Abstract
Objectives
During the COVID-19 pandemic, ethnic minorities have been more susceptible to infection and demonstrated poorer outcomes. This study describes COVID-19 morbidity and mortality by ethnic group, represented by Arab and Jewish localities in Israel, during the different waves of the outbreak and addresses sociocultural aspects of the pandemic.
Study design
A retrospective national archive study was conducted in Israel.
Methods
Data were obtained from the Ministry of Health's database, including daily information on Arab, Jewish or mixed localities, from February 2020 to February 2021.
Results
During the first wave of the pandemic, the incidence of COVID-19 in Arab compared with Jewish localities was 67% lower and mortality was 85% lower, in addition to lower rates of severe disease requiring hospitalisation. During the second and third waves, these trends reversed, with the proportion of positive tests, incidence and mortality in Arab localities reaching and then surpassing rates in Jewish localities. By September 2020, COVID-19 mortality was twice as high in Arab compared with Jewish localities.
Conclusions
After low morbidity during the first wave of the COVID-19 pandemic, a surge in infections occurred in the Arab population during subsequent waves, to match and surpass the high incidence seen in the Jewish population. This unique pattern highlights the changing experiences of a minority group as the pandemic progressed and demonstrates how COVID-19 exacerbates existing disparities.
Keywords: Arab, COVID-19, Ethnic, Minority, Morbidity
Introduction
Higher incidence and severity of COVID-19 infections have been reported among racial and ethnic minorities in the UK and US as early as April 2020,1 4 months after diagnosis of the first case in China. It soon became clear that ‘COVID-19 does not affect all population groups equally’.2 Both morbidity and mortality rates in the UK were shown to be higher in Blacks and Asians than in White ethnic groups. Analysis of data on 47 million Americans showed that by 20 July 2020, hospitalisation rates in Black and Hispanic patients were 3.3 and 4.1 times higher, respectively, than in White patients. In addition, death rates were 2.4 times higher in Black or Hispanic patients than in White patients.3 This consistent pattern of racial/ethnic disparities was suggested to be due to both a higher burden of underlying disease, combined with more crowded living conditions.4
Social behaviours (such as intergenerational interactions), health behaviours (e.g. poor nutrition and lack of physical activity, contributing to obesity) and health status (e.g. comorbidities such as diabetes and hypertension) interact to increase the risk of COVID-19 morbidity and mortality among ethnic minorities.5 Crowded living, working in essential industries during the pandemic and the inability to work from home, as well as higher use of public transportation to travel to work, result in higher vulnerability to the infection among minority populations.6 Some ethnic minority populations are also characterised by lower health literacy7 and less utilisation of digital communication platforms for health-related purposes.8
In Israel, the Arab ethnic minority comprises 21% of the total population of 9.136 million and is characterised by younger age and more crowded living conditions than the majority Jewish population. The Arab population has average lower household income, higher unemployment rates or employment in unskilled or low skilled professions and experiences economic and educational disadvantages. The Arab population reports poorer self-rated health compared with the Jewish population.9 Structural socio-economic factors and living environments were shown to contribute substantially more than individual health behaviours to ethnic inequalities in perceived health in this population.10 Of particular relevance is the greater incidence of comorbidities that have been associated with poorer outcomes of COVID-19 infection, including diabetes, hypertension and cardiovascular disease, and a higher prevalence of smoking among the male population, related to higher incidence of chronic lung disease.9
The first community-acquired COVID-19 infection was diagnosed in Israel on 27 February 2020. By February 2021, Israel had experienced three waves or peaks of new COVID-19 infection cases, the first in March–April 2020, the second peaking in September 2020 and the third reaching the highest incidence rate in January 2021. The latter waves were characterised by considerably higher volumes of infections, with up to 7000 (760 per million population) new daily cases in September 2020 and 10,000 (1090 per million) in January 2021. Over the course of 1 year, Israel counted 820,000 cases (9% of the total population) and 6000 deaths.
The number of COVID-19 cases rose dramatically in the overall Israeli population, as well as in all sectors of Israeli society, including the Arab population and the ultra-Orthodox Jewish population; however, the most dramatic change between the first and subsequent waves was seen in the Arab population. Overall high morbidity contributed to overload on general hospitals all around the country and especially in the Northern region, where the largest proportion of Arab citizens live.11 Concerns about the limited capacity of hospitals and burnout of medical staff were among the reasons to impose a national lockdown in the latter half of September 2020.
This study aimed to examine trends in COVID-19 morbidity and mortality by population group, defined by locality, and explore possible explanations for this change in the pattern of infections between the first and subsequent COVID-19 waves.
