Abstract
Background
Despite high coverage (~98%) of universal varicella vaccination (UVV) in the Republic of Korea since 2005, reduction in the incidence rate of varicella is not obvious. The study aimed to evaluate the vaccine effectiveness (VE) of one-dose UVV by timeline and severity of the disease.
Methods
All children born in Korea in 2011 were included for this retrospective cohort study that analyzed insurance claims data from 2011–2018 and the varicella vaccination records in the immunization registry. Adjusted hazard ratios by Cox proportional hazard models were used to estimate the VE through propensity score matching by the month of birth, sex, healthcare utilization rate, and region.
Results
Of the total 421,070 newborns in the 2011 birth cohort, 13,360 were matched for age, sex, healthcare utilization rate, and region by the propensity score matching method. A total of 55,940 (13.29%) children were diagnosed with varicella, with the incidence rate 24.2 per 1000 person-year; 13.4% of vaccinated children and 10.4% of unvaccinated children. The VE of one-dose UVV against any varicella was 86.1% (95% confidence interval [CI], 81.4–89.5) during the first year after vaccination and 49.9% (95% CI, 43.3–55.7) during the 6-year follow-up period since vaccination, resulting in a 7.2% annual decrease of VE. The overall VE for severe varicella was 66.3%. The VE of two-dose compared to one-dose was 73.4% (95% CI, 72.2–74.6).
Conclusion
We found lower long-term VE in one-dose vaccination and waning of effectiveness over time. Longer follow ups of the vaccinated children as well as appropriately designed studies are needed to establish the optimal strategy in preventing varicella in Korea.
Keywords: Chickenpox Vaccine; Immunity, Heterologous; Varicella Zoster Virus Infection; Cohort Studies; Vaccine
Graphical Abstract
INTRODUCTION
Varicella is a highly contagious acute infectious disease caused by the varicella-zoster virus.1,2 Varicella frequently attacks children between 4 to 6 years old, causing various complications.3 Introduction of varicella vaccination into the national immunization program reduced varicella burden of disease in many countries.
Previously, vaccine effectiveness (VE) of varicella vaccines showed a wide range of results, and methods of the estimation varied by study due to lack of follow-up data.4,5,6,7,8,9,10 Few previous studies revealed VE through a follow-up cohort considering medical utilization, which can be heterogeneous, resulting in the difference in vaccination rate.11 Also, VE on complicated varicella infection may differ from the overall varicella infection since subclinical manifestations of varicella infection occasionally do not require medical attention.12
Varicella vaccine was first introduced in 198813 and it was included in the National Immunization Program (NIP) in Korea since 2005.14 The universal varicella vaccination (UVV) with one-dose is recommended to all children between 12 to 15 months.15,16 Although the vaccine coverage rates are generally over 97% in Korea, national notifiable diseases surveillance system reported that the incidence of varicella continues to increase,17 adding substantial disease burden to the public health health.18
Therefore, it is important to assess the VE of UVV with one-dose in Korea and address the public health implication with regard to vaccination strategy. In this study, we aimed to evaluate the VE in a retrospective cohort using the insurance claims data and the immunization registry information from 2011–2018 by adjusting for major characteristics of the vaccinated and unvaccinated population in a country where UVV coverage is estimated higher than 97% nationwide.
METHODS
Study population and data sources
All newborns in Korea from January 1, 2011 to December 31, 2011 were included in the study population. The annual birth cohort of the corresponding year was 470,000 newborns. Demographic characteristics of children such as date of birth, sex, and address were obtained from the National Health Insurance System (NHIS), which is a single insurer that covers over 97% of the Korean population.14,19 All medical claims are reviewed by the Health Insurance Review and Assessment Service (HIRA), using admissions and diagnoses data submitted to the NHIS.
We used the data from the National Immunization Registry, which contains the vaccination status and detailed information such as the vaccination dates and vaccination counts of all children (0–12 years old) receiving vaccines in Korea, obtained from the Korea Centers for Disease Control and Prevention Agency (KDCA). The vaccination status of the cohort was then linked to the medical claims data of HIRA with de-identified personal information. We followed the International Committee of Medical Journal Editors (ICMJE) recommendations throughout the study.20
Study design and inclusion criteria
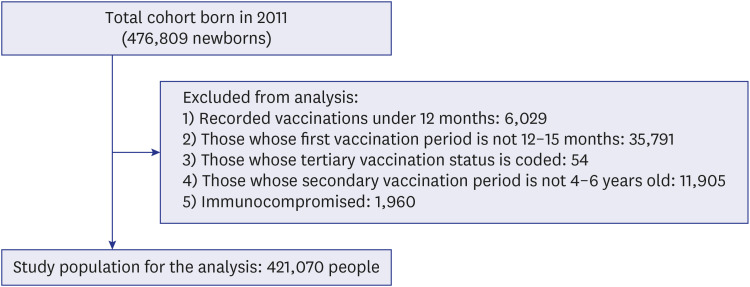
All children born in 2011 were eligible for the study population. Among them, children who did not receive varicella vaccination between 12 to 15 months old, received more than three-doses in total or two-doses within a 4-week window, and immunocompromised children (Supplementary Table 1) were excluded from the analysis (Fig. 1).
