Abstract
Background and Objectives
Identifying the experience of people with mild cognitive impairment (MCI) may help develop research agendas, interventions, and other supports to better match individuals’ needs. The purpose of this study was to explore the subjective experience of a “typical week” living with MCI to document (a) important activities, (b) barriers to usual activities, and (c) facilitators and supports.
Research Design and Methods
We conducted remote individual photo-elicitation interviews with 11 community-dwelling adults aged 55 years or older with MCI. Participants each provided 5–10 photographs of daily life taken over 1 week to facilitate a semistructured qualitative interview. Interview transcriptions were coded in Dedoose software and analyzed using thematic analysis.
Results
Participants shared photos and narratives highlighting the important activities in a typical week, in which physical activity, social engagement, spiritual and religious practice, hobbies, and cognitive stimulation were central. Many also shared disruptions to former routines and reduction of activities alongside increased use of new strategies and environmental supports (e.g., calendars, smartphones). Finally, emergent themes centered on disclosure of their diagnosis and reflections about the future.
Discussion and Implications
Participant-generated images aided data collection and facilitated discussion of sensitive topics with individuals with MCI. Such narratives may illustrate the needs and opportunities to promote well-being in individuals with MCI, including engagement in meaningful and health-promoting activities, assessing barriers to important daily activities, and considering supports that match the experience and needs of those with MCI.
Keywords: Photo-elicitation, Sense of self, Successful aging
Mild cognitive impairment (MCI) is nonnormative cognitive decline in the absence of dementia (Albert et al., 2011; Petersen et al., 2014). Individuals with MCI often present with subjective memory complaints and demonstrate objective cognitive impairment in one or more domains of memory, executive function, attention, visuospatial skills, and language (Petersen et al., 2014). Although functional abilities are generally preserved, particularly in activities of daily living (e.g., hygiene, dressing, grooming, ambulating, feeding), this impairment may render mild problems with instrumental activities of daily living (e.g., managing finances, transportation, household management). The condition affects an estimated 16.6% of adults older than 65, and prevalence increases with age (Petersen et al., 2018). While public health campaigns have spurred early detection and increased awareness, we know little about how to support, manage, or treat this relatively common condition (Cooper et al., 2015). Affected individuals may experience stigma, fear, and reluctance to participate in research or access services.
With increasing attention to diagnosing MCI in clinical practice, empirical study and documentation of the individual experiences of MCI are necessary to inform patient-centered care and allow patients to be part of the decision-making process in their care. To date, there are no disease-modifying treatments for MCI or Alzheimer’s disease. Clinicians may therefore offer information, advise, support, and referrals to patients about available health services and community supports, but such care is best understood in the context of what is meaningful and valuable to the individual. However, the experiences of individuals diagnosed with MCI are still poorly understood. Previous qualitative research has offered a glimpse into the loss experienced by individuals with MCI, such as changing social and familial roles (Frank et al., 2006) and negative emotional experiences and self-evaluation, social withdrawal, and decrease in leisure activities relative to older adults with normal cognitive aging (Parikh et al., 2016). A meta-synthesis of qualitative research on MCI found a common patient experience is a difficulty understanding the meaning of the diagnosis and prognosis (Gomersall et al., 2015). Patient narratives, such as those generated through qualitative inquiry, could assist in developing supports that best match individual experiences, needs, and preferences.
To address such gaps in understanding the patient stakeholder experience, investigators at the University of Pennsylvania launched a project called My Typical Day in which adults with MCI documented their lives using photography. The photo gallery can be viewed at http://www.mytypicalday.org and served as the basis for a published case vignette (Hailu et al., 2017). My Typical Day inspired the present study in which we used photo-elicitation methodology to further explore the lived experience of MCI (Bugos et al., 2014). In photo-elicitation, participants take photographs according to predetermined prompts. The resultant images guide an interview and facilitate reflective dialogue. The photographs provide a shared focus between the interviewer and participant, a method that is appropriate for and supportive of individuals with impairments in memory, language, and other cognitive abilities (Shell, 2015). Such a qualitative approach can broaden our understanding of an understudied group, such as those with MCI, by elucidating patients’ perspectives, meanings, and experiences (Hinton, 2010).
In this article, we expand on the previous work by Hailu et al. (2017) and explore the subjective experience of a “typical week” living with MCI using the narratives offered by our older adult participants. In addition, we expect that a deeper understanding of the experience of MCI—including adverse consequences, but also meaningful activities and compensatory or supportive strategies—is relevant to informing future research and intervention development. By tailoring services to the needs, preferences, and concerns of those with MCI, memory loss interventions, support programs, and other services can better support these individuals. The specific aim was to use photo-elicitation qualitative interviews to consider (a) important daily activities for those living with MCI, (b) barriers to usual activities, and (c) facilitators and supports.
Research Design and Methods
Participants
Participants were recruited from (a) a participant research registry at the University of Washington’s (UW) Harborview Medical Center’s Memory and Brain Wellness Center Registry, and (b) self-referral from the greater Puget Sound regional community in Washington State through flyers shared at local senior centers, older adult housing organizations, and community events. Individuals were eligible to participate if they had (a) a diagnosis of MCI, (b) access to a smartphone or digital camera and the ability to take and upload digital photographs, and (c) ability to speak and understand English. The study was fully remote, so we recruited broadly across the region, inclusive of both urban and rural areas. Twenty-two individuals were screened; 11 (50%) were ineligible or excluded because of loss to follow-up (n = 5), too cognitively impaired (n = 3 with Telephone Interview of Cognitive Status [TICS] scores <20), no longer interested (n = 2), or no access to a smartphone or digital camera (n = 1). Interviews were conducted with 11 participants aged 57–79 (M = 69.82, SD = 5.88). All were non-Hispanic White, five identified as female, three resided in rural areas, and the average educational attainment in the sample was 17 years (SD = 1.95, range 14–18 years). The UW Institutional Review Board approved this study (Study #2788) and we obtained informed consent from participants. Participants did not receive compensation or other incentive for participation.
Measures
Trained research assistants conducted baseline telephone eligibility assessments using the TICS (Brandt et al., 1988), a global test of cognitive functioning assessing orientation, immediate and delayed free-recall, attention and concentration, language, and working memory over the telephone. We used a modified, 13-item version that was shortened for epidemiological research (Brandt et al., 1993) and has been used to assess cognitive functioning, including MCI, in studies of community-dwelling older adults (de Jager et al., 2003). Total possible scores range from 0 to 39; higher scores indicate better cognitive functioning. Participants were eligible if they scored at least 20 on the modified TICS, an equivalent of a Mini-Mental State Examination score of 25 (Fong et al., 2009). Scores in this sample ranged from 20 to 26, M = 23.18, SD = 1.99.
