Abstract
Background and Objectives
Marital dissolution has become more common in midlife with the doubling of the divorce rate among middle-aged adults. Guided by the stress model that stipulates losing economic, social, and psychological resources lowers well-being, we posited that midlife adults who experienced divorce or widowhood were at greater risk of cognitive impairment than the continuously married. Subsequent repartnering was expected to negate the increased risk.
Research Design and Methods
We used data from the 1998–2016 Health and Retirement Study to estimate discrete-time event history models using logistic regression to predict cognitive impairment onset for men and women.
Results
Roughly 27% of men who experienced spousal death in midlife went on to experience mild cognitive impairment by age 65. For women, experiencing divorce or widowhood was associated with higher odds of cognitive impairment onset although these differentials were accounted for by economic, social, and psychological resources. Men and women who repartnered after marital dissolution did not appreciably differ from their continuously married counterparts in terms of their likelihoods of cognitive impairment onset.
Discussion and Implications
A stressful life event, midlife marital dissolution can be detrimental to cognitive well-being, placing individuals at increased risk of developing dementia in later life. The growing diversity of partnership experiences during the second half of life points to the continued importance of examining how union dissolution and formation shape health and well-being.
Keywords: Divorce, Health, Marriage, Social support, Widowhood
Marital dissolution is a stressful life event that has negative consequences for individual well-being, including mental and physical health (Amato, 2010; Liu & Umberson, 2008). Although widowhood has declined in recent decades, divorce during the second half of life has surged. Since 1990, the rate of gray divorce, which refers to divorces that occur among adults aged 50 and older, has more than doubled. Nowadays, one in four persons divorcing in the United States is 50 or older (Brown & Lin, 2012). This trend has reshaped the experience of marital dissolution in midlife, which increasingly occurs through divorce rather than spousal loss (Brown et al., 2018).
Divorced and widowed older adults are at elevated risk of having cognitive impairment, not dementia (CIND) or dementia compared with married older persons (Liu et al., 2019, 2020). Yet, the few studies to date on marital status and cognitive functioning largely overlook the role of marital transitions, obscuring the potential effects of experiencing divorce or widowhood as well as subsequent repartnering on the onset of cognitive impairment and also making it difficult to parse selection effects from possible causation. The rise in gray divorce underscores the shifting terrain of midlife, which is increasingly marked by marital dissolution. Nonetheless, the association between marital dissolution, whether through gray divorce or widowhood, and cognitive impairment in midlife is unknown.
Roughly 12% of individuals aged 55–69 exhibit mild cognitive impairment (Choi et al., 2018). These individuals not only compose the lion’s share of midlife adults with cognitive limitations but also are especially likely to go on to experience dementia (Choi et al., 2018; Petersen, 2004). Moreover, unlike dementia, which appears to be declining among adults older than age 70 (Langa et al., 2017), midlife cognitive impairment has remained stable in recent decades (Choi et al., 2018). These trends signal that an examination of marital dissolution and cognitive impairment is overdue.
Using longitudinal data from the 1998–2016 Health and Retirement Study (HRS), we track cognitively healthy midlife married women and men aged 50–65 through the end of midlife (i.e., age 65) to evaluate the effects of marital dissolution, distinguishing between divorce and widowhood, and subsequent repartnering on the risk of mild cognitive impairment onset. Guided by the stress model (Liu et al., 2020; Williams & Umberson, 2004), which conceptualizes marital dissolution as a traumatic life event that has both short- and long-term negative consequences for health and well-being, we posit that the loss of a partner through marital dissolution contributes to cognitive impairment through the diminishment of economic, social, and psychological resources. Widowhood may have larger effects than divorce given the heightened levels of cognitive limitations and dementia observed for widowed (vs. divorced) persons (Liu et al., 2019), and prior work indicating spousal death has larger socioemotional consequences than a divorce which in turn are related to greater health declines (Pudrovska & Carr, 2008). In line with the stress model, repartnering should be associated with a reduced risk of cognitive impairment onset with the repartnered appearing similar to the continuously married. Differentials in cognitive impairment onset by dissolution and repartnering transition experiences are likely to be attenuated by accounting for economic, social, and psychological resources along with other known risk factors for cognitive limitations including demographic, marital biography, and physical health indicators.
Background
The rapid acceleration in gray divorce coupled with the recent gains in life expectancy has altered the pathways out of marriage during midlife. Among midlife women, 56% of marital dissolutions occur through divorce and 44% result from widowhood. Divorce is the primary pathway to marital dissolution among midlife men at 79%. Just 21% of men’s marital dissolutions occur through widowhood (Brown et al., 2018). The growing prominence of divorce during midlife has ramifications for subsequent repartnering through remarriage or cohabitation. Although repartnering after a midlife marital dissolution remains uncommon, particularly among women, those who experienced divorce are more likely to repartner than their counterparts who became widowed. Gray divorced women are about 4 times more likely to be repartnered than women who became widowed (24% vs. 6%). Gray divorced men are roughly twice as likely to be repartnered as widowers (43% vs. 24%; Brown et al., 2018). These patterns underscore the importance of examining how divorce and widowhood in midlife are linked to well-being.
