ABSTRACT
Introduction: HPV vaccines were administered in mainland China from July 2017 at a gradual rate. We aimed to assess the vaccination rate and vaccination influencing factors among college students in mainland China.
Methods: From October to December 2018, we conducted face-to-face questionnaires including 5 sections and 22 questions to collect demographic information, HPV infection and transmission knowledge, HPV vaccine knowledge and attitudes among college students in Guangzhou, China. HPV vaccine vaccination status and cervical screening behaviors were self-reported. Knowledge and attitudes differences between the vaccinate and non-vaccinate groups were analyzed using univariable logistic regression. Vaccination-related influencing factors were estimated using multivariable logistic regression.
Results: 5307 of 5414 valid questionnaires were collected. The self-reported cervical screening rate and HPV vaccine coverage were 11.82% (9.03%-14.61%) and 3.09% (2.62%-3.56%). In total, 55.57% of the participants were hesitant about vaccination. Urban residence (OR = 2.1, 95%CI: 1.4–3.3), high monthly consumption (OR = 2.6, 95%CI: 1.9–3.6), awareness of vaccination adaptive population (OR = 3.1, 95%CI: 1.9–5.0), awareness of infection-related risk factors (OR = 2.5, 95%CI: 1.1–5.7), and awareness of HPV vaccine effectiveness (OR = 3.2, 95%CI: 2.0–5.2) were significant in multivariable logistic regression.
Conclusion: HPV vaccine coverage is quite low among college students in China Guangzhou. Economic affordability, awareness of HPV infection, and belief in the effectiveness of HPV vaccine are influencing factors for vaccination. In the future, establishing a national financial subsidy and strengthening health education is needed to increase the vaccination rate in China.
KEYWORDS: HPV vaccine, knowledge, attitude, influencing factor
Introduction
Cervical cancer is the fourth most common female malignancy worldwide and represents a major global health challenge. In 2018, an estimated 570K new cases of cervical cancer were diagnosed, and 310K deaths occurred worldwide due to this malignancy.1 Approximately 85% of cases and 90% of deaths occurred in low-income and middle-income countries (LMICs), where mortality is 18 times higher than that in developed countries.2,3 In 2018, the Director General of the World Health Organization (WHO) announced a call to action for the elimination of cervical cancer as a public health problem.
Persistent infection with high-risk human papillomavirus (HPV) is the primary cause of cervical cancer, and cervical screening and vaccination programs are effective strategies for disease prevention.4 The first HPV vaccine (4vHPV) became available in 2006. As of October 2018, over 100 countries had implemented national HPV immunization programs (47%), four countries had implemented subnational HPV immunization programs, and 12 overseas territories had implemented HPV immunization programs.5,6 In recent decades, many women in high-income and upper-middle-income countries have been vaccinated against HPV.7,8 And in countries in which at least 50% of the eligible females were vaccinated, HPV vaccines (2vHPV, 4vHPV and 9vHPV) have been proven to reduce high-grade cervical dysplasia by 40% and decrease HPV infection by 70% to 90%.7,9–13 However, the introduction of vaccine programs in LMICs has been restricted by government policy, cost, paucities of adolescent health platforms, cultural challenges, and difficulties in reaching target populations.14
China, as an upper-middle-income country, is not in a favorable position for the prevention and control of cervical cancer. In the past 3 decades, morbidity of and mortality due to cervical cancer have shown increasing trends, which reported more than 130,000 cervical cancer cases each year.15 Although HPV vaccines have been licensed in mainland China for years, coverage is not very clear. In July 2016, the 2vHPV vaccine targeting HPV16 and HPV18 was introduced and approved for use in female individuals aged 9 to 45 years by the China Food and Drug Administration (CFDA). The 4vHPV (HPV6, HPV11, HPV16, and HPV18) vaccine was launched and approved for use in female individuals aged 20 to 45 years by the CFDA in 2017 May. The following year, the 9vHPV vaccine against HPV6, HPV11, HPV16, HPV18, HPV31, HPV33, HPV45, HPV52, and HPV58 was launched and approved for use in female individuals aged 16 to 26 years by the National Medical Products Administration (NMPA) in 2018 April.16 At present, the HPV vaccine is not approved for use in men and neither is included in the national immunization program and needs to be vaccinated at its own expense. According to CFDA approval, only women aged 20 to 26 can choose any one of these three HPV vaccines. As HPV vaccines coverage has not been reported openly, this study intends to evaluate the uptake rate of HPV vaccine and assess knowledge and attitudes regarding HPV vaccination among university students.
Methods
Participant selection and sampling
We interviewed students at Guangzhou university town from October to December 2018. It is the largest university town in the Guangdong-Hong Kong-Macao Greater Bay Area (GBA), covering an area of 18 square kilometers and containing 12 geographically connected colleges and universities with nearly 200,000 registered students. This particular age group was selected because the HPV vaccines marketed in mainland China have been approved for different age groups (from 9 to 45), and only the 20–26 age group was covered by all three vaccines. To understand all three types of vaccine coverage and consider the quality of sampling and the questionnaires, the inclusion criteria are as follows: (1) students registered in Guangzhou university town, (2) Chinese nationality. Exclusion criteria are as follows: (1) visiting scholars and exchange students, (2) years younger than 20 or older than 26. All the sampled subjects agreed to participate in the investigation and completed a face-to-face interview followed by a 2-page questionnaire. The sample size was calculated to be 3884 using the formula N = t2PQ/d2, d = 0.1 × P, with an assumed coverage of 9%, which was concluded from Hong Kong surveillance.17,18 Considering a non-response rate of 25%, the final sample size was 5179. According to the sample size, we implemented proportion allocation and stratified random sampling: 12 levels were established and divided by the number of colleges in the university town, and the sample size in each level was weighted by the number of registered students. Then, students at each level were randomly selected as participants in this survey (Appendix A).
Questionnaire design and content
We designed the HPV vaccine questionnaire to have 5 sections, including 22 questions. The first section (I) collected demographic information (6 items), including sex, age, hometown, education level, marital status and sexual active, and monthly expenses. Hometowns were classified as “rural” or “urban” according to their family’s address and administrative division. The education level was classified as “college,” “undergraduate” or “graduate or above.” Marital status was classified as “married,” “in a relationship” or “single.” Sexual activity was classified as “heterosexual,” “homosexual,” “bisexual” or “not sexually active,” and monthly expenses were calculated in RMB (exchange rate between RMB and $ is about 6.5:1) and classified as “low (<1000 RMB),” “middle (1000–1999 RMB)” or “high (above 2000 RMB).” The second section (II) collected information about vaccination, cervical screening behavior and initiative learning behavior like actively search for knowledge about HPV infection, cervical cancer, and HPV vaccine via internet, books, magazines and other media platforms (3 items). Vaccination status is self-reported. Cervical screening behavior is asked if students ever had a Pap smear, liquid-based cytology (LBC), visual inspection with acetic acid (VIA) and HPV DNA testing. The third section (III) collected knowledge about HPV infection (4 items) and included the questions “Have you heard of cervical cancer?” “Does HPV infection lead to cervical cancer?” “How is HPV transmitted?” and “Why is HPV infection high risk?”. The fourth section (IV) collected knowledge about the HPV vaccine (4 items) and included the questions “Have you heard of the HPV vaccine?”, “Can the HPV vaccine protect you from cervical cancer?”, “Who is the adaptive vaccination population (only female, only male, both)?” and “What are the differences among the different vaccines?”. The fifth section (V) collected information about attitudes toward HPV vaccination and reasons for these attitudes (5 items); it included the questions “Would you consider being vaccinated?”, “Which vaccine would you select?”, “Will you recommend vaccination to relatives and friends?” and “What factors do you considering when selecting an HPV vaccine?”. Furthermore, we recorded reasons for their willingness to vaccinate. All questions were either closed-ended or multiple-choice. Questionnaire was edited into Wechat applet in advance.
