Abstract
Background
Proton pump inhibitors (PPIs) are associated with microbiome changes of the gut, which in turn may affect the progression of colorectal cancer (CRC). This study aims to assess the associations between PPI use and all-cause and CRC-specific mortality.
Methods
We selected all patients registered in the Swedish Prescribed Drug Registry who were diagnosed with CRC between 2006 and 2012 (N = 32,411, 54.9% PPI users) and subsequently followed them through register linkage to the Swedish Causes of Death Registry until December 2013. PPI users were patients with ≥1 post-diagnosis PPI dispensation. Time-dependent Cox-regression models were performed with PPI use as time-varying exposure.
Results
Overall 4746 (14.0%) patients died, with an aHR of 1.38 (95% CI 1.32–1.44) for all-cause mortality comparing PPI users with PPI nonusers. Higher-magnitude associations were observed among male, cancer stage 0−I, rectal cancer and patients receiving CRC surgery. The PPI-all-cause mortality association was also more pronounced comparing new users to non-users (aHR = 1.47, 95%CI 1.40–1.55) than comparing continuous users to non-users (aHR = 1.32, 95%CI 1.24–1.39). The risk estimates for CRC-specific mortality comparing PPI users to PPI nonusers were similar to those for all-cause mortality.
Conclusion
PPI use after the CRC diagnosis was associated with increased all-cause and CRC-specific mortality.
Subject terms: Gastrointestinal cancer, Epidemiology
Background
Proton pump inhibitors (PPIs) are among the most frequently prescribed drugs worldwide, used in up to 11–30% of all adults [1–3]. Yet, the safety of prolonged PPI use has been increasingly questioned because of the potential carcinogenic effects and other major health complications [4, 5]. PPIs could alter the richness and diversity of the gut microbiota, which effect potentially exceeds the influence of antibiotics on dysbiosis on the population level [6]. Since gut dysbiosis could contribute to the intestinal tumour growth according to evidence from preclinical studies [7], PPIs may play a role in the occurrence and prognosis of colorectal cancer (CRC).
A few epidemiological studies have examined the association between PPI use and the risk of developing CRC. Some studies found PPI use was related to an increased risk of developing CRC [8–10], while other studies indicated the absence of an association [11–15]. However, little is known on PPIs and survival of CRC. One Canadian cohort study showed that PPI use was associated with 34% increased all-cause mortality [16], while a Danish cohort study reported 44% increased CRC-specific mortality associated with PPI use [17]. Nonetheless, the previous studies assessing the impact of PPI on survival of CRC shared several limitations: potential confounding by indication and major effect modifications were insufficiently assessed; immortal time bias and protopathic bias were not controlled appropriately; and lastly, dose–response associations between the dose of PPIs and mortality have not been examined.
This nationwide cohort study of Swedish patients with CRC aims to assess the associations between PPI use and all-cause or CRC-specific mortality while taking into account potential confounding by indication, modifying effects of CRC-related factors, timing of PPI initiation and PPI dosage.
Methods
Data sources
This population-based cohort includes all Swedish residents who had at least one prescription of selected commonly prescribed drugs, covering ~85% of the Swedish population, as described in detail elsewhere [18–22]. The study population comprised all adults (age≥18) within the cohort, who had a first-time CRC diagnosis (International Classification of Diseases—ICD-10 codes: C18-C20, adenocarcinoma, histology code 096) during the period January 1, 2006–December 31, 2012.
Exposure
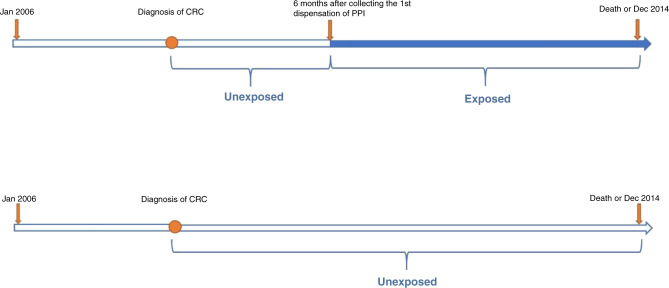
PPI users were patients who had at least one PPI dispensation after CRC diagnosis, as identified by the Anatomical Therapeutic Chemical classification system (ATC) code A02BC in the Swedish Prescribed Drug Registry [23], and PPI nonusers were those without a recorded PPI dispensation after diagnosis. If we considered PPI users as being exposed from the diagnosis of CRC, immortal time bias would be introduced because death cannot occur before receiving the first PPI dispensation after diagnosis [24]. Additionally, it is of great significance to account for a latency period of the drug effect and reduce the potential protopathic bias (reverse causality) [25]. Therefore, we applied a lag-time of 6 months as recommended in the literature [26, 27]. Consequently, PPI users were considered as unexposed from the diagnosis of CRC to six months after first post-diagnosis PPI dispensation (Fig. 1).
Fig. 1. Timing of the use of proton pump inhibitors (PPIs) in relation to the diagnosis of colorectal cancer (CRC).
PPI users were patients who had at least one PPI dispensation after the diagnosis of CRC; PPI nonusers were patients not having PPI dispensation after the diagnosis of CRC.
For analyses of the potential influence of PPI initiation before CRC diagnosis, we further divided PPI users into continuous users and new users based on if they received PPI dispensation before CRC diagnosis and after July 2005 (start of the Swedish Prescribed Drug Registry). The two subgroups of PPI users were also considered as time-dependent variables.
The cumulative dose of PPI use was defined as the cumulative defined daily dose (DDD) per package received from the date of the first PPI dispensation after diagnosis to the end of the study, and the average daily dose was calculated as the cumulative DDD divided by the survival time (days counted from the diagnosis to death or the end of the study).
Outcome
We followed all patients from the first date of CRC diagnosis to the date of death or the end of study period (December 31, 2013), whichever came first. The primary outcome of the study was all-cause mortality. The secondary outcome was CRC-specific mortality, of which the cause of death was identified by ICD-10 codes of C18-C20 in the Swedish Causes of Death Registry [28].