Given the high comorbidity of MCI and depression (Ismail et al., 2017), we screened for depressive symptoms using the eight-item Patient Health Questionnaire (Kroenke et al., 2009) to classify the sample. This standardized measure assesses symptoms of depression except suicidality. Possible scores range from 0 to 24; scores of at least 10 indicate clinically significant depressive symptoms (Kroenke et al., 2001). Scores in this sample ranged from 0 to 18, with minimal depression on average (M = 3.55, SD = 5.41).
Procedures
Participant photographs
We told participants that the purpose of this study was to use photography and interviews to better understand the daily lives of people with MCI. During screening, we asked potential participants about their access to a smartphone or digital camera, and their comfort or willingness to take photographs and send them to us electronically (i.e., via email). In instances where a potential participant had access to a device but did not know how to take or send photographs, we asked if there were family members or others who could assist them by either teaching them how to take photographs or emailing the photographs to our study team.
We asked participants to use their own (or a trusted other’s) digital camera or smartphone to take pictures over the course of 1 week that represented or reflected important features of everyday life, including anything that they find frustrating or challenging because of MCI, and/or facilitators or supports of daily activities. We encouraged them to capture their usual routines and not change anything for the sake of the interview. In accordance with published best practices for photo-elicitation interviews (Bugos et al., 2014), we offered guidelines for taking pictures respectfully, ethically, and safely (e.g., do not take any risks for the sake of a photograph; do not photograph children; do not photograph illegal behavior; do not take any photographs intended to embarrass, shame, or discriminate against individuals or groups). We did not restrict the total number of photographs that participants took over the week, but we asked each participant to select 5–10 photographs for the interview. If they captured more, we asked them to prescreen these photos and send the 5–10 that best reflected the probes above. Because digital cameras allow the participant to take many photographs, we opted to restrict the number they shared with us to keep the interview manageable (Bugos et al., 2014). These instructions also ensured there would also be sufficient breadth of images to guide each interview (i.e., no interviews were conducted with only one photograph). We encouraged, but did not require, participants to write brief notes describing their photographs and associated thoughts to assist them during the interview. Photographs were uploaded to a secure cloud-based server prior to the interview.
Photo-elicitation interview
Individual photo-elicitation interviews were conducted as soon as possible after participants completed their week of photography (i.e., we scheduled interviews for the day after, or as soon as possible, the participant completed their week of photography). This was intended to support the recollection and relevance of the photographs to the interview. Interviews ranged from 45 to 60 min and were conducted by either a clinical geropsychologist (B. N. Renn) and/or a trained graduate student researcher in public health (J. L. Wool). All interviews were conducted and recorded using HIPAA-compliant Zoom Video Communications, Inc. software. To improve usability and comfort with this technology, participants could either dial in by telephone or use the video call feature from their personal computer.
The semistructured interview focused on the 5–10 photographs preselected by the participant. The participant and interviewer both looked at the referenced pictures during the interview, either by using the screen-sharing function of Zoom or by each referring to the pictures on their own devices. The interview centered on two main questions for each photograph: (a) Why did you choose to share this photo with me? and (b) In what way did this photo make you think about your MCI?, with follow-up probes for elaboration or expansion as needed.
Data analysis
Interview recordings were transcribed in full by a third party and were uploaded to Dedoose software for analysis. The two authors who conducted the interviews (B. N. Renn and J. L. Wool) coded each interview using thematic analysis (Braun & Clarke, 2006). Both are experienced with qualitative research. Beginning with the first interview through the completion of data collection, we read and re-read the transcripts to ensure thoroughness and familiarity with the data. We used a constant comparison to construct themes across participants and identified preliminary themes concurrently with data collection. Codebook development began after interviews were complete. Our analysis used both deductive and inductive approaches. Deductive coding relied on an analysis matrix based on the photo-elicitation prompts (i.e., important daily activities, barriers, and facilitators of daily life with MCI) as a frame of categorization. We also used open coding for inductive analysis, allowing for newly emergent themes (i.e., disclosure of diagnosis, contemplation of future) that did not fit into the existing categorization frame (Elo & Kyngäs, 2008). We applied both coding approaches to segments of the interview transcripts ranging from a phrase to several sentences. Units of information were statements about the photographs, guided by the photo-elicitation prompts (e.g., important activities), and any other remarks or examples about living with MCI. An initial sample of transcripts was coded independently by both raters. We refined codes via discussion of specific data segments both within and across transcripts. Broad themes were broken into subthemes (e.g., coding for the photo-elicitation prompt for “Important Activities” yielded subthemes of “Physical activity and diet,” “Social support, engagement, and sense of community,” “Spirituality and religious practice,” “Cognitive stimulation,” and “Hobbies as a reprieve”). The coders met regularly over several meetings during this initial stage of analysis to achieve consensus on grouping, categorization, and abstraction of the data. We ensured intercoder agreement through discussion. For example, we made a distinction between participants’ descriptions of reading for cognitive stimulation, hobby, and participants’ descriptions of difficulties or frustrations with reading due to MCI (see Supplementary Material for a codebook excerpt in which we present the subtheme of “Cognitive stimulation”). We applied this codebook to all transcripts, and the analysis team iteratively reviewed and refined the codes throughout the rest of the study to arrive at a final set of themes. The third member of the research team (B. Belza), a nurse scientist with a specialty in aging research and experienced with qualitative methods, was available for further consensus as needed. Illustrative quotes and a summary of corresponding photographs that exemplified the final themes were selected for inclusion in this manuscript; these data are presented as naturalized transcription (e.g., punctuation added, filler words removed).
Results
Our deductive analyses confirmed three themes that were guided by the photo-elicitation instructions and interview guide: (a) important activities in a typical week, (b) disruptions to a typical week, and (c) facilitators or compensatory supports. Inductive coding also uncovered two unexpected themes of (d) disclosure of diagnosis and (e) reflection about the future. See Table 1 for a list of themes, exemplar quotes, and a summary of participant photographs. Select participant quotes, are also included below as supportive illustrations.
Table 1.
