Abstract
COVID-19 usually begins with respiratory symptoms but may also cause neurological disturbances by direct (viral invasion) or indirect (immune-mediated) mechanism. Common neurological injury described in the literature include infectious toxic encephalopathy, viral encephalitis and Guillain-Barré syndrome. We present two cases diagnosed with COVID-19 who presented with isolated neurological deficit along facial nerve and vestibular nerve. Both recovered with medical management and rehabilitative exercises. Isolated neurological impairment in otorhinolaryngological practice may be the primary presentation or delayed feature of COVID-19.
Keywords: COVID-19, otolaryngology / ENT, cranial nerves
Background
COVID-19 is a novel entity caused by SARS-CoV-2. The disease emerged in Wuhan and now has spread across continents and has been declared as a pandemic causing global concern.1 Weekly epidemiological update by WHO on 25 May 2021 reported 166 352 007 confirmed cases worldwide and 3 449 189 confirmed deaths. Risk of transmission increases on exposure to an infected person, being within 6 ft for at least 15 min, briefer if symptomatic.2 Viral transmission occurs in aerosols of 5 μm and droplets sized around 20 μm. This virus usually enters through nose or oropharynx and presents with respiratory symptoms but may also cause neurological disturbances.3 Neurotropism of this novel virus has been postulated to be due to its affinity towards ACE-2 receptors found in capillary endothelium of vasa nervorum, from where it gains entry into the neural tissue.4 Other pathways of invasion include direct invasion,5 travel through motor and sensory nerve endings,6 encouraging hypoxic damage in neural tissue due to generalised hypoxia in the body during infection7 and immune mediated injury as a response to viral infiltration.8 The most common neurological injury described is acute encephalopathy,9 others include Guillain-Barré syndrome9 and viral encephalitis.10 SARS-CoV-2 infection has also shown to reduce the immunity of a person,11 encouraging reactivation of dormant viruses. Reports on lower motor neuron facial palsy or vestibular neuritis are sparse. We present case reports of lower motor neuron facial palsy and vestibular neuritis in patients with COVID-19.
Both the subjects have given their written informed consent to publish their case, including their images.
Case presentation: acute vestibular neuronitis
A 77-year-old man previously on treatment for primary hypertension, type 2 diabetes mellitus was diagnosed with COVID-19 by real-time PCR test (7 weeks prior to presentation to us) and recovered from acute respiratory distress syndrome (ARDS) 1 month ago. He presented with spinning sensation associated with generalised weakness and two episodes of vomiting. He had no history of decrease in hearing or tinnitus. After confirming stable vitals, evaluation for dizziness was performed. Head impulse test was positive on the left, showing saccadic correction. Cover–uncover test for skew deviation showed no correction of gaze on uncovering. Head shake test was negative. No spontaneous nystagmus was seen, but there was gaze induced nystagmus on the right. The patient swayed to the left during sharpened Romberg test (figure 1). A detailed neurological examination was performed and was normal. He was alert, oriented to time, place and person with good recent and remote memory. His speech was spontaneous, fluent with normal repetition. Cerebellar function revealed normal response to rapid alternating movements, finger-nose test and no pronator drift. He swayed to left on attempting tandem gait. On cranial nerve examination, he had normal smell sensation, direct and consensual light reflex were intact, extraocular movements were normal and full, sensation over face was intact and so was facial nerve function. His palatal movement, voice and tongue movements were normal. He had normal tone, 5/5 power in both upper and lower limb with normal deep tendon reflexes. Sensation to fine touch, temperature, pressure, two-point discrimination and stereognosis was normal. Ophthalmological evaluation was normal.
Figure 1.
