Abstract
Objectives
The WHO’s Global Action Plan on Antimicrobial Resistance (AMR) includes increasing overall public awareness of appropriate antibiotic use and resistance as a key priority area. We aimed to measure public knowledge, attitudes and practices of antibiotics and antibiotic resistance in Singapore, as well as their healthcare-seeking behaviours relating to respiratory illnesses, providing baseline data against which to measure the progress of future interventions.
Design
A cross-sectional study.
Setting
The general population in Singapore.
Participants
Between May and June 2019, we conducted a survey via an online panel in Singapore with 706 respondents.
Results
Our findings indicated common misconceptions surrounding antibiotic effectiveness and mechanisms of antibiotic resistance—most participants thought that resistance occurs when our bodies become resistant to antibiotics (62.5%) or when antibiotics become less powerful (48.5%). In multivariable analyses, better knowledge scores were associated with more favourable antibiotic attitudes (β=0.29; 95% CI 0.20 to 0.37). In addition, more favourable attitude scores were associated with lower odds of both expecting (OR: 0.84, 95% CI 0.72 to 0.99) and being prescribed antibiotics by a primary care doctor (OR: 0.76, 95% CI 0.63 to 0.90).
Conclusions
This study presents important information about population perceptions towards antibiotics and antibiotic resistance in Singapore. Results from this study emphasise the importance of effective public communication strategies to promote responsible antibiotic use locally and should be used to inform future implementation of programmes and activities as laid out in Singapore’s National Strategic Action Plan on AMR.
Keywords: public health, epidemiology, education & training (see medical education & training)
Strengths and limitations of this study.
This is the first population-level study on public knowledge, attitudes and practices of antibiotics and antibiotic resistance in Singapore. Findings from this study provide baseline information against which to measure the progress of future antibiotic interventions.
A key strength of our online survey is increased access to groups and individuals in the community who may not have been reached through other channels.
A potential limitation of our study is that respondents in online surveys may not be fully representative of the general population. In our study, we had an over-representation of respondents with at least a university education and those living in private accommodation. This may affect the generalisability of our results.
In an online survey where the research team is unable to clarify or answer questions in person, respondents may have misinterpreted questions especially relating to the mechanisms of antibiotic resistance.
Introduction
One of five key priority areas highlighted in the WHO’s Global Action Plan on Antimicrobial Resistance (AMR) is the improvement of overall public awareness of antibiotics and AMR to promote effective behavioural change population-level antibiotic use.1 Research on the drivers of antibiotic use in several countries highlights widespread misconceptions among the public regarding appropriate use of antibiotics and the development of antibiotic resistance, showing that less antibiotic knowledge is often associated with unfavourable antibiotic use behaviours, such as self-medication with antibiotics or sharing left-over antibiotics with others.2 These findings are supported by qualitative studies indicating that the general public is unfamiliar with technical terms such as ‘antimicrobial resistance’, that they feel they ‘know’ when they need antibiotics and that antibiotic prescription is often viewed as a form of validation for their illness.3–5
Singapore is a high-income city state in Asia with a comprehensive system of hybrid public and private primary, secondary and tertiary healthcare. Currently, all antimicrobials for human use in the country are prescription-only medicines and regulated by the Health Sciences Authority, the national authority that enforces health product regulation and registration.6 However, antibiotic resistance is an increasing concern in acute care hospitals7 8 and in the community,9 an indicator of inappropriate antibiotic consumption. Although antibiotics can be obtained only via prescription by licensed healthcare professionals6 in Singapore, patients seeking primary healthcare for upper respiratory tract infections are commonly misinformed about the role of antibiotics in the treatment of viral infections and often seek primary care expecting antibiotics from a medical professional.10
The development of the WHO’s Global Action Plan on AMR and subsequent national action plans11 serves to complement existing strategies and to prioritise future AMR interventions in both healthcare institutions and the community in preserving antimicrobial effectiveness. To measure the progress of future interventions, as well as to yield evidence-based insights12 into effective public communication strategies to promote responsible antibiotic use, we conducted an online population survey in Singapore to measure public perceptions of antibiotics and antibiotic resistance.
Methods
Study design + data collection
Survey respondents were participants in an online survey panel recruited and maintained by the Singapore Population Health Improvement Centre (SPHERiC) within the National University Health System. Members of the public are eligible to be part of the online survey panel if they are community-dwelling Singapore citizens or permanent residents, aged 21 and above, English literate, frequent users of web-based services and if they have a personal email account. Panel participants were recruited using two main strategies. The first strategy was a door-to-door approach conducted to recruit eligible community-dwelling Singaporeans and/or permanent residents. The second strategy involved mailing invitations to deidentified household addresses available from the Singapore Department of Statistics.
From 23 May to 1 June 2019, a total of 1001 SPHERiC panel members were invited to participate in the survey via an online link in an email or text message notification. The survey was available to panel members for 10 days and could be completed on any type of personal digital device (eg, laptops, mobile phones). A reminder notification was sent to panel members who did not respond to the first notification within 5 days. The self-completed survey was administered in English using REDCap software13 and took approximately 10–15 min to complete. Participants received a reimbursement of SGD5 (~US$3.70) for completing the survey. Survey data were provided by SPHERiC to the research team in an anonymised form for analysis.