Themes, Exemplar Participant Quotes, and Corresponding Images
| Subtheme | Illustrative quote(s) | Pictorial representations |
|---|---|---|
| Theme: Important activities | ||
| Physical activity and diet | I was reminded by my doctor and one of the other doctors at this class that I went to that aerobic exercise especially, but exercise in general, is a very important part of your brain health and has been shown statistically to preserve your memory longer. I was not aware that there was such a direct correlation. I knew that overall general health was just important in general, but I never realized that it also applied directly to my memory problems. I was easily convinced and actually happy to get back to exercise, and so I’ve launched back into it. I actually feel better in multiple ways because of it, and so I’m glad that I’m back on that track. | Participant at the gym; treadmill; dinner plate featuring fish, vegetables, and blueberries |
| Social support, engagement, and sense of community | The friends that I’m talking about are close friends. I told them early on and they’re very patient. We laugh about it or whatever. The attitude is pretty good. | Friends, party |
| Spirituality and religious practice | Spiritual focus contributes to relaxation and being able to deal with stress. That is one of my tools for fighting [MCI]. | Spiritual readings, church altar |
| Cognitive stimulation | Puzzles and games in general are something that I enjoy. I’ve also heard that they’re good exercise for keeping your brain active and helping it stay healthy longer. In the morning I also like to spend time going through the puzzles in the newspaper. There’s a variety, some of them word-oriented, some number-oriented. They’re a very interesting exercise. | Sudoku, crossword puzzle, jigsaw puzzle, Lego |
| Hobbies as a reprieve | [Gardening] just sort of detracts from thinking about my memory or having to talk or reach any big decisions. It’s sort of a haven; it’s relaxing, and I don’t feel so stressed about not remembering things. If something doesn’t grow right, then it just doesn’t grow, but so far, it’s been working pretty well. It’s just kind of a getaway from everything. | Gardening, museum, painting |
| Theme: Disruptions to daily life | ||
| The photograph [of work computer] turned out really like I wanted it to—gray and drab. That’s kind of what it’s like being at work—it’s gray and drab. Because of MCI, I sometimes find myself having to research an existing project, because I can’t retain all of the details. Now, keep in mind that I’m somebody who never had to take notes—ever. I would be having months-long negotiations with contracts and remember minute details of every single conversation that we had. I’ve lost that now. It’s gone. I really can’t do it anymore. Part of it is my age, of course, but definitely part of it is MCI, and so I find myself having to do coping mechanisms like taking copious notes and having notebooks very handy, [and] doing things like opening a conversation with “Oh, now this is where I think we were at,” and getting the other side’s response back. Again, it’s an uncomfortable way to live. I find that it is becoming more and more difficult to do. | Work; kitchen scenes, including a picture of disorganized utensils; belated birthday greeting card, church (to represent previous participation and leadership) | |
| Theme: Facilitators and supports | ||
| These [organizational aids/memory supports] are all things to kind of say, “Well, how can I be as on top of things as possible as things get harder?” The more I can be on top of things, the more that I can do and be active. What I like about it [wooden block perpetual calendar] is that it’s got that tactile part. I have to go over and change those blocks every day, and so more than just looking at a calendar. I’m physically touching this thing. I’m saying, “Okay, I’m changing the date” or I’ll look at it and say, “I don’t think that I’ve changed the date.” It’s a little strategy to help me with [my memory]. |
Wall calendar, perpetual calendar, daily planner, whiteboard, daily diary, handwritten notes in a novel, supports for baking | |
| Theme: Disclosure of diagnosis | ||
| Fear of stigma or anxiety related to disclosure | I don’t enjoy seeing people that I don’t know very well. I don’t really shy away from it, but at the same time it’s not as enjoyable because I think that I must hide what’s going on. I don’t want any difficult questions or to repeat myself, which I’ve been known to do. It’s just sort of a safe haven with people that I know really well. I’m just not that interested in crowds anymore. | None |
| Disclosure as supportive | When I’m with strangers on the street, then I may have to say, “I just don’t remember things as well.” I don’t talk about it from a diagnostic viewpoint, but just letting them know if you give me a phone number, I can’t remember that so well. “Maybe you could send me an email with your phone number instead.” [I] keep it more practical and don’t go into the details with less familiar people. | |
| Reflection about the future | ||
| Well, I wanted to share this picture, because this is literally looking “out my backdoor.” That potted plant right there was done entirely by my wife. I have to keep reminding myself that I am actually a truly very fortunate person, and that I think it’s important to grasp the beauty in life. I think that this represents a very beautiful scene. I do get depressed. I do have this constant sense of dread always at the back of my mind, and so I need to really proactively ground myself by embracing things that are bigger than myself and learn to appreciate at the same time the small things like looking out my backdoor and seeing this gorgeous scene. | Rainbow, backyard | |
| I like the term MCI. Somebody says, “Well, what’s that?” I say, “Well, it’s mild cognitive impairment,” but I look at it as the doorway to dementia. It’s sort of a right way of saying, “I know that it’s where I’m headed. At whatever stage of the journey I’m in, there is really no backtracking as far as I’m concerned, and so that’s how I present myself.” |
Important Activities in a Typical Week
Participants emphasized specific activities as important to both their daily routines and overall cognitive health. Some of these activities were also described as providing reprieve or solace from the difficulties associated with memory changes.
Physical activity and diet
Optimizing physical health was a priority mentioned by nearly all participants in describing their typical week. Some explicitly linked this to preserving their cognitive functioning as long as possible. Multiple participants indicated they either began or increased cardiovascular exercise at the recommendation of a health care provider. For example, one participant described his decision to no longer use a golf cart following his neurologist’s advice:
I used to ride [a golf cart] before my neurologist made the diagnosis. He said, “Aerobics, aerobics, aerobics, aerobics—it’s all aerobics.” When he talked to me about golfing, he said, “You need to start walking and you need aerobics.”
Three participants also referenced the importance of diet to brain health. Most frequently cited was the Mediterranean diet, which is based on traditional foods of the countries surrounding the Mediterranean Sea and is high in mono- and polyunsaturated fats, vegetables, fruits, and lean proteins. One participant, in describing a picture of his dinner plate, specified, “Of course, diet is important. The Mediterranean diet with fish seems to be one of the factors, one of the lifestyle characteristics of people who are less likely to have dementia issues.”
Social support, engagement, and sense of community
The importance of social support was another frequent code. Participants often referred to familial and spousal support in dealing with their diagnosis and subsequent impairments, as well as engagement with friends and the broader community. One woman recalled the importance of a support group, stating:
I have for years gone to an Early Stage Memory Loss (ESML) support group at the Senior Center. It’s very, very important to me. I just find it so helpful and the people are wonderful, and our facilitator is great.
Five participants also described volunteering to contribute to and connect with their community. The importance of volunteering included a sense of enjoyment, social interaction, and a way to remain engaged, especially in the face of retirement and other activity limitations.
