ABSTRACT
As the coronavirus disease 2019 (COVID-19) spreads across the world, the rapid distribution of an effective vaccine and its acceptability among the population constitute priorities for health authorities. This study aimed to document attitudes of the general population toward a future vaccine against COVID-19. We used the national COCONEL surveys conducted during the lockdown to identify factors associated with vaccine refusal, in the whole population, and separately among men and women. We investigate the role of socioeconomic and demographic factors as well as exposure to COVID-19. Among the 5,018 participants, 24.0% reported their intention to refuse the vaccine. Thinking this vaccine would not be safe, being against vaccination in general, and perceiving COVID-19 to be harmless were the three main reasons given to explain vaccine refusal. Women were more likely to refuse the vaccine, especially due to a reluctance toward vaccination in general or the perception that a COVID-19 vaccine would not be safe. Some factors associated with the intention to refuse the vaccine were the same among men and women such as a lack of prior vaccination against influenza, and concern over being infected with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), while others differed slightly according to gender such as age, and high prevalence of COVID-19 in their region of residence. Authorities should therefore guarantee that all the necessary precautions are taken before marketing the vaccine and communicate transparently on the process of its development, and on the coverage rate required to reach herd immunity.
Abbreviation: EHI: Equivalized Household Income per month; SARS-CoV-2: Severe acute respiratory syndrome coronavirus 2.
KEYWORDS: COVID-19, vaccination attitude, gender analysis, French population, coconel
Introduction
As the authorities implement measures to restrict the movement of people both within countries (such as curfew, and lockdowns) and outside (mandatory quarantines, border closures) to limit the spread of the coronavirus disease 2019 (COVID-19), the rapid distribution of an effective vaccine is a priority for health authorities. At the time of writing, five vaccines were authorized in the world, including two distributed in France. Most of these countries have implemented a targeted vaccination campaign (focusing on the most vulnerable) and are planning to vaccinate the general population before the end of 2021. However, the efficiency of a vaccination campaign is determined by the public’s acceptance of the vaccine and it is quite a sensitive issue. Public health experts have warned about the risk of insufficient vaccine uptake, given the disaffection of a significant part of the public for vaccination around the world, a trend even more salient for new vaccines. This is especially the case in France, which has among the highest levels of doubts about vaccine safety and vaccine complacency in the world.1–3 Recent studies have confirmed these concerns: between 10% and 41% of the French population reported they would not take the shot if a COVID-19 vaccine was available.4–6 A COVID-19 vaccine has not been distributed in general population yet and attitudes currently reported may differ from future vaccination behavior. The failure of the vaccination campaign led in France against the 2009 H1N1 influenza (only 8% of the French population got vaccinated while the government aimed for 70%) incites to take seriously current hesitations and to investigate more deeply the nature of these doubts. However, the number of studies focusing on willingness of the general population to accept a future COVID-19 vaccine is thus far limited. A high refusal rate was observed in Italy where, after the lockdown, 41% of the population reported they were not likely to vaccinate against COVID-19.7 In the United States, between 20% and 33% reported they would decline this vaccine,8,9 and in Saudi Arabia, 7% reported they would not take the shot and 28% reported hesitation about it.10 In Indonesia, the acceptance of a COVID-19 vaccine was strongly associated with its efficacy: 93.3% of respondents would like to be vaccinated with a 95% effective vaccine, while they were only 67.0% for a vaccine with 50% effectiveness.11 Finally, in seven European countries, the willingness to get vaccinated ranged from 62% in France to 80% in Denmark and the UK.5
Previous studies that investigated factors associated with acceptance of a new vaccine highlighted gendered differences in vaccine uptake although findings were inconsistent.12,13 Some of them, mostly from the US, found that women had higher rates of influenza vaccination than men.14,15 On the contrary, many European studies found men were more likely to get vaccinated with the pandemic influenza (H1N1) vaccine,16–19 and with the seasonal influenza vaccine.20–22 A study comparing eleven European countries across seven flu seasons, found that being a male was a predictor of influenza vaccination in seven countries out of eleven, including France.23 In most of these studies, gender was investigated as an explicative factor of vaccine uptake, which prevented them from understanding the extent to which factors might differ between women and men. A Norwegian study used sex-separated analyses but only focused on the effect of vaccine history on influenza vaccine uptake. They also stratified their analyses by composition of the household, and found that men who had previously been vaccinated against influenza were more likely to continue vaccination if their wife had a prior history of vaccination. Conversely, among those who had no history of vaccination, women were more likely to get vaccinated for the first time when they had a spouse who was previously vaccinated.24 In Spain, Jiménez-Garcia et al. found the same predictors of vaccine uptake among both men and women.20 Their gender-stratified analyses led them to suggest that the lower coverage rate observed in women could be explained by less social support, comorbidities and health-care provider bias. Considering that mothers are generally the ones in charge of children’s vaccination,25 and therefore are likely to be more informed about vaccination in general, we thus assumed that they may have a different attitude toward the COVID-19 vaccine from men. Moreover, vaccine uptake, and social factors affecting it, have been shown to vary depending on the type of vaccine and the cultural context.26 The current study aimed therefore to a) identify the role of socioeconomic and demographic factors as well as exposure to COVID-19 in the emergence of negative attitude toward a future COVID-19 vaccine and, b) to investigate more specifically gender differences in unwillingness to get vaccinated against COVID-19, analyzing the differentiated effect of the aforementioned factors according to gender.
Material and methods
Survey design
This article is based on four cross-sectional surveys carried out during and after the national lockdown in France, more exactly at the following dates: 7–9 April 2020 (n = 1,006), 15–17 April 2020 (n = 1,005), 24–26 April 2020 (n = 1,004), and 30 April–4 May 2020 (n = 2,003). Each of these surveys was independently conducted among nationally representative samples selected from an online research panel of more than 750,000 households, developed and maintained by IFOP (Paris, France), a survey research firm. A quota sampling method was applied to achieve samples of respondents, representative for the French adult population in terms of age, gender, occupation and population in the region of residence (rural vs urban). To limit selection bias, panelists with low response rates (e.g. panelists aged between 18 and 24 y.o, workers, and especially workers with intermediate occupations) were oversampled relative to others. The study protocol was approved by the ethical committee of the University Hospital Institute Méditerranée Infection (#2020-018).
Data collection
Attitudes toward the COVID-19 vaccine
Questions and their English version are displayed in appendix Table A. Each survey used in this paper included the following item: “If a vaccine against coronavirus were available, would you get vaccinated? Yes, certainly/Yes, probably/No, probably not/No, certainly not”. Responses were pooled in order to have a binary indicator “Yes” or “No”. In case they answered “No” (probably not or certainly not), they had to explain why. Three non-exclusive reasons were proposed: being against vaccination in general, thinking that a vaccine produced in a rush would be too dangerous, and finally considering the vaccine useless because COVID-19 is harmless. In addition, another alternative was proposed in an open-ended question.
Other collected information
The questionnaire included socioeconomic and demographic characteristics such as gender, age, region of residence, being in a couple, education level, occupational situation, and financial situation. The latter was defined from the equivalized household income per month (EHI) which corresponds to the total income reported for the household divided by the consumption unit calculated according to the household size and composition.27 The EHI was then divided into categories as follows: low (first quartile), intermediate (second and third quartiles), high (last quartile) and missing (when the income was not reported). Participants were also asked whether they got vaccinated against seasonal influenza during the previous winter season. In addition, COVID-19-related information was collected, such as: if they had been diagnosed with COVID-19 (yes/no), if friends or relatives had been diagnosed, if they lived in a strongly impacted region at the time of the survey (namely in the following regions: Hauts-de-France, Grand-Est, Bourgogne-Franche-Comté, and Île-de-France), and the level of concern about the risk of being infected (scored on a 10-item scale from 0, not worried at all, to 10, very worried).