Covariates
We identified the diagnosis of CRC and retrieved sex, age at diagnosis, tumour site, tumour stage, and administration of CRC surgery after diagnosis from the Swedish Cancer Registry, of which ≥98% of all cancer cases were morphologically verified [29]. We categorised age at diagnosis into three distinct groups: 18–65, 65–75 and > = 75 years. We grouped the tumour site into colon (ICD-10 code: C18) and rectum (ICD-10 codes: C19 and C20). We classified the tumour-node-metastasis (TNM) stage into stage 0 + I (Tis, N0, M0 for stage 0; T1 or T2, N0, M0 for stage I), stage II (T3 or T4, N0, M0), stage III (T1–4, N1–2, M0), stage IV (any T, any N, M1) based on the 6th version of American Joint Committee on Cancer Staging Manual [30]. We identified the administration of CRC-surgery through NOMESCO Classification of Surgical Procedures (NCSP) codes of JFB, JFH and JGB [31].
We identified the acid-related indications as having at least one recorded diagnosis of gastroesophageal reflux (ICD-10 code: K20–K21, K44, R12), peptic ulcer (ICD-10 code: K25–K27) or gastroduodenitis (ICD-10 code: K29) in the Swedish Patient Registry. We also considered maintenance use of low-dose aspirin or nonaspirin NSAIDs as indications for PPI use since they are often administered simultaneously with PPI to protect the gastric mucosa and could have a protective effect on CRC risk and prognosis [32–34]. We identified maintenance use of low-dose aspirin (ATC code: B01AC06) or nonaspirin NSAIDs (ATC code: M01A) as having a cumulative dose≥180 defined daily dose (DDD) for each during the study period in the Swedish Prescribed Drug Registry. The above indications for PPI use were not mutually exclusive.
To measure the overall health of the patients with CRC, we used a revised version of the Charlson Comorbidity Index (CCI) [35, 36]. We identified each comorbidity as having at least one recorded diagnosis in the Swedish Patient Registry, and Appendix Table 1 displays the ICD-10 codes used. We further classified the Charlson Comorbidity Index score into four categories as ‘low’ (total score of 2), ‘moderate’ (total score of 3–4), ‘high’ (total score of 5–6) and ‘very high’ (total score of 7–12). Since patients had a CRC diagnosis, a total score of 2 was the minimum CCI score a patient would have (Appendix Table 1).
Data analysis
In the main analyses comparing PPI users with PPI nonusers, we performed time-dependent multivariable Cox proportional hazards models with a 6-month lag-time to calculate hazard ratios with 95% confidence intervals for both all-cause mortality and CRC specific mortality, adjusting for age, sex, pre-diagnosis PPI use, tumour site, tumour stage, CRC surgery, maintenance use of low-dose aspirin, maintenance use of non-aspirin NSAIDs and the Charlson Comorbidity score. In the sensitivity analyses, we removed the lag-time and applied a lag-time of 12 months, respectively.
To examine the confounding by indication, we stratified the PPI-mortality analyses by acid-related indications (gastro-oesophageal reflux, peptic ulcers and gastroduodenitis) and other simultaneously used medications (maintenance use of low-dose aspirin or nonaspirin NSAIDs). We further performed stratified analyses by sex, tumour stage, tumour site and CRC surgery to assess the effect modification of those cancer-related risk factors. Tests of interaction were performed by adding the cross product of PPIs use and the categorical stratification variable into the models.
To evaluate if the associations between PPIs use and mortality differed by time of PPIs initiation, we compared all-cause and CRC-specific mortality among new users and continuous users with PPI nonusers. Furthermore, we examined the linear dose–response associations based on the cumulative dose (by tertiles, <112DDD, 112-512DDD, ≥512DDD) and the average daily dose (by tertiles, <0.15DDD, 0.15-0.75DDD, ≥0.75DDD) of PPI users. Additionally, we solely evaluated the influence of pre-diagnosis PPI use on mortality using multivariable Cox proportional hazards models with a lag-time of 0, 6 months and 12 months accordingly.
Ethics approval and data deposition
This register-based study was entirely based on existing data and, therefore, involved no interaction between patients and researchers. Ethical approval of the study has been obtained from the Regional Ethical Review Board in Stockholm (reference number: 2014/129 - 31/4), and informed consent of the study participants was not required because of the registry-based design. Access to the data can be obtained after the required permissions by the National Ethics Committee; and the National Board of Health and Welfare, who own the data. Therefore, the data cannot be shared publicly. Coding can be made available upon reasonable request.
Results
We included overall 32,411 patients diagnosed with CRC, of whom 17,801 (54.9%) were PPI users. Median follow-up was 2.74 years (interquartile range, 1.32–4.80 years). Among 13,185 (40.7%) deaths during the study period, 9520 (72.2%) were recorded as CRC-specific. The all-cause mortality rate (140 vs 92, per 1000 person-years) and CRC-specific mortality rate (97 vs 48, per 1000 person-years) were higher among PPI users than among PPI nonusers. We observed similar proportions of PPI users and PPI nonusers in each strata of age at diagnosis, sex of patients, tumour site, tumour stage, the administration of CRC surgery, the CCI score, maintenance use of aspirin and NSAIDs, yet patients with recorded acid-related indications were more likely to be PPI users compared with those without recorded indication (Table 1).
Table 1.
Patient and tumour characteristics of the study population by post-diagnosis proton pump inhibitor (PPI) use in individuals with colorectal cancer (CRC).