Social engagement also provided a sense of connection and community. Participants emphasized the critical need to maintain social relationships and interconnection. One shared a picture of his rural property that included an apple orchard, where he hosts cider parties for neighbors and family. Although these parties feature less complicated meals now that he has MCI, he shared his motivation: “Friends and family are really important. They’re ‘number one’. I like putting generations together.”
Spirituality and religious practice
Religious organizations, such as churches, provided a sense of community for many participants. They described opportunities for leadership, volunteering, and social support in connection with their religious practice. For others, religious and spiritual practice was private, but similarly important to their daily lives. One participant shared a photograph of his home altar and relayed that he has been a practicing Buddhist for 50 years and his “centering practice … helps me start the day.”
Cognitive stimulation
While some participants had completed puzzles (e.g., Sudoku) throughout their lives, for others, their MCI diagnosis led to a conscientious decision to use puzzles for cognitive stimulation. One participant shared a photograph of a Lego-brand toy she is building, sharing that building the interlocking plastic bricks is a fun way to stay engaged (Figure 1):
Figure 1.
Participant-generated image of Lego Toy Assembly. Note: This image was captured by a study participant and reprinted with permission. The text referring to the completion status (“1/3 done”) was added by the participant.
I think that the “brain game” piece is critical … things that I had said at one point, “Gee, this would be fun to do.” The diagnosis [of MCI] said, “No, you don’t need to think about it; you need to do it.”
Puzzles were just one of several tools participants used for cognitive engagement. Six of our participants shared photographs of regular reading material as an important (albeit often frustrating) activity. One participant shared a picture of his friend, a native Spanish speaker, with whom he meets weekly to practice his conversational Spanish language skills. He emphasized that learning a foreign language was an important element of cognitive health. Another described his new hobby of coffee roasting as engaging yet “easy enough”—an activity he is capable of learning and executing despite his cognitive challenges. Finally, volunteering was also described as a method of cognitive stimulation:
I felt with my MCI diagnosis that I needed a bit of a challenge. I was looking for volunteer activities outside of work … so I volunteered at this museum and am now a docent in training. I’m hoping that by using the gray matter muscle a lot more in terms of memorization—and there’s a lot of details to memorize as a docent—I’m hoping to extend my normal time and hold off MCI, or maybe worse, Alzheimer’s.
Hobbies as a reprieve
All participants reported regular hobbies and leisure activities; as above, some described hobbies for their social or cognitive engagement. However, seven also shared the stress-reducing benefits and enjoyment of hobbies. For example, one participant shared a picture of her patio garden and described gardening as her “reprieve.” Another woman shared her painting easel and commented that she can engage in this hobby without “worrying about what I’m doing.” Another artist reflected on his craft, “Painting is the most stable thing in my life. Art keeps me going … it keeps me young.”
Disruptions to Daily Life
All participants shared frustrations, disruptions, and reductions in usual activities due to MCI. For example, the same artist described above also reflected that it is increasingly difficult to start projects and maintain concentration, particularly on complex sculptures; a commissioned piece that used to take him 2 or 3 days now takes as many weeks.
Cooking, reading, and navigating new places were a few of the commonly reported challenges illustrated by photographs. Two participants expressed frustrations related to cooking, such as not knowing which ingredients have been used:
I still cook and it’s very frustrating. If I go by a recipe, I’ll look at the ingredients and use them one at a time. But then that doesn’t always work. “Did I put that in?” I’ve thrown away more than one thing; for instance, making cornbread. It’s hard to tell what’s in the dry mix.
Frustrations with reading included not being able to remember characters or plot details in novels. Others struggled with daily demands of remembering errands and tasks. For many, such frustrations served as a catalyst for the compensatory strategies detailed in Facilitators and Supports.
Memory changes led some to reduce or alter their activities. One participant was still employed and described increasing difficulties at work. Two described giving up hobbies, three discussed giving up or reducing driving, and another had stopped flying as an amateur pilot. Three individuals recounted decisions to give up activities at their church. One participant shared a photograph of his church altar, reflecting that he retired as the president of his congregation because of the increasingly difficult cognitive demands. Another participant recounted:
I’m an Episcopalian and I was a part of the Altar Guild. You set up all of the communion stuff ahead of the services. I don’t do that anymore because I get confused, even though there’s a list of things to do. The last time I tried to do it, it upset me so much that I just said, “I’m sorry, I’m out of here.”
Facilitators and Supports
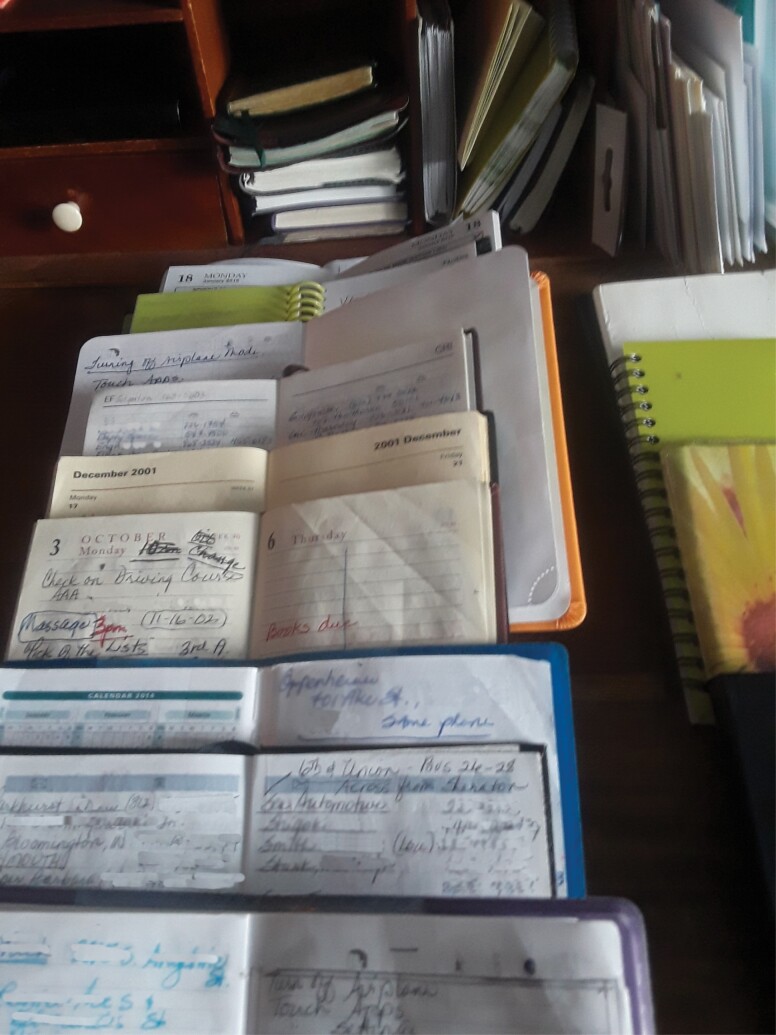
Nine participants described developing new strategies and routines as critical to navigating their cognitive changes. Some of the most common photographs featured in these interviews were calendars, daily planners, and whiteboards to remind participants not only of the date but also various obligations and commitments. One participant expressed his initial embarrassment but ultimate reliance on this tool (Figure 2):
Figure 2.