Survey questionnaire
The questionnaire consisted of six sections, eliciting information from respondents about their sociodemographic characteristics (8 questions), knowledge about the effectiveness of antibiotics (5 questions), knowledge about the mechanisms of antibiotic resistance and the spread of antibiotic-resistant infections (12 questions), attitudes towards appropriate antibiotic use (9 questions), antibiotic practices in relation to the last time they had an acute respiratory illness (11 questions), as well as their healthcare-seeking behaviours (17 questions) (online supplemental appendix A).
bmjopen-2020-048157supp001.pdf (94.7KB, pdf)
The questionnaire was developed by reviewing available questionnaires from previously published surveys.14 15 Additionally, to enhance cross-country comparability, questions about antibiotic resistance were taken from the WHO country survey.16 To ensure that questions in the survey were well understood and adapted to the local context, the questionnaire was field tested with 29 individuals over a period of 6 days.
Data analysis
We assessed representativeness of the survey sample by comparing respondents’ sociodemographic characteristics with the Singapore Census of Population.17 We then assessed respondents’ general awareness towards antibiotics by tabulating variables related to antibiotic effectiveness, resistance and appropriate use. We also tabulated respondents’ practices in relation to antibiotic use for common respiratory illnesses.
We assigned each respondent a knowledge and attitude score based on the number of correct or favourable responses in the respective sections (online supplemental appendix B). All knowledge and attitude questions had three response options: ‘Agree’, ‘Disagree’ or ‘Not sure’. Correct knowledge and favourable attitude responses were assigned 1 point while incorrect or unfavourable responses scored 0 point.
bmjopen-2020-048157supp002.pdf (33.7KB, pdf)
Respondents’ antibiotic practice responses during their last consultation with a primary care provider for acute respiratory illness were dichotomised into: (1) whether respondents expected antibiotics from their doctor (yes=1; no=0), (2) whether they asked their doctor for antibiotics (yes=1; no=0), and (3) whether they were prescribed antibiotics by their doctor (yes=1; no=0).
We first investigated the respective relationships between respondents’ sociodemographic characteristics and their antibiotic knowledge and attitude scores using a multivariable linear (Gaussian) regression. Sociodemographic explanatory variables included age group, gender, housing type, household income, education, ethnicity and marital status.
In subsequent regression analyses, we investigated the association between antibiotic practices and antibiotic knowledge and attitude scores using a multivariable linear (Gaussian) regression, controlling for sociodemographic variables. We then conducted separate multivariable logistic regressions to investigate whether respondents’ attitude scores were associated with each of the three antibiotic practices as outcome variables: (1) whether respondents expected antibiotics, (2) whether they asked for antibiotics, and (3) whether they were prescribed antibiotics. We summarised associations using adjusted ORs and corresponding 95% CIs. Regression residual distributions can be found in online supplemental appendix C.
bmjopen-2020-048157supp003.pdf (185KB, pdf)
All data were analysed using R V.3.6.1.18 No patients were involved.
Patient and public involvement
No patients were involved in the study. To inform the survey content, we pilot tested the survey with members of the public external to our research. Key findings will be disseminated to study respondents in an online newsletter.
Results
Of 1001 eligible panel members, 706 (70.5%) completed the survey. Respondents had a median age of 44 years (range: 22–86 years). Four hundred (56.7%) respondents were female and 306 (43.3%) were male. Most respondents were married (60.8%) and had higher than secondary education (78.0%). The survey sample had a similar gender and ethnic group composition compared with the Singapore Census of Population17 but had slightly lower proportions of individuals who lived in private housing (ie, condominium, landed property) and a higher proportion of individuals with a university education (table 1).
Table 1.
Demographic and socioeconomic characteristics of survey participants compared with Singapore Census of Population (2010)
| Survey respondents n (%) |
Census (2010) (%) |
|
| Gender | ||
| Male | 306 (43.3) | 49.3 |
| Female | 400 (56.7) | 50.7 |
| Age | ||
| Median age | 44 | 37.4 |
| Ethnicity | ||
| Chinese | 549 (77.8) | 74.1 |
| Malay | 82 (11.6) | 13.4 |
| Indian | 51 (7.2) | 9.2 |
| Other | 24 (3.4) | 3.3 |
| Education | ||
| Below secondary | 13 (1.8) | 32.4 |
| Secondary | 138 (19.5) | 18.9 |
| Postsecondary | 243 (34.5) | 11.1 |
| Diploma and professional qualification | 14.8 | |
| University | 308 (43.6) | 11.7 |
| Prefer not to say | 4 (0.6) | – |
| Housing | ||
| 1 to 2-room HDB | 19 (2.7) | 2.1 |
| 3 to 4-room HDB | 393 (55.7) | 38.1 |
| 5-room HDB and executive flat | 247 (35.0) | 21.5 |
| Private housing | 36 (5.1) | 36.5 |
| Others | 11 (1.5) | 1.4 |
| Household income | ||
| <$2000 | 81 (11.5) | 21 |
| $2000–$3999 | 148 (21.0) | 16.5 |
| $4000–$5999 | 141 (20.0) | 15.3 |
| $6000–$9999 | 178 (25.2) | 21.7 |
| $10 000+ | 79 (11.2) | 25.5 |
| Do not know | 35 (5.0) | – |
| Prefer not to say | 44 (6.1) | – |
HDB, Housing and Development Board.
