Abstract
Background
Diastasis recti abdominis (DRA) is a condition affecting many post-partum women. The aim of this study was to evaluate long-term results of surgical repair of DRA in a cohort of post-partum women.
Methods
Sixty post-partum women with DRA and training-resistant core dysfunctions were included. Surgical repair was performed with suture plication of the linea alba. Abdominal core function was evaluated with the abdominal trunk function protocol (ATFP) including a self-report questionnaire and seven functional tests. Urinary incontinence and quality of life were evaluated with the Urogenital Distress Inventory (UDI-6), the Incontinence Impact Questionnaire (IIQ-7) and the SF-36 questionnaire. Follow-up was performed at 1 and 3 years after surgery.
Results
Response rate at the 3-year follow-up was 86.7 per cent for the disability rating index (DRI) questionnaire; and 71.7 per cent for the ATFP, UDI-6, IIQ-7 and SF-36 questionnaires. All DRI parameters were improved (P < 0.001) after 3 years of follow-up compared with preoperative values. The functional tests in the ATFP showed an improvement in core muscle strength and stability (P < 0.001), back muscle strength (P < 0.001) and abdominal muscle strength (P = 0.002) compared to preoperative values as well as an improvement of core muscle strength and stability compared with the 1-year follow-up values (P = 0.003). UDI-6 and IIQ-7 results were improved (P < 0.001 and P = 0.004) compared with preoperative values and showed consistent values compared with the 1-year follow-up (P = 0.09 and P = 1.0). Quality of life measured with SF-36 was improved compared with preoperative values and showed consistent values compared with the 1-year follow-up.
Conclusion
The functional improvement of surgical reconstruction of the DRA persisted for 3 years in this series of post-partum women with DRA.
Post-partum diastasis recti abdominis may cause abdominal core instability symptoms. Surgical repair provides a permanent functional improvement.
Introduction
Diastasis recti abdominis (DRA) is a common condition after pregnancy, affecting approximately one-third of post-partum women1–4. It is defined as a persisting widened and weakened linea alba caused by mechanical and hormonal changes during pregnancy and can present as a bulging or sagging of the abdominal midline. DRA is one of several pathological components5 of a generally stretched abdominal wall after pregnancy and can predispose for abdominal core dysfunctions such as back pain, abdominal core muscle weakness and poor posture6–11. The abdominal core, defined as the circumferential soft tissues of the diaphragm superiorly, the pelvic floor inferiorly and the abdominal wall and flank anterolaterally12, is crucial for upholding the posture and abdominopelvic visceral function. Risk factors for developing DRA include multiparity, advanced maternal age, caesarean section and collagen disposition13,14.
The management of DRA has gained increasing attention during the last decade and studies have reported beneficial short-term results from surgical repair of DRA15–17. Multiple reviews have been published but consensus regarding best treatment is still lacking, due to conflicting results and insufficient follow-up time18–20. Despite this, national guidelines stating recommendations of DRA management have been presented21,22. In general, the first-line treatment recommendation is core-stability training13,23,24. The optimal method and duration of core training are still under debate and the results from core training vary across studies13,23,25–27. If core training fails, guidelines propose surgical repair in certain circumstances, such as a specified minimum of inter-recti distance (IRD) and a specified maximum BMI21,22. Surgical reconstruction has been reported to recover abdominal core function in patients with training-resistant core dysfunction. Studies have shown different surgical methods, open as well as laparoscopic repairs, to be successful regarding prevention of DRA recurrence and postoperative complications16,17,28.
In a previous study, the effect of surgical repair of DRA, defined as greater than 30 mm at the widest distance, was examined in a cohort of 60 post-partum women with training-resistant core instability symptoms, with or without diagnosed concomitant ventral hernias. The study was conducted in Stockholm from 2015 to 2017. DRA was evaluated with ultrasonography as well as CT before surgery and at the 1-year follow-up, and no recurrences were seen17. Functional outcomes were assessed with questionnaires regarding physical function, urinary incontinence and quality of life, as well as seven physical tests monitored by a physiotherapist. Surgical repair was performed with a suture repair of the widened linea alba using absorbable sutures. The 1-year follow-up showed significant improvements in abdominal core function, regardless of the preoperative inter-recti distance, as well as a decrease in urinary incontinence and improved quality of life (QoL), implying that surgical repair of DRA restores the anatomy and recovers abdominal core function17.
The aim of this 3-year follow-up was to determine the long-term effect of surgical reconstruction regarding abdominal core function, urinary incontinence and QoL, with the hypothesis that surgical repair provides a permanent functional improvement. The results may indicate if surgery could be a strategy to recommend for patients with DRA combined with training-resistant core dysfunctions.
Methods
Study population
The study population, which has been presented previously17, consisted of 60 post-partum women with symptomatic DRA recruited between 2015 and 2017.