Participant-generated image of planners and diaries. Note: This image was captured by a study participant and reprinted with permission. Identifying information was redacted by the study team.
I actually bought one of those calendar whiteboards. My wife and I put it on the back of our bedroom door. I was a little embarrassed by it, but more importantly it’s the first thing that I see when I get up. We’ve listed out the days of the week and what’s going to be happening and what day, and so it’s very helpful.
Participants also shared compensatory strategies they developed to adapt to MCI-related challenges. For example, one participant shared that she takes notes about a story’s plot and characters to support her hobby of reading novels. Others relied on technology-enabled supports, relying on their smartphone for navigation and other reminders. The participant who described difficulty with following recipes shared this strategy, illustrated by a photograph of canisters on her kitchen counter, with mixed success:
I take everything out for making cornbread. I take everything out all at once. I started out by putting the ingredients away as I use them, but then I couldn’t remember if I actually took them out to begin with. I’d move them across to a different spot after I used them. That seems to help somewhat, but it’s kind of frustrating.
Additionally, two participants shared their experiences from a local program for people with early-stage memory loss. This program provided concrete strategies (e.g., use of a whiteboard) and recommendations (e.g., exercise) along with tools for discussing MCI with others.
Disclosure of Diagnosis
Fear of stigma or anxiety related to disclosure
The theme of disclosure emerged in conversations related to other difficulties or social support. The majority (n = 7) of our participants discussed their decision-making processes around whom to tell; for many, disclosure was often difficult. One woman shared, “It’s not always easy, you know? Some people don’t understand, and they don’t want to understand, I guess. It’s scary for people to think about people with memory problems.”
One participant who was still employed cited stigma as a constant source of fear:
There is this dread of being found out. If people were to find out here at work that I have MCI or any sort of cognitive issue, they would literally circle the wagons and then try to push me out as quick as they could … and so I’m kind of walking a bit of a tightrope every day coming into work.
Disclosure as supportive
Participants noted the importance of close friends with whom stigma is not a concern. One participant described her close friends as a “safe haven” in contrast to larger and unknown groups of people. Another shared,
There is a variety of ways that I react when meeting people. It depends on how well I know them. We live in a senior living community, and so [to] the people around me it’s easy enough to say, “My memory just doesn’t keep up with things so much anymore.” If anyone asks or is interested, I’ll just say, “Yes, I have mild cognitive impairment now and I’m on my way to Alzheimer’s, and that’s fine.” People accept it because it’s not uncommon.
Reflection About the Future
Finally, for several participants, the diagnosis of MCI was a catalyst for reflection about the future. This theme alternated between accepting one’s diagnosis and uncertainty about prognosis. Participants contemplated this uncertainty and focused on the importance of active engagement in their daily life with a positive attitude. For example, one participant noted his “desire to stay alive and alert as long as possible to see [his] grandchildren grow up.”
Some individuals noted that the diagnosis of MCI led to opportunities for inner reflection and seeking a sense of inner calmness. Experiences of gratitude and transcendence grounded these individuals, even in the face of gradual loss of their former abilities. One shared a photograph of a double rainbow as a way to describe how nature facilitates his reflection:
This MCI diagnosis—it causes you to look inward and to do things like take stock of your life. A scene like the rainbow, which is bigger than oneself, helps to ground me. It helps keep me going—trying to stay positive about things—which is increasingly difficult to do. It’s the little things like that that literally take your breath away when you see them.
Another participant described how thinking about his future inspires him:
It’s extremely important to learn as much as I can while I am able to learn it … to understand what the future holds for me, hopefully leading to a calm acceptance. That way, I can continue and make the most of my life, and keep it as happy as possible going forward.
Participants often tied their reflection on MCI to the possibility of Alzheimer’s disease in the future. Multiple participants cited a family history of Alzheimer’s, and one expressed this motivates him to proactively prepare and work toward acceptance:
I [have planned ahead] with the future in mind, because my mother had Alzheimer’s and so I know what she went through. My oldest sister is now going through Alzheimer’s. It’s fairly predictable due to my genetics that I’ll be going through that eventually, too, and so I had that forewarning which to me is good […] because it allows me to be proactive and prepare and accept.
Discussion and Implications
A “typical week” with MCI is full of important activities, modifications to these activities, and disruptions to everyday life. Using photo-elicitation as a platform for awareness, information gathering, and storytelling, our participants shared compensatory strategies, considerations of whether to disclose their diagnosis, and offered deeper reflections of their diagnosis and their future. These narratives can be used to inform patient-centered care, including guiding self-care and disease management strategies that align with patient values and concerns (Hailu et al., 2017). In particular, given that individuals with MCI may be at risk of withdrawing from activities (Parikh et al., 2016), we encourage clinicians and other support persons to query and support activities that are enjoyable and/or meaningful. This may include activity scheduling and enlisting environmental supports (e.g., memory aids) to facilitate activities.
One prominent theme was the centrality of activities thought to promote and preserve cognitive health, including exercise, diet, social connectedness, and cognitive stimulation through puzzles, foreign language practice, reading, and other intellectually engaging pursuits. These activities align with the growing literature on protective factors for dementia. For example, the association between the Mediterranean diet and preserved cognitive functioning is attributable in part to fewer cardiovascular and metabolic risk factors (Cooper et al., 2015; Dinu et al., 2018; Petersson & Philippou, 2016). Likewise, physical activity may improve aspects of cognitive functioning or slow cognitive decline in older adults with MCI or subjective memory complaints (Lautenschlager et al., 2008; Nagamatsu, 2012; Suzuki et al., 2013), but the research on exercise for secondary prevention in MCI is limited and in need of longitudinal investigation (Kane et al., 2017; Yang et al., 2019). Given Alzheimer’s disease and related dementias (ADRDs) likely emerge from a multifactorial etiology, research on multidomain interventions has grown in recent years. These programs, which target several lifestyle factors simultaneously (e.g., diet, exercise, cognitive and social engagement), have shown promising results in improving or maintaining cognitive functioning in older adults at risk for dementia (Ngandu et al., 2015), but are far from established. Much of the data informing lifestyle interventions derive from epidemiologic studies: high-quality randomized controlled trials to establish causation and bolster the evidence base for dementia prevention.
