Abstract
In 2017, the Korean government launched an unprecedentedly large-scaled latent tuberculosis infection (LTBI) screening project which covered more than a million individuals in congregate settings. A total of 1,047,689 participants of source population (n = 2,336,157) underwent LTBI testing from 2017 to 2018. The overall LTBI test uptake rate during this project was 44.8%. Workers in daycare centers (83.5%) and kindergartens (78.9%) showed high participation rate. A total of 1,012,206 individuals with valid results of interferon-gamma release assay (IGRA) were selected to constitute the IGRA cohort. Most of the enrolled participants in the IGRA cohort were in their working age. Approximately, three-quarters of total enrolled population were female. Investigating the LTBI prevalence, stages of LTBI care cascade, natural history of LTBI, efficacy of LTBI treatment and cost-effectiveness of LTBI screening are feasible within this IGRA cohort.
Keywords: Latent Tuberculosis, Interferon-gamma Release Tests, Republic of Korea, Mass Screening
Graphical Abstract
Strategies to tackle latent tuberculosis infection (LTBI) have been underscored worldwide and implemented in countries with both low- and high-tuberculosis (TB) burdens.1 An estimated pool of LTBI was one-fourth of world's population.2 For TB elimination to incidence of less than one case per million population by 2050, preventing new infection and reducing the preexisting pool of LTBI are crucial, in addition to control active TB cases.3
The TB burden in South Korea is disproportionately high, considering the high level of socioeconomic development.4 Before early 2000's, screening and treatment of LTBI were not feasible in South Korea. In 2004, LTBI screening was implemented for people living with human immunodeficiency virus (HIV) and family contacts under 6 years of age.5 Nationwide contact investigation in both household and congregate environment was launched in 2013. However, as several TB outbreaks at hospitals, daycare centers, schools and military units continuously occurred and became important social issues, Korean government implemented ‘TB-free Korea’ program in 2016. In this program, one of the key strategies was to provide screening and treatment of LTBI among more than 1.6 million individuals in congregate settings. The aim of this study was to identify the LTBI test uptake rate and describe demographic profiles of participants who received interferon-gamma release assay (IGRA).
Study settings, methods of data collection and linkage were described in our protocol article.6 In 2017 and 2018, workers at the prespecified congregate settings underwent LTBI testing (either IGRA or tuberculin skin test [TST]). The source population of each congregate settings were quoted from the 2017's annual survey of government for the number of employees of social welfare institutions, daycare centers, educational institutions, healthcare institutions, postpartum care centers.7,8,9 Total number of first year students in high-school and the average of daily number of inmates in nationwide correctional facility in 2017 were also cited from the official reports of government.7,10 Statistics on ‘out-of-school youth’ were not available, so estimated target number of screening replaced the actual number in that group. Because data of participants with negative LTBI results during their military draft health checkup were not available, candidates for military conscripts were excluded in this analysis.
Korea Disease Control and Prevention Agency (KDCA) collected baseline demographic information of participants and LTBI test results. These participants constituted a prospective cohort named ‘TB FREE COREA.’ The cohort was matched with National Health Information Database (NHID).11 Information about income level and place of residence were extracted from the insurance qualification database of NHID. Korean National TB Surveillance System (KNTSS) database was also linked with the cohort to exclude participants with previous TB history and identify the incident TB cases. In addition, to identify an exposure to TB before or after the screening, the national database of TB epidemiological investigation in congregate settings and that in household contacts were also matched with the cohort. Because of high bacille Calmette-Guérin vaccination rate in South Korea,12 we concerned about possible discrepancies between IGRA and TST results13 and thus excluded participants who underwent only TST. The statistical analyses were performed with descriptive statistics, using SAS software, version 9.4 (SAS Institute Inc., Cary, NC, USA).
