Abstract
Background
Since the declaration of the coronavirus disease 2019 (COVID-19) pandemic, COVID-19 has affected the responses of emergency medical service (EMS) systems to cases of out-of-hospital cardiac arrest (OHCA). The purpose of this study was to identify the impact of the COVID-19 pandemic on EMS responses to and outcomes of adult OHCA in an area of South Korea.
Methods
This was a retrospective observational study of adult OHCA patients attended by EMS providers comparing the EMS responses to and outcomes of adult OHCA during the COVID-19 pandemic to those during the pre-COVID-19 period. Propensity score matching was used to compare the survival rates, and logistic regression analysis was used to assess the impact of the COVID-19 pandemic on the survival of OHCA patients.
Results
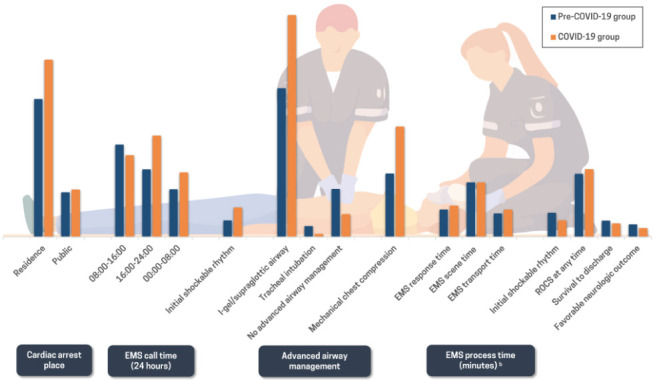
A total of 891 patients in the pre-COVID-19 group and 1,063 patients in the COVID-19 group were included in the final analysis. During the COVID-19 period, the EMS call time was shifted to a later time period (16:00–24:00, P < 0.001), and the presence of an initial shockable rhythm was increased (pre-COVID-19 vs. COVID-19, 7.97% vs. 11.95%, P = 0.004). The number of tracheal intubations decreased (5.27% vs. 1.22%, P < 0.001), and the use of mechanical chest compression devices (30.53% vs. 44.59%, P < 0.001) and EMS response time (median [quartile 1-quartile 3], 7 [5–10] vs. 8 [6–11], P < 0.001) increased. After propensity score matching, the survival at admission rate (22.52% vs. 18.24%, P = 0.025), survival to discharge rate (7.77% vs. 5.52%, P = 0.056), and favorable neurological outcome (5.97% vs. 3.49%, P < 0.001) decreased. In the propensity score matching analysis of the impact of COVID-19, odds ratios of 0.768 (95% confidence interval [CI], 0.592–0.995) for survival at admission and 0.693 (95% CI, 0.446–1.077) for survival to discharge were found.
Conclusion
During the COVID-19 period, there were significant changes in the EMS responses to OHCA. These changes are considered to be partly due to social distancing measures. As a result, the proportion of patients with an initial shockable rhythm in the COVID-19 period was greater than that in the pre-COVID-19 period, but the final survival rate and favorable neurological outcome were lower.
Keywords: Emergency Medical Services, Out-of-Hospital Cardiac Arrest, COVID-19
Graphical Abstract
INTRODUCTION
Since the World Health Organization declared the coronavirus disease 2019 (COVID-19) a pandemic on 11 March 2020, COVID-19 has affected not only individual patients' health but also public health, including the emergency medical service (EMS) system.1 According to a report from the United States, the number of emergency department (ED) visits declined by 23% for myocardial infarction, 20% for stroke, and 10% for hyperglycemic crisis compared with the 10-week period preceding the pandemic declaration.2 This decrease and change in medical service use has also been reported in Korea.3,4
COVID-19 has also had a profound effect on patients with out-of-hospital cardiac arrest (OHCA), a time-sensitive medical emergency.5,6 In the survival of OHCA patients, when the “chain of survival” steps, including early recognition and activation of EMS, prompt provision of bystander cardiopulmonary resuscitation (CPR) and use of an automated external defibrillator (AED), which are well linked, successful outcomes can be expected.7 However, the pandemic appears to have disrupted the system of care for OHCA patients, even in regions with a low prevalence of COVID-19.8 A study in the United States found that the pandemic had an indirect negative impact on OHCA patients, with less bystander CPR, delays in EMS response times, and reduced survival from OHCA, even in communities with a low incidence of COVID-19.9 Another study in France found a higher rate of OHCA at home, less bystander CPR, and longer delays to intervention.10
South Korea has had a low incidence of COVID-19 thus far and continues social distancing.11 However, the impact of the COVID-19 pandemic on the OHCA system of care and outcomes has rarely been a focus. The purpose of this study was to identify the potential impact of the COVID-19 pandemic on EMS response times to OHCA and to compare the outcomes of OHCA patients during the pre-COVID-19 and COVID-19 periods in an area of South Korea.
METHODS
Study design
This was a retrospective observational study of adult OHCA patients attended by EMS providers in the Busan, Ulsan, Gyeongnam, and Changwon regions in South Korea, which was conducted by members of Regionalization and Research of EMS in Yeongnam (RREMSY), a local EMS research group. This study compared the OHCA cases during the COVID-19 period to those during the pre-COVID-19 period. The pre-COVID-19 and COVID-19 periods were defined as from 1 November 2019 to 31 January 2020 and from 1 November 2020 to 31 January 2021, respectively.