| Characteristic | PPI Nonusers (n = 14,610) N (%)a | PPI Users (n = 17,801) N (%)a | Total (n = 32,411) N (%) |
|---|---|---|---|
| Age at diagnosis, years | |||
| <65 | 3823 (26) | 5556 (31) | 9379 (29) |
| 65–75 | 4393 (30) | 5537 (31) | 9950 (31) |
| >=75 | 6394 (44) | 6688 (38) | 13,082 (40) |
| Sex, male | 7877 (54) | 9104 (51) | 16,981 (52) |
| Pre-diagnosis PPI users | 2919 (20) | 7722 (43) | 10,641 (33) |
| Tumour stage | |||
| 0 + I | 2069 (14) | 1981 (11) | 4050 (13) |
| II | 3678 (25) | 3794 (21) | 7472 (23) |
| III | 3002 (21) | 4223 (24) | 7225 (22) |
| IV | 2355 (16) | 3802 (21) | 6157 (19) |
| Tumour site | |||
| Colon | 9518 (65) | 11,895 (67) | 23,980 (66) |
| Rectum | 5092 (35) | 5906 (33) | 10,998 (34) |
| CRC surgery | 11 514 (79) | 14,491 (82) | 26,005 (81) |
| Charlson Comorbidity index score | |||
| Low (2) | 7086 (49) | 7870 (44) | 14,956 (46) |
| Moderate (3–4) | 5258 (36) | 6466 (36) | 11,724 (36) |
| High (5–6) | 1645 (11) | 2262 (13) | 3907 (12) |
| Very High (7+) | 621 (4) | 1203 (7) | 1824 (6) |
| Indications for use of PPI | |||
| Gastro-oesophageal reflux | 820 (6) | 3008 (17) | 3828 (12) |
| Peptic ulcers | 402 (3) | 1484 (8) | 1886 (6) |
| Gastroduodenitis | 471 (3) | 1751 (10) | 2222 (7) |
| Maintenance use of low-dose aspirin | 5652 (39) | 7062 (40) | 12,714 (39) |
| Maintenance use of nonaspirin NSAIDs | 8349 (57) | 11,284 (63) | 19,633 (61) |
| None | 3061 (21) | 2806 (16) | 5867 (18) |
| Follow-up time, median (IQR), years | 2.66 (1.19–4.81) | 2.79 (1.42–4.80) | 2.74 (1.32–4.80) |
NSAIDs nonsteroidal anti-inflammatory drugs, CRC colorectal cancer, IQR interquartile range.
aPPI users were patients who had at least one PPI dispensation after the diagnosis of CRC; PPI nonusers were patients not collecting PPI dispensation after the diagnosis of CRC.
All-cause mortality
Indications for PPI use
The multivariable-adjusted HR (aHR) for all-cause mortality was 1.38 (95% CI, 1.32–1.44) comparing PPI users with PPI nonusers (Table 2). In the analyses stratified by indication subgroups, we observed the highest HRs among patients with maintenance use of low-dose aspirin (aHR, 1.34, 95% CI, 1.25–1.43) and nonaspirin NSAIDs (aHR, 1.48; 95% CI, 1.40–1.57). For patients without a selected indication, PPI use was also associated with an increased risk of all-cause mortality (aHR, 1.25; 95% CI, 1.13–1.38).
Table 2.
Multivariable time-dependent Cox analyses for risks of all-cause mortality and CRC-specific mortality, by indication.
| All-cause Mortality | CRC-Specific mortality | |||
|---|---|---|---|---|
| PPI Nonusersa | PPI Usersa | PPI Nonusersa | PPI Usersa | |
| All patients | ||||
| No. of deaths/ No. of person-years | 8439/68,015 | 4746/33,862 | 6231/68,015 | 3289/33,862 |
| aHRb | 1 (reference) | 1.38 (1.32, 1.44) | 1 (reference) | 1.34 (1.28, 1.41) |
| Gastro-oesophageal reflux | ||||
| No. of deaths/ No. of person-years | 749/5320 | 807/6922 | 549/5320 | 494/6922 |
| aHRb | 1 (reference) | 1.14 (1.01, 1.28) | 1 (reference) | 1.07 (0.93, 1.24) |
| Peptic ulcers | ||||
| No. of deaths/ No. of person-years | 487/2564 | 475/3143 | 335/2564 | 261/3143 |
| aHRb | 1 (reference) | 1.10 (0.94, 1.29) | 1 (reference) | 1.01 (0.83, 1.23) |
| Gastroduodenitis | ||||
| No. of deaths/ No. of person-years | 413/3283 | 511/3944 | 291/3283 | 289/3944 |
| aHRb | 1 (reference) | 1.19 (1.01, 1.39) | 1 (reference) | 1.17 (0.96, 1.43) |
| Low-dose aspirin | ||||
| No. of deaths/ No. of person-years | 3485/26,386 | 1972/14,448 | 2254/26,386 | 1087/14,448 |
| aHRb | 1 (reference) | 1.34 (1.25, 1.43) | 1 (reference) | 1.25 (1.14, 1.36) |
| Nonaspirin NSAIDs | ||||
| No. of deaths/ No. of person-years | 3956/42,584 | 2783/22,977 | 3050/42,584 | 2079/22,977 |
| aHRb | 1 (reference) | 1.48 (1.40, 1.57) | 1 (reference) | 1.48 (1.39, 1.58) |
| No indication | ||||
| No. of deaths/ No. of person-years | 2046/12,271 | 733/4112 | 1618/12,271 | 566/4112 |
| aHRb | 1 (reference) | 1.25 (1.13, 1.38) | 1 (reference) | 1.20 (1.07, 1.34) |
PPI proton pump inhibitors, CRC colorectal cancer, aHR multivariable-adjusted hazard ratio.
aPPI users were patients who had at least one PPI dispensation after the diagnosis of CRC; PPI nonusers were patients not collecting PPI dispensation after the diagnosis of CRC.
baHRs were adjusted for age, sex, pre-diagnosis PPI use, tumour site, tumour stage, CRC surgery, maintenance use of low-dose aspirin, maintenance use of non-aspirin NSAIDs, and the Charlson Comorbidity score.
Stratified analyses by CRC-related factors
Stratified analyses showed the association between PPI use and increased all-cause mortality was more pronounced in men than women (aHR,1.44; 95% CI, 1.36–1.52), patients at cancer stage 0 + I (aHR, 1.61; 95% CI, 1.36–1.90), patients with rectal cancer (aHR, 1.63; 95% CI, 1.50–1.75), and patients who underwent CRC surgery (aHR, 1.51; 95% CI, 1.44–1.59) (Table 3).
Table 3.
