited when assessing HPV vaccine information frequency for ever having seen HPV vaccine information on the top three social media platforms, so a single dichotomous variable (exposure on Facebook, Instagram, and Twitter/no exposure on Facebook, Instagram, and Twitter) was utilized as a proxy in the final model to account for HPV vaccination exposure on social media.
Model selection was conducted using a Purposeful Selection macro,35 which is a more robust form of automated selection. This macro automates the selection of covariates during each step by fitting a univariate model with each covariate, selecting covariates for a multivariate model significant at a chosen alpha inclusion and retention level, and fitting a reduced model while assessing confounding set at a specific level by change in parameter estimates.35 This macro repeats this process until the final model has significant covariates/confounders and places these back in the model individually, matching with previous criteria, and reducing the model again.28 This ultimately leads to a final “main effects model.”35
After starting with a full model that included demographic variables frequently utilized in HPV vaccine research and the different internet and social media variables noted in the measures section, the best model fit was determined. Initial selection parameters were set to default inclusion, retention, and confounding values (0.25, 0.1, and 0.2, respectively). In addition to literature considerations and purposeful selection criteria, models were further evaluated for fit using c values, which assess receiver operating curve values and range from 0.5, a random model prediction, to 1, a perfectly discriminating model.36 Final models were selected based on having a C-value greater than 0.85, requiring the increase of inclusion criteria for the purposeful selection macro to change to 0.4 and retention criteria to adjust to 0.1 for both adult and child models (final C-values 0.869 and 0.853, respectively). Adjusted odds ratios and 95% confidence intervals for both outcomes were calculated based on final models for adult and child HPV vaccine outcomes, adjusting for covariates identified by the model selection process.
Results
Approximately 43% (296 of the 691 participants) were likely to get the HPV vaccine in the next 6 months after learning about the change in guidelines (Table 1). Of the 230 participants with children eligible for HPV vaccination that had yet to receive the HPV vaccine, 126 (55%) were likely to get their child vaccinated for HPV in the next year. Furthermore, adults who reported they were likely to get themselves vaccinated were more commonly male (61.8%), of Hispanic/Latinx ethnicity (89.2%), have a graduate degree (38.9%), carry private insurance (64.5%) and be married (72.0%). Parents who reported they were likely to vaccinate their eligible child were more commonly male (73.0%), have a graduate degree (56.4%), carry private insurance (69.1%) and be married (89.7%). There were significant (p < .05) bivariate associations between sex, Hispanic/Latinx ethnicity, education level, insurance status, and marital status with likelihood to vaccinate themselves and similar significant associations (minus Hispanic/Latinx status) with likelihood to vaccinate their child for HPV.
Table 1.
Descriptive frequencies and percentages of participant demographics by both outcomes among a sample of U.S. Adults aged 27–45, 2020
| Likelihood of vaccinating eligible adolescent (n = 230) |