The surgical reconstruction technique was performed as a double-row suture duplication of the linea alba using absorbable Quill™ PDO suture (Angiotech, Reading, Pennsylvania, USA). Concomitant midline hernias were closed separately with a suture repair as well as reduced in the duplicate. Incision technique varied depending on the participant’s anatomical conditions and surgeon’s preference of incision technique. The Regional Ethics Committee, Stockholm-Karolinska Institute approved the study, and the local ethics committee approved all procedures (Dnr. 2015/1753–31).
Evaluation of outcome
The primary outcome was abdominal core function, evaluated with a self-report questionnaire, the disability rating index (DRI) where the ability to perform 12 different daily activities are rated with a visual analogue scale (VAS)29, and seven different functional tests instructed and monitored by a physiotherapist. The seven functional tests cover: back muscle strength; abdominal muscle strength; left core stability; right core stability; ventral core stability, evaluated with the trunk muscle strength and stability test (TMSST); pelvic stability, evaluated with the active straight leg raising (ASLR) test including evaluation of back pain and pelvic tip; and pelvic pain, evaluated with the posterior pelvic pain provocation (4P) test30,31.
The DRI questionnaire and the seven functional tests were compiled in a protocol, the abdominal trunk function protocol (ATFP) (Supplementary material)17. Secondary outcomes were urinary incontinence, evaluated with the self-report questionnaires, Urogenital Distress Inventory (UDI-6) and Incontinence Impact Questionnaire (IIQ-7)32; quality of life (QoL), evaluated with the SF-36 questionnaire33; as well as recurrence and postoperative complications, evaluated clinically at 3-year follow-up. All participants were given the opportunity to express opinions regarding experiences from the postoperative rehabilitation and changes in their general health situation and gastrointestinal function at the 3-year clinical follow-up. Replies were documented in the patients’ medical record. Primary and secondary outcomes were evaluated prior to, and 1 and 3 years after surgery.
Statistical analyses
Paired t tests and Wilcoxon signed rank tests were used to analyse changes in symptoms at 3-year follow-up compared with values from before surgery and the results from 1-year follow-up. McNemars test was used to evaluate contingency of dichotomous variables. The tests were all two-sided and considered statistically significant at a level of P ≤ 0.050. The DRI parameters were investigated individually, and the total DRI score was used for comparison with preoperative results and the results at 1-year follow-up. The SF-36 results were compared with preoperative and 1-year follow-up results as well as comparison with the normative Swedish female population. Association between preoperative symptoms and symptoms at 1-year follow-up was investigated against symptoms at 3-year follow-up with linear regression. The statistical analyses were performed using Stata®, version 12.1 (Stata Corp, College Station, Texas, USA)
Results
Preoperative demographics are summarized in Table 1. Median age at time for surgery was 39.0 (range 20.5–53) years. Response rate at 3-year follow up was 87 per cent (52 of 60 patients) for the DRI questionnaire; and 72 per cent (43 of 60 patients) for the UDI-6 and IIQ-7 questionnaire, the ATFP and the SF-36 questionnaire. Nine participants (15 per cent) answered only the DRI questionnaire. There were 17 dropouts for the functional tests. One participant was undergoing chemotherapy for a breast malignancy, one participant was rehabilitating from a disc hernia, one participant was under psychiatric treatment, two patients did not want to continue participating in the study and the remaining twelve participants avoided attending the hospital due to the COVID-19 pandemic regulations. A fifth of all participants (12 patients), who had suffered from obstipation, bloating, slow bowel symptoms and long transit time prior to surgery, reported improved bowel function after surgery. Some participants (15 patients) found the rehabilitation programme tedious or uninspiring.
Table 1.
Preoperative characteristics of the 60 patients who underwent surgery for diastasis recti abdominis
| Preoperative characteristics | Results |
|---|---|
| Female patients * | 60 (100) |
| Age (years) † | 38.8(5.5) |
| BMI (kg/m2) | 22.6 (17.2–36.0) |
| Deliveries | 2 (1–5) |
| Vaginal | 2 (1–4) |
| Caesarean | 2 (1–4) |
| Months between last delivery and surgery | 34 (12–192) |
| Months training before surgery | 7 (3–24) |
| Rectus diastasis width (mm) | |
| Ultrasound scan | 45 (30–90) |
| CT scan | 50 (10–100) |
| At surgery | 45 (30–90) |
| Ventral hernia * | 45 (75) |
Values are median (range) unless indicated otherwise;
*values are number (percentage);
†values are mean(s.d.).
DRA recurrence rates and postoperative complications
There were no reported recurrences or long-term postoperative complications at the 3-year follow-up, examined clinically by the physiotherapist during the functional tests (ATFP). At the time of the 3-year follow-up three additional patients, adding to the previous four patients, expressed considerations regarding cosmetic issues, which was not considered as a postoperative complication.
