Abstract
Background
Muscle invasive bladder cancer is a serious clinical problem and is fatal for the majority of patients. Alternative treatments for this condition are radical cystectomy or radical radiotherapy. The choice of treatment varies according to the resident country. The ideal treatment would be a bladder preserving therapy with total eradication of the tumour without compromising survival.
Objectives
The objective of this review was to compare the overall survival after radical surgery (cystectomy) versus radical radiotherapy in patients with muscle invasive cancer.
Search methods
We searched the Cochrane Controlled Trials Register (July 2001), MEDLINE (July 2001), EMBASE (July 2001), CancerLIT (July 2001), Healthstar (July 2001) and the Database of Abstracts of Reviews of Effectiveness (July 2001). Attempts to contact authors of unpublished data were undertaken.
Selection criteria
Randomised trials comparing surgery versus radiotherapy were eligible for assessment.
Data collection and analysis
Three reviewers assessed trial quality based on the Cochrane Guidelines. Data were extracted from the text of the article or extrapolated from the Kaplan‐Meier plot. The Peto odds ratio was determined to compare the overall survival and disease‐specific survival. Analysis was performed on an intention‐to‐treat basis and treatment actually received.
Main results
Three randomised trials comparing pre‐operative radiotherapy followed by radical cystectomy (surgery) versus radical radiotherapy with salvage cystectomy (radical radiotherapy) were eligible for assessment. These trials represented a total of 439 patients, 221 randomised to surgery and 218 to radical radiotherapy. Three trials were combined for the overall survival results and one for the disease‐specific analysis (Bloom 1982).
The mean overall survival (intention‐to‐treat analysis) at 3 and 5 years were 45% and 36% for surgery, and 28% and 20% for radiotherapy, respectively. Peto odds ratio (95% confidence interval) analysis consistently favoured surgery in terms of overall survival. The results were significantly in favour of surgery at 3 years (OR = 1.91, 95% CI 1.30 to 2.82) and at 5 years (OR = 1.85 95% CI 1.22 to 2.82).
On a 'treatment received' basis, the results were significantly in favour of surgery at 3 (OR = 1.84, 95% CI 1.17 to 2.90) and 5 years (OR = 2.17, 95% CI 1.39 to 3.38) for overall survival and at 3 years (OR = 1.96, 95% CI 1.06 to 3.65) for disease‐specific survival.
Authors' conclusions
The analysis of this review suggests that there is an overall survival benefit with radical surgery compared to radical radiotherapy in patients with muscle‐invasive bladder cancer. However, it must be considered that only three trials were included for analysis, the patients numbers were small and that many patients did not receive the treatment they were randomised to. It must also be noted that many improvements in both radiotherapy and surgery have taken place since the initiation of these trials.
Keywords: Female, Humans, Male, Confidence Intervals, Odds Ratio, Randomized Controlled Trials as Topic, Salvage Therapy, Survival Analysis, Urinary Bladder Neoplasms, Urinary Bladder Neoplasms/mortality, Urinary Bladder Neoplasms/radiotherapy, Urinary Bladder Neoplasms/surgery
Plain language summary
Major bladder surgery improves chances of survival for people with bladder cancer that has invaded the muscle, but more studies are needed
Bladder cancer is common worldwide. In rare cases, cancer spreads to the bladder muscle. A combination of surgery and radiation therapy (radiotherapy) is used to try to treat bladder cancer that has invaded the muscle. One treatment involves some radiotherapy, followed by major surgery to remove the bladder. Another treatment uses intensive radiotherapy, followed by smaller surgery if needed. However, it is not clear which treatment offers people the best chance of survival. The review found that survival was better in people receiving major surgery, compared with major radiotherapy although recent surgical and radiotherapy advances have not yet been studied.
Background
The standard therapy in many countries, including the United States, for T2/T3 N0 (UICC stage) muscle invasive transitional cell carcinoma of the bladder is primary radical cystectomy . However, in a number of Oncology Centres in the UK and Canada, a policy of bladder conservation has been pursued for many years. This involves a course of radical radiotherapy treatment to the bladder followed by close observation and salvage cystectomy, if required. This policy has recently been questioned since it has been suggested that the results of radical radiotherapy are inferior to primary cystectomy. In addition, the operative mortality from radical cystectomy has decreased in recent years, and there are now alternative methods to avoid urinary diversion such as reconstructive surgery and the construction of a 'neo‐bladder'.