Likelihood of vaccinating themselves (N = 691) |
|||
|---|---|---|---|---|
| Likely, n (%) |
Unlikely, n (%) |
Likely, N (%) |
Unlikely, N (%) | |
| Agea | 37.2 (4.6) | 38.1 (4.6) | 36.7 (4.8) | 36.4 (5.4) |
| Sex assigned at birth | ||||
| Male | 92 (73.0) | 34 (32.7) | 183 (61.8) | 157 (39.8) |
| Female | 34 (27.0) | 70 (67.3) | 113 (38.2) | 238 (60.3) |
| Race | ||||
| White | 105 (83.3) | 80 (76.9) | 229 (77.4) | 282 (71.4) |
| Black | 7 (5.6) | 10 (9.6) | 21 (7.1) | 39 (9.9) |
| Other | 7 (5.6) | 7 (6.7) | 23 (7.8) | 45 (11.4) |
| Mixed race | 7 (5.6) | 7 (6.7) | 23 (7.8) | 20 (7.3) |
| Hispanic/Latinx ethnicity | ||||
| No | 111 (88.1) | 96 (92.3) | 264 (89.2) | 369 (93.4) |
| Yes | 15 (11.9) | 8 (7.7) | 32 (10.8) | 26 (6.6) |
| Education level | ||||
| High school degree or less | 9 (7.1) | 19 (18.3) | 39 (13.2) | 101 (25.6) |
| Some college/trade school/2-year degree | 11 (8.7) | 39 (37.5) | 53 (17.9) | 123 (31.1) |
| 4-year degree | 35 (27.8) | 20(19.2) | 89 (30.1) | 110 (27.9) |
| Graduate school | 71 (56.4) | 26 (25.0) | 115 (38.9) | 61 (15.4) |
| Insurance status | ||||
| Private insurance | 87 (69.1) | 50 (48.1) | 191 (64.5) | 190 (48.1) |
| Public insurance | 34 (27.0) | 39 (37.5) | 81 (27.4) | 129 (32.7) |
| None/don’t know | 5 (4.0) | 15 (14.4) | 24 (8.1) | 76 (19.2) |
| Marital Status | ||||
| Single | 11 (8.7) | 13 (12.5) | 68 (23.0) | 157 (39.8) |
| Married | 113 (89.7) | 71 (68.3) | 213 (72.0) | 194 (49.1) |
| Other | 2 (1.6) | 20 (19.2) | 15 (5.1) | 44 (11.1) |
aValues displayed are mean (standard deviation).
Among participants who used social media within the last week, Table 2 depicts the frequency of seeing HPV vaccine posts for each social media platform. The top three social media platforms that participants reported using were Facebook (84%), Instagram (68%), and Twitter (49%). Figure 1 depicts the distribution of participants’ frequency of exposure to HPV vaccine related posts on the 3 top social media platforms (e.g., Facebook, Instagram, Twitter) by each of the outcomes (i.e., likelihood to get vaccinated for HPV, likelihood to vaccinate their eligible child for HPV). For the unadjusted bivariate chi-square analyses, HPV vaccine exposure on one of the three of the top social media platforms (Facebook, Instagram, and/or Twitter) was significantly associated with both the child and adult outcomes (p < .05).
Table 2.
Descriptive frequencies and percentages of exposure to HPV vaccine information on social media among a sample of U.S. adults aged 27–45, 2020
| One or more times a day, N (%) |
Less than once a day, at least once a week, N (%) | Less than once a week, at least once ever, N (%) | Never, N (%) | Total (N = 691), N (%) | |
|---|---|---|---|---|---|
| 97 (16.8) | 81 (14.0) | 128 (22.1) | 273 (47.2) | 579 (83.8) | |
| 90 (19.1) | 67 (14.2) | 65 (13.8) | 249 (52.9) | 471 (68.2) | |
| 88 (25.9) | 69 (20.3) | 57 (16.8) | 126 (37.1) | 340 (49.3) | |
| Snapchat | 61 (20.5) | 50 (16.8) | 32 (10.7) | 155 (52.0) | 298 (43.1) |
| 54 (20.0) | 33 (12.2) | 38 (14.1) | 145 (53.7) | 270 (39.1) | |
| 60 (26.0) | 40 (17.3) | 24 (10.4) | 107 (46.3) | 231 (33.4) | |
| 47 (21.8) | 35 (16.2) | 37 (17.1) | 97 (44.9) | 216 (31.3) | |
| Tumblr | 34 (35.1) | 16 (16.5) | 15 (15.5) | 32 (33.0) | 97 (14.0) |
| Ask.fm | 39 (48.2) | 25 (30.9) | 8 (9.9) | 9 (11.1) | 81 (11.7) |
| Yik Yak | 26 (51.0) | 11 (21.6) | 4 (7.8) | 10 (19.6) | 51 (7.4) |
| Other | 33 (33.0) | 20 (20.0) | 17 (17.0) | 30 (30.0) | 100 (14.5) |
Figure 1.