Midlife Marital Dissolution
Marital dissolution may play a pivotal role in the onset of cognitive impairment in midlife. According to the stress model, divorce and widowhood are challenging life experiences that typically entail the loss of economic, social, and psychological resources (Williams & Umberson, 2004), which may contribute to cognitive decline (Liu et al., 2020). Marital dissolution often leads to financial precarity, especially among women (Holden & Kuo, 1996; Lin & Brown, 2020; Sharma, 2015), and economic insecurity tends to be more common among those who experienced gray divorce than widowhood (Lin et al., 2017). A decline in the standard of living is an ongoing stressor that erodes physical and mental health, including cognitive well-being (Turrell et al., 2002). Individuals with fewer economic resources have less access to healthy foods and high-quality medical care, placing them at greater risk for poor health outcomes, such as diabetes and cardiovascular disease, which are risk factors for dementia (Liu et al., 2020). Likewise, marital dissolution involves the loss of social support from a spouse, who likely provided a source of daily engagement and other psychosocial resources (Hakansson et al., 2009; Helmer, 2009). The social ties obtained through one’s spouse, such as friends and in-laws, typically shrink following dissolution (especially divorce), further eroding the previously married individual’s social network and support sources which in turn may contribute to cognitive limitations (Liu et al., 2019). Relationships with others are protective of cognitive health in part because they are negatively associated with depressive symptoms, a key risk factor for dementia. The risk of dementia is twice as high among individuals who are depressed versus those who do not experience depression (Byers & Yaffe, 2011).
Although recent population studies reveal significant marital status differentials in various indicators of cognitive health (Liu et al., 2019, 2020), there has been relatively little attention to whether and how marital transitions are related to changes in cognitive well-being. This is an important omission because the divorced and widowed are a heterogeneous group, with some having experienced dissolution decades ago whereas others experienced marital dissolution only recently. A prevalence-based approach to capturing marital status differentials in cognitive well-being arguably misrepresents the experiences of the divorced and widowed because the long-term divorced and widowed who did not exit via remarriage are overrepresented and the newly divorced and widowed are underrepresented. Remarriage is selective of healthier, more economically advantaged people (Brown et al., 2018; Schimmele & Wu, 2016; Vespa, 2012), meaning that prevalence studies may overestimate the magnitude of the associations between being either divorced or widowed and cognitive impairment and dementia.
Moreover, the limited studies to date on marital dissolution and cognitive well-being have produced mixed results. Some research examining the link between experiencing widowhood and the onset of cognitive impairment or dementia has found no association (Vidarsdottir et al., 2014; Wörn et al., 2020), whereas other studies have revealed a positive effect (Biddle et al., 2020; van Gelder et al., 2006; Gibson & Richardson, 2017; Liu et al., 2020; Sommerlad et al., 2018). Apart from a supplemental analysis performed by Liu et al. (2020) that showed the transition to divorce is unrelated to dementia onset among a national sample of adults older than age 52, prior work has not addressed whether getting divorced is related to subsequent cognitive limitations. Expanding on the robustness check Liu et al. (2020) performed in their work on marital status and dementia, we examine the onset of CIND during midlife when gray divorce is most common. Unlike Liu et al., we also assess gender differences in these associations as the health ramifications of marital dissolution tend to be larger for women than men (Liu & Umberson, 2008), although at least one study has documented the reverse pattern among older adults (Williams & Umberson, 2004).
Repartnering
Repartnering through cohabitation or remarriage is likely to enhance cognitive well-being, largely by bolstering economic resources and providing daily social interaction and widening one’s social network, thereby enhancing psychological well-being. The economic losses associated with marital dissolution are offset by remarriage (Wilmoth & Koso, 2004). Repartnering expands one’s social network ties, which are important for a few reasons. First, social interactions provide mental stimulation and social support that can help individuals to maintain cognitive health (Kelly et al., 2017; Sommerlad et al., 2018). Second, close social relationships, particularly those with intimate partners, often involve health maintenance behaviors that can contribute to overall well-being (Umberson et al., 2010). Third, social ties have direct benefits for multiple indicators of physical and mental health (Umberson & Montez, 2010). Prior studies have shown that repartnering after divorce is associated with reductions in distress and depressive symptoms, although the benefits are temporary (Blekesaune, 2008; Kalmijn, 2017; Lin et al., 2019). We are not aware of any existing studies that have assessed how forming a repartnership relates to subsequent cognitive health. Liu et al.’s (2020) supplemental analysis of adults older than age 52 simply captured the transition to marriage without distinguishing between first marriages versus remarriages and uncovered no association with dementia onset.
The Present Study
Using longitudinal data from the 1998–2016 HRS, we track cognitively healthy midlife married women and men aged 50–65 through the end of midlife (i.e., age 65) to evaluate the effects of marital dissolution, distinguishing between divorce and widowhood, and subsequent repartnering on the risk of mild cognitive impairment onset. We anticipate that widowhood has larger positive effects than divorce on the onset of cognitive impairment given the heightened levels of cognitive limitations and dementia observed for widowed persons (Hakansson et al., 2009; Liu et al., 2019), and prior research showing that compared with divorce, widowhood is linked to larger drops in psychological well-being, which in turn is associated with poorer health (Pudrovska & Carr, 2008). Still, drawing on the stress model, we anticipate that both types of dissolution are positively related to cognitive impairment onset. Individuals who repartner following marital dissolution should be less likely to experience cognitive impairment onset than their counterparts who remain unpartnered based on the literature documenting the higher risk of dementia for the unmarried compared with the married (Sommerlad et al., 2018) as well as the stress model. It is also possible that repartnering is selective of those with better cognitive ability. The repartnered should be comparable to the continuously married. Differentials in cognitive impairment onset by dissolution and repartnering transition experiences are likely to be attenuated by controls for economic, social, and psychological resources along with other known risk factors for cognitive limitations and dementia including demographic, marital biography, and health indicators. Because both dementia onset (Mielke, 2018) and dissolution and repartnering patterns (Brown et al., 2018) differ by gender, we conduct separate analyses for women and men. By focusing on cognitive impairment onset in midlife, our study addresses an often overlooked yet critical dimension of midlife health that in turn is a primary risk factor for cognitive well-being in old age.
