Abstract
Objective:
To evaluate the longitudinal associations between self-reported physical activity and anxiety and depression symptom severity in adults with long-term physical disabilities.
Methods:
A secondary analysis of data from a USA based longitudinal survey study of community-dwelling adults with one of four potential long-term physical disabilities (multiple sclerosis, muscular dystrophy, spinal cord injury, postpoliomyelitis syndrome). The first time point (T1) for the current study was completed by 1594 participants. The second survey (T2) was sent one year later and third (T3) was sent three years later; each were completed by 1380 and 1218 participants respectively. At each time point, participants completed a measure of physical activity (Godin Leisure Time Exercise Questionnaire) and Patient-Reported Outcomes Measurement System short-forms evaluating depression and anxiety severity.
Results:
Mixed growth curve models showed greater quantities of physical activity were associated with decreases in both depression (χ2 [2] = 84.01, p < .001) and anxiety (χ2 [2] = 21.66, p < .001) symptom severity over the three-year period. However, while greater quantities of moderate (anxiety z = −2.24, p < .05; depression z = −5.48, p < .001) and strenuous (anxiety z = −2.59, p < .05; depression z = −3.90, p < .001) physical activity were significantly associated with decreases in negative affect, mild physical activity was not.
Conclusions:
The current study provides evidence that physical activity is longitudinally associated with anxious and depressive symptoms in adults with long-term physical disabilities. Future research should examine the quantities and intensities of physical activity necessary to impart psychological benefits.
Keywords: Physical activity, Depression, Anxiety, Longitudinal Studies, Disabled Persons
Introduction
Affective disorders and symptoms, particularly depression and anxiety, are highly prevalent in individuals with long-term physical disabilities, and considerably more common in this population when compared to both the general population as well as a number of other clinical populations (Battalio, Glette, Alschuler, & Jensen, 2018; Korostil & Feinstein, 2007; Lim et al, 2017; Marrie et al., 2015; Pangalila et al., 2015; Sareen, Cox, Clara, & Asmundson, 2005; Williams & Murray, 2015). In individuals with long-term physical disabilities, depressive and anxious symptoms have been shown to be directly associated with both the severity of the primary physical disability (Brenes et al., 2005; Garfield & Lincoln, 2012; Lester, Stepleman, & Hughes, 2007) and the presence and severity of other secondary health conditions and functional impairments (Battalio et al., 2018; Battalio, Jensen, & Molton, 2019). For example, research has found significant associations between anxious and depressive symptoms and pain, fatigue, physical functioning, self-reported and objective cognitive function, and social functioning (Asmundson & Katz, 2009; Battalio et al., 2018; Korostil & Feinstein, 2007; Lester, Stepleman, & Hughes, 2007; Wood et al., 2013).
Inhibited physical activity is one factor that is thought to contribute to this heightened prevalence and impact of anxiety and depression among individuals with long-term physical disabilities. Physical activity has been directly and indirectly linked with psychological function through various behavioral, psychological, and neurological mechanisms (Aurélio Monteiro Peluso, Silveira Guerra de Andrade, 2005; Awick, Phillips, Lloyd, & McAuley, 2017; Raichlen & Alexander, 2017; Sleiman et al., 2016). Given that persons with physical disabilities can experience substantial individual and environmental barriers to engaging in physical activity (Williams, Smith, & Papathomas, 2014), these individuals can find it challenging to meet recommended levels of physical activity for general health maintenance and promotion (Rocchi et al., 2017). Accordingly, emerging observational evidence shows negative associations between physical activity quantity and depressive or anxious symptom severity in persons with long-term physical disabilities (Jensen et al., 2012; Stroud & Minahan, 2009; Suh, Motl, & Mohr, 2010; Tawashy et al., 2009).
An extensive body of research has evaluated the role of physical activity in promoting psychological well-being in different clinical and non-clinical populations without physical disabilities (Teychenne, Ball, & Salmon, 2008). Evidence suggests that being physically active protects against developing both anxious and depressive conditions (Bélair, Kohen & Kingsbury, 2018; Mammen & Faulkner, 2013) and increases in physical activity can reduce anxious and depressive symptoms (Carek, Laibstain, & Carek, 2011; Craft & Landers, 1998; Cooney et al., 2013; Ströhle, 2009; Stronerock et al., 2015). Research also supports using physical activity interventions to treat depression, with some evidence showing antidepressive effects comparable to antidepressant medications (Carek et al., 2011; Blumenthal et al., 2007). Relative to the research literature examining the relationship between physical activity and depression, research examining the relationship between physical activity and anxiety is not as well-developed, although preliminary findings are promising (Carek et al., 2011; Martinsen, 2008; McEntee & Halgin, 1999). Taken together, the collective body of evidence supports a causal relationship between physical activity and both anxiety and depression in individuals without physical disabilities.
Research has also suggested that the quantity (or dose) of one’s physical activity may also have implications for affect regulation (Ströhle, 2008), although this research is mixed with regard to the particular quantities necessary for psychological benefits (Teychenne et al., 2008). For example, a trial that compared low- versus high- quantity physical activity regimens in adults with medication resistant depression found evidence of a dose-response relationship between physical activity and cognitive functioning, such that higher doses of physical activity were associated with greater improvements in cognitive functioning than were lower doses (Greer et al., 2015). Conversely, research in support of low quantities of physical activity posits that physical inactivity, in particular, is a risk factor for increased physical and psychological dysfunction, including increased negative affect and stress (Schultchen et al., 2019; Strohle, 2009). Consistent with this finding, some research suggests that even relatively low quantities of physical activity may be protective against the development of depression in the general population (Mammen & Faulkner, 2013; Dunn, Trivedi, & O’Neal, 2001). Collectively, the lack of consensus regarding the precise quantities of physical activity necessary to produce psychological benefits highlights the need for additional research in this area.
The existing research examining the effects of varied intensity of physical activity on psychological functioning is also collectively inconclusive. One study of adults with depression found that acute bouts of light, moderate, and hard exercise each produced the same levels of short-term improvements in depressed mood, suggesting the acute affective benefits of physical activity may not necessarily be influenced by the degree of intensity (Meyer et al., 2016). A cross-sectional study of adults with multiple sclerosis found that moderate physical activity was associated with reduced depression severity, and that quantity of strenuous physical activity was inversely associated with depression in middle-aged adults (45–64 years), but not younger (<45 years) or older (>64 years) age groups (Jensen et al., 2012). A meta-analysis of both observational and interventional research evaluating the relationship between physical activity and negative affect (anxiety and depression) found mixed evidence concerning the extent to which physical activity intensity played a significant role, with observational studies tending to favor vigorous-intensity physical activity, and interventional work finding comparable effects regardless of intensity (Teychenne et al., 2008). These inconsistencies suggest that further research clarifying the role of physical activity intensity for negative affect regulation is needed.
