Abstract
Objective
The 2019 coronavirus disease pandemic (COVID-19) required strict confinement measures that differentially impacted the individual's daily life. Thus, this work aimed to study postpartum women's mental health in Argentina during mandatory social isolation.
Design
A cross-sectional survey was conducted from May to July 2020, which included five validated questionnaires to assess postpartum depression (Postpartum Depression Screening Scale‐Short Form), insomnia (Insomnia Severity Index), memory complaints (Memory Complaint Scale), metacognition (Brief Metamemory and Metaconcentration Scale), and breastfeeding self-efficacy (Breastfeeding Self-Efficacy Scale-Short Form). Sociodemographic variables, social isolation characteristics, and breastfeeding practices were also collected. This study was conducted in accordance with the Declaration of Helsinki. Statistical analysis included zero-order correlations, multiple logistic regressions, and a set of structural equation models (SEM) to test direct and indirect effects. Goodness-of-fit indices were calculated for SEM.
Setting
Postpartum women were recruited from public hospitals, private health clinics, and online community recruitment in the Cordoba province (Argentina).
Participants
305 postpartum women from Argentina.
Measurements and findings
37% of women reported postpartum depression, 46% insomnia, 42% memory impairment, 60% low metaconcentration, 50% low metamemory, and 23% low breastfeeding efficacy. Also, significant associations were found demonstrating that social isolation promoted postpartum depression and insomnia were reciprocally related, which compromised female cognition and efficacy. This situation was aggravated in women during late postpartum, with previous children, and by low social support (e.g., family, health professionals), with non-exclusive breastfeeding being increased.
Key conclusions
This is the first study addressing postpartum women's mental status during social isolation in Argentina, which was a promoting factor for postpartum depression and insomnia that were reciprocally related. This situation was also aggravated by reproductive factors, such as late postpartum, multiparity, breastfeeding frequency, and non-exclusive breastfeeding. Additionally, breastfeeding self-efficacy depended on mental health status, and euthymia therefore favoured the practice of exclusive breastfeeding.
Keywords: Pandemics; Depression, Postpartum; Sleep; Self efficacy; Metacognition; Cognitive dysfunction
Implications for practice.
Women's health must be addressed by clinicians and researchers during COVID-19 pandemic, as early evaluation and promotion of mental health and breastfeeding will improve the health status of specific female populations (e.g., multiparous and advanced postpartum women, essential workers, and women without adequate social support). Also, these issues must be considered during political decision-making processes to protect the well-being of vulnerable groups.
Alt-text: Unlabelled box
Introduction
The 2019 coronavirus disease pandemic (COVID-19) required rapid and substantial responses by health systems around the world, which generally proceeded with strict confinement measures (Matias et al., 2020). Consequently, the Argentinian government early enforced the Preventive and Mandatory Social Isolation (PMSI) on March 20th, 2020, after the first cases were confirmed (Argentine National Ministry of Health, 2020). Social distancing and reduction of population movement were enforced through the cancellation of public events and transport, religious activities, tourism, schools, many works, among others. These measures drastically modified people's lifestyles and potentially impacted their mental health, which needs to be properly studied (Johnson et al., 2020; Sher, 2020), to develop well-being promoting strategies for the general population and those who need additional support during certain vital moments, such as women under reproductive demands (PAHO, 2020).
Psychological disturbances are frequently found during the postpartum period (Zubaran et al., 2010b). Postpartum depression is a public health issue affecting 13 to 19% of women, characterised by feelings of sadness, anger, or frustration that interfere with daily life shortly after birth and can last up to a year after that (Hutchens and Kearney, 2020). Despite its prevalence, it is underdiagnosed, with different risk factors being identified, such as insomnia, childcare and life stress, lack of social support, domestic violence, prenatal depression, and negative breastfeeding experiences (Hutchens and Kearney, 2020).
Some authors predict an increment in the prevalence of postpartum depression during the pandemic due to its effects on mental health (Viaux et al., 2020). Insomnia, mood changes, fear, stress, and financial worries have been identified in confined people during the COVID-19 pandemic (Torales et al., 2020). It is more complex in groups with psychological vulnerability, such as women in perinatological stages. Studies about peripartum women's mental health during the COVID-19 pandemic are scarce. Durankuş and Aksu (2020) found a 35% prevalence of depression in Turkish childbearing women with significant effects of social isolation. Davenport et al. (2020) studied the influence of pandemic and social distancing/isolation measures on mental health during peripartum in Canada, finding a 41% prevalence of maternal depression, which was confirmed by Cameron et al. (2020) in North America (prevalence: 33.16% to 43.37%). In Italy, these concerns also increased depressive prevalence in peripartum women (29%) (Zanardo et al., 2020).
Although the effects of lockdown restrictions during the COVID-19 pandemic on sleep problems are currently studied, they have not been addressed in women during postpartum (Ramírez-Ortiz et al., 2020). Some reports identified a 37% increase in insomnia rates in the general population, which correlated with states of depression, anxiety, and stress (Morin and Carrier, 2020). In Argentina, a high prevalence of insomnia was found in university students during the early stages of social isolation, which was associated with worry, coping, and academic engagement (Scotta et al., 2020).
Studies on mental health during the COVID-19 pandemic in Argentina showed that women are more vulnerable to developing mental disorders during prolonged social isolation and quarantine periods (López Steinmetz et al. 2020). Moreover, Canet-Juric et al. (2020) evaluated longitudinally the emotional impact of these measures on the Argentinian general population and found that depression impairs over time and reduces women's positive affectivity (i.e., the level of subjective experiences with positive emotions and feelings). These studies suggest that women's mental health must be monitored when lockdown measures are implemented or extended, and the promotion of mental health must be encouraged. However, there are no studies to date that investigate this during the postpartum period to reduce women's vulnerability (Bermejo-Sánchez et al., 2020). In this sense, postpartum is a time of adaptation and learning for women, who need to develop new behaviours to efficiently care for their child and obtain satisfaction in motherhood (Carrizo et al., 2020). Maternal self-efficacy is a construct defined as the “beliefs a mother holds of their capabilities to organise and execute the tasks related to parenting a child”, which is affected by their mental status and previous experiences, among other factors (Kohlhoff and Barnett, 2013). Self-efficacy is part of the psychological capital of a person, which is defined as a positive mental state during growth and development (Minglu et al., 2020). Peripartum women with high psychological capital show less psychological stress and anxiety, less postpartum depression, and more optimism (Minglu et al., 2020; Nadjafi-Semnani et al., 2018). Besides, women who do not feel effective at breastfeeding may experience feelings of failure and low mood, and therefore increased risk of postpartum depression and breastfeeding cessation (Haga et al., 2012). Given the influence of psychological capital on well-being, it becomes more relevant in the current pandemic context. Consequently, it has been studied during the lockdown measures due to the COVID-19 pandemic, with results suggesting that these psychological resources (self-efficacy, optimism, hope, wisdom, gratitude toward the world, gratitude of being, peaceful disengagement, and acceptance) improve the psychological well-being of isolated individuals (Pellerin and Raufaste, 2020).
Thus, this study aimed to evaluate postpartum depression, insomnia, and cognitive impairment during the pandemic COVID-19 social isolation in Argentina, in relation to different factors. Based on the literature outlined above, the hypothesis was that these mental health concerns are aggravated in postpartum women during the COVID-19 social isolation, which are conditioned by sociodemographic and health characteristics, having different direct and indirect interactions to impact breastfeeding self-efficacy.
Methods
Subjects
For this cross-sectional study, self-report online questionnaires were administered to 305 postpartum women from Argentina, who were recruited from May to July 2020, during the COVID-19 pandemic PMSI. Women were recruited from three sources: public hospitals, private health clinics, and online community recruitment. Inclusion criteria were: adult (≥ 18 years-old), Argentina's inhabitant, postpartum (first twelve months), and breastfeeding.
All participants signed informed consent before being voluntarily included. This research was approved by the corresponding Research Ethics Committee (registration code REPIS-3177), following the Declaration of Helsinki and current legislation.
Instruments
Insomnia assessment
The Insomnia Severity Index (ISI) was used to assess the nature, severity, and impact of insomnia during the previous month (Morin et al., 2011). The ISI is a 7-item self-report questionnaire typically used in insomnia research (Goldstein and Chervin, 2016) which evaluates the following dimensions: severity of sleep onset, sleep maintenance, early morning awakening problems, sleep dissatisfaction, interference of sleep difficulties with daytime functioning, noticeability of sleep problems by others, and distress caused by the sleep difficulties. Each item was rated on a 5-point Likert scale (0 to 4, where 0 indicates no problem and 4 corresponds to a very severe problem) and scores were transformed on a scale ranging from 0 to 28. Thus, higher scores indicate more severe insomnia and a higher impact on the quality of a person's life. The optimal cut-off for community samples is ≥10 (sensitivity of 86% and a specificity of 88%) (Morin et al., 2011). The ISI exhibited adequate properties regarding reliability and validity (Fernandez-Mendoza et al., 2012). In this study, Chronbach's alpha was calculated to assess its reliability, which was acceptable (alpha=0.805).