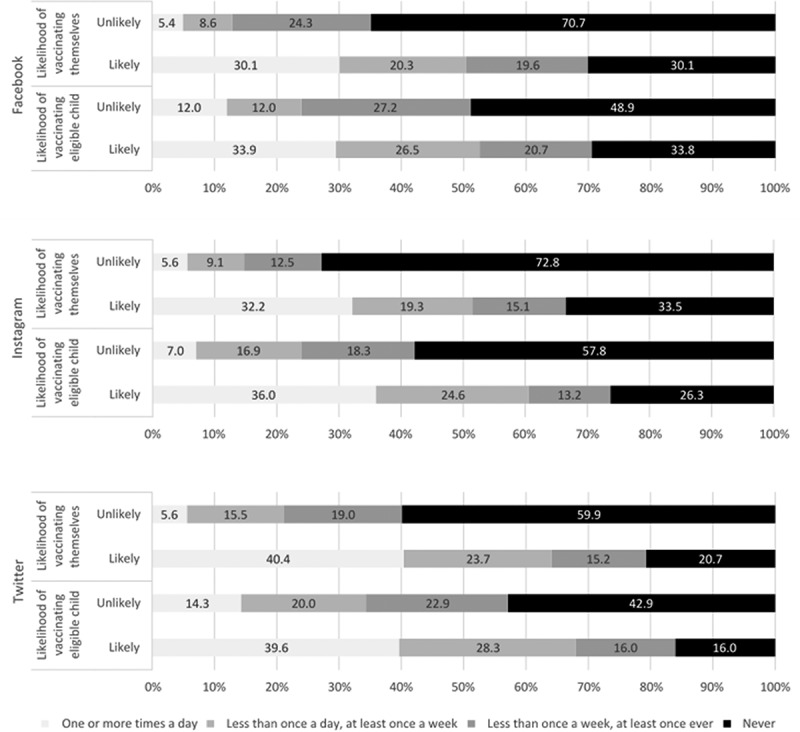
Descriptive frequencies by two HPV vaccine outcomes for the top three social media platforms (Facebook, Instagram, Twitter) among a sample of U.S. adults aged 27–45, 2020
Vaccination likelihood – adults aged 27-45 years
Table 3 displays adjusted models that assessed associations between social media perceptions (e.g., credibility, polarity, etc.), information seeking, and knowledge about HPV vaccine information and both HPV vaccine likelihood outcomes. Exposure to HPV vaccine information on Facebook, Twitter, and/or Instagram was no longer statistically significant in both adjusted models for adult and adolescent outcomes. Regarding polarity of HPV information, participants who had seen “mostly negative or mixed” HPV vaccination information on social media had lower odds (aOR = 0.34, 95%CI 0.15, 0.79) of reporting a likelihood to vaccinate than those who had seen “mostly positive” HPV vaccine information. Moreover, those who stated that they did not agree that HPV vaccine information on social media was credible had lower odds (aOR = 0.16, 95%CI 0.10, 0.29) of reporting a likelihood to vaccinate than those who said the information was credible. Additionally, both those who reporting using the internet as a source of HPV vaccine information (aOR = 1.76, 95%CI 1.10, 2.84) and those who were aware of recent HPV guideline changes (aOR = 2.05, 95%CI 1.29, 3.26) had higher odds of having a likelihood of vaccination than those who reported “no” to these questions. Furthermore, Hispanic/Latinx ethnicity (aOR = 2.22, 95%CI 1.08, 4.56) and being married (aOR = 0.60, 95%CI 0.38, 0.94) were both significantly associated with a higher likelihood to vaccinate.
Table 3.