Data collection and quality management
This survey was approved by the ethics committee of the Guangzhou Center for Disease Control and Prevention. All participants provided informed consent before completing the questionnaire survey. Pilot surveys were conducted in July 2018 before the study to guarantee both the validity and logicality of the questionnaire content and order. Investigators consisted of epidemiologists and dialect interpreters and spent an average of 3 hours a day recruiting participants. All interviewers attended 3 hours of pre-training before conducting interviews. During the interview, which lasted about 20 minutes, investigators asked 22 questions face to face and fill in the questionnaire online using the WeChat applet. All collected data submitted and recorded in an online database and downloaded after investigation. Valid questionnaires are defined as fulfilled primary outcome (vaccinate HPV vaccine or not) and basic demographic information.
Data analysis
The primary outcome of this survey is to estimate HPV vaccine coverage in college students. Rate and 95%CI were calculated to assess variability. The multiple-choice questions (2 questions for HPV vaccine knowledge and vaccination attitude) were analyzed by the multiple response method using count and proportions. Univariable logistic regression analysis and chi-square analysis were used to compare differences in demographic & Basic information (8 variables: sex, hometown, education, marital status and sexual active, type of sexual active, monthly expenses, cervical cancer screen behavior, knowledge acquisition behavior) HPV knowledge (4 variables in the third section of questionnaire), HPV vaccine knowledge (3 variables in the fourth section of questionnaire), and vaccination attitudes (3 variables in the fifth section of questionnaire) between the vaccination and non-vaccination groups, between the sexual and not sexually active groups, and between the urban and rural groups. The significant variables in univariable regression were selected and multivariable logistic regression analyses were performed to clarify the relationships between HPV vaccination behavior and vaccine knowledge, attitudes and demographic variables. To identify significant independent predictors of HPV vaccination behavior, odds ratios (ORs) were calculated after controlling for gender, hometown, and monthly expenses. We used EpiData 3.1 (Odense, Denmark; available at http://www.epidata.dk/) for data recording and duplication checking. IBM SPSS Statistics (version 17.0; SPSS Inc., Chicago, IL, USA) and R project were used for further analysis.
Results
Demographic characteristics and HPV coverage
In total, 5414 college students participated in the study, and 5307 valid questionnaires were collected. The demographic characteristics and coverage of the study population are shown in Table 1. Among these students, 3804 (72.5%) were female. The median age was 21 years old (IQR 20–24). The numbers of students from rural areas and urban areas were approximately equal (50.7% vs 49.3%). Most students were undergraduates (96.6%), and the participants' number ratio of “natural science & technology” to “social sciences” was 0.4 (1571:3736). Nearly all students were unmarried (99.7%), with less than half (46.1%) reporting that they have/had a boyfriend/girlfriend. A majority (85.2%) of students claimed that they had never engaged in sexual activity, while 12.8% reported having prior heterosexual intercourse; 1.5% reported having prior homosexual intercourse, and 0.4% reported having both homosexual and heterosexual intercourse. The median average monthly expenditure was 1200 RMB (IQR 1000–1500). Overall, the HPV vaccine coverage rate was 3.1% (2.6%, 3.6%). For six demographic characteristics, HPV vaccine coverage is higher in female (3.5%), urban area (4.6%), graduate or above education level (5.6%), married status (6.7%), bisesual behavior (13.6%), and monthly expense over 2000 RMB (7.6%) groups.
Table 1.
Demographic characteristics of the study participants (N = 5307)
| Demographic & Basic Information | Coverage |
Total (%, N = 5307) | Vaccination group (%, n = 164) | Non-vaccination groups |
χ2 | p | OR |
|---|---|---|---|---|---|---|---|
| (rate, 95%CI) | (%, n = 5143) | ||||||
| Sex | |||||||
| Male | 2.0(1.3, 2.8) | 1475 (27.8) | 30 (18.3) | 1445 (28.1) | 7.6 | <.05 | 1.0 |
| Female | 3.5(2.9, 4.1) | 3832 (72.2) | 134 (81.7) | 3698 (71.9) | 1.8 (1.2–2.6) | ||
| Hometown | |||||||
| Rural area | 1.6(1.1, 2.1) | 2690 (50.7) | 43 (26.2) | 2647 (51.5) | 40.5 | <.001 | 1.0 |
| Urban area | 4.6(3.8, 5.4) | 2617 (49.3) | 121 (73.8) | 2496 (48.5) | 3.0 (2.1–4.2) | ||
| Education | |||||||
| College:1–3 years of technical school training | 2.3(0.0, 5.5) | 86 (1.6) | 2 (1.2) | 84 (1.6) | 5.6 | .1 | 1.0 |
| Undergraduate | 3.0(2.6, 3.5) | 5041 (95.0) | 152 (92.7) | 4889 (95.1) | 1.3 (0.3–5.4) | ||
| Graduate or above | 5.6(2.21, 8.9) | 180 (3.4) | 10 (6.1) | 170 (3.3) | 2.5 (0.5–11.5) | ||
| Marital status and sexually active | |||||||
| Single without sexually active | 2.2(1.7, 2.7) | 2824 (53.2) | 62 (37.8) | 2762 (53.7) | 16.6 | <.05 | 1.0 |
| Married | 6.7(0.0, 19.3) | 15 (0.3) | 1 (0.6) | 14 (0.3) | 3.2 (0.4–24.6) | ||
| In a relationship with sexually active | 3.9(2.5, 5.3) | 742 (14.0) | 29 (17.7) | 713 (13.9) | 1.8 (1.2–2.8) | ||
| In a relationship without sexually active | 4.2(3.2, 5.1) | 1698 (32.0) | 71 (43.3) | 1627 (31.6) | 1.9 (1.4–2.8) | ||
| Single with sexually active | 3.6(0.0, 10.4) | 28(0.5) | 1 (0.6) | 27 (0.5) | 1.7 (0.2–12.3) | ||
| Sexual active | |||||||
| Not sexually active | 2.9(2.5, 3.4) | 4522 (85.2) | 133 (81.1) | 4389 (85.3) | 9.4 | <.05 | 1.0 |
| Homosexual | 3.8(0.0, 7.9) | 80 (1.5) | 3 (1.8) | 77 (1.5) | 1.3 (0.4–4.1) | ||
| Heterosexual | 3.7(2.3, 5.1) | 683 (12.9) | 25 (15.2) | 658 (12.8) | 1.3 (0.8–1.9) | ||
| Bisexual | 13.6(0.0, 28.0) | 22 (0.4) | 3 (1.8) | 19 (0.4) | 5.2 (1.5–17.8) | ||
| Monthly expenses | |||||||
| <1000 RMB | 1.3(0.6, 2.0) | 1021 (19.2) | 13 (7.9) | 1008 (19.6) | 78.6 | <.001 | 1.0 |
| 1000–1999 RMB | 2.5(1.9, 3.0) | 3422 (64.5) | 84 (51.2) | 3338 (64.9) | 2.0 (1.1–3.5) | ||
| ≥2000 RMB | 7.8(6.0, 9.5) | 864 (16.3) | 67 (40.9) | 797 (15.5) | 6.5 (3.6–11.9) | ||
| Cervical cancer screen | |||||||
| No | 3.1 (2.6, 3.7) | 3771 (98.4) | 118 (88.1) | 3653 (98.8) | 99.9 | <.001 | 1.0 |