All patients with OHCA during the study periods were eligible for inclusion. Patients were excluded if they were less than 18 years old, if resuscitation was not attempted due to obvious signs of death or if they had a valid do-not-resuscitate order. Patients who were pulseless because of trauma, intoxication, or drowning were excluded.
Study setting
The Busan, Ulsan, Gyeongnam, and Changwon regions, located in southeastern South Korea, consist of two metropolitan cities (Busan, Ulsan), one city (Changwon), and one province (Gyeongnam), with a total population of 792 million, spread over almost 12,369 km2.12
The EMS system in the region, which is government-based and single-tiered, provides basic to intermediate levels of EMS, such as supraglottic airway insertion, tracheal intubation and basic life support from fire agency headquarters. The EMS resuscitation protocol introduces multiple dispatches (two or more ambulance teams), provides on-site CPR and transports patients to an ED in an ambulance with ongoing CPR. EMS providers cannot stop CPR unless the patient has return of spontaneous circulation (ROSC), either on-site or during transportation to the ED, and only physicians in hospital EDs can declare death.13
After 1 November 2019, some authorized EMS providers in the region started to provide advanced life support by administering intravenous epinephrine under the direct medical oversight of medical directors via mobile video calls as a pilot project to expand the scope of EMS providers' services.14 Mechanical CPR devices are available for prolonged cardiac arrests and select patients. During both study periods, this change was applied equally.
The first confirmed case of COVID-19 in Busan was reported on 21 February 2020. To reduce EMS provider exposure to COVID-19, it was recommended that personal protective equipment (PPE) be put on before entering a scene, the number of dispatched personnel be limited, and the use of mechanical chest compression devices be considered. In addition, it was recommended that high-efficiency particulate air filter respirators be used for all ventilation procedures and that an EMS provider intubate with the highest chance of first-pass success and, if intubation was delayed, to consider the use of a supraglottic airway according to the guideline.15 Unlike EMS systems in other countries where the volume of confirmed COVID-19 patients was large, there were no significant behavior changes in the EMS and medical directions in Korea, as COVID-19 confirmed cases in the region occurred at a level that quarantine could control.
Data sources
Prehospital data on all dispatches of EMS are collected and managed by regional fire agencies electronically from scene-dispatched EMS providers. For cases where resuscitation is performed, the EMS providers file a prehospital cardiac arrest patient care report. In this study, anonymous prehospital data were collected from the four headquarters of the national fire agencies by submitting a research proposal. In-hospital data were collected from treating hospital EDs (76 EDs during the pre-COVID-19 period and 69 EDs during the COVID-19 period). Data on daily confirmed COVID-19 cases were obtained from the Korea Disease Control and Prevention Agency.16
Variables and measurements
Data for the patient variables of age, sex, and medical history, including a history of hypertension, diabetes, stroke, cardiac disease, pulmonary disease, liver disease, renal disease, and malignancy, were collected.
The following data were collected as bystander variables: cardiac arrest place (residence, public, nursing facility, or ambulance), EMS call time (08:00-16:00, 16:00-24:00, or 00:00-08:00), bystander-witnessed or not, bystander (family member, nonfamily member, or EMS provider), bystander CPR or not, and bystander AED use or not.
Data for the EMS variables of the presence of an initial shockable rhythm on scene, the use of advanced airway management (I-gel/supraglottic airway, tracheal intubation, or no advanced airway management), the use of mechanical chest compression devices, the use of epinephrine, and EMS process time (response, scene, and transport times) were collected. EMS response, scene and transport times were defined as the time elapsed from the call to EMS to EMS arrival at the scene, from EMS arrival at the scene to EMS departure from the scene, and from EMS departure from the scene to EMS arrival at the ED, respectively.
Data for the hospital variables of the presence of an initial shockable rhythm, ROSC at any time, survival at admission, survival to discharge, and favorable neurological outcome were collected. ROSC at any time was defined as whether there was a pulse at any time during in-hospital CPR regardless of the patient's survival. Survival at admission and survival to discharge were defined as the case in which a patient survived until admission to the intensive care unit and until hospital discharge, respectively. Favorable neurological outcome was defined by cerebral performance category 1 or 2.17
Main outcomes
The primary outcome of the study was the neurological outcome of OHCA patients. The secondary outcome of the study was the survival to discharge of OHCA patients. Both the primary outcome and the secondary outcome were compared for the pre-COVID-19 and COVID-19 periods.
Statistical analysis
Descriptive analysis was performed to examine the distribution of variables. Continuous variables are presented as the mean and standard deviation (SD) or median and interquartile range (IQR), and categorical variables are presented as frequencies and proportions. In the comparison of the two groups, differences in continuous variables were assessed using the independent t-test or Mann-Whitney test, and differences in categorical variables were assessed using the chi-square (χ2) test as appropriate. Propensity score matching was used to compare the survival rates of OHCA patients in the pre-COVID-19 and COVID-19 periods. The variables used in matching were the following: age, sex, cardiac disease, malignancy, cardiac arrest place (public), bystander-witnessed, bystander CPR, bystander AED use, the presence of an initial shockable rhythm on scene, and EMS process time. Logistic regression analysis was used to calculate odds ratios (ORs) and 95% confidence intervals (CIs) to assess the effect of the COVID-19 pandemic on the survival of OHCA patients. All statistical analyses were performed using SPSS 26.0 (SPSS, Inc., Chicago, IL) and SAS 9.4 (SAS Institute Inc., Cary, NC, USA). A two-sided P value of <0.05 was considered statistically significant.
Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Board of Gyeongsang National University Changwon Hospital (approval no. 2021-02-008). The requirement for informed consent from patients was waived because the study was a retrospective analysis of existing data.