It is important to note, however, that the majority of the research evaluating the relationship between physical activity and anxiety or depression was conducted in non-clinical populations who do not have physical disabilities (Cooney et al., 2013; Teychenne et al., 2008; Rebar et al., 2015). In fact, this research often explicitly excludes individuals with physical impairments or disabilities (Cooney et al., 2013; Teychenne et al., 2008; Rebar et al., 2015). For example, a recent Cochrane review of trials examining physical activity interventions for treating depression included 39 trials, of which none studied populations with physical disabilities (Cooney et al., 2013). As stated previously, individuals with physical disabilities experience additional barriers to performing conventional physical activity, such as issues with ambulation and symptoms such as pain and fatigue (Williams, Smith, & Papathomas, 2014). Accordingly, physical activity for persons with physical disabilities often requires substantial modification and external assistance (Motl, 2014). The majority of the research examining the relationship between physical activity and psychological function has evaluated specific forms of physical activity (e.g., running or jogging, Blumenthal et al., 2007) that are difficult or even impossible for a large segment of the population of persons with physical disabilities. Thus, research examining the relationship between physical activity and psychological function in this population is needed to inform specific recommendations for physical activity, as well as how to most optimally adapt physical activity interventions to produce benefits to psychological health.
Given these considerations, here we sought to examine the longitudinal associations between physical activity and anxious and depressive symptom severity in adults with chronic physical disabilities. We hypothesized that greater levels of physical activity would be associated with reductions in the severity of depression and anxiety symptoms over time. Considering that research evaluating the relationship between different quantities and intensities of physical activity and negative affect is largely inconclusive, we also planned to evaluate whether the longitudinal associations between physical activity and negative affect varied as a function the quantity and intensity of physical activity.
Methods
Participants
The sample consisted of adults with one of four long-term physical disabilities (multiple sclerosis [MS], spinal cord injury [SCI], post-polio syndrome [PPS], and muscular dystrophy [MD]) who were participating in a large and ongoing USA based longitudinal survey study. These specific conditions were selected because they are each associated with substantial physical and psychological impairment. They each also represent a unique segment of the disability spectrum in terms of disability onset and progression: PPS represents late-life onset, SCI represents traumatic onset occurring throughout the lifespan, MS represents gradual, late-life onset, and MD represents rapid, early-life onset. Study inclusion criteria were: (1) the ability to read, write, and understand English; (2) self-report of a physician’s diagnosis of the primary physical condition; and (3) being at least 18 years of age. Prospective participants were screened over the phone by study staff and 2041 were deemed eligible and sent a copy of the consent form and baseline survey between June 2009 and March 2010. These 2041 eligible participants were recruited from the following sources: (1) advertisements in organization newsletters and websites (661; 33%); (2) involvement in a previous survey study at the University of Washington (473; 23%); (3) a University of Washington disability registry (398; 20%); (4) disability specific registries (375; 18%); (5) referral from a friend or relative (90; 4%); and other sources (44; 2%).
Procedures
The current study used data from a large, longitudinal survey which has also been described in other publications (e.g., Battalio et al., 2018; Battalio et al., 2019). A total of 1,862 out of the 2,041 eligible participants enrolled in the study (completed and returned the baseline survey and consent form). Enrolled individuals were mailed surveys on an approximately annual basis following the initial baseline survey. The current study used data from surveys corresponding to years four, five, and seven, as the other time points did not contain the necessary data to examine the current study’s aims and hypotheses. The year four survey (T1) was mailed between August 2012 and March 2013, and returned by 1594 participants. The year five survey (T2) was mailed between October 2014 and April 2014 and returned by 1380 participants. The year seven survey (T3) was mailed between October 2016 and May 2017 and returned by 1218 participants.
Several procedures were enacted to encourage compliance and ensure data integrity. Surveys were assessed by research staff for completeness, and staff called participants to obtain missing data if any were identified. Reminder letters were mailed to participants if no response survey was received by four weeks after the initial mailing, and staff made reminder calls if no response survey was received by six weeks after the initial mailing. Participants were also compensated $25 for each completed survey. All study procedures were approved by the institutional review board at the University of Washington (STUDY00000836).
Measures
Demographic/Descriptive variables.
Demographic data, including age, ethnicity, diagnosis, gender self-identification, and education level, were collected to describe the sample.
Anxiety and Depression severity.
Anxiety and depression symptom severity were each assessed using their respective Patient-Reported Outcomes Measurement System (PROMIS) short-forms (Cell et al., 2007, 2010; Pilkonis et al., 2011). PROMIS is an item bank measurement system intended for use across a broad clinical demographic. PROMIS measures are normed and scored into a t-score metric in which 50 is the mean and 10 is the standard deviation. PROMIS measures have been shown to be valid and reliable in populations with physical conditions (Cook, Bamer, Amtmann, Molton, & Jensen, 2012). Internal consistencies (Cronbach’s alphas) provided evidence for good reliability for the measure of anxiety (0.88) and excellent reliability for the measure of depression (0.91).
Physical Activity.
Physical activity was assessed using an adapted version of the Godin Leisure-Time Exercise Questionnaire (GLTEQ; Godin, 2011). With the GLTEQ, respondents are asked to report the number of days in the past week that they engaged in three different types of exercise for at least 15 minutes: (1) strenuous exercise (“heart beats rapidly”), (2) moderate exercise (“not exhausting”), and (3) mild exercise (“minimal effort”). These values are then converted into a weekly MET equivalent value (Godin, 2011; Amireault & Godin, 2015). For example, if respondents indicate engaging in no physical activity, the corresponding MET value would be zero. The difference between the adapted GLTEQ used here and the original measure is that we chose to assess the number of days in the past week that the respondent engaged in each type of exercise for at least 15 minutes, rather than the number of times the respondent engaged in each type of exercise for at least 15 minutes in the past week. We employed the same recommended scoring technique as the original measure. In order support the validity of this adaptation, we computed a bivariate correlation between the weekly MET activity score from the adapted GLTEQ and the total MET score from the International Physical Activity Questionnaire (IPAQ; Hagströmer, Oja, & Sjöström, 2006) at T1. We found a moderate correlation coefficient between the two measures (r = .45, p < 0.001), which was comparable to the bivariate correlation coefficient found between the unadapted GLTEQ and IPAQ in a study of physical activity measurement tools in a sample of adults with MS (r = .37, p = 0.44; Gosney, Scott, Snook, & Motl, 2007).