Descriptive analysis
Tabulations and frequencies of the descriptive analysis are shown in table 2.
Table 2.
Participants’ responses on antibiotic knowledge, attitudes and antibiotic resistance
| Antibiotic knowledge | Response | n=706 n (%) |
| Have you ever heard of a type of medication called ‘antibiotics’? | Yes | 688 (97.5) |
| No | 18 (2.5) | |
| n=688 n (%) | ||
| Antibiotics can help me recover from bacterial infections. | Agree | 574 (83.4) |
| Disagree | 43 (6.2) | |
| Not sure | 71 (10.3) | |
| Antibiotics can help me recover from viral infections. | Agree | 314 (45.6) |
| Disagree | 266 (38.7) | |
| Not sure | 108 (15.7) | |
| Antibiotics can help me recover from the common cold and influenza. | Agree | 228 (33.1) |
| Disagree | 364 (52.9) | |
| Not sure | 96 (14.0) | |
| Antibiotics can help me recover from serious symptoms of cold and influenza. | Agree | 319 (46.4) |
| Disagree | 256 (37.2) | |
| Not sure | 113 (16.4) | |
| Antibiotics can speed up my recovery from the common cold and influenza. | Agree | 250 (36.3) |
| Disagree | 315 (45.8) | |
| Not sure | 123 (17.9) | |
| Antibiotic attitudes | Response | n=688 n (%) |
| It is okay to share my antibiotics with family and friends when they are sick with the same symptoms. | Agree | 50 (7.3) |
| Disagree | 595 (86.5) | |
| Not sure | 43 (6.2) | |
| It is okay to share my antibiotics with family and friends when they are sick with different symptoms. | Agree | 9 (1.3) |
| Disagree | 652 (94.8) | |
| Not sure | 27 (9.3) | |
| It is okay to share my antibiotics with my pets when they are sick. | Agree | 7 (1.0) |
| Disagree | 661 (96.1) | |
| Not sure | 20 (2.9) | |
| It is okay to keep left-over antibiotics and use them again when I fall sick in the future. | Agree | 39 (5.7) |
| Disagree | 604 (87.8) | |
| Not sure | 45 (6.5) | |
| It is okay for me to use my left-over antibiotics when I have the same symptoms as before. | Agree | 59 (8.6) |
| Disagree | 590 (85.8) | |
| Not sure | 39 (5.7) | |
| It is important to always finish the course of antibiotics prescribed to me. | Agree | 642 (93.3) |
| Disagree | 28 (4.1) | |
| Not sure | 18 (2.6) | |
| It is okay not to finish the course of antibiotics prescribed to me when I feel better. | Agree | 56 (8.4) |
| Disagree | 592 (86.0) | |
| Not sure | 67 (9.7) | |
| It is okay not to finish the course of antibiotics prescribed to me when I have an alternative remedy. | Agree | 58 (8.4) |
| Disagree | 563 (81.8) | |
| Not sure | 67 (9.7) | |
| It is okay to miss a dose during the course of antibiotics prescribed to me. | Agree | 139 (20.2) |
| Disagree | 433 (62.9) | |
| Not sure | 116 (16.9) | |
| Antibiotic resistance knowledge | Response | n=706 n (%) |
| Have you ever heard of the abbreviation ‘AMR’? | Yes | 78 (11.0) |
| No | 628 (89.0) | |
| Have you ever heard of the term ‘antibiotic resistance’? | Yes | 427 (60.5) |
| No | 279 (39.5) | |
| n=427 n (%) | ||
| Antibiotic resistance occurs when antibiotics become less powerful so they don’t work as well. | Agree | 207 (48.5) |
| Disagree | 177 (41.4) | |
| Not sure | 43 (10.1) | |
| Antibiotic resistance occurs when your body becomes resistant to the antibiotics and they no longer work as well. | Agree | 266 (62.3) |
| Disagree | 127 (29.7) | |
| Not sure | 34 (8.0) | |
| Antibiotic resistance occurs when bacteria become resistant to the antibiotics so they are more difficult to kill. | Agree | 382 (89.5) |
| Disagree | 18 (4.2) | |
| Not sure | 27 (6.3) | |
| Antibiotic resistance only affects people with serious infections in hospitals. | Agree | 31 (7.3) |
| Disagree | 334 (78.2) | |
| Not sure | 62 (14.5) | |
| Antibiotic resistance affects common infections such as sore throats and urinary tract infections. | Agree | 188 (44.0) |
| Disagree | 100 (23.4) | |
| Not sure | 139 (32.6) | |
| If I use antibiotics appropriately, I don’t have to worry about getting antibiotic-resistant infections. | Agree | 190 (44.5) |
| Disagree | 141 (33.0) | |
| Not sure | 96 (22.5) | |
| How other people use antibiotics doesn’t affect my chance of getting antibiotic-resistant infections. | Agree | 157 (36.8) |
| Disagree | 183 (42.9) | |
| Not sure | 87 (20.4) | |
| How I use antibiotics doesn’t affect other peoples’ chances of getting antibiotic-resistant infections. | Agree | 169 (39.6) |
| Disagree | 176 (41.2) | |
| Not sure | 82 (19.2) |
AMR, antimicrobial resistance.