RESULTS
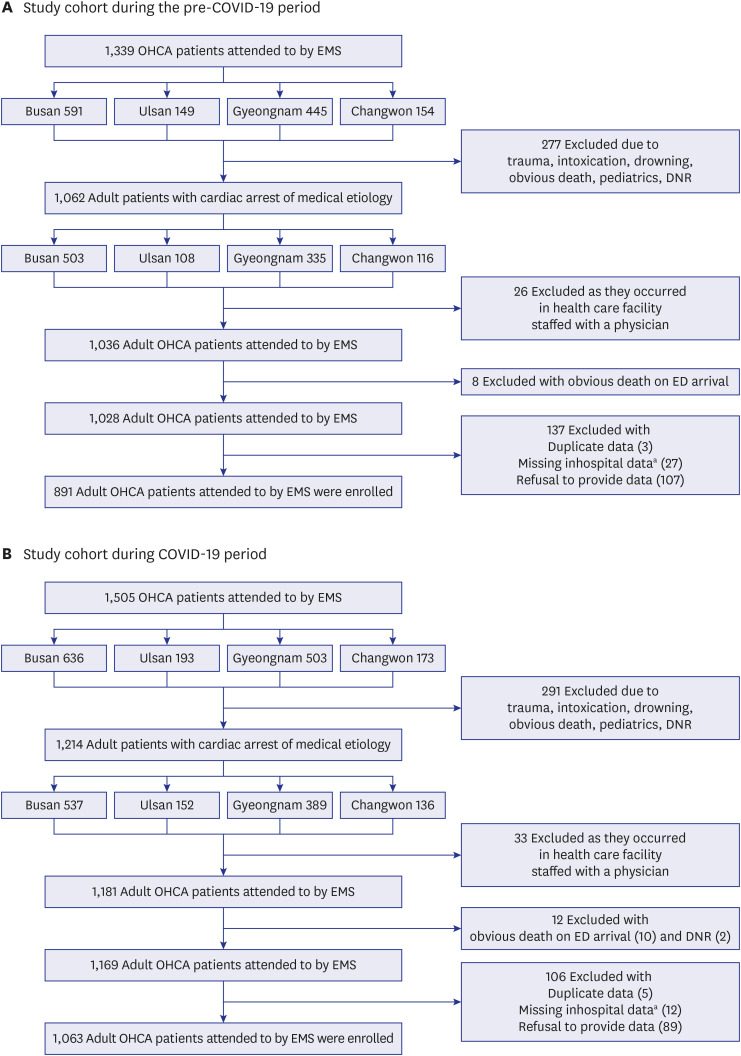
A total of 2,844 adult OHCA patients were eligible for CPR during the study period. Patients who did not meet the inclusion criteria (448 in the pre-COVID-19 group and 442 in the COVID-19 group) were excluded, and 891 OHCA patients in the pre-COVID-19 group and 1,063 in the COVID-19 group were included in the final analysis (Fig. 1).
Fig. 1. Definition of the study cohort. (A) Study cohort during the pre-COVID-19 period. (B) Study cohort during COVID-19 period.
OHCA = out-of-hospital cardiac arrest, EMS = emergency medical service, ED = emergency department, DNR = do not resuscitate.
aPrehospital emergency medical service data exist, but no record of patients visiting the ED exists.
Characteristics of adult OHCA patients during the pre-COVID-19 and COVID-19 periods
The COVID-19 group was older (P = 0.047) and had a lower proportion of patients with cardiac disease (P = 0.033) (Table 1). The daily incidences of confirmed COVID-19 cases and adult OHCA in the study area during the COVID-19 period are shown in Fig. 2.
Table 1. Characteristics of adult out-of-hospital cardiac arrest during the pre-COVID-19 and COVID-19 periods.
| Variables | Pre-COVID-19 group (n = 891) | COVID-19 group (n = 1,063) | P value | ||
|---|---|---|---|---|---|
| Patient variables | |||||
| Age, yra | 70.07 ± 15.06 | 71.05 ± 14.98 | 0.047* | ||
| Age, yrb | 73 (60–81) | 75 (62–82) | |||
| Sex (male %) | 577 (64.76) | 647 (60.87) | 0.076 | ||
| Medical history | |||||
| Hypertension | 235 (26.37) | 305 (28.69) | 0.254 | ||
| Diabetes | 175 (19.64) | 193 (18.16) | 0.403 | ||
| Stroke | 77 (8.64) | 74 (6.96) | 0.166 | ||
| Cardiac disease | 159 (17.85) | 152 (14.3) | 0.033* | ||
| Pulmonary disease | 52 (5.84) | 90 (8.47) | 0.026* | ||
| Liver disease | 16 (1.8) | 20 (1.88) | 0.888 | ||
| Renal disease | 38 (4.26) | 40 (3.76) | 0.572 | ||
| Malignancy | 76 (8.53) | 121 (11.38) | 0.037* | ||
| Bystander variables | |||||
| Cardiac arrest place | 0.079 | ||||
| Residence | 592 (66.44) | 761 (71.59) | |||
| Public | 192 (21.55) | 204 (19.19) | |||
| Nursing facility | 41 (4.6) | 37 (3.48) | |||
| Ambulance | 66 (7.41) | 61 (5.74) | |||
| EMS call time (24 hr) | < 0.001*** | ||||
| 08:00–16:00 | 396 (44.44) | 351 (33.02) | |||
| 16:00–24:00 | 290 (32.55) | 435 (40.92) | |||
| 00:00–08:00 | 205 (23.01) | 277 (26.06) | |||
| Bystander-witnessed | 414 (46.46) | 470 (44.21) | 0.320 | ||
| Bystander | 0.061 | ||||
| Family member | 517 (58.02) | 666 (62.65) | |||
| Nonfamily member | 280 (31.43) | 283 (26.62) | |||
| EMS provider | 94 (10.55) | 114 (10.72) | |||
| Bystander CPR | 541 (60.72) | 636 (59.83) | 0.690 | ||
| Bystander AED use | 97 (10.89) | 91 (8.56) | 0.083 | ||
| EMS variables | |||||
| Initial shockable rhythm | 71 (7.97) | 127 (11.95) | 0.004* | ||
| Advanced airway management | < 0.001*** | ||||
| I-gel/supraglottic airway | 638 (71.6) | 952 (89.56) | |||
| Tracheal intubation | 47 (5.27) | 13 (1.22) | |||
| No advanced airway management | 206 (23.12) | 98 (9.22) | |||
| Mechanical chest compression device | 272 (30.53) | 474 (44.59) | < 0.001*** | ||
| Epinephrine use | 147 (16.5) | 190 (17.87) | 0.423 | ||
| EMS process time, minb | |||||
| 1) EMS response time | 7 (5–10) | 8 (6–11) | < 0.001*** | ||
| 2) EMS scene time | 14 (10–18) | 14 (11–18) | 0.627 | ||
| 3) EMS transport time | 6 (4–10) | 7 (4–12) | < 0.001*** | ||
| Hospital variables | |||||
| Initial shockable rhythm | 104 (11.67) | 72 (6.77) | < 0.001*** | ||
| ROSC at any time | 271 (30.42) | 291 (27.38) | 0.004** | ||
| Survival at admission | 201 (22.56) | 196 (18.44) | 0.024* | ||
| Survival to discharge | 70 (7.86) | 58 (5.46) | 0.030* | ||
| Favorable neurological outcome | 54 (6.06) | 38 (3.57) | < 0.001*** | ||
