Abstract
Aims
In March and April 2020, at the start of the COVID-19 pandemic, our previous survey of Italian pediatric diabetes centers showed that 75% of telemedicine use was voluntary. We hypothesized that the COVID-19 pandemic has acted as a picklock to overcome barriers to telemedicine regulation, use, and reimbursement.
Methods
Between March 22nd and April 12th, 2021, the same survey administered in 2020 was sent to all 68 Italian pediatric diabetes centers belonging to the Italian Society for Pediatric Endocrinology and Diabetes (ISPED) to collect data on the demographic variables of respondents; information about the center; the use, codification, and reimbursement of telemedicine; and used tools. Descriptive data were evaluated to establish how the COVID-19 pandemic has changed telemedicine practice.
Results
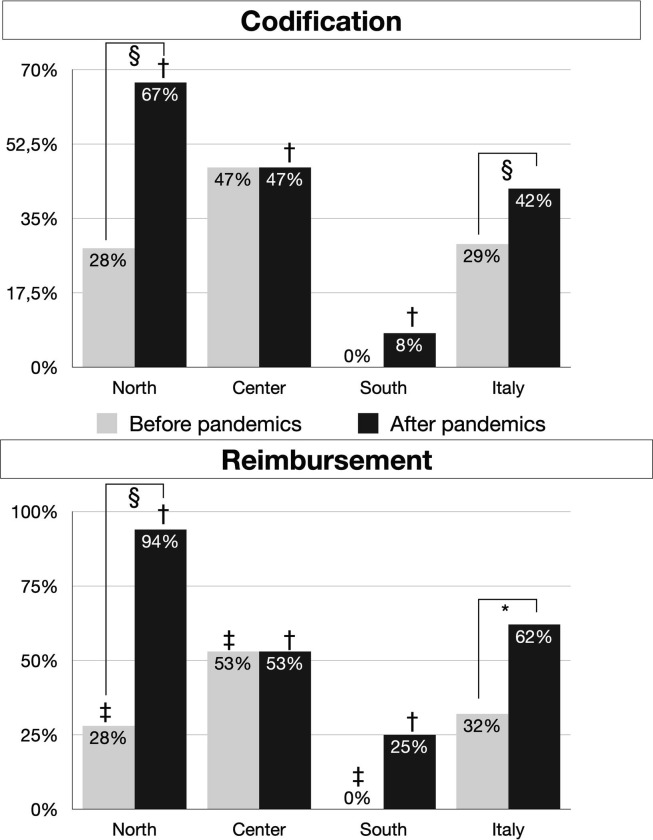
Eighty-two percent of responder centers reported an increase in the use of telemedicine, with televisits by video calling implemented in over half of centers. There was a significant increase in the number of centers formally tracking telemedicine use and obtaining reimbursement from the national health service (42% vs. 29% and 62% vs. 32%; p < 0.001, respectively). No reimbursement was provided to centers not using televisits.
Conclusions
From a voluntary procedure with a lack of traceability, telemedicine has become a new structured reality that may help our pediatric patients beyond this pandemic.
Keywords: Telemedicine, Continuous glucose monitoring, Insulin pump, Continuous subcutaneous insulin infusion, Pediatric diabetes
1. Introduction
The digitalization of healthcare has evolved over many years, from telemedicine and remote patient engagement to new digital approaches for diagnostics and information exchange. Already rising before the pandemic [1], [2], the COVID-19 outbreak in early 2020 accelerated the widespread adoption of virtual healthcare [3], [4], [5].
While the benefits of virtual healthcare are neither surprising nor new, the unique circumstances of the pandemic resulted in its rapid and widespread implementation. With more patients unable or unwilling to visit their primary care physicians and a need for social distancing requirements and strict infection prevention protocols, hospitals and healthcare centers relied more heavily on virtual healthcare approaches and technologies, confirming their vital role in modern healthcare.
Centers caring for pediatric type 1 diabetes were among those who already used digital technologies and rapidly expanded telemedicine services to facilitate patient care [6]. In the pre-COVID-19 era [7], it was clear that one of digital health’s main problems was its regulation and policy in individual countries, which have not been easy to distinguish. We highlighted these problems in our previous survey [8] and found that, in Italy, telemedicine was run in a largely voluntary manner, with a lack of legal traceability of services offered and no remuneration for the time consumed to deliver the services.