Awareness of antibiotic effectiveness
Almost all the respondents (97.5%) had heard of the term ‘antibiotics’ before. When asked if antibiotics were effective against bacterial and viral infections, only about a third of the respondents (35.6%) answered both questions correctly. A large proportion of respondents believed that antibiotics could help speed up recovery from the common respiratory illness (35.4%), or alleviate serious symptoms associated with these illnesses (45.2%).
Awareness of antibiotic resistance
Among respondents, 60.5% reported having heard of the term ‘antibiotic resistance’, but only 11% had heard of the abbreviation ‘AMR’. About half of the respondents were aware that resistance occurs when bacteria become resistant to the antibiotics. However, many respondents also thought that resistance occurs when our bodies become resistant to antibiotics (62.5%) or when antibiotics become less powerful (48.5%).
There was also lower awareness among respondents about how antibiotic-resistant infections could spread or affect common conditions. More than half (56.1%) either disagreed or were not sure that antibiotic resistance can affect the treatment of common infections such as sore throat and urinary tract infection. More than a third of respondents (39.7%) believed that their own use of antibiotics does not have any impact on other people’s chances of acquiring antibiotic-resistant infections, and that they do not have to worry about getting antibiotic-resistant infections as long as they use antibiotics appropriately themselves (44.5%). Overall, respondents agreed that interventions to reduce AMR include implementing better infection control measures in hospitals (76.2%) and using fewer antibiotics (71.9%), although a lower percentage recognised hand hygiene (61.7%) and vaccination (59.5%) as important interventions.
Awareness on how to use antibiotics responsibly
There was generally high awareness about appropriate practices in sharing antibiotics—respondents generally agreed that it is inappropriate to share antibiotics with family and friends when they are sick with either same (84.3%) or different (92.4%) symptoms. Respondents were also reluctant to share antibiotics with their household pets—only 1% thought it was appropriate to do so.
Less than 10% of the respondents said that they felt comfortable keeping left-over antibiotics for future use. While over 90% of the respondents agreed that it is important to always finish the course of antibiotics prescribed, a small proportion of respondents believed that they do not have to finish a prescribed course of antibiotics when they feel better (7.9%) or when they have an alternative remedy (8.2%).
Cold/influenza practices
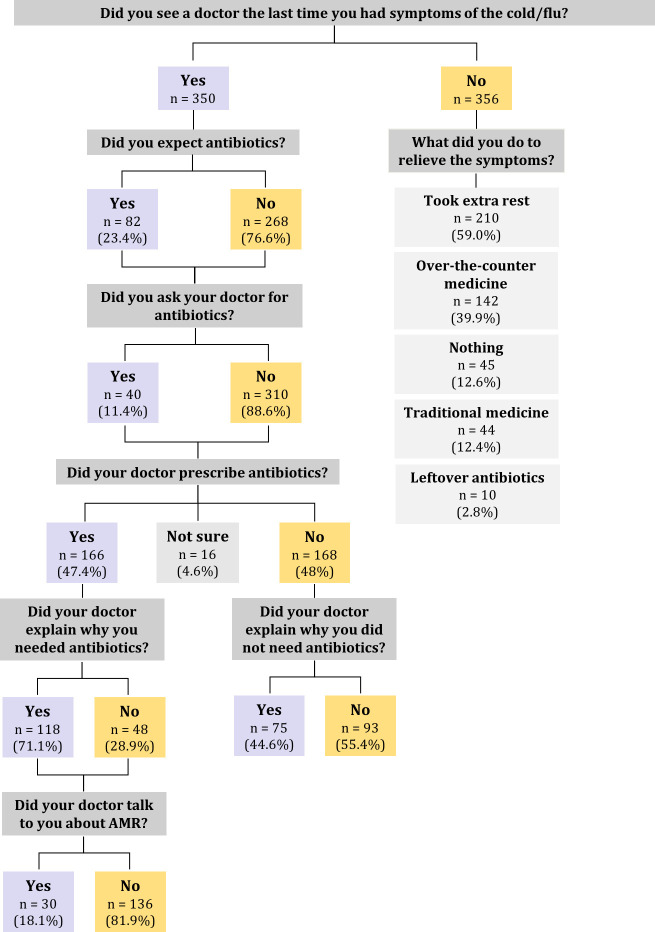
We asked all 706 respondents what they did the last time they had symptoms of the common cold or influenza (figure 1). More than half (50.6%) chose to see a doctor. The rest chose to take extra rest (59.0%), over-the-counter medication (39.9%), traditional Chinese medicine (12.4%) or did nothing about the symptoms (12.6%). Only 2.8% of respondents used left-over antibiotics (1.4%).
Figure 1.
Participants’ cold/influenza practices. AMR, antimicrobial resistance.
Of the 350 respondents who chose to see a doctor for their cold and influenza symptoms, 12.6% expected an antibiotic prescription and 11.4% explicitly asked their doctor for antibiotics. Despite this, nearly half (49.7%) of the respondents who visited the doctor for cold or influenza symptoms reported that their doctor prescribed them antibiotics, regardless of whether they asked for them explicitly or not.