The possibility that radiotherapy may be less effective than surgery has arisen partly because in some published non‐randomised clinical trials, radiotherapy appears to result in a poorer overall survival than surgery. However, this difference in overall survival may be attributable to a number of confounding factors, including selection bias. For example, patients undergoing cystectomy are likely to be younger and fitter than those having radiotherapy. Secondly, their tumours are likely to be staged pathologically rather than clinically, which usually results in an increase in the assigned stage for some patients. The equivalence of radiotherapy and surgery in achieving tumour control is however, supported by a study from the UK (Duncan 1986). Here radiotherapy was given to all patients as a departmental policy, hence selection bias was mostly avoided. In this series, of almost one thousand patients, overall survival was comparable with that achieved by surgery.
A number of clinical trials (Miller 1977; Sell 1991) where a strategy of preoperative radiotherapy and immediate cystectomy was compared to a full course of radical radiotherapy with surgical salvage, showed no statistically significant difference in overall survival between the two arms. However, there appear to be no data available where surgery alone and radiotherapy have been compared in randomised controlled trials.
Our goal was to conduct a systematic review and, if possible, a meta‐analysis to evaluate the impact of surgery or radiotherapy on survival in patients with muscle invasive bladder cancer.
Objectives
The aim of this review is to define the overall survival and disease‐specific survival in patients with localised muscle invasive bladder cancer receiving radical cystectomy or radical radiotherapy. A secondary objective is to evaluate trials where preoperative radiotherapy and immediate cystectomy were compared to a course of radical radiotherapy with surgical salvage.
Methods
Criteria for considering studies for this review
Types of studies
All randomized and quasi‐randomised controlled clinical trials comparing primary surgery with radical radiotherapy in bladder cancer patients whose tumours have locally invaded the muscle wall were eligible. All randomised trials in patients receiving preoperative radiotherapy and immediate cystectomy or radical radiotherapy with surgical salvage were eligible.
Types of participants
Both male and female patients of any age with histologically proven transitional cell carcinoma of the bladder were studied. Eligible patients will have stage T2 to T4a NO MO as defined by the UICC TNM staging criteria.
Types of interventions
All randomised studies comparing radical cystectomy (with or without preoperative radiotherapy) to radiotherapy with surgical salvage.
Types of outcome measures
The primary outcome measure was the efficacy of treatment as measured by overall survival and disease‐specific survival. Secondary outcomes included treatment morbidity.
Search methods for identification of studies
The electronic database MEDLINE was searched from 1966 to July 2001 using the following strategy:
randomized controlled trial.pt.
controlled clinical trial.pt.
randomized controlled trials.sh.
random allocation.sh.
double blind method.sh.
single‐blind method.sh.
or/1‐6
(animal not human).sh.
7 not 8
clinical trial.pt.
exp clinical trials/
(clin$adj25 trial$).tw.
((singl$ or doubl$ or trebl$ or tripl$) ajd25 (blind$ or mask$)).tw
placebos.sh.
placebo$.tw.
random$tw.
research design.sh.
or/10‐17
18 not 19
19 not 9
comparative study.sh
exp evaluation studies/
follow up studies.sh.
prospective studies.sh.
(control$ or propectiv$ or volunteer$).tw.
or/21‐25
26 not 8
26 not (9 or 20)
9 or 20 or 28
exp bladder neoplasms/
(bladder adj4 cancer$).tw.
(bladder adj4 neoplas$).tw.
(bladder adj4 carcinoma$).tw.
or 30‐33
exp radiotherapy/
rt.fs.
irradiat$.tw.
radiation.tw
or/35‐38
cystectomy/
exp urologic surgical procedures/
exp surgery/
su.fs.
cystectomy.tw.
or/40‐44
29 and 34 and 39 and 45
CancerLIT, EMBASE, DARE (Database of Abstracts of Reviews of Effectiveness) and the Cochrane Controlled Clinical Trials Register were also searched to identify all relevant randomised clinical trials. There were no language restrictions. Investigators carrying out ongoing trials were contacted for availability of unpublished data. The bibliography of retrieved articles were scrutinised for additional randomised controlled trials or meta‐analyses.
Data collection and analysis
Information on patients, interventions and outcomes were extracted and evaluated against the inclusion criteria. The methodology quality was assessed by the allocation concealment method (Cochrane Collaboration Handbook). Quantitative outcomes were evaluated using the Peto odds ratio (Cochrane statistics package Revman.4.1). Survival data were extracted either from the text or extrapolated from the presented Kaplan‐Meier plots. Peto odds ratios and their 95% confidence intervals were determined for both overall and disease‐specific survival data at 3, 5 and 10 years.