Data Analysis
We first computed descriptive statistics (frequencies for categorical variables; means and standard deviations for continuous variables) of demographic variables to describe the sample. Prior to performing the primary study analyses, we assessed the distributions of the study variables to ensure they met necessary assumptions. Specifically, we assessed the variables for multivariate normality by inspecting histograms and computing the skewness score for each primary study variable at each time point. We used an a priori skewness cutoff value of <3 to identify problematic skew (Tabachnick & Fidell, 1996). All histograms appeared approximately normal, and no skewness value surpassed an absolute value of 1.63. Missing data across time were accounted for using maximum likelihood estimation in order to preserve statistical power. Spaghetti plots also evidenced approximately linear relationships between each primary study variable and time. Therefore, we treated time linearly in the primary analyses.
To test the primary study hypothesis and evaluate the longitudinal relationships between anxiety symptom severity, depression symptom severity, and physical activity, we conducted mixed growth curve models using a multilevel modeling approach (also known as hierarchical linear modeling and mixed-effects modeling). See Kwok et al. (2008) for a detailed overview of this mixed growth curve modeling approach to assessing panel data. Although other analytic techniques (such as structural equation modeling or ordinary least squares regression) can also be used to analyze longitudinal data, mixed growth curve models are preferable because they account for the dependency of repeated measurements in longitudinal data, and allow one to assess between-persons differences in within-person change over time (Curran, Obeidat, & Losardo, 2010; Kwok et al., 2008; Rabe-Hesketh & Skrondal, 2008; Twisk, 2003, 2006). Mixed growth curve models are effectively an extension of linear regression; because of this, many of the model components can be interpreted similarly. For example, model estimates corresponding to each independent variable are comparable to the beta coefficient in a linear regression analysis. Changes in fit statistics and other model parameters that occur with each model progression (outlined below) can be interpreted in the same way as changes in fit corresponding to each step in hierarchical linear regression analyses.
We conducted two series of mixed growth curve models; one with anxiety symptom severity as the criterion and one with depression symptom severity as the criterion. Each series involved the same model progressions. The first model (Model ICC) was a random-intercept model, and was used to compute the Intraclass Correlation (ICC), which is a ratio of within- to between- person variance. The second model (Model A) was a linear growth model, in which time (treated continuously and coded such that T1 was 0, T2 was 1, and T3 was 3) was entered as both a fixed and random effect. In the third model (Model B), we entered demographic control variables (gender [dummy coded such that self-report of female was the reference group], diagnostic group [dummy coded such that SCI was the reference group in order to remain consistent with past research from our group), and age [at T1]). These control variables were included because it is best practice in rehabilitation research, and, as a result, it is common practice in observational and longitudinal studies (e.g., De la Vega et al., 2018; Brienza et al., 2018). In the fourth model (Model C), we entered the measure of weekly physical activity. Physical activity was decomposed into two separate terms: (1) the person-level mean value across all time points and (2) the deviation from the mean at each time point (Hoffman & Stawski, 2009). The person-level mean term was used to represent the between-persons relationship between physical activity and the criterion, and the deviation score was used to represent the relationship between within-person change in physical activity over time and the criterion (Hoffman & Stawski, 2009).
In order to examine the nature of the relationship between physical activity quantity in the longitudinal associations, we also added a squared physical activity term to Model C (Model Ca). This squared term allowed us to identify whether relationships between physical activity, anxiety symptoms, and depression symptoms exhibited curvilinear qualities; in other words, whether the strength of the association varied depending on the total quantity of physical activity. The coefficient corresponding to the squared physical activity term was assessed for statistical significance to determine whether a potential curvilinear relationship between physical activity and each criterion was present. In addition, we also computed prediction plots for each criterion variable (using the Stata twoway function) in order to visualize statistically significant associations between physical activity and the criterion. If the squared physical activity term from Model Ca was statistically significant, we fitted a quadratic prediction plot. If the squared physical activity term was not statistically significant, we fitted a linear prediction plot. These plots served to clarify the role of intensity by both probing potential curvilinear relationships and showing differences in statistical significance in the relationship between physical activity and anxiety or depression symptom severity across different quantities of physical activity.
Finally, in order to determine whether different intensities of physical activity were differentially associated with changes in affect over time, we replaced the weekly physical activity terms in Model C with three frequency terms corresponding to the days in which the participant reported engaging in mild, moderate, and strenuous physical activity during the past week. Effect sizes and statistical significance of each physical activity intensity term were evaluated to determine whether different intensities of physical activity demonstrated unique longitudinal associations with negative affect over time.
The likelihood ratio test was used to assess improvements in model fit with each new model. We tested an unstructured covariance structure for between-individual random effects and an autoregressive covariance structure for within-individual random errors. If either resulted in statistically significant improvements in model fit, they were maintained in subsequent models. The coefficients corresponding to each physical activity term and the likelihood ratio test corresponding to Model C were used to assess the association between physical activity and the criterion measure (anxiety or depression symptom severity).
The descriptive analyses were conducted in SPSS version 19 for Windows; all other analyses were conducted in Stata version 12.1 for Windows. Mixed growth curve models were computed using the xtmixed function.
Results
Participant Characteristics
The final sample (n=1594) is described in Table 1. As can be seen, the majority of the sample was White (91%) and well-educated (56% college educated or higher). Table 2 presents ICC, means and standard deviations of primary study variables. As can be seen, the sample reported an average of 18.28 (SD=10.50) years since formal diagnosis of the primary physical disability. All three primary study variables had comparable levels of stability. Mean values of the weekly MET activity score ranged between 20.55 and 23.06. On average, participants reported engaging in mild exercise most frequently, followed by moderate then strenuous (we did not formally test these differences for statistical significance).
Table 1.