As expected, participants shared cognitive-related barriers to their daily routines, but in many cases also revealed their own compensatory strategies. Even though functional independence is generally preserved in MCI, individuals may have mild problems with complex activities such as managing finances, cooking, and other instrumental activities of daily living (Albert et al., 2011; Mansbach & Mace, 2019). Emerging data also suggest individuals with MCI struggle with everyday technology (Nygård et al., 2012). As with the previous photo-elicitation project at the Penn Memory Center (Hailu et al., 2017), our participants shared their experiences of increasing effort to handle quotidian demands. This varied from increasing reliance on family and friends to the use of external supports and reminder systems. These narratives offered insight into themes of both loss and resilience in the experience of MCI.
An unexpected but important emergent theme was deeper reflection related to one’s MCI diagnosis and prognosis. Our study adds to previous work on subjective experiences of both normal aging and living with MCI. We encourage further research and clinical intervention to support such reflections about one’s roles, values, and sense of self in face of a diagnosis of MCI. Given the increased likelihood of progression to ADRD among those with MCI (Petersen et al., 2018), earlier exploration of these existential and practical themes in MCI may facilitate acceptance or preparation for later stages, should cognition worsen. A synthesis of qualitative studies of MCI revealed a commonly endorsed theme of “using it, losing it, and living for the moment” (Gomersall et al., 2015) in which participants with MCI expressed narratives of lost capabilities, giving up previous roles and responsibilities, and reconfiguring one’s new place in the world. Interestingly, in contrast to other qualitative studies of MCI (Gomersall et al., 2015), our participants were not prone to reporting despair or even depression. Although MCI is associated with a high prevalence of depression (Ismail et al., 2017), our sample evidenced a low level of depressive symptoms. Of course, this is likely due to selection bias in our sample. Nonetheless, updated practice guidelines for MCI (Petersen et al., 2018) advise clinicians to evaluate and treat neuropsychiatric symptoms, including depression, which may add additional barriers and reduce well-being.
Limitations
Despite recruitment across a range of diverse community stakeholders and settings, our sample was exclusively non-Hispanic White with high educational and occupational attainment. There may be a reduced risk of incident dementia among those with such purported cognitive reserves (Valenzuela & Sachdev, 2006; Wang et al., 2017). Thus, researchers interested in the transferability of our findings to their populations of interest should consider the characteristics of our sample and how our themes may or may not resonate for other populations. Unfortunately, this mirrors the general research landscape in ADRD, in which ethnic and racial minorities are underrepresented in clinical trials (Faison et al., 2007), contributing to further disparities in diagnosis, access to and utilization of disease management strategies, and outcomes. Indeed, our sample appeared to have a high degree of health literacy and was able to obtain and understand information related to their physical and cognitive health. The themes of important activities (e.g., physical activity, Mediterranean diet, cognitive stimulation) revealed a sophisticated understanding of health-promoting lifestyle factors. The leisure activities reported in our sample—including golfing and recreational boating—and access to various opportunities (e.g., early retirement, participation in social groups) may also be considered privileges and may not be reflective of those of lower socioeconomic status.
Our participants were required to have access to and be able to use a smartphone or digital camera to take and send photographs. Although the vast majority (81%) of Americans own smartphones, this includes only 53% of adults aged 65 and older, and smartphone ownership increases with educational attainment, income, and urban or suburban dwelling (Pew Research Center, 2019). MCI may impart additional barriers to using everyday technology, including mobile phones, which may have discouraged participation in our study (Schmidt & Wahl, 2019). We attempted to offset these technology-related participation barriers by leveraging spousal or familial support as appropriate; for example, one participant had her husband email her pictures to the study team. Similarly, one participant struggled to connect to videoconferencing for the interview, so we called her telephone and walked her through the process. Nonetheless, this knowledge of, access to, and comfort with technology likely limited our sample and excluded individuals at greatest risk of not accessing health care and community services and supports.
Our study did not account for diagnostic precision as we allowed self-reported MCI diagnosis. TICS has limited utility classifying MCI separately from dementia and should not be used as a standalone measure (Knopman et al., 2010); rather, we intended it as a rough indicator of those for whom a retrospective interview, even supported by photographs, would likely be too onerous. We did not differentiate between subtypes of MCI, which may encompass different experiences and may predict later conversion to ADRDs (Busse et al., 2006). Finally, it is unknown how recall distortions or confabulation may have affected the interview data.
Conclusions
Given the ambiguity surrounding MCI diagnosis and prognosis, clinicians, researchers, and patients alike may be fraught with uncertainty. Identifying key features of daily life that patients find most meaningful may bolster the quality of life and resilience in the face of loss. As we improve our understanding of prognosis and modifiable risk factors that influence conversion to ADRD, disease management should focus on behaviors and outcomes most relevant to patients (e.g., quality of life, functional independence). Our thematic analysis revealed activities, such as exercise and social connectedness, that were important to individuals with MCI, alongside common barriers and compensatory strategies. Individuals with MCI may need additional assistance with problem-solving or implementing environmental supports to offset barriers to activity engagement. Our emergent themes of disclosure of diagnosis and reflections about the future could similarly be explored and emphasized in existing programs.
Photo-elicitation is a novel methodology to understand the experience of cognitive impairment. These visual portrayals of a typical week, expanded upon with qualitative interviews, allowed an intimate view of daily life with MCI. This methodology may have enhanced participants’ retrieval and ability to share their thoughts and feelings (Shell, 2015). Although reliance on photographs may lead participants to focus on observable phenomena rather than abstract concepts, our participants were able to reflect on nuanced and sophisticated experiences of their typical week, in line with prior photo-elicitation work on the experience of happiness among individuals with Alzheimer’s disease (Shell, 2015). Such patient narratives, illustrated with depictions of daily life, may elucidate the important determinants of quality of life and assist providers or caregivers in clinically meaningful and relevant management strategies. In the face of increasing language and memory difficulty, a picture can be worth a thousand words.