Results
Description of studies
See: Table of included studies.
A total of 571 citations were retrieved from the literature search. These were categorised as 'A' relevant, 'B' reviews and 'C' not relevant. After screening the 'A' category containing 217 references, 6 articles describing relevant randomised trials were obtained: (Bloom 1982; Wallace1976; Horwich 1999; Miller 1973; Miller 1977; Sell 1991). One reference, Miller 1973, was excluded from the analysis as this was an initial report of Miller 1977. Wallace1976 and Bloom 1982 reported on the same trial and patients, however, Wallace1976 presented overall survival only and Bloom 1982 presented disease‐specific survival only. Therefore both reports were included for analysis using their respective outcomes. The long‐term (10 year) disease‐specific survival data for the Bloom 1982 study was reported by Horwich 1999. For simplicity, this trial will generally be referred to as Bloom 1982 unless otherwise specified. The three included trials (Miller 1977; Bloom 1982; Sell 1991) all randomised patients with invasive bladder cancer (T2 to T4) to either preoperative radiotherapy followed by radical cystectomy or radical radiotherapy followed by salvage cystectomy. No trials addressed our primary objective evaluating radical cystectomy alone versus radical radiotherapy.
In the Bloom 1982 study, preoperative radiation treatment consisted of 4000 cGy in 4 weeks to the whole pelvis followed 4 weeks later by cystectomy (method not stated). The radical radiotherapy schedule was 4000 cGy in 4 weeks plus a 2000 cGy boost in 2 weeks to the bladder and perivesical tissue. Eighteen patients had salvage cystectomy for recurrent or residual tumour.
In the Miller 1973 study the preoperative and radical radiotherapy schedules were 5000 cGy in 25 fractions over 5 weeks and 7000 cGy in 35 fractions over 7 weeks, respectively. Radical cystectomy consisted of radical cystoprostatectomy (anterior pelvic exenteration in women) and bilateral ureto‐ileostomy with no node dissection. Two patients underwent salvage cystectomy following radical radiotherapy.
The study of Sell 1991 employed radiotherapy to the whole pelvis with rectal shielding using schedules of 4000 cGy in 20 fractions over 5 weeks (pre‐operative) and a total dose of 6000 cGy (radical). Cystectomy was performed according to the method of Whitmore 1977, which included cystoprostatectomy plus pelvic lymph node dissection, and diversion as an ileal conduit. A nerve‐sparing procedure was carried out in 9 patients from the radical cystectomy group and 2 from the radical radiotherapy group.
Risk of bias in included studies
Bloom 1982 and Miller 1977 did not specify the method of randomisation whereas Sell 1991 employed the method reported by Zelen 1979.
Effects of interventions
For purposes of analysis, preoperative radiotherapy plus radical cystectomy was considered the experimental group, abbreviated to 'surgery', therefore an odds ratio of greater than one would indicate a beneficial effect of surgery. The radical radiotherapy plus salvage cystectomy group was abbreviated to 'radiotherapy'. The three included trials represented a total of 439 patients with invasive bladder cancer ('Table 1' ‐ 'Characteristics of included studies'). Two hundred and twenty‐one patients were randomised to the surgery arm and 218 to the radiotherapy arm. However, not all the patients received the protocol treatment after randomisation. In the Bloom study, 21 patients (15 surgery and 6 radiotherapy) did not complete the allocated protocol treatment due to medical unfitness or the development of metastatic disease. In the study by Miller, 5 patients did not receive cystectomy (surgery) due to metastatic disease. Twenty‐nine patients in the Sell study did not receive the protocol treatment (22 surgery and 5 radiotherapy) because of refusal or lack of adherence to the protocol. All these patients were excluded from the ITT group and considered as the ' treatment received' group and numbered in total 378, with 173 randomised to surgery and 205 to radiotherapy. All three studies reported data on an intention‐to‐treat (ITT) and treatment received basis. Wallace1976 (same study as Bloom), Miller 1977 and Sell 1991 reported overall survival, whilst Bloom 1982 only reported disease‐specific survival.