Fig. 1. Included study population for the evaluation of the varicella vaccine effectiveness in Korea.
The included study population were followed-up until the endpoint of the cohort (December 31, 2018). Based on the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10), a primary outcome was selected as the diagnosis of varicella (ICD-10: B01). The secondary outcome was diagnosis of severe varicella, which was defined as including people who experienced one or more of the following: 1) admitted to hospital due to varicella, 2) prescribed for acyclovir to treat varicella, or 3) had complications due to varicella: varicella meningitis, varicella encephalomyelitis, varicella pneumonia, varicella keratitis, other varicella complications (ICD-10: B010, B011, B012, B0180, and B0188, respectively).
The breakthrough infections, which were defined as the occurrence of varicella more than 42 days after the vaccination, were included for the evaluation of the incidence.21
Statistical analysis
Frequencies of varicella and severe varicella were measured by vaccination status over time. Crude incidence density and incidence rate ratio of varicella and severe varicella were calculated. In the setting of high vaccination coverage rate (> 95%), we chose to apply propensity score matching (PSM) to compare the VE of the vaccines in order to minimize the risk of selection bias.22 The propensity score consisted of: month of birth, sex, region of address by SIDO, and frequency of out-patient visits per year. The mean propensity score were 0.97 (standard deviation [SD], 0.01) in the vaccinated group and 0.98 (SD, 0.02) in the unvaccinated group. All unvaccinated cases were 1:1 matched for randomly sampled vaccinated group with the nearest neighbor match method.23,24 VE was calculated as (1-hazard ratio)*100, which was estimated by the Cox proportional hazard models.25 We checked the linearity and proportionality by the log-cumulative hazard plots and Shoenfeld residuals in each model.26 In addition, we estimated cumulative VE by year during a 6-year follow-up to estimate the long-term protective effect of the vaccine. The population who received the two-dose vaccination between 4 to 6 years old were compared with the population who received only primary vaccination by the same methods. All statistical methods were performed by SAS 9.4 software (SAS Institute Inc., Cary, NC, USA).
Ethics statement
The institutional review board (IRB) of the Seoul National University Hospital approved this study to conduct under the exemption of IRB review (IRB No. 1809-064-971). Informed consent was waived since we used secondary de-identified data from the KDCA and HIRA as a part of public health research.
RESULTS
Total vaccination rate and incidence of varicella
Among 421,070 births in 2011, 97.5% (410,393) received at least one-dose of varicella vaccines. Of the total, 13.3% (55,940) had diagnoses of varicella during the follow-up period. An average follow-up period was 5.5 years per person, resulting in a varicella incidence of 24.2 per 1,000 person-year in total. Severe varicella occurred in 0.98% (total n = 4,132; 3,449 complicated varicella, 700 hospitalizations, and 240 acyclovir prescriptions). Among the vaccinated population, 26.7% (108,797) received second-dose vaccinations at 4 to 6 years of age.
Demographics of the study population
Table 1 shows the demographic characteristics of the studied cohort by vaccination status. After adjusting for age, sex, and region, the mean of out-patient visit for the unvaccinated group was significantly lower (7.69 per year; SD, 11.90) than the vaccinated group (26.39 per year; SD, 12.78; Table 1). After propensity score matching to estimate the VE of varicella, demographics of unvaccinated and vaccinated group were matched (Supplementary Table 2).
Table 1. Demographic characteristics and varicella infection frequencies of a vaccinated and unvaccinated population.