Methods
Data sources
A retrospective archive study was conducted in Israel from 27 February 2020 (the patient zero case) to 28 February 2021 (12 full consecutive months).
Data were obtained from the Ministry of Health (MOH) of Israel's open COVID-19 database (https://data.gov.il/dataset/covid-19), which includes information on 1270 localities (in Israel, the term locality refers to distinct communities that range in size from a very small settlement to the largest city with more than 900,000 inhabitants) and is updated daily.
This study presents data on the following: the rate of COVID-19 diagnostic tests (real-time quantitative reverse-transcriptase polymerase chain reaction assay) performed; incidence rate of COVID-19 (number of positive polymerase chain reaction [PCR] tests in each of the study months, per 100 population); positivity rate of tests (i.e. percentage of all tests that were positive); numbers and rates of hospitalised, PCR-confirmed patients with COVID-19; and the number of deaths from COVID-19 per 100,000 population. Patients who were hospitalised with COVID-19 were classified (according to the World Health Organization classification) as having mild, moderate or severe disease. The latter classification includes patients who are intubated and mechanically ventilated.12 Our analysis focuses on this category of severely ill (including intubated) patients.
The study protocol was approved by the Institutional Ethics Committee of Tel Aviv University (approval number 0002952-1).
Data analyses
Variables included MOH data on tests performed, confirmed COVID-19 cases (referring to positive PCR tests), disease severity and deaths due to COVID-19, which were examined by locality, as a proxy for ethnic group. These data were available by locality and were categorised into (1) Jewish localities; (2) Arab localities; and (3) mixed localities. Because localities are predominantly separated by ethnic groups in Israel, this is an accepted proxy measure. Mixed localities are defined as areas with residents of diverse ethnicity or religion, with the minority group comprising more than 10% of the population.13
Population size was obtained from the Central Bureau of Statistics database.11 Of 8,939,993 citizens (97.9% of the total population) for whom residence is specified, 5,610,025 (62.7%) of them reside in Jewish localities, 1,398,547 (15.6%) reside in Arab localities and 1,931,421 reside in mixed localities (21.6%).11 Within mixed towns, homogenous ethnic residential areas were not separately assessed.
The proportion of positive tests was evaluated as the number of cases at the end of the relevant months, divided by the number of tests, for the relevant population group. Morbidity rate of incident cases in the population was the number of positive cases divided by the size of the relevant population group for the relevant month. Status of hospitalised patients with COVID-19 was reflected as the rate of severely ill and intubated patients of all hospitalised patients and was evaluated on the last day of the relevant month. Mortality rate per population group was calculated per 100,000 population.
Results
Overall, rates of testing were 11.8 and 7.6 tests per 100 population in Jewish and Arab localities, respectively (Appendix 1 in the supplementary material). Fig. 1 presents the proportion of positive tests out of all tests performed in each month during the study period, by population group. During the first wave of infection, the proportion of positive tests was considerably lower in Arab localities than in Jewish and mixed localities (0.03, 0.09 and 0.10, respectively, in April 2020). In the second wave (starting in the second half of June 2020 and continuing into September 2020), the pattern of infection was reversed, with positivity rates in Arab localities surpassing those in Jewish localities. Mixed cities demonstrated a pattern similar to Jewish localities in the first wave and a pattern of intermediate values between Jewish and Arab localities in the second wave. During the third wave, the proportion of positive tests continued to be the highest in Arab localities (0.12 compared with 0.07 in Jewish localities).
Fig. 1.
Positivity rate of COVID-19 tests (percentage of tests with confirmed infection), by population group and month, February 2020–February 2021.
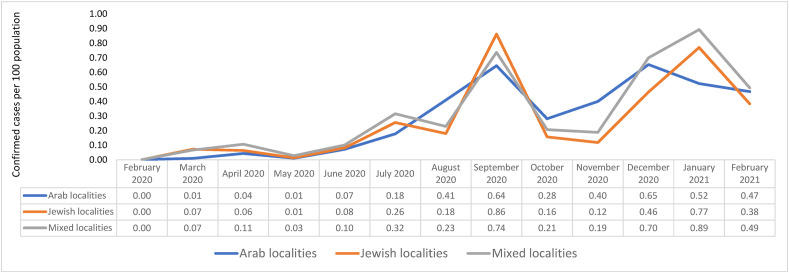
Fig. 2 presents the incidence of COVID-19 (i.e. the number of confirmed cases in each of the study months, per 100 population). In the first wave (April 2020), the incidence of COVID-19 in Arab localities was 67% of that in Jewish localities.