For respondents who were prescribed antibiotics, 71.1% said that the doctor explained to them why they needed antibiotics, but only a minority stated that their doctor talked to them about possible side effects of antibiotics (28.3%) or about antibiotic resistance (18.1%). For respondents who were not prescribed antibiotics, 44.6% of them said that the doctor explained why they did not need them.
Multivariable analysis
Respondents’ knowledge and attitude scores
Respondents’ median knowledge score was 8 (range: 0–14) and median attitude score was 7 (range: 0–11).
Compared with female respondents, males scored better in terms of antibiotic knowledge (β: 0.68; 95% CI −0.15 to 1.22) but scored worse for attitudes (β: −0.40; 95% CI −0.77 to −0.03). Malays had lower knowledge (β: −0.69; 95% CI −1.81 to −0.43) and attitude scores (β: −1.04; 95% CI −1.76 to −0.33) relative to their Chinese counterparts. Respondents with secondary education also scored lower for both knowledge (β: −1.64; 95% CI −2.53 to −0.75) and attitudes (β: −1.16; 95% CI −1.71 to −0.60) compared with respondents with a university education. Respondents in three-room Housing and Development Board (HDB) (public housing) flat scored lower for both knowledge (β: −1.01; 95% CI −1.90 to −0.13) and attitudes (β: −0.83; 95% CI −1.42 to −0.24) compared with respondents in five-room HDB and executive flats (table 3).
Table 3.
Univariate analysis: participant characteristics associated with knowledge and attitude scores
| Knowledge score | Attitude score | |||
| Coefficient | 95% CI | Coefficient | 95% CI | |
| Estimate | 10.99 | 7.80 to 11.35 | 8.19 | 6.99 to 9.38 |
| Sex | ||||
| Female† | ||||
| Male | 0.68* | 0.15 to 1.22 | −0.40* | −0.77 to −0.03 |
| Ethnicity | ||||
| Chinese† | ||||
| Malay | −0.69 | −1.81 to −0.43 | −1.04** | −1.76 to −0.33 |
| Indian | 0.23 | −0.62 to 1.08 | −0.32 | −0.89 to 0.25 |
| Other | −0.13 | −1.61 to 1.35 | 0.25 | −0.73 to 1.22 |
| Age | −0.03* | −0.06 to −0.01 | 0.01 | −0.00 to 0.03 |
| Education | ||||
| University† | ||||
| Primary (Primary School Leaving Examination) | −0.47 | −4.48 to 3.53 | −1.10 | −3.06 to 0.86 |
| Secondary (‘O’/’N’ level) | −1.64*** | −2.53 to −0.75 | −1.16*** | −1.71 to −0.60 |
| ‘A’ level/polytechnic/diploma | 0.33 | −0.26 to 0.94 | −0.50* | −0.94 to −0.06 |
| Institute of Technical Education (ITE)/National Technical Certificate (NTC) | 0.06 | −1.92 to 2.04 | −0.13 | −1.17 to 0.91 |
| Housing | ||||
| 5–room HDB/executive flat† | ||||
| 1 to 2-room HDB‡ | 0.23 | −2.13 to 2.59 | −0.59 | −1.79 to 0.62 |
| 3–room HDB | −1.01* | −1.90 to −0.13 | −0.83** | −1.42 to −0.24 |
| 4–room HDB | −0.24 | −0.81 to 0.34 | −0.37 | −0.78 to 0.05 |
| Condominium | 0.22 | −1.13 to 1.56 | −0.56 | −1.56 to 0.44 |
| Landed house | −1.02 | −2.79 to 0.74 | 0.78 | −0.73 to 2.28 |
| Income | ||||
| <$2000† | ||||
| $2000–$3999 | −0.80 | −1.91 to 0.31 | −0.26 | −0.95 to 0.42 |
| $4000–$5999 | −0.49 | −1.63 to 0.65 | −0.24 | −0.95 to 0.48 |
| $6000–$10 000 | −0.21 | −1.35 to 0.94 | −0.12 | −0.84 to 0.60 |
| >$10 000 | 0.40 | −0.83 to 1.62 | −0.17 | −1.01 to 0.68 |
| Marital status | ||||
| Married† | ||||
| Divorced | −0.34 | −1.97 to 1.29 | 0.04 | −0.88 to 0.96 |
| Never married | 0.23 | −0.44 to 0.91 | −0.32 | −0.79 to 0.14 |
| Widowed | −0.71 | −3.50 to 2.19 | −0.34 | −1.95 to 1.29 |
| Separated but not divorced | 2.02 | −1.80 to 5.83 | 0.85 | −1.85 to 3.56 |
| Adjusted R2=0.12 | Adjusted R2=0.05 | |||
*P≤0.05; **p≤0.01; ***p≤0.001.
†Reference groups.
‡Public housing in Singapore managed by the Housing and Development Board (HDB).
Attitude scores increased by 0.29 (95% CI 0.20 to 0.37) for every unit increase in antibiotic knowledge score (table 4).
Table 4.