Healthcare related to diabetes is free of charge for individuals with diabetes in Italy; hospitals receive reimbursement for medical services by the National Health System, which covers their costs. Nonetheless, before the pandemic, only 30% of Italian pediatric diabetes centers received reimbursement for telemedicine interventions [8].
However, the COVID-19 pandemic has prompted changes in regulations, the pandemic acting as a picklock to overcome barriers to regulation by defining the ways in which digital services should be used. Also, in Italy, the lockdown regulations seem to have accelerated the official recognition of telemedicine, especially televisits in which a medical professional interacts at a distance in real-time with an already known patient through a video call.
Therefore, the present survey aimed to investigate, one year after our previous investigation [8], changes in: (a) the use of telemedicine services for children and adolescents with type 1 diabetes; (b) the traceability of telemedicine activities; and (c) formal reimbursement by the national health service for telemedicine activities.
2. Methods
Between March 22nd and April 12th, 2021, our previous survey [8] was again sent to all 68 Italian pediatric diabetes centers belonging to the Italian Society for Pediatric Endocrinology and Diabetes (ISPED) [9]. Data were collected on the demographic variables of respondents; information about the center, including staff composition; the use, codification, and reimbursement of telemedicine; and used tools.
According to insulin treatment and blood glucose monitoring, pediatric patients with type 1 diabetes were allocated into two groups: the “no-tech group”, for individuals using multiple daily injections and self-monitoring blood glucose, and the “tech group”, for those using insulin pumps and/or flash or continuous glucose monitoring.
Data are presented as frequencies and percentages or as medians and interquartile ranges (IQRs). Two-tailed Fisher’s exact test was performed to evaluate relationships between categorical variables, and the Wilcoxon signed-rank test was used to assess differences between paired data. A p-value < 0.05 was considered statistically significant. Statistical analyses were conducted using JMP software (v16.1.0, SAS Institute Inc., Cary, NC).
3. Results
Among the 68 ISPED centers, 49 (72%) completed the web-based survey and returned complete data, including the 41 centers that completed the previous survey [8]. The main characteristics of the centers are reported in Table 1 .
Table 1.
Survey center characteristics.
| Center characteristics | Percentage of centers | Number of centers |
|---|---|---|
| Region | ||
| Northern Italy | 41% | 20 |
| Central Italy | 35% | 17 |
| Southern Italy | 24% | 12 |
| Number of individuals with T1DM treated in the center | ||
| <100 individuals | 22% | 11 |
| 100–299 individuals | 45% | 22 |
| ≥300 individuals | 33% | 16 |
| Setting | ||
| Hospital | 59% | 29 |
| Academic | 41% | 20 |
| Median | IQR | |
| Staff | ||
| Pediatric diabetologist | 2 | (1–3) |
| Dedicated registered nurse | 1 | (1–2) |
| Dedicated dietician | 1 | (1–2) |
| Dedicated psychologist | 1 | (0–1) |
The different instruments used for telemedicine are summarized in Table 2 . The most frequently used tools to communicate with the diabetes team, both at the start and one year into the pandemic, were: generic download portals (e.g., Tidepool, Diasend™, Glooko™); instant messaging (e.g., WhatsApp, Telegram) on personal physicians’ mobile; e-mails to work accounts; and phone calls on physicians’ personal mobile, with no significant difference at the start and one year into the pandemic. Branded download portals (e.g., CareLink Personal™, Dexcom Clarity™) were also broadly used in the tech group. The use of generic data download portals significantly increased in the no-tech group, while instant messaging and e-mails to personal accounts significantly decreased in the tech group. Overall, less than 20% of the centers had a hospital-dedicated portal for telemedicine, while only 10% had a dedicated portal at the start of the pandemic.
Table 2.