| Yes | 26.2 (14.9, 37.6) | 61 (1.6) | 16 (11.9) | 45 (1.2) | 11.0 (6.1–20.0) | ||
| Knowledge acquisition | |||||||
| No | 1.9 (1.1, 2.8) | 978 (35.7) | 19 (14.3) | 959 (36.8) | 27.9 | <.001 | 1.0 |
| Yes | 6.5 (5.3, 7.6) | 1762 (64.3) | 114 (85.7) | 1648 (63.2) | 3.5 (2.1–5.7) |
Demographic characteristics and behavior differences between vaccination and non-vaccination group
In the vaccination group, female, urban, undergraduates took a part of 81.7%, 73.8%, and 92.7%; students who were not sexually active, had cervical cancer screen and active knowledge acquisition took a part of 81.1%, 11.90%, and 85.7%. Chi-square tests showed that sex, hometown, marital status and sexually active, sexual active, monthly expenses, cervical cancer screening, and knowledge acquisition were significantly different between vaccination and non-vaccination groups, while education background difference was not significant (p value showed in Table 1). Univariable logistic regression models showed: female. Urban area, ever had cervical cancer screen, ever had knowledge acquisition behavior significantly differed between vaccination group and non-vaccination group, with OR and 95% CI were 1.8 (1.2–2.6), 3.00 (2.1–4.2), 11.0 (6.1–20.0), 3.5 (2.1–5.7) respectively for monthly expenses, compared with <1000 RMB level, OR and 95%CI of “1000–1999 RMB” and “≥2000 RMB” level were 2.0 (1.1–3.5) and 6.5 (3.6–11.9); for sexual active, compared with not sexually active, OR and 95%CI of bisexual level was 5.2 (1.5–17.8) for marital status and sexually active variable, compared with “single without sexually active” level, OR and 95%CI of “in a relationship with sexually active” and “in a relationship without sexually active” level were 1.8 (1.2–2.8) and 1.9 (1.4–2.8).
Knowledge of HPV and differences between vaccination and non-vaccination group
Even though 64.3% (1762/2740) of college students declared that they had actively educated themselves about HPV and the HPV vaccine, only 5.7% (300/5307), 14.2% (754/5307) and 6.6% (348/5307) of participants clearly and correctly understood the causality between HPV infection and cervical cancer, the HPV transmission route and HPV infection risk factors, respectively (Table 2). Chi-square test showed only knowledge about “HPV infection lead to cervical cancer,” “route of transmission,” “risk factors of infection” were significantly differed between vaccination and non-vaccination group (p value showed in Table 2). Univariable logistic regression was revealed: when compared with “Yes” level, OR and 95%CI of “No” and “Not sure” level were 0.6 (0.4–0.9) and 0.3 (0.2–0.5) for knowledge about “HPV infection lead to cervical cancer” variable; OR and 95%CI in “No” level was 0.6 (0.4–0.8) for knowledge about “route of transmission” variable, OR and 95%CI in “No” level was 6.3 (1.2–32.3) for knowledge about “risk factors of infection” varaiable.
Table 2.
Knowledge of the HPV among college students, 2018 (N = 5307)
| Vaccination status |
||||||
|---|---|---|---|---|---|---|
| Knowledge of the HPV | % (n/N*100%) | Vaccination group (164) | Non-vaccination group −5143 | χ2 | p | OR |
| Q1: Have you ever be heard of cervical cancer, anus cancer penile cancer and genital wart? | ||||||
| Yes | 4234 (79.8) | 141 (86.0) | 4093 (79.6) | 4.1 | .1 | 1.0 |
| NO | 655 (12.5) | 15 (9.2) | 650 (12.6) | 0.7 (0.4–1.1) | ||
| Not sure | 408 (7.7) | 8 (4.9) | 400 (7.8) | 0.6 (0.3–1.2) | ||
| Q2: Dose HPV infection lead to cervical cancer? | ||||||
| Yes | 300 (5.7) | 21 (12.8) | 279 (5.4) | 35.6 | <.001 | 1.0 |
| No | 1858 (35.0) | 79 (48.2) | 1779 (34.6) | 0.6 (0.4–0.9) | ||
| Not sure | 3149 (59.3) | 64 (39.0) | 3085 (60.0) | 0.3 (0.2–0.5) | ||
| Q3: How do you think about transmission way of HPV infection? (multiple choice) | ||||||
| Sexually | 5164 (97.3) | 160 (97.6) | 5004 (97.3) | - | - | - |
| Blood | 4356 (82.1) | 118 (72.0) | 4238 (82.4) | |||
| Airborne | 365 (6.9) | 13 (7.9) | 352 (6.8) | |||
| Contact | 302 (5.7) | 12 (7.3) | 290 (5.6) | |||
| Insect borne | 646 (12.2) | 19 (11.6) | 627 (12.2) | |||
| Humoral | 824 (15.5) | 18 (11.0) | 806 (15.7) | |||
| Q4: How do you think of the high-risk about the HPV infection? (multiple choice) | ||||||
| Unprotective sexual behavior | 4940 (93.1) | 155 (94.5) | 4785 (93.0) | - | - | - |
| Obesity | 125 (2.4) | 8 (4.9) | 117 (2.3) | |||
| Premature sexual behavior | 1888 (35.6) | 52 (31.7) | 1836 (35.7) | |||
| Contact with infected case | 1573 (29.6) | 56 (34.2) | 1517 (29.5) | |||
| On the sexually active age | 1240 (23.4) | 41 (25.0) | 1199 (23.3) | |||
| 50 years old or above | 213 (4.0) | 5 (3.1) | 208 (4.0) | |||
| Multiple sexual partners | 3461 (65.2) | 98 (40.2) | 3363 (34.6) | |||
| HPV carriers’ sexual partners | 4368 (82.3) | 136 (17.1) | 4232 (17.7) | |||
| Sexual precocity | 156 (2.9) | 6 (96.3) | 150 (97.1) | |||
| Low immunity | 2308 (43.5) | 62 (62.2) | 2246 (56.3) | |||
| Sexually transmitted diseases | 3479 (65.6) | 100 (39.0) | 3379 (34.3) | |||
| Q5:Understood the rout of transmission (based on Q3) | ||||||
| Yes | 754 (14.2) | 36 (22.0) | 718 (14.0) | 8.3 | <.05 | 1.0 |
| No | 4410 (83.1) | 124 (75.6) | 4286 (83.3) | 0.6 (0.4–0.8) | ||
| Not sure | 143 (2.7) | 4 (2.4) | 139 (2.7) | 0.6 (0.2–1.6) | ||
| Q6: Understood the risk factors of infection (based on Q4) | ||||||
| Yes | 348 (6.6) | 9 (5.5) | 339 (6.6) | 6.2 | <.05 | 1.0 |
| No | 14 (0.3) | 2 (1.2) | 12 (0.2) | 6.3 (1.2–32.3) | ||
| Not sure | 4945 (93.2) | 153 (93.3) | 4792 (93.2) | 1.2 (0.6–2.4) | ||
Q3 ”How do you think about transmission way of HPV infection? “ and Q4 ”How do you think of the high-risk about the HPV infection? “ are multiple choice questions. Answers were classified into “Yes”, “No”, “Not sure”. For Q3, answers only choose “Sexually” classified to “Yes”, never choose “Sexually” classified to “NO”, except for these, classified to “Not sure”. For Q4, only if ”Unprotective sexual”, “Premature sexual behavior”, “On the sexually active age”, “Multiple sexual partners”, “HPV carriers’ sexual”, “Low immunity”, “Sexually transmitted” items are completely selected, were classified to “Yes”. Never choose ”Unprotective sexual”, “Premature sexual behavior”, “On the sexually active age”, “Multiple sexual partners”, “HPV carriers’ sexual”, “Low immunity”, “Sexually transmitted” items are completely selected, were classified to “No”. Except for these, classified to “Not sure”.