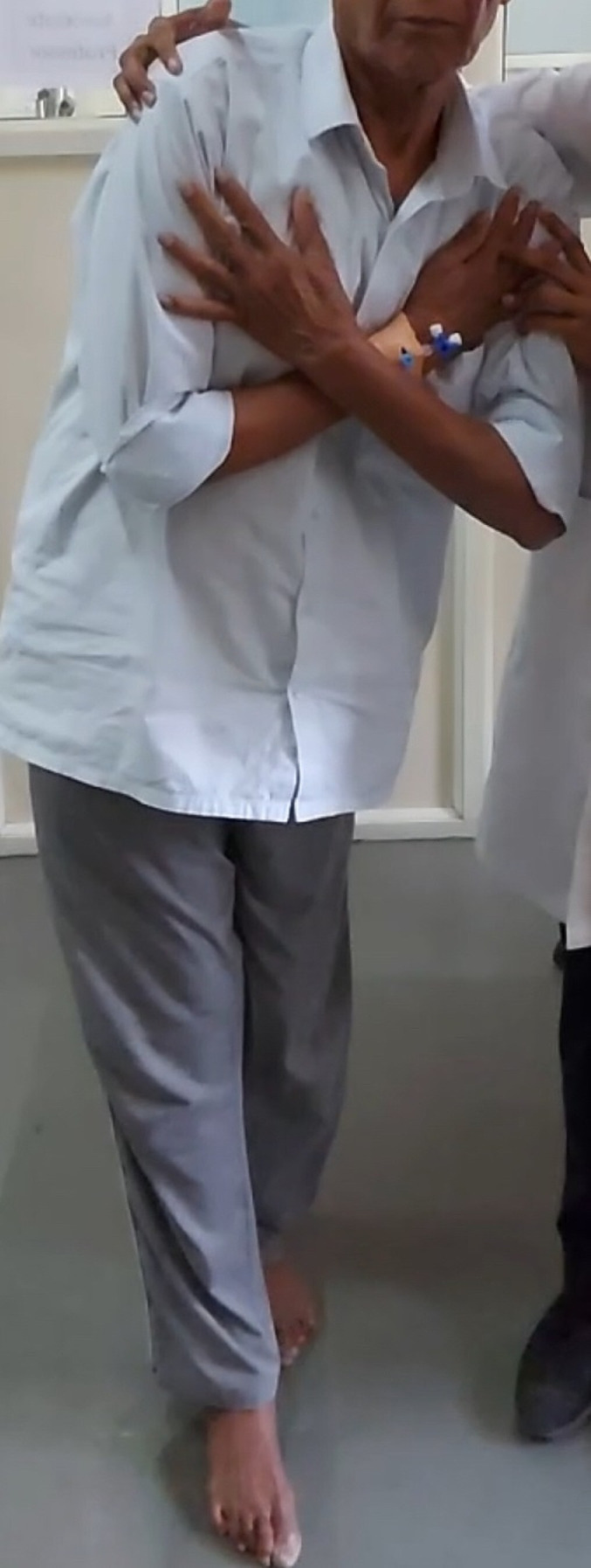
Figure shows the patient swaying to the left during sharpened Romberg’s testing.
Investigations
Pure tone audiogram showed bilaterally symmetrical moderate sensorineural hearing loss suggestive of presbycusis. The patient being hypertensive and as per institutional protocol, MRI with diffusion-weighted imaging of brain was performed and was normal.
Treatment
He was treated with prochlorperazine 5 mg three times a day and vestibular rehabilitative exercises from the second day.
Outcome and follow-up
Re-evaluation after 5 days and again after 10 days showed improvement in symptoms. Head impulse test returned to normal. No sway was noted on sharpened Romberg’s testing (figure 2).
Figure 2.