Telemedicine tools used by the no-tech and tech groups.
|
No-Tech Group |
Tech Group |
|||
|---|---|---|---|---|
| Before | After | Before | After | |
| Generic data download portal | 69%§ | 80%§ | 88% | 80% |
| Instant messaging on personal phone | 65% | 69% | 76%§ | 60%§ |
| E-mail to work account | 60% | 62% | 59% | 62% |
| Call on personal phone | 50% | 49% | 63% | 51% |
| Call on hospital phone | 44% | 51% | 41% | 40% |
| SMS on personal phone | 27%§ | 18%§ | 27% | 24% |
| E-mail to personal account | 23% | 31% | 34%§ | 29%§ |
| Hospital-dedicated portal | 10% | 18% | 10% | 13% |
| SMS on hospital phone | 8% | 4% | 7% | 7% |
| Instant messaging on hospital phone | 2% | 7% | 5% | 4% |
| Branded data download portal | 90% | 89% | ||
| Televisits (by video call) | 51% | 56% | ||
|
22% | 20% | ||
|
36% | 42% | ||
| None of the previous | 0% | 0% | 3% | 2% |
| Number of used tools | 4 (3–5)@ | 4 (3–5)# | 5 (4–6)@ | 5 (4–7)# |
* p < 0.01 and § p < 0.05, Wilcoxon signed-rank test at the start and during the pandemic
@ p < 0.01 and # p < 0.05, Wilcoxon signed-rank test between the no-tech and tech groups
During the pandemic, video calls (“televisits”) using both dedicated or generic platforms (e.g., Skype, Zoom, Lifesize) were implemented in over half of centers, with no significant differences between no-tech and tech groups. Overall, 47% of centers registered the televisits, which were reimbursed with a specific code, albeit with significant differences between regions (72% northern, 40% central, 17% southern; p < 0.01).
Since the start of the pandemic, 82% of centers reported increased use of telemedicine, again with significant differences between regions (89% northern, 93% central, 58% southern; p = 0.04); between centers receiving reimbursement or not (93% vs. 64%; p = 0.02); and between those who performed televisits or not (95% vs. 71%; p = 0.03).
While at the start of the pandemic only 29% of centers could use reimbursement codes and 32% received a reimbursement for telemedicine interventions, one year later there was a significant increase in both code allowance and use (42% and 62%, respectively; p < 0.01), with significant differences between regions (Fig. 1 ). While no reimbursement was provided in centers not using televisits, 75% of centers that implemented televisits were paid for them (p < 0.01).
Fig. 1.
Percentage of centers with codification of and reimbursement for telemedicine activities at the start of and during the pandemic among regions and in the whole country. † p < 0.01 and ‡ <0.05, Fisher’s exact test between regions; * p < 0.01 and § p < 0.05, Wilcoxon signed-rank test before and during the pandemic.
4. Discussion
To our best knowledge, this is the first nationwide longitudinal survey investigating the impact of the COVID-19 pandemic on telemedicine use in pediatric diabetes centers. Eighty-two percent of responding Italian pediatric diabetes centers reported an increase in telemedicine usage and, one year after our first survey, there was a significant increase in the number of centers tracing telemedicine and obtaining reimbursement from the national health service (42% vs. 29%, and 62% vs. 32%; p < 0.001, respectively). The increased but variable use of telemedicine was significantly associated with the implementation of televisits and their reimbursement.
Even before the pandemic, the increased use of technology to manage type 1 diabetes offered the possibility to remotely access data for convenient downloaded by patients [1], [2], [10]. However, pre-COVID-19, in most countries including Italy, the use of telemedicine in pediatric diabetes centers was largely voluntary, lacking legal traceability and proper codification to reimburse each center by the health service [6].
Remote consultations have provided crucial support to patients with chronic conditions, reducing pressure on hospitals and minimizing the hazards of direct face-to-face exposure [11], [12]. People with diabetes and their caregivers were open to using telemedicine, with the most used communication channel being phone calls [13], [14], [15].
Considering new ways to deliver medical care provided a tremendous boost to telemedicine, both in terms of rapid expansion of its use and the discussion and actions required to formalize it, amend laws, and change regulations to enable telehealth solutions [16].
With the limitations of a survey design and lack of generalizability to other specialties and countries, this is the first nationwide study of telemedicine use in pediatric diabetes centers at the start of and after a year of pandemic conditions, thereby providing the opportunity to examine the evolution of telemedicine use [17]. Our findings are consistent with a cross-sectional survey of 21 US clinics in the T1D Exchange Quality Improvement Collaborative network, who reported an increase in telemedicine usage, with the majority of clinics (62%) performing both video and telephone visits and > 95% using generic or commercial data download portals to view device data; video visits and also phone calls were reimbursed in almost all centers [18].
After this rush to set up new telemedicine services, there now needs to be global reconsideration of: (a) what we can consider telemedicine; (b) reimbursement systems; and (c) the need for telemedicine after the pandemic.