Adjusted odds ratios and 95% confidence intervals for likelihood to vaccinate themselves and their eligible adolescents for HPV among a sample of U.S. adults aged 27–45, 2020
| Intent of vaccinating eligible adolescent (n = 223) | Intent of vaccinating themselves (N = 636) | |
|---|---|---|
| Social Media-Related Covariates | ||
| Ever seen HPV Vaccine posts on social media | ||
| No | Reference | Reference |
| Yes | 0.56 (0.22, 1.41) | 1.53 (0.88, 2.67) |
| HPV vaccine information on social media | ||
| Mostly positive | Reference | Reference |
| Mostly negative or mixed | 0.34 (0.15, 0.79)* | 0.34 (0.21, 0.53)* |
| HPV vaccine information on social media is credible | ||
| Agree | Reference | Reference |
| Neutral/Disagree | 0.17 (0.07, 0.41)* | 0.16 (0.10, 0.29)* |
| Source of HPV vaccine information: Internet | ||
| No | Reference | Reference |
| Yes | 0.48 (0.19, 1.22) | 1.76 (1.10, 2.84)* |
| Aware of recent HPV guideline changes | ||
| No | – | Reference |
| Yes | – | 2.05 (1.29, 3.26)* |
| Demographic Covariates | ||
| Age | 0.93 (0.85, 1.02) | 1.00 (0.95, 1.04) |
| Sex assigned at birth | ||
| Male | Reference | Reference |
| Female | 0.32 (0.13, 0.78)* | 0.73 (0.46, 1.15) |
| Race | ||
| White | Reference | Reference |
| Nonwhite | 1.13 (0.43, 3.00) | 0.79 (0.48, 1.30) |
| Hispanic ethnicity | ||
| Non-Hispanic | Reference | Reference |
| Hispanic | 1.82 (0.57, 5.74) | 2.22 (1.08, 4.56)* |
| Completed bachelor’s degree | ||
| No | Reference | Reference |
| Yes | 1.93 (0.68, 5.46) | 1.10 (0.68, 1.79) |
| Insurance status | ||
| Private insurance | Reference | Reference |
| Public insurance | 0.66 (0.27, 1.65) | 1.35 (0.80, 2.29) |
| None/Don’t know | 0.28 (0.06, 1.37) | 1.05 (0.52, 2.12) |
| Marital status | ||
| Married | Reference | Reference |
| Not married | 0.49 (0.15, 1.57) | 0.60 (0.38, 0.94)* |
* statistical significance (p < .05).
Vaccination likelihood – eligible adolescents
Regarding likelihood of vaccinating their eligible adolescents, participants who had seen “mostly negative or mixed” HPV vaccination information on social media had lower odds (aOR = 0.34, 95%CI 0.15, 0.79) of reporting a likelihood to vaccinate their child than those who had seen “mostly positive” HPV vaccine information. Furthermore, those who stated that they did not agree that HPV vaccine information on social media was credible had lower odds (aOR = 0.17, 95%CI 0.07, 0.41) of reporting a likelihood to vaccinate their child than those who said the information was credible. After adjusting for other factors, female sex assigned at birth was associated with less likelihood to vaccinate an eligible child (aOR = 0.32, 95%CI 0.13, 0.78).
Discussion
HPV vaccination uptake is critical in reducing HPV-related cancers and other HPV-related sequelae. The use of social media, a common channel through which information about HPV vaccination is disseminated, is highly prevalent among adults aged 27–45. Given recent changes in HPV vaccination guidelines for adults in this age range and the role of parental decision-making for vaccination, understanding factors related to HPV vaccination uptake is of critical importance. Two key factors related to both likelihood of respondents to vaccinate an eligible child and their likelihood to vaccine themselves were polarity of content and perceived credibility. An awareness of recent HPV guideline changes and use of the internet as a source of HPV information was associated with parents’ likelihood to vaccinate themselves. Participants of Hispanic/Latinx ethnicity and married participants were significantly more likely to vaccinate themselves, whereas female sex assigned at birth was associated with less likelihood of vaccinating their adolescent child.