Design and Methods
We used data from the 1998–2016 HRS. The HRS is a nationally representative sample of persons older than age 50 (i.e., born in 1947 or earlier) as of 1998. Respondents are interviewed biennially and refresher cohorts aged 51–56 are added to the sample every 6 years (2004, 2010, and 2016) to ensure the sample remains representative of adults older than age 50. The HRS is well suited for our study as it includes a sufficiently large sample of married individuals who experience dissolution through either divorce or widowhood and also contains detailed measures of cognitive performance that have been substantiated in other studies as providing a reliable and valid indicator of cognitive impairment (Crimmins et al., 2011, 2016).
Our initial sample was composed of the 42,051 respondents in the RAND HRS 1992–2016 file (V2). The sample was limited to those with records after 1998, who were 50 and older at baseline (n = 37,007). To ensure each respondent was married in their baseline wave, we excluded individuals who were unmarried throughout their observation period (n = 12,925). Some individuals had more than one gray divorce or experienced more than one spousal death during the observation period. We only included the first marital transition and removed subsequent ones from the analytic sample, dropping 254 individuals. We also excluded respondents who had a baseline weight of 0, dropping 440 respondents. After linking respondents to the Langa–Weir classification of HRS cognition data (Langa et al., 2020), our sample excluded those who already had cognitive impairment at baseline (n = 3,765). We further excluded those older than 65 or present in just one wave (n = 8,683), yielding a final sample size of 10,940 respondents: 9,951 (4,656 men and 5,295 women) were continuously married, 373 (153 men and 220 women) experienced a divorce, 419 (86 men and 333 women) became widowed, and 197 (116 men and 81 women) went on to repartner through cohabitation or remarriage.
Measures
Cognitive impairment onset
The dependent variable cognitive impairment onset was coded 1 if the respondent experienced cognitive impairment during the interview year and 0 otherwise. The HRS uses a modified version of the Telephone Interview for Cognitive Status (TICS) to measure cognitive function on a 27-point scale composed of three parts. First, participants were asked to recall a list of 10 words immediately and again at a later point in the interview. They were assigned 1 point for each correct response. Second, respondents were asked to subtract 7 from 100 for five trials. Correct responses were assigned 1 point each (up to 5 points total). Third, respondents were assessed in their performance of counting backward to measure the speed of mental processing, scored between 0 and 2 points. Following the coding strategy of Crimmins et al. (2011, 2016), these responses were summed to classify respondents into one of the three categories: demented (0–6), CIND (7–11), and normal (12–27; Langa et al., 2020). These categories were recoded into either no cognitive impairment (12–27) or cognitive impairment onset (0–11) in this study.
For respondents who were not capable of participating in the TICS test functions, a proxy was used. The scale was composed of three elements. First, the proxy was asked to rate the respondent’s memory from 0 (excellent) to 4 (poor). Second, the proxy rated the respondent’s ability to complete five instrumental activities of daily living (IADLs): managing money, taking medication, preparing hot meals, using the phone, and shopping for groceries (0 = Yes vs. 1 = No, with a sum ranging from 0 to 5). Third, the interviewer assessed how much they felt the respondent was unable to complete the interview due to cognitive limitations (0 = None, 1 = Some, 2 = Prevented completion). In total, those who scored a sum of 0–2 were classified as no cognitive impairment onset (= 0), and those who scored 3–11 were coded as having cognitive impairment onset (= 1). Items used for the proxy report are consistent across waves except that in 1998 a 9-point scale was operationalized for proxy respondents that included the five IADLs and the proxy’s assessment of the respondent’s memory (0–2 = Normal and 3–9 = CIND or Demented). A supplemental analysis that excluded the 1998 wave suggested a similar pattern of the results and thus we retained the 1998 wave in the analysis.
Marital transition status
Respondents were classified as continuously married until they experienced a marital transition, which distinguished among three pathways: divorced, widowed, or repartnered. These were time-varying dichotomous covariates (1 = Yes, 0 = No). The categories were mutually exclusive. Once an individual repartnered after a divorce or widowhood, they were considered repartnered and no longer divorced or widowed. In the event that a respondent reported having experienced both a marital dissolution and repartnering during the 2-year interval between interviews, they were coded as repartnered.
Economic resources
Education was an ordinal, time-invariant variable: less than high school (reference category), high school diploma, some college, and college or more. Income was a continuous, time-varying measure for which the natural log was used for the respondent’s total household income for the calendar year prior to the interview. Those with an income beyond the 95th percentile were top-coded to the 95th percentile. Respondents who had no income were assigned an income value of $1 prior to taking the natural log.
Social resources
Volunteering was a dichotomous, time-varying measure (1 = Yes, 0 = No) that was lagged. Respondents were asked in the past 12 months how many hours they spent volunteering. Respondents who spent no time volunteering were coded as 0, and any time spent volunteering was coded as 1. Helping others was a dichotomous, time-varying measure that was lagged. Respondents were asked in the past 12 months whether they spent any time helping friends, neighbors, or relatives without pay (1 = Yes, 0 = No).
Psychological resources
Depressive symptoms were lagged to responses from the previous wave. Eight symptoms were measured using an abbreviated version of the Center for Epidemiologic Studies—Depression scale (Radloff, 1977). Respondents were asked whether they experienced the following symptoms much of the time during the week prior to the interview (1 = Yes, 0 = No): feeling depressed, feeling that everything was an effort, having restless sleep, being unhappy, feeling lonely, feeling sad, being unable to get going, and not enjoying life. These items were summed with a range from 0 to 8, with internal reliability coefficients ranging from 0.74 to 0.80 across waves.
Demographic characteristics
Age was measured in years and treated as a time-varying covariate. Race–ethnicity was composed of four categories: non-Hispanic White (reference category, hereafter White), non-Hispanic Black (hereafter Black), Hispanic, and non-Hispanic other race (hereafter other race). Living alone was a dichotomous, time-varying measure that captured whether respondents were living by themselves (or, if repartnered, with no one other than their spouse/partner) versus with others at a given wave. Respondents were asked how many residents lived in their household, including the respondent and any spouse/partner. For respondents who were divorced or widowed, those who reported themselves as the only household member were coded as 1 (living alone) and those who reported two or more residents were coded as 0 (living with others). For those who were repartnered, respondents who reported two or fewer household residents were coded as 1 (living alone) and those who reported more than two residents were coded as 0 (living with others).