1. Patient number based on Intention‐To‐Treat or actual Treatment Received.
| Trial | Intention‐To‐Treat | Treatment received |
| Total Surgery Radiotherapy | Total Surgery Radiotherapy | |
| Bloom 1982 | 189 98 91 | 162 66 88 |
| Miller 1977 | 67 35 32 | 62 30 32 |
| Sell 1991 | 183 88 95 | 154 66 88 |
| totals | 439 221 218 | 378 173 205 |
The pooled overall survival at 3 years on an ITT basis was 45% for surgery and 28% for radiotherapy, giving an absolute improvement of 17% and at 5 years the respective values were 36% and 20% (absolute improvement of 16%). On a 'treatment received' basis the overall survival at 3 years was 47% (surgery) and 32% (radiotherapy), and at 5 years were 41% (surgery) and 21% (radiotherapy).
The ITT analysis for overall survival at 3 and 5 years favoured surgery over radiotherapy and was statistically significant at 3 years with an odds ratio (95% confidence interval) = 1.91 (1.30 ‐ 2.82) and at 5 years OR = 1.85 (1.22 ‐ 2.82). The corresponding ratios for 'treatment received' were also significantly in favour of surgery at 3 years OR = 1.84 (1.17 to 2.90) and at 5 years 2.17 (1.39 to 3.38).
For the Bloom 1982 study, the disease‐specific survival on an ITT basis at 3, 5 and 10 years for surgery were 45%, 38% and 30% and for radiotherapy were 33%, 29% and 20% (the 10 year values were reported by Horwich 1999). On a 'treatment received' basis, the disease‐specific survival at 3 and 5 years was 53% and 44% (surgery) and 36% and 31% (radiotherapy). No 10‐year data were reported.
The odds ratios (95% confidence interval) for disease‐specific survival on an ITT basis as reported by Bloom 1982 at 3, 5, and 10 years were respectively 1.65 (0.92 to 2.95), 1.38 (0.75 to 2.54) and 1.77 (0.92 to 3.40), in favour of surgery but not statistically significant. The ratios for the 'treatment received' group at 3 and 5 years (no data are available for 10 years of follow up) were 1.96 (1.06 to 3.65) and 1.78 (0.94 to 3.37), respectively.
No toxicity data were reported in the Bloom 1982 study. Miller 1977 did not report treatment complications for the randomised study included in this review, but did report on 724 patients receiving radiation therapy for carcinoma of the urinary bladder at the M.D. Anderson Hospital and Tumour Institute between 1954 and 1970. In 533 patients receiving definitive radiation (7000 cGy in 35 fractions over 7 weeks) the complication rate was 14% with a mortality rate of 4%. The most common major sites of complication were bladder (27%), rectum (13%) and renal (10%). For 125 patients receiving pre‐operative radiation and cystectomy the complication rate was 48%. The most common complications were wound infection and/or dehiscence (18%), ureto‐ileal obstruction or leakage (10%), pyelonephritis (10%) and bowel fistula or obstruction (9 and 8%).
The most frequent early side effect for both radical and pre‐operative radiation therapy in the Sell 1991 study was diarrhoea, requiring medical attention in 20% of patients. One third in each group experienced urinary frequency and dysuria. Early complications of radical cystectomy were cicatricial rupture (5%), intestinal fistula (5%), urinary fistula (5%), wound infection (3%), haematoma (3%), pelvic abscess (3%) and defecatory problems (3%). Ileus (5%) was the main early complication of pre‐operative radiotherapy. Thirty‐eight percent of early complications following cystectomy needed treating compared to 30% following salvage cystectomy. The major late complication following radical radiotherapy was contracted bladder (10%), whereas late rectal complications were observed in 30% of patients receiving radical radiotherapy compared to 36% in the cystectomy group. Additionally, all male patients following radical cystectomy experienced impotence whereas 41% of patients following radical radiotherapy could practice normal coitus.
Discussion
The prognosis for invasive bladder is poor with 5 year survival ranging between 20% to 50%. Our knowledge of the genetic and molecular mechanisms of bladder cancer have increased considerably in recent years, but this has not yet been translated in to improved survival figures. Many urologists consider cystectomy to be generally indicated for patients with muscle invasive tumours (Turner 1999). However, the ideal treatment for this disease would be to totally eradicate the tumour whilst preserving bladder and sexual function. Bladder‐sparing radical radiotherapy may be just as effective as surgery in terms of patient survival (Tsujii 1998).