| Factors | Unvaccinated | Vaccinated | Total | |
|---|---|---|---|---|
| Month of birth | ||||
| 01 | 991 (2.4) | 40,089 (97.6) | 41,080 (9.7) | |
| 02 | 826 (2.5) | 32,618 (97.5) | 33,444 (7.9) | |
| 03 | 919 (2.4) | 37,394 (97.6) | 38,313 (9.1) | |
| 04 | 865 (2.4) | 35,181 (97.6) | 36,046 (8.6) | |
| 05 | 942 (2.7) | 34,183 (97.3) | 35,125 (8.3) | |
| 06 | 878 (2.6) | 32,525 (97.4) | 33,403 (8.0) | |
| 07 | 938 (2.7) | 33,521 (97.3) | 34,459 (8.2) | |
| 08 | 852 (2.4) | 34,748 (97.6) | 35,600 (8.5) | |
| 09 | 923 (2.6) | 34,026 (97.4) | 34,949 (8.3) | |
| 10 | 854 (2.5) | 33,453 (97.5) | 34,307 (8.2) | |
| 11 | 812 (2.4) | 32,540 (97.6) | 33,352 (8.0) | |
| 12 | 877 (2.8) | 30,115 (97.2) | 30,992 (7.4) | |
| Total | 10,677 (2.5) | 410,393 (97.5) | 421,070 (100.0) | |
| Sex | ||||
| Male | 4,601 (52.1) | 210,394 (51.3) | 214,995 (51.3) | |
| Female | 4,227 (47.9) | 199,967 (48.7) | 204,194 (48.7) | |
| Out-patient visits per year (SD) | 7.69 (11.9) | 26.39 (12.8) | 26.00 (13.0) | |
| Any varicellaa | 1,110 (10.4) | 54,830 (13.4) | 55,940 (13.3) | |
| Severe varicellab | 134 (1.3) | 3,998 (1.0) | 4,132 (1.0) | |
SD = standard deviation, OR = odds ratio, CI = confidence interval.
aOR, 1.33 (95% CI, 1.25–1.42), P < 0.001; bOR, 0.77 (95% CI, 0.65–0.92), P = 0.004.
Incidence of varicella and severe varicella
During the studied period, vaccinated group showed higher frequency of varicella diagnosis compared to unvaccinated group (13.4% vs. 10.4%, Table 1), whereas severe varicella was more frequent in the unvaccinated group than in the vaccinated group (1.3% vs. 0.97%, Table 1). The incidence density of breakthrough varicella was 23.3 (95% confidence interval [CI], 23.1–23.4) per 1,000 person-year. The incidence of varicella in the unvaccinated group was 13.7 (95% CI, 13.0–14.5) per 1,000 person-year. The mean age at infection was 2.0 (SD, 1.62) years old in the unvaccinated group and 4.3 (SD, 1.85) years old in the vaccinated group.
VE and its waning immunity
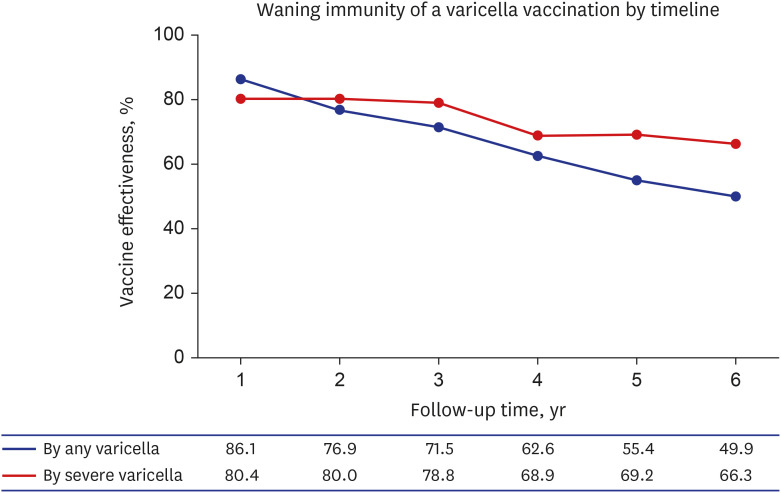
Table 2 describes the overall VE after matching the propensity score by the month of birth, sex, out-patient visits per year, and region. During the first year from vaccination, the overall VE was 86.1%, but it decreased to 62.6% at four years and further to 49.9% at six years from vaccination. The VE for severe varicella was 80.4% in the first vaccinated year and decreased to 66.3% after six years following vaccination (Supplementary Table 2). The VE trend over time is shown in Fig. 2.
Table 2. Estimated vaccine effectivenessa by any varicella or severe varicellab .
| Follow-up year | Any varicella | Severe varicella | ||
|---|---|---|---|---|
| Frequency, % (unvaccinated/vaccinated) | Vaccine effectiveness, % (95% CI) | Frequency, % (unvaccinated/vaccinated) | Vaccine effectiveness, % (95% CI) | |
| 1 | 381/65 (5.91/0.97) | 86.1 (81.4–89.5) | 46/9 (0.69/0.13) | 80.4 (60.0–90.4) |
| 2 | 489/130 (7.59/1.95) | 76.9 (71.6–81.2) | 60/12 (0.90/0.18) | 80.0 (62.8–89.2) |
| 3 | 577/194 (8.95/2.91) | 71.5 (66.1–76.1) | 66/14 (1.00/0.21) | 78.8 (62.2–88.1) |
| 4 | 659/287 (10.22/4.3) | 62.6 (56.6–67.8) | 74/23 (1.12/0.34) | 68.9 (50.4–80.5) |
| 5 | 743/378 (11.53/5.66) | 55.4 (49.1–61.0) | 79/25 (1.19/0.37) | 69.2 (51.4–80.5) |
| 6 | 824/469 (12.79/7.03) | 49.9 (43.3–55.7) | 85/29 (1.28/0.43) | 66.3 (48.2–78.0) |
| Total | 862/515 (13.37/7.71) | 48.3 (41.7–54.2) | 86/30 (0.65/0.23) | 65.1 (46.7–77.1) |
Propensity score matched vaccinated group was compared to the unvaccinated group. The month of birth, sex, regions of address, and frequency of out-patient visits per year was used for the propensity score calculation.