Fig. 2.
Incidence of COVID-19, expressed as monthly number of confirmed cases, by population group, February 2020–February 2021.
This trend reversed in mid-July, with Arab localities showing a 56% increase in August 2020. Between November and December 2020, the confirmed case rate was the highest in Arab localities, before dropping in January–February 2021, with the decrease preceding reductions in other groups. Mixed localities demonstrated trends similar to Jewish localities.
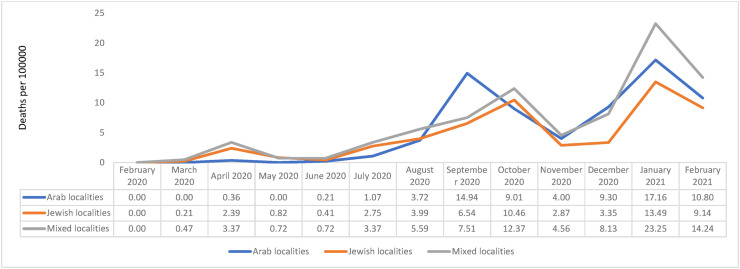
Overall mortality differed by population group at 5.4 per 1000 population in Arab localities, 4.3 per 1000 in Jewish localities and 6.5 per 1000 in mixed localities. Fig. 3 presents mortality figures, with Arab localities demonstrating very low rates in April 2020, which were only 15% of the rates seen in Jewish localities. The initial advantage seen in the Arab population gradually diminished to almost identical rates (0.97 of the Jewish rates) in August 2020. By September, mortality was twice as high in Arab localities compared with Jewish localities. In subsequent months (except October), mortality in Arab localities was slightly higher or similar compared with Jewish and mixed localities.
Fig. 3.
Mortality rate (the number of deaths per 100,000) by population group and month, February 2020–February 2021.
The overall hospitalisation rate was the highest in the mixed localities (1.85 per 1000 population), lowest in Jewish localities (1.09/1000) and in the middle for Arab localities (1.35/1000). Table 1 presents the numbers and rates of hospitalised patients with COVID-19 who were classified as severely ill or intubated. In March and April 2020 together, only 5 Arab patients compared with 140 Jewish patients with severe disease were hospitalised in acute care wards. In April 2020, the rate of severely ill patients from Jewish localities was 12.7 per million population compared with 2.1 per million from Arab localities. These trends changed in the second wave, with the proportion of hospitalised patients who had severe disease and the proportion of those intubated equalising in July 2020 (31.2 per million in Jewish localities and 30.0 per million Arab localities) and subsequently rising to much higher rates in Arab localities.
Table 1.
Severely ill and intubated patients by population group (number and rate per million population) and month, February 2020–February 2021.
| Year | Month | Severe disease [n (rate per million population)] |
Intubated patientsa [n (rate per million population)] |
||||
|---|---|---|---|---|---|---|---|
| Jewish | Arab | Mixed | Jewish | Arab | Mixed | ||
| 2020 | February | 0 | 0 | 0 | 0 | 0 | 0 |
| (0) | (0.0) | (0.0) | (0.00) | (0.00) | (0.00) | ||
| March | 69 | 2 | 26 | 50 | 2 | 12 | |
| (12.3) | (1.4) | (13.5) | (8.9) | (1.4) | (6.2) | ||
| April | 71 | 3 | 35 | 59 | 3 | 25 | |
| (12.7) | (2.1) | (18.1) | (10.5) | (2.1) | (12.9) | ||
| May | 21 | 1 | 11 | 18 | 1 | 10 | |
| (3.7) | (0.7) | (5.7) | (3.2) | (0.7) | (5.2) | ||
| June | 30 | 2 | 22 | 12 | 0 | 10 | |
| (5.3) | (1.4) | (11.4) | (2.1) | (0.00) | (5.2) | ||
| July | 175 | 42 | 94 | 53 | 12 | 26 | |
| (31.2) | (30.0) | (48.7) | (9.4) | (8.5) | (13.5) | ||
| August | 131 | 68 | 113 | 51 | 39 | 29 | |
| (23.4) | (48.6) | (58.5) | (9.1) | (27.9) | (15.0) | ||
| September | 330 | 105 | 127 | 91 | 59 | 46 | |
| (58.8) | (75.1) | (65.7) | (16.2) | (42.2) | (23.8) | ||
| October | 114 | 51 | 59 | 104 | 29 | 36 | |
| (20.3) | (36.5) | (30.5) | (18.5) | (20.7) | (18.6) | ||
| November | 50 | 62 | 50 | 43 | 21 | 22 | |
| (8.9) | (44.3) | (25.9) | (7.7) | (15.0) | (11.4) | ||
| December | 205 | 133 | 142 | 61 | 48 | 53 | |
| (36.5) | (95.1) | (73.5) | (10.9) | (34.3) | (27.4) | ||
| 2021 | January | 423 | 123 | 193 | 142 | 67 | 86 |
| (75.4) | (87.9) | (99.9) | (25.3) | (47.9) | (44.5) | ||
| February | 224 | 100 | 122 | 113 | 48 | 63 | |
| (39.9) | (72.2) | (63.2) | (20.1) | (34.3) | (32.6) | ||
Number of severe cases includes intubated patients.