Multivariable regression analysis
| |
Multivariable linear regression | Multivariable logistic regression | ||||||
| Attitudes | Expected antibiotics | Asked for antibiotics | Prescribed antibiotics | |||||
| Coefficient | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Estimate | 7.49 | 5.80 to 9.18 | – | – | – | – | – | – |
| Knowledge score | 0.29*** | 0.20 to 0.37 | 0.90 | 0.77 to 1.04 | 0.96 | 0.79 to 1.16 | 0.90 | 0.79 to 1.05 |
| Attitude score | – | – | 0.84* | 0.72 to 0.99 | 0.78 | 0.71 to 1.07 | 0.76 | 0.63 to 0.90 |
All regression results are adjusted for sociodemographic variables (ie, gender, income, housing, education, ethnicity, marital status and age)
*p≤0.05; ***p≤0.001.
Respondents’ knowledge and attitude scores with practice variables
We found that more favourable antibiotic attitude scores were associated with lower odds of expecting antibiotics (OR: 0.84, 95% CI 0.72 to 0.99) per unit increase in score. Antibiotic knowledge and attitude scores were not associated with whether participants asked their doctors for antibiotics. However, higher scores on knowledge of antibiotic resistance (OR: 0.90, 95% CI 0.79 to 1.05) and attitude (OR: 0.76, 95% CI 0.63 to 0.90) were associated with lower odds of being prescribed antibiotics by the doctor (table 4).
Discussion
Our cross-sectional study of 706 participants in Singapore showed that there is a high level of awareness towards appropriate antibiotic use among the Singapore general population, but greater knowledge and awareness can be beneficial for curbing expectation and receipt of antibiotics during primary care consultations.
While most of the respondents said that they had heard of the term antibiotics before, only about a third of the respondents could correctly identify that antibiotics are effective towards bacterial and not viral infections. Comparable to previously published surveys in other countries,15 19 20 almost half of the respondents believed that antibiotics could be used for speeding up recovery or alleviating symptoms from conditions like the common cold and the influenza, indicating knowledge gaps in the appropriate use of antibiotics.
In terms of awareness of antibiotic resistance, only about a tenth of the respondents were able to correctly identify the mechanisms of resistance, suggesting a need for increased public education in this area. These misconceptions are also mirrored in other population-level antibiotic surveys21–23 as well as the WHO multicountry antibiotic resistance public awareness survey in 12 countries.16 Similar to our findings, a majority of respondents in all countries surveyed thought that antibiotic resistance occurs when our bodies become resistant to antibiotics, while approximately half of the respondents thought that antibiotic resistance is only a problem for people who take antibiotics regularly.
Approximately half of the respondents went to a medical doctor when they experienced symptoms of the cold or influenza, and a tenth of these respondents expressed that they explicitly asked for antibiotics. These results are congruent with a previously published study on Singaporean adult patients seeking medical care for upper respiratory tract infection symptoms, where a third of patients said that they would ask the doctor for antibiotics or see another doctor if antibiotics were not prescribed.10 While the studies looked at different target populations, this could indicate favourable population-level changes in antibiotic-seeking behaviours over time.
While only a small proportion of respondents who sought care for their symptoms of the cold or influenza said that they expected antibiotics, close to half of them left the clinic with antibiotics whether they asked for them or not. While respondents with higher attitude scores were less likely to expect antibiotics and to leave the clinic with an antibiotic prescription, this discrepancy between patient expectation and prescription is an indication of suboptimal antibiotic prescribing. As respondents’ antibiotic prescribing information was self-reported, we were unable to verify whether they actually received antibiotics, or if those who knew more about antibiotics were less likely to take any form of prescription. We also do not know from our study if there are significant differences in patient antibiotic-seeking behaviours or clinician-prescribing practices between public and private healthcare sectors. However, previous research in other countries indicates the effectiveness of potential strategies such as delayed prescription24 25 and shared decision-making26 27 to reduce inappropriate antibiotic use especially for acute respiratory infections. Additional strategies from other settings have also found that decreasing the frequency of medical consultations pertaining to respiratory illnesses was effective in reducing ambulatory antibiotic prescriptions.28 29
These findings highlight the importance of disseminating clear information about antibiotics and antibiotic resistance to reduce public expectations surrounding antibiotic prescriptions. It also emphasises the need to provide resources such as clinical practice guidelines on antibiotic use in acute upper respiratory infections,30 accessible diagnostic tools in upskilling primary care healthcare professionals as well as more comprehensive policies to manage profit making in antibiotic dispensation.31 32 Further, while public campaign messages have focused on antibiotic effectiveness towards specific medical conditions,12 28 33 34 our findings suggest that more should be done with regard to how people can use antibiotics more effectively and how health professionals can communicate that information. Future research should further explore where people usually get information about antibiotics and how this influences their antibiotic-seeking behaviours. Additionally, follow-up population surveys using consistent methods and question structures can provide valuable insights into progress of future AMR interventions.