Multivariable time-dependent Cox analyses for risk of all-cause mortality related to post-diagnosis PPI use in different risk groups.
| PPI nonusersa | PPI usersa | aHRb | P for interaction | |
|---|---|---|---|---|
| No. of deaths/No. of person-years | ||||
| Sex | 0.007 | |||
| Male | 4548/36 324 | 2508/16,802 | 1.44 (1.36, 1.52) | |
| Female | 3891/31 691 | 2238/17,060 | 1.32 (1.24, 1.40) | |
| Tumour stage | <0.001 | |||
| 0 + I | 351/10 830 | 299/4811 | 1.61 (1.36, 1.90) | |
| II | 1010/18 413 | 718/8666 | 1.44 (1.30, 1.60) | |
| III | 1414/14 966 | 1130/8339 | 1.53 (1.41, 1.66) | |
| IV | 3474/6419 | 1482/2886 | 1.20 (1.12, 1.27) | |
| Tumour site | <0.001 | |||
| Colon | 5741/43 720 | 3147/22,399 | 1.29 (1.23, 1.36) | |
| Rectum | 2698/24 295 | 1599/11,472 | 1.63 (1.50, 1.75) | |
| CRC surgery | <0.001 | |||
| Yes | 4939/59 767 | 3657/30,735 | 1.51 (1.44, 1.59) | |
| No | 3500/8248 | 1089/3127 | 1.06 (0.97, 1.16) | |
PPI proton pump inhibitors, CRC colorectal cancer, aHR multivariable-adjusted hazard ratio.
aPPI users were patients who had at least one PPI dispensation after the diagnosis of CRC; PPI nonusers were patients not collecting PPI dispensation after the diagnosis of CRC.
baHRs were adjusted for age, sex, pre-diagnosis PPI use, tumour site, tumour stage, CRC surgery, maintenance use of low-dose aspirin, maintenance use of non-aspirin NSAIDs, and the Charlson Comorbidity score.
Timing of initiation, cumulative dose and average daily dose of PPI use
Compared to PPI nonusers, we found an increased risk of all-cause mortality (aHR, 1.32; 95% CI, 1.24–1.39) in continuous users (Table 4), and also in new users (aHR, 1.47; 95% CI, 1.40–1.55). In the dose–response analysis, PPI users with a median cumulative dose of 112-512DDD (aHR, 1.92; 95%CI,1.82–2.03) and median average daily dose of 0.15-0.75DDD (aHR, 1.74; 95%CI,1.64–1.84) was associated with the most prominent increase in all-cause mortality (Table 4). Pre-diagnosis PPI users also showed increased risks for all-cause and CRC-specific mortality as compared with pre-diagnosis PPI nonusers, with aHRs of 1.15 (95%CI, 1.09–1.22), and the risk estimates for CRC-specific mortality comparing PPI users to PPI nonusers were similar to those for all-cause mortality (Tables 2–4, Appendix Tables 2–4).
Table 4.
Multivariable time-dependent Cox analyses for risk of all-cause mortality and CRC-specific mortality, related to initiation and cumulative dose of PPI use.
| All-cause mortality | CRC-Specific Mortality | ||||
|---|---|---|---|---|---|
| No. of patients | No. of deaths/ No. of person-years | aHRc | No. of deaths/ No. of person-years | aHRc | |
| PPIs nonusersa | 14,610 | 8439/68,015 | 1 (reference) | 6231/68,015 | 1 (reference) |
| Initiation of PPI use | |||||
| New PPI usersa | 7722 | 2603/17,758 | 1.47 (1.40, 1.51) | 1972/17,758 | 1.44 (1.36, 1.53) |
| Continuous PPI usersa | 10,079 | 2143/16,103 | 1.32 (1.24, 1.39) | 1317/16,103 | 1.27 (1.19, 1.36) |
| Cumulative dose, DDDb | |||||
| <112 | 5870 | 799/8663 | 1.11 (1.02, 1.21) | 572/8663 | 1.11 (1.01, 1.22) |
| 112–512 | 5993 | 2069/9565 | 1.92 (1,82, 2.03) | 1652/9565 | 1.96 (1.84, 2.08) |
| ≥512 | 5938 | 1878/15,634 | 1.09 (1.03, 1.16) | 1065/15,634 | 0.99 (0.92, 1.07) |
| Average daily dose, DDD | |||||
| <0.15 | 5950 | 906/13,485 | 0.84 (0.78, 0.91) | 612/10,408 | 0.81 (0.73, 0.89) |
| 0.15–0.75 | 6045 | 1868/9968 | 1.74 (1,64, 1.84) | 1476/9968 | 1.77 (1.66, 1.89) |
| ≥0.75 | 5806 | 1972/10,408 | 1.55 (1.46, 1.65) | 1201/13,485 | 1.42 (1.32, 1.53) |
PPI proton pump inhibitors, DDD defined daily dose, CRC colorectal cancer, aHR multivariable-adjusted hazard ratio.
aPPI nonusers were patients not collecting PPI dispensation after the diagnosis of CRC. Continuous users were patients collecting at least one PPI dispensation both before and after diagnosis; new users were patients not collecting PPI dispensation before diagnosis but collecting at least one PPI dispensation after diagnosis.
bThe cumulative dose of PPI use was calculated based on cumulative DDD of PPI use after diagnosis of CRC, and the average daily dose was calculated as the cumulative DDD divided by the survival time (days from the diagnosis to death).
caHRs were adjusted for age, sex, pre-diagnosis PPI use, tumour site, tumour stage, CRC surgery, maintenance use of low-dose aspirin, maintenance use of non-aspirin NSAIDs, and the Charlson Comorbidity score. aHRs were additionally adjusted for pre-diagnosis PPI use in the analyses related to the cumulative dose and the average daily dose.
Sensitivity analyses
In the model which we set no lag-time, PPI use was also associated with an increased risk of all-cause mortality (aHR, 2.32; 95%CI, 2.23–2.42) compared with PPI nonuse (Appendix Table 3). The association was less pronounced when we set a 12-month lag-time (aHR, 1.24; 95%CI, 1.18–1.30).