Postpartum depression
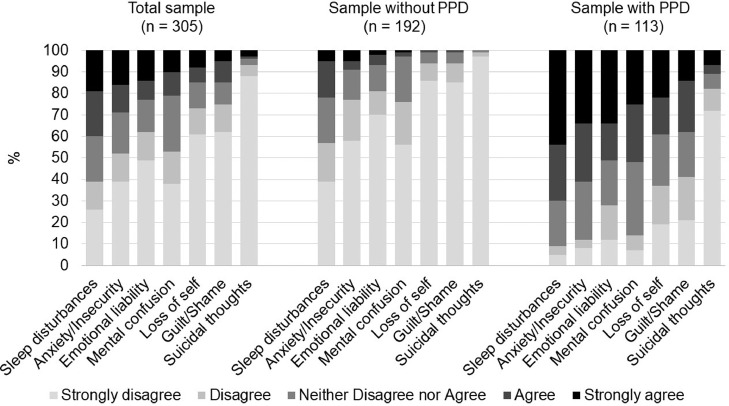
The Spanish version of the Postpartum Depression Screening Scale‐Short Form (PDSS‐SF) was used to assess signs suggestive of depressive disorders during the postpartum period (Le et al., 2010). The questionnaire has 7-items that study sleep/eating disturbances, anxiety/insecurity, emotional lability, mental confusion, loss of self, guilt/shame, and suicidal thoughts during the last two weeks. Each item was rated on a 5-point Likert scale (1 to 5, where 0 indicates “strongly disagree” and 5 corresponds to “strongly agree”). Scores were transformed on a scale ranging from 7 to 35, with higher scores indicating a higher level of depression. The cut-off score for the PDSS-SF is 17 (89% sensitivity and 77% specificity) (Zubaran et al., 2010a). Previous studies tested the psychometric properties of the PDSS‐SF, showing its validity and reliability (Lara et al., 2013; Rodríguez-Muñoz et al., 2018; Zubaran et al., 2010a). In the current study, its alpha was acceptable (alpha=0.830). The PDSS shows some advantages over other instruments: it is more comprehensive, covers a wider array of symptoms, can be used during the first postpartum year, exhibits good psychometric properties, and is available for Latin American women, among others (Lara et al., 2013).
Cognitive status
Metacognition: Metacognition encompasses the self-regulatory mechanisms of cognitive processes (i.e., knowledge, monitoring, and control of cognitive awareness). For this study, metacognition was assessed using the Brief Metamemory and Metaconcentration Scale (BMMS) (Manzar et al., 2020; Klusmann et al., 2011). Metamemory refers to awareness about one's memory, whereas metaconcentration represents self-perceived concentration abilities and regulation. The BMMS is a 9-item scale, divided into two dimensions: metamemory (5-items) and metaconcentration (4 items). The responses were given on a 5-Likert scale (1 for “absolutely wrong” to 5 for “absolutely true”). Higher scores indicate better metacognition (Klusmann et al., 2011). Previous studies reported that the BMMS has adequate psychometric reliability and validity (Klusmann et al., 2011; Manzar et al., 2020; Albougami et al., 2020). In this study, Cronbach's alpha was 0.784.
Memory complaints: The Spanish version of the Memory Complaint Scale for patients (MCS-P) was used. This scale explores the subjective complaints of participants judging their daily behaviours concerning memory functioning and to what extent they are affected (Vale et al., 2012). The questionnaire has seven questions with graded responses of increasing intensity (0, 1, and 2), and scores were transformed on a scale ranging from 0 to 14, where higher scores indicate a higher degree of memory complaints. Then, women were classified based on cut-off values as no memory impairment (<3) and memory impairment (≥3). Similar to previous studies (Hwang and Kim, 2019), internal consistency was adequate (alpha=0.867).
Breastfeeding self-efficacy
Women's breastfeeding confidence was assessed using the Breastfeeding Self-Efficacy Scale-Short Form (BSES-SF) in Spanish (Oliver-Roig et al., 2012). The BSES is valid for identifying women with breastfeeding difficulties and has been used for the evaluation of supportive interventions. This instrument contains 14 items presented positively with the phrase “I can always” and anchored with a 5-point Likert-type scale (1 for “not at all confident” to 5 for “always confident”). Then, scores are added up to produce a range from 14 to 70, with higher scores indicating higher levels of breastfeeding self-efficacy. The identified BSES-SF cut-off score is 50 points, where scores >50 are indicators of adequate breastfeeding confidence (sensitivity >70% and specificity >50%) (Nanishi et al., 2015). Moreover, its psychometric characteristics have been tested, confirming its validity, reliability, and structure (Tuthill et al., 2016; Oliver-Roig, et al., 2012). In the current study, reliability was good (alpha=0.869).
Sociodemographic and health questionnaire
-
•
A questionnaire was used to collect data about sociodemographic variables, social isolation characteristics, and breastfeeding practices (Cortez et al., 2020). Self-reported information was registered about:
Sociodemographic variables: age, partnership status (single or in a couple), years of education (≥12 years or <12 years), employment (formal employment or informal employment/unemployment), health insurance (yes or no). Since advanced maternal age has been associated with peripartum complications that can lead to anxiety and worry (Lampinen et al., 2009), age was dichotomised as <35 years old and ≥35 years old.
-
•
Obstetric and breastfeeding characteristic: mode of delivery (vaginal or Cesarean), parity (primiparous, secondiparous, or multiparous), number of pregnancies (1 or >1), postpartum period (months), gestation characteristics (single or multiple, number of weeks), type of breastfeeding (exclusive or non-exclusive), previous breastfeeding experience (yes or no), breastfeeding frequency (hours between feedings), assistance and/or information about breastfeeding received from doctors (yes or no) or other health professionals (yes or no), attendance to events, groups, workshops or other activities about breastfeeding organised by community support organizations (-BFS- yes or no).
-
•
Social isolation characteristics: days of isolation, being an essential worker (yes or no), telecommuting (yes or no), home studying (yes or no), number of cohabitants (number of people with whom she is isolated without counting herself).
Statistical analysis
All statistical analyses were performed using the Stata software (version 15, StataCorp). P values below 0.05 were considered significant (p<0.05). The reliability related to internal consistency was measured by the alpha coefficient. Descriptive statistics (mean and standard deviation) were calculated for all numerical variables; the percentage of categorical variables was also described. Multiple logistic regression was performed to compare the prevalence of mental health conditions among sociodemographic, obstetric, and social isolation characteristics. Results were expressed as odds ratios (OR) with a confidence interval (IC95%) and p-values.
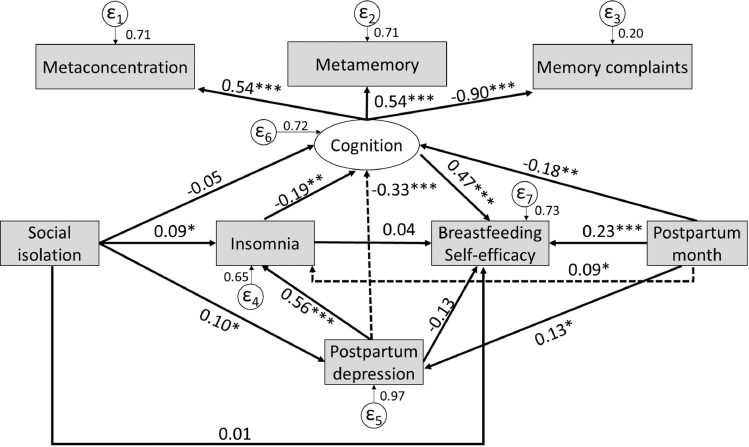
Structural equation models (SEM) were used to test direct and indirect relationships. These models can be interpreted as a combination of multiple regressions and factor analysis. Three steps were conducted. First, kurtosis and skewness were assessed to test the normality of mental health questionnaires (cut-off point ±2) because a normal distribution is required for the application of full information maximum likelihood in SEM (Soh et al., 2020). Second, a set of confirmatory factor analyses were conducted to confirm the dimensionality of the five questionnaires, with the calculation of goodness-of-fit indices: Chi-square to degree of freedom ratio (χ2/df), Root Mean Square Error of Approximation (RMSEA), Comparative Fit Index (CFI), Tucker Lewis Index (TLI), and Standardised Root Mean Square Residual (SRMR) (Miranda et al., 2020a; Miranda et al., 2020b). Third, Pearson's correlations (r) were performed to test associations between the variables included in the hypothesised model.
A theoretical SEM was established based on previous studies (Soh et al., 2020; Miranda et al., 2020c; Carrizo et al., 2020). This model consisted of one latent variable (cognition), represented by metamemory, metaconcentration, and memory complaints. This latent variable was integrated with five observed variables: social isolation, insomnia, depression, breastfeeding self-efficacy, and postpartum months. The detailed model was developed by specifying the pathways in these models. Total effects were decomposed into direct and indirect effects. Finally, goodness-of-fit indices were calculated.
The minimum sample size to detect effects in the tested SEM was 242, with different conditions considered to determine the appropriate sample size (α=0.05, β=0.20, and effect size=0.06). Thus, the sample size used (N=305) exceeds the recommended minimum.
Results
Characteristics of Participants and other Descriptive Statistics
Sociodemographic, obstetric, and social isolation characteristics are summarised in Table 1 . The mean age of the sample was 30.51 years (SD=5.65). The majority were in a couple (96%) and had ≥12 years of formal education (93%). Also, 68% were employed, and 86% had health insurance. Regarding obstetric data, 58% of participants were primiparous, 49% were primigravidae, and 73% were recruited during the first 6 months of postpartum. They gave birth after ≥38 weeks of pregnancy in 85% of cases, with 65% being by Caesarean section. Multiple gestation pregnancies were infrequent (3%). Exclusive breastfeeding practice was mainly found (65%), showing a daily frequency every ≤3 hours, with 77% of participants reporting adequate breastfeeding efficacy. Nonetheless, 60% did not have previous breastfeeding experience, and 40% did not receive information nor support from their health professionals about it.
Table 1.