Abdominal trunk function protocol
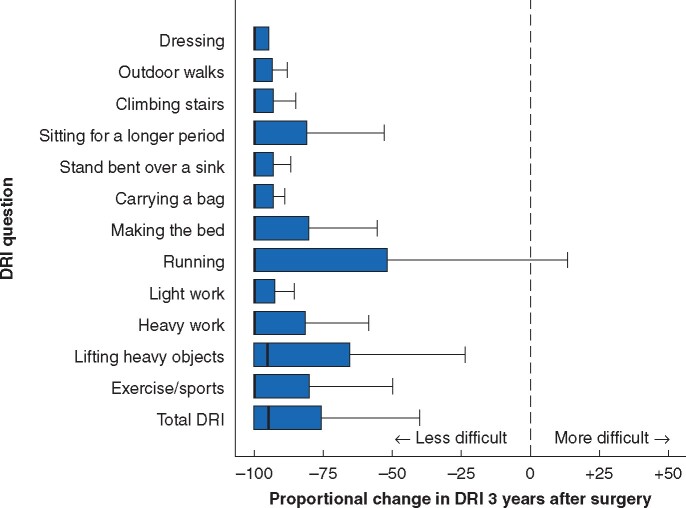
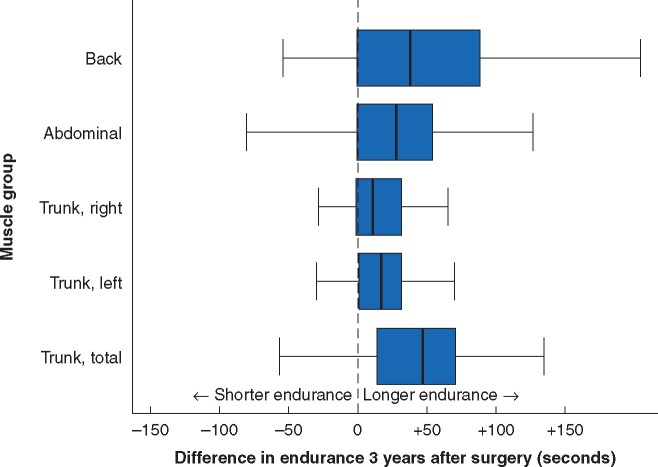
The core function results are summarized in Table 2. In the self-reported DRI, all patients (52 of 52) reported fewer symptoms 3 years after surgery, with a score that was 82.3 (range 74.9– 89.7) per cent lower than prior to surgery (Fig. 1). Fifteen patients reported a higher score than at the 1-year follow-up. There were no significant changes in any of the 12 DRI parameters between 1- and 3-year follow-up, except for doing dishes, heavy lifts and exercise/sports, where the score was significantly improved, as was the total DRI score. Evaluation of the functional tests monitored by a physiotherapist showed significantly improved performance regarding back muscle strength, abdominal muscle strength and core stability, compared with preoperative results in a majority of the participants (33 of 42, 79 per cent), while two thirds of patients (28 of 42, 67 per cent) had a score equal to or higher than that at the 1-year follow-up (Table 2, Fig. 2). There was a significant improvement in core muscle strength and stability (TMSST): 120 (range 11–240) seconds at 3 years after surgery compared with 74 (range 3–180) seconds 1 year after surgery and 60 (range 0–180) seconds prior to surgery. No significant changes in back muscle or abdominal muscle strength were found, between 1- and 3-year follow-up. Evaluation of the pelvic tip and performance difficulties, two components of the ASLR test, showed a significant increase between 3-year follow-up and the other two time-points. None of the other components of the ASLR and 4P tests showed significant changes.
Table 2.