By December 2020, earlier trends had reversed with a rate of 36.5 per million with severe disease in Jewish localities compared with 95.1 per million in Arab localities.
Discussion
The first 4 months of Israel's COVID-19 outbreak witnessed a promising outlook for the Arab ethnic minority,14 with infection rates 3 times lower and mortality rates 10 times lower than those of the Jewish population, despite their low soci-oeconomic position, high overall comorbidities and health inequalities. This slower rise in test positivity cannot be explained by a delayed uptake of testing among the Arab population. Other possible explanations include the viral spread initially ‘imported’ via travellers returning from abroad, which did not reach most of the Arab towns and villages during March and April 2020, and high compliance with public health measures during the first wave within the Arab minority. In contrast, the ultra-Orthodox Jewish population (also a low socio-economic status [SES] minority group) demonstrated high rates of infection.
However, the second and third waves saw a dramatic change, with a sudden increase in both morbidity and mortality in the Arab population, rising to equal and then surpassing rates seen in the Jewish population. These steeply rising trends, particularly in the Northern region, were among the factors that contributed to the healthcare system reaching its capacity and suggest that the government did not sufficiently equip this minority group with the required resources to deal with the pandemic.
A similar pattern has been seen in other countries, with initially lower incidence in low SES groups at the start of the pandemic, followed by a sharp rise, for example, in Spain,15 which was possibly due to lower testing in these areas during the initial stages and thus less detected cases. Similarly, in the US, initially rates were higher in high SES areas, but this reversed once public health measures were implemented because high SES groups were more able to comply.16 In Israel, where minority groups are characterised by lower SES, not all groups showed the same pattern of infection. For example, high COVID-19 morbidity was evident in the ultra-Orthodox population throughout the pandemic, while within the Arab population, the pattern of incidence changed between the first and subsequent waves.17 , 18
The high proportion of severely ill and intubated patients in the Arab population, despite the relatively younger mean age, is likely due to an overrepresentation of comorbidities in this group, including more prevalent obesity, diabetes, hypertension and smoking.19 This higher disease burden is related to greater economic disadvantage and deprivation. These data from the second and third waves mirror reports from other countries where ethnic minorities have suffered disproportionately from COVID-19, for example, in the US, where Black patients have been overrepresented in those hospitalised compared with White patients.20 In the UK, a case control study reported a higher rate of hospital admissions among Blacks compared with White inner city residents but not a higher mortality rate. The authors suggested that a higher prevalence of comorbidities may contribute to more frequent progression to severe disease but that other ethnic factors, beyond comorbidity and socio-economic conditions, are likely to be involved.21 The Open Safely study, which included 17 million NHS patients and 5683 COVID-19 deaths, found that all non-White ethnic minority groups had higher mortality risk and that risk increased with deprivation.22
Several factors may have contributed to the change in the COVID-19 landscape among the Arab minority between the first, second and third waves in Israel.