Knowledge of the HPV vaccine and differences between vaccination and non-vaccination group
According to survey, 51.6%of the college students had heard about the HPV vaccine and 64.3% had a good understanding of the vaccination population. However, the proportion of college students who knew the HPV vaccine prevented cervical cancer was very low (2.5%). In addition, there were 47.5%, 47.0%, and 38.4% of college students who believed that the 2vHPV, 4vHPV and 9vHPV vaccine have different protective effects, protected pathogens, and price (Table 3). Importantly, the chi-square test showed knowledge about “heard of HPV vaccine,” “HPV vaccine protect effect” and “vaccination adaptive population” were significantly different between vaccination and non-vaccination groups (p value showed in Table 3). And uivariable logistic regression revealed: compared with “Yes” level, OR and 95%CI of “No” and “Not sure” level were 0.2 (0.1–0.3) and 0.4 (0.2–0.7) for knowledge about “heard of HPV vaccine” variable, and 0.3 (0.2–0.7) and 0.1 (0.0–0.2) for knowledge about “HPV vaccine protect effect” variable.
Table 3.
Knowledge of the HPV vaccine among college students, 2018 (N = 5307)
| Vaccination Status |
||||||
|---|---|---|---|---|---|---|
| Knowledge of the HPV | % (n/N*100%) | Vaccination group (164) | Non-vaccination group −5143 | χ2 | p | OR |
| Have you ever been heard of HPV vaccine? | ||||||
| 5307 | 164 | 5143 | ||||
| Yes | 2740 (51.6) | 133 (81.1) | 2607 (50.7) | 60.1 | <.001 | 1.0 |
| No | 1859 (35.0) | 18 (11.0) | 1841 (35.8) | 0.2 (0.1–0.3) | ||
| Not sure | 708 (13.3) | 13 (7.9) | 695 (13.5) | 0.4 (0.2–0.7) | ||
| HPV vaccine can100% protect from getting cervical cancer? | ||||||
| 2740 | 133 | 2607 | 29.9 | <.001 | ||
| Yes | 67 (2.5) | 10 (7.5) | 57 (2.2) | 1.0 | ||
| No | 2153 (78.6) | 116 (87.2) | 2037 (78.2) | 0.3 (0.2–0.7) | ||
| Not sure | 520 (19.0) | 7 (5.3) | 513 (19.7) | 0.1 (0.0–0.2) | ||
| How do you think of the adaptive population for HPV vaccine? | ||||||
| 2740 | 133 | 2607 | ||||
| Both | 1762 (64.3) | 112 (84.2) | 1650 (63.3) | 27.6 | <.001 | 1.0 |
| Only female | 973 (35.5) | 20 (15.0) | 953 (36.6) | 0.3 (0.2–0.5) | ||
| Only male | 5 (0.2) | 1 (0.8) | 4 (0.2) | 3.7 (0.4–33.2) | ||
| How do you think of the difference between the bivalent vaccine, tetravalent vaccine and nine valent vaccine? (multiple choice) | ||||||
| 2740 | 133 | 2607 | ||||
| Protective effect | 1300 (47.5) | 70 (52.6) | 1230 (47.2) | - | - | - |
| Protected pathogens | 1288 (47.0) | 91 (68.4) | 1197 (45.9) | |||
| Price | 1051 (38.4) | 53 (39.8) | 998 (383) | |||
| Adaptive population | 679 (24.8) | 30 (22.6) | 649 (24.9) | |||
| Adaptive age | 673 (24.6) | 26 (19.6) | 647 (24.8) | |||
| Inoculation process | 367 (13.4) | 18 (13.5) | 349 (13.4) | |||
| Duration of protection | 341 (12.5) | 11 (8.3) | 330 (12.7) | |||
| Side effect | 326 (11.9) | 11 (8.3) | 315 (12.1) | |||
| Manufacturer | 140 (5.1) | 11 (8.3) | 129 (5.0) | |||
“How do you think of the difference between the bivalent vaccine, tetravalent vaccine and nine valent vaccine?” is a multiple choice question, was not included in univariable logistic regression.
Vaccination attitude and the reasons
There were 55.6% and 50.2% of participant hesitant about vaccination and recommending vaccines to their families. 50.3% of college students, who are willing to vaccinate, preferred to choose 9vHPV vaccine. The most considering factors while selecting HPV vaccine were protective effect (92.05%), side effects (65.00%), and price (64.39%) (Table 4). Chi-square test showed “whether recommend HPV vaccine to relatives” was significantly differed between vaccination and non-vaccination group (p value showed in Table 4), and univariable logistic regression showed, compared with “Yes” level, OR and 95%CI of “No” and “Not sure” level were 0.2 (0.1–0.5) and 0.2 (0.1–0.3). However, there was no difference between the two groups in the selection of vaccine type. The reasons why college students decided to receive the HPV vaccine or not were analyzed; the results showed that the main reason college students received the vaccination was that the vaccine would protect them from HPV infection (97.04%), while a doctor’s recommendation had a limited effect on college students’ vaccination willingness (20.74%). Among vaccination rejection reasons, uncertainty about the long-term effects of the HPV vaccine was the largest barrier for vaccination (62.75%). More than half of the students chose not to be vaccinated because of the high prices (54.30%), they had not heard about the HPV vaccines (53.45%), they feared the side effects of the vaccines (51.99%) or they did not believe in the effectiveness of vaccines (51.84%) (Figure 1).
Table 4.