Abdominal trunk function protocol including disability rating index, Urogenital Distress Inventory, and Incontinence Impact Questionnaire, before, 1 year and 3 years after surgery for DRA
| Before surgery | 1-year follow-up | 3-year follow-up |
P
‡
|
|||
|---|---|---|---|---|---|---|
| 1 year after versus before surgery | 3 years after versus before surgery | 3 years after versus 1 year after surgery | ||||
| Abdominal trunk function protocol | n = 57 | n = 55 | n = 52 | |||
| Specific DRI† | ||||||
| Get dressed and undressed without help | 1 (0–70) | 0 (0–10) | 0 (0–13) | 0.006 | 0.001 | 0.13 |
| Taking walks | 4 (0–95) | 0 (0–44) | 0 (0–50) | <0.001 | <0.001 | 0.13 |
| Walk in stairs | 4 (0–94) | 0 (0–44) | 0 (0–42) | <0.001 | <0.001 | 0.31 |
| Sitting down for a longer period | 28 (0–96) | 0 (0–52) | 0 (0–73) | <0.001 | <0.001 | 0.26 |
| Stand bentover doing dishes | 40 (0–100) | 0 (0–53) | 0 (0–47) | <0.001 | <0.001 | 0.01 |
| Carry a suitcase or bag | 29 (0–83) | 1 (0–49) | 0 (0–90) | <0.001 | <0.001 | 0.02 |
| Making the bed | 13 (0–84) | 0 (0–45) | 0 (0–39) | <0.001 | <0.001 | 1.00 |
| Running | 49 (0–100) | 1 (0–96) | 0 (0–100) | <0.001 | <0.001 | 0.72 |
| Light manual labour | 21 (0–100) | 0 (0–50) | 0 (0–46) | <0.001 | <0.001 | 0.23 |
| Heavy manual labour | 64 (0–100) | 4 (0–98) | 0 (0–83) | <0.001 | <0.001 | 0.18 |
| Heavy lifts | 63 (1–100) | 10 (0–98) | 0 (0–98) | <0.001 | <0.001 | 0.02 |
| Exercise/sports | 54 (1–100) | 5 (0–94) | 0 (0–88) | <0.001 | <0.001 | 0.03 |
| Total DRI (0–1200 points) | 401 (19–1051) | 50 (0–696) | 0 (0–656) | <0.001 | <0.001 | 0.03 |
| Physiological tests | n = 53 | n = 55 | n = 43 | |||
| Back strength (seconds) | 75 (0–240) | 113 (0–240) | 138 (32–240) | <0.001 | <0.001 | 0.13 |
| Abdominal strength (seconds) | 49 (0–240) | 66 (15–240) | 79 (0–240) | <0.001 | 0.002 | 1.0 |
| Core stability, side plank (seconds) | 40 (0–120) | 56 (10–115) | 70 (6–118) | <0.001 | 0.002 | 0.75 |
| Core muscle strength and stability test (seconds) | 60 (0–180) | 74 (3–180) | 120 (11–240) | 0.004 | <0.001 | 0.003 |
| Difficulties with active straight leg raising (1–5 points) | 1 (1–5) | 1 (0–2) | 1 (1–3) | <0.001 | 0.18 | 0.01 |
| Pain during straight leg raising* | 8 (17) | 3 (6) | 4 (9) | 0.16§ | 0.32§ | 0.41§ |
| Pelvic tip during straight leg raising* | 9 (24) | 9 (17) | 22 (51) | 0.32§ | 0.03§ | 0.005§ |
| Pain during pelvic provocation* | 12 (24) | 3 (6) | 6 (14) | 0.008§ | 0.48§ | 0.10§ |
| Urogenital Distress Inventory (UDI-6) | 5 (0–16) | 2 (0–13) | 3 (0–13) | 0.001 | <0.001 | 0.09 |
| Incontinence Impact Questionnaire (IIQ-7) | 2 (0–18) | 0 (0–17) | 0 (0–17) | 0.001 | 0.004 | 1.0 |
Values are medians (range) unless otherwise indicated.
*values in parentheses are percentages.
The disability rating index (DRI) was standardized recorded on visual analogue scales measured in millimetres, and provided a score with a range of 0–100 for each activity, where 0 represented no difficulties at all performing the specific task, and 100 not being able to perform the task at all.
Wilcoxon signed rank test, except
McNemars test.
Fig. 1.
Proportional change in disability rating index (DRI) 3 years after surgery compared with preoperative values
Fig. 2.
Proportional change in endurance during the functional tests in the abdominal trunk function protocol
Quality of life
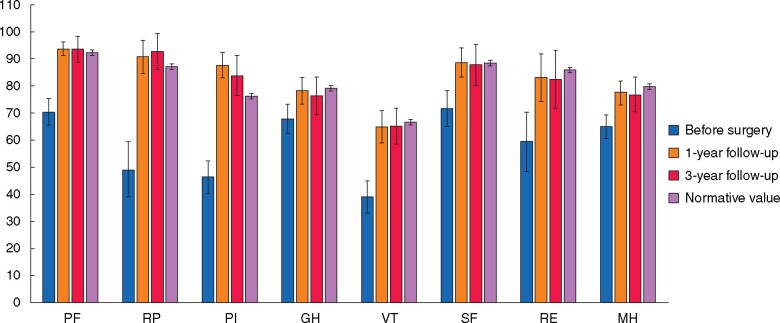
Figure 3 shows the SF-36 subscales, prior to surgery, at 1-year follow-up, at 3-year follow-up and the expected ratings for the normative Swedish female population34. Preoperative ratings for the studied cohort were significantly lower than those for the normative population in all subscales. Postoperative ratings were increased to a level significantly higher than or equal to the ratings of the normative female population. There were no significant changes in any subscale between the 1- and the 3-year follow-up after surgery.
Fig. 3.
SF-36 assessment of quality of life
PF, physical function; RP, role physical; PI, pain; GH, general health; VT, vitality; SF, social functioning; RE, role emotional; MH, mental health.
Urinary incontinence
Urinary incontinence was evaluated with the self-report questionnaires UDI-6 and IIQ-7. Results from the UDI-6 showed a significant improvement compared with preoperative results (P < 0.001), but no significant change between 1- and 3-year follow-up was observed (P = 0.09). Results from the IIQ-7 showed a significant improvement from the preoperative results (P = 0.004), and no significant change compared with 1-year follow-up (P = 1.00) (Table 2).