Sample characteristics of 305 postpartum women from Argentina during the COVID-19 pandemic.
| Variables | N | % | Mean | SD |
|---|---|---|---|---|
| Sociodemographic characteristics | ||||
| Age | 30.51 | 5.65 | ||
| <35 years old | 230 | 75 | ||
| ≥35 years old | 75 | 25 | ||
| Educational level | ||||
| <12 years | 22 | 7 | ||
| ≥12 years | 283 | 93 | ||
| Partnership status | ||||
| In couple | 292 | 96 | ||
| Single | 13 | 4 | ||
| Employment status | ||||
| Employed | 208 | 68 | ||
| Unemployed | 97 | 32 | ||
| Health insurance | ||||
| Yes | 261 | 86 | ||
| No | 44 | 14 | ||
| Obstetric and breastfeeding characteristics | ||||
| Parity | 1.61 | 1.16 | ||
| Primiparous | 177 | 58 | ||
| Secondiparous | 97 | 32 | ||
| Multiparous | 31 | 10 | ||
| Gestation pregnancy | ||||
| Single | 297 | 97 | ||
| Multiple | 8 | 3 | ||
| Gestation time | 38.59 | 2.22 | ||
| <38 weeks | 47 | 15 | ||
| ≥38 weeks | 258 | 85 | ||
| Mode of delivery | ||||
| Vaginal Delivery | 106 | 35 | ||
| Cesarean | 199 | 65 | ||
| Postpartum months | 4.88 | 3.33 | ||
| ≤6 months | 223 | 73 | ||
| >6 months | 82 | 27 | ||
| Number of pregnancies | 1.90 | 1.32 | ||
| 1 | 150 | 49 | ||
| >1 | 155 | 51 | ||
| Type of breastfeeding | ||||
| Exclusive | 197 | 65 | ||
| Non-exclusive | 108 | 35 | ||
| Frequency of breastfeeding | 2.93 | 2.07 | ||
| ≤3 hours | 242 | 79 | ||
| >3-6 hours | 55 | 18 | ||
| >6 hours | 8 | 3 | ||
| Breastfeeding experience | ||||
| Yes | 123 | 40 | ||
| No | 182 | 60 | ||
| Support from doctors | ||||
| Yes | 193 | 63 | ||
| No | 112 | 37 | ||
| Support from other health professionals | ||||
| Yes | 187 | 61 | ||
| No | 118 | 39 | ||
| Attendance to BFS activities | ||||
| Yes | 125 | 41 | ||
| No | 180 | 59 | ||
| Breastfeeding self-efficacy | ||||
| BSES-SF >50 (Adequate) | 234 | 77 | ||
| BSES-SF ≤50 (Poor) | 71 | 23 | ||
| Social isolation characteristics | ||||
| Days of isolation | 67.88 | 12.19 | ||
| <60 days | 69 | 23 | ||
| ≥60 days | 236 | 77 | ||
| Number of cohabitants | ||||
| 2 persons | 143 | 47 | ||
| 3-4 persons | 131 | 43 | ||
| 5 or more persons | 31 | 10 | ||
| Telecommuting | ||||
| Yes | 78 | 26 | ||
| No | 227 | 74 | ||
| Essential worker a | ||||
| Yes | 60 | 20 | ||
| No | 245 | 80 | ||
| Home studying | ||||
| Yes | 86 | 28 | ||
| No | 219 | 72 | ||
| Mental health | ||||
| Postpartum depression | ||||
| PDSS-SF <17 (No depression) | 192 | 63 | ||
| PDSS-SF ≥17 (Depression) | 113 | 37 | ||
| Insomnia | ||||
| ISI <10 (No insomnia) | 164 | 54 | ||
| ISI ≥10 (Insomnia) | 141 | 46 | ||
| Memory complaints | ||||
| MCS <3 (No memory impairment) | 176 | 58 | ||
| MCS ≥3 (Memory impairment) | 129 | 42 | ||
| Metamemory | ||||
| BMMS ≤19 (Low) | 153 | 50 | ||
| BMMS >19 (Adequate) | 152 | 50 | ||
| Metaconcentration | ||||
| BMMS ≤14 (Low) | 184 | 60 | ||
| BMMS >14 (Adequate) | 121 | 40 | ||
Note. a = According to the Argentinian Government, essential workers are those who are employed in vital sectors during COVID-19 pandemic; ISI = Insomnia Severity Index; PDSS‐SF = Postpartum Depression Screening Scale‐Short Form; MCS-P = Memory Complaint Scale for patients; BMMS-MM = Brief Metamemory and Metaconcentration Scale (MM = Metamemory subscale; MC = Metaconcentration subscale); BSES-SF = Breastfeeding Self-Efficacy Scale-Short Form.
Most participants had been socially isolated for ≥60 days at the survey time (77%), accompanied by two or more persons. Also, 26% of women telecommuted, 20% were essential workers, and 28% were studying at home.
Regarding mental health, 37% of women showed suggestive symptoms of postpartum depression (Figure 1 ), 46% reported insomnia, and 42% had indicative complaints of memory impairment. The metacognition assessment showed that 60% of participants had low metaconcentration, and 50% had low metamemory. Table 2 shows descriptive statistics and the internal consistency of each questionnaire.
Fig. 1.
Distributional patterns of the level of postpartum depressive symptomatology.
Table 2.
Descriptive statistics and internal consistencies of the used questionnaires.
| Questionnaire | Items | Mean | SD | Range | Median | Skewness | Kurtosis | Cronbach's α |
|---|---|---|---|---|---|---|---|---|
| ISI | 7 | 9.45 | 5.56 | 0-25 | 9 | 0.36 | -0.49 | 0.805 |
| PDSS‐SF | 7 | 15.10 | 6.49 | 7-35 | 13 | 0.79 | -0.27 | 0.830 |
| MCS-P | 7 | 3.80 | 3.26 | 0-14 | 3 | 0.92 | 0.13 | 0.867 |
| BMMS-MM | 5 | 17.98 | 4.61 | 5-25 | 19 | -0.95 | 0.19 | 0.790 |
| BMMS-MC | 4 | 13.41 | 3.18 | 5-19 | 14 | -0.28 | -0.52 | 0.630 |
| BSES-SF | 14 | 56.88 | 8.54 | 20-70 | 59 | -0.87 | 0.73 | 0.869 |
Note. ISI = Insomnia Severity Index; PDSS‐SF = Postpartum Depression Screening Scale‐Short Form; MCS-P = Memory Complaint Scale for patients; BMMS-MM = Brief Metamemory and Metaconcentration Scale (MM = Metamemory subscale; MC = Metaconcentration subscale); BSES-SF = Breastfeeding Self-Efficacy Scale-Short Form.
Postpartum Mental Health and Conditioning Factors
Depression was associated with having ≥12 years of education (OR=5.34, CI95%=1.39-20.54, p=0.0149), and cohabiting with 3-4 persons during social isolation (OR=0.55, CI95%=0.33-0.92, p=0.0233; respect to 2 persons). Besides, insomnia was associated with >6 months of postpartum (OR=2.25, CI95%=1.27-4.01, p=0.0057), and breastfeeding frequency every >3-6 hours (OR=0.46, CI95%=0.24-0.90, p=0.0230; respect to ≤3 hours).
Regarding cognitive status, memory complaints were associated with age >35 years-old (OR=1.77, CI95%=1.03-3.02, p=0.0375), multiparity (OR=6.20, CI95%=1.36-28.15, p=0.0181), and >6 months of postpartum (OR=1.95, CI95%=1.10-3.47, p=0.0222). Women who practiced exclusive breastfeeding showed lower metamemory dysfunction (OR=0.46, CI95%=0.27-0.79, p=0.0046).
Low metaconcentration was associated with being >35 years-old (OR=1.98, CI95%=1.11-3.53, p=0.0209), essential worker (OR=1.93, CI95%=1.01-3.66, p=0.0452), in >6 months of postpartum (OR=2.06, CI95%=1.10-3.84, p=0.0231), and exclusive breastfeeding practitioner (OR=0.30, CI95%=0.16-0.54, p=0.0001) with a frequency of >3-6 hours (OR=0.49, CI95%=0.25-0.97, p=0.0416; respect to ≤3 hours).
An adequate breastfeeding self-efficacy was associated with multigravidity (OR=0.34, CI95%=0.12-0.96, p=0.0423), medical support (OR=2.20, CI95%=1.08-4.46, p=0.0288), >6 months of postpartum (OR=2.94, CI95%=1.32-6.55, p=0.0085), and exclusive breastfeeding (OR=15.85, CI95%=7.59-33.09, p=0.0001).
Zero-order correlations between the studied variables are shown in Table 3 . Isolation time was positively correlated to insomnia, depression, and memory complaints (r= 0.169, 0.113 and 0.151, respectively; p<0.05). Also, significant positive associations were found among the scores of postpartum depression, memory complaints, and insomnia (p<0.0001). On the other hand, metacognition was inversely associated with the severity of insomnia and postpartum depression, and memory complaints (p<0.0079). Also, breastfeeding self-efficacy showed the same associations as metacognition.
Table 3.
Correlation matrix for the study variables (N = 305).
| ISI | PDSS-SF | MCS-P | BMMS-MM | BMMS-MC | BSES-SF | Isolation days | |
|---|---|---|---|---|---|---|---|
| ISI | - | <0.0001 | <0.0001 | 0.0079 | <0.0001 | 0.0007 | 0.0031 |
| PDSS‐SF | 0.571 | - | <0.0001 | <0.0001 | <0.0001 | <0.0001 | 0.0494 |
| MCS-P | 0.369 | 0.412 | - | <0.0001 | <0.0001 | 0.0777 | 0.0087 |
| BMMS-MM | -0.152 | -0.223 | -0.453 | - | <0.0001 | <0.0001 | 0.7451 |
| BMMS-MC | -0.271 | -0.269 | -0.453 | 0.586 | - | <0.0001 | 0.5012 |
| BSES-SF | -0.193 | -0.308 | -0.101 | 0.257 | 0.263 | - | 0.5930 |
| Isolation days | 0.169 | 0.113 | 0.151 | -0.019 | -0.039 | -0.031 | - |
Note. ISI = Insomnia Severity Index; PDSS‐SF = Postpartum Depression Screening Scale‐Short Form; MCS-P = Memory Complaint Scale for patients; BMMS-MM = Brief Metamemory and Metaconcentration Scale (MM = Metamemory subscale; MC = Metaconcentration subscale); BSES-SF = Breastfeeding Self-Efficacy Scale-Short Form.