aVaccine effectiveness is estimated via (1-hazard ratio)*100 (%); bSevere varicella was defined as including people who experienced one or more of the following: 1) admitted to hospital due to varicella, 2) prescribed for acyclovir to treat varicella, or 3) had complications due to varicella: varicella meningitis, varicella encephalomyelitis, varicella pneumonia, varicella keratitis, other varicella complications (10th revision of the International Statistical Classification of Diseases and Related Health Problems: B010, B011, B012, B0180, and B0188, respectively).
Fig. 2. Waning immunity of varicella vaccination by any varicella infection and severe varicella infection. Vaccine effectiveness (%, the y-axis) decreases by follow-up time (year, the x-axis) cumulates. Propensity score matched by the month of birth, sex, regions of address, and frequency of out-patient visits per year.
VE of two-dose varicella vaccination
Among the vaccinated population, 2,233 (2.11%) of the two-dose vaccinated group and 23,192 (8.42%) of the one-dose vaccinated group were diagnosed with varicella. The VE of two-dose vaccination compared to the one-dose-only vaccination was 73.4% (95% CI, 72.2–74.6), after being adjusted for month of birth, sex, region, and healthcare utilization. Adjusted two-dose VE for severe varicella was 61.4% (54.0–67.6).
DISCUSSION
In this study, we found a substantial incidence density of breakthrough varicella of 23.3 per 1,000 person-year (95% CI, 23.1–23.4). In a pooled analysis of breakthrough infection, the incidence rate of breakthrough varicella for one-dose vaccination was 8.5 cases per 1,000 person-year (95% CI, 5.3–13.7) and 2.2 cases per 1,000 person-year (95% CI, 0.5–9.3) for two-dose vaccination.27 Through estimating the incidence density, we attempted to present more informative results on varicella by comparing the frequency of varicella in two groups, which was 13.4% in vaccinated group and 10.4% in unvaccinated group.
Breakthrough varicella is likely associated with time-lapse since vaccination, as demonstrated in a previous study that showed higher risk at 5 and 6 years of age among the vaccinated children (P < 0.001).28 This is in line with our finding that varicella VE has decreased over time from 86.1% to 49.9% during the six-year observation period in Korea. The serial decrease in VE by outcome, any varicella and severe varicella, indicates possible waning immunity of the vaccine.29 Concerns about vaccine failure due to waning immunity were suggested by previous studies of specific vaccine types or population cohorts.30,31,32,33 In this study, considering the mean age of varicella was older in the vaccinated population, the waning immunity may be the result from secondary vaccine failure.34,35 Moreover, the reason for the possibility of the waning immunity could originate from not only population outbreaks but also from the vaccine itself.36,37 Therefore, a thorough analysis of the overall process of vaccine development, production, transportation, and storage is strongly required to resolve this issue. Cumulative VE over time since the vaccination is important because the target age should match the main infected age of varicella to control outbreaks. In addition, cumulative VE can help predict the loss of protection and determine the optimal timing of second dose vaccination. In studies conducted in the United States38 and Germany,39 the VE declines over time, and for this reason, discussion of the two-dose strategy began.
We also found higher VE of second-dose vaccination, which was in line with reports from the U.S., Europe, and Asia.33,38,39,40,41 Earlier studies showed a decline in incidence with the introduction of a two-dose program40,42 or a decreased occurrence of outbreaks,16,43 but the actual effectiveness compared to the single-dose vaccine group was rarely studied. In this study, the effectiveness of secondary vaccination was estimated with consistency, enabling comparison with the primary-only vaccinated group. Also, we were able to suggest ideal timing of second-dose varicella vaccination since the estimated decrease of VE by year was presented. Our data suggest the optimal timing of second-dose vaccine needs to be further investigated, given the rapid decline of the VE between three to four years after the first-dose vaccination.44,45 With the consideration about the cost-effectiveness of two-dose vaccination strategy in Korean context,46 the recommended timing of second-dose vaccination should be considered according to this epidemiologic finding.