Discussion
DRA is a condition affecting a large proportion of the female post-partum population, which may cause debilitating symptoms such as back pain, abdominal muscle weakness, urinary incontinence and decreased QoL35. This long-term follow-up study shows that surgical repair of the weakened and stretched abdominal wall results in a long-term improvement in core stability, abdominal muscle strength and back muscle strength, as well as an improvement in QoL. The high prevalence of postpartum DRA7 has been a neglected public health problem. Many women have suffered in vain from training-resistant symptoms and this study suggests that surgical repair is an effective option that should be considered in the treatment of DRA.
The detailed and comprehensive assessment methods used in this study include self-reported physical function, and several aspects of core function evaluated objectively by a physiotherapist monitoring examinations of back muscle strength, abdominal muscle strength, core stability and pelvic stability, compiled in the ATFP. The ATFP covers a panorama of functional symptoms associated with DRA. Furthermore, evaluation of QoL and urinary incontinence were performed. The multiple aspects explored in this study give a broad understanding of the complex symptomatology associated with DRA. The ATFP is a suitable assessment instrument for research situations but may be too extensive for the daily clinical situation. QoL has been reported to improve after abdominoplasty due to perception of a cosmetic improvement36. There were no differences in QoL outcomes between the different surgical approaches in this study, indicating that cosmetic improvement alone was unlikely to explain the persistent improved QoL.
There was a significant improvement in urinary incontinence in the terms of decreased urinary leakage at both 1- and 3-year follow-up. This finding indicates an association between surgical repair of the anterior abdominal wall and stabilization of the pelvic floor, which underlines that the abdominal canister is a collaborating system of interacting muscle groups. A surgical intervention on one muscle group could possibly provide benefits to other parts of this cooperating system.
The statistically significant improvement from preoperative results in most evaluated parameters suggests a persistent positive outcome. One unexpected finding was the significant increase in pelvic tip and difficulty performing the ASLR test at the 3-year follow-up compared with the preoperative and 1-year follow-up outcomes. The pelvic tip exercise measures pelvic stability and monitors the combined function of pelvic, gluteal, back and abdominal muscle groups. There is no available information regarding training frequency during the postoperative period in this study, and sparse physical training can therefore not be excluded as a possible explanation to this finding. There were four physiotherapists involved in the 3-year follow-up which could imply a theoretical risk of inter-rater variability, although the instructions to the physiotherapist in the protocol are detailed and designed to avoid any variation of the evaluation procedure.
In the present study, only six participants had a BMI greater than 30 kg/m2 at inclusion and extrapolation of results to obese patients should, thus, be made with caution. There were no observed differences in results in sub-analyses stratified by BMI greater than or less than 25 kg/m2 (data not shown). The clinical manifestations of DRA were evaluated: physical function as well as clinical signs such as bulging, doming or sagging. Radiological signs of recurrence cannot be excluded but would then have been clinically insignificant and not warrant any additional treatment, surgical or otherwise. There were no reports of late postoperative complications and there were no recurrences of DRA in this study, which is in line with comparable studies19. Even though the functional improvement was statistically significant there are always risks associated with surgery which should be taken into consideration when deciding the best line of treatment.
A possible explanation to the reported improved bowel function may be increased abdominal muscle strength affecting the intra-abdominal pressure which could prevent intestinal dilatation. Persistent change in intra-abdominal pressure after surgical repair of DRA has not been described in earlier studies28 but more research is needed to examine this further. Future studies exploring whether surgical repair of DRA resulting in decreased intra-abdominal space could lead to improved bowel function are warranted.
The monotony and tediousness of the standardized rehabilitation programme reported by many women could affect the compliance with the postoperative rehabilitation and a new rehabilitation programme has therefore been designed with increasing progressive exercises and a more dynamic and, hopefully, inspiring approach, that will be evaluated in a future study.
During the last decade DRA has gained attention as a debilitating clinical issue for a large amount of the female population. As DRA and its consequences are gaining more attention, national guidelines are beginning to emerge. Recommendations for national guidelines have been presented from Germany22 and Sweden21. The Americas Hernia Society has presented an advanced programme for abdominal core health management37. The first line of treatment is core-stability training but the impact of training in general, and what specific training to recommend, is still under debate, and studies have shown diverging results. Improvement in core function after training has been reported38,39, while contradicting studies report no improvement from training25,27.
Studies that examine the change of IRD after training also have conflicting results, where some recent studies report decreased IRD after training24,40, while older studies report no change in IRD27. The training methods as well as the evaluation methods in these studies vary, making comparisons difficult. The recent reported improvement could be the result of more adequate assessment methods, such as ultrasonography prior to digital width measurement41,42, as well as evaluating core function and not solely measuring the IRD.