Findings from this study demonstrate that frequency of exposure to HPV vaccine posts varied between different social media platforms. Furthermore, unadjusted associations for frequency of exposure to HPV vaccine posts were significant for the top three platforms: Facebook, Instagram, and Twitter. However, when adjusting for perceived social media information credibility and content polarity, as well as key demographic covariates, ever seeing HPV vaccination content, regardless of frequency, on social media was not significantly associated with vaccination outcomes. This highlights the importance of credibility and polarity of HPV vaccine content on social media and indicates that those factors may be more impactful than just sheer exposure to content. The importance of credibility is not entirely surprising given that a Twitter-based intervention found increased peer-to-peer dissemination of factual cervical cancer information posted by reputable and trusted organizational social media accounts37 but noted that the dose of messages provided in the intervention may not be realistic or ecologically valid in the social media landscape where cervical cancer messages are likely to be fewer than provided in the intervention.
In addition to content polarity and perceived credibility, key demographic covariates were significant. Given the new ACIP recommendation that adults ages 27–45 years old can receive the HPV vaccine based on a shared clinical decision with their healthcare provider,4 there is a need to explore how HPV vaccine information exposure, including on social media, may be associated with this new recommendation. In this study, 27–45 year olds were more likely to receive the HPV vaccine if they were aware of HPV vaccine guideline change for this age group. Note that previous research has shown only two-thirds of U.S. adults in this age group are aware of HPV vaccination in general,38 yet in this study, only 40% were aware of the new HPV vaccination guidelines. The current results should be taken into account in tandem with results from other work utilizing a large national sample, which indicated that HPV awareness among adults with children is associated with reported social media use and Black or Hispanic racial/ethnic status.17 Findings from the present study support the possibility that increased awareness through social media via information that is perceived as positive and credible may serve as a facilitator to increasing HPV awareness and promoting HPV vaccine uptake in adults as well as adolescents. In addition to overall awareness of the new guideline, social media-specific factors were related to likelihood to vaccinate, including exposure to more positive information on HPV vaccination; agreeing that HPV vaccine information on social media is credible; and using the Internet as a source of HPV vaccine information. Thus, persons who may have been exposed to more positive information on HPV vaccination on social media and have the health literacy skills to find information online may be a group more inclined for vaccination.
An understanding of how social media strategies may be used to sway parents who may be more amenable to changing their vaccine beliefs is an important next step in targeting misinformation about the HPV vaccine. Pregnant women who were assigned to social media interventions including blogs, forums, chat functions, and direct connection to vaccination experts (i.e., credible sources) were more likely to be up-to-date on infant immunizations than those who received usual routine care.39,40 Although these studies were not directly related to HPV vaccination and focused on pregnant women instead of parents of older children, these findings suggest that a similar intervention for parents and/or caregivers of vaccination eligible children as well as those adults eligible for the vaccination may be similarly effective in increasing HPV vaccination uptake.
Despite making important contributions to the literature, there are several limitations of the current study. First, since the data collected were self-report and were acquired through an online survey, there is the potential of sampling bias, which could result in data not representative of the general population. In addition, since the study was cross-sectional in nature, temporal sequence and other aspects of causal inference could not be established. This research cannot determine whether there is a causal relationship between having access to HPV vaccination that is perceived to be uncredible and decision-making that results in lower vaccine uptake. Future studies should seek to understand this complex relationship with specific research designs such as experimental or randomized controlled trials which can elucidate causality. Another limitation is, though likelihood of vaccinating may be predictive of behavior, it is not itself behavior. Thus, future research using longitudinal designs and behavioral outcomes need to be conducted to determine how the factors included in this study related to actual vaccination behavior among parents and their children over time. Although social media has become a near ubiquitous influence, it is important to note that this study does not account for the influences of other sources of health information outside of social media, such as health care providers, friends, family, television or newspapers, that may also impact decisions to vaccinate. A final limitation is that multi-categorical variables needed to be dichotomized, which could result in respondents being misclassified into inappropriate categories.