Statistical analysis
A weighting procedure using the CALMAR method28 was applied to individual characteristics in such a way that the structure of the weighted sample matched the structure of the sampling frame in terms of age, gender, occupation and population in the region of residence. We presented unweighted and weighted data in Table 1. To take into account the non-response bias, all the analyses were performed using these weights. First, we described the study population by performing univariate and bivariate analyses and we used Chi-square tests to compare sociodemographic characteristics of men and women. Then, we analyzed differences in the prevalence of negative attitudes toward a future COVID-19 vaccine (intention to refuse the vaccine) among men and women, separately. Bivariate analyses and multivariate logistic regression models were performed to identify factors associated with the intention to refuse a COVID-19 vaccine in the entire study population and then separately for women and men. The relevance of this stratification was confirmed by a likelihood-ratio test (p < 5%). Finally, bivariate analyses with Chi-square tests were conducted to explore gender differences in reasons reported for the refusal to vaccinate. In order to describe the population who reported their intention to refuse the vaccine for a specific reason in comparison with the population who intend to accept, the factors associated with each reason for refusing the vaccine were investigated in three separate multivariate logistic regression models. Each of the latter compared vaccines refusal for only one reason with acceptance (people who reported also another reason than the one analyzed were excluded from the model). The automatic selection Stepwise procedure (p < 5%) was used for these models in order to explore the factors associated with vaccine refusal for each reason. All statistical analyses were performed with SAS version 9.4 (SAS Institute, Cary, NC, USA).
Table 1.
Characteristics of the study population by gender (column percentages) (COCONEL 2020, N = 5,018)
| All |
|||||
|---|---|---|---|---|---|
| unweighted | weighted | Women | Men | ||
| All | 100 | 100 | 52.4 | 47.6 | |
| Gender | |||||
| Women | 52.5 | 52.4 | |||
| Men | 47.5 | 47.6 | |||
| Date of the survey | ns | ||||
| 7–9 April | 20.1 | 20.1 | 20.1 | 20.1 | |
| 15–17 April | 20.0 | 20.0 | 20.0 | 20.0 | |
| 24–26 April | 20.0 | 20.0 | 20.0 | 20.0 | |
| 30 April – 04 May | 39.9 | 39.9 | 39.9 | 39.9 | |
| Age (years) | *** | ||||
| 18–24 | 9.9 | 10.3 | 12.2 | 8.2 | |
| 25–34 | 15.5 | 15.4 | 16.9 | 13.8 | |
| 35–54 | 34.7 | 34.2 | 33.1 | 35.5 | |
| 55–64 | 15.1 | 15.5 | 14.1 | 17.0 | |
| 65–74 | 12.8 | 12.6 | 13.3 | 11.8 | |
| > 74 | 12.0 | 12.0 | 10.4 | 13.7 | |
| Education level | |||||
| Lower than High school degree | 27.4 | 50.8 | 49.9 | 51.8 | |
| High school degree | 26.2 | 19.0 | 20.6 | 17.1 | |
| Higher | 46.4 | 30.2 | 29.4 | 31.1 | |
| Being in a couple | |||||
| Yes | 62.2 | 67.9 | 65.5 | 70.4 | |
| No | 37.8 | 32.2 | 34.5 | 29.6 | |
| Level of Equivalized Household Income | |||||
| Low | 19.0 | 22.2 | 25.8 | 18.3 | |
| Intermediate | 43.1 | 44.0 | 44.4 | 43.5 | |
| High | 26.8 | 22.6 | 16.9 | 29.0 | |
| Missing | 11.1 | 11.1 | 12.9 | 9.2 | |
| Occupational situation | |||||
| Working | 54.6 | 50.8 | 47.0 | 54.9 | |
| Not working | 17.8 | 21.8 | 27.1 | 15.9 | |
| Retired | 27.5 | 27.4 | 25.9 | 29.2 | |
| Vaccinated against the flu the year before | |||||
| Yes | 28.4 | 28.4 | 24.8 | 32.4 | |
| No | 71.6 | 71.6 | 75.2 | 67.6 | |
| Living in a region strongly by impacted COVID-19 | |||||
| Yes | 40.9 | 40.6 | 39.4 | 42.0 | |
| No | 59.1 | 59.4 | 60.6 | 58.0 | |
| Diagnosed with COVID-19 | |||||
| Yes | 2.5 | 2.5 | 2.4 | 2.6 | |
| No | 97.5 | 97.5 | 97.6 | 97.4 | |
| COVID-19-related concern | |||||
| High | 19.2 | 20.6 | 24.4 | 16.5 | |
| Lower | 80.8 | 79.4 | 75.6 | 83.5 | |
| Friends or relatives diagnosed with COVID-19 | |||||
| Yes | 23.9 | 22.2 | 21.8 | 22.6 | |
| No | 76.1 | 77,8 | 78.2 | 77.4 | |
| Intention to get a COVID-19 vaccine | |||||
| Yes, certainly | 36.8 | 36.1 | 31.4 | 41.4 | |
| Yes, probably | 39.9 | 39.9 | 41.6 | 38.1 | |
| No, probably not | 16.3 | 16.1 | 18.3 | 13.7 | |
| No, certainly not | 7.0 | 7.9 | 8.8 | 6.9 | |
Chi-Square test: ns no significant; $ p < 0.10; * p < 0.05; ** p < 0.01; *** p < 0.001. Population: respondents for the COCONEL surveys 7–9 April wave, 15–17 April wave, 24–26 April wave, and 30 April- 4 May wave (N = 5,018).
RESULTSStudy population and attitudes toward the COVID-19 vaccine
The combination of the four COCONEL pre-cited surveys allowed to study a sample of 5,018 respondents composed of 52.4% of women and 47.6% of men Table 1, aged 49 years old on average (51 for men and 48 for women). Women reported lower EHI than men, they were less frequently in a couple, and they reported higher scores of concern about being infected by the coronavirus. Regarding attitudes toward a potential COVID-19 vaccine, 24.0% of the participants (men: 20.6%; women: 27.1%; p < .001) reported their intention to refuse the COVID-19 vaccine once it becomes available: 16.1% “probably not”, and 7.9% “certainly not” (while 39.9% reported they will “probably” take the shot and 36.1% they will “certainly” take it). The percentage of uncertain answers also varied by gender: 59.8% of women reported doubts (i.e. they will “probably” or “probably not”) about getting vaccinated against a future COVID-19 vaccine versus 51.7% of men (p.value<0.001). Women also reported more frequently than men that they would certainly refuse the vaccine (8.8% of women against 6.9% of men, p.value<5%).
Attitudes toward a future COVID-19 vaccine vary according to the survey period and age of respondents
The intention to refuse a vaccine against COVID-19 varied according to the date of the survey Figure 1. Among women, it significantly increased in the last survey. The differences observed between men and women became significant for the two last surveys and mainly occurred among those aged 35–64. Moreover, Figure 2 shows that negative attitude toward a COVID-19 vaccine significantly declined with age for both men and women. It decreased almost linearly for men, while it started to decrease from around 45–54 years old for women.
Figure 1.
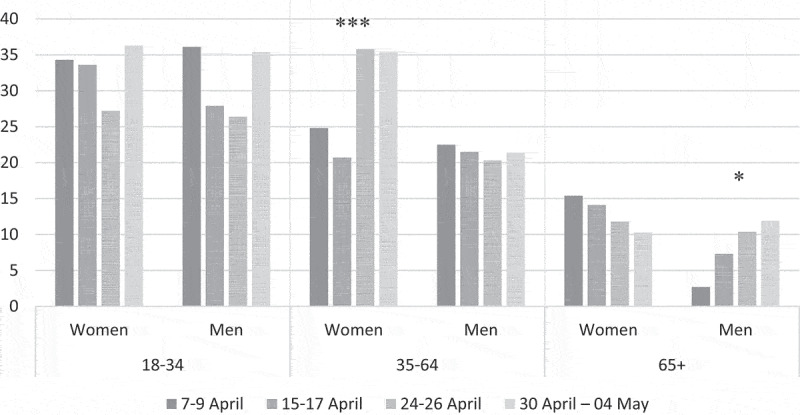
Evolution of negative attitudes toward a potential future COVID-19 vaccine over the four surveys, by age and gender (COCONEL 2020, N = 5,018)
Note: In the first survey, conducted between 7–9 April 2020, 25.0% of women reported a negative attitude toward a future COVID-19 vaccine, namely they reported their intention to refuse the vaccine once it becomes available, versus 21.2% of men. Population: respondents for the COCONEL surveys 7–9 April wave, 15–17 April wave, 24–26 April wave, and 30 April- 4 May wave (N = 5,018).