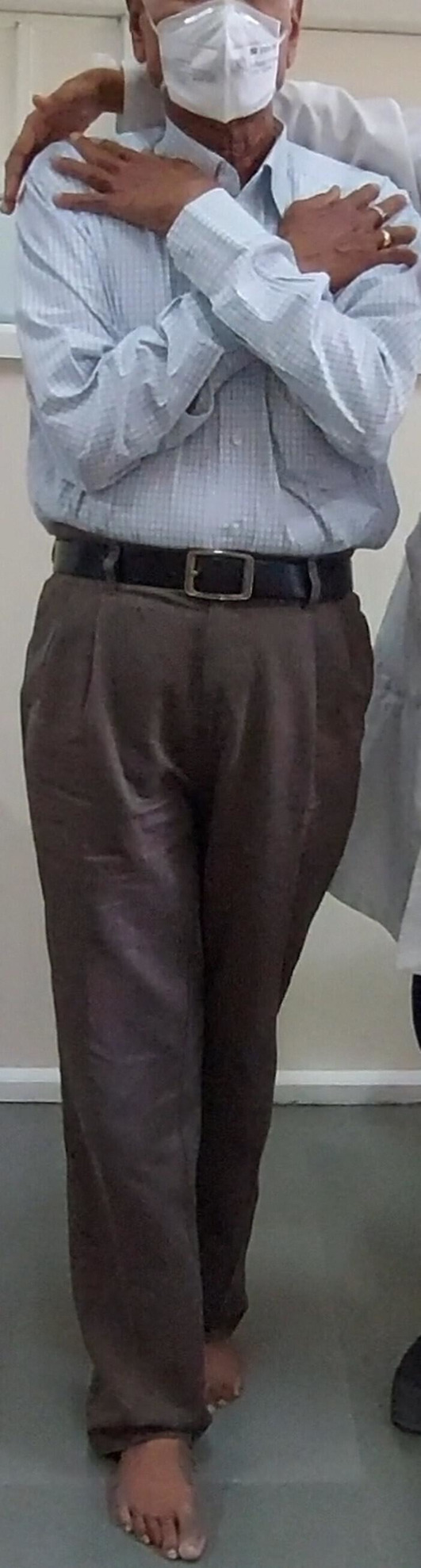
Figure shows the same patient being able to balance himself during sharpened Romberg’s testing.
Case presentation: lower motor neuron facial palsy
A 64-year-old man with medically controlled primary hypertension presented with slowly progressive facial weakness on the right side over a period of 7 days. On examination, there was loss of frontal crease on upward gaze, incomplete closure of eyelid on the right side and deviation of angle of mouth to left side (figure 3) and was classified as House-Brackmann grade-5 facial palsy. He also had a macular erythematous rash along zygomatic arch, maxillary and mandibular division of trigeminal nerve, suggestive of herpes zoster (figure 4). Rest of the ear, nose and throat examination was normal. No other neurological deficit was noted. Other cranial nerve examination was normal. He had no history of fever, upper or lower respiratory symptoms or any other symptom suggestive of COVID-19.
Figure 3.
Patient has loss of right nasolabial fold and deviation of angle of mouth to the left side.
Figure 4.

Image shows patient’s right side of face. Arrow marks point toward macular rash along zygomatic arch, maxillary and mandibular division of trigeminal nerve.
Investigations
High-resolution CT scan of temporal lobe and brain showed normal facial nerve course. He had no history of fever, upper or lower respiratory symptoms or any other symptom suggestive of COVID-19. His chest X-ray was normal. As a part of surveillance, he had undergone antibody testing for IgG SARS-CoV-2 1 week ago. Report was positive and it was presented to us after his admission to hospital.
Treatment
He was taught eye care and was started on acyclovir 800 mg five times a day along with tapering dose of steroid and 1500 μg of methyl cobalamin.
Outcome and follow-up
The rash improved with medications and he is now undergoing physiotherapy rehabilitation for facial weakness. Facial weakness improved to House-Brackmann grade 3 at the end of 1 month of therapy.
Discussion
Several places have been severely hit by COVID-19 pandemic in the past 6 months and they have now moved into post-COVID-19 era. Asymptomatic or symptomatic COVID-19 can cause immunosuppression,12 encouraging diseases or presentations unusual to before. We present two such cases in this report of neurological abnormalities due to two different pathophysiological process.
