Abstract
Objective
Echocardiography is helpful in assessment of pulmonary hemodynamic, however its correlation with Right heart catheterization (RHC) is conflicting. We conducted a study to evaluate sensitivity and specificity of pulmonary hemodynamic parameters measured in echocardiography. Furthermore its correlation with the values measured in RHC was assessed.
Method
Retrospective, cross-sectional study conducted at King Fahad medical City, Riyadh, Saudi Arabia. 95 adult patients referred for right heart catheterization were enrolled in the study. All the patients had echocardiography and RHC within one week of each other.
Result
Diabetes mellitus, hypertension and dyslipidemia were present among 55%, 66% and 41% of patients respectively. 85% of the study participants were diagnosed to have pulmonary hypertension and 79% of the study participants had postcapillary pulmonary hypertension. Sensitivity of pulmonary artery systolic pressure (PAPs), mean pulmonary artery pressure (PAPm) using PAPs and pulmonary artery acceleration velocity (PAcT) were 86%, 93% and 89% respectively. Correlation of PAPs, PAPm using PAPs and PAcT on echo with invasive hemodynamic in RHC were 0.56, 0.43 and 0.24 respectively. Among patients with moderate to severe Tricuspid Regurgitation (TR) and tricuspid annular plane systolic excursion (TAPSE) <1.5cm correlation of PAPs, PAPm using PAPs and PAcT on echocardiography with right heart catheterization were 0.31, 0.24 and 0.42 respectively.
Conclusion
Echocardiographic assessment of PAPs and PAPm has high sensitivity and weak to moderate correlation with hemodynamic data in RHC. PAPs measurement on echocardiogram has best correlation with invasive measurement followed by PAPm measurement using PAPs. Among patients with moderate to severe TR and TAPSE <1.5cm PAPm measurement using PAcT has better correlation than using PAPs.
Keywords: Pulmonary hypertension, Echocardiography, Right heart catheterization
1. Introduction
Pulmonary hypertension (PH) is classified into three categories depending upon severity [1] and five categories [2] depending upon etiology. Irrespective of the etiology it is associated with poor prognosis and increase morbidity. Right heart catheterization (RHC) is the standard of care for the measurement of pulmonary pressures [2]. Invasive measurements require skill, appropriate catheter, computer module, and critical care setting or catheterization lab. These arrangements are not present even at some secondary care health facilities and in addition right heart catheterization is associated with morbidity of 1.1% and mortality of 0.05% [3]. Echocardiography (echo) is available at most places and can be used for measurement of pulmonary artery systolic, diastolic, or mean pressures utilizing various validated formulas [4]. Tricuspid regurgitation (TR) velocity and Pulmonary artery acceleration velocity (PAcT) were used in various formulas for the estimation of pulmonary artery pressures [4].
Pulmonary artery systolic pressure (PAPs) or mean pulmonary artery pressure (PAPm) in echo is usually calculated by measuring tricuspid regurgitation peak velocity and using it in various validated formulas. Pulmonary regurgitation velocity or pulmonary artery acceleration velocity measurements can also be used for calculating systolic, diastolic, or mean pulmonary artery pressures. Correlation of PAPm derived by measuring TR peak velocity in echo with measurements obtained in right heart catheterization was documented in the literature with confilting accurasies. Measurement of pulmonary pressures using echo was found to have a good correlation with the invasive measurement using RHC in some studies [5,6], however, it was inaccurate in others [7–9].
This study was conducted to compare the pulmonary artery pressures (Systolic and Mean), cardiac out (CO) and pulmonary vascular resistance (PVR) measured in right heart catheterization and echocardiography to assess the accuracy and reliability of noninvasive measurements. PAPm in echo was calculated by using two formulas. One formula used PAPs derived from peak TR and other formula utilized PAcT. Both the formulas were compared with invasive measurement in right heart catheterization for correlation.
2. Patients and methods
This cross-sectional study was conducted at King Fahad Medical City. King Fahad Medical City in Riyadh is one of the largest and leading tertiary care referral medical complexes in Saudi Arabia with a total bed capacity of 1200. It was approved by the IRB of King Fahad Medical City. All consecutive adult patients undergoing right heart catheterization for evaluation of pulmonary hypertension at King Fahad Medical City from January till December 2019 were enrolled in the study. Patients were required to give consent before the right heart catheterization. Patients had echo within one week before undergoing right heart catheterization and most of the patients had 2 days before RHC. Echocardiogram was done by expert technicians and read by two experienced echocardiologist. Right heart catheterization was done by one cardiologist experienced in performing the procedure. Patients with congenital heart disease or intubated on mechanical ventilator were excluded from the study. Demographic data, cardiovascular risk factors, invasive and noninvasive hemodynamic parameters were recorded and statistical tests were applied for significance and comparision.
Pulmonary Hypertension (PH) is define as PAPm ≥ 25 mmHg measured during RHC [2]. On echocardiography PAPs of ≥37 mmHg is suggestive of PH with or without any additional echocardiographic feature of PH or PAPs <37 if any additional feature of PH present in echocardiogram [2]. In our study PAPs of ≥37 mmHg was considered as suggestive of PH. Right atrial pressure is estimated by measuring inferior vena cava (IVC) and collapsibility with breathing. IVC size of <2.1 cm and collapsibility of >50% suggests right atrial pressure (RAP) of 3 mmHg, IVC size of >2.1 cm and collapsibility of <50% suggest RAP of 13 mmHg and 8 mmHg is suggested if IVC is > 2.1 cm with >50% collapsibility or IVC is < 2.1 cm with collapsibility of <50% [2]. PAPm was calculated by two formulas in our study. One formula used tricuspid valve regurgitation velocity [PAPm mmHg = 0.6(PAPs) + 2] [10] and other formula used pulmonary artery acceleration time (PAcT) [PAPm mmHg = 79–0.45(PAcT)] [5]. CO in RHC was measured using fick formula [CO L/min = VO2/(SaO2 - SvO2) × Hb × 13.4] [11,12] and in echo was measured using a formula incorporating flow across the Left ventricle outflow tract (LVOT) [CO L/min = Heart rate × 0.785 (diameter LVOT)2 × VTI LVOT].