Given the influence of social media on health behaviors of individuals, it is crucial to understand the exposure to and perceptions of HPV vaccine-related information on social media and the likelihood to get vaccinated. Providing more credible positive information and debunking misinformation regarding HPV vaccination on social media has potential to help improve the uptake of this primary prevention method. Thus, future interventions for promoting HPV vaccination should utilize social media to improve health literacy of individuals and help them make more informed decision about their vaccination choices. To counter lack of knowledge and negative, inaccurate, or uncredible messages, public health campaigns should focus on increasing exposure to positive, accurate, and credible information, especially about safety and efficacy,20 through social media platforms. Since the current recommendations for HPV vaccination in this age group place the onus on the patient to discuss vaccination with their provider, having this exposure to positive and credible information online may prompt patient-provider conversations about HPV vaccination.
Disclosure of potential conflicts of interest
Author Erika Thompson is a consultant to Merck.
References
- 1.Satterwhite CL, Torrone E, Meites E, Dunne EF, Mahajan R, Ocfemia MC, Su J, Xu F, Weinstock H.. Sexually transmitted infections among us women and men: prevalence and incidence estimates, 2008. Sex Transm Dis. 2013;40(3):187–93. doi: 10.1097/OLQ.0b013e318286bb53. [DOI] [PubMed] [Google Scholar]
- 2.Senkomago V, Henley SJ, Thomas CC, Mix JM, Markowitz LE, Saraiya M.. Human papillomavirus-attributable cancers - United States, 2012-2016. Morb Mortal Wkly Rep. 2019;68(33):724–28. doi: 10.15585/mmwr.mm6833a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Petrosky E, Bocchini JA Jr., Hariri S, Chesson H, Curtis CR, Saraiya M, Unger ER, Markowitz LE. Use of 9-valent human papillomavirus (HPV) vaccine: updated HPV vaccination recommendations of the advisory committee on immunization practices. Morb Mortal Wkly Rep. 2015;64(11):300–04. PMCID: PMC4584883. [PMC free article] [PubMed] [Google Scholar]
- 4.Meites E, Szilagyi PG, Chesson HW, Unger ER, Romero JR, Markowitz LE. Human papillomavirus vaccination for adults: updated recommendations of the advisory committee on immunization practices. Morb Mortal Wkly Rep. 2019;68(32):698–702. doi: 10.1111/ajt.15633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization . HPV vaccine communication: special considerations for a unique vaccine. 2016 update; 2016. [accessed 2020Oct01]. https://www.who.int/immunization/documents/WHO_IVB_13.12/en/.
- 6.Reiter PL, Gerend MA, Gilkey MB, Perkins RB, Saslow D, Stokley S, Tiro JA, Zimet GD, Brewer NT. Advancing human papillomavirus vaccine delivery: 12 priority research gaps. Acad Pediatr. 2018;18(2):S14–S16. doi: 10.1016/j.acap.2017.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dunn AG, Surian D, Leask J, Dey A, Mandl KD, Coiera E. Mapping information exposure on social media to explain differences in HPV vaccine coverage in the United States. Vaccine. 2017;35(23):3033–40. doi: 10.1016/j.vaccine.2017.04.060. [DOI] [PubMed] [Google Scholar]
- 8.Ekram S, Debiec KE, Pumper MA, Moreno MA. Content and commentary: HPV vaccine and Youtube. J Pediatr Adolesc Gynecol. 2019;32(2):153–57. doi: 10.1016/j.jpag.2018.11.001. [DOI] [PubMed] [Google Scholar]
- 9.Margolis MA, Brewer NT, Shah PD, Calo WA, Gilkey MB. Stories about HPV vaccine in social media, traditional media, and conversations. Prev Med. 2019;118:251–56. doi: 10.1016/j.ypmed.2018.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Pew Research Center . Social media fact sheet; 2019. [accessed 2020 Oct 01]. https://www.pewresearch.org/internet/fact-sheet/social-media/.