Assessment of Structural Model: Testing Direct and Mediation Effects
When conducting the set of confirmatory factor analyses, all the questionnaires used in the current study showed adequate goodness-of-fit indices (Table 4 ). Moreover, the SEM model showed suitable indices (χ2/df=1.20, CFI=0.990, TLI=0.981, SRMR=0.028, RMSA=0.025), and explained 29% of the variability. These values, therefore, support the hypothetical model.
Table 4.
Model fit statistics of the study variables and structural equation model (N= 305).
| Study variables and SEM model | Model goodness-of-fit indices | ||||
|---|---|---|---|---|---|
| χ2/df | CFI | TLI | SRMR | RMSA | |
| ISI | 2.03 | 0.987 | 0.971 | 0.035 | 0.058 |
| PDSS‐SF | 2.81 | 0.966 | 0.945 | 0.037 | 0.077 |
| MCS-P | 2.55 | 0.981 | 0.967 | 0.031 | 0.071 |
| BMMS | 2.14 | 0.959 | 0.941 | 0.037 | 0.061 |
| BSES-SF | 2.78 | 0.921 | 0.901 | 0.056 | 0.077 |
| SEM model | 1.20 | 0.990 | 0.981 | 0.028 | 0.025 |
Note. ISI = Insomnia Severity Index; PDSS‐SF = Postpartum Depression Screening Scale‐Short Form; MCS-P = Memory Complaint Scale for patients; BMMS-MM = Brief Metamemory and Metaconcentration Scale; BSES-SF = Breastfeeding Self-Efficacy Scale-Short Form; SEM = Structural Equation Model; χ2/df = Chi-square to degree of freedom ratio; RMSEA = Root Mean Square Error of Approximation; CFI = Comparative Fit Index; TLI = Tucker–Lewis Index; SRMR = Standardized Root Mean Square Residual.
Table 5 shows the direct and indirect effects derived from the SEM model (Figure 2 ). Social isolation had significant direct effects on insomnia (β=0.09, SE=0.05, p=0.048) and postpartum depression (β=0.10, SE=0.05, p=0.043), and indirect effects on cognition (β=-0.02, SE=0.01, p=0.048, mediated by depression and insomnia) and insomnia (β=0.03, SE=0.01, p=0.046, through depression).
Table 5.
Decomposition table of standardized direct and indirect effects of the structural equation model for postpartum women's mental health during COVID-19 pandemic social isolation (N = 305).
| β | SE | p | |
|---|---|---|---|
| Direct effects | |||
| Insomnia ← | |||
| Postpartum depression | 0.56 | 0.04 | 0.000 |
| Social isolation | 0.09 | 0.05 | 0.048 |
| Postpartum months | 0.09 | 0.05 | 0.048 |
| Postpartum depression ← | |||
| Social isolation | 0.10 | 0.05 | 0.043 |
| Postpartum months | 0.13 | 0.06 | 0.027 |
| Breastfeeding self-efficacy ← | |||
| Insomnia | 0.04 | 0.07 | 0.585 |
| Postpartum depression | -0.13 | 0.08 | 0.100 |
| Cognition | 0.47 | 0.12 | 0.000 |
| Social isolation | 0.01 | 0.05 | 0.809 |
| Postpartum months | 0.23 | 0.05 | 0.000 |
| Cognition ← | |||
| Insomnia | -0.19 | 0.06 | 0.003 |
| Postpartum depression | -0.33 | 0.07 | 0.000 |
| Social isolation | -0.05 | 0.06 | 0.433 |
| Postpartum months | -0.18 | 0.06 | 0.002 |
| Metamemory ← cognition | 0.54 | 0.06 | 0.000 |
| Metaconcentration ← cognition | 0.54 | 0.05 | 0.000 |
| Memory complaints ← cognition | -0.90 | 0.06 | 0.000 |
| Indirect effects | |||
| Social isolation→Insomnia→Cognition→Breastfeeding self-efficacy | -0.04 | 0.02 | 0.099 |
| Postpartum depression→Insomnia→Cognition→Breastfeeding self-efficacy | -0.24 | 0.07 | 0.001 |
| Insomnia→Cognition→Breastfeeding self-efficacy | -0.14 | 0.05 | 0.014 |
| Postpartum months→Depression→Insomnia→Cognition→Breastfeeding self-efficacy | -0.09 | 0.04 | 0.043 |
| Postpartum depression→Insomnia→Cognition | -0.07 | 0.01 | 0.000 |
| Social isolation→Depression→Insomnia→Cognition | -0.02 | 0.01 | 0.048 |
| Postpartum months→Depression→Insomnia→Cognition | -0.09 | 0.04 | 0.043 |
| Social isolation→Postpartum depression→Insomnia | 0.03 | 0.01 | 0.046 |
| Postpartum months→Postpartum depression→Insomnia | 0.11 | 0.05 | 0.032 |
Note: Bold values indicate p<0.05. SE = Standard error.
Fig. 2.
Structural equation model with standardised coefficients for postpartum women's mental health during COVID-19 pandemic social isolation (N = 305). Direct effects are presented. *p<0.05, **p<0.01; ***p<0.0001.
Regarding insomnia, this variable had direct effects on cognition (β=-0.19, SE=0.06, p=0.003), and indirect effects on breastfeeding self-efficacy (β=-0.14, SE=0.05, p=0.014, through cognition). Likewise, it was found that depression had direct effects on insomnia (β=0.56, SE=0.04, p<0.0001) and cognition (β=-0.33, SE=0.07, p<0.0001). Cognition and breastfeeding self-efficacy were shown to receive indirect effects from depression, with values of β=-0.07 (SE=0.01, p<0.0001, through insomnia) and β=-0.24 (SE=0.07, p<0.0001, mediated by insomnia and cognition) respectively.
Finally, postpartum time showed direct effects on insomnia (β=0.09, SE=0.04, p=0.048), depression (β=0.13, SE=0.06, p=0.027), cognition (β=-0.18, SE=0.06, p=0.002), and breastfeeding self-efficacy (β=0.23, SE=0.05, p<0.0001). Its indirect effects were also statistically significant (Table 5).
Discussion
The measures of social isolation imposed by governments to prevent the spread of SARS-CoV-2 and the saturation of health systems have impacted the normality of daily life. The effect of the pandemic on women's mental health has been recently highlighted, suggesting that they are more vulnerable to the psychological effects of social isolation (López Steinmetz et al., 2020). However, to our knowledge, this is the first study that evaluated it in postpartum women during the COVID-19 pandemic in Latin America with its epidemiological relations.
It was found that postpartum depression and insomnia in Argentinians were more frequent than in pre-pandemic reports. Postpartum depression is a highly relevant public health issue, with a pre-pandemic prevalence ranging between 13 and 19%, depending on the country's income level (O'hara and McCabe, 2013), whereas we found it in 37% of postpartum women during social isolation.
Little research has been conducted in Argentina on postpartum depression. Rozic et al. (2012) found a prevalence of 18% in the private sector during the first days of postpartum (n=398). These women were reevaluated during the second postpartum semester, showing a prevalence of 22%. Another local research studied 86 women between 4 to 12 postpartum weeks in a private healthcare center, who achieved different EPDS scores: ≥10-12 (19%) and ≥13 (19%) (Mathisen et al., 2013). Pham et al. (2018), studied a cohort of 539 women in northwestern Argentina and found prevalences of 31% and 18% using the score cut-off ≥10 and ≥13 (EPDS), respectively. In another study, 45 puerperal women hospitalised in a public maternal hospital were interviewed during the first three postpartum days to find 37% with EPDS scores above 9 (Paolini et al., 2012).
The evidence is scarce in Argentina and generally based on immediate puerperium data, using the EPDS scale with different cut-off points and criteria. Although the difference of a three-point score seems insignificant, it has demonstrated that it causes a significant difference in prevalence outcomes (Matthey et al., 2006). In this sense, researchers should use the value ≥13 to identify postpartum depression in a more specific way (Levis et al., 2020). In our study, the women were assessed using the PPDS scale with a more adequate cut-off point for diagnosis and screening (Zubaran et al., 2010a). If the cut-off points are lowered as in previous studies, the prevalence increases to 50% (cut-off point 14) and 67% (cut-off point 11) (Rodríguez-Muñoz et al., 2018; Quelopana and Champion, 2010). However, we consider that the cut-off point of 17 is better to obtain more precise and stable data and reduce false positives. Therefore, comparisons should be made taking into account that the cut-off points of 13 for the EPDS and 17 for the PDSS are optimal for epidemiological investigations in Latin America (Vega-Dienstmaier et al., 2002, Zubaran et al., 2010b).
The two-fold increase is consistent with other studies about peripartum mental disorders conducted in Turkey (Durankuş and Aksu, 2020), Canada and the United States (Davenport et al. 2020; Cameron et al. 2020), and Italy (Zanardo et al., 2020), during the pandemic. According to these authors, the social and economic impact of COVID-19 combined with fear of contagion, increased domestic workload, among other factors, adversely affected postpartum women's mental health. We found that depression is associated with a high educational level. Education can influence the way women experience and report postpartum depressive symptoms, by influencing subjective experience, self-awareness, and acceptance. This allows more educated women to have resources to disclose symptoms, express themselves, and seek help. Also, education contributes to a less stigmatizing view of mental health (Di Florio et al., 2017; Cook, and Wang, 2010). Nevertheless, our results demonstrate the family social network (cohabitants) during social isolation was a protective factor. Family social support moderates stress and increases maternal self-efficacy, reducing the risk of developing depressive symptoms during postpartum (Vaezi et al., 2019).