Funding
This work was supported by the National Institute of Mental Health [grant number T32MH073553] and the Healthy Brain Research Network (HBRN) funded by the Centers for Disease Control and Prevention (CDC) Alzheimer’s Disease and Healthy Aging Program. The HBRN is a thematic network of CDC’s Prevention Research Centers Program. Support was provided in part via cooperative agreements U48 DP 005053 and 005013. This research would not have been possible without additional funding provided to the HBRN Scholar Program by the Alzheimer’s Foundation of America. The views and findings shared in this publication are those of the authors and do not necessarily represent the official views of the NIH or CDC.
Conflicts of Interest
None declared.
Supplementary Material
Acknowledgments
The authors thank Tigist Hailu, MPH, Jason Karlawish, MD, and the rest of the My Typical Day project team at the University of Pennsylvania for their guidance and inspiration for this project. Their website MyTypicalDay.org offers a platform for awareness, education, and storytelling for people affected by cognitive impairment. We also extend our gratitude to Gwen Moni and Madelyn Mendlen for their programmatic support of this project. Portions of this work were previously presented at The Gerontological Society of America’s 2019 Annual Scientific Meeting in Austin, TX.
References
- Albert, M. S., DeKosky, S. T., Dickson, D., Dubois, B., Feldman, H. H., Fox, N. C., Gamst, A., Holtzman, D. M., Jagust, W. J., Petersen, R. C., Snyder, P. J., Carrillo, M. C., Thies, B., & Phelps, C. H. (2011). The diagnosis of mild cognitive impairment due to Alzheimer’s disease: Recommendations from the National Institute on Aging–Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s & Dementia, 7(3), 270–279. doi: 10.1016/j.jalz.2011.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandt, J., Specter, M., & Folstein, M. F. (1988). The telephone interview for cognitive status. Neuropsychiatry, Neuropsychology & Behavioral Neurology, 1, 111–117. [Google Scholar]
- Brandt, J., Welsh, K. A., Breitner, J. C., Folstein, M. F., Helms, M., & Christian, J. C. (1993). Hereditary influences on cognitive functioning in older men. A study of 4000 twin pairs. Archives of Neurology, 50(6), 599–603. doi: 10.1001/archneur.1993.00540060039014 [DOI] [PubMed] [Google Scholar]
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. doi: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- Bugos, E., Frasso, R., FitzGerald, E., True, G., Adachi-Mejia, A. M., & Cannuscio, C. (2014). Practical guidance and ethical considerations for studies using photo-elicitation interviews. Preventing Chronic Disease, 11, E189. doi: 10.5888/pcd11.140216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busse, A., Hensel, A., Gühne, U., Angermeyer, M. C., & Riedel-Heller, S. G. (2006). Mild cognitive impairment: Long-term course of four clinical subtypes. Neurology, 67(12), 2176–2185. doi: 10.1212/01.wnl.0000249117.23318.e1 [DOI] [PubMed] [Google Scholar]
- Cooper, C., Sommerlad, A., Lyketsos, C. G., & Livingston, G. (2015). Modifiable predictors of dementia in mild cognitive impairment: A systematic review and meta-analysis. The American Journal of Psychiatry, 172(4), 323–334. doi: 10.1176/appi.ajp.2014.14070878 [DOI] [PubMed] [Google Scholar]
- De Jager, C. A., Budge, M. M., & Clarke, R. (2003). Utility of TICS-M for the assessment of cognitive function in older adults. International Journal of Geriatric Psychiatry, 18(4), 318–324. doi: 10.1002/gps.830 [DOI] [PubMed] [Google Scholar]
- Dinu, M., Pagliai, G., Casini, A., & Sofi, F. (2018). Mediterranean diet and multiple health outcomes: An umbrella review of meta-analyses of observational studies and randomised trials. European Journal of Clinical Nutrition, 72(1), 30–43. doi: 10.1038/ejcn.2017.58 [DOI] [PubMed] [Google Scholar]
- Elo, S., & Kyngäs, H. (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62(1), 107–115. doi: 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- Faison, W. E., Schultz, S. K., Aerssens, J., Alvidrez, J., Anand, R., Farrer, L. A., Jarvik, L., Manly, J., McRae, T., Murphy, G. M.Jr, Olin, J. T., Regier, D., Sano, M., & Mintzer, J. E. (2007). Potential ethnic modifiers in the assessment and treatment of Alzheimer’s disease: Challenges for the future. International Psychogeriatrics, 19(3), 539–558. doi: 10.1017/S104161020700511X [DOI] [PubMed] [Google Scholar]
- Fong, T. G., Fearing, M. A., Jones, R. N., Shi, P., Marcantonio, E. R., Rudolph, J. L.,Yang, F. M., Kiely, D. K., & Inouye, S. K. (2009). Telephone interview for cognitive status: Creating a crosswalk with the Mini-Mental State Examination. Alzheimer’s & Dementia, 5(6), 492–497. doi: 10.1016/j.jalz.2009.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank, L., Lloyd, A., Flynn, J. A., Kleinman, L., Matza, L. S., Margolis, M. K., Bowman, L., & Bullock, R. (2006). Impact of cognitive impairment on mild dementia patients and mild cognitive impairment patients and their informants. International Psychogeriatrics, 18(1), 151–162. doi: 10.1017/S1041610205002450 [DOI] [PubMed] [Google Scholar]
- Gomersall, T., Astell, A., Nygård, L., Sixsmith, A., Mihailidis, A., & Hwang, A. (2015). Living with ambiguity: A meta-synthesis of qualitative research on mild cognitive impairment. The Gerontologist, 55(5), 892–912. doi: 10.1093/geront/gnv067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hailu, T., Cannuscio, C. C., Dupuis, R., & Karlawish, J. (2017). A typical day with mild cognitive impairment. American Journal of Public Health, 107(6), 927–928. doi: 10.2105/AJPH.2017.303752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinton, L. (2010). Qualitative research on geriatric mental health: Progress, challenges, and opportunities. The American Journal of Geriatric Psychiatry, 18(7), 563–566. doi: 10.1097/jgp.0b013e3181e16a26 [DOI] [PubMed] [Google Scholar]
- Ismail, Z., Elbayoumi, H., Fischer, C. E., Hogan, D. B., Millikin, C. P., Schweizer, T., Mortby, M. E., Smith, E. E., Patten, S. B., & Fiest, K. M. (2017). Prevalence of depression in patients with mild cognitive impairment: A systematic review and meta-analysis. JAMA Psychiatry, 74(1), 58–67. doi: 10.1001/jamapsychiatry.2016.3162 [DOI] [PubMed] [Google Scholar]