Demographics
| Variable | N | Mean ± SD or Percent |
|---|---|---|
|
| ||
| Age | 1594 | 59.25 ± 12.96 |
| Gender | ||
| Men | 577 | 36% |
| Women | 1,016 | 64% |
| Education Level | ||
| 9th grade or less | 4 | <1% |
| Some high school | 19 | 1% |
| High school graduate or GED | 189 | 12% |
| Vocational or technical school | 99 | 6% |
| Some college | 377 | 24% |
| College graduate | 499 | 31% |
| Professional/Graduate School | 405 | 25% |
| Ethnicity/Race | ||
| White/Caucasian | 1454 | 91% |
| Black/African American | 52 | 3% |
| Native American/Alaska Native | 9 | <1% |
| Asian | 13 | 1% |
| Hispanic | 20 | 1% |
| More than one race | 33 | 2% |
| Unknown | 4 | <1% |
| Missing | 9 | <1% |
| Diagnosis | ||
| Muscular Dystrophy | 282 | 18% |
| Multiple Sclerosis | 509 | 32% |
| Post-Polio Syndrome | 389 | 24% |
| Spinal Cord Injury | 414 | 26% |
| Years since diagnosis | 1530 | 18.28 ± 10.50 |
Abbreviation: GED, General Educational Development.
Table 2.
Means and standard deviations of the study variables at each assessment point
| Variable | T1 | T2 | T3 | ICC |
|---|---|---|---|---|
|
| ||||
| Anxiety* | 51.74 ± 8.89 | 50.95 ± 9.03 | 51.16 ± 8.87 | 0.59 |
| Depression* | 50.10 ± 8.82 | 52.09 ± 8.79 | 51.33 ± 8.95 | 0.62 |
| Physical activity | ||||
| Weekly Met | 20.55 ± 24.64 | 18.89 ± 23.11 | 23.06 ± 23.23 | 0.51 |
| Mild days | 2.35 ± 2.56 | 2.34 ± 2.55 | 2.75 ± 2.70 | |
| Moderate days | 1.33 ± 2.08 | 1.09 ± 1.91 | 1.80 ± 2.30 | |
| Strenuous days | 0.76 ± 1.61 | 0.74 ± 1.61 | 0.65 ± 1.47 | |
Note: Values presented are mean ± standard deviation.
Mean general U.S. population ± SD is 50±10 on all PROMIS measures.
We also evaluated the data to determine whether those with some missing data across follow-up time points (n=476) differed from those with no missing data (n=1,118). Those with some missing data were slightly older (mean, 60.43±14.99y) than those without missing data (mean, 58.76±11.96y; t1592 = 2.36, P = 0.018). There were not statistically significant differences in missingness based on gender (χ2[1] = 2.09, p = 0.15). To determine whether possible patterns in missingness across time biased results, we conducted multiple imputation using multivariate normal regression and compared the primary final mixed growth curve models against the same model with imputed data (Schafer, 1997). The models did not differ in terms of estimates (no estimates that were significant became non-significant or the inverse, and effect sizes remained comparable). Log likelihood values indicated that primary models using full information maximum likelihood estimation for missing data had slightly better fit than models using imputed data. This slight worsening of fit, accompanied by the lack of differences in terms of estimates, suggests missingness did not bias the study analyses.
Mixed Growth Curve Models
For models with anxiety symptom severity as the criterion, neither an unstructured nor autoregressive covariance structure resulted in improvements in model fit. For models with depression symptom severity as the criterion, however, an autoregressive covariance structure resulted in significant improvements in model fit, χ2[1] = 5.14, p < .05.
Table 3 reports results of the mixed growth curve models evaluating the longitudinal associations between physical activity, anxiety symptom severity, and depression symptom severity. In models assessing anxiety severity, the addition of the physical activity terms to the model (Model C) resulted in significant improvements in model fit, χ2[2] = 21.66, p < .001. Only the between-person physical activity estimate was significantly associated with anxiety (z = −4.26, p < .001), though the within-person estimate was trending toward statistical significance (z = −1.94, p = .052). In models assessing depression severity, the addition of physical activity terms to the model (Model C) resulted in significant improvements in model fit, χ2[2] = 84.01, p < .001. Both the between-person (z = −8.47, p < .001) and within-person (z = −3.70, p < .001) physical activity terms were statistically significant.
Table 3.
Summary of random growth curve models
| Estimate | Anxiety | Depression | ||
|---|---|---|---|---|
|
| ||||
| Coefficient | Z-score | Coefficient | Z-score | |
|
| ||||
| Physical Activity: Fixed Effects | ||||
| Between | −0.04 ± 0.01 | −4.26* | −0.08 ± 0.01 | −8.51* |
| [−0.06, −0.02] | [−0.10, −0.06] | |||
| Within | −0.01 ± 0.01 | −1.94 | −0.02 ± 0.01 | −3.61* |
| [−0.03, 0.00] | [−0.04, −0.01] | |||
| Quadratic | 0.00±0.00 | 0.65 | 0.00 ± 0.00 | 2.23* |
| [−0.00, 0.00] | [0.00, 0.00] | |||
| Mild | −0.03 ± 0.05 | −0.59 | −0.06 ± 0.05 | −1.29 |
| [−0.12, 0.07] | [−0.15, 0.03] | |||
| Moderate | −0.14 ± 0.06 | −2.24* | −0.33 ± 0.06 | −5.48* |
| [−0.26, −0.02] | [−0.45, −0.21] | |||
| Strenuous | −0.22 ± 0.09 | −2.59* | −0.32 ± 0.08 | −3.90* |
| [−0.39, −0.05] | [−0.48, −0.16] | |||
| Model C Fit | ||||
| Likelihood Ratio | χ2 [2] = 21.66* | χ2 [2] = 84.01* | ||
| −2LL | 13905.04 | 13670.80 | ||
Note: ± Designates Standard Error; Values in brackets are 95% confidence intervals.