Variables are presented as the mean ± standard deviationa, median (quartile 1-quartile 3)b and number (%). COVID-19 = coronavirus disease 2019, EMS = emergency medical services, CPR = cardiopulmonary resuscitation, AED = automated external defibrillator, ROSC = return of spontaneous circulation.
Fig. 2. The daily incidence of adult OHCA patients and confirmed COVID-19 during the study period.
OHCA = out-of-hospital cardiac arrest, COVID-19 = coronavirus disease.
Neurological outcomes of adults with OHCA during the pre-COVID-19 and COVID-19 periods
The favorable neurological outcome decreased from 6.06% to 3.59% (P < 0.001) (Table 1). After propensity score matching, it decreased from 5.97% to 3.49% (P < 0.001) (Table 2).
Table 2. Propensity score matching analysis of adult out-of-hospital cardiac arrest patients during the pre-COVID-19 and COVID-19 periods.
| Variables | Pre-COVID-19 period (n = 888) | COVID-19 period (n = 888) | P value | ||
|---|---|---|---|---|---|
| Patient variables | |||||
| Age, yra | 70.07/15.07 | 70.70/15.17 | 0.234 | ||
| Age, yrb | 73 (60–81) | 74 (61–82) | |||
| Sex (male %) | 574 (64.64) | 570 (64.19) | 0.843 | ||
| Medical history | |||||
| Hypertension | 235 (26.46) | 251 (28.27) | 0.394 | ||
| Diabetes | 175 (19.71) | 165 (18.58) | 0.546 | ||
| Stroke | 77 (8.67) | 68 (7.66) | 0.435 | ||
| Cardiac disease | 156 (17.57) | 146 (16.44) | 0.528 | ||
| Pulmonary disease | 52 (5.86) | 81 (9.12) | 0.009** | ||
| Liver disease | 16 (1.8) | 16 (1.8) | 1.000 | ||
| Renal disease | 36 (4.05) | 36 (4.05) | 1.000 | ||
| Malignancy | 76 (8.56) | 88 (9.91) | 0.325 | ||
| Bystander variables | |||||
| Cardiac arrest place | 0.832 | ||||
| Residence | 592 (66.67) | 609 (68.58) | |||
| Public | 191 (21.51) | 184 (20.72) | |||
| Nursing facility | 41 (4.62) | 37 (4.17) | |||
| Ambulance | 64 (7.21) | 58 (6.53) | |||
| EMS call time (24 hr) | < 0.001*** | ||||
| 08:00–16:00 | 394 (44.37) | 294 (33.11) | |||
| 16:00–24:00 | 290 (32.66) | 358 (40.32) | |||
| 00:00–08:00 | 204 (22.97) | 236 (26.58) | |||
| Bystander-witnessed | 411 (46.28) | 412 (46.4) | 0.962 | ||
| Bystander | 0.127 | ||||
| Family member | 517 (58.22) | 540 (60.81) | |||
| Nonfamily member | 279 (31.42) | 242 (27.25) | |||
| EMS provider | 92 (10.36) | 106 (11.94) | |||
| Bystander CPR | 538 (60.59) | 537 (60.47) | 0.961 | ||
| Bystander AED use | 94 (10.59) | 87 (9.8) | 0.583 | ||
| EMS variables | |||||
| Initial shockable rhythm | 71 (8.00) | 83 (9.35) | 0.312 | ||
| Advanced airway management | < 0.001*** | ||||
| I-gel/supraglottic airway | 637 (71.73) | 792 (89.19) | |||
| Tracheal intubation | 47 (5.29) | 11 (1.24) | |||
| No advanced airway management | 204 (22.97) | 85 (9.57) | |||
| Mechanical chest compression device | 272 (30.63) | 393 (44.26) | < 0.001*** | ||
| Epinephrine use | 147 (16.55) | 160 (18.02) | 0.415 | ||
| EMS process time, minb | |||||
| 1) EMS response time | 7 (5–10) | 8 (6–10) | < 0.001*** | ||
| 2) EMS scene time | 14 (10–18) | 14 (11–18) | 0.820 | ||
| 3) EMS transport time | 6 (4–10) | 6 (4–10) | 0.142 | ||
| Hospital variables | |||||
| Initial shockable rhythm | 103 (11.6) | 57 (6.42) | < 0.001*** | ||
| ROSC at any time | 270 (30.41) | 238 (26.8) | 0.008** | ||
| Survival at admission | 200 (22.52) | 162 (18.24) | 0.025* | ||
| Survival to discharge | 69 (7.77) | 49 (5.52) | 0.056 | ||
| Favorable neurological outcome | 53 (5.97) | 31 (3.49) | < 0.001*** | ||
Variables included in propensity score matching analysis are age, sex, cardiac disease, malignancy, cardiac arrest place (public), bystander-witnessed, bystander CPR, bystander AED use, the presence of an initial shockable rhythm on scene, and EMS process time. Variables are presented as athe mean ± standard deviation, bmedian (quartile 1-quartile 3) and number (%).