Figure 2.
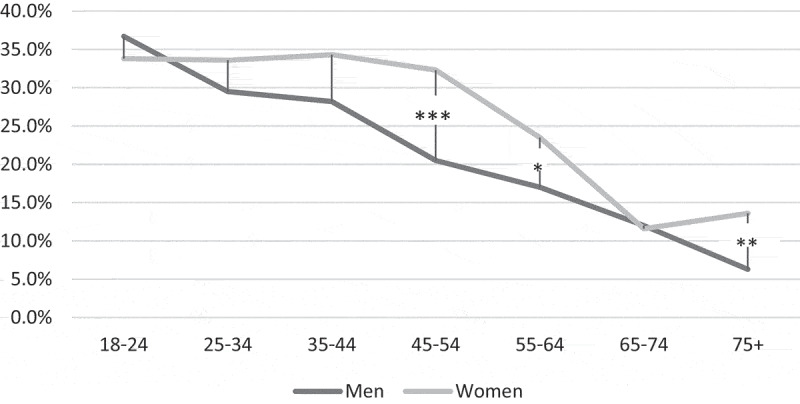
Refusal rate to vaccinate against COVID-19 according to age and gender (COCONEL 2020, N = 5,018)
Note: Among men aged between 18–24 years old, 36.7% reported their intention to refuse a future COVID-19 vaccine against 33.8% of women aged 18–24. Population: respondents for the COCONEL surveys 7–9 April wave, 15–17 April wave, 24–26 April wave, and 30 April- 4 May wave (N = 5,018).
Factors associated with a negative attitude toward a future COVID-19 vaccine
Bivariate analyses show that women were more likely than men to report the intention to refuse the vaccine. In addition, being aged 54 and above, having an higher education level than the High school degree, and being in a couple were negatively associated with vaccine refusal. Conversely, reporting low or intermediate levels of income was positively associated with this negative attitude. The date of the survey was also significantly associated with the variable of interest: women surveyed between the 30th of April and the 04th of May were more likely to refuse the vaccine than those surveyed earlier. In addition, people previously vaccinated against seasonal influenza, those reporting high concern about COVID-19, and those having friends or relatives diagnosed with COVID-19 were less likely to report a negative attitude toward this vaccine. However, no significant difference in attitudes toward a future vaccine was found depending on whether people were diagnosed with COVID-19 or not (only 2.5% of the sample were). Although this relation was not significant in both men and women separately, the relation was heading in the opposite direction between men and women: men diagnosed with COVID-19 were more likely to refuse the vaccine than those not diagnosed with COVID-19, whereas we observed the opposite in women diagnosed with COVID-19.
Focus on gender-differentiated effects
Age had a different effect in men and women Table 2: men aged under 25 were more likely to report they would refuse a future vaccine than those aged 35–54; conversely, those aged over 74 were less likely to refuse it. Among women, those aged over 54 were less likely to refuse the vaccine (no difference was identified between women aged under 35 and those aged 35–54).
Table 2.
Factors associated with negative attitudes toward a future COVID-19 vaccine by gender (COCONEL 2020, N = 5,018)
| All (n = 5,018) |
Women (n = 2,635) |
Men (n = 2,383) |
|||||
|---|---|---|---|---|---|---|---|
| Row % | Adjusted OR [95% CI] | Row % | Adjusted OR [95% CI] | Row % | Adjusted OR [95% CI] | ||
| Gender | *** | ||||||
| Men | 20.6 | 0.77 [0.67;0.89]*** | |||||
| Women | 27.1 | –1– | |||||
| Date of survey | ** | ** | |||||
| 7–26 April | 22.6 | –1– | 25.0 | –1– | 20.0 | –1– | |
| 30 April – 04 May | 26.0 | 1.18 [1.03;1.36]* | 30.2 | 1.25 [1.03;1.50]* | 21.5 | 1.14 [0.92;1.41] | |
| Age | *** | *** | *** | ||||
| 18–24 | 33.1 | 1.08 [0.87;1.35] | 33,1 | 0.83 [0.62;1.10] | 30.1 | 1.66 [1.16;2.37]** | |
| 25–34 | 1.09 [0.90; 1.32] | 0.97 [0.75; 1.24] | 1.30 [0.97; 1.75] | ||||
| 35–54 | –1– | –1– | –1– | ||||
| 55–64 | 25.8 | 0.72 [0.58; 0.89]** | 25.8 | 0.69 [0.52; 0.93]* | 18.7 | 0.77 [0.56; 1.06] | |
| 65–74 | 11.8 | 0.62 [0.46; 0.82]** | 10.7 | 0.45 [0.31;0.67]*** | 12.0 | 0.93 [0.60;1.44] | |
| > 74 | 9.6 | 0.60 [0.43;0.82]** | 13.6 | 0.61 [0.40;0.94]* | 6.3 | 0.54 [0.32;0.90]* | |
| Education level | * | * | |||||
| High school degree or lower | 27.5 | –1– | 29.2 | –1– | 25.1 | –1– | |
| Higher than High school degree | 22.5 | 0.82 [0.70;0.96]* | 27.5 | 0.84 [0.68;1.04] | 18.4 | 0.77 [0.60;0.99]* | |
| Being in a couple | *** | ** | ** | ||||
| Yes | 21.8 | 0.79 [0.68;0.92]** | 25.0 | 0.69 [0.57;0.84]*** | 18.6 | 0.98 [0.77;1.24] | |
| No | 27.4 | –1– | 29.9 | –1– | 24.1 | –1– | |
| EHI | *** | *** | *** | ||||
| Low | 31.8 | 1.62 [1.28;2.06]*** | 33.6 | 1.40 [1.01;1.92]* | 28.8 | 2.03 [1.42; 2.90]*** | |
| Intermediate | 24.8 | 1.50 [1.22;1.84]*** | 26.6 | 1.38 [1.03;1.84]* | 22.8 | 1.65 [1.22; 2.23]** | |
| High | 14.5 | –1– | 19.9 | –1– | 11.0 | –1– | |
| Missing | 24.5 | 1.05 [0.83;1.32] | 25.0 | 1.14 [0.84;1.53] | 23.7 | 0.91 [0.63;1.32] | |
| Living in a region strongly by impacted COVID-19 | ns | ns | * | ||||
| Yes | 22.7 | 0.89 [0.78; 1.03] | 27.2 | 1.03 [0.85;1.24] | 18.1 | 0.75 [0.60;0.93]** | |
| No | 24.8 | –1– | 27.0 | –1– | 22.4 | –1– | |
| Vaccinated against the flu the year before | *** | *** | *** | ||||
| Yes | 5.5 | 0.17 [0.13; 0.22]*** | 5,5 | 0.14 [0.10;0.21]*** | 5.4 | 0.19 [0.13;0.28]*** | |
| No | 31.3 | –1– | 34.2 | –1– | 27.8 | –1– | |
| COVID-19-related concern | *** | *** | *** | ||||
| High (>8) | 16.9 | 0.60 [0.50;0.73]*** | 19.0 | 0.60 [0.48;0.76]*** | 13.6 | 0.61 [0.44;0.84]** | |
| Lower | 25.8 | –1– | 29.7 | –1– | 22.0 | –1– | |
| Friends or relatives diagnosed with COVID-19 | * | $ | $ | ||||
| Yes | 21.1 | 0.83 [0.70;0.98]* | 24.1 | 0.84 [0.66;1.06] | 18.0 | 0.82 [0.63;1.06] | |
| No | 24.8 | –1– | 27.9 | –1– | 21.3 | –1– | |
| Diagnosed with COVID-19 | ns | ns | $ | ||||
| Yes | 23.8 | NI | 18.7 | NI | 29.0 | NI | |
| No | 24.0 | 27.3 | 20.3 | ||||
Chi-Square test: $p < 0.10; *p ≤ 0.05; ** p < 0.01; p < 0.001. NI covariate not included in the model because of small effectives. Note: The following model fit measures were use: Likelihood ratio test: −2Log (Model for All) – [−2Log (Model for Women) + −2Log (Model for Men)] = 4919.504–4890.198 = 29.306, p < 0.001, which confirms the relevance of gender stratification. In addition, the Nagelkerke R2 = 0.1710 for the model for all, 0.1712 for the model among women and 0.1712 for the model performed among men. Population: respondents for the COCONEL surveys 7–9 April wave, 15–17 April wave, 24–26 April wave, and 30 April- 4 May wave (N = 5,018).