Attitude of the HPV vaccine vaccination among college students, 2018 (N = 5307)
| vaccination status |
||||||
|---|---|---|---|---|---|---|
| Knowledge of the HPV | % (n/N*100%) | Vaccination group (164) | Non-vaccination group −5143 | χ2 | p | OR |
| (n/N*100%) | group (164) | −5143 | χ2 | p | ||
| Are you considering of taking the HPV vaccine? | ||||||
| 5307 | 164 | 5143 | ||||
| Yes | 1320 (24.9) | 164(100.0) | 1156 (22.5) | 309.7 | <.001 | 1.0 |
| Not sure | 2949 (55.6) | - | 2949 (57.3) | 0.0 (0.0–0.0) | ||
| No | 1038 (19.7) | - | 1038 (20.2) | 0.0 (0.0–0.0) | ||
| What kind of HPV vaccine will you select? | ||||||
| 1313 | 164 | 1149 | 3.3 | .2 | ||
| Bivalent | 190 (14.5) | 27(16.3) | 163 (14.2) | 1.0 | ||
| Quadrivalent | 463 (35.3) | 40 (24.4) | 423 (36.8) | 0.6 (0.2–1.6) | ||
| Nine valent | 660 (50.3) | 97 (59.3) | 563 (49.0) | 1.2 (0.5–2.7) | ||
| Will you recommend your relatives to vaccinate? | ||||||
| 5307 | 164 | 5143 | 105.0 | <.001 | ||
| Yes | 2213 (41.7) | 132 (80.5) | 2081 (40.5) | 1 | ||
| No | 430 (8.1) | 6 (3.7) | 424 (8.2) | 0.2 (0.1–0.5) | ||
| Not sure | 2664 (50.2) | 26 (15.9) | 2638 (51.3) | 0.2 (0.1–0.3) | ||
| The considering factors while selecting HPV vaccine. (multiple choice) | ||||||
| 1320 | 164 | 1156 | ||||
| Protect effect | 1215 (92.1) | 149 (91.1) | 1066 (92.2) | - | - | - |
| Side effect | 858 (65.0) | 97 (59.3) | 761 (65.8) | |||
| Price | 850 (64.4) | 78(47.4) | 772 (66.8) | |||
| Doctor recommendation | 353 (26.7) | 41 (25.2) | 312 (27.0) | |||
| Vaccine manufacturer | 591 (44.8) | 74 (45.2) | 517 (44.7) | |||
Figure 1.
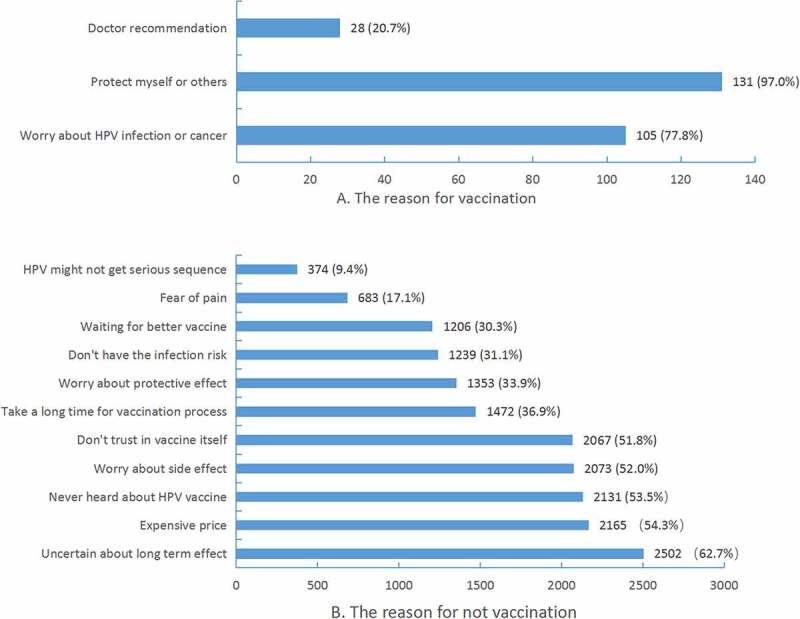
The reason decide to vaccinate or not
Multivariable analysis of HPV vaccination
Setting HPV vaccination behavior as the primary outcome, we conducted a multivariable analysis to determine which independent variables were significant in a logistic regression model. The results are shown in Table 5. For the demographic elements, urban hometown (OR = 2.1, 95% CI: 1.46–3.3) was a significant influencing factor. It is not surprising that students with higher monthly expenses are likely to be vaccinated against HPV (OR = 2.59, 95% CI: 1.85–3.62). Beside demographic factors, knowledge about vaccination population (OR = 3.1, 95% CI: 1.9–5.0), HPV infection risk factors (OR = 2.5, 95% CI: 1.1–5.7) and positive attitude about HPV vaccine effect (OR = 3.2, 95% CI: 2.0–5.2) were significant influencing factors. Interestingly, considering the sexually active dimensions, bisexual compared with not sexually active was a significant factor for HPV vaccination, while heterosexual and homosexual activity were not significant factors (Table 5).
Table 5.
Multivariable logistic regression analysis of the predictors for college students’ vaccination behavior
| Factors | B | S.E | Wald | df | P | |
95% CI |
|
|---|---|---|---|---|---|---|---|---|
| OR | lowwer | upper | ||||||
| Gender: female | 0.7 | 0.3 | 4.6 | 1.0 | <.05 | 2.0 | 1.1 | 3.7 |
| Hometown: urban area | 0.6 | 0.2 | 10.9 | 1.0 | <.05 | 2.1 | 1.4 | 3.3 |
| Monthly expenses | 1.0 | 0.2 | 30.8 | 1.0 | <.05 | 2.6 | 1.9 | 3.6 |
| Sexual behavior | 8.1 | 3.0 | <.05 | |||||
| Asexual behavior (reference) | - | - | - | - | - | 1.0 | - | - |
| Heterosexual behavior | −0.3 | 0.6 | 0.3 | 1.0 | .6 | 0.7 | 0.2 | 2.5 |
| Homosexual behavior | −0.4 | 0.3 | 2.2 | 1.0 | .1 | 0.7 | 0.4 | 1.1 |
| Bisexual behavior | 1.7 | 0.8 | 5.1 | 1.00 | <.05 | 5.4 | 1.3 | 23.3 |
| HPV vaccine do protected from cancer: NO or not sure | 1.6 | 0.4 | 16.6 | 1.0 | <.05 | 3.2 | 2.0 | 5.2 |
| Will recommendate relatives to vaccinate: yes | 1.6 | 0.3 | 29.9 | 1.0 | <.05 | 4.7 | 2.7 | 8.3 |
| Quite know of HPV vaccine adaptive population | 1.1 | 0.3 | 20.1 | 1.0 | <.05 | 3.1 | 1.9 | 5.0 |
| Know of HPV infection high risk factors | 0.9 | 0.4 | 4.6 | 1.0 | <.05 | 2.5 | 1.1 | 5.7 |
*The option of “Will you recommendate your relatives to vaccinate?” has been classed to “yes” (original “yes” option) and “not sure” (original “no” and “not sure” options). The response option of “adaptive population for HPV vaccine” classed to “yes” (original “both male and female” option) and “not sure” (original “only male” and “only female” options). Assign values (0 or 1) to each option of question “How do you think of the high-risk about the HPV infection?” and assembled into ordered categorical variable as followed: 1 = completely know, 2 = know some, 3 = don’t know. “Monthly expenses” was input into multivariable logistic regression model as continuous variable.
Discussion
From July 2017 to December 2018, 2vHPV, 4vHPV and 9vHPV vaccines were administered in mainland China gradually. To the best of our knowledge, this is the first survey on HPV vaccination behaviors, knowledge and willingness of college students after the HPV vaccine was released in mainland China. In this survey, we identified very low HPV vaccine coverage rates of 3.1% in college students in South China. What is more, records from the vaccination system, which recorded all age group’s vaccination history, showed that the overall three doses HPV vaccine coverage rate in Guangzhou city citizens, from October 2017 to March 2019 was extremely low of 0.7%, with 0.3% for 2vHPV vaccine, 0.5% for 4vHPV, and 0.1% for 9vHPV vaccine. The main results of this study revealed the situation of HPV vaccination among the college population in a developed area of China, which may help influence the strategy of HPV vaccination in China and provide effective educational guidance and interventions for improving the vaccination rate of the target population in the future.