However, one important question is if there are differences in waning immunity by the varicella vaccine type. Our study results demonstrated that waning immunity soon facilitate discussion about change to two-dose policy in Korea. Before doing this, the VE should be measured by the vaccine type. Four different varicella vaccine types were available to the 2011 birth cohort. PSM analysis cannot be applied for the analysis of VE by the vaccine type because each vaccine type must be matched separately for PSM analysis. After matching birth months, sex, geographic region, and the number of healthcare visits, VE by the vaccine type was analyzed in the retrospective cohort. In the retrospective cohort analysis, we found one specific vaccine type showed a significant higher incidence rate of breakthrough varicella (27.09/1,000 person-year) than the remaining three vaccine types (16.95–18.57/1,000 person-year). Among four vaccine types, the vaccine that contains MAV strain showed the highest incidence, while three remaining vaccine types that contain Oka strain had lower rates,47,48 indicating potential difference in VE between strains.
There are some limitations to this study. Firstly, the cohort consisted of newborns in 2011, so we cannot exclude possible cohort effects of vaccination trends since all participants received varicella vaccination during a similar period. Although the long-term follow-up and the estimation from secondary vaccination, which had a wide range of vaccinated dates (2015 to 2017), can indirectly reflect the vaccination trends in Korea, further cohort studies with longer enrollment periods are needed for confirmation. Second, since the secondary vaccination was evaluated by the data in the immunization registry of NHIS, the effectiveness of secondary vaccination might have been underestimated due to missing data for the secondary vaccination rate. Fortunately, the direction of the effectiveness would not change due to the possibility of a differential misclassification.49 To minimize the risk of misleading, we used the PSM method to adjust for sociodemographic factors which could affect the vaccination status.11,50 Third, because varicella appears to be a relatively mild clinical manifestation, not all people with varicella visit medical institutions.12,51 Because of this, it is possible that the varicella record of the unvaccinated person may have been omitted from the claims data, which was adjusted in our analyses. However, since we defined the presence of immunosuppression by using diagnostic code, and it was indeed challenging to include children taking immunosuppressant drugs from our research scheme.52
Despite these limitations, our study extends previous findings reported from other continents with different settings in the US and Europe, that varicella VE wanes over time, and the two-dose vaccination provides additional protection compared to the one-dose vaccination. The large cohort comprising more than 470,000 children gives larger power to the estimated VE at a national level. In countries where vaccination rates are maintained above 95%, the unvaccinated children group may not be a representative population. Therefore, it is imperative to take this into account when evaluating the effectiveness of a vaccine with a retrospective cohort design in countries with an extremely high vaccination rate. Through the methodologic novelty, we were able to calculate VE in the population with high vaccine coverage in a comprehensive way.
In conclusion, we found lower long-term VE of one-dose UVV and waning of effectiveness over time. Longer follow ups of the vaccinated children as well as appropriately designed studies are needed to establish the optimal strategy in containing varicella in Korea.
Footnotes
Funding: This work was supported by the Korea Disease Control and Prevention Agency [grant number 2017NE240300]. The funder only provided the raw data and research funding and were not involved in data analysis or manuscript writing.
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Choi EH.
- Data curation: Rhie K, Lee JK, Sohn S, Hong K.
- Formal analysis: Hong K.
- Funding acquisition: Choi EH.
- Investigation: Rhie K, Lee JK, Sohn S, Hong K, Han MS, Choe YJ.
- Methodology: Chun BC, Hong K, Sohn S.
- Software: Hong K.
- Validation: Choe YJ, Choi EH.
- Writing - original draft: Hong K.
- Writing - review & editing: Hong K, Choe YJ, Choi EH.