The Italian National Guidelines on Telemedicine [19] state that “the use of information and communication technology tools for the treatment of health information or the online sharing of data and health information do not in themselves constitute telemedicine services: as an example, telemedicine does not include health information portals, social networks, forums, newsgroups, e-mail or other.” However, the most widely used tools were generic download portals (especially for patients not using any technological device), followed by instant messaging to personal mobiles, e-mails to work accounts, and phone calls to personal mobiles. Thus, most of the tools used in Italy (i.e., emails, text and instant messaging, phone calls) lack legal traceability and are not subject to any accreditation system that might provide guarantees for patients, healthcare providers, and the paying subject [20]. During the pandemic, over half of centers started “televisits” through video calls, which were the primary means to get the service recognized and reimbursed. This explains why centers that did not implement video calls (while using other tools) did not receive any reimbursement. An alternative to video calls to ensure confidentiality, direct codification, and subsequent reimbursement could be encrypted web-based applications (such as dedicated-hospital portals) [8]; however, to date, <20% of centers have had the chance to use this option in Italy. It is arguable whether data download from portals with suggestions given by e-mail, messaging, or phone calls [13], but not through a video call, constitute “telemedicine”. Nevertheless, the impact of such tools (e.g., instant messaging and phone calls to personal mobiles) on professional workloads needs to be addressed: healthcare professionals can experience telemedicine increasing their work burden and being overloaded, even outside working hours [21], [22].
Regarding reimbursement, we witnessed a considerable increase in centers remunerated for telemedicine over the last year. Unsurprisingly, the centers implementing reimbursement were also those in which telemedicine grew the most. On the other hand, only 75% of centers performing televisits received reimbursement, with a huge difference between regions, due to the variable quality of healthcare facilities across Italy. The healthcare system in Italy is region-based, and regional governments are responsible for ensuring the delivery of a benefits package to the population, including telemedicine [18]. Although the Italian guidelines on telemedicine that provie the regulatory framework were published in 2014 [15] and the new basic healthcare levels (what the National Health System reimburse) were approved in 2017 [19], the lack of reimbursement was one of the main reasons hindering the implementation of effective telemedicine solutions for long-term patient management in Italy prior to the pandemic [20]. When telemedicine is not reimbursed, hospitals incur a financial loss even though the healthcare providers are running that service; conversely, telehealth seems to reduce overall costs, mitigating against the need for additional expensive procedures by providing competent care more efficiently [11], [21]. Additionally, although telemedicine services are free of charge for individuals with diabetes in Italy, the issue of equity must be kept in mind [14], [15] since a stable internet connection and quality digital devices are necessary preconditions. During the COVID-19 pandemic in Italy, however, 46% of families received new digital devices from their child’s school and 25% of families were provided with a paid internet connection to enable remote learning [22], helping to reduce inequalities not just in education but also in telemedicine use.
Whether or not there is a public health emergency, regulatory health systems should recognize the potential of telehealth and remember that any care performed outside a clinic at home is always beneficial [2], [23], [24], [25], [26], [27]. We hope that the focus on telehealth over the last year continues after the pandemic and that its use can be considered a vital part of diabetes physician’s “virtual bag” [2]. From a voluntary procedure with a lack of traceability, telemedicine has now become a new structured reality that may help our pediatric patients even when the pandemic is over. The emergence of telehealth and virtual care as an alternative way to deliver care to patients with diabetes may be a silver lining to the cloud of all the devastating consequences of COVID-19.
Funding statement
No funding was used for the present study.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix.