In addition, the survey period (7 to 26 April versus 30 April to 04 May) and being in a couple were negatively associated with intention to refuse a future COVID-19 vaccine only among women. Conversely, an education level higher than the High School degree, and residing in a region strongly impacted by COVID-19 were negatively associated with vaccine refusal among men only.
In both men and women, similar factors were positively associated with a negative attitude toward the vaccine such as not having been vaccinated against the flu the year before, and reporting lower concern about COVID-19.
Although the level of EHI (people with low or intermediate income) was positively associated with vaccine refusal in both men and women, the effects were significantly stronger in men than in women.
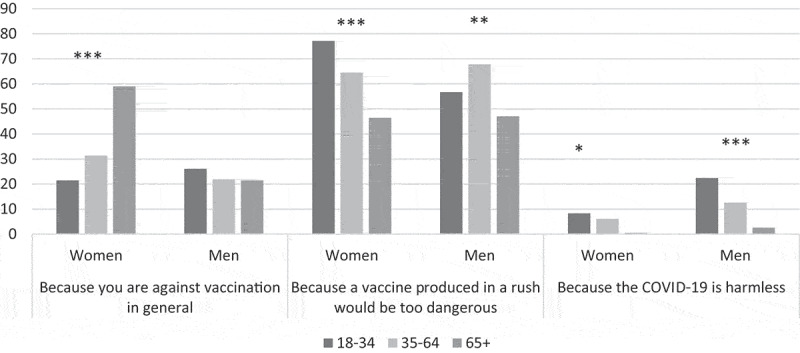
Reasons for refusing a future COVID-19 vaccine and associated factors
Among people who reported a negative attitude toward a future COVID-19 vaccine, 92.1% selected at least one of the three reasons proposed, namely thinking this vaccine would not be safe, being against vaccination in general, and the perception that COVID-19 is harmless, while the remaining 7.9% selected exclusively the open-ended modality. The latter included a general lack of trust (about politics, or medicine, science, the pharmaceutical industry or unspecified), doubts about the efficiency of the vaccine (because of possible mutations of the virus, or by comparison to the seasonal influenza vaccine), as well as thinking they are immune to the virus. These responses were too diverse to be pooled into a new category. Furthermore, as shown in Figure 3, motives for refusing the vaccine varied by gender. Women more frequently reported reasons related to vaccination in general (30.8% were against vaccination versus 23.3% among men, p < .001) or to the safety of a new COVID-19 vaccine (67.1% thought that a vaccine produced in a rush is too dangerous, versus 61.7% among men, p < .001). Conversely, men more frequently motivated their refusal of the vaccine by a perceived harmless nature of the COVID-19 (6.3% against 14.9%, p < .01).
Figure 3.
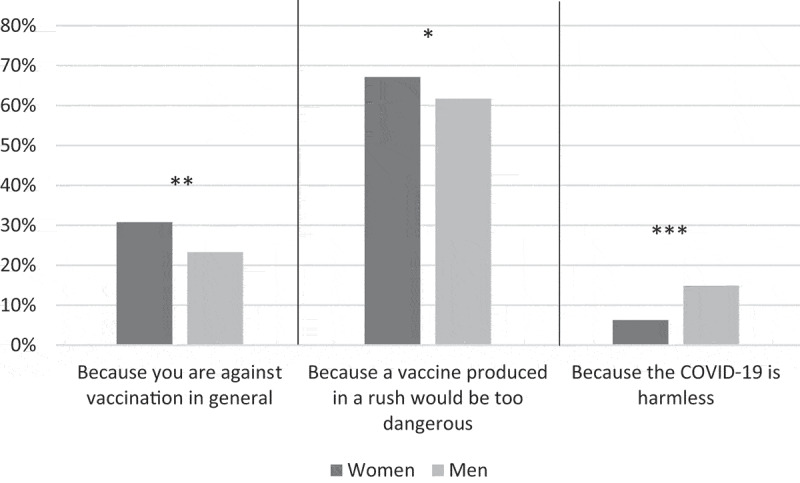
Reasons for intending to refuse a future COVID-19 vaccine by gender (COCONEL 2020, N = 1,203)
Chi-Square test: *p ≤ 0.05; ** p < .01; ***p < .001. Note: the modalities were not exclusive, the sum is thus not equal to 100. Population: respondents for the COCONEL surveys 7–9 April wave, 15–17 April wave, 24–26 April wave, and 30 April- 4 May wave who reported their intention to refuse the COVID-19 vaccine if available (N = 1,203).
Multivariate analyses confirmed these findings. Table 3 shows that the male gender was strongly associated with intention to refuse the vaccine because of the perception that the disease is harmless (versus acceptance). Conversely, the female gender was strongly associated with vaccine refusal due to the perception that the vaccine would not be safe or due to reluctance toward vaccination in general. After adjustment for gender and other covariates, a young age (<35) was positively associated with vaccine refusal due to the perception that the vaccine would not be safe or that the disease is harmless while older age (>64) was negatively associated with vaccine refusal, irrespective of the reason given. In addition, high EHI, serious concern about being infected by COVID-19 and having friends or relatives diagnosed with COVID-19 were negatively associated with intention to refuse the vaccine because of a general rejection of vaccination or thinking that this vaccine would not be safe. Finally, being in a couple was only significantly associated with being against vaccination in general, while education level and degree of COVID-19 exposition in the region of residence were only significantly associated with explaining refusal by the perceived harmless nature of COVID-19.
Table 3.