SUPPLEMENTARY MATERIALS
Definitions of underlying immunocompromised conditions according to the ICD-10
Demographic characteristics of vaccinated and non-vaccinated group after propensity score matching for the estimation of varicella vaccine effectiveness
References
- 1.Gilden DH, Kleinschmidt-DeMasters BK, LaGuardia JJ, Mahalingam R, Cohrs RJ. Neurologic complications of the reactivation of varicella-zoster virus. N Engl J Med. 2000;342(9):635–645. doi: 10.1056/NEJM200003023420906. [DOI] [PubMed] [Google Scholar]
- 2.Gnann JW., Jr Varicella-zoster virus: atypical presentations and unusual complications. J Infect Dis. 2002;186(Suppl 1):S91–S98. doi: 10.1086/342963. [DOI] [PubMed] [Google Scholar]
- 3.Liese JG, Grote V, Rosenfeld E, Fischer R, Belohradsky BH, Kries R, et al. The burden of varicella complications before the introduction of routine varicella vaccination in Germany. Pediatr Infect Dis J. 2008;27(2):119–124. doi: 10.1097/INF.0b013e3181586665. [DOI] [PubMed] [Google Scholar]
- 4.Sheridan SL, Quinn HE, Hull BP, Ware RS, Grimwood K, Lambert SB. Impact and effectiveness of childhood varicella vaccine program in Queensland, Australia. Vaccine. 2017;35(27):3490–3497. doi: 10.1016/j.vaccine.2017.05.013. [DOI] [PubMed] [Google Scholar]
- 5.Siedler A, Rieck T, Tolksdorf K. Strong additional effect of a second varicella vaccine dose in children in Germany, 2009–2014. J Pediatr. 2016;173:202–206.e2. doi: 10.1016/j.jpeds.2016.02.040. [DOI] [PubMed] [Google Scholar]
- 6.Varela FH, Pinto LA, Scotta MC. Global impact of varicella vaccination programs. Hum Vaccin Immunother. 2019;15(3):645–657. doi: 10.1080/21645515.2018.1546525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang Y, Zhang L, Sun X, Cao Y, Wang Z, Liu L, et al. Effectiveness and failure rate of the varicella vaccine in an outbreak in Jiangsu, China: a 1:2 matched case-control study. Hum Vaccin Immunother. 2020;16(3):506–512. doi: 10.1080/21645515.2019.1665959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu Y, Liu S, Che X, Liu Y, Zhang X, Du J, et al. Seroepidemiology of varicella in Hangzhou, China in the vaccine era. Hum Vaccin Immunother. 2018;14(10):2464–2471. doi: 10.1080/21645515.2018.1477909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xu Y, Liu Y, Zhang X, Zhang X, Du J, Cai Y, et al. Epidemiology of varicella and effectiveness of varicella vaccine in Hangzhou, China, 2019. Hum Vaccin Immunother. 2021;17(1):211–216. doi: 10.1080/21645515.2020.1769395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Quinn HE, Gidding HF, Marshall HS, Booy R, Elliott EJ, Richmond P, et al. Varicella vaccine effectiveness over 10 years in Australia; moderate protection from 1-dose program. J Infect. 2019;78(3):220–225. doi: 10.1016/j.jinf.2018.11.009. [DOI] [PubMed] [Google Scholar]
- 11.Sohn S, Hong K, Hwang H, Chun BC. Paradoxical health care utilization patterns among children in Korea who did not receive mandatory pneumococcal vaccination. Vaccine. 2021;39(7):1096–1100. doi: 10.1016/j.vaccine.2021.01.012. [DOI] [PubMed] [Google Scholar]
- 12.Chen TM, George S, Woodruff CA, Hsu S. Clinical manifestations of varicella-zoster virus infection. Dermatol Clin. 2002;20(2):267–282. doi: 10.1016/s0733-8635(01)00012-2. [DOI] [PubMed] [Google Scholar]
- 13.Gabutti G, Franchi M, Maniscalco L, Stefanati A. Varicella-zoster virus: pathogenesis, incidence patterns and vaccination programs. Minerva Pediatr. 2016;68(3):213–225. [PubMed] [Google Scholar]
- 14.Choe YJ, Yang JJ, Park SK, Choi EH, Lee HJ. Comparative estimation of coverage between national immunization program vaccines and non-NIP vaccines in Korea. J Korean Med Sci. 2013;28(9):1283–1288. doi: 10.3346/jkms.2013.28.9.1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oh SH, Choi EH, Shin SH, Kim YK, Chang JK, Choi KM, et al. Varicella and varicella vaccination in South Korea. Clin Vaccine Immunol. 2014;21(5):762–768. doi: 10.1128/CVI.00645-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee YH, Choe YJ, Cho SI, Park H, Bang JH, Lee JK. Effects of one-dose varicella vaccination on disease severity in children during outbreaks in Seoul, Korea. J Korean Med Sci. 2019;34(10):e83. doi: 10.3346/jkms.2019.34.e83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee YH, Choe YJ, Cho SI, Bang JH, Oh MD, Lee JK. Increasing varicella incidence rates among children in the Republic of Korea: an age-period-cohort analysis. Epidemiol Infect. 