COVID-19 = coronavirus disease 2019, EMS = emergency medical service, CPR = cardiopulmonary resuscitation, AED = automated external defibrillator, ROSC = return of spontaneous circulation.
The survival to discharge of adults with OHCA during the pre-COVID-19 and COVID-19 periods
The survival to discharge rate decreased from 7.86% to 5.46% (P = 0.030) (Table 1). After propensity score matching, it decreased from 7.77% to 5.52% (P = 0.056) (Table 2). In the analysis of the impact of COVID-19 after propensity score matching, an adjusted OR of 0.693 (95% CI, 0.446–1.007) for survival to discharge was found (Table 3). The survival outcomes for the two groups are shown in Fig. 3.
Table 3. The impact of COVID-19 on the hospital outcomes.
| Group | Survival at admission | Survival to discharge | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Survival | Incidence | Adjusted OR (95% CI) | Total | Survival | Incidence | Adjusted OR (95% CI) | ||
| Total patient group | |||||||||
| Pre-COVID-19 | 891 (45.60) | 201 (50.63) | 22.56 | Reference | 891 (45.60) | 70 (54.69) | 7.86 | Reference | |
| COVID-19 | 1,063 (54.40) | 196 (49.37) | 18.44 | 0.776 (0.605–0.996) | 1,063 (54.40) | 58 (45.31) | 5.46 | 0.677 (0.442–1.034) | |
| Propensity groupa | |||||||||
| Pre-COVID-19 | 888 (50.00) | 200 (55.25) | 22.52 | Reference | 888 (50.00) | 69 (58.47) | 7.78 | Reference | |
| COVID-19 | 888 (50.00) | 162 (44.75) | 18.24 | 0.768 (0.592–0.995) | 888 (50.00) | 49 (41.53) | 5.52 | 0.693 (0.446–1.077) | |
Variables are presented as the number (%).
COVID-19 = coronavirus disease 2019, OR = odds ratio, CI = confidence interval, CPR = cardiopulmonary resuscitation, AED = automated external defibrillator, EMS = emergency medical service.
aThe variables included in propensity score matching analysis are age, sex, cardiac disease, malignancy, arrest place (public), bystander-witnessed, bystander CPR, bystander AED use, the presence of an initial shockable rhythm on scene, and EMS process time.
Fig. 3. Neurological outcomes and survival results of adult OHCA patients during the study period. (A) Pre-COVID-19 period. (B) COVID-19 period.
OHCA = out-of-hospital cardiac arrest, EMS = emergency medical service, ED = emergency department, ROSC = return of spontaneous circulation, CPC = cerebral performance category.
aThe data of transferred patients was not traceable.
Prehospital response to adult OHCA during the pre-COVID-19 and COVID-19 periods
In the COVID-19 period, there were more EMS calls in the 16:00-24:00 and 00:00-08:00 time periods than in the pre-COVID-19 period (P < 0.001). In the COVID-19 period, the use of tracheal intubation was decreased (P < 0.001), and the use of mechanical chest compression devices was increased (P < 0.001). The EMS response and transport times were increased (P < 0.001) (Table 1).
DISCUSSION
This study found significant changes in the prehospital response to and outcomes of adult OHCA during the COVID-19 period in an area of South Korea. To the best of our knowledge, this is the first study to identify prehospital responses to and outcomes of adult OHCA in South Korea during the COVID-19 period. Although the difference was small, the COVID-19 group of OHCA patients was older. During the COVID-19 period, the numbers of OHCA patients with an initial shockable rhythm on scene and EMS calls in the later time period were higher than those in the pre-COVID-19 period. Furthermore, during the COVID-19 period, there were changes in the practices of EMS providers, such as a decrease in the number of tracheal intubations and an increase in the use of mechanical chest compression devices and EMS response time. As a result, survival rates decreased.