Factors associated with negative attitudes toward a future COVID-19 vaccine according the reason given (COCONEL 2020, N = 5,018)
| Intention to refuse a future COVID-19 vaccine because against vaccination in general versus acceptance (n = 4,073) | Intention to refuse a future COVID-19 vaccine because it would be safe versus acceptance (n = 4,532) | Intention to refuse a future COVID-19 vaccine because the COVID-19 is harmless versus acceptance (n = 3,915) | ||
|---|---|---|---|---|
| Adjusted OR [95% CI] | Adjusted OR [95% CI] | Adjusted OR [95% CI] | ||
| Gender | ||||
| Men | 0.48 [0.36;0.64]*** | 0.68 [0.58;0.80]*** | 1.71 [1.08;2.72]* | |
| Women | –1– | –1– | –1– | |
| Date of survey | ||||
| 7–26 April | NS | –1– | NS | |
| 30 April – 04 May | 1.20 [1.01;1.42]* | |||
| Age | ||||
| 18–34 | 0.82 [0.59;1.13] | 1.33 [1.11;1.60]** | 2.59 [1.62;4.14]*** | |
| 35–64 | –1– | –1– | –1– | |
| > 64 | 0.62 [0.44;0.87]** | 0.24 [0.18;0.33]*** | 0.04 [0.01;0.28]*** | |
| Education level | ||||
| Lower than High school degree | NS | NS | 2.06 [1.29;3.29]** | |
| High school degree or higher | –1– | |||
| Being in a couple | ||||
| Yes | 0.70 [0.53;0.92]** | NS | NS | |
| No | –1– | |||
| Level of EHI | ||||
| High | 0.42 [0.28;0.64]*** | 0.61 [0.48;0.77]*** | NS | |
| Other | –1– | –1– | ||
| Living in a region strongly by impacted COVID-19 | ||||
| Yes | NS | NS | 0.57 [0.35;0.94]** | |
| No | –1– | |||
| COVID-19-related concern | ||||
| High (>8) | 0.41 [0.28;0.62]*** | 0.68 [0.55;0.85]*** | NI | |
| Lower | –1– | –1– | ||
| Friends or relatives diagnosed with COVID-19 | ||||
| Yes | 0.69 [0.49;0.98]* | 0.78 [0.64;0.97]** | NS | |
| No | –1– | –1– | ||
NScovariate not selected by the stepwise procedure. NI covariate not included in the model. *p < 0.05; ** p < 0.01; ***p < 0.001.Population: respondents for the COCONEL surveys 7–9 April wave, 15–17 April wave, 24–26 April wave, and 30 April- 4 May wave (N = 5,018). Note: Each model compared separately vaccine refusal for only one reason, with acceptance, people who reported (also) another reason than the one analyzed were excluded from the corresponding model. The automatic selection Stepwise procedure (p < 5%) was used for these models in order to explore the factors associated with vaccine refusal for each reason.
Discussion
As the SARS-CoV-2 continues to circulate across the world, health authorities turn a hopeful eye toward a rapid development of a vaccination campaign.28,29 The slow start of this campaign in France is leading in the short term to a demand for vaccines that exceeds the available supply, but in the longer term, the choice of those hesitating could be decisive in obtaining herd immunity. According to the national COCONEL surveys, almost a quarter of the French population reported they would refuse the COVID-19 vaccine once it becomes available. Women were more reluctant to be vaccinated than men (respectively, 27.1% versus 20.6%, p < .001). Three main reasons were reported in the following declining order of frequency: thinking this vaccine will not be safe, being against vaccination in general, and perceiving COVID-19 to be harmless. After adjustment for covariates, the female gender, young age, low level of income, lack of previous practice of seasonal influenza vaccination, and perceived low risk of infection were associated with a negative attitude toward vaccination. In addition, the survey period and gender-specific factors were found to be associated with the intention to refuse a future COVID-19 vaccine such as age, being in a couple, education level, and living in a region strongly impacted by COVID-19.
Factors associated with intentions to refuse a COVID-19 vaccine: comparison with previous research
Age and gender have often been highlighted in the literature as factors associated with vaccination attitudes and behavior. Regarding the acceptability of a future COVID-19 vaccine, our results support recent findings: negative attitudes toward COVID-19 vaccination decrease with age,5–7,9 and women are more likely to refuse this vaccine.5,9 In research on influenza vaccination, high levels of education and high levels of income were found to be positively associated with vaccine acceptance, as in our study, as well as being in a couple.20,30 In addition, our finding that history of vaccination, in our case being vaccinated against the seasonal influenza during the previous season, was strongly negatively associated with reporting the intention to refuse to get vaccinated, is in line with previous research, including research on a future COVID-19 vaccine.9,17,30–33 Also, since having reported high concern about being infected with COVID-19 was negatively associated with the intention to refuse a future vaccine against COVID-19, our study confirmed the previous result that attitudes toward vaccination are strongly associated with risk perception.17,30,34 Finally, we found a decrease, over the survey period, of the willingness of the population to get vaccinated against COVID-19. This trend was confirmed in multivariate analysis and is consistent with the result of an Italian study that found such decrease between before and after their lockdown period.7 In this study, the authors assumed that the decrease of the willingness to vaccinate was related to the decrease they observed in the population’s trust in science between before and after the lockdown. This hypothesis is supported by the correlation they found between willingness to vaccinate and both trust in scientific research and general attitude toward the vaccine’s efficacy. However, because the Italian study found no difference in the decrease of the willingness to get vaccinated according to age nor gender, as we did, this hypothesis needs more investigation.
Women are more worried about the SARS-CoV-2, and more concerned by the risks of a future vaccine
While our finding that women were significantly more worried than men about being infected by the SARS-CoV-2 and about the safety of vaccines in general and especially a future COVID-9 vaccine seems paradoxical (high-risk perception being positively associated with vaccine acceptance), it might be explained by a different age structure in the two groups. People who reported their intention to refuse the future vaccine, were younger than people who reported high concerns about being infected by the virus (Appendix, Figure A1). In addition, while we found no age structure difference between men and women in the intention to refuse the vaccine, we found that, among people with high-risk perception of the COVID-19 and who reported a negative attitude toward vaccine, women were younger than men (Appendix, Figure A2). Therefore, even in people who are very concerned by the virus, vaccine acceptability varies according to age.
Nevertheless, irrespective of the risk perception level, the gender difference remained strong. Indeed, while both men and women reported the following main reasons in the same order – thinking this vaccine will not be safe, being against vaccination in general, and perceiving COVID-19 to be harmless – women were more likely than men to report vaccine-related reasons (the first two reasons above) and, conversely, men were more likely than women to report a disease-related reason (the last reason above). A review showed that vaccination may have differentiated adverse effects according to sex, as females report more frequent adverse side effects of vaccines.34,35 This might explain their greater reluctance toward vaccines. Furthermore, among people who reported their intention to refuse a COVID-19 vaccine, men were more likely than women to believe this vaccine would be useless because they tended to downplay more the severity of this disease. However, residing in a region strongly impacted by COVID-19 reduced the risk to refuse the vaccine because of the perception that the disease is harmless.
The age effect on vaccine acceptance varied according to gender
Among men, vaccine acceptance increased linearly with age, while in women, the refusal rate remained high until the age of 45–54, and decreased linearly after an inflection point at 55 years old. A lower general risk aversion in young men, as shown in the literature,36,37 might explain that being aged under 25 was strongly associated with refusing the vaccine in men, even after adjustment: young men might under-estimate the risks of COVID-19 to them, and might not have integrated their role in collective protection. According to our results, the future vaccination campaign should pay particular attention to young men and women, as they were less favorable to accept the future COVID-19 vaccine and considering that their vaccination has been found in literature as essential for the protection of older people.38 Furthermore, among people who reported their intention to refuse the vaccine, women aged 65+ mainly explained this refusal by a general hostility toward vaccination, while women aged under 35 mainly reported that the future vaccine would not be safe (Appendix, Figure A3). Those age differences need also to be considered to properly adapt the messages of future promotion campaigns to the characteristics of the public.
The better acceptance of a future COVID-19 vaccine by women in a couple than by those not in a couple might suggest a better integration, by the former, of the notion of collective protection provided by vaccination, at least at the family level, than the latter. Women might also be influenced by the opinion of their partner about vaccination but further research is needed to confirm this hypothesis.
Socioeconomic effects were stronger among men than among women: although having low or intermediate EHI was associated with the intention to refuse a future COVID-19 vaccine for men and women, the adjusted OR showed a stronger effect in men. Similarly, the effect of the level of education was stronger (and significant) in men compared with women.
The gender gap in vaccine acceptance increased in the last days of the lockdown
According to our findings, women’s reluctance toward a COVID-19 vaccine increased at the end of April-beginning of May while we found at the same time a decrease of the concern with being infected by the virus. This might be explained by increasing distrust in vaccines or in science in general at this moment, as suggested in another study in Italy.7 Indeed, a number of scientific controversies about the management of the heath crisis and the treatment of the COVID-19 have emerged during the lockdown period, and it may have negatively affected trust of the population in scientists and health authorities in general.39 Moreover, considering that women are more concerned and aware of vaccination issues because they are more often in charge of children’s vaccination,25 they are therefore more likely to be aware of previous controversies surrounding vaccines leading them to be more hesitant toward this (future) new vaccine.