The literature search in the present study (1966 to July 2000), did not identify any randomised controlled trials comparing primary cystectomy with definitive radiotherapy for invasive bladder cancer. Three randomised trials were found that compared pre‐operative radiotherapy followed by radical cystectomy (surgery) versus radical radiotherapy with salvage cystectomy (radiotherapy). Analysis of these three studies indicated that overall survival at 3 and 5 years was significantly better with surgery in the 'intention‐to‐treat' group and in the 'treatment received' group.
Disease‐specific survival is an assessment of treatment efficacy which eliminates confounding factors due to other causes of death, in an ostensibly elderly population. In the present analysis, a substantial number of patients (14 %) did not receive the treatment they were randomised to receive. Although in both the 'intention‐to‐treat' and the 'treatment received' analysis the odds ratios were in favour of surgery, it was only significant at 3 years for the latter group.
An attempt to contact the author, SD Cutler of the National Bladder Cancer Group, cited as a personal communication in a review by Scher 1997 has so far proved unsuccessful. It was reported in this review that T2 to T4a bladder cancer patients were randomised to 50 Gy followed by cystectomy (37 patients ) or 60 Gy to 80 Gy plus salvage cystectomy (35 patients). The 5 years survival rates were 27% and 40%, respectively. Although these figures support the view that radical radiotherapy provides a better outcome in terms of survival, it was considered inappropriate to include these data in the present review because there was insufficient trial information and the data were not first hand. We will continue our attempts to contact SD Cutler and if successful will include the results in an update of this review. We have also been unable to obtain individual patient data on the three included trials, to perform an updated meta‐analysis. The results are therefore based on published data.
Authors' conclusions
Implications for practice.
Based on the review of three randomised trials, comparing pre‐operative radiotherapy with radical radiotherapy followed by salvage cystectomy and the results of our subsequent meta‐analysis, we consider that the evidence consistently favours surgery in terms of survival. However, it must also be considered that the randomised trials evaluated in this analysis were not recent and that major advances have been made since these trials commenced in both surgery (with respect to neobladder construction), and radiotherapy and include areas such as CT planning, higher dose delivery, conformal radiotherapy and supportive care.
Implications for research.
Taking into account the poor 5 year survival figures for invasive bladder cancer and the limited data available, we would propose that a further randomised trial of sufficient power be undertaken to provide convincing evidence that one modality is superior. Although radical radiotherapy showed a reduced overall and disease‐specific survival in the present review, it is uncertain whether the optimal treatment conditions were used because of the variation in dose and schedule given in these studies. Future randomised trials with radiotherapy in invasive bladder cancer, using modern doses, schedules and planning techniques, should provide a more realistic comparison with radical cystectomy.
What's new
| Date | Event | Description |
|---|---|---|
| 5 March 2012 | Amended | Linked various references and 'Table 1'. |
History
Protocol first published: Issue 2, 2000 Review first published: Issue 3, 2001
| Date | Event | Description |
|---|---|---|
| 28 May 2008 | Amended | Converted to new review format. |
| 22 August 2001 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
We are extremely grateful for the expert librarian skills of Mrs Bernadette Coles M.Sc for developing the search strategy and under taking the searches of all the databases. Thanks go to Dr Jon Court for his comments on the manuscript.
Data and analyses
Comparison 1. Preoperative Radiotherapy plus Cystectomy versus Radical Radiotherapy plus Salvage Cystectomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 overall survival at 3 years: intention to treat analysis | 3 | 439 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.91 [1.30, 2.82] |
| 2 overall survival at 5 years: intention to treat analysis | 3 | 439 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.85 [1.22, 2.82] |
| 3 overall survival at 3 years: treatment received analysis | 2 | 316 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.84 [1.17, 2.90] |
| 4 overall survival at 5 years: treatment received analysis | 3 | 378 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.17 [1.39, 3.38] |
| 5 disease‐specific survival at 3 years: intention to treat analysis | 1 | 189 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.65 [0.92, 2.95] |
| 6 disease‐specific survival at 5 years: intention to treat analysis | 1 | 189 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.38 [0.75, 2.54] |
| 7 disease‐specific survival at 10 years: intention to treat analysis | 1 | 189 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.77 [0.92, 3.40] |
| 8 disease‐specific survival at 3 years: treatment received analysis | 1 | 162 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.96 [1.06, 3.65] |
| 9 disease‐specific survival at 5 years: treatment received analysis | 1 | 162 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.78 [0.94, 3.37] |
1.1. Analysis.
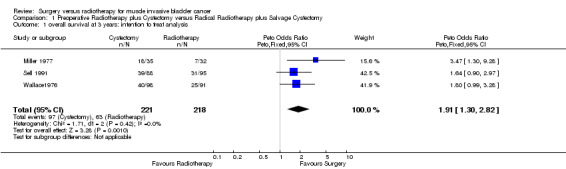
Comparison 1 Preoperative Radiotherapy plus Cystectomy versus Radical Radiotherapy plus Salvage Cystectomy, Outcome 1 overall survival at 3 years: intention to treat analysis.