Discussion
This large population-based study indicated increased risks for all-cause and CRC-specific mortality comparing PPI users with PPI nonusers, which were less pronounced but still significant among patients without recorded indications for PPI use. The analyses comparing mortality risks among new users, continuous users and PPI nonusers revealed the highest risk estimates among new users. The further dose–response analyses suggested no linear dose–response relationship between average daily dose and increased mortality. We also observed similar increased risks for all-cause and CRC-specific mortality comparing PPI users with PPI nonusers in the sensitivity analyses, though the magnitude of the risk estimates decreased as the lag-time increased from 0 to 12 months.
The magnitude of the risk estimates for all-cause/CRC-specific mortality decreased as the lag-time increased from 0 to 12 months. While removing the lag-time results in an overestimation of the PPI-mortality associations, it is possible the lag-time of 6 months did not entirely rule out the protopathic bias. Nonetheless, analyses with longer lag-time could yield conservative risk estimates and lose efficiency because deaths and person-years within the lag-time period could be unjustifiably excluded from the exposed group as the lag-time increases [37]. Since PPI users were still associated with an increased risk for mortality when the lag-time was 12 months, the associations observed in our study were not likely to be totally explained by protopathic bias.
Our findings align with previous studies suggesting elevated mortality risks linked to PPI use. The aforementioned Canadian and Danish cohort studies reported 34–44% higher mortality comparing PPI users to PPI nonusers [16, 17]. Furthermore, a few studies have observed PPI use was associated with increased risks for cancer-specific mortality in patients with other gastrointestinal cancers such as pancreatic cancers [38], gastric non-cardia cancer and hepatocellular carcinoma [39]. In addition to the studies conducted in patients with the diagnosis of cancer, a cohort study conducted in the US veterans reported 17% increased risk for overall mortality and 41% increased risk for upper gastrointestinal cancer-specific mortality comparing PPI users to PPI nonusers [40]. Our study extended the rarely examined PPIs-CRC prognosis associations by showing the effect modification of sex, tumour stage, tumour site and the CRC surgery. The more pronounced PPI-mortality associations among the subgroup analyses with rectum cancers compared to those with colon cancers could be attributed to the different molecular, embryological, biological features of colon and rectum cancer [41]. Further study is warranted to further explore whether and how the influence of PPI on mortality may differ in the left-sided and right-sided colon cancers. Interestingly, we also found the PPI-mortality associations were more evident among those who were at early cancer stages or underwent the CRC surgery. This could be interpreted as the evidence against reverse causality, that is, patients who were more severe at baseline are more likely to be prescribed with PPIs after the diagnosis and therefore should have higher mortality risks.
According to the stratified analyses by different indication groups, the PPI use-mortality associations were less evident in patients with acid-related indications compared with patients with the maintenance low-dose aspirin/NSAIDs use. This might be explained by the possible independent influence on CRC prognosis of the maintenance low-dose aspirin/NSAIDs use [32, 33, 42]. Additionally, we observed generally similar associations in each acid-related indication strata (gastro-oesophageal reflux, peptic ulcers and gastroduodenitis), making confounding by those acid-related diseases less likely. Among patients without the selected indications, PPI users also had increased all-cause and CRC-specific mortality compared with PPI nonusers. Therefore, the observed association between PPI use and increased mortality is not likely to be totally explained by the influence of the indications.
In contrast to what was identified in the previous US veteran study [40], we did not observe a linear dose–response association between the cumulative dose of PPI use and the increased risk for mortality, possibly due to the residual immortal-time bias. Though we carefully addressed immortal-time bias by conducting the analyses in a time-dependent manner, patients need to survive longer to acquire high cumulative dosage. Unfortunately, we were unable to differentiate the exposed person-time for each cumulative dose group since PPI users received the dispensation gradually and were continuously exposed. To avoid the potential influence of the residual immortal time, we further identified the average daily dose of PPI users and confirmed the absence of the linear dose–response associations.
With regard to the influence of the timing of PPI initiation, we found an increased risk for mortality in new users and continuous users compared with PPI nonusers, while the association was seemly more pronounced in new users. This may because that patients who initiated PPI use after the CRC diagnosis tend to start with a relatively higher dose, but requires further confirmation. Our definition of the initiation of PPI use could have misclassified continuous users into new users because it is possible that patients redeem PPI therapy before the start of the drug register in July 2005 and continue PPI use after the diagnosis of CRC. Therefore, the mortality risk comparing new users to nonusers could have been underestimated.
Though not explicitly clear, several mechanisms have been postulated to underlie the correlation between PPI use and CRC prognosis. PPI use could alter the gut microbiota toward a dysbiosis state characterised by decreased diversity and increased pathogenic bacteria taxa [6, 43]. Microbiota perturbation is associated with chronic inflammation, carcinogen accumulation (e.g. nitrogenous products) and epithelial barrier dysfunction and could, therefore, contribute to CRC carcinogenesis [7, 43, 44]. Second, previous studies have suggested that PPI was linked to weaker chemotherapy response and may therefore be associated with decreased efficacy of chemotherapeutic agents [17, 45, 46]. Third, PPI use could lead to prominent acid suppression in the stomach and further induce high serum gastrin [47], which may further contribute to colonic adenoma progression [48, 49]. Lastly, the possibility for PPIs to affect mortality through directly impairing endothelial function should be of note [50].
Our study has multiple strengths. Our data from high-quality nationwide registries with almost complete population coverage have minimised selection bias. We also controlled for several important prognostic factors to reduce potential confounding. Furthermore, we performed time-dependent analyses with the lag-time to control immortal time bias and protopathic bias. Finally, we were able to capture both all-cause mortality and CRC-specific mortality owing to the complete records of the cause of death.
This study has several limitations. First, patients may not completely comply with the dispensations. Nevertheless, we identified PPI users based on the dispensation at pharmacies that requires personal ID to purchase, strongly increasing the possibility of the actual use. Furthermore, we did not have access to data on over-the-counter PPI use. But during the study period, only small packages with high cost of PPIs were available over the counter in Sweden [51]. More importantly, pharmaceutical drugs are subsidised in Sweden when prescribed by a physician. Thus, the magnitude of this potential misclassification of exposure should be small. Additionally, socioeconomic factors and lifestyle factors were not available for the present study. However, the heterogeneity regarding the distribution of socioeconomic factors would be small due to the highly representative study population. Furthermore, PPI users without any recorded indications might still have acid-related diseases given only up to 35% PPI users had the recorded acid-related indications, possibly explained by that the mild and unspecific symptoms of the acid-related indications were less rigorously recorded [18]. Beyond the possibility of residual confounding, our findings may not be predictive of the long-term mortality because the follow-up is relatively short.