2019;147:e245. doi: 10.1017/S0950268819001389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Choi JK, Park SH, Park S, Choi SM, Kim SH, Lee DG, et al. Trends in varicella and herpes zoster epidemiology before and after the implementation of universal one-dose varicella vaccination over one decade in South Korea, 2003–2015. Hum Vaccin Immunother. 2019;15(11):2554–2560. doi: 10.1080/21645515.2019.1603985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sohn S, Hong K, Chun BC. Evaluation of the effectiveness of pneumococcal conjugate vaccine for children in Korea with high vaccine coverage using a propensity score matched national population cohort. Int J Infect Dis. 2020;93:146–150. doi: 10.1016/j.ijid.2020.01.034. [DOI] [PubMed] [Google Scholar]
- 20.Editors ICoMJ. Recommendations for the Conduct, Reporting, Editing and Publication of Scholarly Work in Medical Journals. 2019. [PubMed] [Google Scholar]
- 21.Leung J, Broder KR, Marin M. Severe varicella in persons vaccinated with varicella vaccine (breakthrough varicella): a systematic literature review. Expert Rev Vaccines. 2017;16(4):391–400. doi: 10.1080/14760584.2017.1294069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arriola CS, Anderson EJ, Baumbach J, Bennett N, Bohm S, Hill M, et al. Does influenza vaccination modify influenza severity? Data on older adults hospitalized with influenza during the 2012–2013 season in the United States. J Infect Dis. 2015;212(8):1200–1208. doi: 10.1093/infdis/jiv200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Caliendo M, Kopeinig S. Some practical guidance for the implementation of propensity score matching. J Econ Surv. 2008;22(1):31–72. [Google Scholar]
- 24.Randolph JJ, Falbe K, Manuel AK, Balloun JL. A step-by-step guide to propensity score matching in R. PARE. 2014;19(1):18. [Google Scholar]
- 25.Fox J. Cox proportional-hazards regression for survival data. An R and S-PLUS companion to applied regression. Seattle, WA, USA: University of Washington; 2002. [Google Scholar]
- 26.Collett D. Modelling Survival Data in Medical Research. Boca Raton, FL, USA: CRC Press; 2015. [Google Scholar]
- 27.Zhu S, Zeng F, Xia L, He H, Zhang J. Incidence rate of breakthrough varicella observed in healthy children after 1 or 2 doses of varicella vaccine: Results from a meta-analysis. Am J Infect Control. 2018;46(1):e1–e7. doi: 10.1016/j.ajic.2017.07.029. [DOI] [PubMed] [Google Scholar]
- 28.Huang WC, Huang LM, Chang IS, Tsai FY, Chang LY. Varicella breakthrough infection and vaccine effectiveness in Taiwan. Vaccine. 2011;29(15):2756–2760. doi: 10.1016/j.vaccine.2011.01.092. [DOI] [PubMed] [Google Scholar]
- 29.Asano Y, Suga S, Yoshikawa T, Kobayashi I, Yazaki T, Shibata M, et al. Experience and reason: twenty-year follow-up of protective immunity of the Oka strain live varicella vaccine. Pediatrics. 1994;94(4 Pt 1):524–526. [PubMed] [Google Scholar]
- 30.Di Pietrantonj C, Rivetti A, Marchione P, Debalini MG, Demicheli V. Vaccines for measles, mumps, rubella, and varicella in children. Cochrane Database Syst Rev. 2020;4(4):CD004407. doi: 10.1002/14651858.CD004407.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dinleyici EC, Kurugol Z, Kara A, Tezer H, Tas MA, Guler E, et al. Children with breakthrough varicella infection requiring hospitalization in Turkey (VARICOMP Study 2008–2013) Vaccine. 2015;33(32):3983–3987. doi: 10.1016/j.vaccine.2015.06.029. [DOI] [PubMed] [Google Scholar]
- 32.Andrade AL, da Silva Vieira MA, Minamisava R, Toscano CM, de Lima Souza MB, Fiaccadori F, et al. Single-dose varicella vaccine effectiveness in Brazil: a case-control study. Vaccine. 2018;36(4):479–483. doi: 10.1016/j.vaccine.2017.12.011. [DOI] [PubMed] [Google Scholar]
- 33.Chan YD, Edmunds WJ, Chan HL, Wong ML, Au KA, Chuang SK, et al. Varicella vaccine dose depended effectiveness and waning among preschool children in Hong Kong. Hum Vaccin Immunother. 2020;16(3):499–505. doi: 10.1080/21645515.2019.1663121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lopez AS, Guris D, Zimmerman L, Gladden L, Moore T, Haselow DT, et al. One dose of varicella vaccine does not prevent school outbreaks: is it time for a second dose? Pediatrics. 2006;117(6):e1070–e1077. doi: 10.1542/peds.2005-2085. [DOI] [PubMed] [Google Scholar]