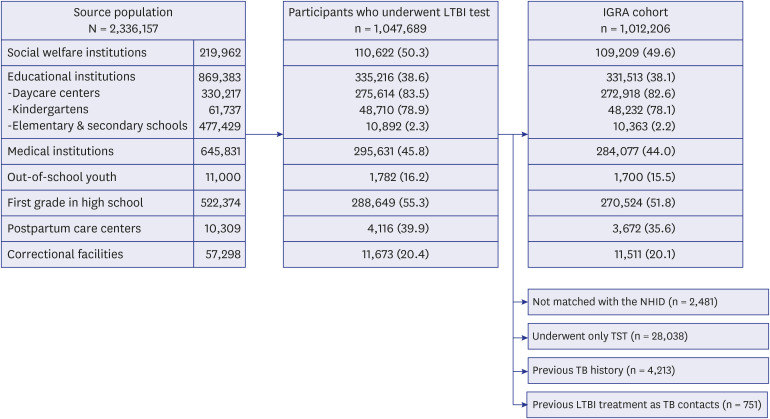
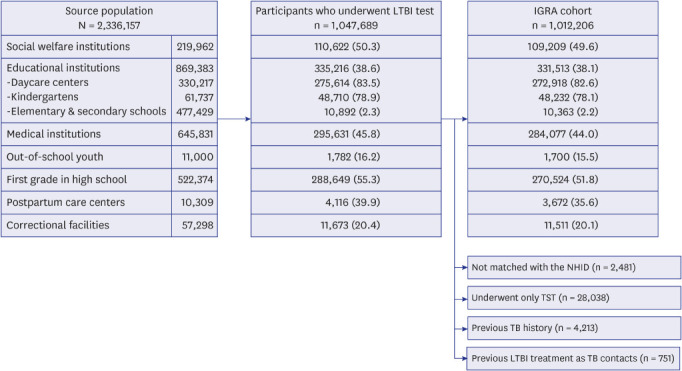
A total of 1,047,689 individuals of 2,336,157 source population underwent either TST or IGRA. The LTBI test uptake rate was 44.8% (Fig. 1). Workers of daycare centers (83.5%) and kindergartens (78.9%) showed the highest, followed by first year students in high school (55.3%) and workers of social welfare institutions (50.3%). After exclusion of individuals who were not matched with the NHID (n = 2,481), those who underwent only TST between 2017 and 2018 (n = 28,038), those with past TB history (n = 4,213) and those who underwent LTBI treatment as TB contacts before the participation in ‘TB-free Korea’ program (n = 751), a total of 1,012,206 individuals with valid results of IGRA were selected to constitute the IGRA cohort.
Fig. 1. Flow chart showing the process of IGRA cohort constitution. Number of source population, participation rate of LTBI testing and that of IGRA by each congregate setting were presented.
IGRA = Interferon-gamma release assay, LTBI = latent tuberculosis infection, TST = tuberculin skin test, NHID = National Health Information Database, TB = tuberculosis.
Baseline demographic features of the IGRA cohort were presented in Table 1. As this screening was carried out among the employees of congregate facilities, most of the enrolled participants were of working age. People in their 50s accounted for the largest proportion among the workers of social welfare institutions and those of postpartum care centers, whereas those in their 20s among the workers of medical institutions. Except for the inmates of correctional facilities, in which the proportion of male was 93.8%, female accounted for three-quarters of total enrolled population among the workers of other congregate facilities. Among the workers of medical institutions and groups of youth, proportion of high-income group was higher than that of other groups.
Table 1. Baseline demographic features of participants enrolled in IGRA cohort.