On the other hand, sleep disturbances during the postpartum period also have a high health impact. Pre-pandemic self-report and actigraphy studies agree that nearly 30% of women have sleep disturbances after childbirth (Nowakowski et al., 2013). As far as we know, the study by Pham et al. (2018) is the only available research which found that 29.5% of Argentinean postpartum women have sleep problems. Nonetheless, they did not use a specific instrument to evaluate insomnia.
The abrupt hormonal disruption triggered by birth and new-born sleeping/eating patterns explain the high prevalence of these disorders (Nowakowski et al., 2013). Likewise, other sleep-modifying factors are previous reproductive experiences (e.g., parity, breastfeeding practice, maternal trauma), mood state, pathologies, family support, and others, with the postpartum depression-insomnia bidirectional association being well known (Andrade Rebolledo and Vicente Parada, 2018). The insomnia frequency that we found in socially isolated women during the COVID-19 pandemic is higher than in pre-pandemic reports in other countries (Tikotzy, 2016; Belete and Misgan, 2019). Although pre-pandemic studies from Norway and the United States report similar values, they are based on different study conditions (e.g., inclusion criteria, instruments) (Dørheim et al., 2009; Swanson et al., 2011). The difference in diagnostic methods (e.g., self-report, clinic history, sleep diaries, actigraphy, polysomnography) and sample characteristics (e.g., parity, postpartum period, mode of delivery, breastfeeding practice, income level) account for this heterogeneity. Also, the increased risk of insomnia after 6 months of postpartum, whereas pre-pandemic studies report that postpartum sleep problems decline during puerperium mainly due to improved infant's sleep efficiency (Dørheim et al., 2009). The sleep conditioning during peripartum is multifactorial (Baglioni et al., 2020), which is complicated even more by the pandemic situation, with little evidence on sleep-wake patterns in infants and mothers suggesting that home confinement causes delays in sleep consolidation and fragmentation (Kahn et al., 2020). Also, family factors (infant, couple, and other relatives) influence sleep homeostasis, such as the sleep habits and health of family members, who dynamically interact with women (Saxbe et al., 2016). Furthermore, the psychological well-being of families has been affected by this pandemic (Gassman-Pines et al., 2020). For example, women with more family responsibilities exhibited negative changes in their sleep (Robillard et al., 2021). On the hand, this sleep compromise can be mitigated by promoting exclusive breastfeeding practice, as shown in our results and by other authors (Dørheim et al., 2009; Tobback et al., 2017). In this sense, babies and lactating women exhibit longer waking periods if they use formulas (Doan et al., 2014). In fact, the presence of nucleotides in human milk with hypnotic action promotes infant sleep homeostasis (Sánchez et al., 2009). Also, women who breastfeed have deeper sleep due to higher levels of circulating prolactin (Blyton et al., 2002). Thus, the psychoneuroendocrinological processes that underlie breastfeeding improve the architecture of sleep to promote recovery during postpartum, with exclusive lactating women being less overexposed to environmental and physical demands with respect to those who use formula (Montgomery-Downs et al., 2013).
The high percentage of caesarean sections found is a well-known problem in Latin America and particularly in Argentina, where they are applied in 35% of deliveries in the public sector and 70% in the private sector (Ceriani Cernadas, 2019). Furthermore, the COVID-19 pandemic and its biosecurity measures impacted obstetric practices and increased interventionism and medicalization with higher rates of caesarean sections and unnecessary interventions (Castrillo, 2020). Although it has been reported that caesarean deliveries increase the risk of postpartum depression and insomnia by enhancing stress (Xu et al., 2017), no associations were found herein. The WHO stated that “Mode of birth should be individualised, based on obstetric indications and the woman's preferences. WHO recommends that induction of labour and Cesarean sections should only be undertaken when medically justified and based on maternal and foetal condition. COVID-19 positive status alone is not an indication for the Cesarean section” (WHO, 2020a).
Given that social isolation measures negatively affected the psychological status during the COVID-19 pandemic, bivariate analyses firstly showed that the duration of isolation positively correlated with postpartum depression, insomnia, and memory complaints. Also, the restrictions to reduce COVID-19 transmission (social isolation, quarantines, social distancing, etc.) impaired family functioning, which puts the most vulnerable members (e.g. women during postpartum) at psychosocial risks (Cameron et al., 2020). This was aggravated by a decrease in access to health services during the COVID-19 pandemic (Pfefferbaum and North, 2020).
A SEM model examined complex pathways that explain with greater parsimony the mental status during social isolation of Argentinian postpartum women, supporting our hypothesis. The theoretical model explained 29% of the variability and showed validity, as it had acceptable values in the goodness of fit indices. The social isolation showed direct effects on postpartum depression and insomnia. However, postpartum depression was the variable with the strongest and most significant direct effects in the model, specifically on insomnia and the cognitive status of postpartum women. In other words, the greater the symptoms of postpartum depression, the greater the severity of insomnia, and the lower the cognitive abilities.
Moreover, postpartum depression had the strongest indirect effect on breastfeeding self-efficacy, mediated by its effect on cognitive functioning. Self-efficacy is one of the components of a person's psychological capital, and it is based on Bandura's social cognitive theory (Noel‐Weiss et al., 2006; Bandura, 1977). The breastfeeding self-efficacy theory (Dennis, 1999) applies Badura's theory to analyse women's confidence in their ability to breastfeed. Self-efficacy is essential for lactating women to have positive perceptions about their role in breastfeeding practice. If the perception of self-efficacy is high, it is more likely that the woman is engaged, effectively performing her activities, and thus positively affecting her psychological well-being. Likewise, for a person to achieve an adequate level of self-efficacy to become engaged and motivated by breastfeeding, it requires the integrity of physical, emotional, and cognitive resources (Meedya et al., 2010). This can be discussed from the theory of resource conservation, which states that a person who sees his/her resources threatened or does not have them restricts the energy he/she invests in this practice, reducing the engagement to it and consequently affecting his/her self-efficacy (Miranda et al., 2020d).
Although social isolation did not affect self-efficacy in our work, it has shown effects on emotional status and quality of sleep, which have been strong predictors of self-efficacy (both by their interactions through cognition). Furthermore, a successful breastfeeding experience is determined by the four influential sources of self-efficacy described by Bandura's theory (Brockway et al., 2017):
-
•
Performance accomplishment: It is the previous successful experiences that constitute the source of self-efficacy information, they are based on real domain experiences, repeated success in certain tasks increases positive evaluations of self-efficacy.
-
•
Vicarious experience: It consists of learning by seeing others perform a task. Therefore, lactating women would reinforce their self-efficacy based on the experiences and perceptions of other lactating women.
-
•
Social or verbal persuasion: This construct refers to the verbal expressions that provide reasons and motivation to start and continue breastfeeding, which can come from family, friends, and health professionals.
-
•
Emotional/physiological arousal: This construct refers to an individual's evaluation of the emotional and physiological state when performing a task. Pain, fatigue, anxiety, stress, and depression can be interpreted by lactating women as signs of her inadequacy.
The current study shows that self-efficacy is positively related to the practice of exclusive breastfeeding and that communication with health professionals is essential to reinforce social and verbal persuasion. Given that COVID-19-related social isolation significantly modified the ways of socializing, vicarious experiences were reduced by the ban on social meetings. Moreover, seeing other women breastfeed enhance breastfeeding, mainly in primiparous women (Bartle and Harvey, 2017). Similarly, social, or verbal persuasion can be limited; thus, emotional support and encouragement for breastfeeding women may be scarce during social isolation. Previous studies demonstrated that higher levels of support are predictive of higher levels of breastfeeding self-efficacy (McCarter-Spaulding and Gore, 2012). Although the theory of self-efficacy suggests that previous experiences favour adequate breastfeeding practice, women with previous children require special attention, as they showed low breastfeeding self-efficacy and cognitive impairment. This may be explained by the increased burden of care on women at home due to the COVID-19 pandemic (UNICEF, 2020).
Educational training sessions, one-on-one postnatal support, daily scripted telephone calls, telephone counselling, follow-up clinic visits, completing activities from a workbook, are some of the most common interventions to increase breastfeeding self-efficacy (Brockway et al., 2017). These social support networks for postpartum women should be guaranteed by the health system, adapting their strategies to the pandemic scenario. This allows addressing the mental health problems, diagnosing, and treating them early to ensure their biopsychosocial health status in a historical context of great complexity. Routine postpartum care is recommended and has different protocols and interventions (Aziz et al., 2020; Sharma et al., 2020; Werner et al., 2020), with telehealth being a feasible tool for addressing postpartum health mentally and physically.
Midwives are important agents of maternity care services, which were substantially modified by the COVID-19 pandemic, impacting on the quality of care and human rights of women and newborns: over-medicalization (e.g., Cesarean section), restrictions on services (e.g., close of infant feeding services), limitation of community services, restrictions on home births, among others (Renfrew et al., 2020). The health system must deal with this global epidemiological scenario to ensure quality and equity, with scientific evidence demonstrating that midwifery-led models of care result in excellent maternal and neonatal outcomes (Nove et al., 2018). This can respond to the high demand of maternal physical and mental health (Renfrew et al., 2020). During the COVID-19 pandemic, peripartum women require increased emotional accompaniment and support in the practice of breastfeeding (Chrzan-Dętkoś et al. 2021; Latorre et al., 2021), both covered by midwifery services (Renfrew et al., 2020). Nonetheless, it is necessary for health services to increase the midwifery workforce, since there is still a shortage of human resources worldwide (WHO, 2020b).