- 35.Bonanni P, Gershon A, Gershon M, Kulcsár A, Papaevangelou V, Rentier B, et al. Primary versus secondary failure after varicella vaccination: implications for interval between 2 doses. Pediatr Infect Dis J. 2013;32(7):e305–e313. doi: 10.1097/INF.0b013e31828b7def. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rentier B, Gershon AA European Working Group on Varicella. Consensus: varicella vaccination of healthy children--a challenge for Europe. Pediatr Infect Dis J. 2004;23(5):379–389. doi: 10.1097/01.inf.0000122606.88429.8f. [DOI] [PubMed] [Google Scholar]
- 37.Gershon AA. Live-attenuated varicella vaccine. Infect Dis Clin North Am. 2001;15(1):65–81. doi: 10.1016/s0891-5520(05)70268-3. [DOI] [PubMed] [Google Scholar]
- 38.Vázquez M, LaRussa PS, Gershon AA, Niccolai LM, Muehlenbein CE, Steinberg SP, et al. Effectiveness over time of varicella vaccine. JAMA. 2004;291(7):851–855. doi: 10.1001/jama.291.7.851. [DOI] [PubMed] [Google Scholar]
- 39.Liese JG, Cohen C, Rack A, Pirzer K, Eber S, Blum M, et al. The effectiveness of varicella vaccination in children in Germany: a case-control study. Pediatr Infect Dis J. 2013;32(9):998–1004. doi: 10.1097/INF.0b013e31829ae263. [DOI] [PubMed] [Google Scholar]
- 40.Barrenechea GG, Bastos LS. Evaluation of impact of one dose varicella vaccine on the incidence of chickenpox in Argentina. Vaccine. 2020;38(2):330–335. doi: 10.1016/j.vaccine.2019.10.003. [DOI] [PubMed] [Google Scholar]
- 41.Marin M, Marti M, Kambhampati A, Jeram SM, Seward JF. Global varicella vaccine effectiveness: a meta-analysis. Pediatrics. 2016;137(3):e20153741. doi: 10.1542/peds.2015-3741. [DOI] [PubMed] [Google Scholar]
- 42.Pan X, Shu M, Ma R, Fang T, Dong H, Sun Y, et al. Varicella breakthrough infection and effectiveness of 2-dose varicella vaccine in China. Vaccine. 2018;36(37):5665–5670. doi: 10.1016/j.vaccine.2018.05.025. [DOI] [PubMed] [Google Scholar]
- 43.Leung J, Lopez AS, Blostein J, Thayer N, Zipprich J, Clayton A, et al. Impact of the US two-dose varicella vaccination program on the epidemiology of varicella outbreaks: data from nine states, 2005–2012. Pediatr Infect Dis J. 2015;34(10):1105–1109. doi: 10.1097/INF.0000000000000821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yin M, Xu X, Liang Y, Ni J. Effectiveness, immunogenicity and safety of one vs. two-dose varicella vaccination: a meta-analysis. Expert Rev Vaccines. 2018;17(4):351–362. doi: 10.1080/14760584.2018.1433999. [DOI] [PubMed] [Google Scholar]
- 45.Perella D, Wang C, Civen R, Viner K, Kuguru K, Daskalaki I, et al. Varicella vaccine effectiveness in preventing community transmission in the 2-dose era. Pediatrics. 2016;137(4):e20152802. doi: 10.1542/peds.2015-2802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Esmaeeli S, Yaghoubi M, Nojomi M. Cost-effectiveness of varicella vaccination program in Iran. Int J Prev Med. 2017;8(1):103. doi: 10.4103/ijpvm.IJPVM_295_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lee YH, Choe YJ, Cho SI, Kang CR, Bang JH, Oh MD, et al. Effectiveness of varicella vaccination program in preventing laboratory-confirmed cases in children in Seoul, Korea. J Korean Med Sci. 2016;31(12):1897–1901. doi: 10.3346/jkms.2016.31.12.1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kim SH, Lee HJ, Park SE, Oh SH, Lee SY, Choi EH. Seroprevalence rate after one dose of varicella vaccine in infants. J Infect. 2010;61(1):66–72. doi: 10.1016/j.jinf.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 49.Ozasa K. The effect of misclassification on evaluating the effectiveness of influenza vaccines. Vaccine. 2008;26(50):6462–6465. doi: 10.1016/j.vaccine.2008.06.039. [DOI] [PubMed] [Google Scholar]
- 50.Emch M, Ali M, Park JK, Yunus M, Sack DA, Clemens JD. Relationship between neighbourhood-level killed oral cholera vaccine coverage and protective efficacy: evidence for herd immunity. Int J Epidemiol. 2006;35(4):1044–1050. doi: 10.1093/ije/dyl100. [DOI] [PubMed] [Google Scholar]
- 51.Salmon DA, Dudley MZ, Glanz JM, Omer SB. Vaccine hesitancy: causes, consequences, and a call to action. Vaccine. 2015;33(Suppl 4):D66–D71. doi: 10.1016/j.vaccine.2015.09.035. [DOI] [PubMed] [Google Scholar]
- 52.Kuhle S, Kirk SF, Ohinmaa A, Veugelers PJ. Comparison of ICD code-based diagnosis of obesity with measured obesity in children and the implications for health care cost estimates. BMC Med Res Methodol. 2011;11:173. doi: 10.1186/1471-2288-11-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Definitions of underlying immunocompromised conditions according to the ICD-10
Demographic characteristics of vaccinated and non-vaccinated group after propensity score matching for the estimation of varicella vaccine effectiveness