Women were more hesitant than men
Regardless of the response given on the intention to accept or refuse the future vaccine, most participants were not sure about their answer (as the items including “probably” rather than “certainty” were more often selected), and women more frequently than men. We may assume that among people who reported they will probably get vaccinated once the vaccine becomes available, some of them would still have doubts when taking the vaccine. Such doubts about the future vaccine’s efficacy might have been boosted by the lack of information on this new virus (and new vaccine), especially on the level and the duration of the immune response, and therefore the possibility to be re-infected by the virus, which has been recently confirmed in a scientific publication.40 This uncertainty may express a difficulty to make a decision among reluctant people who may either decline the vaccine, delay it or accept it despite their doubts (i.e. vaccine hesitants).26 Considering that vaccine hesitancy has been found to be correlated with unfavorable perception of vaccines’ risk–benefit balance,22 vaccine hesitancy should therefore be investigated in further research among both people who present a negative attitude toward a future COVID-19 vaccine and people who present a positive attitude, to better understand what motivates the decision, irrespective of the choice made.
Strengths and limitations of the study
The surveys conducted during the lockdown period allowed us to explore the attitudes toward a future COVID-19 vaccine of French men and women during the acute phase of the epidemic. However, this study has some limitations. The lockdown affected data collection activities and online surveys were an effective way to carry out surveys in this context but it may involve some selection biases that we attempted to limit. First, most French households have Internet access (89% estimated for 2018)41 and the survey samples were stratified to be representative of the French population in terms of gender, age, occupation, area of residence, and region. In addition, the theme of the survey was not mentioned in the invitation e-mail to avoid influencing participation. Furthermore, this paper aimed to explore factors associated with negative attitudes toward a future COVID-19 vaccine that did not exist at the time of data collection. We thus need to keep in mind that intentions reported during the lockdown period can vary with time, and that intention does not necessarily translate into behavior.42
Conclusion
In conclusion, this study contributes to the advancement of knowledge on public attitudes toward COVID-19 vaccines, which could be useful to design and adapt vaccination campaigns. More specifically, our findings regarding gender differences are not intended to promote the implementation of a gender-differentiated vaccination campaign; however, these results must be known to guide future prevention messages. Public health authorities should pay specific attention to the public likely to not get a COVID-19 vaccine when one becomes available, driven by concerns about safety and effectiveness. This public represented a quarter of the French population during the lockdown period, but it may have increased since.6,43,44 It therefore seems crucial to guarantee that all the necessary precautions are taken before marketing each vaccine and to communicate transparently on this process as we have previously argued,45 but also on the coverage rate needed to reach herd immunity. Furthermore, more research is needed to explore the evolution of attitudes toward vaccination against the coronavirus, separately among men and women, and the media coverage of vaccination campaigns. Media and journalists should be able to rely on information tools and intervention strategies to enhance acceptability of the future COVID-19 vaccine.
Acknowledgments
This work was supported by grants from the Agence Nationale de la Recherche (ANR-20-COVI-0035-01). The authors would like to thank the COCONEL Group that includes Patrick Peretti-Watel, Valérie Seror, Sébastien Cortaredona, Odile Launay, Jocelyn Raude, Pierre Verger, Caroline Alleaume, Lisa Fressard, François Beck, Stéphane Legleye, Damien Léger, Olivier L’Haridon, and Jeremy Ward.
Appendices.
Figure A1.
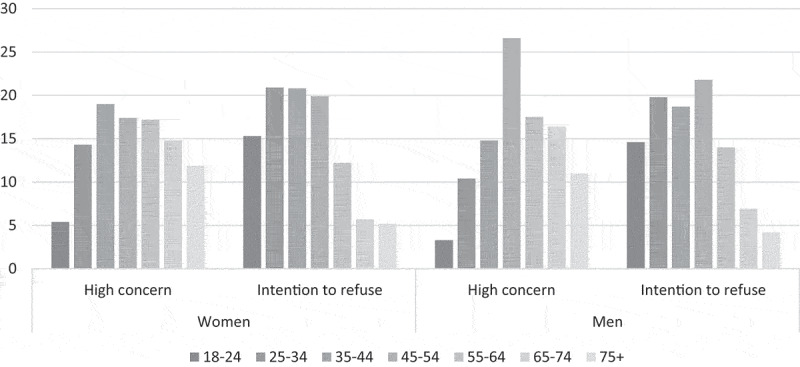
Age structure of people with high concern and those who reported their intention to refuse the COVID-19 vaccine by gender (COCONEL 2020, N = 5,018)
Population: respondents for the COCONEL surveys 7–9 April wave, 15–17 April wave, 24–26 April wave, and 30 April- 4 May wave (N = 5,018).
Figure A2.
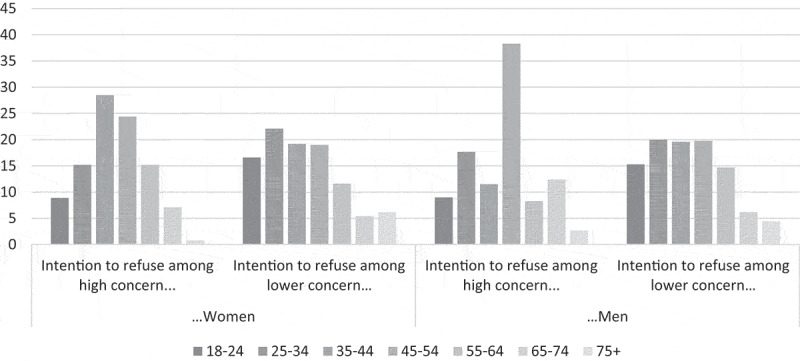
Age structure of people who reported their intention to refuse the COVID-19 vaccine according to gender and level of concern about the COVID-19 (COCONEL 2020, N = 5,018)
Population: respondents for the COCONEL surveys 7–9 April wave, 15–17 April wave, 24–26 April wave, and 30 April- 4 May wave (N = 5,018).
Figure A3.
Evolution across surveys of the reasons for intending to refuse a future COVID-19 vaccine by gender (COCONEL 2020, N = 1,203)
Population: respondents for the COCONEL surveys 7–9 April wave, 15–17 April wave, 24–26 April wave, and 30 April- 4 May wave (N = 5,018).
Table A.