There were some limitations to this study. First, the cross-sectional study design does not allow assessing the direction and relation of the selected study variables over time. We recommend that future research longitudinally study the mental health of a larger sample. Also, the following questions appear: How long do the effects last? Once the restriction measures are dimmed or terminated, will the prevalences return to pre-pandemic levels? Given that second and third waves are taking place with the consequent government measures, is the impact on mental health differentiated in each outbreak? Second, other variables that were not analysed may regulate postpartum sleep quality, such as bed-sharing, sleep patterns of other family members, or the infant's medical conditions. Certain previous risk factors for depression were not collected (e.g., psychological records, loss of children, situations of abuse). Last, future studies should collect information about specific aspects of daily life that have been impacted by the pandemic, such as the consumption of psychostimulants, and mental or physical disorders. Links between mental health and unhealthy lifestyle changes are well-documented (Ryerson, 2020). Notwithstanding these limitations, our findings contribute to the available evidence and open new questions for future research in other populations, using different methodological designs and variables.
Conclusion
This is the first study addressing the mental health status of postpartum women during the preventive and mandatory social isolation in Argentina, with higher rates of postpartum depression and insomnia being found compared with pre-pandemic studies. Maternal mental health status was affected by social isolation and reproductive factors, such as late postpartum, multiparity, frequency and type of breastfeeding. Additionally, breastfeeding self-efficacy depended on mental health status, and euthymia therefore favoured the practice of exclusive breastfeeding. Women's health must be addressed by clinicians and researchers during COVID-19 pandemic, as early evaluation and promotion of mental health and breastfeeding will improve the health status of specific female populations (e.g., multiparous and advanced postpartum women, essential workers, and women without adequate social support). Also, these issues must be considered during political decision-making processes to protect the well-being of vulnerable groups. In this sense, midwives play a central role by supporting breastfeeding. Given that the current work establishes that breastfeeding is conditioned by mental health status during social isolation, findings allow midwives to be aware about special needs and risk factors that impair self-efficacy in order to follow women closely under isolation and give them additional emotional support and promote breastfeeding.
CRediT author statement
Agustín R. Miranda: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Software; Validation; Visualization; Writing - original draft; Writing - review & editing
Ana V. Scotta: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Software; Visualization; Writing - original draft; Writing - review & editing
Mariela V. Cortez: Conceptualization; Investigation; Methodology; Visualization; Writing - original draft; Writing - review & editing
Elio A. Soria: Conceptualization; Funding acquisition; Investigation; Methodology; Project administration; Resources; Supervision; Writing - original draft; Writing - review & editing
Declaration of Competing Interest
The authors declare there are no conflicts of interest.
Acknowledgments
Ethical approval
All participants consented to be included voluntarily. This research was approved by the Research Ethics Committee of the National Clinics Hospital, National University of Cordoba (registration code REPIS-3177), in accordance with the Declaration of Helsinki and current legislation.
Funding sources
Funding was provided by Secretaría de Ciencia y Tecnología, Universidad Nacional de Córdoba (grant number SECYT-UNC 273/2020).
Acknowledgments
The work of Agustín Ramiro Miranda, Ana Verónica Scotta and Mariela Valentina Cortez was supported by the fellowships provided by Secretaría de Ciencia y Tecnología, Universidad Nacional de Córdoba.
The authors gratefully acknowledge the participating women.
References
- Albougami A., Manzar M.D., Almansour A.M., Alrasheadi B.A. Metamemory and Metaconcentration Scale (MMS) for Health Professionals: A Psychometric Investigation in Nurses. Journal of Medical and Health Sciences. 2020;14(1):530–536. [Google Scholar]
- Argentine National Ministry of Health, 2020. Confirmación del primer caso importado de COVID-19 en la República Argentina. https://www.argentina.gob.ar/sites/default/files/actualizacion-epidemiologica-coronavirus-confirmacion-caso_2020.pdf
- Andrade Rebolledo, D., Vicente Parada, B. 2018. Fatiga postparto: revisión de la literatura. Revista chilena de obstetricia y ginecología, 83(2), pp. 161-169. http://dx.doi.org/ 10.4067/s0717-75262018000200161
- Aziz A., Zork N., Aubey J.J., Baptiste C.D., D’alton M.E., Emeruwa U.N., et al. Telehealth for high-risk pregnancies in the setting of the COVID-19 pandemic. Am. J. Perinatol. 2020;37(8):800–808. doi: 10.1055/s-0040-1712121. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baglioni C., Tang N.K., Johann A.F., Altena E., Bramante A., Riemann D., Palagini L. Insomnia and poor sleep quality during peripartum: a family issue with potential long term consequences on mental health. J. Matern. Fetal Neonatal Med. 2020:1–9. doi: 10.1080/14767058.2020.1854718. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol. Rev. 1977;84(2):191–215. doi: 10.1037/0033-295X.84.2.191. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Bartle N.C., Harvey K. Explaining infant feeding: The role of previous personal and vicarious experience on attitudes, subjective norms, self-efficacy, and breastfeeding outcomes. Br. J. Health Psychol. 2017;22(4):763–785. doi: 10.1111/bjhp.12254. 22https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belete H., Misgan E. Determinants of insomnia among mothers during postpartum period in Northwest Ethiopia. Sleep Disorders. 2019 doi: 10.1155/2019/3157637. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bermejo-Sánchez F.R., Peña-Ayudante W.R., Espinoza-Portilla E. Depresión perinatal en tiempos del COVID-19: rol de las redes sociales en Internet. Acta Médica Peruana. 2020;37(1):88–93. doi: 10.35663/amp.2020.371.913. http://dx.doi.org/ [DOI] [Google Scholar]
- Blyton D.M., Sullivan C.E., Edwards N. Lactation is associated with an increase in slow-wave sleep in women. J. Sleep Res. 2002;11(4):297–303. doi: 10.1046/j.1365-2869.2002.00315.x. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Brockway M., Benzies K., Hayden K.A. Interventions to improve breastfeeding self-efficacy and resultant breastfeeding rates: a systematic review and meta-analysis. J. Hum. Lact. 2017;33(3):486–499. doi: 10.1177/0890334417707957. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Cameron E., Joyce K., Delaquis C., Reynolds K., Protudjer J., Roos L.E. Maternal Psychological Distress & Mental Health Services Use during the COVID-19 Pandemic. J. Affect. Disord. 2020;276:765–774. doi: 10.1016/j.jad.2020.07.081. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canet-Juric L., Andrés M.L., del Valle M., López-Morales H., Poó F., Galli J.I., et al. A Longitudinal Study on the Emotional Impact Cause by the COVID-19 Pandemic Quarantine on General Population. Frontiers in Psychology. 2020;11:2431. doi: 10.3389/fpsyg.2020.565688. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrizo E., Domini J., Quezada R.Y.J., Serra S.V., Soria E.A., Miranda A.R. Variaciones del estado cognitivo en el puerperio y sus determinantes: una revisión narrativa. Ciência & Saúde Coletiva. 2020;25:3321–3334. doi: 10.1590/1413-81232020258.26232018. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Castrillo B. La pandemia no es excusa: parir en tiempos de derechos humanos. Avatares de la Comunicación y la Cultura. 2020;20:1–14. [Google Scholar]
- Ceriani Cernadas J.M. La epidemia de cesáreas no justificadas, ¿podremos revertirla? Archivos Argentinos de Pediatría. 2019;117(2):66–67. doi: 10.5546/aap.2019.eng.66. [DOI] [PubMed] [Google Scholar]
- Chrzan-Dętkoś M., Walczak-Kozłowska T., Lipowska M. The need for additional mental health support for women in the postpartum period in the times of epidemic crisis. BMC pregnancy and childbirth. 2021;21(1):1–9. doi: 10.1186/s12884-021-03544-8. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook T.M., Wang J. Descriptive epidemiology of stigma against depression in a general population sample in Alberta. BMC psychiatry. 2010;10(1):29. doi: 10.1186/1471-244X-10-29. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortez M.V., Miranda A.R., Scotta A.V., Aballay L.R., Soria E.A. Food patterns in Argentinian women related to socioeconomic and health factors during puerperium. Revista Médica del Instituto Mexicano del Seguro Social. 2020 doi: 10.24875/RMIMSS.M21000047. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Davenport M.H., Meyer S., Meah V.L., Strynadka M.C., Khurana R. Frontiers in Global Women's Health; 2020. Moms are not ok: COVID-19 and maternal mental health. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis C.L. Theoretical underpinnings of breastfeeding confidence: a self-efficacy framework. J. Hum. Lact. 1999;15(3):195–201. doi: 10.1177/089033449901500303. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Di Florio A., Putnam K., Altemus M., Apter G., Bergink V., Bilszta J., et al. The impact of education, country, race and ethnicity on the self-report of postpartum depression using the Edinburgh Postnatal Depression Scale. Psychol. Med. 2017;47(5):787–799. doi: 10.1017/S0033291716002087. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doan T., Gay C.L., Kennedy H.P., Newman J., Lee K.A. Nighttime breastfeeding behavior is associated with more nocturnal sleep among first-time mothers at one month postpartum. Journal of Clinical Sleep Medicine. 2014;10(3):313–319. doi: 10.5664/jcsm.3538. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dørheim S.K., Bondevik G.T., Eberhard-Gran M., Bjorvatn B. Sleep and depression in postpartum women: a population-based study. Sleep. 2009;32(7):847–855. doi: 10.1093/sleep/32.7.847. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durankuş F., Aksu E. Effects of the COVID-19 pandemic on anxiety and depressive symptoms in pregnant women: a preliminary study. J. Matern. Fetal Neonatal Med. 2020 doi: 10.1080/14767058.2020.1763946. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Fernandez-Mendoza J., Rodriguez-Muñoz A., Vela-Bueno A., Olavarrieta-Bernardino S., Calhoun S.L., Bixler E.O., Vgontzas A.N. The Spanish version of the Insomnia Severity Index: a confirmatory factor analysis. Sleep Med. 2012;13(2):207–210. doi: 10.1016/j.sleep.2011.06.019. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Gassman-Pines A., Ananat E.O., Fitz-Henley J. COVID-19 and Parent-Child Psychological Well-being. Pediatrics. 2020;146(4) doi: 10.1542/peds.2020-007294. e2020007294https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haga S.M., Ulleberg P., Slinning K., Kraft P., Steen T.B., Staff A. A longitudinal study of postpartum depressive symptoms: multilevel growth curve analyses of emotion regulation strategies, breastfeeding self-efficacy, and social support. Archives of Women's Mental Health. 2012;15(3):175–184. doi: 10.1007/s00737-012-0274-2. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Hutchens B.F., Kearney J. Risk factors for postpartum depression: an umbrella review. Journal of Midwifery & Women's Health. 2020;65(1):96–108. doi: 10.1111/jmwh.13067. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Johnson M.C., Saletti L., Tumas N. Emociones, preocupaciones y reflexiones frente a la pandemia del COVID-19 en Argentina. Ciência e Saúde Coletiva. 2020;25:2447–2456. doi: 10.1590/1413-81232020256.1.10472020. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Kahn M., Barnett N., Glazer A., Gradisar M. Infant sleep during COVID-19: longitudinal analysis of infants of US mothers in home confinement vs working as usual. Sleep Health. 2020 doi: 10.1016/j.sleh.2020.11.004. In presshttps://doi.org/ [DOI] [PubMed] [Google Scholar]
- Klusmann V., Evers A., Schwarzer R., Heuser I. A brief questionnaire on metacognition: psychometric properties. Aging Ment. Health. 2011;15(8):1052–1062. doi: 10.1080/13607863.2011.583624. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Kohlhoff J., Barnett B. Parenting self-efficacy: Links with maternal depression, infant behaviour and adult attachment. Early Hum. Dev. 2013;89(4):249–256. doi: 10.1016/j.earlhumdev.2013.01.008. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Lara M.A., Navarrete L., Navarro C., Le H.N. Evaluation of the Psychometric Measures for the Postpartum Depression Screening Scale–Spanish Version for Mexican Women. J. Transcult. Nurs. 2013;24(4):378–386. doi: 10.1177/1043659613493436. [DOI] [PubMed] [Google Scholar]
- Le H.N., Perry D.F., Ortiz G. The Postpartum Depression Screening Scale-Spanish version: examining the psychometric properties and prevalence of risk for postpartum depression. Journal of Immigrant and Minority Health. 2010;12(2):249–258. doi: 10.1007/s10903-009-9260-9. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- López Steinmetz L.C., Fong S.B., Leyes C.A., Dutto Florio M.A., Godoy J.C. General mental health state indicators in Argentinean women during quarantine of up to 80-day duration for COVID-19 pandemic. Frontiers in Global Women's Health. 2020 doi: 10.3389/fgwh.2020.580652. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein, C.A., Chervin, R.D., 2016. Use of clinical tools and tests in sleep medicine. In: Kryger M.H. (Ed.), Sleep and Breathing Disorders E-Book. Elsevier Health Sciences, Amsterdam. pp. 35-45.
- Hwang E.H., Kim K.H. Effects of Cognition, Daily-living Stress, and Health-promotion Behavior on Subjective Memory Complaints by Community-dwelling Elders. Journal of Korean Gerontological Nursing. 2019;21(3):135–143. doi: 10.17079/jkgn.2019.21.3.135. https://doi.org/ [DOI] [Google Scholar]
- Lampinen R., Vehviläinen-Julkunen K., Kankkunen P. A review of pregnancy in women over 35 years of age. The Open Nursing Journal. 2009;3:33–38. doi: 10.2174/1874434600903010033. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latorre G., Martinelli D., Guida P., Masi E., De Benedictis R., Maggio L. Impact of COVID-19 pandemic lockdown on exclusive breastfeeding in non-infected mothers. International Breastfeeding Journal. 2021;16(1):1–7. doi: 10.1186/s13006-021-00382-4. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levis B., Negeri Z., Sun Y., Benedetti A., Thombs B.D. Accuracy of the Edinburgh Postnatal Depression Scale (EPDS) for screening to detect major depression among pregnant and postpartum women: systematic review and meta-analysis of individual participant data. BMJ. 2020;371:m4022. doi: 10.1136/bmj.m4022. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manzar M.D., Salahuddin M., Khan T.A., Shah S.A., Mohammad N.S., Nureye D., et al. Psychometric Properties of a Brief Metamemory and Metaconcentration Scale in Substance Use Problem. International Journal of Mental Health and Addiction. 2020 doi: 10.1007/s11469-020-00256-6. https://doi.org/ [DOI] [Google Scholar]
- Mathisen S.E., Glavin K., Lien L., Lagerløv P. Prevalence and risk factors for postpartum depressive symptoms in Argentina: a cross-sectional study. International Journal of Women's Health. 2013;5:787–793. doi: 10.2147/IJWH.S51436. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matias T., Dominski F.H., Marks D.F. Human needs in COVID-19 isolation. J. Health Psychol. 2020 doi: 10.1177/1359105320925149. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Matthey, S., Henshaw, C., Elliott, S., Barnett, B., 2006. Variability in use of cut-off scores and formats on the Edinburgh Postnatal Depression Scale–implications for clinical and research practice. Archives of Women's Mental Health, 9(6), pp. 309-315. https://doi.org/ 10.1007/s00737-006-0152-x [DOI] [PubMed]
- McCarter-Spaulding D., Gore R. Social support improves breastfeeding self-efficacy in a sample of black women. Clinical Lactation. 2012;3(3):112–115. doi: 10.1891/215805312807022923. https://doi.org/ [DOI] [Google Scholar]
- Meedya S., Fahy K., Kable A. Factors that positively influence breastfeeding duration to 6 months: a literature review. Women and Birth. 2010;23(4):135–145. doi: 10.1016/j.wombi.2010.02.002. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Minglu L., Fang F., Guanxi L., Yuxiang Z., Chaoqiong D., Xueqin Z. Influencing factors and correlation of anxiety, psychological stress sources, and psychological capital among women pregnant with a second child in Guangdong and Shandong Province. J. Affect. Disord. 2020;264:115–122. doi: 10.1016/j.jad.2019.11.148. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Miranda A.R., Rivadero L., Serra S.V., Soria E.A. Multidomain self-report assessment of fronto-executive complaints in Spanish-speaking adults. Psychology & Neuroscience. 2020;13(3):357–374. doi: 10.1037/pne0000187. https://doi.org/ [DOI] [Google Scholar]
- Miranda A.R., Scotta A.V., Méndez A.L., Serra S.V., Soria E.A. Public Sector Workers’ Mental Health in Argentina: Comparative Psychometrics of the Perceived Stress Scale. Journal of Preventive Medicine and Public Health. 2020;53(6):429–438. doi: 10.3961/jpmph.20.229. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda A.R., Cortez M.V., Scotta A.V., Rivadero L., Serra S.V., Soria E.A. Memory enhancement in Argentinian women during postpartum by the dietary intake of lignans and anthocyanins. Nutr. Res. 2020 doi: 10.1016/j.nutres.2020.10.006. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Miranda A.R., Rivadero L., Bruera J.Á., Villarreal V., Bernio L.Y., Baydas L.A., Brizuela M.L., Serra S.V. Examining the relationship between engagement and perceived stress-related cognitive complaints in the Argentinian working population. Europe's Journal of Psychology. 2020;16(1):12–31. doi: 10.5964/ejop.v16i1.1832. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery-Downs H.E., Stremler R., Insana S.P. Postpartum sleep in new mothers and fathers. The Open Sleep Journal. 2013;6:87–97. doi: 10.2174/1874620901306010087. https://doi.org/ [DOI] [Google Scholar]
- Morin C.M., Belleville G., Bélanger L., Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. doi: 10.1093/sleep/34.5.601. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morin C.M., Carrier J. The acute effects of the COVID-19 pandemic on insomnia and psychological symptoms. Sleep Med. 2020 doi: 10.1016/j.sleep.2020.06.005. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadjafi-Semnani A., Mohammadi Y., Nadjafi-Semnani F., Nadjafi-Semnani M., Shahriyari A., Ghanbarzadeh N. Evaluation of Relation between Psychiatric Capital and Prevalence of Postpartum Anxiety and Depression in Different Health Centers of Birjand. Journal of Surgery and Trauma. 2018;6(2):66–70. [Google Scholar]