Marital biography
Higher-order marriage was a time-invariant covariate that accounted for whether the respondent’s marriage at baseline was a remarriage for at least one spouse (1 = Yes, 0 = No). Marital duration was a time-varying covariate that characterized the number of years spent in that marriage. The value on this variable became time-invariant if and when marital dissolution occurred.
Physical health
Number of cardiometabolic conditions was a time-varying measure that summed whether a respondent had been diagnosed with heart disease, high blood pressure, diabetes, or a stroke (Diaz-Venegas et al., 2019). This measure was lagged, ranging from 0 to 4. Self-rated health was rated from 1 (poor) to 5 (excellent).
Analytic Strategy
We began by estimating survival probabilities for women and men by years since marital dissolution to examine the levels and patterns of cognitive impairment onset for those who either got divorced, became widowed, or experienced marital dissolution and then repartnered. Next, we calculated descriptive statistics (means or percentages as appropriate) across all study variables at baseline, separately for women and men by marital transition pathway to evaluate how women and men who either (a) got divorced, (b) became widowed, (c) experienced marital dissolution and then repartnered, or (d) remained continuously married differed in terms of economic, social, and psychological resources, demographic characteristics, marital biography, and physical health. These descriptive statistics are reported in Supplementary Table 1.
Finally, we estimated discrete-time event history models using logistic regression to predict the onset of cognitive impairment separately for women and men. Discrete-time modeling is more appropriate than continuous-time modeling because marriage start and end dates were measured as time intervals. Individuals were censored after they experienced cognitive impairment, became 65 years of age, or at the 2016 interview. The initial model included the marital dissolution and repartnering pathways to test whether those who became widowed or got divorced were at elevated risk of cognitive impairment compared with the continuously married. We also distinguished those who repartnered after marital dissolution to test whether their risk of cognitive impairment did not differ from that of the continuously married, as well as whether the repartnered were less likely than the divorced and the widowed to experience cognitive impairment onset. The full model incorporated the known risk factors for cognitive impairment to determine whether they attenuated the effects of marital transition type on the likelihood of cognitive impairment. Models were estimated separately for men and women.
Missing data were rare and handled by performing multiple imputation using chained equations (MICE) in Stata with the mi impute chained command. MICE imputes missing values on a given variable as a function of both the dependent variable and other covariates in the model (Raghunathan et al., 2001; van Buuren et al., 1999). We performed 10 random, multiple-imputed replicates to generate our results. Both the bivariate and multivariate analyses were adjusted using the baseline weights (Ofstedal et al., 2011).
Results
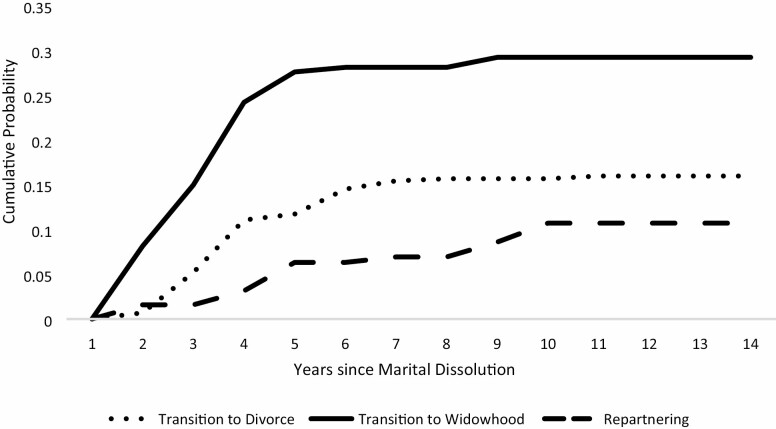
Figure 1 depicts the cumulative probability of cognitive impairment onset for men by marital transition type. Men who became widowers experienced rapidly accelerating probabilities of impairment as time elapsed since marital dissolution. Within about 5 years following a spousal loss, about 27% of men had exhibited cognitive impairment. Men who divorced experienced comparatively lower risks of impairment with less than 12% classified as cognitively impaired by 5 years after the divorce. For men who repartnered, the cumulative probability of cognitive impairment was even lower at just over 6% by 5 years after dissolution and plateaued at just below 12% by about 10 years after dissolution.
Figure 1.
Men’s cumulative probability of cognitive impairment onset by marital transition type.
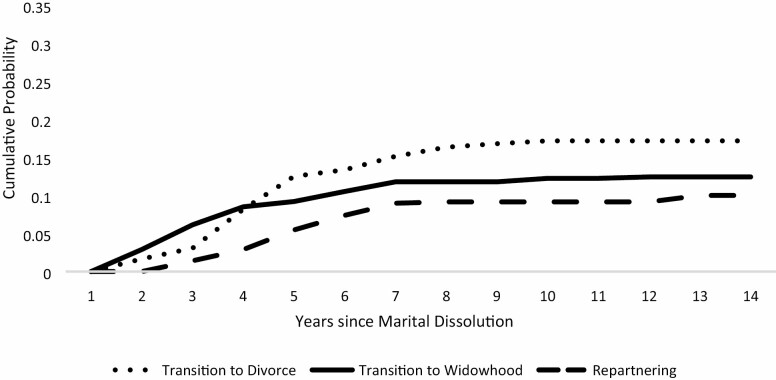
Figure 2 shows the cumulative probability of cognitive impairment onset for women by marital transition type. Women’s overall levels of impairment were lower than men’s, as expected. Also, women who became widowed did not exhibit appreciably higher probabilities of cognitive impairment than other women. In the first few years following dissolution, widowed women had somewhat larger risks of becoming cognitively impaired than did divorced women, but after 5 or more years had elapsed since dissolution this pattern reversed. The probability of cognitive impairment was greatest among women who got divorced at about 16%, followed by women who became widowed at 12%. Among women who repartnered after marital dissolution, the risk of cognitive impairment was still lower at about 10%. Supplementary Table 1 shows the weighted means or percentages for respondents’ characteristics according to their marital transition type by gender.