Questions extracted from the questionnaires in French and translated in English
| Question title | Question title translated |
|---|---|
| Sociodemographic questions | |
| Vous êtes … ? Un homme/Une femme | You are … ? A man/A woman |
| Quel âge avez-vous ? | How old are you ? |
| À ce jour, le plus haut diplôme que vous possédez est … ? | To date, the highest degree you hold is … ? |
| En prenant en compte tous les types de revenus que touchent les membres de votre foyer, quel est actuellement le montant mensuel net des ressources de l’ensemble votre ménage ? | Considering all types of income your household members receive, what is currently the net monthly amount of resources in your household as a whole? |
| De combien de personnes se compose votre foyer y compris vous-même ? | How many people make up your household, including yourself? |
| Au total, combien y a-t-il d’enfants de moins de 14 ans dans votre foyer ? | In total, how many children under the age of 14 are in your household? |
| Quelle est, approximativement, la surface totale du logement où vous vivez actuellement en mètres carrés habitables ? | What is, approximately, the total area of the dwelling where you currently live in square meters of living space? |
| Êtes-vous actuellement en couple ? Oui, avec une personne qui vit dans votre logement/Oui, avec une personne qui vit dans un autre logement/Non, mais vous avez déjà été en couple par le passé/Non, vous n’avez jamais été en couple. | Are you currently in a relationship? Yes, with a person who lives in your dwelling/Yes, with a person who lives in another dwelling/No, but you have been in a relationship in the past/No, you have never been in a relationship. |
| Avant le confinement, quelle était votre situation ? Vous exerciez une activité professionnelle (actifs, apprentis, stagiaires)/Vous étiez chômeur ayant déjà travaillé/Vous étiez à la retraite ou en pré-retraite/Vous étiez à la recherche d’’un premier emploi/Vous étiez collégien, lycéen ou étudiant/Vous étiez homme ou femme au foyer/Vous étiez dans une autre situation (invalide, sans activité professionnelle …) | Before lockdown, what was your occupational situation? You had a professional activity (working, apprentice, trainee)/You were unemployed and had already worked/You were retired or in pre-retirement/You were looking for your first job/You were at college, high school or student/You were a man or a housewife/You were in another situation (invalid, without professional activity …) |
| Actuellement, continuez-vous à travailler ? Oui, à l’extérieur de mon domicile à temps complet/Oui, à l’extérieur de mon domicile à temps partiel/Oui, en télétravail/Non, vous êtes arrêté le temps du confinement (chômage partiel, congé maladie)/Non, vous êtes en recherche d’emploi. | Are you currently still working? Yes, outside my home full time/Yes, outside my home part time/Yes, teleworking/No, you are stopped during the time of confinement (part-time unemployment, sick leave)/No, you are looking for work. |
| COVID-19 related questions | |
| Si un vaccin contre le coronavirus était disponible, vous feriez-vous vacciner ? Oui certainement/Oui, probablement/Non, probablement pas/Non, certainement pas |
If a vaccine against coronavirus were available, would you get vaccinated? Yes, certainly/Yes, probably/No, probably not/No, certainly not |
| Pour quelles raisons ne vous feriez-vous pas vacciner ? (plusieurs réponses possibles) Parce que vous êtes contre la vaccination en général; Parce que vous pensez qu’un vaccin élaboré dans l’urgence est trop dangereux; Parce que vous pensez que c’est inutile de toute façon, le COVID-19 est peu dangereux; Autre, précisez [champ ouvert]. |
For what reasons wouldn’t you get vaccinated? (multiple answers possible) Because you are against vaccination in general; Because you think a vaccine developed in an emergency is too dangerous; Because you think it’s useless anyway, COVID-19 is not very dangerous; Other, specify [open field]. |
| Vous-même avez-vous, ou avez-vous eu, une infection à coronavirus confirmée par un test ou diagnostiquée par un médecin ? Oui/Non | Do you have, or have you had, a coronavirus infection confirmed by a test or diagnosed by a doctor? Yes/No |
| Avez-vous des proches (familles, amis) qui sont ou qui ont été malades du coronavirus ? Oui/Non | Do you have loved ones (family, friends) who are or have been sick with coronavirus? Yes/No |
| Sur une échelle de 0 à 10, à quel point la possibilité [d’attraper/d’attraper à nouveau] le Coronavirus (COVID-19) d’ici la fin de l’épidémie vous inquiète-t-elle ? 0/1/2/3/4/5/6/7/8/9/10/Je ne sais pas |
On a scale of 0 to 10, how worried are you about the possibility of [catching/re-catching] the Coronavirus (COVID-19) by the end of the epidemic? 0/1/2/3/4/5/6/7/8/9/10/I don’t know |
| Other | |
| Vous êtes-vous fait vacciner contre la grippe lors de l’hiver 2019–2020 ? Oui/Non | Did you get vaccinated against the influenza in the winter of 2019–2020? Yes/No |
Disclosure statement
The authors declare no competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Larson HJ, De Figueiredo A, Xiahong Z, Schulz WS, Verger P, Johnston IG, Cook AR, Jones NS.. The state of vaccine confidence 2016: global insights through a 67-country survey. EBioMedicine. 2016;12:295–301. doi: 10.1016/j.ebiom.2016.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gallup . Wellcome global monitor. First Wave Findings. https://wellcome.org/sites/default/files/wellcome-global-monitor-2018.pdf;2019. [accessed 19 October 2020].
- 3.De Figueiredo A, Simas C, Karafillakis E, Paterson P, Larson HJ.. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. The Lancet. 2020;396(10255):898–908. doi: 10.1016/S0140-6736(20)31558-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ward JK, Alleaume C, Peretti-Watel P; the COCONEL Group . The French public’s attitudes to a future COVID-19 vaccine: the politicization of a public health issue. Soc Sci Med. 2020;265:113414. doi: 10.1016/j.socscimed.2020.113414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neumann-Böhme S, Varghese NE, Sabat I, Barros PP, Brouwer W, Van Exel J, Schreyögg J, Stargardt T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J HEalth Econ. 2020;21(7):977–82. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, Kimball S, El-Mohandes A, Global A. Survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2020:1–4. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Palamenghi L, Barello S, Boccia S, Graffigna G. Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. Eur J Epidemiol. 2020:1–4. doi: 10.1007/s10654-020-00675-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thunstrom L, Ashworth M, Finnoff D, S N. Hesitancy towards a COVID-19 vaccine and prospects for Herd immunity. SSRN Scholarly Paper. Rochester (NY): Social Science Research Network; 2020. doi: 10.2139/ssrn.3593098. [DOI] [Google Scholar]
- 9.Malik AA, S-am M, Elharake J, Omer SB. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Padhi BK, Almohaithef MA. Determinants of COVID-19 vaccine acceptance in Saudi Arabia: a web-based national survey. MedRxiv 2020, doi: 10.1101/2020.05.27.20114413. [DOI] [PMC free article] [PubMed]