In this study, an increased number of cardiac arrests in residences and a decreased number of cardiac arrests in public places were observed during the COVID-19 period, and these results are consistent with those of other studies. In a study in Australia in which the incidence of COVID-19 was low, the rate of public-place cardiac arrests decreased from 20.8% to 10.0%.18 The increase in the number of cardiac arrests in residences would have been because patients stayed at home more with the emphasis on social distancing. Before COVID-19, older people, in particular, were able to spend time at senior centers. However, since the COVID-19 pandemic began, many of these facilities have closed.
The EMS call time shifted to a later time period in the COVID-19 period. In addition, the number of cases in which a family member was the first responder increased. However, the number of witnessed cardiac arrests decreased. In cases in which the family member was the first responder, it is presumed that the family member arrived home after work, found the patient, and called EMS. Several studies have reported that the number of witnessed cardiac arrests declined during the COVID-19 pandemic, even though many people stayed at home. According to a study in the United States, during the COVID-19 pandemic, the number of cardiac arrests in residences increased from 63% to 76%, while the number of witnessed cardiac arrests decreased from 53% to 50%.9 The witnessing of cardiac arrests in residences by nonfamily members is rare. In particular, older people are often alone at home during the daytime. One study found that the daytime OHCA survival rate was higher than the nighttime OHCA survival rate.19 The changes in prehospital responses to OHCA in this study are thought to be consequences of social distancing measures.
The decrease in the use of tracheal intubation and increase in the use of mechanical chest compression devices by EMS providers are considered to be in accordance with the recommendations of the prehospital management guideline since the onset of the COVID-19 pandemic. In South Korea, when EMS providers' intubation skills are not proficient, they should not be forced to attempt intubation.20 However, mechanical chest compression devices have been continuously supplied since 2014, and all EMS providers can use them without guidance from a medical director. Thus, the use of mechanical chest compression devices was likely to have increased.21
The increase in EMS process time during the COVID-19 period in this study is consistent with the findings of other studies. In a Japanese study, it was reported that the prehospital processing time increased from 32.2 ± 10.8 minutes before the COVID-19 outbreak to 33.8 ± 11.6 minutes (P < 0.001) after the COVID-19 outbreak, and the response and scene times were especially increased.22 In a study in the United States, it was also found that the response and scene times increased from 9.1 ± 5.5 to 9.2 ± 5.3 minutes and from 15.7 ± 9.5 to 18.3 ± 10.8 minutes, respectively, but the transport time decreased from 14.1 ± 9.1 to 13.2 ± 8.3 minutes.23 Each country has a different scope and range of EMS provider skills, so there will be variation in scene times. However, an approximately 1-minute increase in response time after COVID-19 was a commonly reported change in many studies. This increase would be the time it took for EMS providers to put on PPE before dispatching.
A remarkable finding of this study is the presence of an initial shockable rhythm on scene during both study periods. In OHCA, the presence of a shockable rhythm during resuscitation was associated with higher odds of survival than a sustained nonshockable rhythm.24 During the pre-COVID-19 period, the percentages of patients with shockable rhythms on scene and at hospital arrival were 7.97% and 11.67%, respectively; however, during the COVID-19 period, these percentages were 11.95% and 6.77%, respectively. In a previous study of EMS response time, for every minute of added ambulance response time, the odds of the patient having a shockable rhythm decreased by 8%.25 However, in this study, even though the response time increased by approximately 1 minute during the COVID-19 period, the rate of the presence of a shockable rhythm was higher than that in the pre-COVID-19 period.
EMS providers use AEDs on scene, and they would have performed appropriate shocks for all patients with shockable rhythms. Therefore, the differences in EMS intervention during the two study periods were due only to the decrease in the number of tracheal intubations and the increase in the use of mechanical chest compression devices and EMS process time. However, in a previous study in Japan, prehospital advanced airway management (AAM) was not related to the survival of shockable rhythm OHCA patients (survival rate with AAM vs. with no AAM, 19.2% vs. 18.6%; adjusted risk ratio 1.00, 95% CI, 0.93-1.07). This finding was related to the survival of nonshockable rhythm OHCA patients (survival rate with AAM vs. with no AAM, 2.3% vs. 1.8%; adjusted risk ratio 1.27, 95% CI, 1.20-1.30).26 Therefore, it is unlikely that the decline in the number of tracheal intubations during the COVID-19 period was mainly responsible for the lower survival rate despite the high percentage of patients with an initial shockable rhythm. To date, the evidence in humans on whether the use of mechanical chest compression devices during CPR is associated with benefit or harm is insufficient to draw conclusions.27 Some studies have reported that the use of mechanical chest compression devices during CPR does not improve survival.28,29 However, it has been reported that shortening the EMS response time increases witnessed OHCA survival. The result of this study—a higher incidence of an initial shockable rhythm during COVID-19 but a lower final survival rate—is probably due to the increase in EMS response time.
A recent study using machine learning confirmed that the most important predictor of OHCA survival was the presence of an initial shockable rhythm, followed by age, time to the initiation of CPR, EMS response time and the place of cardiac arrest.30 In particular, among patients found with a shockable rhythm, the five most important predictors were the time to defibrillation, age, defibrillation (yes/no), place of cardiac arrest, and time from cardiac arrest to the initiation of CPR. In our study, although the COVID-19 group had a higher incidence of an initial shockable rhythm than the pre-COVID-19 group, they were older and had fewer cases of cardiac arrest in public places, fewer cases of bystander CPR and AED use, and delayed EMS response time. All of these factors would have contributed to the decline in survival rates. In this study, EMS response time was used in propensity score matching. If this factor had been excluded from matching, there would have been a slightly larger difference in survival rates. However, this study tried to report the difference in the survival rate between the two groups after strictly controlling for this factor.