P < .05;
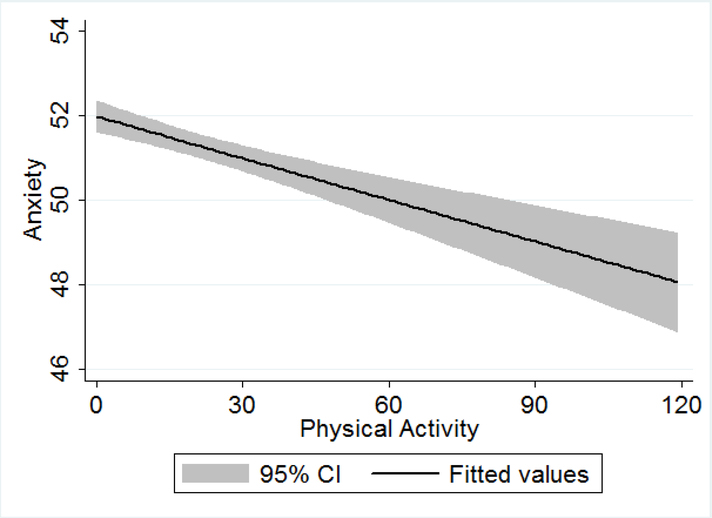
The quadratic estimate – used to examine whether the strength and significance of associations differed curvilinearly based on physical activity quantity – for depression severity (z = 2.23, p < .05) was significant, but the estimate for anxiety severity (z = 0.65, p > .05) was not. Therefore, we fitted a quadratic prediction plot for depression severity and a linear prediction plot for anxiety severity (Figures 1 and 2, respectively). The plots show that the associations between physical activity and both anxiety and depression are strongest at low-to-moderate quantities of physical activity, after which the statistical significance and strength of the associations weakened considerably.
Figure 1.
Depression by physical activity quantity prediction plot
Figure 2.
Anxiety by physical activity quantity prediction plot
In models assessing the mild, moderate, and strenuous physical activity intensity terms, the mild physical activity terms were not significantly associated with either anxiety or depression severity. However, the moderate (anxiety z = −2.24, p < .05; depression z = −5.48, p < .001) and strenuous (anxiety z = −2.59, p < .05; depression z = −3.90, p < .001) physical activity terms were statistically significant and showed comparable effect sizes.
Discussion
We sought to examine the longitudinal associations between physical activity and measures of depression and anxiety symptom severity in a sample of adults with chronic physical conditions. We hypothesized that greater quantities of physical activity would be associated with subsequent reductions in anxious and depressive symptom severity over the approximately four-year period. We also examined whether the features of the association between physical activity and psychological function differed depending on the total quantity of physical activity (i.e., would be curvilinear) or based on the composition of the physical activity in terms of intensity. In support of the study hypothesis, greater quantities of physical activity were associated with reductions in both anxiety and depression severity over time. In addition, the association between physical activity and depression severity was found to be curvilinear. While the association between physical activity and anxiety severity was not curvilinear, the associations between physical activity and both anxiety and depression were found to be strongest for low-to-moderate physical activity quantity, with statistical significance becoming lower as the quantity of physical activity increased. Analyses examining the associations between different intensities of physical activity found that strenuous and moderate, but not mild, physical activity were associated with improved physical function over time. These findings provide novel insight into the longitudinal associations between physical activity and psychological function in individuals with long-term physical conditions.
The current study is, to our knowledge, the first to evaluate the longitudinal association between physical activity and psychological function over time in persons with long-term physical disabilities. The findings are consistent with previous research on this topic, providing evidence that physical activity is not only concurrently associated with psychological function, but also associated with improved psychological function over time. In addition, although physical activity was associated with reductions in both anxiety and depression over time, physical activity was more strongly associated with depression symptom severity than anxiety symptom severity. This finding is consistent with current evidence in non-clinical adult populations, which has shown that physical activity tends to be more strongly associated with depression than with anxiety (Rebar et al., 2015). The current study is the first (to our knowledge) to directly evaluate the associations between physical activity and both anxiety and depression severity in the same sample of adults with physical disabilities. Future research should continue to examine whether physical activity is differentially associated with various dimensions of negative affect (e.g., emotions, mood, and core affect) and affective disorders (e.g., depressive disorders, anxiety disorders).
We also found that the association between physical activity and psychological functioning differed as a function of the quantity and intensity of physical activity. The associations between physical activity and both depression and anxiety symptom severity were stronger in the low-to-moderate range of total weekly quantity of physical activity, with statistical significance tapering off considerably from moderate quantities onward. In addition, the association between physical activity and depression severity was curvilinear, such that the effect size of the association between physical activity and depression severity also reduced substantially from moderate quantities of physical activity and greater. However, moderate and strenuous intensities of physical activity appeared to be the primary drivers of the association between physical activity and negative affect, with mild physical activity demonstrating no significant association with negative affect.
In terms of overall physical activity quantity, the findings are consistent with existing cross-sectional research that has suggested that physical inactivity may be a key behavioral factor implicated in negative affect dysregulation. In other words, our findings suggest the possibility that only moderate quantities of physical activity may be necessary in order to impart negative affective benefits. However, given that mild physical activity was not significantly associated with negative affect, the findings also suggest the possibility that, while only moderate quantities of physical activity may be necessary to support benefits relevant to negative affect, this physical activity may need to be moderate intensity or greater to exact tangible benefits. It is also possible that there exists a physical activity quantity threshold that must be met in order to see tangible benefits, and that this threshold may be met through at least moderate intensities of physical activity. Yet another possible explanation for this finding is that individuals who are more functionally able, and thus more capable of intense physical activity, also tended to be more psychologically healthy. It is not possible to clarify these intricacies with observational research alone; future experimental research is needed to determine the precise role of physical activity quantity and intensity in regulating negative affect.
The current findings have important clinical implications for populations of individuals with physical disabilities. Given that physical activity was associated longitudinally with reductions in negative affect, this suggests that rehabilitation clinicians should consider targeting increases in physical activity in patients with long-term physical conditions who also present with high levels of anxiety and depression symptom severity. However, given that quantity and intensity of physical activity appear to be relevant, the specific program of physical activity most appropriate for any one patient may require refinement if a goal of the intervention is negative affect regulation. Furthermore, for individuals with long-term physical conditions, there are numerous additional complications and barriers that can make engaging in physical activity challenging (Williams, Smith, & Papathomas, 2014; Rocchi et al., 2017). This difficulty in engaging in physical activity is also reflected in the current sample, as mean levels of weekly physical activity were lower than commonly endorsed guidelines (Amireault & Godin, 2015). Given these factors, physical activity interventions to improve psychological function will need to balance feasibility with the necessary overall quantity and intensity of physical activity. In addition, prescribing physical activity interventions in combination with supported behavioral and psychological treatments (Butler, Chapman, Forman, & Beck, 2006; Hofmann & Gómez, 2017) may result in synergistic improvement in affective conditions among adults with physical conditions. Future research to evaluate this possibility is warranted.