* List of the contributing Authors of the Diabetes Study Group of the Italian Society for Pediatric Endocrinology and Diabetology (ISPED)
The following people were actively involved in the collection of data and must be considered authors of the paper: G. Bracciolini, C. Grosso (Alessandria); V. Cherubini (Ancona); A. Bobbio (Aosta); E. Schieven (Arzignano); M. Delvecchio, C. Zecchino (Bari); S. Zucchini (Bologna); P. Reinstadler (Bolzano); B. Felappi, E. Prandi (Brescia); F. Gallo (Brindisi); A.P. Frongia (Cagliari); R. Maccioni (Carbonia); F.A. Stamati (Castrovillari); D. Lo Presti, L. Tomaselli, T. Timpanaro (Catania); F. Citriniti (Catanzaro); V. Graziani, S.Monti, T. Suprani, (Cesena, Ravenna); F. De Berardinis (Cetraro); S. Tumini (Chieti); A. Scaramuzza (Cremona); V. De Donno (Cuneo); L. Lenzi, S.Toni (Florence); B. Mainetti (Forlì); M.S. Coccioli (Francavilla Fontana); N. Minuto, (Genoa); R. Maccioni, M.Scanu (Iglesias); P. Macellaro (Legnano); S. Sordelli (Mantova); F. Lombardo (Messina); R. Bonfanti, A. Rigamonti; V. Calcaterra, C. Mameli (Milan), L. Iughetti, B.Predieri (Modena); A. Franzese, E. Mozzillo, D. Iafusco, A. Zanfardino (Naples); I. Rabbone, S. Savastio (Novara); G. Piredda (Olbia); B. Iovane (Parma); C. Pistone (Pavia); M.G. Berioli (Perugia); E. Randazzo (Pisa); A. Lasagni (Reggio Emilia); I. Patera, M.C. Matteoli; R. Schiaffini, (Rome); I. Rutigliano (San Giovanni Rotondo); L. De Sanctis, D. Tinti, M. Trada (Turin); L. Guerraggio, S. Zonca (Tradate); V. Cauvin, R. Franceschi (Trento); G. Tornese, E. Faleschini (Trieste); A.A. Trattene (Varese); C. Maffeis, A. Sabbion (Verona); C. Arnaldi (Viterbo).
References
- 1.Döğer E., Bozbulut R., Soysal Acar A.Ş., Ercan Ş., Kılınç Uğurlu A., Akbaş E.D., et al. Effect of Telehealth System on Glycemic Control in Children and Adolescents with Type 1 Diabetes. J Clin Res Pediatr Endocrinol. 2019;11(1):70–75. doi: 10.4274/jcrpe.galenos.2018.2018.0017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Laptev D.N., Emelyanov A.O., Samoilova Y.G., Khramova E.B., Petriaikina E.E., Rybkina I.G., et al. Remote monitoring and treatment of children and adolescents with type 1 diabetes. Probl Endokrinol (Mosk) 2020;66(4):50–60. doi: 10.14341/probl12201. [DOI] [PubMed] [Google Scholar]
- 3.Keesara S., Jonas A., Schulman K. Covid-19 and health care's digital revolution. N Engl J Med. 2020;382 doi: 10.1056/NEJMp2005835. [DOI] [PubMed] [Google Scholar]
- 4.Bilic Curcic I., Cigrovski Berkovic M., Kizivat T., Canecki Varzic S., Smolic R., Smolic M. Effect of COVID-19 on management of type 1 diabetes: Pushing the boundaries of telemedical healthcare. World J Diabetes. 2021;12(6):780–785. doi: 10.4239/wjd.v12.i6.780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elbarbary N.S., Dos Santos T.J., de Beaufort C., et al. COVID-19 outbreak and pediatric diabetes: Perceptions of health care professionals worldwide. Pediatr Diabetes. 2020;21:1083–1092. doi: 10.1111/pedi.13084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tornese G., Ceconi V., Monasta L., Carletti C., Faleschini E., Barbi E. Glycemic control in type 1 diabetes mellitus during COVID-19 quarantine and the role of in-home physical activity. Diabetes Technol Ther. 2020;22(6):462–467. doi: 10.1089/dia.2020.0169. [DOI] [PubMed] [Google Scholar]
- 7.Flannery D., Jarrin R. Building a regulatory and payment framework flexible enough to withstand technological progress. Health Aff. 2018;37(12):2052–2059. doi: 10.1377/hlthaff.2018.05151. [DOI] [PubMed] [Google Scholar]
- 8.Tornese G., Schiaffini R., Mozzillo E., et al. Telemedicine in the time of the COVID-19 pandemic: results from the first survey among Italian pediatric diabetes centers. Healthcare (Basel). 2021;9:815. doi: 10.3390/healthcare9070815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Giorgetti C., Ferrito L., Zallocco F., et al. Organization and regional distribution of centers for the management of children and adolescents with diabetes in Italy. Ital J Pediatr. 2015;41:74. doi: 10.1186/s13052-015-0179-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fogel J.L., Raymond J.K. Implementing telehealth in pediatric type 1 diabetes mellitus. Pediatr Clin North Am. 2020;67(4):661–664. doi: 10.1016/j.pcl.2020.04.009. [DOI] [PubMed] [Google Scholar]