Our first case describes a patient who recently recovered from COVID-19-associated ARDS and presented with sudden-onset dizziness. On further evaluation, he was diagnosed to have vestibular neuritis. The presentation fulfilled all criteria to diagnose vestibular neuritis due to COVID-19.13 His nasopharyngeal swab was positive for SARS-CoV-2 PCR testing, vertigo began within 4 weeks of treatment for COVID-19, head impulse test showed saccadic correction on the left side and MRI brain was normal, ruling out retrocochlear pathologies. This case adds to the few cases reported on dizziness due to COVID-19 in the literature. First reports on neurological abnormalities seen in COVID-19 comes from Wuhan, China where the index case was reported.3 Kong et al described a 53-year-old woman who presented with persistent dizziness and was diagnosed to have COVID-19 on further evaluation.14 Malayala and Raza from USA reported a similar case, a 29-year-old woman who presented with dizziness and was later diagnosed to have COVID-19 illness.15 Both these patients had characteristic changes on CT imaging of the chest. This was similar to our case who also suffered from severe form of COVID-19. Steroid was part of the treatment plan for the case reported by Malayala and Raza.15 We did not initiate steroids as our patient was 77 years old, had recently recovered from COVID-19 and had improved with prochlorperazine and vestibular rehabilitation exercises in 10 days.
Second case of our report describes a 64-year-old man with sudden-onset lower motor neuron facial palsy and macular rash along zygomatic arch and mandible with no inciting event other than a positive COVID-19 report. Figueiredo et al reported a similar case, a case of pregnant woman presenting with facial palsy and was found positive for SARS-CoV-2 PCR testing.16 Similar to our case, she never had fever, cough, chest tightness, disturbance in smell sensation or any other respiratory symptom. Acyclovir and tapering prednisolone was the treatment of choice in both cases along with physiotherapy. It is unclear if the rash was due to reactivation of herpes infection or was a cutaneous manifestation of SARS-CoV-2 infection itself. The rash lacked the characteristic vesicles seen in herpes zoster, but it maintained dermatomal distribution, a characteristic of herpes infection. Herpes reactivation in COVID-19 has been reported in the literature.17 Ferreira et al described an immunocompetent 39 years old presenting with herpetic rash along all three divisions of trigeminal nerve, a scenario similar to ours. Herpetic reactivation in other parts of the body (over loin and over nape of neck) has also been reported in patients with COVID-19.18 Involvement of three or more dermatomes is known as disseminated zoster, as seen in our case and also the case reported by Ferreira et al. This is particularly seen in immunocompromised individuals. This points further to the immunocompromised state COVID-19 infection can produce. Though no definitive evidence can be provided on causal relationship, ongoing pandemic and lack of any other inciting factors, make SARS-CoV-19 infection the likely cause of Bell’s palsy.
Lower motor neuron facial palsy may be due to direct (viral) or indirect (immune-mediated) effects of SARS-CoV-2 virus.19 Direct neuroinvasion may occur by the virus entering the cell using ACE-2 receptors.20 On the other hand, in indirect mechanism, SARS-CoV-2 infection triggers the immune system, stimulating production of a plethora of antibodies. Some of which may have autoimmune properties towards neural proteins, causing parainfectious or postinfectious immune-mediated nerve injury.19 21 Literature on the occurrence of acute demyelinating neuropathy, such as Guillain-Barré syndrome following COVID-19, may be an example for the same.22–24 Morbilliform rash has been described in the literature as one of the cutaneous manifestation of COVID-19 illness.25 The lesion was typically seen over trunk and limbs, different from the location seen in the case reported.
Reviewing the literature for otoneurological complications of COVID-19 revealed that varying degrees of facial nerve paresis, sensorineural hearing loss, tinnitus and vestibular dysfuction has been reported. Facial nerve palsy was common during the acute phase of COVID-19 infection, that is, from the time of symptom onset to 3 weeks into the illness.16 26–29 Sensorineural hearing loss, on the other hand, was more common during postacute phase of COVID-19, that is, most presented with hard of hearing, or tinnitus after being 3 weeks into the illness.30–32 Decreased auditory function has also been documented in patients who have had asymptomatic COVID-19 disease.33 34 This further adds on to the deleterious effect COVID-19 has on vestibulocochlear nerve.