In this study, information on chemotherapy and radiotherapy was not available. Notwithstanding, it is not likely that the uncontrolled therapy would majorly distort the results. First, the PPI-mortality associations also presented among patients with stage I–II disease, who were unlikely to receive chemotherapy as surgery was long recommended as the standard treatment [52]. Second, it is conceivable that patients undergoing chemotherapy were more likely to be prescribed with PPIs for managing the post-chemotherapy side effects. The receipt of chemotherapy would, however, need to be linked with increased mortality to explain the observed PPI-mortality associations. Third, previous studies comparing the mortality of patients with PPI use during chemotherapy and patients without concurrent PPI use reported inconsistent associations between PPI and survival of patients with CRC. [45, 46, 53, 54]. The assessment of PPI use after the diagnosis of CRC rather than concomitant PPI use with the chemotherapy, as well as larger sample size and considerations of time-related biases in this study, may explain why our results differed from studies reporting insignificant or decreased mortality correlated with PPI use [53, 54].
In conclusion, with the effort to minimise the likelihood of immortal time bias and protopathic bias, we found PPI use after diagnosis of CRC was associated with increased all-cause and CRC-specific mortality among this nationwide cohort of patients with first-time diagnosed CRC. Whether PPI use is causally linked or contributory to an increased mortality risk of patients with CRC, findings of this study may have implications for improving PPIs prescribing practices.
Supplementary information
Acknowledgements
We thank all the patients, healthcare workers and the Swedish National Board of Health and Welfare for their contributions to data collection.
Author contributions
Study design: all authors. Data acquisition: NB. Statistical analysis: XW under supervision of NB. Data interpretation: all authors. Drafting of the manuscript: XW. Revising manuscript critically for important intellectual content and approving the final version of manuscript: all authors. Obtained funding: NB. Study supervision: NB. NB takes responsibility for the integrity of the data analysis.
Funding
This work was supported by Svenska Läkaresallskapet (SLS-788731, SLS-788751 SLS-783091) and The Swedish Research Council/Vetenskapsrådet (2020-01058). HZ was supported by a UNSW Scientia Fellowship. None of these sponsors had any role in the study design, the collection, analysis and interpretation of data.
Data availability
Data used for this study cannot be shared, but the original data from the registries can be obtained by application to Swedish National Board of Health and Welfare.
Competing interests
The authors report no conflict of interest. HZ works at the Centre for Big Data Research in Health, UNSW Sydney, which has received funding from AbbVie Australia to conduct research, unrelated to the present study. AbbVie did not have any knowledge of, or involvement in, the present study.
Ethics approval and consent to participate
Individual consent from the participants was waived for this register-based study. Ethical approval of the study has been obtained from the Regional Ethical Review Board in Stockholm (reference number: 2014/129 - 31/4).
Consent to publish
Not applicable.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41416-021-01480-0.
References
- 1.Hálfdánarson ÓÖ, Pottegård A, Björnsson ES, Lund SH, Ogmundsdottir MH, Steingrímsson E, et al. Proton-pump inhibitors among adults: a nationwide drug-utilization study. Ther Adv Gastroenterol. 2018;11:175628481877794. doi: 10.1177/1756284818777943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lassalle M, Le Tri T, Bardou M, Biour M, Kirchgesner J, Rouby F, et al. Use of proton pump inhibitors in adults in France: a nationwide drug utilization study. Eur J Clin Pharmacol. 2020;76:449–57. doi: 10.1007/s00228-019-02810-1. [DOI] [PubMed] [Google Scholar]
- 3.Daniels B, Pearson S-A, Buckley NA, Bruno C, Zoega H. Long-term use of proton-pump inhibitors: whole-of-population patterns in Australia 2013–2016. Ther Adv Gastroenterol. 2020;13:175628482091374. doi: 10.1177/1756284820913743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Savarino V, Dulbecco P, de Bortoli N, Ottonello A, Savarino E. The appropriate use of proton pump inhibitors (PPIs): Need for a reappraisal. Eur J Intern Med. 2017;37:19–24. doi: 10.1016/j.ejim.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 5.Freedberg DE, Kim LS, Yang Y-X. The risks and benefits of long-term use of proton pump inhibitors: expert review and best practice advice from the American Gastroenterological Association. Gastroenterology. 2017;152:706–15. doi: 10.1053/j.gastro.2017.01.031. [DOI] [PubMed] [Google Scholar]
- 6.Imhann F, Bonder MJ, Vich Vila A, Fu J, Mujagic Z, Vork L, et al. Proton pump inhibitors affect the gut microbiome. Gut. 2016;65:740–8. doi: 10.1136/gutjnl-2015-310376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saus E, Iraola-Guzmán S, Willis JR, Brunet-Vega A, Gabaldón T. Microbiome and colorectal cancer: roles in carcinogenesis and clinical potential. Mol Asp Med. 2019;69:93–106. doi: 10.1016/j.mam.2019.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robertson DJ, Larsson H, Friis S, Pedersen L, Baron JA, Sørensen HT. Proton pump inhibitor use and risk of colorectal cancer: a population-based, case–control study. Gastroenterology. 2007;133:755–60. doi: 10.1053/j.gastro.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 9.Lei W-Y, Wang J-H, Yi C-H, Liu T-T, Hung J-S, Wong M-W, et al. Association between use of proton pump inhibitors and colorectal cancer: a nationwide population-based study. Clin Res Hepatol Gastroenterol. 2021;45:101397. [DOI] [PubMed]