Research suggests that the deep core-muscle training including preactivation of the inner unit, for example transverse abdominis muscles, prior to heavier exercises is an effective training method to rebuild core stability23,43. Deep core-muscle stabilizing training could be recommended as a first-line treatment and is useful as a tool for sorting symptomatic DRA to either training or to surgery. The benefit from core training is presumably mainly due to improved core control and strength, and not due to a decrease of IRD, but future studies are needed to explore this further. Regardless of training method, surgical repair becomes a relevant alternative when core training is insufficient.
Management strategies differ today, not only between but also within countries, emphasizing the need for guidelines. DRA is still mainly classified as a cosmetic issue and an American study revealed that the majority of insurance companies did not cover surgical repair of DRA regardless of symptoms44. The financial aspect is therefore highly relevant when developing guidelines, both for the individual and on a national scale. To stratify better which patients with DRA would gain the most from surgical repair, therefore maximizing private and public cost–benefit, it is recommended that the DRA classification should include an objective functional aspect.
The limitations of this study include that it is a ‘pre–post’ study without a comparator arm. As the subjects were their own controls over time, the study results are deemed significant even though a placebo effect cannot be excluded. The interaction of several questionnaires with overlapping information may have had an impact on the responses. On the other hand, the combination of the monitored functional tests, self-reported grading and questionnaires regarding urinary incontinence and QoL, captures a more complete understanding of the panorama of symptoms. The significant improvements are also persistent compared with the 1-year follow-up results, which underlines the strength of the results in this study.
Another limitation is the 72 per cent response rate for the functional tests. This can, to a large extent be explained by the COVID-19 pandemic, but the risk of an underlying bias should be considered. The studied population was homogeneous in age, location and family situation, which limits the generalizability of the results. On the other hand, the debilitating situation with symptomatic DRA affects mainly individuals like the studied population, that is women of childbearing age. Even though aesthetics are important for QoL, this study focused only on physical function. The purpose was to evaluate the effect of functional change without any considerations of possible impact of aesthetic improvement. The study showed a long-term increase in QoL which indicates that a functional improvement is crucial for an improved and maintained QoL38.
This study shows that surgical reconstruction of DRA is a safe and effective treatment in persistent, symptomatic DRA. Surgery provides long-term improved function and increase in quality of life. We suggest that women with DRA combined with abdominal core dysfunctions and insufficiently improved by core training should be considered for surgical reconstruction.
Funding
Grants were provided from Stockholm County Council and the Swedish Society of Medicine.
Disclosure. The authors declare no conflict of interest.
Supplementary material
Supplementary material is available at BJS Open online.
Supplementary Material
Acknowledgements
The authors acknowledge the participating physiotherapists who monitored the functional tests, Lisa Nordquist, Frida Blom and Ignacio Pacheto Vivanco, and naprapath, Anna Hansson.
Contributor Information
Anders Olsson, Department of Clinical Science and Education, Karolinska Institutet, Södersjukhuset, Stockholm, Sweden; Department of Surgery, Södersjukhuset, Stockholm, Sweden.
Olivia Kiwanuka, Department of Clinical Science and Education, Karolinska Institutet, Södersjukhuset, Stockholm, Sweden; Department of Surgery, Södersjukhuset, Stockholm, Sweden.
Sofia Wilhelmsson, Functional Area Occupational Therapy & Physiotherapy, Allied Health Professionals Function, Karolinska University Hospital, Stockholm, Sweden.
Gabriel Sandblom, Department of Clinical Science and Education, Karolinska Institutet, Södersjukhuset, Stockholm, Sweden; Department of Surgery, Södersjukhuset, Stockholm, Sweden.
Otto Stackelberg, Department of Clinical Science and Education, Karolinska Institutet, Södersjukhuset, Stockholm, Sweden; Department of Surgery, Södersjukhuset, Stockholm, Sweden; Unit of Cardiovascular and Nutritional Epidemiology, Institute of Environmental Medicine, Karolinska Institutet, Stockholm, Sweden.