Long-standing socio-economic inequalities
Most of the Arab population lives in ethnically homogenous localities, with less developed physical infrastructures, separate educational systems, lower academic achievements, higher unemployment and less skilled and lower income jobs. In addition, crowded living, frequently intergenerational, may accelerate COVID-19 infection of the older, more vulnerable population, despite an overall younger mean age.9 Limited resources coupled with lower health literacy are likely to contribute to the increased vulnerability of this population in the pandemic.23 , 24 The first wave of the pandemic was characterised by fear of the unknown and high compliance with mitigation measures. During the second wave, with a far higher incidence of new cases, fear of losing one's job and being unable to provide for one's family might have contributed to lower compliance with physical distancing measures (e.g. continued working, refusal to close businesses), resulting in high infection rates. This situation may be more evident in the Arab population, where a high percentage of men are employed in manual jobs (45% in construction, manufacturing or agriculture), which does not allow work from home conditions.25
It is likely that COVID-19 hits the hardest and spreads the fastest where inequalities have weakened the social fabric and capital and where the economic effects of lockdown measures may be the most severe.26 A recently published comment suggests that COVID-19 is not a pandemic but rather a ‘syndemic’, involving biological and social interactions, where the infection meets non-communicable diseases, which cluster in the weakest segments of the population.27
Lack of trust
The Arab minority in Israel differs culturally and religiously from the Jewish majority and demonstrates poorer health outcomes compared with the Jewish population. The Statnet Poll (2014) showed a genuine feeling of discrimination among the Arab community: 39% of respondents believe there is discrimination in Israeli institutions and 53% believe there is only partial equality.28 Trust in governmental institutions is lower than for the Jewish population,29 although trust in the health system was found to be higher among Arab compared with Jewish respondents in a survey.30 The COVID-19 crisis was managed by collaboration between central government, local authorities and the MOH. An already low level of confidence in the authorities may have been exacerbated by swift changes in policy. Low trust in the system probably contributed to low adherence to COVID-19 restrictions.
Recommendations for the success of messages to help reduce COVID-19 transmission by a group of behavioural scientists in the UK included ‘clear and specific guidance’ as a key tenet,31 alongside ‘stand together’ messages that build on group identity and solidarity, which is particularly important for reaching marginalised groups. Growing debates and fractures in Israeli society eroded its resistance.32 , 33 Efforts were made to bring the voice of Arab society as early as the first COVID-19 wave to the national COVID-19 situation room. The MOH recruited marketing experts who work with different Arab communities (Bedouin, East Jerusalem and the Northern 15 region) to improve the cultural adaptation of the public health messages.
Sociocultural and religious characteristics
Religious holidays and wedding celebrations in both the Jewish and Arab populations were associated with rises in COVID-19 morbidity. Within the Arab population, early in the pandemic, during the month of Ramadan, religious leaders conveyed messages to the public to refrain from large gatherings of family and friends and all mosques were closed with no exceptions. The Arab community refrained from large gatherings during Ramadan and also seemed to comply with other public health measures of physical distancing.9 At the beginning of August, another important holiday in the Muslim calendar (Eid al-Adha) occurred, where families typically gather in large numbers to celebrate. In contrast to the first wave when religious leaders united in their message to stay home, during Eid al-Adha, the mosques remained open. The Arab religious and political leadership, witnessing that many Jewish gathering places, such as synagogues, were left open while they ordered their community to close all mosques during Ramadan, changed their attitude to a more pragmatic approach.
July and August are typically the most popular time for weddings in the Arab community, where wedding gatherings, which take place over several days, regularly include 1000 guests.34 Although official guidelines did not allow such large gatherings, restrictions were not sufficiently enforced and many weddings were allowed to take place in private homes (after wedding halls were closed), with local authorities turning a blind eye. Many infections occurred at weddings due to lack of physical distancing and non-compliance with wearing face masks. A similar disregard for the rules was seen in some ultra-Orthodox Jewish communities where large weddings and funerals were held, leading to rises in COVID-19 morbidity in this population.
Maintenance of health behaviours
It is well known that short-term behaviour changes are easy to make but hard to maintain in the long term.35 , 36 This applies to weight loss, smoking cessation and uptake of physical activity and can equally apply to the changes required during the pandemic, including physical distancing, hygiene and mask wearing. Health-promoting behaviours are generally more prevalent in the Jewish population, whereas a higher rate of smoking and obesity and lower physical activity are seen in the Arab population.37 While some small-scale programmes have aimed to address these problems, too few resources have been invested in campaigns specifically targeting the Arab population with relation, for example, to smoking cessation and increasing physical activity. In the initial phase of the pandemic, adherence to restrictions was high, with people refraining from gatherings. As time progressed, adherence naturally decreased. In the brief respite between the waves, restrictions were gradually removed and behaviour could return almost to ‘normal’. The fact that Israel tackled the first wave with great success (albeit with a huge economic toll) led the public to perceive the threat had been ‘inflated’, creating a sense of complacence and even indifference to the pandemic. And indeed, when the low number of new infections was soon followed by the escalation of cases and reintroduction of restrictions, people were lulled into a false sense of security by the pre-emptive celebration which may have been less receptive to the renewal of efforts to prevent transmission.
Adherence to physical distancing faces a myriad of obstacles, social, practical and motivational, which are even more marked in disadvantaged populations.38 Deprived populations find it less feasible to use digital platforms to work from home, use public transportation more often to travel to work and might be more overwhelmed by economic losses. When struggling to earn a living, most people would take fewer precautions to protect their health.39, 40, 41
Limitations
Data used in this study were aggregative, without individual-level data, which did not allow for more complex statistical analyses.