1.2. Analysis.

Comparison 1 Preoperative Radiotherapy plus Cystectomy versus Radical Radiotherapy plus Salvage Cystectomy, Outcome 2 overall survival at 5 years: intention to treat analysis.
1.3. Analysis.

Comparison 1 Preoperative Radiotherapy plus Cystectomy versus Radical Radiotherapy plus Salvage Cystectomy, Outcome 3 overall survival at 3 years: treatment received analysis.
1.4. Analysis.

Comparison 1 Preoperative Radiotherapy plus Cystectomy versus Radical Radiotherapy plus Salvage Cystectomy, Outcome 4 overall survival at 5 years: treatment received analysis.
1.5. Analysis.

Comparison 1 Preoperative Radiotherapy plus Cystectomy versus Radical Radiotherapy plus Salvage Cystectomy, Outcome 5 disease‐specific survival at 3 years: intention to treat analysis.
1.6. Analysis.

Comparison 1 Preoperative Radiotherapy plus Cystectomy versus Radical Radiotherapy plus Salvage Cystectomy, Outcome 6 disease‐specific survival at 5 years: intention to treat analysis.
1.7. Analysis.

Comparison 1 Preoperative Radiotherapy plus Cystectomy versus Radical Radiotherapy plus Salvage Cystectomy, Outcome 7 disease‐specific survival at 10 years: intention to treat analysis.
1.8. Analysis.

Comparison 1 Preoperative Radiotherapy plus Cystectomy versus Radical Radiotherapy plus Salvage Cystectomy, Outcome 8 disease‐specific survival at 3 years: treatment received analysis.
1.9. Analysis.

Comparison 1 Preoperative Radiotherapy plus Cystectomy versus Radical Radiotherapy plus Salvage Cystectomy, Outcome 9 disease‐specific survival at 5 years: treatment received analysis.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bloom 1982.
| Methods | Multicenter prospective randomised trial ‐ method not stated | |
| Participants | 189 patients T3 or B2C bladder cancer treated from 1966 ‐ 1975 | |
| Interventions | pre‐operative radiotherapy ‐4000 cGy in 4 weeks (whole pelvis) plus elective cystectomy versus radical radiotherapy ‐4000 cGy in 4 weeks plus 2000 cGy boost with salvage cystectomy | |
| Outcomes | disease‐specific survival. analysed on an intention‐to‐treat basis (n = 189) and according to treatment received (n = 162) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Horwich 1999.
| Methods | Same trial as Bloom1982 | |
| Participants | ||
| Interventions | ||
| Outcomes | 10‐year disease‐specific survival. analysed on an intention‐to‐treat | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Miller 1977.
| Methods | Randomised prospective study ‐ method not stated | |
| Participants | 68 patients with B‐2 or C (primary or secondary) bladder cancer treated from 1964 to 1970 | |
| Interventions | preoperative radiotherapy of 5000 cGy in 25 fractions over 5 weeks plus radical cystectomy versus definitive radiotherapy 7000 cGy in 35 fractions over 7 weeks plus salvage cystectomy | |
| Outcomes | overall survival analysed on an intention‐to‐treat basis (n = 67) and according to treatment received (n = 62) | |
| Notes | I patient lost after randomised to preoperative radiotherapy plus cystectomy group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Sell 1991.
| Methods | Multicenter prospective randomised trial ‐ randomisation according to the method of Zelen 1979 | |
| Participants | 183 patients with T2 ‐T4a bladder tumours treated from 1983 ‐ 1986 | |
| Interventions | preoperative radiotherapy of 4000 cGy in 20 fractions (5 per week) plus cystectomy versus radical radiotherapy 6000 cGy (total dose) | |
| Outcomes | overall survival analysed on an intention‐to‐treat basis (n = 183) and according to treatment received (n = 154) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Wallace1976.