| Variables | Congregate settings | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Workers of social welfare institutions (n = 109,209) | Workers of educational institutions (n = 331,513) | Workers of medical institutions (n = 284,077) | Out-of-school youths (n = 1,700) | First year students in high school (n = 270,524) | Workers of postpartum care centers (n = 3,672) | Inmates of correctional facilities (n = 11,511) | Total (n = 1,012,206) | ||
| Age, yr | |||||||||
| < 30 | 12,787 (11.7) | 67,858 (20.5) | 90,899 (32.0) | 1,679 (98.8) | 270,453 (100.0) | 243 (6.6) | 1,626 (14.1) | 445,545 (44.0) | |
| 30–39 | 15,467 (14.2) | 83,423 (25.2) | 75,475 (26.6) | 11 (0.6) | 17 (0.0) | 521 (14.2) | 2,753 (23.9) | 177,667 (17.6) | |
| 40–49 | 23,994 (22.0) | 120,296 (36.3) | 61,651 (21.7) | 8 (0.5) | 17 (0.0) | 1,085 (29.5) | 3,183 (27.7) | 210,234 (20.8) | |
| 50–59 | 38,363 (35.1) | 49,818 (15.0) | 41,165 (14.5) | 2 (0.1) | 31 (0.0) | 1,311 (35.7) | 2,887 (25.1) | 133,577 (13.2) | |
| ≥ 60 | 18,598 (17.0) | 10,118 (3.1) | 14,887 (5.2) | 0 (0.0) | 6 (0.0) | 512 (13.9) | 1,062 (9.2) | 45,183 (4.5) | |
| Sex | |||||||||
| Male | 21,619 (19.8) | 14,432 (4.4) | 65,638 (23.1) | 921 (54.2) | 150,602 (55.7) | 118 (3.2) | 10,798 (93.8) | 264,128 (26.1) | |
| Female | 87,590 (80.2) | 317,081 (95.6) | 218,439 (76.9) | 779 (45.8) | 119,922 (44.3) | 3,554 (96.8) | 713 (6.2) | 748,078 (73.9) | |
| Income levela | |||||||||
| Medicaid group | 1,016 (0.9) | 1,058 (0.3) | 557 (0.2) | 163 (9.7) | 10,218 (3.8) | 29 (0.8) | 806 (7.6) | 13,847 (1.4) | |
| Low | 37,410 (34.7) | 158,317 (48.4) | 39,123 (14.1) | 379 (22.6) | 47,303 (17.8) | 1,297 (35.7) | 4,600 (43.2) | 288,429 (29.0) | |
| Moderate low | 35,714 (33.1) | 96,832 (29.6) | 75,830 (27.3) | 243 (14.5) | 39,300 (14.8) | 1,233 (34.0) | 2,150 (20.2) | 251,302 (25.3) | |
| Moderate high | 25,283 (23.4) | 39,446 (12.1) | 91,161 (32.8) | 297 (17.7) | 54,642 (20.5) | 656 (18.1) | 1,555 (14.6) | 213,040 (21.4) | |
| High | 8,421 (7.8) | 31,205 (9.5) | 71,441 (25.7) | 593 (35.4) | 114,694 (43.1) | 415 (11.4) | 1,529 (14.4) | 228,298 (22.9) | |
| Place of residenceb | |||||||||
| Metropolitan city | 48,658 (44.6) | 196,918 (59.4) | 193,169 (68.0) | 858 (50.5) | 160,521 (59.4) | 2,344 (64.0) | 6,093 (58.5) | 608,561 (60.2) | |
| Small to medium-sized city | 42,109 (38.6) | 111,169 (33.5) | 72,246 (25.5) | 578 (34) | 83,952 (31.1) | 1,238 (33.8) | 3,324 (31.9) | 314,616 (31.1) | |
| Rural area | 18,400 (16.9) | 23,381 (7.1) | 18,451 (6.5) | 263 (15.5) | 25,836 (9.6) | 83 (2.3) | 994 (9.5) | 87,408 (8.6) | |
Data were expressed as number and column percentage.
IGRA = interferon-gamma release assay.
aNumber of missing value was 17,290; bNumber of missing value was 1,621.
Main goal of the ‘TB-free Korea’ program was to protect younger generation from TB, by direct screening themselves, or by screening the potential source of TB transmission to them—workers of postpartum care centers, social welfare institutions, daycare centers, kindergartens and schools. Considering the large generation gap in TB burden, protecting younger generation from TB should be a key strategy for national TB control program in South Korea, which could reduce TB burden drastically within 10 to 20 years. Historically, younger generation was the main target of national LTBI screening programs.14 In the United States (US), since the efficacy of isoniazid preventive therapy was demonstrated in 1960's,15 the government implemented massive LTBI screening program with TST which targeted mainly for younger generations such as periodic school-based TST.16 After decrement of TB incidence in the US, selective screening for high-risk groups was recommended officially by Centers for Disease Control and Prevention in 199517 and by American Thoracic Society in 1999.18 In Japan, since the isoniazid preventive therapy was introduced in 1965, LTBI screening for children 4 years of age, those who entered elementary schools or middle schools was carried out, as in the US.19,20 Since 2005, as the TB burden in Japan had drastically decreased, strategy of mass screening was terminated and selective screening for high-risk groups was adopted.21
In ‘TB-free Korea’ program, mass screening in two congregate settings—high schools and military units were carried out. Considering that entrance rate of high school in 2017 was 93.7%,22 approximately half of the population born in the same year underwent LTBI screening. Additionally, although not included in this study, almost all the male population born in another same year underwent LTBI screening as a medical check-up in the military conscription. The long-term effect of such massive LTBI screening will be investigated in individual and community's perspectives.
