A 17-year-old boy was referred to the ophthalmology service at St Thomas' Hospital (London, UK) with bilateral red eyes, bilateral eye pain independent of eye movement that disturbed his sleep, photophobia, and mild, subjective blurring of vision. He had become infected with SARS-CoV-2 5 weeks before referral and had been diagnosed with paediatric inflammatory multisystem syndrome temporally associated with COVID-19 (PIMS-TS) and associated myocarditis.
His Snellen visual acuity was excellent: 6/4 unaided in both eyes. He had bilateral, diffuse episcleral and deep scleral injection (vasodilatation with hyperaemia) that did not blanch with topical 10% phenylephrine; a bilateral anterior chamber grading of 2+ (16–25 cells in a 1 mm × 1 mm field); no vitritis, retinitis, or vasculitis; and an otherwise unremarkable fundal examination (figure A, B ). A B-scan ultrasound did not show any posterior scleritis. He was diagnosed with bilateral, diffuse, anterior non-necrotising scleritis with anterior uveitis.
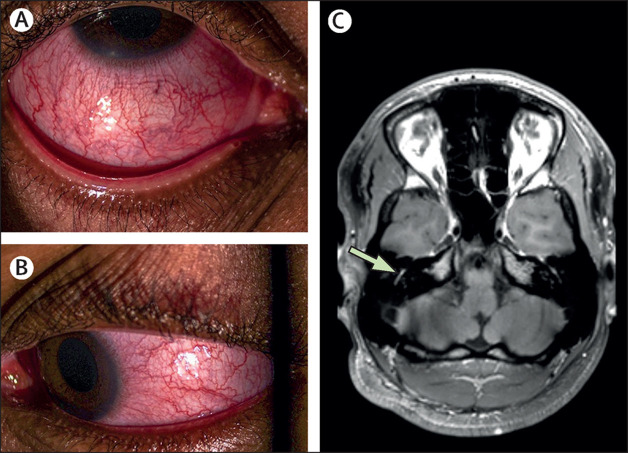
Figure.
Eye photographs and MRI image
Colour photographs taken at presentation to the ophthalmology service showing the violaceous hue of diffuse anterior non-necrotising scleritis in the right eye (A) and left eye (B). (C) T1-weighted MRI image showing asymmetrical, mildly increased post-gadolinium contrast enhancement of the tympanic portion of the right facial nerve (arrow).
Before his ophthalmology referral, the patient had been treated for PIMS-TS with a 3-day course of intravenous methylprednisolone (950 mg/day). He subsequently developed fever, had a rising C-reactive protein concentration 1 week post-admission (from 47 mg/L to 94 mg/L over the course of 1 day), and received 800 mg of intravenous tocilizumab on the day of his referral. After attending the ophthalmology service, he started a course of oral prednisolone (starting dose 40 mg/day for 17 days), guttae 0·1% dexamethasone (eye drops to both eyes at an initial schedule of once every 2 h for 3 days), and a 1-week course of guttae 1% cyclopentolate (eye drops to both eyes twice daily). Treatment (prednisolone and guttae 0·1% dexamethasone) was tapered over a 6-week period. 7 days after ophthalmology referral and review, the patient's symptoms had resolved and he had normal vision and no ongoing inflammation.
10 days after referral, the patient presented with a right facial (VIIth) nerve palsy and his prescribed regimen of prednisolone (40 mg/day, before tapering) was not changed. Neuroimaging showed mild inflammation of the right tympanic facial nerve (figure 1C). Prompt resolution of facial weakness occurred within 4 weeks.
It is imperative not to misdiagnose the potentially sight-threatening conditions of scleritis and uveitis as conjunctivitis, which is the commonly known ophthalmic association in PIMS-TS.
Declaration of interests
We declare no competing interests.
Contributors
MI, MC, and TB contributed to manuscript conceptualisation. All authors contributed to the analysis of clinical data and the preparation of the figure, and reviewed the final draft for approval. Informed consent was obtained from the patient for publication.