References
- 1. Noble E. Exercises for the Childbearing Year (3rd edn). Houghton Mifflin: Boston, 1988. [Google Scholar]
- 2. Fernandes da Mota PG, Pascoal AG, Carita AI, Bø K. Prevalence and risk factors of diastasis recti abdominis from late pregnancy to 6 months postpartum, and relationship with lumbo-pelvic pain. Man Ther 2015;20:200–205. [DOI] [PubMed] [Google Scholar]
- 3. Spitznagle TM, Leong FC, Van Dillen LR. Prevalence of diastasis recti abdominis in a urogynecological patient population. Int Urogynecol J Pelvic Floor Dysfunct 2007;18:321–328. [DOI] [PubMed] [Google Scholar]
- 4. Turan V, Colluoglu C, Turkyilmaz E, Korucuoglu U. Prevalence of diastasis recti abdominis in the population of young multiparous adults in Turkey. Ginekol Pol 2011;82:817–821. [PubMed] [Google Scholar]
- 5. Brauman D. Diastasis recti: clinical anatomy. Plast Reconstr Surg 2008;122:1564–1569. [DOI] [PubMed] [Google Scholar]
- 6. Hills NF, Graham RB, McLean L. Comparison of trunk muscle function between women with and without diastasis recti abdominis at 1 year postpartum. Phys Ther 2018;98:891–901. [DOI] [PubMed] [Google Scholar]
- 7. Benjamin DR, Frawley HC, Shields N, van de Water ATM, Taylor NF. Relationship between diastasis of the rectus abdominis muscle (DRAM) and musculoskeletal dysfunctions, pain and quality of life: a systematic review. Physiotherapy 2019;105:24–34. [DOI] [PubMed] [Google Scholar]
- 8. Keshwani N, Mathur S, McLean L. Relationship between interrectus distance and symptom severity in women with diastasis recti abdominis in the early postpartum period. Phys Ther 2018;98:182–190. [DOI] [PubMed] [Google Scholar]
- 9. Parker MM, Dugan S. Diastasis rectus abdominis and lumbo-pelvic pain and dysfunction –are they related? J Womens Health Phys Therapy 2009;33:15–22.. [Google Scholar]
- 10. Doubkova L, Andel R, Palascakova-Springrova I, Kolar P, Kriz J, Kobesova A. Diastasis of rectus abdominis muscles in low back pain patients. J Back Musculoskelet Rehabil 2018;31:107–112. [DOI] [PubMed] [Google Scholar]
- 11. Liaw LJ, Hsu MJ, Liao CF, Liu MF, Hsu AT. The relationships between inter-recti distance measured by ultrasound imaging and abdominal muscle function in postpartum women: a 6-month follow-up study. J Orthop Sports Phys Ther 2011;41:435–443. [DOI] [PubMed] [Google Scholar]
- 12. Poulose BK, Adrales GL, Janis JE. Abdominal core health – a needed field in surgery. JAMA Surg 2020;155:185–186. [DOI] [PubMed] [Google Scholar]
- 13. Candido G, Lo T, Janssen PA. Risk factors for diastasis of the recti abdominis. J. Assoc. Chart. Physiother Women’s Health. 2005;97:49–54. [Google Scholar]
- 14. Blotta RM, Costa SDS, Trindade EN, Meurer L, Maciel-Trindade MR. Collagen I and III in women with diastasis recti. Clinics (Sao Paulo) 2018;73:e319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Emanuelsson P, Gunnarsson U, Strigård K, Stark B. Early complications, pain, and quality of life after reconstructive surgery for abdominal rectus muscle diastasis: a 3-month follow-up. J Plast Reconstr Aesthet Surg 2014;67:1082–1088. [DOI] [PubMed] [Google Scholar]
- 16. Emanuelsson P, Gunnarsson U, Dahlstrand U, Strigård K, Stark B. Operative correction of abdominal rectus diastasis (ARD) reduces pain and improves abdominal wall muscle strength: a randomized, prospective trial comparing retromuscular mesh repair to double-row, self-retaining sutures. Surgery 2016;160:1367–1375. [DOI] [PubMed] [Google Scholar]
- 17. Olsson A, Kiwanuka O, Wilhelmsson S, Sandblom G, Stackelberg O. Cohort study of the effect of surgical repair of symptomatic diastasis recti abdominis on abdominal trunk function and quality of life. BJS Open 2019;3:750–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Akram J, Matzen SH. Rectus abdominis diastasis. J Plast Surg Hand Surg 2014;48:163–169. [DOI] [PubMed] [Google Scholar]
- 19. Mommers EHH, Ponten JEH, Al Omar AK, de Vries Reilingh TS, Bouvy ND, Nienhuijs SW. The general surgeon's perspective of rectus diastasis. A systematic review of treatment options. Surg Endosc 2017;31:4934–4949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Michalska A, Rokita W, Wolder D, Pogorzelska J, Kaczmarczyk K. Diastasis recti abdominis – a review of treatment methods. Ginekol Pol 2018;89:97–101. [DOI] [PubMed] [Google Scholar]
- 21. Carlstedt A, Bringman S, Egberth M, Emanuelsson P, Olsson A, Petersson U et al. Management of diastasis of the rectus abdominis muscles: recommendations for Swedish national guidelines. Scand J Surg 2020;1457496920961000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Reinpold W, Köckerling F, Bittner R, Conze J, Fortelny R, Koch A et al. Classification of rectus diastasis – a proposal by the German Hernia Society (DHG) and the International Endohernia Society (IEHS). Front Surg 2019;6: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lee D, Hodges PW. Behavior of the linea aAlba during a curl-up task in diastasis rectus abdominis: an observational study. J Orthop Sports Phys Ther 2016;46:580–589. [DOI] [PubMed] [Google Scholar]