- 10.Hwang IC, Chang J, Park SM. Emerging hazard effects of proton pump inhibitor on the risk of colorectal cancer in low-risk populations: a Korean nationwide prospective cohort study. PLoS ONE. 2017;12:e0189114. [DOI] [PMC free article] [PubMed]
- 11.Chubak J, Boudreau DM, Rulyak SJ, Mandelson MT. Colorectal cancer risk in relation to use of acid suppressive medications. Pharmacoepidemiol Drug Saf. 2009;18:540–4. doi: 10.1002/pds.1749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Siersema PD, Yu S, Sahbaie P, Steyerberg EW, Simpson PW, Kuipers EJ, et al. Colorectal neoplasia in veterans is associated with Barrett’s esophagus but not with proton-pump inhibitor or aspirin/NSAID use. Gastrointest Endosc. 2006;63:581–6. doi: 10.1016/j.gie.2005.08.043. [DOI] [PubMed] [Google Scholar]
- 13.Yang Y, Hennessy S, Propert K, Hwang W, Sedarat A, Lewis JD. Chronic proton pump inhibitor therapy and the risk of colorectal cancer. Gastroenterology. 2007;133:748–54. doi: 10.1053/j.gastro.2007.06.022. [DOI] [PubMed] [Google Scholar]
- 14.Lee JK, Merchant SA, Schneider JL, Jensen CD, Fireman BH, Quesenberry CP, et al. Proton pump inhibitor use and risk of gastric, colorectal, liver, and pancreatic cancers in a community-based population. Am J Gastroenterol. 2020;115:706–15. [DOI] [PubMed]
- 15.van Soest EM, van Rossum LGM, Dieleman JP, van Oijen MGH, Siersema PD, Sturkenboom MCJM, et al. Proton pump inhibitors and the risk of colorectal cancer. Am J Gastroenterol. 2008;103:966–73. doi: 10.1111/j.1572-0241.2007.01665.x. [DOI] [PubMed] [Google Scholar]
- 16.Graham C, Orr C, Bricks CS, Hopman WM, Hammad N, Ramjeesingh R. A retrospective analysis of the role of proton pump inhibitors in colorectal cancer disease survival. Curr Oncol. 2016;23:583. doi: 10.3747/co.23.3204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tvingsholm SA, Dehlendorff C, Østerlind K, Friis S, Jäättelä M. Proton pump inhibitor use and cancer mortality. Int J Cancer. 2018;143:1315–26. doi: 10.1002/ijc.31529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brusselaers N, Wahlin K, Engstrand L, Lagergren J. Maintenance therapy with proton pump inhibitors and risk of gastric cancer: a nationwide population-based cohort study in Sweden. BMJ Open. 2017;7:e017739. doi: 10.1136/bmjopen-2017-017739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brusselaers N, Tamimi RM, Konings P, Rosner B, Adami H-O, Lagergren J. Different menopausal hormone regimens and risk of breast cancer. Ann Oncol. 2018;29:1771–6. doi: 10.1093/annonc/mdy212. [DOI] [PubMed] [Google Scholar]
- 20.Ma Y, Brusselaers N. Maintenance use of aspirin or other non-steroidal anti-inflammatory drugs (NSAIDs) and prostate cancer risk. Prostate Cancer Prostatic Dis. 2018;21:147–52. doi: 10.1038/s41391-017-0021-x. [DOI] [PubMed] [Google Scholar]
- 21.Doorakkers E, Lagergren J, Engstrand L, Brusselaers N. Helicobacter pylori eradication treatment and the risk of gastric adenocarcinoma in a Western population. Gut. 2018;67:2092–6. doi: 10.1136/gutjnl-2017-315363. [DOI] [PubMed] [Google Scholar]
- 22.Brusselaers N, Lagergren J, Engstrand L. Duration of use of proton pump inhibitors and the risk of gastric and oesophageal cancer. Cancer Epidemiol. 2019;62:101585. doi: 10.1016/j.canep.2019.101585. [DOI] [PubMed] [Google Scholar]
- 23.Loikas D, Wettermark B, von Euler M, Bergman U, Schenck-Gustafsson K. Differences in drug utilisation between men and women: a cross-sectional analysis of all dispensed drugs in Sweden. BMJ Open. 2013;3:e002378. doi: 10.1136/bmjopen-2012-002378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Suissa S. Immortal time bias in pharmacoepidemiology. Am J Epidemiol. 2008;167:492–9. doi: 10.1093/aje/kwm324. [DOI] [PubMed] [Google Scholar]
- 25.Pottegård A, Friis S, Stürmer T, Hallas J, Bahmanyar S. Considerations for pharmacoepidemiological studies of drug-cancer associations. Basic Clin Pharm Toxicol. 2018;122:451–9. doi: 10.1111/bcpt.12946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pottegård A, Hallas J. New use of prescription drugs prior to a cancer diagnosis: use of prescription drugs prior to cancer diagnosis. Pharmacoepidemiol Drug Saf. 2017;26:223–7. doi: 10.1002/pds.4145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tamim H, Monfared AAT, LeLorier J. Application of lag-time into exposure definitions to control for protopathic bias. Pharmacoepidemiol Drug Saf. 2007;16:250–8. doi: 10.1002/pds.1360. [DOI] [PubMed] [Google Scholar]
- 28.Brooke HL, Talbäck M, Hörnblad J, Johansson LA, Ludvigsson JF, Druid H, et al. The Swedish cause of death register. Eur J Epidemiol. 2017;32:765–73. doi: 10.1007/s10654-017-0316-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barlow L, Westergren K, Holmberg L, Talbäck M. The completeness of the Swedish Cancer Register—a sample survey for year 1998. Acta Oncol. 2009;48:27–33. doi: 10.1080/02841860802247664. [DOI] [PubMed] [Google Scholar]
- 30.Greene FL, Page DL, Fleming ID, Fritz A, Balch CM, Haller DG, et al. AJCC cancer staging manual. 6th. American Joint Committee on Cancer. 2002.
- 31.Nordic Medico-Statistical Committee. NOMESCO classification of surgical procedures (NCSP). Copenhagen: Nordic Medico-Statistical Committee, 2011.