Demographic characteristics were associated with HPV vaccine vaccination in this survey. The coverage rates in college students from urban areas and with high monthly expenses were significantly higher than those in college students from rural areas and with low monthly expenses, respectively, and students who had no sex but were in a relationship had a much higher vaccination rate than their counterparts. These results reflected three important social relative factors influencing HPV vaccine vaccination. Firstly, price may be the critical element in deciding whether to vaccinate in college population. In mainland China, the cost of HPV vaccination is between $300 and $750 for 3 doses, which is higher than minimum wage standard in Guangzhou. In many situations, direct costs for HPV vaccines are partially covered by private entities. However, in our survey, only 16.3% of the participants, college students, have a monthly consumption capacity of over 2000 RMB (approximately equal to $300). Therefore, a cost-effective strategy should be considered.19 A study in rural China estimated that vaccination-only and some combined strategies (vaccination and screening) would be cost-effective at a cost per vaccinated girl (CVG) of ∼$50.20 However, the willingness to pay for the vaccine is very limited; 7.6% of urban and 0.4% of rural women in China reported that they were willing to pay $15 for vaccination, and 60% of women reported that the acceptable price for the 3-dose HPV vaccination was < $7.21 This implies that affordability is still an issue. China is no longer considered a GAVI (The Global Alliance for Vaccines and Immunization) supported country and thus may not receive extensive financial assistance to maintain the vaccine supply. Secondly, the college students who are most likely to have sex for the first time are the people who can vaccinate HPV voluntarily. So, school-based programs targeting HPV vaccinations, such as educating students about HPV infection and prevention and scheduling vaccinations during annual school physical examinations, should be considered. Last but not least, 2.0% of male participants self-reported HPV vaccine vaccination, which implied they may vaccinate in Hong Kong, as HPV vaccine was allowed for both male and female, but only administered for females in mainland China. We call for the consideration of carrying out a phase III clinical trial of HPV vaccination for men in mainland China, and gradually lift the gender restriction on vaccination.
Furthermore, HPV vaccine vaccination depended on HPV and vaccine knowledge and vaccine effectiveness from a subjective point of view for the college population. Nearly 40% of the students were unaware of HPV infection and cervical cancer, only 14.2% and 6.6% of them understood the transmission route and risk factors for HPV infection, respectively. Only 2.5% of the students reported that the HPV vaccine could prevent cervical cancer. Consequently, over half of the students (55.6%) were hesitant to receive the HPV vaccination. Among the vaccination hesitation reasons chosen by over 50% of students, 80% were related to the effects of the vaccine, including the protective effect, long-term effects, and side effects. The relationship between insufficient knowledge about HPV vaccination and vaccination hesitancy has been reported in many European countries.22–32 Targeted health education programs have been proven to improve people’s knowledge and the population vaccination rate.33–35 The “low knowledge – vaccine hesitancy – low coverage” relation chain can be corrected by educational intervention. The results of this study verify the presence of insufficient educational interventions for cervical cancer and HPV vaccination and the unsatisfactory effect of interventions in China. Therefore, it is necessary to learn from successful experiences and develop a group education intervention program for students focused on 1) basic reproductive system anatomy and function, 2) common pathological features of genital organs, 3) HPV, 4) cancer caused by HPV and 5) HPV vaccination and 6) sexual behavior safety. During targeted health education, interactions are very important and require positive and clear answers and feedback instead of uncertain answers. Because sexual activity in most Chinese women does not begin until after 16 years of age36 and because of the high concentration of college students, this age is the most convenient age group for the promotion and popularization of HPV vaccines. So we suggested applied school-based vaccination in the college population is a proper strategy to protect the most vulnerable group. What is more, individualized doctor-patient education is significant in diminishing vaccine hesitancy, but this is still rare in China. Therefore, it is necessary to change the current situation of clinicians emphasizing treatment rather than prevention in China and establish close links between medical institutions and vaccination clinics. The following measures should be performed: 1) set up vaccination sites in hospitals to provide one-stop vaccination services and 2) carry out reservation services in gynecology clinics and health examination centers to improve accessibility to vaccines and promote individualized doctor-patient education interventions.
In 2018, the Director General of the WHO announced a call to action for the elimination of cervical cancer as a public health problem. In a modeling study, it was estimated that rapid vaccination scale-up to achieve 80–100% coverage globally by 2020 with a broad-spectrum HPV vaccine could prevent 6.7–7.7 million cases of HPV in this period, and more than half of these cases will be prevented after 2060.37 Therefore, rapid roll-out of the vaccine might be the only feasible way to narrow present inequalities in cervical cancer burden and prevention.5 Results from our survey revealed mainland China coverage just only similar to LMICs level, which was estimated by 2014, 33.6% of girls and women aged 10–20 years in high-income countries had received the full HPV vaccine series compared with 2.7% of girls in LMICs.5 In reality, HPV vaccine coverage in China was lower than those in many other countries and areas. Australia, the first country to establish an HPV vaccination program (in 2007), achieved more than 70% vaccine coverage in girls and boys aged 12 and 13 years.7 The US Center for Disease Control and Prevention (CDC) reported that in 2017, roughly half (49%) of adolescents had received the HPV vaccine to date, and 66% of the adolescents aged 13–17 years had received the first dose of the vaccine series.8 On average, the percentage of adolescents who started the HPV vaccine series increased by 5% each year over the course of five years (2013–2017).8 In 2008, a survey conducted on female university students in Hong Kong, China, showed that the uptake rate of the HPV vaccine was 9.7%. In 2012, the mothers in Hong Kong reported that 9.1% (7.0–11.6%) of their daughters were in the same age range (11–18 years) as the schoolgirls who had been vaccinated (p < .01) in 2015.38 The coverage gap is partly associated with the HPV vaccine not being included in the mainland China national vaccination program. Australia, the US, Germany, Hong Kong, and other countries or regions, through legislation, financial subsidies, and vaccination programs, have allowed appropriately aged women and girls to receive the HPV vaccine series for free or almost free.39 Although the introduction of vaccine programs in LMICs has been restricted by cost, a paucity of adolescent health platforms, cultural challenges, and difficulties in reaching the target population,40 the optimistic view is that the HPV vaccine market in mainland China has been increasing; therefore, whether to establish a national financial subsidy or include the HPV vaccine in the national vaccination program is worthy of consideration by the current government.
Limitations
This study had several limitations. First, the vaccination rate obtained in this survey does not represent the national or GBA regional vaccination rate but only Guangzhou city in GBA; however, it is a small-scale representation of the current vaccination situation in mainland China, especially in developed areas. Accordingly, coverage across the country should be lower than that reported here, as we found that the vaccination rate was higher in students from urban areas and with higher monthly incomes. Second, vaccination uptake was self-reported in this survey, thus does not represent a real uptake rate. Third, only college students (18–30 years) participated in the questionnaire survey. The HPV vaccine target age (9–45) in China can be divided into children, teenagers and adults, and vaccination behaviors and predictive factors differ in each age group. However, college students are most likely to influence the change in HPV vaccination rate in China in the next 10 years, whether they receive the vaccination for themselves or their child. Therefore, this study will help us to better understand vaccination status and willingness, and may further guide comprehensive prevention and control strategies for cervical cancer.