The current findings are generally consistent with existing physical activity guidelines for populations with physical disability (Ginis et al., 2011; Latimer-Cheung et al., 2013). Although some degree of variability in specific recommendations exist depending on the particular disability of interest, they generally recommend modestly amounts of weekly moderate-to-vigorous physical activity (e.g., two 20-minute bouts of moderate to vigorous aerobic activity per week; Ginis et al., 2011), which are roughly comparable to the levels found here to support associations with negative affect over time. However, while these guidelines may be sufficient to inform physical activity for persons with mild-to-moderate functional impairment, they may be insufficient for persons with severely impaired physical capacity. Further research is necessary to create or modify physical activity interventions to circumvent impairment and still obtain sufficient quantities of moderate-to-intense physical activity for negative affect regulation. This research should use objective, physical markers (e.g., heart rate) to identify and tailor adapted physical activity interventions to match non-adapted counterparts.
In addition, the current study and the vast majority of the research to date in this area has relied on self-reported, retrospective measures to evaluate physical activity. While self-reported physical activity can provide valid and useful information, reports of the validity of self-reported physical activity are mixed, with some evidence suggesting a tendency to under-report sedentary behavior and overestimate physical activity (Nicolson et al., 2018; Kormos & Gifford, 2014; Affuso et al., 2011). Recent technological advancements allow researchers to complement self-reported data with objective ambulatory monitoring technologies (e.g., actigraphy, portable electrocardiography) (Clark et al., 2017; Evenson, Goto, & Furberg, 2015). Furthermore, real-time self-report (e.g., ecological momentary assessment) can address recall issues with retrospective self-reported measures (Knell et al., 2017). However, many of these technologies are still in their infancy, and numerous factors can influence their validity and reliability (Migueles et al., 2017). Future research should continue to explore the optimal approach to measuring physical activity, which likely involves some combination of real-time self-reported assessment and objective ambulatory monitoring.
Study Limitations
The current study has several important limitations that warrant consideration when interpreting the results. The study used a convenience sample of adults that were primarily white and well-educated. In addition, missingness across time was associated with being slightly older. For these reasons, future research that evaluates the role of physical activity in regulating negative affect in additional samples of individuals with physical disabilities is needed to increase our confidence in the generalizability of the study findings. In addition, while the study analyses are robust and longitudinal, they are still correlational. As a result, the direction of the relationship between physical activity and psychological function remains unclear; there could be additional confounding variables that may explain the associations found between physical activity and psychological function. Given these considerations, a causal relationship between physical activity and negative affect can only be inferred from the current findings. Prospective and experimental research is necessary to clarify causal relationships. In addition, as mentioned previously, self-reported, retrospective measures of physical activity can suffer from reporting and recall biases. Real-time self-report (ecological momentary assessment) alongside objective, ambulatory physical activity monitoring should be employed when possible to replicate and build upon these findings. Finally, although the current study evaluated two key domains of physical activity (quantity and intensity) it did not evaluate the role of physical activity frequency in regulating negative affect. Future research should examine the how frequency might influence the relationship between physical activity and negative affect, as well as how frequency may interact with quantity and intensity to influence this relationship. Granular, ambulatory assessment methods (such as those outlined above) are particularly well-suited to address this research inquiry.
Conclusions
The current study evaluated the longitudinal associations between physical activity and psychological function in adults with chronic physical conditions. The findings demonstrated that moderate quantities of physical activity, consisting primarily of moderate-to-vigorous intensities, were associated with reductions in depression and anxiety symptom severity over time. These findings suggest that rehabilitation clinicians should incorporate physical activity interventions into the treatment of adults with physical conditions who present with anxiety and depression. Future experimental and prospective research that employs real-time, self-reported assessments along with objective ambulatory monitoring is necessary to clarify the causal associations between physical activity and different domains of psychological function.
Acknowledgement of financial support and conflict of interest:
The contents of this publication were developed under a grant from National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant number 90RT5023-01-00, NIDIRR grant number H133B080024). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this publication do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government.
References
- Affuso O, Stevens J, Catellier D, McMurray RG, Ward DS, Lytle L, … & Young DR (2011). Validity of self-reported leisure-time sedentary behavior in adolescents. Journal of negative results in biomedicine, 10(1), 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amireault S, & Godin G (2015). The Godin-Shephard Leisure-Time Physical Activity Questionnaire: Validity evidence supporting its use for classifying healthy adults into active and insufficiently active categories. Perceptual and Motor Skills, 120(2), 604–622 [DOI] [PubMed] [Google Scholar]
- Asmundson GJ, & Katz J (2009). Understanding the co-occurrence of anxiety disorders and chronic pain: State-of-the-art. Depression and Anxiety, 26, 888–901. 10.1002/da.20600 [DOI] [PubMed] [Google Scholar]
- Awick EA, Phillips SM, Lloyd GR, & McAuley E (2017). Physical activity, self-efficacy and self-esteem in breast cancer survivors: a panel model. Psycho-Oncology, 26(10), 1625–1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Battalio SL, Glette M, Alschuler KN, & Jensen MP (2018). Anxiety, depression, and function in individuals with chronic physical conditions: A longitudinal analysis. Rehabilitation psychology, 63(4), 532. [DOI] [PubMed] [Google Scholar]