Identification of the ethnic group was by locality, with no discrimination between high and low socio-economic areas. SES, including living conditions, has been shown to impact the infection rate of COVID-19, with lower SES associated with higher morbidity and mortality rates, in studies both in Israel and elsewhere.18 , 42 , 43
The Jewish population includes the ultra-Orthodox subpopulation, a socially and culturally separate group, making up 12% of the total population, which exhibited high COVID-19 morbidity from the beginning and throughout the pandemic.17 Their inclusion here in the overall Jewish population reduces the actual gap between non-Orthodox Jewish and Arab populations.
Public health implications
Despite a promising start, with high adherence to public health measures and low mortality during the initial stages of the pandemic, the Arab ethnic minority suffered a marked increase in cases and deaths during Israel's second and third COVID-19 waves. COVID-19 acted as a magnifying glass, exacerbating the existing ethnic disparities in health. This, coupled with suboptimal enforcement of restrictions, may have contributed to lack of trust in this disadvantaged population and to increased health burden of the pandemic. Despite efforts to include stakeholders at the decision-making level, minority groups could be better represented to increase trust and compliance among these groups. Their routine inclusion in policy making, and not just in times of crisis, may help to reduce disparities and better target resources. It is possible that the grave health and economic toll of subsequent national lockdowns could have been avoided if public health measures had been better tailored to populations at greatest risk. Further research may examine the relationship between health behaviour during the pandemic, varying levels of health literacy and culture of ethnic minorities and how these impact adherence of minority populations to public health measures. Moving forward, mitigation plans, including the widespread vaccination drive that started on 20 December 2020, should be culturally tailored to reduce the disproportionate burden of COVID-19 experienced by disadvantaged groups.
Author statements
Ethical approval
The study protocol was approved by the Institutional Ethics Committee of Tel Aviv University (Approval number 0002952-1).
Funding
None declared.
Competing interests
None declared.
Data access and integrity
The authors declare that they had full access to all of the data in this study, and the authors take complete responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhe.2021.07.018.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Khunti K., Singh A.K., Pareek M., Hanif W. Is ethnicity linked to incidence or outcomes of covid-19? BMJ. 2020;369 doi: 10.1136/bmj.m1548. [DOI] [PubMed] [Google Scholar]
- 2.Public Health England . 2020. Beyond the data: understanding the impact of COVID-19 on BAME communities.https://www.gov.uk/government/publications/covid-19-understanding-the-impact-on-bame-communities [Google Scholar]
- 3.Rubin-Miller L., Alban C., Artiga S., Sullivan S. 2020. COVID-19 racial disparities in testing, infection, hospitalization, and death: analysis of epic data.https://www.kff.org/coronavirus-covid-19/issue-brief/covid-19-racial-disparities-testing-infection-hospitalization-death-analysis-epic-patient-data/ Published September 16. [Google Scholar]
- 4.Webb Hooper M., Nápoles A.M., Pérez-Stable E.J. COVID-19 and racial/ethnic disparities. JAMA, J Am Med Assoc. 2020;323(24):2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pareek M, Bangash MN, Pareek N, Pan D, Sze S, Minhas JS, et al. Ethnicity and COVID-19: an urgent public health research priority. Lancet. 2020;395(10234):1421. doi: 10.1016/S0140-6736(20)30922-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tai D., Shah A., Doubeni C., Sia I., Wieland M. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin Infect Dis. 2020 Jun 20;72(4):703–706. doi: 10.1093/cid/ciaa815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heinrich C. Health literacy: the sixth vital sign. J Am Acad Nurse Pract. 2012;24(4):218–223. doi: 10.1111/j.1745-7599.2012.00698.x. [DOI] [PubMed] [Google Scholar]
- 8.Gordon N., Hornbrook M.C. Differences in access to and preferences for using patient portals and other eHealth technologies based on race, ethnicity, and age: a database and survey. J Med Internet Res. 2016;18(3) doi: 10.2196/jmir.5105. https://www.jmir.org/2016/3/e50/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chernichovsky D., Bisharat B., Bowers L., Brill A., Sharony C. Taub Center for Population Research; 2017. The health of the Arab Israeli population.https://www.iataskforce.org/entities/view/1468 [Google Scholar]