- 11.Richardson E., Aissat D., Williams G.A., et al. Keeping what works: remote consultations during the COVID-19 pandemic. Eurohealth. 2020;26(2) [Google Scholar]
- 12.Predieri B., Leo F., Candia F., et al. Glycemic Control Improvement in Italian Children and Adolescents With Type 1 Diabetes Followed Through Telemedicine During Lockdown Due to the COVID-19 Pandemic. Front Endocrinol. 2020;11 doi: 10.3389/fendo.2020.595735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tejera-Perez C., Moreno-Pérez Ó., Rios J., et al. People living with type 1 diabetes point of view in COVID-19 times (COVIDT1 study): Disease impact, health system pitfalls and lessons for the future. Diabetes Res Clin Pract. 2021;171 doi: 10.1016/j.diabres.2020.108547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krisiunas E., Sibomana L. Benefits of Technology in the Age of COVID-19 and Diabetes… Mobile Phones From a Rwanda Perspective. J Diabetes Sci Technol. 2020;14(4):748–749. doi: 10.1177/1932296820930032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Odeh R., Gharaibeh L., Daher A., et al. Caring for a child with type 1 diabetes during COVID-19 lockdown in a developing country: Challenges and parents' perspectives on the use of telemedicine. Diabetes Res Clin Pract. 2020;168 doi: 10.1016/j.diabres.2020.108393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bodulovic G, Wang S, de Morpurgo M, et al. Telehealth around the world: A global guide. DLA Piper - https://www.dlapiper.com/~/media/files/insights/publications/2020/12/dla-piper-global-telehealth-guide-december-2020.pdf (accessed August 19th 2021)
- 17.Tornese G., Scaramuzza A., Schiaffini R. Telemedicine in the time of the Coronavirus. Medico e bambino. 2020;39:142. [Google Scholar]
- 18.Lee JM, Carlson E, Albanese-O'Neill A, et al. (2021) Adoption of telemedicine for type 1 diabetes care during the COVID-19 pandemic. Diabetes Technol Ther. (Epub ahead of print) [DOI] [PMC free article] [PubMed]
- 19.Italian Ministry of Health. Telemedicine—National Guidelines. http://www.salute.gov.it/imgs/C_17_pubblicazioni_2129_allegato.pdf (accessed August 19th 2021).
- 20.Caffery L.J., Smith A.C. A literature review of email-based telemedicine. Stud Health Technol Inform. 2010;161:20–34. [PubMed] [Google Scholar]
- 21.MacNeill V., Sanders C., Fitzpatrick R., Hendy J., Barlow J., Knapp M., et al. Experiences of front-line health professionals in the delivery of telehealth: a qualitative study. Br J Gen Pract. 2014;64(624):e401–e407. doi: 10.3399/bjgp14X680485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Frielitz FS, Dördelmann J, Lemke S, et al. (2020) Assessing the benefits and challenges of video consultations for the treatment of children with type 1 diabetes - A qualitative study among diabetes professionals. Exp Clin Endocrinol Diabetes (Epub ahead of print) [DOI] [PubMed]
- 23.World Health Organization – Regional office for Europe. Italy. https://www.euro.who.int/en/countries/italy (accessed August 19th 2021)
- 24.Ferorelli D., Nardelli L., Spagnolo L., et al. Medical legal aspects of telemedicine in Italy: Application fields, professional liability and focus on care services during the COVID-19 health emergency. J Prim Care Community Health. 2020;11 doi: 10.1177/2150132720985055. 2150132720985055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Omboni S. Telemedicine During the COVID-19 in Italy: A Missed Opportunity? Telemed J E Health. 2020;26(8):973–975. doi: 10.1089/tmj.2020.0106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Snoswell C.L., Taylor M.L., Comans T.A., et al. Determining if Telehealth Can Reduce Health System Costs: Scoping Review. J Med Internet Res. 2020;22 doi: 10.2196/17298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mascheroni G, Saeed M, Valenza M, et al. (2021) Learning at a Distance: Children’s remote learning experiences in Italy during the COVID-19 pandemic. UNICEF Office of Research – Innocenti, Florence.