- 32.Bastiaannet E, Sampieri K, Dekkers OM, de Craen AJM, van Herk-Sukel MPP, Lemmens V, et al. Use of Aspirin postdiagnosis improves survival for colon cancer patients. Br J Cancer. 2012;106:1564–70. doi: 10.1038/bjc.2012.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Din FVN, Theodoratou E, Farrington SM, Tenesa A, Barnetson RA, Cetnarskyj R, et al. Effect of aspirin and NSAIDs on risk and survival from colorectal cancer. Gut. 2010;59:1670–9. doi: 10.1136/gut.2009.203000. [DOI] [PubMed] [Google Scholar]
- 34.Flossmann E, Rothwell PM. Effect of aspirin on long-term risk of colorectal cancer: consistent evidence from randomised and observational studies. Lancet. 2007;369:1603–13. doi: 10.1016/S0140-6736(07)60747-8. [DOI] [PubMed] [Google Scholar]
- 35.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 36.Sadr-Azodi O, Oskarsson V, Discacciati A, Videhult P, Askling J, Ekbom A. Pancreatic cancer following acute pancreatitis: a population-based Matched Cohort Study. Am J Gastroenterol. 2018;113:1711–9. [DOI] [PubMed]
- 37.Tamim H, Monfared AT, LeLorier J. Application of lag‐time into exposure definitions to control for protopathic bias. Pharmacoepidemiol. Drug Saf. 2007;16:250–8. doi: 10.1002/pds.1360. [DOI] [PubMed] [Google Scholar]
- 38.Kearns MD, Boursi B, Yang Y-X. Proton pump inhibitors on pancreatic cancer risk and survival. Cancer Epidemiol. 2017;46:80–4. doi: 10.1016/j.canep.2016.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ayyagari S, Tan MC, Liu Y, El-Serag HB, Thrift AP. Use of acid-suppressant medications after diagnosis increases mortality in a subset of gastrointestinal cancer patients. Dig. Dis. Sci. 2020;65:2691–9. doi: 10.1007/s10620-019-05984-x. [DOI] [PubMed] [Google Scholar]
- 40.Xie Y, Bowe B, Yan Y, Xian H, Li T, Al-Aly Z. Estimates of all cause mortality and cause specific mortality associated with proton pump inhibitors among US veterans: cohort study. BMJ. 2019;29:l1580. doi: 10.1136/bmj.l1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dekker E, Tanis PJ, Vleugels JLA, Kasi PM, Wallace MB. Colorectal cancer. Lancet. 2019;394:1467–80. doi: 10.1016/S0140-6736(19)32319-0. [DOI] [PubMed] [Google Scholar]
- 42.Chan AT, Ogino S, Fuchs CS. Aspirin use and survival after diagnosis of colorectal cancer. JAMA. 2009;302:649–58. [DOI] [PMC free article] [PubMed]
- 43.Freedberg DE, Toussaint NC, Chen SP, Ratner AJ, Whittier S, Wang TC, et al. Proton pump inhibitors alter specific taxa in the human gastrointestinal microbiome: a crossover trial. Gastroenterology. 2015;149:883–885.e9. doi: 10.1053/j.gastro.2015.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Louis P, Hold GL, Flint HJ. The gut microbiota, bacterial metabolites and colorectal cancer. Nat Rev Microbiol. 2014;12:661–72. doi: 10.1038/nrmicro3344. [DOI] [PubMed] [Google Scholar]
- 45.Chu MP, Hecht JR, Slamon D, Wainberg ZA, Bang Y-J, Hoff PM, et al. Association of proton pump inhibitors and capecitabine efficacy in advanced gastroesophageal cancer: secondary analysis of the TRIO-013/LOGiC randomized clinical trial. JAMA Oncol. 2017;3:767. doi: 10.1001/jamaoncol.2016.3358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sun J, Ilich AI, Kim CA, Chu MP, Wong GG, Ghosh S, et al. Concomitant administration of proton pump inhibitors and capecitabine is associated with increased recurrence risk in early stage colorectal cancer patients. Clin Colorectal Cancer. 2016;15:257–63. doi: 10.1016/j.clcc.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 47.Lundell L, Vieth M, Gibson F, Nagy P, Kahrilas PJ. Systematic review: the effects of long-term proton pump inhibitor use on serum gastrin levels and gastric histology. Aliment Pharm Ther. 2015;42:649–63. doi: 10.1111/apt.13324. [DOI] [PubMed] [Google Scholar]
- 48.Watson SA, Smith AM. Hypergastrinemia promotes adenoma progression in the APC(Min−/+) mouse model of familial adenomatous polyposis. Cancer Res. 2001;61:625–31. [PubMed] [Google Scholar]
- 49.Colucci R, Blandizzi C, Tanini M, Vassalle C, Breschi MC, Tacca MD. Gastrin promotes human colon cancer cell growth via CCK-2 receptor-mediated cyclooxygenase-2 induction and prostaglandin E2 production: Gastrin, cyclooxygenase-2 and colon cancer growth. Br J Pharmacol. 2005;144:338–48. doi: 10.1038/sj.bjp.0706053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yepuri G, Sukhovershin R, Nazari-Shafti TZ, Petrascheck M, Ghebre YT, Cooke JP. Proton pump inhibitors accelerate endothelial senescence. Circ Res. 2016;118:e36-42. [DOI] [PMC free article] [PubMed]
- 51.FASS (Farmacevtiska specialiteter i Sverige/ Farmaceutical specialities in Sweden). http://www.fass.se. Accessed 21 August 2020.
- 52.Team AP. Early Stage Colon Cancer-Clinical Practice Guideline GI-004. Alberta Health Services, Alberta. 2008.
- 53.Wong GG, Ha V, Chu MP, Dersch-Mills D, Ghosh S, Chambers CR, et al. Effects of proton pump inhibitors on FOLFOX and CapeOx regimens in colorectal cancer. Clin Colorectal Cancer. 2019;18:72–9. doi: 10.1016/j.clcc.2018.11.001. [DOI] [PubMed] [Google Scholar]
- 54.Zhang J-L, Liu M, Yang Q, Lin S-Y, Shan H-B, Wang H-Y, et al. Effects of omeprazole in improving concurrent chemoradiotherapy efficacy in rectal cancer. World J Gastroenterol. 2017;23:2575. doi: 10.3748/wjg.v23.i14.2575. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data used for this study cannot be shared, but the original data from the registries can be obtained by application to Swedish National Board of Health and Welfare.