Conclusion
In conclusion, a low vaccination rate and vaccination hesitation are important obstacles in achieving the cervical cancer elimination goal established by the WHO in China. At present, the prevalence of HPV and incidence of cervical cancer in mainland China peaks in the 20- to 25-year-old and 45- to 50-year-old groups.41 Implementation of HPV immunization programs might be the feasible strategy to reduce the present cancer risk. What is more, as with the largest population in the world, China has the opportunity to contribute the most to the WHO cervical cancer elimination goal. The introduction of HPV vaccines in China is only the first step. In the future, the Chinese government needs to improve the vaccination rate among target populations and strengthen primary and secondary prevention measures in cervical cancer control and elimination.
Appendix A. Sample size and distribution
| University Name | Registered student’s number | Constituent ratio(%) | Sample size |
|---|---|---|---|
| Guangzhou Academy of Fine Arts | 5465 | 3.24% | 168 |
| Guangdong Pharmaceutical University | 9000 | 5.34% | 276 |
| Guangdong University of Technology | 29619 | 17.56% | 910 |
| South China University of Technology | 16860 | 10.00% | 518 |
| Guangzhou Medical University | 5290 | 3.14% | 162 |
| South China Normal University | 16400 | 9.72% | 504 |
| Sun Yat-sen University | 18450 | 10.94% | 567 |
| Guangdong University of Foreign Studies | 13380 | 7.93% | 411 |
| Guangzhou University | 29622 | 17.56% | 910 |
| Xinghai Conservatory of music | 3953 | 2.34% | 121 |
| Guangzhou University of Chinese Medicine | 13000 | 7.71% | 399 |
| Jinan University | 7618 | 4.52% | 233 |
| Total | 168657 | 5179 |
Sample size is calculated as 3884 by formula N=t2PQ/d2, d = 0.1 × P and assumed coverage of 9%, which is concluded from Hong Kong surveys. Taking a no response rate of 25%, the final sample size is 5179.
Funding Statement
The Project for Key Medicine Discipline Construction of Guangzhou Municipality (2013-2015-07). The Key Project of Medicine Discipline of Guangzhou (No. 2021-2023-11).
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A.. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.WHO . Cervical cancer. 2018. [accessed 2018 Apr 25]. http://www.who.int/cancer/prevention/diagnosis-screening/cervical-cancer/en/.
- 3.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F.. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359–86. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 4.Denny L. Nine-valent human papillomavirus vaccine: great science, but will it save lives? Lancet. 2017;390(10108):2123–24. doi: 10.1016/S0140-6736(17)32144-X. [DOI] [PubMed] [Google Scholar]
- 5.Bruni L, Diaz M, Barrionuevo-Rosas L, Herrero R, Bray F, Bosch FX, De Sanjosé S, Castellsagué X. Global estimates of human papillomavirus vaccination coverage by region and income level: a pooled analysis. Lancet Glob Health. 2016;4(7):e453–63. doi: 10.1016/S2214-109X(16)30099-7. [DOI] [PubMed] [Google Scholar]
- 6.WHO . Countries with HPV vaccine in the national immunization programme; and planned introductions in 2018. 2018. [accessed 2018 Oct 4]. https://www.who.int/immunization/monitoring_surveillance/data/en/.
- 7.Brotherton JM, Fridman M, May CL, Chappell G, Saville AM, Gertig DM. Early effect of the HPV vaccination programme on cervical abnormalities in Victoria, Australia: an ecological study. Lancet. 2011;377(9783):2085–92. doi: 10.1016/S0140-6736(11)60551-5. [DOI] [PubMed] [Google Scholar]
- 8.(CDC) CfDCaP . HPV vaccination coverage data. 2018. [accessed 2018 Aug 23]. https://www.cdc.gov/hpv/hcp/vacc-coverage/.
- 9.Crosbie EJ, Einstein MH, Franceschi S, Kitchener HC. Human papillomavirus and cervical cancer. Lancet. 2013;382(9895):889–99. doi: 10.1016/S0140-6736(13)60022-7. [DOI] [PubMed] [Google Scholar]
- 10.Huh WK, Joura EA, Giuliano AR, Iversen O-E, De Andrade RP, Ault KA, Bartholomew D, Cestero RM, Fedrizzi EN, Hirschberg AL, et al. Final efficacy, immunogenicity, and safety analyses of a nine-valent human papillomavirus vaccine in women aged 16–26 years: a randomised, double-blind trial. Lancet. 2017;390(10108):2143–59. doi: 10.1016/S0140-6736(17)31821-4. [DOI] [PubMed] [Google Scholar]
- 11.McGregor S, Saulo D, Brotherton JML, Liu B, Phillips S, Skinner SR, Luey M, Oliver L, Stewart M, Tabrizi SN, et al. Decline in prevalence of human papillomavirus infection following vaccination among Australian indigenous women, a population at higher risk of cervical cancer: the VIP-I study. Vaccine. 2018;36(29):4311–16. doi: 10.1016/j.vaccine.2018.05.104. [DOI] [PubMed] [Google Scholar]
- 12.Drolet M, Benard E, Boily MC, Ali H, Baandrup L, Bauer H, Beddows S, Brisson J, Brotherton JML, Cummings T, et al. Population-level impact and herd effects following human papillomavirus vaccination programmes: a systematic review and meta-analysis. Lancet Infect Dis. 2015;15(5):565–80. doi: 10.1016/S1473-3099(14)71073-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spinner C, Ding L, Bernstein DI, Brown DR, Franco EL, Covert C, Kahn JA. Human papillomavirus vaccine effectiveness and herd protection in young women. Pediatrics. 2019;143(2):e20181902. doi: 10.1542/peds.2018-1902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Denny L. Control of cancer of the cervix in low- and middle-income countries. Ann Surg Oncol. 2015;22(3):728–33. doi: 10.1245/s10434-014-4344-8. [DOI] [PubMed] [Google Scholar]
- 15.Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–32. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 16.Li K, Li Q, Song L, Wang D, Yin R. The distribution and prevalence of human papillomavirus in women in mainland China. Cancer. 2019; 125(7):1030–1037. doi: 10.1002/cncr.32003. [DOI] [PubMed] [Google Scholar]
- 17.Choi HC, Leung GM, Woo PP, Jit M, Wu JT. Acceptability and uptake of female adolescent HPV vaccination in Hong Kong: a survey of mothers and adolescents. Vaccine. 2013;32(1):78–84. doi: 10.1016/j.vaccine.2013.10.068. [DOI] [PubMed] [Google Scholar]
- 18.Li SL, Lau YL, Lam TH, Yip PS, Fan SY, Ip P. HPV vaccination in Hong Kong: uptake and reasons for non-vaccination amongst Chinese adolescent girls. Vaccine. 2013;31(49):5785–88. doi: 10.1016/j.vaccine.2013.10.027. [DOI] [PubMed] [Google Scholar]
- 19.Yin Y. HPV vaccination in China needs to be more cost-effective. Lancet. 2017;390(10104):1735–36. doi: 10.1016/S0140-6736(17)32606-5. [DOI] [PubMed] [Google Scholar]