- Battalio SL, Jensen MP, & Molton IR (2019). Secondary health conditions and social role satisfaction in adults with long-term physical disability. Health Psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bélair MA, Kohen DE, Kingsbury M, & Colman I (2018). Relationship between leisure time physical activity, sedentary behaviour and symptoms of depression and anxiety: evidence from a population-based sample of Canadian adolescents. BMJ open, 8(10), e021119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenthal JA, Babyak MA, Doraiswamy PM, Watkins L, Hoffman BM, Barbour KA, … & Hinderliter A (2007). Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosomatic medicine, 69(7), 587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler AC, Chapman JE, Forman EM, & Beck AT (2006). The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clinical psychology review, 26(1), 17–31. [DOI] [PubMed] [Google Scholar]
- Brenes GA, Guralnik JM, Williamson JD, Fried LP, Simpson C, Simonsick EM, & Penninx BW (2005). The influence of anxiety on the progression of disability. Journal of the American Geriatrics Society, 53(1), 34–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brienza D, Krishnan S, Karg P, Sowa G, & Allegretti AL (2018). Predictors of pressure ulcer incidence following traumatic spinal cord injury: a secondary analysis of a prospective longitudinal study. Spinal cord, 56(1), 28. [DOI] [PubMed] [Google Scholar]
- Carek PJ, Laibstain SE, & Carek SM (2011). Exercise for the treatment of depression and anxiety. The International Journal of Psychiatry in Medicine, 41(1), 15–28. [DOI] [PubMed] [Google Scholar]
- Clark CC, Barnes CM, Stratton G, McNarry MA, Mackintosh KA, & Summers HD (2017). A review of emerging analytical techniques for objective physical activity measurement in humans. Sports medicine, 47(3), 439–447. [DOI] [PubMed] [Google Scholar]
- Craft LL, & Landers DM (1998). The effect of exercise on clinical depression and depression resulting from mental illness: A meta-analysis. Journal of Sport and Exercise Psychology, 20(4), 339–357. [Google Scholar]
- Curran PJ, Obeidat K, & Losardo D (2010). Twelve frequently asked questions about growth curve modeling. Journal of cognition and development, 11(2), 121–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De la Vega R, Groenewald C, Bromberg MH, Beals-Erickson SE, & Palermo TM (2018). Chronic pain prevalence and associated factors in adolescents with and without physical disabilities. Developmental Medicine & Child Neurology, 60(6), 596–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn AL, Trivedi MH, & O’Neal HA (2001). Physical activity dose-response effects on outcomes of depression and anxiety. In Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews [Internet]. Centre for Reviews and Dissemination; (UK: ). [DOI] [PubMed] [Google Scholar]
- Evenson KR, Goto MM, & Furberg RD (2015). Systematic review of the validity and reliability of consumer-wearable activity trackers. International Journal of Behavioral Nutrition and Physical Activity, 12(1), 159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfield AC, & Lincoln NB (2012). Factors affecting anxiety in multiple sclerosis. Disability and rehabilitation, 34(24), 2047–2052. [DOI] [PubMed] [Google Scholar]
- Gay MC, Vrignaud P, Garitte C, & Meunier C (2010). Predictors of depression in multiple sclerosis patients. Acta Neurologica Scandinavica, 121(3), 161–170. [DOI] [PubMed] [Google Scholar]
- Ginis KM, Hicks AL, Latimer AE, Warburton DER, Bourne C, Ditor DS, … & Pomerleau P (2011). The development of evidence-informed physical activity guidelines for adults with spinal cord injury. Spinal cord, 49(11), 1088. [DOI] [PubMed] [Google Scholar]
- Godin G (2011). The Godin-Shephard leisure-time physical activity questionnaire. Health & Fitness Journal of Canada, 4(1), 18–22. [Google Scholar]
- Gosney JL, Scott JA, Snook EM, & Motl RW (2007). Physical activity and multiple sclerosis: validity of self-report and objective measures. Family & community health, 30(2), 144–150. [DOI] [PubMed] [Google Scholar]
- Greer TL, Grannemann BD, Chansard M, Karim AI, & Trivedi MH (2015). Dose-dependent changes in cognitive function with exercise augmentation for major depression: results from the TREAD study. European Neuropsychopharmacology, 25(2), 248–256. [DOI] [PubMed] [Google Scholar]
- Hagströmer M, Oja P, & Sjöström M (2006). The International Physical Activity Questionnaire (IPAQ): a study of concurrent and construct validity. Public health nutrition, 9(6), 755–762. [DOI] [PubMed] [Google Scholar]
- Hoffman L, & Stawski RS (2009). Persons as contexts: Evaluating between-person and within-person effects in longitudinal analysis. Research in Human Development, 6, 97–120. [Google Scholar]
- Hofmann SG, & Gómez AF (2017). Mindfulness-based interventions for anxiety and depression. Psychiatric Clinics, 40(4), 739–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen MP, Molton IR, Gertz KJ, Bombardier CH, & Rosenberg DE (2012). Physical activity and depression in middle and older-aged adults with multiple sclerosis. Disability and health journal, 5(4), 269–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knell G, Gabriel KP, Businelle MS, Shuval K, Wetter DW, & Kendzor DE (2017). Ecological momentary assessment of physical activity: validation study. Journal of medical Internet research, 19(7), e253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kormos C, & Gifford R (2014). The validity of self-report measures of proenvironmental behavior: A meta-analytic review. Journal of Environmental Psychology, 40, 359–371. [Google Scholar]
- Korostil M, & Feinstein A (2007). Anxiety disorders and their clinical correlates in multiple sclerosis patients. Multiple Sclerosis Journal, 13(1), 67–72. [DOI] [PubMed] [Google Scholar]
- Kwok OM, Underhill AT, Berry JW, Luo W, Elliott TR, & Yoon M (2008). Analyzing longitudinal data with multilevel models: An example with individuals living with lower extremity intra-articular fractures. Rehabilitation psychology, 53(3), 370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latimer-Cheung AE, Ginis KAM, Hicks AL, Motl RW, Pilutti LA, Duggan M, … & Smith KM (2013). Development of evidence-informed physical activity guidelines for adults with multiple sclerosis. Archives of physical medicine and rehabilitation, 94(9), 1829–1836. [DOI] [PubMed] [Google Scholar]
- Lester K, Stepleman L, & Hughes M (2007). The association of illness severity, self-reported cognitive impairment, and perceived illness management with depression and anxiety in a multiple sclerosis clinic population. Journal of Behavioral Medicine, 30(2), 177–186. [DOI] [PubMed] [Google Scholar]
- Lim SW, Shiue YL, Ho CH, Yu SC, Kao PH, Wang JJ, & Kuo JR (2017). Anxiety and depression in patients with traumatic spinal cord injury: a nationwide population-based cohort study. PloS one, 12(1), e0169623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mammen G, & Faulkner G (2013). Physical activity and the prevention of depression: a systematic review of prospective studies. American journal of preventive medicine, 45(5), 649–657. [DOI] [PubMed] [Google Scholar]