- 10.Daoud N., Soskolne V., Mindell J.S., Roth M.A., Manor O. Ethnic inequalities in health between Arabs and Jews in Israel: the relative contribution of individual-level factors and the living environment. Int J Publ Health. 2018;63(3):313–323. doi: 10.1007/s00038-017-1065-3. [DOI] [PubMed] [Google Scholar]
- 11.Israel Central Bureau of Statistics . 2020. Israel localities.https://www.cbs.gov.il/he/publications/Pages/2019/יישובים-בישראל.aspx [Google Scholar]
- 12.Marshall, J. C, Murthy, S, Diaz, J, Adhikari, N. K, Angus, D. C, Arabi, Y.M, et al. A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect Dis. 2020;20(8):e192–e197. doi: 10.1016/S1473-3099(20)30483-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tzfadia E. Mixed cities in Israel localities of contentions. Asian Stud Rev. 2011;26(1):153–165. https://www.berghahnjournals.com/downloadpdf/journals/israel-studies-review/26/1/isr260114.xml [Google Scholar]
- 14.Saban M., Myers V., Wilf-Miron R. Coping with the COVID-19 pandemic - the role of leadership in the Arab ethnic minority in Israel. Int J Equity Health. 2020;19(1):154. doi: 10.1186/s12939-020-01257-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marí-Dell’olmo M., Gotsens M., Pasarín M.I., et al. Socioeconomic inequalities in COVID-19 in a European urban area: two waves, two patterns. Int J Environ Res Publ Health. 2021;18(3):1–12. doi: 10.3390/ijerph18031256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clouston S.A.P., Natale G., Link B.G. Socioeconomic inequalities in the spread of coronavirus-19 in the United States: a examination of the emergence of social inequalities. Soc Sci Med. 2021:268. doi: 10.1016/j.socscimed.2020.113554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Waitzberg R., Davidovitch N., Leibner G., Penn N., Brammli-Greenberg S. Israel's response to the COVID-19 pandemic: tailoring measures for vulnerable cultural minority populations. Int J Equity Health. 2020;19(1):71. doi: 10.1186/s12939-020-01191-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saban M., Shachar T., Miron O., Wilf-Miron R. 2020. Effect of socioeconomic and ethnic characteristics on COVID-19 infection: the case of the Ultra-Orthodox and the Arab communities in Israel. Available at SSRN 3605101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jaffe, A, Giveon, S, Wulffhart, L, Oberman, B, Baidousi, M, Ziv, A., et al. Adult Arabs have higher risk for diabetes mellitus than Jews in Israel. PloS One. 2017;12(5) doi: 10.1371/journal.pone.0176661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Karaca-Mandic P., Georgiou A., Sen S. Assessment of COVID-19 hospitalizations by race/ethnicity in 12 states. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.3857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zakeri R., Bendayan R., Ashworth M., Bean D.M., Dodhia H., Durbaba S., et al. Public and Global Health; 2020 Jul. A case-control and cohort study to determine the relationship between ethnic background and severe COVID-19.http://medrxiv.org/lookup/doi/10.1101/2020.07.08.20148965 [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Williamson, E., Walker, A.J., Bhaskaran, K., Bacon, S., Bates, C., Morton, C.E., et al. OpenSAFELY: factors associated with COVID-19-related hospital death in the linked electronic health records of 17 million adult NHS patients. MedRxiv. May 2020 doi: 10.1101/2020.05.06.20092999. 2020.05.06.20092999. [DOI] [Google Scholar]
- 23.Saban M., Myers V., Luxenburg O., Wilf-Miron R. Tipping the scales: a theoretical model to describe the differential effects of the COVID-19 pandemic on mortality. Int J Equity Health. 2021;20(1):1–6. doi: 10.1186/s12939-021-01470-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Levin-Zamir D., Baron-Epel O.B., Cohen V., Elhayany A. The association of health literacy with health behavior, socioeconomic indicators, and self-assessed health from a national adult survey in Israel. J Health Commun. 2016;21:61–68. doi: 10.1080/10810730.2016.1207115. [DOI] [PubMed] [Google Scholar]
- 25.Yashiv E., Katsir N. 2014. The labor market of Israeli Arabs key features and policy solutions.https://www.tau.ac.il/∼yashiv/Israeli%20Arabs%20in%20the%20Labor%20Market%20--%20Policy%20Paper.pdf [Google Scholar]