Figure 2.
Women’s cumulative probability of cognitive impairment onset by marital transition type.
Table 1 depicts the odds ratios from the logistic regression models estimating the likelihood of experiencing cognitive impairment onset separately for men and women. As shown in Model 1A for men, the likelihood of cognitive impairment onset was nearly 3 times higher for those who became widowers than those who remained married. By comparison, getting divorced was not significantly associated with the risk of cognitive impairment. As expected, men who repartnered did not experience any appreciable difference in their risk of cognitive impairment compared with the continuously married. In fact, men who repartnered after dissolution had a lower risk of cognitive impairment onset than men who transitioned to widowhood (as indicated by the superscript a in the table).
Table 1.
Odds Ratios from Discrete-Time Logistic Regressions of Cognitive Impairment Onset
| Men | Women | |||
|---|---|---|---|---|
| Model 1A | Model 2A | Model 1B | Model 2B | |
| Marital transition status | ||||
| Continuously married (reference) | ||||
| Divorce | 1.32 | 1.01 | 1.74** | 1.35 |
| Widow | 2.83a** | 1.78b,** | 1.39* | 0.82 |
| Repartnered | 0.93a | 0.72b | 1.19 | 0.96 |
| Economic resources | ||||
| Education | ||||
| Less than high school (reference) | ||||
| High school | 0.45*** | 0.51*** | ||
| Some college | 0.33*** | 0.31*** | ||
| College or higher | 0.19*** | 0.21*** | ||
| Income | 0.92*** | 0.94** | ||
| Social resources | ||||
| Volunteering (lagged) | 0.64*** | 0.77** | ||
| Helping others (lagged) | 0.79* | 0.68*** | ||
| Psychological resources | ||||
| Depressive symptoms (lagged) | 1.18*** | 1.23*** | ||
| Demographic characteristics | ||||
| Age | 1.04** | 1.06*** | ||
| Race | ||||
| White (reference) | ||||
| Black | 2.26*** | 3.35*** | ||
| Hispanic | 1.19 | 2.15*** | ||
| Other | 1.98*** | 3.60*** | ||
| Living alone | 1.01 | 1.00 | ||
| Marital biography | ||||
| Higher-order marriage | 1.17 | 1.16 | ||
| Marital duration | 1.01 | 1.00 | ||
| Physical health | ||||
| Cardiometabolic conditions (lagged) | 1.12* | 1.13* | ||
| Self-rated health (lagged) | 0.90* | 0.86** | ||
| Years since baseline | ||||
| 2 (reference) | ||||
| 4 | 0.82* | 0.82* | 0.74** | 0.73* |
| 6 | 0.75* | 0.72* | 0.74* | 0.71** |
| 8 | 0.98 | 0.96 | 0.84 | 0.78 |
| 10 | 0.69 | 0.65* | 0.72 | 0.62* |
| 12 | 0.74 | 0.67 | 0.43** | 0.37** |
| 14 | — | — | 1.00 | 0.94 |
| Constant | 0.06*** | 0.02*** | 0.05*** | 0.01*** |
| Model fit statistics | F(8,54.1) = 3.47 | F(24, 54) = 29.94 | F(9,54.1) = 4.75 | F(25,54.0) = 89.14 |
| Person-year observations | 14,694 | 19,081 | ||
Notes: Coefficients sharing the same superscript (e.g., a or b) statistically differ at p < .05. Model 1A = baseline model for men; Model 2A = full model for men; Model 1B = baseline model for women; Model 2B = full model for women.
*p < .05, **p < .01, ***p < .001.
These marital transition effects are largely impervious to the inclusion of controls in the full model as shown in Model 2A. The odds of experiencing cognitive impairment onset were nearly twice as high for men who became widowers as men who were continuously married. Nonetheless, men who repartnered after dissolution remained less likely to experience impairment onset than widowers (as indicated by the superscript b in the table). Economic, social, and psychological resources were protective against cognitive impairment onset for men. Education and income were negatively associated with cognitive impairment. Men who volunteered or helped others were less likely to become cognitively impaired than their counterparts who did not participate in these forms of social involvement. And, depressive symptoms were positively related to men’s cognitive impairment. Older men as well as Black and other race men were more likely to experience cognitive impairment onset than younger and White men, respectively. Men’s number of chronic conditions was associated positively with cognitive impairment.
Among women, becoming either divorced or widowed was associated with elevated risks of cognitive impairment as shown in Model 1B. Women who repartnered after divorce or widowhood were no more likely to become cognitively impaired than their counterparts who were continuously married. These marital dissolution differentials were accounted for by the inclusion of resources and controls in the full model (Model 2B). Economic, social, and psychological resources operated as expected based on the stress model. Both education and income were negatively associated with the onset of cognitive impairment. Social involvement was protective against cognitive impairment with those engaged in volunteer work and helping others less likely to become cognitively impaired. Depressive symptoms were positively related to women’s cognitive impairment onset. Older women as well as Black, Hispanic, and other race women were at greater risk of cognitive impairment than their younger and White counterparts, respectively. Women’s number of chronic conditions was positively related to cognitive impairment.
Discussion and Implications
A traumatic life event, marital dissolution has enduring consequences for multiple dimensions of physical and mental health (Amato, 2010; Hughes & Waite, 2009; Lin et al., 2019), but its implications for cognitive well-being are largely unknown. In line with the stress model, which stipulates individuals who experience marital dissolution lose key economic, social, and psychological resources that may compromise their well-being, we uncovered notable marital transition differentials in the risk of midlife cognitive impairment onset.