- 11.Aydin S. A review of research on Facebook as an educational environment. Educ Technol Res Dev. 2012;60(6):1093–106. doi: 10.1007/s11423-012-9260-7. [DOI] [Google Scholar]
- 12.Nosko A, Wood E, Molema S. All about me: disclosure in online social networking profiles: the case of Facebook. Comput Human Behav. 2010;26(3):406–18. doi: 10.1016/j.chb.2009.11.012. [DOI] [Google Scholar]
- 13.Zhang H, Lu Y, Wang B, Wu S. The impacts of technological environments and co-creation experiences on customer participation. Inf Manage. 2015;52(4):468–82. doi: 10.1016/j.im.2015.01.008. [DOI] [Google Scholar]
- 14.Perrin A, Anderson M. Share of U.S. Adults using social media, including Facebook, is mostly unchanged since 2018; 2019. [accessed 2020 Oct 01]. https://www.pewresearch.org/fact-tank/2019/04/10/share-of-u-s-adults-using-social-media-including-facebook-is-mostly-unchanged-since-2018/.
- 15.Statista . Facebook user share in the United States 2020, by age and gender 2020; 2020. [accessed 2020 May 3]. https://www.statista.com/statistics/187041/us-user-age-distribution-on-facebook/.
- 16.Duggan M, Lenhart A, Lampe C, Ellison NB. Parents and social media. Pew Research Center; 2015. [accessed 2020 Oct 01]. https://www.pewresearch.org/internet/2015/07/16/parents-and-social-media/. [Google Scholar]
- 17.Lama M, Quinn SC, Nan X, Cruz-Cano R. Social media use and human papillomavirus awareness and knowledge among adults with children in the household: examining the role of race, ethnicity, and gender. Hum Vaccin Immunother. 2021;17(4):1014–24. doi: 10.1080/21645515.2020.1824498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dilley SE, Peral S, Straughn JM, Scarinci IC. The challenge of HPV vaccination uptake and opportunities for solutions: lessons learned from Alabama. Prev Med. 2018;113:124–31. doi: 10.1016/j.ypmed.2018.05.021. PMID: 29800594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Phua J, Jin SV, Kim JJ. Uses and gratifications of social networking sites for bridging and bonding social capital: a comparison of Facebook, Twitter, Instagram, and Snapchat. Comput Human Behav. 2017;72:115–22. doi: 10.1016/j.chb.2017.02.041. [DOI] [Google Scholar]
- 20.Ortiz RR, Smith A, Coyne-Beasley T. A systematic literature review to examine the potential for social media to impact HPV vaccine uptake and awareness, knowledge, and attitudes about HPV and HPV vaccination. Hum Vaccin Immunother. 2019;15(7–8):1465–75. doi: 10.1080/21645515.2019.1581543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Luisi MLR. From bad to worse: the representation of the HPV vaccine on Facebook. Vaccine. 2020;38(29):4564–73. doi: 10.1016/j.vaccine.2020.05.016. [DOI] [PubMed] [Google Scholar]
- 22.Tankovska H. U.S. social media activities 2019, by platform; 2019. [accessed 2020 Oct 01]. https://www.statista.com/statistics/200843/social-media-activities-by-platform-usa/.
- 23.Nicholson MS, Leask J. Lessons from an online debate about Measles–Mumps–Rubella (MMR) immunization. Vaccine. 2012;30(25):3806–12. doi: 10.1016/j.vaccine.2011.10.072. [DOI] [PubMed] [Google Scholar]
- 24.Witteman HO, Zikmund-Fisher BJ. The defining characteristics of Web 2.0 and their potential influence in the online vaccination debate. Vaccine. 2012;30(25):3734–40. doi: 10.1016/j.vaccine.2011.12.039. [DOI] [PubMed] [Google Scholar]
- 25.Fox S. The social life of health information. Pew Research Center; 2014. [accessed 2020 Oct 01]. https://www.pewresearch.org/fact-tank/2014/01/15/the-social-life-of-health-information/. [Google Scholar]
- 26.Cruz A, Chen D, Hsu P, Pandit V, Omesiete P, Vij P, Nfonsam V. Racial and gender disparities in the incidence of anal cancer: analysis of the Nationwide Inpatient Sample (NIS). J Gastrointest Oncol. 2019;10(1):37. doi: 10.21037/jgo.2018.10.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Islami F, Fedewa SA, Jemal A. Trends in cervical cancer incidence rates by age, race/ ethnicity,histological subtype, and stage at diagnosis in the United States. Prev Med. 2019;123:316–23. doi: 10.1016/j.ypmed.2019.04.010. [DOI] [PubMed] [Google Scholar]
- 28.U.S. Census Bureau . American Community Survey 2018; 2018. [accessed 2020 June 28]. https://data.census.gov/cedsci/table?q=Hispanic&hidePreview=false&tid=ACSDP1Y2018.DP05&t=Hispanic%20or%20Latino.