- Kane, R. L., Butler, M., Fink, H. A., Brasure, M., Davila, H., Desai, P., Jutkowitz, E., McCreedy, E., Nelson, V., McCarten, J., Calvert, C., Ratner, E., Hemmy, L., & Barclay, T. (2017). Interventions to prevent age-related cognitive decline, mild cognitive impairment, and clinical Alzheimer’s-type dementia (Comparative Effectiveness Review No. 188). Agency for Healthcare Research and Quality (AHRQ). doi: 10.23970/AHRQEPCCER188 [DOI] [PubMed] [Google Scholar]
- Knopman, D. S., Roberts, R. O., Geda, Y. E., Pankratz, V. S., Christianson, T. J., Petersen, R. C., & Rocca, W. A. (2010). Validation of the telephone interview for cognitive status-modified in subjects with normal cognition, mild cognitive impairment, or dementia. Neuroepidemiology, 34(1), 34–42. doi: 10.1159/000255464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke, K., Strine, T. W., Spitzer, R. L., Williams, J. B. W., Berry, J. T., & Mokdad, A. H. (2009). The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders, 114(1–3), 163–173. doi: 10.1016/j.jad.2008.06.026 [DOI] [PubMed] [Google Scholar]
- Lautenschlager, N. T., Cox, K. L., Flicker, L., Foster, J. K., van Bockxmeer, F. M., Xiao, J., Greenop, K. R., & Almeida, O. P. (2008). Effect of physical activity on cognitive function in older adults at risk for Alzheimer’s disease: A randomized trial. Journal of the American Medical Association, 300(9), 1027–1037. doi: 10.1001/jama.300.9.1027 [DOI] [PubMed] [Google Scholar]
- Mansbach, W. E., & Mace, R. A. (2019). Predicting functional dependence in mild cognitive impairment: Differential contributions of memory and executive functions. The Gerontologist, 59(5), 925–935. doi: 10.1093/geront/gny097 [DOI] [PubMed] [Google Scholar]
- Nagamatsu, L. S., Handy, T. C., Hsu, C. L., Voss, M., & Liu-Ambrose, T. (2012). Resistance training promotes cognitive and functional brain plasticity in seniors with probable mild cognitive impairment. Archives of Internal Medicine, 172(8), 666–668. doi: 10.1001/archinternmed.2012.379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngandu, T., Lehtisalo, J., Solomon, A., Levälahti, E., Ahtiluoto, S., Antikainen, R.,Bäckman, L., Hänninen, T., Jula, A., Laatikainen, T., Lindström, J., Mangialasche, F., Paajanen, T., Pajala, S., Peltonen, M., Rauramaa, R., Stigsdotter-Neely, A., Strandberg, T., Tuomilehto, J., … Kivipelto, M. (2015). A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomised controlled trial. Lancet (London, England), 385(9984), 2255–2263. doi: 10.1016/S0140-6736(15)60461-5 [DOI] [PubMed] [Google Scholar]
- Nygård, L., Pantzar, M., Uppgard, B., & Kottorp, A. (2012). Detection of activity limitations in older adults with MCI or Alzheimer’s disease through evaluation of perceived difficulty in use of everyday technology: A replication study. Aging & Mental Health, 16(3), 361–371. doi: 10.1080/13607863.2011.605055 [DOI] [PubMed] [Google Scholar]
- Parikh, P. K., Troyer, A. K., Maione, A. M., & Murphy, K. J. (2016). The impact of memory change on daily life in normal aging and mild cognitive impairment. The Gerontologist, 56(5), 877–885. doi: 10.1093/geront/gnv030 [DOI] [PubMed] [Google Scholar]
- Petersen, R. C., Caracciolo, B., Brayne, C., Gauthier, S., Jelic, V., & Fratiglioni, L. (2014). Mild cognitive impairment: A concept in evolution. Journal of Internal Medicine, 275(3), 214–228. doi: 10.1111/joim.12190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen, R. C., Lopez, O., Armstrong, M. J., Getchius, T. S. D., Ganguli, M., Gloss, D.,Gronseth, G. S., Marson, D., Pringsheim, T., Day, G. S., Sager, M., Stevens, J., & Rae-Grant, A. (2018). Practice guideline update summary: Mild cognitive impairment: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology, 90(3), 126–135. doi: 10.1212/WNL.0000000000004826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersson, S. D., & Philippou, E. (2016). Mediterranean diet, cognitive function, and dementia: A systematic review of the evidence. Advances in Nutrition (Bethesda, MD), 7(5), 889–904. doi: 10.3945/an.116.012138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center . (2019, June 12). Demographics of mobile device ownership and adoption in the United States. Pew Research Center: Internet, Science & Tech. https://www.pewresearch.org/internet/fact-sheet/mobile/ [Google Scholar]
- Schmidt, L. I., & Wahl, H. W. (2019). Predictors of performance in everyday technology tasks in older adults with and without mild cognitive impairment. The Gerontologist, 59(1), 90–100. doi: 10.1093/geront/gny062 [DOI] [PubMed] [Google Scholar]
- Shell, L. (2015). The picture of happiness in Alzheimer’s disease: Living a life congruent with personal values. Geriatric Nursing (New York, N.Y.), 36(2 Suppl), S26–S32. doi: 10.1016/j.gerinurse.2015.02.021 [DOI] [PubMed] [Google Scholar]
- Suzuki, T., Shimada, H., Makizako, H., Doi, T., Yoshida, D., Ito, K., Shimokata, H., Washimi, Y., Endo, H., & Kato, T. (2013). A randomized controlled trial of multicomponent exercise in older adults with mild cognitive impairment. PLoS One, 8(4). doi: 10.1371/journal.pone.0061483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valenzuela, M. J., & Sachdev, P. (2006). Brain reserve and dementia: A systematic review. Psychological Medicine, 36(4), 441–454. doi: 10.1017/S0033291705006264 [DOI] [PubMed] [Google Scholar]
- Wang, H. X., MacDonald, S. W., Dekhtyar, S., & Fratiglioni, L. (2017). Association of lifelong exposure to cognitive reserve-enhancing factors with dementia risk: A community-based cohort study. PLoS Medicine, 14(3), e1002251. doi: 10.1371/journal.pmed.1002251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang, C., Moore, A., Mpofu, E., Dorstyn, D., Li, Q., & Yin, C. (2019). Effectiveness of combined cognitive and physical interventions to enhance functioning in older adults with mild cognitive impairment: A systematic review of randomized controlled trials. The Gerontologist, 60(8), e633–e642. doi: 10.1093/geront/gnz149 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.