- Nanishi K., Green J., Taguri M., Jimba M. Determining a cut-off point for scores of the Breastfeeding Self-Efficacy Scale–Short Form: secondary data analysis of an intervention study in Japan. PLoS One. 2015;10(6) doi: 10.1371/journal.pone.0129698. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noel-Weiss J., Bassett V., Cragg B. Developing a prenatal breastfeeding workshop to support maternal breastfeeding self-efficacy. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2006;35(3):349–357. doi: 10.1111/j.1552-6909.2006.00053.x. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Nove A., ten Hoope-Bender P., Moyo N.T., Bokosi M. The midwifery services framework: What is it, and why is it needed? Midwifery. 2018;57:54–58. doi: 10.1016/j.midw.2017.11.003. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowakowski S., Meers J., Heimbach E. Sleep and women's health. Sleep Medicine Research. 2013;4(1):1–22. doi: 10.17241/smr.2013.4.1.1. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'hara M.W., McCabe J.E. Postpartum depression: current status and future directions. Annual Review of Clinical Psychology. 2013;9:379–407. doi: 10.1146/annurev-clinpsy-050212-185612. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Oliver-Roig A., d’Anglade-González M.L., García-García B., Silva-Tubio J.R., Richart-Martínez M., Dennis C.L. The Spanish version of the breastfeeding self-efficacy scale-short form: reliability and validity assessment. Int. J. Nurs. Stud. 2012;49(2):169–173. doi: 10.1016/j.ijnurstu.2011.08.005. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- PAHO, 2020. COVID-19: Recomendaciones para el cuidado integral de mujeres embarazadas y recién nacidos. https://www.paho.org/clap/images/PDF/COVID19embarazoyreciennacido/COVID-19_embarazadas_y_recin_nacidos_CLAP_Versin_27-03-2020.pdf?ua=1&ua=1
- Paolini C.I., Oiberman A.J., Balzano S. Factores psicosociales asociados a un alto, medio y bajo riesgo de síntomas depresivos en el posparto inmediato. Revista Brasileira de Saúde Materno Infantil. 2012;12(1):65–73. doi: 10.1590/S1519-38292012000100007. https://doi.org/ [DOI] [Google Scholar]
- Pellerin N., Raufaste E. Psychological Resources Protect Well-Being During the COVID-19 Pandemic: A Longitudinal Study During the French Lockdown. Frontiers in Psychology. 2020;11:3200. doi: 10.3389/fpsyg.2020.590276. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Pham D., Cormick G., Amyx M.M., Gibbons L., Doty M., Brown A., Norwood A., Daray F.M., Althabe F., Belizán J.M. Factors associated with postpartum depression in women from low socioeconomic level in Argentina: A hierarchical model approach. J. Affect. Disord. 2018;227:731–738. doi: 10.1016/j.jad.2017.11.091. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quelopana A.M., Champion J.D. Validación del cuestionario “Postpartum depression screening scale” versión en español en mujeres de Arica, Chile. Ciencia y Enfermería. 2010;16(1):37–47. [Google Scholar]
- Ramírez-Ortiz J., Castro-Quintero D., Lerma-Córdoba C., Yela-Ceballos F., Escobar-Córdoba F. Mental health consequences of the COVID-19 pandemic associated with social isolation. Colombian Journal of Anesthesiology. 2020;48(4) doi: 10.5554/22562087.e930. https://doi.org/ [DOI] [Google Scholar]
- Renfrew M.J., Cheyne H., Craig J., Duff E., Dykes F., Hunter B., Lavender T., Page L., Ross-Davie M., Spiby H., Downe S. Sustaining quality midwifery care in a pandemic and beyond. Midwifery. 2020;88 doi: 10.1016/j.midw.2020.102759. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robillard R., Dion K., Pennestri M.H., Solomonova E., Lee E., Saad M., Murkar A., Godbout R., Edwards J.D., Quilty L., Daros A.R., Bhatla R., Kendzerska T. Profiles of sleep changes during the COVID-19 pandemic: Demographic, behavioural and psychological factors. J. Sleep Res. 2021;30(1):e13231. doi: 10.1111/jsr.13231. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Muñoz M., Izquierdo N., Olivares M., Picos M.D.C., Rodríguez M., Herráiz M.A., Le H.N., Fonseca J. ¿Es posible el uso de la postpartum Depression Screening Scale Short Form en la depresión antenatal? Clínica y Salud. 2018;29(3):147–150. doi: 10.5093/clysa2018a21. http://dx.doi.org/ [DOI] [Google Scholar]
- Rozic P.R., Schvartzman J.A., Paolini C.I., Gadow A., Calvo D.A., Paesani F., Pieczanski P., Vázquez G.H., Lolich M., Krupitzki H.B. Detección de síntomas depresivos durante el postparto inmediato y el seguimiento a largo plazo: estabilidad temporal y factores asociados. Revista Argentina de Psiquiatría. 2012;23:409–417. [PubMed] [Google Scholar]
- Ryerson, N. C. (2020). Behavioral and Psychological Correlates of Well-Being during COVID-19. Psychological reports. https://doi.org/ 10.1177/0033294120978160 [DOI] [PubMed]
- Sánchez C.L., Cubero J., Sánchez J., Chanclón B., Rivero M., Rodríguez A.B., Barriga C. The possible role of human milk nucleotides as sleep inducers. Nutr. Neurosci. 2009;12(1):2–8. doi: 10.1179/147683009X388922. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Saxbe D.E., Schetter C.D., Guardino C.M., Ramey S.L., Shalowitz M.U., Thorp J., et al. Sleep quality predicts persistence of parental postpartum depressive symptoms and transmission of depressive symptoms from mothers to fathers. Ann. Behav. Med. 2016;50(6):862–875. doi: 10.1007/s12160-016-9815-7. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scotta A.V., Cortez M.V., Miranda A.R. Insomnia is associated with worry, cognitive avoidance and low academic engagement in Argentinian university students during the COVID-19 social isolation. Psychology, Health & Medicine. 2020 doi: 10.1080/13548506.2020.1869796. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Sharma J.B., Sharma E., Sharma S., Singh J. Recommendations for prenatal, intrapartum, and postpartum care during COVID-19 pandemic in India. Am. J. Reprod. Immunol. 2020;84(5):e13336. doi: 10.1111/aji.13336. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Sher L. COVID-19, anxiety, sleep disturbances and suicide. Sleep Med. 2020 doi: 10.1016/j.sleep.2020.04.019. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soh Y.X., Razak N.K.B.A., Cheng L.J., Lau Y. Determinants of childbirth self-efficacy among multi-ethnic pregnant women in Singapore: A structural equation modelling approach. Midwifery, 2020;87 doi: 10.1016/j.midw.2020.102716. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Swanson L.M., Pickett S.M., Flynn H., Armitage R. Relationships among depression, anxiety, and insomnia symptoms in perinatal women seeking mental health treatment. Journal of Women's Health. 2011;20(4):553–558. doi: 10.1089/jwh.2010.2371. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Tikotzky L. Postpartum maternal sleep, maternal depressive symptoms and self-perceived mother-infant emotional relationship. Behav. Sleep Med. 2016;14(1):5–22. doi: 10.1080/15402002.2014.940111. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Tobback E., Behaeghel K., Hanoulle I., Delesie L., Loccufier A., Van Holsbeeck A., et al. Comparison of subjective sleep and fatigue in breast-and bottle-feeding mothers. Midwifery. 2017;47:22–27. doi: 10.1016/j.midw.2017.01.009. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Torales J., O’Higgins M., Castaldelli-Maia J.M., Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry. 2020;66(4):317–320. doi: 10.1177/0020764020915212. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Tuthill E.L., McGrath J.M., Graber M., Cusson R.M., Young S.L. Breastfeeding self-efficacy: A critical review of available instruments. J. Hum. Lact. 2016;32(1):35–45. doi: 10.1177/0890334415599533. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF . UNICEF; Buenos Aires: 2020. Encuesta de Percepción y Actitudes de la Población. El impacto de la pandemia COVID-19 y las medidas adoptadas por el gobierno sobre la vida cotidiana. [Google Scholar]
- Vaezi A., Soojoodi F., Banihashemi A.T., Nojomi M. The association between social support and postpartum depression in women: A cross sectional study. Women and Birth. 2019;32(2):238–242. doi: 10.1016/j.wombi.2018.07.014. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Vale F.A., Balieiro-Jr A.P., Silva-Filho J.H. Memory complaint scale (MCS): Proposed tool for active systematic search. Dementia & Neuropsychologia. 2012;6(4):212–218. doi: 10.1590/S1980-57642012DN06040004. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vega-Dienstmaier J.M., Mazzotti Suarez G., Campos Sanchez M. Validación de una versión en español de la Escala de Depresión Postnatal de Edimburgo. Actas Españolas de Psiquiatría. 2002;30(2):106–111. [PubMed] [Google Scholar]
- Viaux S., Maurice P., Cohen D., Jouannic J.M. Giving birth under lockdown during the COVID-19 epidemic. Journal of Gynecology Obstetrics and Human Reproduction. 2020;49(6) doi: 10.1016/j.jogoh.2020.101785. http://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner E.A., Aloisio C.E., Butler A.D., D’Antonio K.M., Kenny J.M., Mitchell A., Ona S., Monk C. Addressing Mental Health in Patients and Providers during the COVID-19 Pandemic. Semin. Perinatol. 2020;44(7) doi: 10.1016/j.semperi.2020.151279. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO, 2020a. Clinical management of COVID-19: interim guidance, May 27 2020. https://apps.who.int/iris/handle/10665/332196
- WHO, 2020b. Nursing and midwifery, January 9, 2020. https://www.who.int/news-room/fact-sheets/detail/nursing-and-midwifery
- Xu H., Ding Y., Ma Y., Xin X., Zhang D. Cesarean section and risk of postpartum depression: a meta-analysis. J. Psychosom. Res. 2017;97:118–126. doi: 10.1016/j.jpsychores.2017.04.016. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Zanardo V., Manghina V., Giliberti L., Vettore M., Severino L., Straface G. Psychological impact of COVID-19 quarantine measures in northeastern Italy on mothers in the immediate postpartum period. International Journal of Gynecology & Obstetrics. 2020 doi: 10.1002/ijgo.13249. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zubaran C., Schumacher M.V., Foresti K., Thorell M.R., Amoretti A., Müller L. The Portuguese version of the Postpartum Depression Screening Scale-Short Form. J. Obstet. Gynaecol. Res. 2010;36(5):950–957. doi: 10.1111/j.1447-0756.2010.01282.x. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Zubaran C., Schumacher M., Roxo M.R., Foresti K. Screening tools for postpartum depression: validity and cultural dimensions. African Journal of Psychiatry. 2010;13(5) doi: 10.4314/ajpsy.v13i5.63101. http://doi.org/ [DOI] [PubMed] [Google Scholar]