These two reports highlight the possible otoneurological presentations of COVID-19. Otoneurological impairments (such as idiopathic sudden sensorineural hearing loss,30 lower motor neuron facial nerve palsy or acute vestibular neuronitis) could be the primary presentation or a delayed feature of COVID-19 in an ear, nose and throat outpatient department. In them, it is advisable to perform tests to confirm SARS-CoV-2 infection. It is also important to note the pattern of these illnesses as and when the disease in encountered worldwide. Reporting these cases helps formulate a management plan appropriate for this disease and hence improve patient outcomes. There is great paucity of information on long-term complication of COVID-19, as most parts of the world are yet reaching the peak of pandemic. More reports on post-COVID-19 complications are needed, to help build up early management plans for these patients.
Learning points.
Diagnosis of lower motor neuron facial palsy, or acute vestibular neuronitis, may be the primary presentation or delayed feature of COVID-19.
Review of literature shows lower motor neuron facial palsy to be more common during acute COVID-19 disease and vestibulocochlear nerve dysfunction to be more common during the postacute phase.
Early diagnosis, management and addition of these cases to the medical literature will help in formulating treatment guidelines at the earliest.
Footnotes
Contributors: TK: data collection and writing. KJS and AMY: editing.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Thompson R. Pandemic potential of 2019-nCoV. Lancet Infect Dis 2020;20:280. 10.1016/S1473-3099(20)30068-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wiersinga WJ, Rhodes A, Cheng AC, et al. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA 2020;324:782–93. 10.1001/jama.2020.12839 [DOI] [PubMed] [Google Scholar]
- 3.Mao L, Wang M, Chen S, et al. Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: a retrospective case series study. medRxiv 2020. 10.2139/ssrn.3544840 [DOI] [Google Scholar]
- 4.Baig AM, Khaleeq A, Ali U, et al. Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host-virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci 2020;11:995–8. 10.1021/acschemneuro.0c00122 [DOI] [PubMed] [Google Scholar]
- 5.Koyuncu OO, Hogue IB, Enquist LW. Virus infections in the nervous system. Cell Host Microbe 2013;13:379–93. 10.1016/j.chom.2013.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Swanson PA, McGavern DB. Viral diseases of the central nervous system. Curr Opin Virol 2015;11:44–54. 10.1016/j.coviro.2014.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu Y, Xu X, Chen Z, et al. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun 2020;87:18–22. 10.1016/j.bbi.2020.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bohmwald K, Gálvez NMS, Ríos M, et al. Neurologic alterations due to respiratory virus infections. Front Cell Neurosci 2018;12:386. 10.3389/fncel.2018.00386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xiang P, XM X, Gao LL. First case of 2019 novel coronavirus disease with encephalitis. ChinaXiv 2020. [Google Scholar]
- 10.Paybast S, Gorji R, Mavandadi S. Guillain-Barré syndrome as a neurological complication of novel COVID-19 infection: a case report and review of the literature. Neurologist 2020;25:101–3. 10.1097/NRL.0000000000000291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cao X. COVID-19: immunopathology and its implications for therapy. Nat Rev Immunol 2020;20:269–70. 10.1038/s41577-020-0308-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zheng M, Gao Y, Wang G, et al. Functional exhaustion of antiviral lymphocytes in COVID-19 patients. Cell Mol Immunol 2020;17:533–5. 10.1038/s41423-020-0402-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Satar B. Criteria for establishing an association between Covid-19 and hearing loss. Am J Otolaryngol 2020;41:102658. 10.1016/j.amjoto.2020.102658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kong Z, Wang J, Li T, et al. 2019 novel coronavirus pneumonia with onset of dizziness: a case report. Ann Transl Med 2020;8:506. 10.21037/atm.2020.03.89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Malayala SV, Raza A. A case of COVID-19-Induced vestibular neuritis. Cureus 2020;12:e8918. 