- 29.U.S. Cancer Statistics Working Group . U.S. cancer statistics data visualizations tool, based on 2019 submission data (1999-2017): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; 2020. [accessed 2020 June 1]. www.cdc.gov/cancer/dataviz. [Google Scholar]
- 30.Niccolai LM, Mehta NR, Hadler JL. Racial/ethnic and poverty disparities in human papillomavirus vaccination completion. Am J Prev Med. 2011;41(4):428–33. doi: 10.1016/j.amepre.2011.06.032. [DOI] [PubMed] [Google Scholar]
- 31.Benard VB, Johnson CJ, Thompson TD, Roland KB, Lai SM, Cokkinides V, Tangka F, Hawkins NA, Lawson H, Weir HK, et al. Examining the association between socioeconomic status and potential human papillomavirus‐associated cancers. Cancer. 2008;113(S10):2910–18. doi: 10.1002/cncr.23742. [DOI] [PubMed] [Google Scholar]
- 32.Kahn JA, Lan D, Kahn RS. Sociodemographic factors associated with high-risk human papillomavirus infection. Obstet Gynol. 2007;110(1):87–95. doi: 10.1097/01.AOG.0000266984.23445.9c. [DOI] [PubMed] [Google Scholar]
- 33.Santana D. What makes a latino, hispanic or latinx? Embracing diversity; 2017. [accessed 2020 June 28]. http://embracingdiversity.us/what-makes-a-latino-hispanic-latinx.
- 34.SAS Institute Incorporated . Base SAS 9.4 procedures guide: statistical procedures. Cary (NC): USA; 2013. [Google Scholar]
- 35.Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3(17):1–8. doi: 10.1186/1751-0473-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Janes H, Longton G, Pepe MS. Accommodating covariates in receiver operating characteristic analysis. Stata J. 2009;9(1):17–39. doi: 10.1177/1536867X0900900102. PMID: 20046933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang J, Le G, Larochelle D, Pasick R, Sawaya GF, Sarkar U, Centola D. Facts or stories? How to use social media for cervical cancer prevention: a multi-method study of the effects of sender type and content type on increased message sharing. Prev Med. 2019;126:105751. doi: 10.1016/j.ypmed.2019.105751. PMID: 31226342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thompson EL, Wheldon CW, Rosen BL, Maness SB, Kasting ML, Massey PM. Awareness and knowledge of HPV and HPV vaccination among adults ages 27-45 years. Vaccine. 2020;38(15):3143–48. doi: 10.1016/j.vaccine.2020.01.053. PMID: 32029321. [DOI] [PubMed] [Google Scholar]
- 39.Daley MF, Narwaney KJ, Shoup JA, Wagner NM, Glanz JM. Addressing parents’ vaccine concerns: a randomized trial of a social media intervention. Am J Prev Med. 2018;55(1):44–54. doi: 10.1016/j.amepre.2018.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Glanz JM, Wagner NM, Narwaney KJ, Kraus CR, Shoup JA, Xu S, O’Leary ST, Omer SB, Gleason KS, Daley MF. Web-based social media intervention to increase vaccine acceptance: a randomized controlled trial. Pediatr. 2017;140(6):e20171117. doi: 10.1542/peds.2017-1117. [DOI] [PMC free article] [PubMed] [Google Scholar]