- 24. Thabet AA, Alshehri MA. Efficacy of deep core stability exercise program in postpartum women with diastasis recti abdominis: a randomised controlled trial. J Musculoskelet Neuronal Interact 2019;19:62–68. [PMC free article] [PubMed] [Google Scholar]
- 25. Benjamin DR, van de Water AT, Peiris CL. Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods: a systematic review. Physiotherapy 2014;100:1–8. [DOI] [PubMed] [Google Scholar]
- 26. Gallus KM, Golberg KF, Field R. Functional improvement following diastasis rectus abdominus repair in an active duty navy female. Mil Med 2016;181:e952–e954. [DOI] [PubMed] [Google Scholar]
- 27. Gluppe SL, Hilde G, Tennfjord MK, Engh ME, Bø K. Effect of a postpartum training program on the prevalence of diastasis recti abdominis in postpartum primiparous women: a randomized controlled trial. Phys Ther 2018;98:260–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rodrigues MA, Nahas FX, Reis RP, Ferreira LM. Does diastasis width influence the variation of the intra-abdominal pressure after correction of rectus diastasis? Aesthet Surg J 2015;35:583–588. [DOI] [PubMed] [Google Scholar]
- 29. Salén BA, Spangfort EV, Nygren AL, Nordemar R. The disability rating index: an instrument for the assessment of disability in clinical settings. J Clin Epidemiol 1994;47:1423–1435. [DOI] [PubMed] [Google Scholar]
- 30. Biering-Sørensen F. Physical measurements as risk indicators for low-back trouble over a one-year period. Spine (Phila Pa 1976) 1984;9:106–119. [DOI] [PubMed] [Google Scholar]
- 31. Laslett M, Aprill CN, McDonald B, Young SB. Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests. Man Ther 2005;10:207–218. [DOI] [PubMed] [Google Scholar]
- 32. Franzén K, Johansson JE, Karlsson J, Nilsson K. Validation of the Swedish version of the incontinence impact questionnaire and the urogenital distress inventory. Acta Obstet Gynecol Scand 2013;92:555–561. [DOI] [PubMed] [Google Scholar]
- 33. Sullivan M, Karlsson J, Ware JE. The Swedish SF-36 Health Survey – I. Evaluation of data quality, scaling assumptions, reliability and construct validity across general populations in Sweden. Soc Sci Med 1995;41:1349–1358. [DOI] [PubMed] [Google Scholar]
- 34. Sullivan M, Karlsson J. The Swedish SF-36 Health Survey III. Evaluation of criterion-based validity: results from normative population. J Clin Epidemiol 1998;51:1105–1113. [DOI] [PubMed] [Google Scholar]
- 35. Eriksson Crommert M, Petrov Fieril K, Gustavsson C. Women’s experiences of living with increased inter-recti distance after childbirth: an interview study. BMC Womens Health 2020;20: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lazar CC, Clerc I, Deneuve S, Auquit-Auckbur I, Milliez PY. Abdominoplasty after major weight loss: improvement of quality of life and psychological status. Obes Surg 2009;19:1170–1175. [DOI] [PubMed] [Google Scholar]
- 37. Poulose BK, Roll S, Murphy JW, Matthews BD, Todd Heniford B, Voeller G et al. Design and implementation of the Americas Hernia Society Quality Collaborative (AHSQC): improving value in hernia care. Hernia 2016;20:177–189. [DOI] [PubMed] [Google Scholar]
- 38. Chiarello C, Falzone L, McCaslin K, Patel M, Ulery K. Effects of an exercise program on diastasis recti abdominis in pregnant women. J Womens Health Physical Therapy 2005;29:11–16.. [Google Scholar]
- 39. Mesquita L, Machado A, Andrade A. Physiotherapy for reduction of diastasis of the recti abdominis muscles in the postpartum period. Rev Bras Ginecol Obstet 1999;21:267–272.. [Google Scholar]
- 40. Yalfani A, Bigdeli N, Gandomi F. Effect of isometric–isotonic exercises of core stability in women with postpartum diastasis recti and its secondary disorders (randomized controlled clinical trial). J Health Care 2020;22:123–137.. [Google Scholar]
- 41. Bursch SG. Interrater reliability of diastasis recti abdominis measurement. Phys Ther & Rehabil J 1987;67:1077–1079.. [DOI] [PubMed] [Google Scholar]
- 42. van de Water AT, Benjamin DR. Measurement methods to assess diastasis of the rectus abdominis muscle (DRAM): a systematic review of their measurement properties and meta-analytic reliability generalisation. Man Ther 2016;21:41–53. [DOI] [PubMed] [Google Scholar]
- 43. Dufour S, Bernard S, Murray-Davis B, Graham N. Establishing expert-based recommendations for the conservative management of pregnancy-related diastasis rectus abdominis: a Delphi consensus study. 2019;43:73–81. [Google Scholar]
- 44. Rosen CM, Ngaage LM, Rada EM, Slezak S, Kavic S, Rasko Y. Surgical management of diastasis recti: a systematic review of insurance coverage in the United States. Ann Plast Surg 2019;83:475–480. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.