- 26.Hutchins S.S., Fiscella K., Levine R.S., Ompad D.C., McDonald M. Protection of racial/ethnic minority populations during an influenza pandemic. Am J Publ Health. 2009;99(SUPPL. 2):S261–S270. doi: 10.2105/AJPH.2009.161505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Horton R. Offline: COVID-19 is not a pandemic. Lancet. 2020;396(10255):874. doi: 10.1016/S0140-6736(20)32000-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Radai I., Elran M., Makladeh Y., Kornberg M. The Arab citizens in Israel: current trends according to recent opinion polls. Vol 18. Strat Assess. 2015;18(2):101. https://www.inss.org.il/he/wp-content/uploads/sites/2/systemfiles/adkan18_2ENG_4_Radai et al.pdf [Google Scholar]
- 29.Hermesh B., Rosenthal A., Davidovitch N. The cycle of distrust in health policy and behavior: lessons learned from the Negev Bedouin. PloS One. 2020;15(8) doi: 10.1371/journal.pone.0237734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pinchas-Mizrachi R., Zalcman B.G., Daoud N. Trust in the Israeli healthcare system Among Arabs, Jewish immigrants, and non-immigrants. Int J Behav Med. 2020 Dec;27(6):647–659. doi: 10.1007/s12529-020-09902-8. [DOI] [PubMed] [Google Scholar]
- 31.Bonell, C., Michie, S., Reicher, S., West, R., Bear, L., Yardley, L., et al. Harnessing behavioural science in public health campaigns to maintain “social distancing” in response to the COVID-19 pandemic: key principles. J Epidemiol Community Health. 2020;74(8):617–619. doi: 10.1136/jech-2020-214290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Efrati I. Haaretz; 2020. Ultra-Orthodox, Arab cities across Israel challenge planned coronavirus lockdown; p. 2020. [Google Scholar]
- 33.Israel's Arab doctors surmount challenges in combating coronavirus - the National. 2020. https://www.thenational.ae/world/mena/israel-s-arab-doctors-surmount-challenges-in-combating-coronavirus-1.1014907 [Google Scholar]
- 34.Analysis of trends in morbidity in the Arab population. National Center for information and knowledge on Covid; 2020. https://www.gov.il/he/departments/publications/reports/research-report-n178-morbidity-trends-arab-society [Google Scholar]
- 35.Ory M., Smith M.L., Mier N., Wenicke M. The science of sustaining health behavior change: the health maintenance consortium. Am J Health Behav. Nov-Dec 2010;34(6):647–659. doi: 10.5993/ajhb.34.6.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fjeldsoe B.S., Neuhaus M., Winkler E. Systematic review of maintenance of behavior change following physical activity and dietary interventions. Health Psychol. 2011. Jan;30(1):99–109. doi: 10.1037/a0021974. [DOI] [PubMed] [Google Scholar]
- 37.Muhsen K., Green M.S., Soskolne V., Neumark Y. Inequalities in non-communicable diseases between the major population groups in Israel: achievements and challenges. Lancet. 2017;389(10088):2531. doi: 10.1016/S0140-6736(17)30574-3. [DOI] [PubMed] [Google Scholar]
- 38.West R., Michie S., Rubin G., Behaviour R.A.-N.H. U. Applying principles of behaviour change to reduce SARS-CoV-2 transmission. Nat Human Behav. 2020;2020(4):451–459. doi: 10.1038/s41562-020-0887-9. https://www.nature.com/articles/s41562-020-0887-9 [DOI] [PubMed] [Google Scholar]
- 39.Kelly S., Martin S., Kuhn I., Cowan A., Brayne C., Lafortune L. In: Wang Y., editor. vol. 11. PLoS One; 2016. (Barriers and facilitators to the uptake and maintenance of healthy behaviours by people at mid-life: a rapid systematic review). (1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Farmer N., Wallen G.R., Baumer Y., Powell-Wiley T.M. COVID-19: growing health disparity gaps and an opportunity for health behavior discovery? Health Equity. 2020;4(1):316–319. doi: 10.1089/heq.2020.0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Owen W., Carmona R., Jama C.P.- 2020 U. Failing another national stress test on health disparities. J Am Med Assoc. 2020;323(19):1905. doi: 10.1001/jama.2020.6547. https://jamanetwork.com/journals/jama/article-abstract/2764788 [DOI] [PubMed] [Google Scholar]
- 42.Birenbaum-Carmeli D., Chassida J. Covid-19 in Israel: socio-demographic characteristics of first wave morbidity in Jewish and Arab communities. Int J Equity Health. 2020;19(1) doi: 10.1186/s12939-020-01269-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Office for National Statistics . 2020. Deaths involving COVID-19 by local area and socioeconomic deprivation: deaths occurring between 1 March and 31 july 2020.https://backup.ons.gov.uk/wp-content/uploads/sites/3/2020/08/Deaths-involving-COVID-19-by-local-area-and-socioeconomic-deprivation-deaths-occurring-between-1-March-and-31-.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.