Postmortem COVID-19 testing in OHCA patients is not routine practice and is not included in quarantine statistics in Korea. Therefore, it was not possible to obtain accurate data on the number of postmortem COVID-19 tests in the region during the COVID-19 study period. However, to the best of our knowledge, there was one postmortem confirmed COVID-19 case for OHCA patients.
There are some limitations of this work. First, this study had a limited sample size from one area, and the COVID-19 study period was only 3 months. However, the results of this study are impressive enough and highlight the changes that occurred during the study periods. Second, some patients were excluded from data collection due to refusal to provide data, and patients who survived at admission but were transferred to another hospital were excluded from data analysis (Figs. 1 and 3). Therefore, the actual survival to discharge rate and favorable neurological outcomes could be slightly higher. Third, it has been reported that the incidence of a shockable rhythm decreases when cardiac arrest occurs in a residence.31 However, this study found the opposite result. Further studies are needed to determine whether this result is due to factors other than the study period setting.
In conclusion, during the COVID-19 period, there were significant changes in the prehospital responses that affected the outcomes of OHCA patients. These changes were considered to be partly due to social distancing measures. As a result, the presence of an initial shockable rhythm, with which favorable outcomes can be expected, was higher in the COVID-19 period, but the final survival rate was lower.
ACKNOWLEDGMENTS
The authors are grateful to all of the emergency physicians working in Busan, Ulsan, Gyeongnam, and Changwon for their assistance in collecting data and RREMSY members who devoted their time and efforts to the development of local EMS systems.
Footnotes
Funding: This research was supported by Dong-A University Research foundation grant (No. 20210501).
Disclosure: The authors have no potential conflicts of interest to disclose
- Conceptualization: Park SY.
- Data curation: Park SY, Lim D.
- Formal analysis: Park SY, Lim D.
- Funding acquisition: Park SY.
- Investigation: BC, Kim SH, Ryu JH, Kim YH, Sung AJ, Bae BG, Kim HB.
- Methodology: Park SY, Lim D.
- Software: Park SY, Lim D.
- Validation: Lim D.
- Visualization: Park SY.
- Writing - original draft: Park SY, Lim D.
- Writing - review & editing: Lim D, Park SY, Choi B, Kim SH, Ryu JH, Kim YH, Sung AJ, Bae BG, Kim HB.
References
- 1.Hartley DM, Perencevich EN. Public health interventions for COVID-19: emerging evidence and implications for an evolving public health crisis. JAMA. 2020;323(19):1908–1909. doi: 10.1001/jama.2020.5910. [DOI] [PubMed] [Google Scholar]
- 2.Lange SJ, Ritchey MD, Goodman AB, Dias T, Twentyman E, Fuld J, et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions—United States, January–May 2020. Wiley Online Library; 2020. MMWR Morb Mortal Wkly Rep. 2020;69(25):795–800. doi: 10.15585/mmwr.mm6925e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sung HK, Paik JH, Lee YJ, Kang S. Impact of the COVID-19 outbreak on emergency care utilization in patients with acute myocardial infarction: a nationwide population-based study. J Korean Med Sci. 2021;36(16):e111. doi: 10.3346/jkms.2021.36.e111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yoon D, Kim KE, Lee JE, Kim M, Kim JH. Impact of the coronavirus disease 2019 (COVID-19) pandemic on medical use of military hospitals in Korea. J Korean Med Sci. 2021;36(28):e204. doi: 10.3346/jkms.2021.36.e204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, et al. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med. 2020;383(5):496–498. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chan PS, Girotra S, Tang Y, Al-Araji R, Nallamothu BK, McNally B. Outcomes for out-of-hospital cardiac arrest in the United States during the coronavirus disease 2019 pandemic. JAMA Cardiol. 2021;6(3):296–303. doi: 10.1001/jamacardio.2020.6210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deakin CD. The chain of survival: not all links are equal. Resuscitation. 2018;126:80–82. doi: 10.1016/j.resuscitation.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 8.Elmer J, Okubo M, Guyette FX, Martin-Gill C. Indirect effects of COVID-19 on OHCA in a low prevalence region. Resuscitation. 2020;156:282–283. doi: 10.1016/j.resuscitation.2020.08.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Uy-Evanado A, Chugh HS, Sargsyan A, Nakamura K, Mariani R, Hadduck K, et al. Out-of-hospital cardiac arrest response and outcomes during the COVID-19 pandemic. JACC Clin Electrophysiol. 2021;7(1):6–11. doi: 10.1016/j.jacep.2020.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marijon E, Karam N, Jost D, Perrot D, Frattini B, Derkenne C, et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020;5(8):e437–e443. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. (COVID-19) dashboard. [Updated 2021]. [Accessed May 12, 2021]. https://covid19.who.int/table.
- 12.Statistics Korea. Statistical geographic information service. [Updated 2021]. [Accessed May 12, 2021]. https://sgis.kostat.go.kr/view/index.
- 13.Ro YS, Shin SD, Song KJ, Hong SO, Kim YT, Lee DW, et al. Public awareness and self-efficacy of cardiopulmonary resuscitation in communities and outcomes of out-of-hospital cardiac arrest: a multi-level analysis. Resuscitation. 2016;102:17–24. doi: 10.1016/j.resuscitation.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 14.National Fire Agency. [Updated 2021]. [Accessed May 12, 2021]. https://www.nfa.go.kr/nfa/news/pressrelease/press/?boardId.