It is noteworthy that high-risk congregate settings were selected not only for the individual's net benefit, but also for the potential risk of secondary TB cases from a population perspective. The World Health Organization (WHO) recommends an individual-level approach in LTBI screening and treatment in low incidence countries.23 Only in cases that benefit outweigh the risk of treatment such as contacts or people living with HIV, screening and treatment was recommended. However, according to a recently published study, the WHO's recommendation could only protect 4.2% of notified TB cases in Canada, which indicated that such approach would minimally impact national TB burden.24 Recently in low incidence countries, target groups for screening and treatment of LTBI were expanded considering the countries' epidemiologic status, in which benefit in individual level was limited but that in population level was demonstrated.25 Hospitals and correctional facilities were well-known high-risk congregate settings,26,27,28,29 whereas postpartum care centers, daycare centers, kindergartens, and schools were not included in high-risk congregate settings in previous guidelines. Selection of such congregate settings was based on a cost-effectiveness analysis,30 but there were many limitations due to lack of preceding evidence needed for cost-effectiveness analysis. Impact of this screening program on the TB burden in South Korea, especially among the young generation, should be evaluated at the population level.
In this program, only 44.8% of source population underwent LTBI test. However, due to the limited budget of Korean government, the number of actual target population that Korean government had set was 985,000 after exclusion of candidates for military conscription (n = 670,000). Considering that actual goal, we identified that the actual participation rate was more than 100%. We speculated that this full achievement might result from the revised Tuberculosis Prevention Act which ordered the mandatory LTBI screening among this source population since 2016.
This is an unprecedentedly large-scaled population-based LTBI study in South Korea. Except for some groups of young generation, people in various age group were included. The effect of age on prevalence of LTBI, which was the most important predictors for LTBI in a previous population-based survey,31 and effects of other factors will be investigated. The adherence to the program, which should be warranted for cost-effectiveness of the screening program,32 will be evaluated in the frame of LTBI cascade of care. Additionally, this cohort contains more than one million IGRA results as quantitative values, not only as binary outcomes. According to the recent research assessing the usefulness of quantitative values of IGRA results,33,34,35 we will demonstrate the value of quantitative IGRA in prediction of active TB disease and efficacy of LTBI treatment. Based on future analysis of the IGRA cohort, it is feasible to prepare and implement more evidence-based LTBI strategies, which may contribute to TB elimination in South Korea.
Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Boards of Incheon St. Mary's Hospital, the Catholic University of Korea (IRB No. OC19ZESE0023). Korea Disease Control and Prevention Agency collected informed consent of all participants when they were enrolled according to Tuberculosis Prevention Act.
Footnotes
Funding: The work was supported by the Research Program funded by the Korea Disease Control and Prevention Agency (2020E310100). The funder had no role in the study design and conduct, data analysis and interpretation or preparation of the manuscript.
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Kim JS.
- Formal analysis: Kim HW, Lee Y.
- Investigation: Choi JY, Shin AY, Lee Y, Kang JY, Lee SS, Park JS.
- Methodology: Myong JP, Yim HW, Jeong H, Bae S.
- Project administration: Shim E, In H, Chun C, Kim G.
- Writing - original draft preparation: Kim HW, Min J.
- Writing - review & editing: Min J, Kim JS.