A potential limitation of our study is that respondents in online surveys may not be fully representative of the general population. Although our survey sample was compared with the Singapore census population in terms of gender and ethnic group, there was a pronounced over-representation of respondents with at least a university education and those living in private accommodation. This may affect the generalisability of our results as these sociodemographic characteristics might be associated with greater awareness about health-related issues as well as knowledge relating to AMR,35–37 as indicated in prior survey findings in similar contexts. Further, although preserving question structure enabled us to maintain comparability with WHO’s multicountry antibiotic resistance public awareness survey, respondents may have misinterpreted questions relating to the mechanisms of antibiotic resistance, especially in an online survey where the research team is unable to clarify or answer questions in person.
Conclusion
This is the first study on public knowledge, attitudes and practices of antibiotics and antibiotic resistance in Singapore, providing baseline information against which to measure the progress of future interventions. Results from this study serve to emphasise the importance of raising awareness surrounding effective antibiotic use, as well as the mechanisms of antibiotic resistance. They also highlight the benefit of clinical practice guidelines on antibiotic prescribing, educational resources and clinical diagnostic tools for providers. These recommendations should be used to inform future implementation of programmes and activities as laid out in Singapore’s National Strategic Action Plan on AMR.
Supplementary Material
Acknowledgments
We thank the SPHS unit for their assistance in pretesting and data management for the questionnaire fielded to the online panel.
Footnotes
Contributors: JML, MCD and CCT conceived the research study and developed the questionnaire. JML and CCT analysed the data and drafted the manuscript. ARC and LYH provided critical feedback on the manuscript.
Funding: This work was funded by the Singapore Ministry of Health’s National Medical Research Council under the Centre Grant Programme–Singapore Population Health Improvement Centre (NMRC/CG/C026/2017_NUHS).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study was approved by the Institutional Review Board of the National University of Singapore (reference number: B-16-269).
References
- 1.Global action plan on antimicrobial resistance, 2015. Available: https://apps.who.int/iris/handle/10665/193736
- 2.Jamhour A, El-Kheir A, Salameh P, et al. Antibiotic knowledge and self-medication practices in a developing country: a cross-sectional study. Am J Infect Control 2017;45:384–8. 10.1016/j.ajic.2016.11.026 [DOI] [PubMed] [Google Scholar]
- 3.Gaarslev C, Yee M, Chan G, et al. A mixed methods study to understand patient expectations for antibiotics for an upper respiratory tract infection. Antimicrob Resist Infect Control 2016;5:39. 10.1186/s13756-016-0134-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davis ME, Liu T-L, Taylor YJ, et al. Exploring patient awareness and perceptions of the appropriate use of antibiotics: a mixed-methods study. Antibiotics 2017;6:23. 10.3390/antibiotics6040023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Torres NF, Solomon VP, Middleton LE. Patterns of self-medication with antibiotics in maputo city: a qualitative study. Antimicrob Resist Infect Control 2019;8:161. 10.1186/s13756-019-0618-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Health products (therapeutic products) regulations, 2016. Available: https://sso.agc.gov.sg/SL/HPA2007-S329-2016 [Accessed 15 Sep 2020].
- 7.Hsu L-Y, Tan T-Y, Jureen R, et al. Antimicrobial drug resistance in Singapore hospitals. Emerg Infect Dis 2007;13:1944–7. 10.3201/eid1312.070299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cai Y, Venkatachalam I, Tee NW, et al. Prevalence of healthcare-associated infections and antimicrobial use among adult inpatients in Singapore acute-care hospitals: results from the first national point prevalence survey. Clin Infect Dis 2017;64:S61–7. 10.1093/cid/cix103 [DOI] [PubMed] [Google Scholar]
- 9.Shankar N, Chow ALP, Oon J, et al. The epidemiology and transmission of methicillin-resistant staphylococcus aureus in the community in Singapore: study protocol for a longitudinal household study. BMC Infect Dis 2017;17:678. 10.1186/s12879-017-2793-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pan DST, Huang JH, Lee MHM, et al. Knowledge, attitudes and practices towards antibiotic use in upper respiratory tract infections among patients seeking primary health care in Singapore. BMC Fam Pract 2016;17:148. 10.1186/s12875-016-0547-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agri-Food & Veterinary Authority of Singapore, Ministry of Health, National Environment Agency, National Environment Agency National Water Agency . The National strategic action plan on antimicrobial resistance, Singapore, 2017. Available: http://extwprlegs1.fao.org/docs/pdf/sin171511.pdf [Accessed 6 September 2021].