- 20.Canfell K, Shi JF, Lew JB, Walker R, Zhao F-H, Simonella L, Chen J-F, Legood R, Smith MA, Nickson C, et al. Prevention of cervical cancer in rural China: evaluation of HPV vaccination and primary HPV screening strategies. Vaccine. 2011;29(13):2487–94. doi: 10.1016/j.vaccine.2010.12.085. [DOI] [PubMed] [Google Scholar]
- 21.Li J, Li LK, Ma JF, Wei L-H, Niyazi M, Li C-Q, Xu A-D, Wang J-B, Liang H, Belinson J, et al. Knowledge and attitudes about human papillomavirus (HPV) and HPV vaccines among women living in metropolitan and rural regions of China. Vaccine. 2009;27(8):1210–15. doi: 10.1016/j.vaccine.2008.12.020. [DOI] [PubMed] [Google Scholar]
- 22.Lasset C, Kalecinski J, Regnier V, Barone G, Leocmach Y, Vanhems P, Chauvin F, Lutringer-Magnin D. Practices and opinions regarding HPV vaccination among French general practitioners: evaluation through two cross-sectional studies in 2007 and 2010. Int J Public Health. 2014;59(3):519–28. doi: 10.1007/s00038-014-0555-9. [DOI] [PubMed] [Google Scholar]
- 23.Brabin L, Roberts SA, Stretch R, Baxter D, Chambers G, Kitchener H, McCann R. Uptake of first two doses of human papillomavirus vaccine by adolescent schoolgirls in Manchester: prospective cohort study. BMJ. 2008;336(7652):1056–58. doi: 10.1136/bmj.39541.534109.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Forster AS, Marlow LA, Wardle J, Stephenson J, Waller J. Understanding adolescents’ intentions to have the HPV vaccine. Vaccine. 2010;28(7):1673–76. doi: 10.1016/j.vaccine.2009.11.082. [DOI] [PubMed] [Google Scholar]
- 25.Forster AS, Waller J, Bowyer HL, Marlow LA. Girls’ explanations for being unvaccinated or under vaccinated against human papillomavirus: a content analysis of survey responses. BMC Public Health. 2015;15:1278. doi: 10.1186/s12889-015-2657-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gefenaite G, Smit M, Nijman HW, Tami A, Drijfhout IH, Pascal A, Postma MJ, Wolters BA, Van Delden JJM, Wilschut JC, et al. Comparatively low attendance during human papillomavirus catch-up vaccination among teenage girls in the Netherlands: insights from a behavioral survey among parents. BMC Public Health. 2012;12(1):498. doi: 10.1186/1471-2458-12-498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Giambi C, D’Ancona F, Del Manso M, De Mei B, Giovannelli I, Cattaneo C, Possenti V, Declich S. Exploring reasons for non-vaccination against human papillomavirus in Italy. BMC Infect Dis. 2014;14(1):545. doi: 10.1186/s12879-014-0545-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hofman R, van Empelen P, Richardus JH, De Kok IMCM, De Koning HJ, Van Ballegooijen M, Korfage IJ. Predictors of HPV vaccination uptake: a longitudinal study among parents. Health Educ Res. 2014;29(1):83–96. doi: 10.1093/her/cyt092. [DOI] [PubMed] [Google Scholar]
- 29.Lee Mortensen G, Adam M, Idtaleb L. Parental attitudes towards male human papillomavirus vaccination: a pan-European cross-sectional survey. BMC Public Health. 2015;15:624. doi: 10.1186/s12889-015-1863-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maier C, Maier T, Neagu CE, Vladareanu R. Romanian adolescents’ knowledge and attitudes towards human papillomavirus infection and prophylactic vaccination. Eur J Obstet Gynecol Reprod Biol. 2015;195:77–82. doi: 10.1016/j.ejogrb.2015.09.029. [DOI] [PubMed] [Google Scholar]
- 31.Mammas IN, Theodoridou M, Koutsaftiki C, Bertsias G, Sourvinos G, Spandidos DA. Vaccination against human papillomavirus in relation to financial crisis: the “evaluation and education of Greek female adolescents on human papillomaviruses’ prevention strategies” ELEFTHERIA study. J Pediatr Adolesc Gynecol. 2016;29(4):362–66. doi: 10.1016/j.jpag.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 32.Remschmidt C, Walter D, Schmich P, Wetzstein M, Delere Y, Wichmann O. Knowledge, attitude, and uptake related to human papillomavirus vaccination among young women in Germany recruited via a social media site. Hum Vaccines Immunother. 2014;10(9):2527–35. doi: 10.4161/21645515.2014.970920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Byrd TL, Wilson KM, Smith JL, Coronado G, Vernon SW, Fernandez-Esquer ME, Thompson B, Ortiz M, Lairson D, Fernandez ME, et al. AMIGAS: a multicity, multicomponent cervical cancer prevention trial among Mexican American women. Cancer. 2013;119(7):1365–72. doi: 10.1002/cncr.27926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Staples JN, Wong MS, Rimel BJ. An educational intervention to improve human papilloma virus (HPV) and cervical cancer knowledge among African American college students. Gynecol Oncol. 2018;149(1):101–05. doi: 10.1016/j.ygyno.2017.10.015. [DOI] [PubMed] [Google Scholar]
- 35.Maxwell AE, Wang JH, Young L, Crespi CM, Mistry R, Sudan M, Bastani R. Pilot test of a peer-led small-group video intervention to promote mammography screening among Chinese American immigrants. Health Promot Pract. 2011;12(6):887–99. doi: 10.1177/1524839909355550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhao FH, Xu LN, Hong Y, Niyazi M, Gao XH, Ju LR, Zhang LQ, Feng XX, Duan XZ, Qiao YL. A multi-center survey on age of sexual debut in Chinese women: suggestions for optimal age of HPV vaccination in China. Cancer Epidemiol. 2012; 36(4):384–90. doi: 10.1016/j.canep.2012.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Simms KT, Steinberg J, Caruana M, Smith MA, Lew J-B, Soerjomataram I, Castle PE, Bray F, Canfell K. Impact of scaled up human papillomavirus vaccination and cervical screening and the potential for global elimination of cervical cancer in 181 countries, 2020–99: a modelling study. Lancet Oncol. 2019;20:394–407. doi: 10.1016/S1470-2045(18)30836-2. [DOI] [PubMed] [Google Scholar]
- 38.Yuen WWY, Lee A, Chan PKS, Tran L, Sayko E. Uptake of human papillomavirus (HPV) vaccination in Hong Kong: facilitators and barriers among adolescent girls and their parents. PLoS One. 2018;13(3):e0194159. doi: 10.1371/journal.pone.0194159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.(CDC) CfDCaP . Vaccines for children program (VFC). [accessed2018May25]. https://www.cdc.gov/vaccines/programs/vfc/about/index.html.
- 40.Cohen PA, Jhingran A, Oaknin A, Denny L. Cervical cancer. Lancet. 2019;393(10167):169–82. doi: 10.1016/S0140-6736(18)32470-X. [DOI] [PubMed] [Google Scholar]
- 41.Zhou HL, Zhang W, Zhang CJ, Wang S-M, Duan Y-C, Wang J-X, Yang H, Wang X-Y. Prevalence and distribution of human papillomavirus genotypes in Chinese women between 1991 and 2016: a systematic review. J Infect. 2018;76(6):522–28. doi: 10.1016/j.jinf.2018.02.008. [DOI] [PubMed] [Google Scholar]