References
- 1.World Health Organization (WHO) Latent Tuberculosis Infection: Updated and Consolidated Guidelines for Programmatic Management. Geneva, Switzerland: WHO; 2018. [PubMed] [Google Scholar]
- 2.Houben RM, Dodd PJ. The global burden of latent tuberculosis infection: a re-estimation using mathematical modelling. PLoS Med. 2016;13(10):e1002152. doi: 10.1371/journal.pmed.1002152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dye C, Glaziou P, Floyd K, Raviglione M. Prospects for tuberculosis elimination. Annu Rev Public Health. 2013;34(1):271–286. doi: 10.1146/annurev-publhealth-031912-114431. [DOI] [PubMed] [Google Scholar]
- 4.GBD Tuberculosis Collaborators. Global, regional, and national burden of tuberculosis, 1990–2016: results from the Global Burden of Diseases, Injuries, and Risk Factors 2016 Study. Lancet Infect Dis. 2018;18(12):1329–1349. doi: 10.1016/S1473-3099(18)30625-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Go U, Park M, Kim UN, Lee S, Han S, Lee J, et al. Tuberculosis prevention and care in Korea: evolution of policy and practice. J Clin Tuberc Other Mycobact Dis. 2018;11:28–36. doi: 10.1016/j.jctube.2018.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Min J, Kim HW, Stagg HR, Lipman M, Rangaka MX, Myong JP, et al. Latent tuberculosis infection screening and treatment in congregate settings (TB FREE COREA): protocol for a prospective observational study in Korea. BMJ Open. 2020;10(2):e034098. doi: 10.1136/bmjopen-2019-034098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Korean Statistical Information Service. [Accessed April 15, 2021]. https://kosis.kr/index/index.do.
- 8.Ministry of Health and Welfare, Republic of Korea. Health and Welfare Statistical Yearbook 2018. Sejong, Korea: Ministry of Health and Welfare; 2018. [Google Scholar]
- 9.Ministry of Health and Welfare, Republic of Korea. National Prevention and Control Policy for Tuberculosis among the Staffs of Postpartum Care Centers Is Implemented. Sejong, Korea: Ministry of Health and Welfare; 2015. [Google Scholar]
- 10.Ministry of Justice, Republic of Korea. Korea Correctional Service Statistics 2018. Gwacheon, Korea: Ministry of Justice; 2018. [Google Scholar]
- 11.Seong SC, Kim YY, Khang YH, Park JH, Kang HJ, Lee H, et al. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017;46(3):799–800. doi: 10.1093/ije/dyw253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Song JH, Huh K, Chung DR. Modern history of tuberculosis in Korea. Infect Chemother. 2019;51(4):414–426. doi: 10.3947/ic.2019.51.4.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kang YA, Lee HW, Yoon HI, Cho B, Han SK, Shim YS, et al. Discrepancy between the tuberculin skin test and the whole-blood interferon γ assay for the diagnosis of latent tuberculosis infection in an intermediate tuberculosis-burden country. JAMA. 2005;293(22):2756–2761. doi: 10.1001/jama.293.22.2756. [DOI] [PubMed] [Google Scholar]
- 14.Edwards PQ. Tuberculin testing of children. Pediatrics. 1974;54(5):628–630. [PubMed] [Google Scholar]
- 15.Jenkins D, Davidson FF. Isoniazid chemoprophylaxis of tuberculosis. Calif Med. 1972;116(4):1–5. [PMC free article] [PubMed] [Google Scholar]
- 16.Starke JR. Universal screening for tuberculosis infection. School's out! JAMA. 1995;274(8):652–653. [PubMed] [Google Scholar]
- 17.Screening for tuberculosis and tuberculosis infection in high-risk populations. Recommendations of the Advisory Council for the Elimination of Tuberculosis. MMWR Recomm Rep. 1995;44(RR-11):19–34. [PubMed] [Google Scholar]
- 18.Targeted tuberculin testing and treatment of latent tuberculosis infection. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. This is a Joint Statement of the American Thoracic Society (ATS) and the Centers for Disease Control and Prevention (CDC). This statement was endorsed by the Council of the Infectious Diseases Society of America. (IDSA), September 1999, and the sections of this statement. Am J Respir Crit Care Med. 2000;161(4 Pt 2):S221–S247. doi: 10.1164/ajrccm.161.supplement_3.ats600. [DOI] [PubMed] [Google Scholar]