- 15.Edelson DP, Sasson C, Chan PS, Atkins DL, Aziz K, Becker LB, et al. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: from the emergency cardiovascular care committee and get with the guidelines-resuscitation adult and pediatric task forces of the American Heart Association. Circulation. 2020;141(25):e933–e943. doi: 10.1161/CIRCULATIONAHA.120.047463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Korea Disease Control and Prevention Agency. [Updated 2021]. [Accessed May 12, 2021]. http://www.kdca.go.kr/index.es?sid=a3.
- 17.Mak M, Moulaert VR, Pijls RW, Verbunt JA. Measuring outcome after cardiac arrest: construct validity of Cerebral Performance Category. Resuscitation. 2016;100:6–10. doi: 10.1016/j.resuscitation.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 18.Ball J, Nehme Z, Bernard S, Stub D, Stephenson M, Smith K. Collateral damage: Hidden impact of the COVID-19 pandemic on the out-of-hospital cardiac arrest system-of-care. Resuscitation. 2020;156:157–163. doi: 10.1016/j.resuscitation.2020.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wallace SK, Abella BS, Shofer FS, Leary M, Agarwal AK, Mechem CC, et al. Effect of time of day on prehospital care and outcomes after out-of-hospital cardiac arrest. Circulation. 2013;127(15):1591–1596. doi: 10.1161/CIRCULATIONAHA.113.002058. [DOI] [PubMed] [Google Scholar]
- 20.Lim D, Kim SC, Park SY, Rhu JH, Bae BK, Kim SH, et al. A survey on the perception of emergency medical services (EMS) providers and medical directors toward EMS provider's field skill proficiency. J Korean Soc Emerg Med. 2020;31(4):401–419. [Google Scholar]
- 21.Jung E, Park JH, Lee SY, Ro YS, Hong KJ, Song KJ, et al. Mechanical chest compression device for out-of-hospital cardiac arrest: a nationwide observational study. J Emerg Med. 2020;58(3):424–431. doi: 10.1016/j.jemermed.2019.11.022. [DOI] [PubMed] [Google Scholar]
- 22.Ageta K, Naito H, Yorifuji T, Obara T, Nojima T, Yamada T, et al. Delay in emergency medical service transportation responsiveness during the COVID-19 pandemic in a minimally affected region. Acta Med Okayama. 2020;74(6):513–520. doi: 10.18926/AMO/61210. [DOI] [PubMed] [Google Scholar]
- 23.Satty T, Ramgopal S, Elmer J, Mosesso VN, Martin-Gill C. EMS responses and non-transports during the COVID-19 pandemic. Am J Emerg Med. 2021;42:1–8. doi: 10.1016/j.ajem.2020.12.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rajan S, Folke F, Hansen SM, Hansen CM, Kragholm K, Gerds TA, et al. Incidence and survival outcome according to heart rhythm during resuscitation attempt in out-of-hospital cardiac arrest patients with presumed cardiac etiology. Resuscitation. 2017;114:157–163. doi: 10.1016/j.resuscitation.2016.12.021. [DOI] [PubMed] [Google Scholar]
- 25.Renkiewicz GK, Hubble MW, Wesley DR, Dorian PA, Losh MJ, Swain R, et al. Probability of a shockable presenting rhythm as a function of EMS response time. Prehosp Emerg Care. 2014;18(2):224–230. doi: 10.3109/10903127.2013.851308. [DOI] [PubMed] [Google Scholar]
- 26.Izawa J, Komukai S, Gibo K, Okubo M, Kiyohara K, Nishiyama C, et al. Pre-hospital advanced airway management for adults with out-of-hospital cardiac arrest: nationwide cohort study. BMJ. 2019;364:l430. doi: 10.1136/bmj.l430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brooks SC, Hassan N, Bigham BL, Morrison LJ. Mechanical versus manual chest compressions for cardiac arrest. Cochrane Database Syst Rev. 2014;(2):CD007260. doi: 10.1002/14651858.CD007260.pub3. [DOI] [PubMed] [Google Scholar]
- 28.Perkins GD, Lall R, Quinn T, Deakin CD, Cooke MW, Horton J, et al. Mechanical versus manual chest compression for out-of-hospital cardiac arrest (PARAMEDIC): a pragmatic, cluster randomised controlled trial. Lancet. 2015;385(9972):947–955. doi: 10.1016/S0140-6736(14)61886-9. [DOI] [PubMed] [Google Scholar]
- 29.Gates S, Quinn T, Deakin CD, Blair L, Couper K, Perkins GD. Mechanical chest compression for out of hospital cardiac arrest: systematic review and meta-analysis. Resuscitation. 2015;94:91–97. doi: 10.1016/j.resuscitation.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 30.Al-Dury N, Ravn-Fischer A, Hollenberg J, Israelsson J, Nordberg P, Strömsöe A, et al. Identifying the relative importance of predictors of survival in out of hospital cardiac arrest: a machine learning study. Scand J Trauma Resusc Emerg Med. 2020;28(1):60. doi: 10.1186/s13049-020-00742-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oving I, de Graaf C, Karlsson L, Jonsson M, Kramer-Johansen J, Berglund E, et al. Occurrence of shockable rhythm in out-of-hospital cardiac arrest over time: a report from the COSTA group. Resuscitation. 2020;151:67–74. doi: 10.1016/j.resuscitation.2020.03.014. [DOI] [PubMed] [Google Scholar]