- 12.Huttner B, Saam M, Moja L, et al. How to improve antibiotic awareness campaigns: findings of a WHO global survey. BMJ Glob Health 2019;4:e001239. 10.1136/bmjgh-2018-001239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform 2019;95:103208. 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.André M, Vernby A, Berg J, et al. A survey of public knowledge and awareness related to antibiotic use and resistance in Sweden. J Antimicrob Chemother 2010;65:1292–6. 10.1093/jac/dkq104 [DOI] [PubMed] [Google Scholar]
- 15.You JHS, Yau B, Choi KC, et al. Public knowledge, attitudes and behavior on antibiotic use: a telephone survey in Hong Kong. Infection 2008;36:153–7. 10.1007/s15010-007-7214-5 [DOI] [PubMed] [Google Scholar]
- 16.WHO . Antibiotic resistance: multi-country public awareness survey, 2015. Available: https://apps.who.int/iris/bitstream/handle/10665/194460/9789241509817_eng.pdf?sequence=1
- 17.Department of statistics singapore . Singapore census of population 2010: statistical release 1: demographic characteristics, education, language and religion. Singapore Government, 2011. [Google Scholar]
- 18.RStudio Team . RStudio: integrated development for R. Boston, MA: RStudio, Inc, 2015. http://www.rstudio.com/ [Google Scholar]
- 19.Chan GC, Tang SF. Parental knowledge, attitudes and antibiotic use for acute upper respiratory tract infection in children attending a primary healthcare clinic in Malaysia. Malaysian Family Physician 2012;2:5. [PubMed] [Google Scholar]
- 20.Chanvatik S, Kosiyaporn H, Lekagul A, et al. Knowledge and use of antibiotics in Thailand: a 2017 national household survey. PLoS One 2019;14:e0220990. 10.1371/journal.pone.0220990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lim JM, Chhoun P, Tuot S, et al. Public knowledge, attitudes and practices surrounding antibiotic use and resistance in Cambodia. JAC Antimicrob Resist 2021;3:dlaa115. 10.1093/jacamr/dlaa115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aslam A, Gajdács M, Zin CS, et al. Public awareness and practices towards self-medication with antibiotics among the Malaysian population. A development of questionnaire and pilot-testing. Antibiotics 2020;9:97. 10.3390/antibiotics9020097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tsuzuki S, Fujitsuka N, Horiuchi K, et al. Factors associated with sufficient knowledge of antibiotics and antimicrobial resistance in the Japanese general population. Sci Rep 2020;10:1–9. 10.1038/s41598-020-60444-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Little P, Moore M, Kelly J, et al. Delayed antibiotic prescribing strategies for respiratory tract infections in primary care: pragmatic, factorial, randomised controlled trial. BMJ 2014;348:g1606. 10.1136/bmj.g1606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spurling GK, Del Mar CB DL, Foxlee R, et al. Delayed antibiotic prescriptions for respiratory infections. Cochrane Database of Systematic Reviews 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coxeter P, Del Mar CB, McGregor L, et al. Interventions to facilitate shared decision making to address antibiotic use for acute respiratory infections in primary care. Cochrane Database Syst Rev 2015:CD010907. 10.1002/14651858.CD010907.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Légaré F, Labrecque M, Cauchon M, et al. Training family physicians in shared decision-making to reduce the overuse of antibiotics in acute respiratory infections: a cluster randomized trial. CMAJ 2012;184:E726–34. 10.1503/cmaj.120568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chahwakilian P, Huttner B, Schlemmer B, et al. Impact of the French campaign to reduce inappropriate ambulatory antibiotic use on the prescription and consultation rates for respiratory tract infections. J Antimicrob Chemother 2011;66:2872–9. 10.1093/jac/dkr387 [DOI] [PubMed] [Google Scholar]
- 29.Gulliford M, Latinovic R, Charlton J, et al. Selective decrease in consultations and antibiotic prescribing for acute respiratory tract infections in UK primary care up to 2006. J Public Health 2009;31:512–20. 10.1093/pubmed/fdp081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee T-H, Wong JG, Lye DC, et al. Medical and psychosocial factors associated with antibiotic prescribing in primary care: survey questionnaire and factor analysis. Br J Gen Pract 2017;67:e168–77. 10.3399/bjgp17X688885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Singh SR, Chua AQ, Tan ST, et al. Combating antimicrobial resistance in Singapore: a qualitative study exploring the policy context, challenges, facilitators, and proposed strategies. Antibiotics 2019;8:201. 10.3390/antibiotics8040201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chua AQ, Kwa AL-H, Tan TY, et al. Ten-Year narrative review on antimicrobial resistance in Singapore. Singapore Med J 2019;60:387–96. 10.11622/smedj.2019088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Al Omari S, Al Mir H, Wrayde S, et al. First Lebanese antibiotic awareness week campaign: knowledge, attitudes and practices towards antibiotics. J Hosp Infect 2019;101:475–9. 10.1016/j.jhin.2018.07.009 [DOI] [PubMed] [Google Scholar]
- 34.Saam M, Huttner B, Harbarth S, et al. Evaluation of antibiotic awareness campaigns. Geneva, Switzerland: WHO Collaborating Centre on Patient Safety, 2017. [Google Scholar]
- 35.Adekanmbi V, Jones H, Farewell D, et al. Antibiotic use and deprivation: an analysis of Welsh primary care antibiotic prescribing data by socioeconomic status. J Antimicrob Chemother 2020;75:2363–71. 10.1093/jac/dkaa168 [DOI] [PubMed] [Google Scholar]
- 36.Thomson K, Berry R, Robinson T, et al. An examination of trends in antibiotic prescribing in primary care and the association with area-level deprivation in England. BMC Public Health 2020;20:1–9. 10.1186/s12889-020-09227-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Covvey JR, Johnson BF, Elliott V, et al. An association between socioeconomic deprivation and primary care antibiotic prescribing in Scotland. J Antimicrob Chemother 2014;69:835–41. 10.1093/jac/dkt439 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-048157supp001.pdf (94.7KB, pdf)
bmjopen-2020-048157supp002.pdf (33.7KB, pdf)
bmjopen-2020-048157supp003.pdf (185KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.