In particular, men who became widowers were at much greater risk of cognitive decline than other men. About 27% of men who experienced spousal loss in midlife went on to experience mild cognitive impairment by age 65. This nonnormative transition to widowhood may be uniquely stressful for midlife men (who are even less likely than midlife women to experience spousal death), as the finding persists net of economic, social, and psychological resources. Family interactions can help to mitigate cognitive decline and engagement with friends is more protective against cognitive limitations for women than men (Béland et al., 2005). Our models accounted for social resources including volunteer work and helping others, but these measures gauge only some aspects of relationships with family and friends, which could be a fruitful direction for future research.
For women, divorce and widowhood were associated with elevated risks of cognitive impairment in midlife, but these risks attenuated after accounting for resources and other covariates. Women with fewer economic resources were both especially likely to experience marital dissolution and cognitive impairment onset (results not shown). For both men and women, the repartnered were comparable to the continuously married in terms of their likelihood of cognitive impairment onset, aligning with the stress model.
Our study adds to the small but growing literature on marital status and cognitive well-being and is among the first to adopt a dynamic approach that focuses on the role of marital transitions, which are increasingly common in midlife (Brown et al., 2018). The patterns we uncover for the linkages between transitions to widowhood or divorce and cognitive impairment onset in midlife are consonant with those Liu et al.’s (2020) supplemental analyses documented for dementia in the second half of life. Our study is distinctive because it focuses on marital transitions rather than marital status and zeroes in on CIND that emerged during midlife. Liu et al. investigated dementia only and did not distinguish between mid- and later-life adults, nor did they address gender differentials. They also did not consider repartnering. Our work reveals that repartnering essentially offsets the negative effects of marital dissolution on cognitive impairment, underscoring the value of tracking marital dynamics across time.
We recognize that our study has some limitations. The HRS includes a large sample of midlife married adults who are at risk of marital dissolution and subsequent repartnering. However, because marital dissolution during midlife is a relatively uncommon event, the numbers who experienced divorce, widowhood, or repartnering were somewhat modest. Consequently, we may lack sufficient statistical power to fully detect differences between marital transition groups. Ultimately, our results are conservative and thus may understate the extent to which widowhood and divorce are linked to midlife cognitive decline. It is possible that cognitive difficulties may precipitate marital dissolution, especially divorce. By using longitudinal data to track marital transitions among cognitively healthy midlife adults, we have minimized the possibility that cognitive decline is contributing to marital dissolution, a concern in some prior studies that have relied on cross-sectional data (Helmer, 2009). Our modeling approach relied on lagged covariates, and supplemental analyses indicated our results were robust to longer lags (e.g., two waves instead of one), additional evidence that the results we obtained do not merely reflect short-term stress effects. Another limitation of our study is that the HRS does not include measures of dating or living apart together relationships, which may provide key resources to midlife adults after marital dissolution. However, our inclusion of a measure of living alone, which might be indicative of available economic, social, and psychological resources following marital dissolution, was not associated with cognitive impairment onset.
Our study demonstrates that midlife married adults who experience either divorce or widowhood are at elevated risk of cognitive impairment. Although much of this increased risk seems to be attributable to corresponding losses in economic, social, and psychological resources, it remains quite sizeable for men following spousal loss. Roughly 27% of men who become widowers in midlife will experience mild cognitive impairment by age 65, a magnitude that exceeds twice that of the midlife population at large (12%; Choi et al., 2018). Men who repartner are less likely than those who remain widowed to experience cognitive impairment onset in midlife, underscoring the salience of partnership for men’s cognitive well-being. Men tend to have fewer confidantes and friends than women, relying primarily on partners for support (McWilliams & Barrett, 2014). This differential contributes to the larger gap in depressive symptoms observed for married versus widowed men than women (Lee et al., 2001) and likely contributes to the persistent disadvantage in cognitive well-being we documented for widowed men.
Our findings have implications for practitioners and policymakers alike. Men who experience spousal loss in midlife are especially vulnerable to eroding cognitive ability, and this risk is likely to be greatest among widowers who are disadvantaged (Connidis & Barnett, 2019). Midlife marital dissolution is a factor in rising kinlessness (Margolis & Verdery, 2017), meaning midlife adults are more often lacking the family supports that can help to buffer the stresses and strains that typically accompany marital disruption. Midlife widowers in particular are a group in need of evidence-based programs to ensure they have the support and resources to maintain their cognitive reserve. The growing diversity of partnership experiences during the second half of life points to the continued importance of both basic and applied research that examines how union dissolution and formation shape health and well-being.
Supplementary Material
Funding
This work was supported by a grant from the National Institute on Aging (R15AG047588 to S. L. Brown and I.-F. Lin) and by the Center for Family and Demographic Research at Bowling Green State University which has funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (P2CHD050959).
Conflict of Interest
None declared.