- 11.Harapan H, Wagner AL, Yufika A, Winardi W, Anwar S, Gan AK, Setiawan AM, Rajamoorthy Y, Sofyan H, Mudatsir M. Acceptance of a COVID-19 vaccine in Southeast Asia: a cross-sectional study in Indonesia. Front Public Health. 2020:8. doi: 10.3389/fpubh.2020.00381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nguyen T, Henningsen KH, Brehaut JC, Hoe E, Wilson K. Acceptance of a pandemic influenza vaccine: a systematic review of surveys of the general public. Infect Drug Resist. 2011;4:197–207. doi: 10.2147/IDR.S23174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu S, Su J, Yang P, Zhang H, Li H, Chu Y, Hua W, Li C, Tang Y, Wang Q. Factors associated with the uptake of seasonal influenza vaccination in older and younger adults: a large, population-based survey in Beijing, China. BMJ Open. 2017;7(9):e017459. doi: 10.1136/bmjopen-2017-017459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.La EM, Trantham L, Kurosky SK, Odom D, Aris E, Hogea C. An analysis of factors associated with influenza, pneumoccocal, Tdap, and herpes zoster vaccine uptake in the US adult population and corresponding inter-state variability. Hum Vaccin Immunother. 2018;14(2):430–41. doi: 10.1080/21645515.2017.1403697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Applewhite A, Stancampiano FF, Harris DM, Manaois A, Dimuna J, Glenn J, Heckman MG, Brushaber DE, Sher T, Valery J-R, et al. Analysis of gender-based difference in adherence to influenza vaccination during the 2018-2019 season. J Prim Care Community Health. 2020;11:215013272095853. doi: 10.1177/2150132720958532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raude J, A-l C-B, Setbon M. The 2009 pandemic H1N1 influenza vaccination in France: who accepted to receive the vaccine and why? PLoS Curr. 2010;2:RRN1188. doi: 10.1371/currents.RRN1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bish A, Yardley L, Nicoll A, Michie S. Factors associated with uptake of vaccination against pandemic influenza: a systematic review. Vaccine. 2011;29(38):6472–84. doi: 10.1016/j.vaccine.2011.06.107. [DOI] [PubMed] [Google Scholar]
- 18.Velan B, Kaplan G, Ziv A, Boyko V, L L-G. Major motives in non-acceptance of A/h1n1 flu vaccination: the weight of rational assessment. Vaccine. 2011;29(6):1173–79. doi: 10.1016/j.vaccine.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 19.Peretti-Watel P, Raude J, Sagaon-Teyssier L, Constant A, Verger P, Beck F. Attitudes toward vaccination and the h1n1 vaccine: poor people’s unfounded fears or legitimate concerns of the elite? Soc Sci Med. 2014;109:10–18. doi: 10.1016/j.socscimed.2014.02.035. [DOI] [PubMed] [Google Scholar]
- 20.Jiménez-García R, Hernández-Barrera V, Lopez De Andres A, Jimenez-Trujillo I, Esteban-Hernández J, Carrasco-Garrido P. Gender influence in influenza vaccine uptake in Spain: time trends analysis (1995–2006). Vaccine. 2010;28(38):6169–75. doi: 10.1016/j.vaccine.2010.07.029. [DOI] [PubMed] [Google Scholar]
- 21.Pulcini C, Massin S, Launay O, Verger P. Factors associated with vaccination for Hepatitis B, Pertussis, Seasonal and Pandemic influenza among French general practitioners: a 2010 survey. Vaccine. 2013;31(37):3943–49. doi: 10.1016/j.vaccine.2013.06.039. [DOI] [PubMed] [Google Scholar]
- 22.Rey D, Fressard L, Cortaredona S, Bocquier A, Gautier A, Peretti-Watel P, Verger P; the Baromètre santé 2016 Group . Vaccine hesitancy in the French population in 2016, and its association with vaccine uptake and perceived vaccine risk–benefit balance. Eurosurveillance. 2018;23(17):17–00816. doi: 10.2807/1560-7917.ES.2018.23.17.17-00816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Endrich MM, Blank PR, Szucs TD. Influenza vaccination uptake and socioeconomic determinants in 11 European countries. Vaccine. 2009;27(30):4018–24. doi: 10.1016/j.vaccine.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 24.Mamelund S-E, Bergsaker MAR. Vaccine history, gender and influenza vaccination in a household context. Vaccine. 2011;29(51):9441–50. doi: 10.1016/j.vaccine.2011.10.035. [DOI] [PubMed] [Google Scholar]
- 25.Peretti‐Watel P, Ward JK, Vergelys C, Bocquier A, Raude J, Verger P. Vaccine hesitancy, commitment and trust among parents of young children. Sociol Health Illn ‘I Think I Made The Right Decision … I Hope I’m Not Wrong’. 2019;41(6):1192–206. doi: 10.1111/1467-9566.12902. [DOI] [PubMed] [Google Scholar]
- 26.Peretti-Watel P, Larson HJ, Ward JK, Schulz WS, Verger P. Vaccine hesitancy: clarifying a theoretical framework for an ambiguous notion. PLoS Curr. 2015:7. doi: 10.1371/currents.outbreaks.6844c80ff9f5b273f34c91f71b7fc289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Insee . Consumption unit, https://www.insee.fr/en/metadonnees/definition/c1802;2016. [accessed 8 November 2020].
- 28.Sautory ORedressement d’échantillons d’enquêtes auprès des ménages par calage sur marges. Document de travail de l’INSEE 1991, n° F 9103.
- 29.Yamey G, Schäferhoff M, Hatchett R, Pate M, Zhao F, McDade KK. Ensuring global access to COVID-19 vaccines. The Lancet. 2020;395(10234):1405–06. doi: 10.1016/S0140-6736(20)30763-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ward L, Draper JA. Review of the factors involved in older people’s decision making with regard to influenza vaccination: a literature review. J Clin Nurs. 2008;17(1):5–16. doi: 10.1111/j.1365-2702.2006.01861.x. [DOI] [PubMed] [Google Scholar]
- 31.Szucs TD, Müller D. Influenza vaccination coverage rates in five European countries—a population-based cross-sectional analysis of two consecutive influenza seasons. Vaccine. 2005;23(43):5055–63. doi: 10.1016/j.vaccine.2005.06.005. [DOI] [PubMed] [Google Scholar]
- 32.Kan T, Zhang J. Factors influencing seasonal influenza vaccination behaviour among elderly people: a systematic review. Public Health. 2018;156:67–78. doi: 10.1016/j.puhe.2017.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Verger P, Bocquier A, Vergélys C, Ward JK, Peretti-Watel P. Flu vaccination among patients with diabetes: motives, perceptions, trust, and risk culture - a qualitative survey. BMC Public Health. 2018:569. doi: 10.1186/s12889-018-5441-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Van Der Weerd W, Timmermans DR-M, Beaujean DJ-M-A, Oudhoff J, Van Steenbergen JE. Monitoring the level of government trust, risk perception and intention of the general public to adopt protective measures during the influenza A (H1N1) pandemic in the Netherlands. BMC Public Health. 2011;575. https://doi.10.1186/1471-2458-11-575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Flanagan KL, Fink AL, Plebanski M, Klein SL. Sex and gender differences in the outcomes of vaccination over the life course. Annu Rev Cell Dev Biol. 2017;33(1):577–99. doi: 10.1146/annurev-cellbio-100616-060718. [DOI] [PubMed] [Google Scholar]
- 36.Eckel CC, Grossman PJ.Chapter 113 men, women and risk aversion: experimental evidence.Plott CR, Smith VL, editors. Handbook of experimental economics results. Vol. 1; 2008: p.1061–73. Elsevier. doi: 10.1016/S1574-0722(07)00113-8 [DOI] [Google Scholar]
- 37.Borghans L, Heckman JJ, Golsteyn BHH, Meijers H. gender differences in risk aversion and ambiguity aversion. J Eur Econ Assoc. 2009;7(2–3):649–58. doi: 10.1162/JEEA.2009.7.2-3.649. [DOI] [Google Scholar]
- 38.Giubilini A, Savulescu J, Wilkinson D. COVID-19 vaccine: vaccinate the young to protect the old? J Law Biosci. 2020;7(1). doi: 10.1093/jlb/lsaa050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Watson J. Open letter to MR Mehra et al., and to R Horton (editor of The Lancet) Concerns regarding the statistical analysis and data integrity. The Lancet. 2020. doi: 10.5281/zenodo.3862789. [DOI] [Google Scholar]
- 40.To KK-W, Hung IF-N, Ip JD, Chu AW-H, Chan W-M, Tam AR, Fong CH-Y, Yuan S, Tsoi H-W, Chin-Ki Ng A, Lap-Yip Lee L, Wan P, Tso E, To W-K, Tsang D, Chan K-H, Huang J-D, Kok K-H, Chi-Chung Cheng V, Yuen K-Y.Coronavirus disease 2019. (COVID-19) re-infection by a phylogenetically distinct severe acute respiratory syndrome coronavirus 2 strain confirmed by whole genome sequencing. Clin Infect Dis. 2020. doi: 10.1093/cid/ciaa1275 [DOI] [PMC free article] [PubMed]
- 41.Statistica . Part des ménages ayant un accès internet en France de 2006 à 2018, https://fr.statista.com/statistiques/509227/menage-francais-acces-internet;2019. [accessed 23 September 2020].
- 42.Armitage CJ, Conner M. Efficacy of the theory of planned behaviour: a meta-analytic review. Br J Social Psychol. 2001;40(4):471–99. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- 43.Ipsos . Global attitudes on a COVID-19 vaccine, http://www3.weforum.org/docs/WEF_survey_vaccine_confidence_2020.pdf;2020. [accessed 23 September 2020].
- 44.World Economic Forum . Survey shown rising vaccine hesitancy threatening COVID-19 recovery, https://www.weforum.org/press/2020/11/survey-shows-rising-vaccine-hesitancy-threatening-covid-19-recovery/;2020. [accessed 10 November 2020].
- 45.The COCONEL Group . A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation. Lancet Infect Dis. 2020;20(7):769–70. doi: 10.1016/S1473-3099(20)30426-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