| Methods | Earlier report of Bloom 1982 | |
| Participants | ||
| Interventions | ||
| Outcomes | Overall survival. analysed on an intention‐to‐treat basis (n = 189) and according to treatment received (n = 162) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Miller 1973 | Initial report of Miller 1977 |
Contributions of authors
Mike D Shelley: primary contact, literature search and screen, protocol, data extraction, analysis, draft manuscript, quality assessment
Jim Barber: concept, protocol, screen literature search, analysis review, manuscript review, quality assessment
Timothy J Wilt: protocol review, analysis review, manuscript review,
Malcolm D Mason: secondary contact, concept, quality assessment, analysis review, manuscript review
Sources of support
Internal sources
Velindre NHS Trust Hospital, UK.
Minneapolis VA Center for Chronic Disease Outcomes Research, USA.
External sources
No sources of support supplied
Declarations of interest
None.
Edited (no change to conclusions)
References
References to studies included in this review
Bloom 1982 {published data only}
- Bloom HJ, Hendry WF, Wallace DM, Skeet RG. Treatment of T3 bladder cancer: controlled trial of pre‐operative radiotherapy and radical cystectomy versus radical radiotherapy. British Journal of Urology 1982;54(2):136‐51. [DOI] [PubMed] [Google Scholar]
Horwich 1999 {published data only}
- Horwich A. Commentary 1. In: Hall RR editor(s). Cinical management of bladder cancer. London: Arnold, 1999:236‐8. [Google Scholar]
Miller 1977 {published data only}
- Miller LS. Bladder cancer: superiority of preoperative irradiation and cystectomy in clinical stages B2 and C. Cancer 1977;138:193‐201. [DOI] [PubMed] [Google Scholar]
Sell 1991 {published data only}
- Sell A, Jacobson A, Nerstrom B, Sorensen BL, Steven K, Barlebo H. Treatment of advanced bladder cancer category T2 T3 and T4. A randomized multicenter study of preoperative irradiation and cystectomy versus radical irradiation and early salvage cystectomy for residual tumour. DAVECA protocol 8201. Scandinavian Journal of Urology and Nephrology 1991;138(Suppl):192‐201. [PubMed] [Google Scholar]
Wallace1976 {published data only}
- Wallace DM, Bloom HJG. The management of deeply infiltrating (T3) bladder carcinoma: Controlled trial of radical radiotherapy versus preoperative radiotherapy and radical cystectomy (First Report). British Journal of Urology 1976;48:587‐94. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Miller 1973 {published data only}
- Miller LS, Johnson DE. Megavoltage irradiation for bladder cancer: Alone, postoperative, or preoperative. Seventh National Cancer Conference Proceedings 1973:771‐82. [PubMed] [Google Scholar]
Additional references
Duncan 1986
- Duncan W, Quilty PM. The results of a series of 963 patients with transitional cell carcinoma of the urinary bladder primarily treated by radical megavoltage X‐ray therapy.. Radiotherapy & Oncology 1986;7(4):299‐310. [DOI] [PubMed] [Google Scholar]
Scher 1997
- Scher HI, Shipley WU, Herr H. Cancer of the bladder. In: DeVita VT, Hellman S, Rosenberg SA editor(s). Cancer Principles & Practice of Oncology. 5th Edition. Vol. 1, Philadelphia: Lippencott‐Raven, 1997:1300‐22. [Google Scholar]
Tsujii 1998
- Tsujii H, Gospodarowicz MK, Bolla M, Fujita K, M'Liss Hudson M, Mitsuhashi N, Roberts JT, Shimazaki J. The place of radiotherapy for localized invasive bladder cancer. Urologic Oncology 1998;4:153‐4. [DOI] [PubMed] [Google Scholar]
Turner 1999
- Turner WH, Studer UE. Cystectomy, bladder reconstruction, urinary diversion and stomatherapy. In: Hall RR editor(s). Clinical Management of Bladder Cancer. London: Arnold, 1999:171‐211. [Google Scholar]
Whitmore 1977
- Whitmore WF, Batata MA, Ghoneim MA, Grabstrald H, Unol A. Radical cystectomy or without prior irradiation in the treatment of bladder cancer. Journal of Urology 1977;300:1242‐5. [DOI] [PubMed] [Google Scholar]
Zelen 1979
- Zelen M. A new design for randomised clinical trials. New England Journal of Medicine 1979;300:1242‐5. [DOI] [PubMed] [Google Scholar]