References
- Amato, P. R. (2010). Research on divorce: Continuing trends and new developments. Journal of Marriage and Family, 72, 650–666. doi: 10.1111/j.1741-3737.2010.00723.x [DOI] [Google Scholar]
- Béland, F., Zunzunegui, M. V., Alvarado, B., Otero, A., & Del Ser, T. (2005). Trajectories of cognitive decline and social relations. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 60(6), 320–330. doi: 10.1093/geronb/60.6.p320 [DOI] [PubMed] [Google Scholar]
- Biddle, K. D., Jacobs, H. I. L., d’Oleire Uquillas, F., Zide, B. S., Kirn, D. R., Properzi, M. R., Rentz, D. M., Johnson, K. A., Sperling, R. A., & Donovan, N. J. (2020). Associations of widowhood and β-amyloid with cognitive decline in cognitively unimpaired older adults. JAMA Network Open, 3(2), e200121. doi: 10.1001/jamanetworkopen.2020.0121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blekesaune, M. (2008). Partnership transitions and mental distress: Investigating temporal order. Journal of Marriage and Family, 70, 879–890. doi: 10.1111/j.1741-3737.2008.00533.x [DOI] [Google Scholar]
- Brown, S. L., & Lin, I.-F. (2012). The gray divorce revolution: Rising divorce among middle-aged and older adults, 1990–2010. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 67, 731–741. doi: 10.1093/geronb/gbs089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, S. L., Lin, I.-F., Hammersmith, A. M., & Wright, M. R. (2018). Later life marital dissolution and repartnership status: A national portrait. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 73(6), 1032–1042. doi: 10.1093/geronb/gbw051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Buuren, S., Boshuizen, H. C., & Knook, D. L. (1999). Multiple imputation of missing blood pressure covariates in survival analysis. Statistics in Medicine, 18(6), 681–694. doi: [DOI] [PubMed] [Google Scholar]
- Byers, A. L., & Yaffe, K. (2011). Depression and risk of developing dementia. Nature Reviews. Neurology, 7(6), 323–331. doi: 10.1038/nrneurol.2011.60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi, H., Schoeni, R. F., Martin, L. G., & Langa, K. M. (2018). Trends in the prevalence and disparity in cognitive limitations of Americans 55–69 years old. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 73(Suppl. 1), 29–37. doi: 10.1093/geronb/gbx155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connidis, I. A., & Barnett, A. E. (2019). Family ties and aging (3rd ed). Sage. doi: 10.4135/9781544342306 [DOI] [Google Scholar]
- Crimmins, E. M., Kim, J. K., Langa, K. M., & Weir, D. R. (2011). Assessment of cognition using surveys and neuropsychological assessment: The Health and Retirement Study and the Aging, Demographics, and Memory Study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 66(Suppl. 1), 162–171. doi: 10.1093/geronb/gbr048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins, E. M., Saito, Y., & Kim, J. K. (2016). Change in cognitively healthy and cognitively impaired life expectancy in the United States: 2000–2010. SSM Population Health, 2, 793–797. doi: 10.1016/j.ssmph.2016.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Díaz-Venegas, C., Downer, B., Langa, K. M., & Wong, R. (2019). Cognitive functioning of US adults by race and Hispanic origin. In Contextualizing health and aging in the Americas (pp. 85–107). Springer. doi: 10.1007/978-3-030-00584-9_5 [DOI] [Google Scholar]
- van Gelder, B. M., Tijhuis, M., Kalmijn, S., Giampaoli, S., Nissinen, A., & Kromhout, D. (2006). Marital status and living situation during a 5-year period are associated with a subsequent 10-year cognitive decline in older men: The FINE Study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 61(4), 213–219. doi: 10.1093/geronb/61.4.p213 [DOI] [PubMed] [Google Scholar]
- Gibson, A. K., & Richardson, V. E. (2017). Living alone with cognitive impairment: Findings from the National Health and Aging Trends Study. American Journal of Alzheimer’s Disease & Other Dementias, 32, 56–62. doi: 10.1177/1533317516673154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Håkansson, K., Rovio, S., Helkala, E. L., Vilska, A. R., Winblad, B., Soininen, H., Nissinen, A., Mohammed, A. H., & Kivipelto, M. (2009). Association between mid-life marital status and cognitive function in later life: Population based cohort study. BMJ (Clinical Research ed.), 339, b2462. doi: 10.1136/bmj.b2462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helmer, C. (2009). Dementia and marital status at midlife and late life. BMJ (Clinical Research ed.), 339, b1690. doi: 10.1136/bmj.b1690 [DOI] [PubMed] [Google Scholar]
- Holden, K. C., & Kuo, H. H. (1996). Complex marital histories and economic well-being: The continuing legacy of divorce and widowhood as the HRS cohort approaches retirement. The Gerontologist, 36(3), 383–390. doi: 10.1093/geront/36.3.383 [DOI] [PubMed] [Google Scholar]
- Hughes, M. E., & Waite, L. J. (2009). Marital biography and health at mid-life. Journal of Health and Social Behavior, 50(3), 344–358. doi: 10.1177/002214650905000307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalmijn, M. (2017). The ambiguous link between marriage and health: A dynamic reanalysis of loss and gain effects. Social Forces, 95, 1607–1636. doi: 10.1093/sf/sox015 [DOI] [Google Scholar]
- Kelly, M. E., Duff, H., Kelly, S., McHugh Power, J. E., Brennan, S., Lawlor, B. A., & Loughrey, D. G. (2017). The impact of social activities, social networks, social support and social relationships on the cognitive functioning of healthy older adults: A systematic review. Systematic Reviews, 6(1), 259. doi: 10.1186/s13643-017-0632-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langa, K. M., Larson, E. B., Crimmins, E. M., Faul, J. D., Levine, D. A., Kabeto, M. U., & Weir, D. R. (2017). A comparison of the prevalence of dementia in the United States in 2000 and 2012. JAMA Internal Medicine, 177(1), 51–58. doi: 10.1001/jamainternmed.2016.6807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langa, K. M., Weir, D. R., Kabeto, M., and Sonnega, A. (2020). Langa-Weir classification of cognitive function (1995 onward). Survey Research Center Institute for Social Research, University of Michigan. [Google Scholar]