- Martinsen EW (2008). Physical activity in the prevention and treatment of anxiety and depression. Nordic journal of psychiatry, 62(sup47), 25–29. [DOI] [PubMed] [Google Scholar]
- Marrie RA, Cohen J, Stuve O, Trojano M, Sørensen PS, Reingold S, … & Reider N (2015). A systematic review of the incidence and prevalence of comorbidity in multiple sclerosis: overview. Multiple Sclerosis Journal, 21(3), 263–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEntee DJ, & Halgin RP (1999). Cognitive group therapy and aerobic exercise in the treatment of anxiety. Journal of College Student Psychotherapy, 13(3), 37–55. [Google Scholar]
- Cooney GM, Dwan K, Greig CA, Lawlor DA, Rimer J, Waugh FR, … & Mead GE (2013). Exercise for depression. Cochrane database of systematic reviews, (9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer JD, Koltyn KF, Stegner AJ, Kim JS, & Cook DB (2016). Influence of exercise intensity for improving depressed mood in depression: a dose-response study. Behavior therapy, 47(4), 527–537. [DOI] [PubMed] [Google Scholar]
- Migueles JH, Cadenas-Sanchez C, Ekelund U, Nyström CD, Mora-Gonzalez J, Löf M, … & Ortega FB (2017). Accelerometer data collection and processing criteria to assess physical activity and other outcomes: a systematic review and practical considerations. Sports medicine, 47(9), 1821–1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motl RW (2014). Benefits, safety, and prescription of exercise in persons with multiple sclerosis. Expert review of neurotherapeutics, 14(12), 1429–1436. [DOI] [PubMed] [Google Scholar]
- Nicolson PJ, Hinman RS, Wrigley TV, Stratford PW, & Bennell KL (2018). Self-reported Home Exercise Adherence: A Validity and Reliability Study Using Concealed Accelerometers. journal of orthopaedic & sports physical therapy, 48(12), 943–950. [DOI] [PubMed] [Google Scholar]
- Pangalila RF, Van Den Bos GA, Bartels B, Bergen M, Stam HJ, & Roebroeck ME (2015). Prevalence of fatigue, pain, and affective disorders in adults with Duchenne muscular dystrophy and their associations with quality of life. Archives of physical medicine and rehabilitation, 96(7), 1242–1247. [DOI] [PubMed] [Google Scholar]
- Peluso Marco Aurélio Monteiro, & Andrade Laura Helena Silveira Guerra de. (2005). Physical activity and mental health: the association between exercise and mood. Clinics, 60(1), 61–70. 10.1590/S1807-59322005000100012 [DOI] [PubMed] [Google Scholar]
- Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, & Cella D (2011). Item Banks for Measuring Emotional Distress from the Patient-Reported Outcomes Measurement Information System (PROMIS): Depression, Anxiety, and Anger. Assessment, 18(3), 263–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabe-Hesketh S, & Skrondal A (2008). Multilevel and longitudinal modeling using Stata. College Station, TX: STATA Press. [Google Scholar]
- Raichlen DA, & Alexander GE (2017). Adaptive capacity: an evolutionary neuroscience model linking exercise, cognition, and brain health. Trends in neurosciences, 40(7), 408–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rebar AL, Stanton R, Geard D, Short C, Duncan MJ, & Vandelanotte C (2015). A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health psychology review, 9(3), 366–378. [DOI] [PubMed] [Google Scholar]
- Rocchi M, Routhier F, Latimer-Cheung AE, Ginis KM, Noreau L, & Sweet SN (2017). Are adults with spinal cord injury meeting the spinal cord injury-specific physical activity guidelines? A look at a sample from a Canadian province. Spinal cord, 55(5), 454. [DOI] [PubMed] [Google Scholar]
- Sareen J, Cox BJ, Clara I, & Asmundson GJ (2005). The relationship between anxiety disorders and physical disorders in the US National Comorbidity Survey. Depression and anxiety, 21(4), 193–202. [DOI] [PubMed] [Google Scholar]
- Schafer JL (1997). Analysis of incomplete multivariate data. Chapman and Hall/CRC. [Google Scholar]
- Schultchen D, Reichenberger J, Mittl T, Weh TRM, Smyth JM, Blechert J, & Pollatos O (2019). Bidirectional relationship of stress and affect with physical activity and healthy eating. British Journal of Health Psychology. 10.1111/bjhp.12355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sleiman SF, Henry J, Al-Haddad R, El Hayek L, Haidar EA, Stringer T, … & Ninan I (2016). Exercise promotes the expression of brain derived neurotrophic factor (BDNF) through the action of the ketone body β-hydroxybutyrate. Elife, 5, e15092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stonerock GL, Hoffman BM, Smith PJ, & Blumenthal JA (2015). Exercise as treatment for anxiety: systematic review and analysis. Annals of behavioral medicine, 49(4), 542–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ströhle A (2009). Physical activity, exercise, depression and anxiety disorders. Journal of neural transmission, 116(6), 777. [DOI] [PubMed] [Google Scholar]
- Stroud NM, & Minahan CL (2009). The impact of regular physical activity on fatigue, depression and quality of life in persons with multiple sclerosis. Health and quality of life outcomes, 7(1), 68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suh Y, Motl RW, & Mohr DC (2010). Physical activity, disability, and mood in the early stage of multiple sclerosis. Disability and Health Journal, 3(2), 93–98. [DOI] [PubMed] [Google Scholar]
- Tabachnick B, & Fidell L (1996). Using multivariate statistics (3rd ed.). New York, NY: Harper Collins. [Google Scholar]
- Tawashy AE, Eng JJ, Lin KH, Tang PF, & Hung C (2009). Physical activity is related to lower levels of pain, fatigue and depression in individuals with spinal-cord injury: a correlational study. Spinal cord, 47(4), 301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teychenne M, Ball K, & Salmon J (2008). Physical activity and likelihood of depression in adults: a review. Preventive medicine, 46(5), 397–411. [DOI] [PubMed] [Google Scholar]
- Twisk J (2003). Applied longitudinal data analysis for epidemiology: A practical guide. New York, NY: Cambridge University Press. [Google Scholar]
- Twisk J (2006). Applied multilevel analysis: A practical guide. New York, NY: Cambridge University Press. [Google Scholar]
- Williams R, & Murray A (2015). Prevalence of depression after spinal cord injury: a meta-analysis. Archives of physical medicine and rehabilitation, 96(1), 133–140. [DOI] [PubMed] [Google Scholar]
- Williams TL, Smith B, & Papathomas A (2014). The barriers, benefits and facilitators of leisure time physical activity among people with spinal cord injury: a meta-synthesis of qualitative findings. Health Psychology Review, 8(4), 404–425. [DOI] [PubMed] [Google Scholar]
- Wood B, van der Mei IA, Ponsonby A-L, Pittas F, Quinn S, Dwyer T, … Taylor BV (2013). Prevalence and concurrence of anxiety, depression and fatigue over time in multiple sclerosis. Multiple Sclerosis Journal, 19, 217–224. 10.1177/1352458512450351 [DOI] [PubMed] [Google Scholar]