10.7759/cureus.8918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Figueiredo R, Falcão V, Pinto MJ, et al. Peripheral facial paralysis as presenting symptom of COVID-19 in a pregnant woman. BMJ Case Rep 2020;13:e237146. 10.1136/bcr-2020-237146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferreira ACAdeF, Romão TT, Macedo YS, et al. COVID-19 and herpes zoster co-infection presenting with trigeminal neuropathy. Eur J Neurol 2020;27:1748-1750. 10.1111/ene.14361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elsaie ML, Youssef EA, Nada HA. Herpes zoster might be an indicator for latent COVID 19 infection. Dermatol Ther 2020;33:e13666. 10.1111/dth.13666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Todisco M, Alfonsi E, Arceri S, et al. Isolated bulbar palsy after SARS-CoV-2 infection. Lancet Neurol 2021;20:169–70. 10.1016/S1474-4422(21)00025-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Doblan A, Kaplama ME, Ak S, et al. Cranial nerve involvement in COVID-19. Am J Otolaryngol 2021;42:102999. 10.1016/j.amjoto.2021.102999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sedaghat Z, Karimi N. Guillain Barre syndrome associated with COVID-19 infection: a case report. J Clin Neurosci 2020;76:233–5. 10.1016/j.jocn.2020.04.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alberti P, Beretta S, Piatti M, et al. Guillain-Barré syndrome related to COVID-19 infection. Neurol Neuroimmunol Neuroinflamm 2020;7:e741. 10.1212/NXI.0000000000000741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhao H, Shen D, Zhou H, et al. Guillain-Barré syndrome associated with SARS-CoV-2 infection: causality or coincidence? Lancet Neurol 2020;19:383–4. 10.1016/S1474-4422(20)30109-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ottaviani D, Boso F, Tranquillini E, et al. Early Guillain-Barré syndrome in coronavirus disease 2019 (COVID-19): a case report from an Italian COVID-hospital. Neurol Sci 2020;41:1351–4. 10.1007/s10072-020-04449-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gisondi P, PIaserico S, Bordin C, et al. Cutaneous manifestations of SARS-CoV-2 infection: a clinical update. J Eur Acad Dermatol Venereol 2020;34:2499–504. 10.1111/jdv.16774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Homma Y, Watanabe M, Inoue K, et al. Coronavirus Disease-19 pneumonia with facial nerve palsy and olfactory disturbance. Intern Med 2020;59:1773–5. 10.2169/internalmedicine.5014-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Decio A, Mazza A, Quadri V, et al. Neurological manifestations of COVID-19 in children: a case of facial nerve palsy. Pediatr Neurol 2021;116:59. 10.1016/j.pediatrneurol.2020.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cabrera Muras A, Carmona-Abellán MM, Collía Fernández A, et al. Bilateral facial nerve palsy associated with COVID-19 and Epstein-Barr virus co-infection. Eur J Neurol 2021;28:358–60. 10.1111/ene.14561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ribeiro BNdeF, Marchiori E. Facial palsy as a neurological complication of SARS-CoV-2. Arq Neuropsiquiatr 2020;78:667. 10.1590/0004-282x20200127 [DOI] [PubMed] [Google Scholar]
- 30.Koumpa FS, Forde CT, Manjaly JG. Sudden irreversible hearing loss post COVID-19. BMJ Case Rep 2020;13:e238419. 10.1136/bcr-2020-238419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Munro KJ, Uus K, Almufarrij I, et al. Persistent self-reported changes in hearing and tinnitus in post-hospitalisation COVID-19 cases. Int J Audiol 2020;59:889–90. 10.1080/14992027.2020.1798519 [DOI] [PubMed] [Google Scholar]
- 32.Lamounier P, Franco Gonçalves V, Ramos HVL, et al. A 67-year-old woman with sudden hearing loss associated with SARS-CoV-2 infection. Am J Case Rep 2020;21:e927519. 10.12659/AJCR.927519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mustafa MWM. Audiological profile of asymptomatic Covid-19 PCR-positive cases. Am J Otolaryngol 2020;41:102483. 10.1016/j.amjoto.2020.102483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kilic O, Kalcioglu MT, Cag Y, et al. Could sudden sensorineural hearing loss be the sole manifestation of COVID-19? an investigation into SARS-COV-2 in the etiology of sudden sensorineural hearing loss. Int J Infect Dis 2020;97:208–11. 10.1016/j.ijid.2020.06.023 [DOI] [PMC free article] [PubMed] [Google Scholar]