- Lee, G. R., DeMaris, A., Bavin, S., & Sullivan, R. (2001). Gender differences in the depressive effect of widowhood in later life. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 56(1), 56–61. doi: 10.1093/geronb/56.1.s56 [DOI] [PubMed] [Google Scholar]
- Lin, I.-F., & Brown, S. L. (2020). The economic consequences of gray divorce for women and men. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. Advance online publication. doi: 10.1093/geronb/gbaa157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, I.-F., Brown, S. L., & Hammersmith, A. M. (2017). Marital biography, social security receipt, and poverty. Research on Aging, 39(1), 86–110. doi: 10.1177/0164027516656139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, I.-F., Brown, S. L., Wright, M. R., & Hammersmith, A. M. (2019). Depressive symptoms following later-life marital dissolution and subsequent repartnering. Journal of Health and Social Behavior, 60(2), 153–168. doi: 10.1177/0022146519839683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, H., & Umberson, D. J. (2008). The times they are a changin’: Marital status and health differentials from 1972 to 2003. Journal of Health and Social Behavior, 49(3), 239–253. doi: 10.1177/002214650804900301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, H., Zhang, Y., Burgard, S. A., & Needham, B. L. (2019). Marital status and cognitive impairment in the United States: Evidence from the National Health and Aging Trends Study. Annals of Epidemiology, 38, 28–34.e2. doi: 10.1016/j.annepidem.2019.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, H., Zhang, Z., Choi, S. W., & Langa, K. M. (2020). Marital status and dementia: Evidence from the Health and Retirement Study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 75, 1783–1795. doi: 10.1093/geronb/gbz087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margolis, R., & Verdery, A. M. (2017). Older adults without close kin in the United States. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 72(4), 688–693. doi: 10.1093/geronb/gbx068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McWilliams, S., & Barrett, A. E. (2014). Online dating in middle and later life: Gendered expectations and experiences. Journal of Family Issues, 35, 411–436. doi: 10.1177/0192513x12468437 [DOI] [Google Scholar]
- Mielke, M. M. (2018). Sex and gender differences in Alzheimer’s disease dementia. The Psychiatric Times, 35, 14. [PMC free article] [PubMed] [Google Scholar]
- Ofstedal, M. B., Weir, D. R., Chen, K. T., & Wagner, J. (2011). Updates to HRS sample weights (HRS Report No. DR-013). University of Michigan, Health and Retirement Study.http://hrsonline.isr.umich.edu/sitedocs/userg/dr-013.pdf [Google Scholar]
- Petersen, R. C. (2004). Mild cognitive impairment as a diagnostic entity. Journal of Internal Medicine, 256, 183–194. doi: 10.1111/j.1365-2796.2004.01388.x [DOI] [PubMed] [Google Scholar]
- Pudrovska, T., & Carr, D. (2008). Psychological adjustment to divorce and widowhood in mid- and later life: Do coping strategies and personality protect against psychological distress?. Advances in Life Course Research, 13, 283–317. doi: 10.1016/s1040-2608(08)00011-7 [DOI] [Google Scholar]
- Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- Raghunathan, T. E., Lepkowski, J. M., van Hoewyk, J., & Solenberger, P. (2001). A multivariate technique for multiply imputing missing values using a sequence of regression models. Survey Methodology, 27, 85–95. [Google Scholar]
- Schimmele, C. M., & Wu, Z. (2016). Repartnering after union dissolution in later life. Journal of Marriage and Family, 78, 1013–1031. doi: 10.1111/jomf.12315 [DOI] [Google Scholar]
- Sharma, A. (2015). Divorce/separation in later-life: A fixed effects analysis of economic well-being by gender. Journal of Family and Economic Issues, 36, 299–306. doi: 10.1007/s10834-014-9432-1 [DOI] [Google Scholar]
- Sommerlad, A., Ruegger, J., Singh-Manoux, A., Lewis, G., & Livingston, G. (2018). Marriage and risk of dementia: Systematic review and meta-analysis of observational studies. Journal of Neurology, Neurosurgery, and Psychiatry, 89(3), 231–238. doi: 10.1136/jnnp-2017-316274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turrell, G., Lynch, J. W., Kaplan, G. A., Everson, S. A., Helkala, E. L., Kauhanen, J., & Salonen, J. T. (2002). Socioeconomic position across the lifecourse and cognitive function in late middle age. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 57(1), 43–51. doi: 10.1093/geronb/57.1.s43 [DOI] [PubMed] [Google Scholar]
- Umberson, D., & Montez, J. K. (2010). Social relationships and health: A flashpoint for health policy. Journal of Health and Social Behavior, 51(Suppl), S54–S66. doi: 10.1177/0022146510383501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson, D., Crosnoe, R., & Reczek, C. (2010). Social relationships and health behavior across life course. Annual Review of Sociology, 36, 139–157. doi: 10.1146/annurev-soc-070308-120011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vespa, J. (2012). Union formation in later life: Economic determinants of cohabitation and remarriage among older adults. Demography, 49(3), 1103–1125. doi: 10.1007/s13524-012-0102-3 [DOI] [PubMed] [Google Scholar]
- Vidarsdottir, H., Fang, F., Chang, M., Aspelund, T., Fall, K., Jonsdottir, M. K., Jonsson, P. V., Cotch, M. F., Harris, T. B., Launer, L. J., & Gudnason, V. (2014). Spousal loss and cognitive function in later life: A 25-year follow-up in the AGES-Reykjavik study. American Journal of Epidemiology, 179, 674–683. doi: 10.1093/aje/kwt321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams, K., & Umberson, D. (2004). Marital status, marital transitions, and health: A gendered life course perspective. Journal of Health and Social Behavior, 45, 81–98. doi: 10.1177/002214650404500106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilmoth, J., & Koso, G. (2002). Does marital history matter? Marital status and wealth outcomes among preretirement adults. Journal of Marriage and Family, 64(1), 254–268. doi: 10.1111/j.1741-3737.2002.00254.x [DOI] [Google Scholar]
- Wörn, J., Comijs, H., & Aartsen, M. (2020). Spousal loss and change in cognitive functioning: An examination of temporal patterns and gender differences. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 75, 195–206. doi: 10.1093/geronb/gby104 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.