- 19.Mori T. Reform of Japan's NTP and its technical perspectives. Kekkaku. 2004;79(10):587–604. [PubMed] [Google Scholar]
- 20.Nakatani H, Fujii N, Mori T, Hoshinot H. Epidemiological transition of tuberculosis and future agenda of control in Japan: results of the Ad-Hoc National Survey of Tuberculosis 2000. Int J Tuberc Lung Dis. 2002;6(3):198–207. [PubMed] [Google Scholar]
- 21.Ushio M. Amendment of tuberculosis prevention law and prospect of tuberculosis control program. Kekkaku. 2005;80(7):541–546. [PubMed] [Google Scholar]
- 22.Korean Educational Development Institute. Data Collection for Education Statistics, 2017. Jincheon, Korea: Korean Educational Development Institute; 2017. [Google Scholar]
- 23.Lönnroth K, Migliori GB, Abubakar I, D'Ambrosio L, de Vries G, Diel R, et al. Towards tuberculosis elimination: an action framework for low-incidence countries. Eur Respir J. 2015;45(4):928–952. doi: 10.1183/09031936.00214014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ronald LA, Campbell JR, Rose C, Balshaw R, Romanowski K, Roth DZ, et al. Estimated impact of World Health Organization latent tuberculosis screening guidelines in a region with a low tuberculosis incidence: retrospective cohort study. Clin Infect Dis. 2019;69(12):2101–2108. doi: 10.1093/cid/ciz188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Campbell JR, Dowdy D, Schwartzman K. Treatment of latent infection to achieve tuberculosis elimination in low-incidence countries. PLoS Med. 2019;16(6):e1002824. doi: 10.1371/journal.pmed.1002824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.European Centre for Disease Prevention and Control (ECDC) Programmatic Management of Latent Tuberculosis Infection in the European Union. Stockholm, Sweden: ECDC; 2018. [Google Scholar]
- 27.National Institute for Health and Care Excellence. Tuberculosis, NICE guideline [NG33] [Accessed April 15, 2021]. https://www.nice.org.uk/guidance/ng33. [PubMed]
- 28.Public Health Agency of Canada. Canadian Tuberculosis Standards. 7th Edition. Ottawa, Canada: Government of Canada; 2014. [Google Scholar]
- 29.US Preventive Services Task Force. Bibbins-Domingo K, Grossman DC, Curry SJ, Bauman L, Davidson KW, et al. Screening for latent tuberculosis infection in adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2016;316(9):962–969. doi: 10.1001/jama.2016.11046. [DOI] [PubMed] [Google Scholar]
- 30.Park S. Prioritizing the Target Population for Screening of Latent Tuberculosis Infection through ICER (Incremental Cost Effectiveness Ratio) in Korea. Seoul, Korea: Yonsei University; 2016. [Google Scholar]
- 31.Korean National Tuberculosis Association. 7th Korea National Health and Nutrition Examination Survey, 1st Year (2016): Tuberculin Survey Support and Quality Control. Seoul, Korea: Korea Centers for Disease Control and Prevention; 2017. [Google Scholar]
- 32.Alsdurf H, Hill PC, Matteelli A, Getahun H, Menzies D. The cascade of care in diagnosis and treatment of latent tuberculosis infection: a systematic review and meta-analysis. Lancet Infect Dis. 2016;16(11):1269–1278. doi: 10.1016/S1473-3099(16)30216-X. [DOI] [PubMed] [Google Scholar]
- 33.Andrews JR, Nemes E, Tameris M, Landry BS, Mahomed H, McClain JB, et al. Serial QuantiFERON testing and tuberculosis disease risk among young children: an observational cohort study. Lancet Respir Med. 2017;5(4):282–290. doi: 10.1016/S2213-2600(17)30060-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gupta RK, Lipman M, Jackson C, Sitch AJ, Southern J, Drobniewski F, et al. Quantitative IFN-γ release assay and tuberculin skin test results to predict incident tuberculosis. a prospective cohort study. Am J Respir Crit Care Med. 2020;201(8):984–991. doi: 10.1164/rccm.201905-0969OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Winje BA, White R, Syre H, Skutlaberg DH, Oftung F, Mengshoel AT, et al. Stratification by interferon-γ release assay level predicts risk of incident TB. Thorax. 2018;73(7):652–661. doi: 10.1136/thoraxjnl-2017-211147. [DOI] [PubMed] [Google Scholar]