All adult patients aged >18 years undergoing RHC from January 2019 till December 2019 were included in the study. Patients were excluded if they had congenital heart disease or echo was not done within 1 week of right heart catheterization.
2.1. Statistical analysis
The data were entered into a database and analyzed with the SPSS statistical software package (SPSS v25.0 Chicago, Illinois, USA). The one-sample Kolmogorov–Smirnov test was used to test for normality. A descriptive analysis was carried out in which categorical variables were expressed as absolute and relative frequencies and continuous variables as means (SD) or median with range. Pearson chi-square test was used to compare proportions in independent groups. The Spearman analysis was used to compare the correlation between two independent groups. A P-value of less than 0.05 was considered to show a statistically significant difference. Sensitivity, specificity, accuracy, and positive and negative predictive values were calculated using standard formulae. Pressures and measurments gathered during RHC were considered as gold standard and used as a reference for calculation of sensitivity and specificity of measurement obtained in echocardiography. Correlation between the variables measured in echo and RHC was carried out by using Spearman analysis. In our study Correlation coefficient ‘r’ between 0.2 and 0.39, 0.4–0.59, 0.6–0.79, and 0.8–1.0 are considered weak, moderate, strong, and very strong correlation respectively.
3. Results
There were 95 patients enrolled in the study. All had RHC and echo within a week of each other. These included 42 (44%) females and the mean age of study participants was 54.6 ± 14.9 years. Diabetes mellitus, hypertension, dyslipidemia, and coronary artery disease were present in 55%, 66%, 41% and 62% of the patients respectively. Smoking was prevalent among 46% of study participants. Left ventricular ejection fraction (LVEF) was ≥50% in 61% of patients and Pulmonary hypertension (PH) was present in 85% of study participants (Table 1).
Table 1.
Demographic and characteristics of study participants.
| Characteristics of study participants | N = 95 |
|---|---|
| Age in years (mean) | 54.6 ± 14.9 (18–87) |
| Female | 42 (44%) |
| Diabetes | 52 (55%) |
| Hypertension | 63 (66%) |
| Dyslipidemia | 36 (38%) |
| Coronary artery disease | 57 (60%) |
| Smoking | 44 (46%) |
| LVEF ≤ 40% | 30 (32%) |
| LVEF 41%–49% | 7 (7%) |
| LVEF ≥ 50% | 58 (61%) |
| Hemoglobin (g/L) | 12.18 ± 2.06 |
| Systolic Blood Pressure (mmHg) | 128.6 ± 23.8 |
Pulmonary capillary wedge pressure (PCWP) was elevated among 83% of the patients and 79% of the patients had post-capillary pulmonary hypertension (Table 2).
Table 2.
Mean values and percentages of variable among right heart catheterization (n = 95).
| Right heart catheterization parameters | Mean ± SD (min – max) |
|---|---|
| Right atrial Pressure (mmHg) | 15.5 ± 7.6 (2–37) |
| Pulmonary artery systolic pressure (mmHg) | 60.3 ± 22.2 (27–118) |
| Pulmonary artery diastolic pressure (mmHg) | 26.0 ± 10.8 |
| Mean pulmonary artery pressure (mmHg) | 40.2 ± 14.2 (18–75) |
| Pulmonary Capillary Wedge Pressure (mmHg) | 22.9 ± 10.2 (7–59) |
| Cardiac Output (L/min) | 4.1 ± 1.1 (2.0–6.7) |
| Cardiac Index | 2.27 ± 0.65 (1.15–3.90) |
| Pulmonary Vascular Resistance (WU) | 4.71 ± 3.55 (0.47–15.70) |
| Pulmonary Vascular Resistance ≥3WU (WU) | 58% |
| Pulmonary Hypertension (mPAP ≥25 mmHg) | 85% |
| Elevated Pulmonary capillary Wedge Pressure (PCWP ≥ 15) | 89% |
| Post Capillary Pulmonary Hypertension (mPAP ≥25 mmHg, PCWP ≥ 15 mmHg) | 79% |
| Trans Pulmonary Gradient ≥ 12 mmHg | 68% |
| Diastolic Pulmonary Gradient ≥ 7 mmHg | 28% |
The mean values of RHC variables are shown in Table 2 and the mean values of echo variables are given in Table 3. The mean values were comparable for PAPs (60 mmHg) measured in RHC and echo, and PAPm (40 mmHg) measured in RHC and echo using PAPs).
Table 3.
Percentage and mean values of the variable during echocardiography (n = 79).
| Echocardiographic Parameters | Mean ± SD (min – max) |
|---|---|
| Pulmonary artery systolic pressure (4TR2+RAP) (mmHg) | 59.7 ± 21.4 (20–110) |
| Mean Pulmonary artery pressure [0.6(PSAP)+2] (mmHg) | 37.6 ± 13.7 (14–71) |
| Mean Pulmonary artery pressure [79–0.45(AcT)] (mmHg) | 32.5 ± 13.5 (2.9–56.5) |
| Cardiac Output (L/min) | 3.9 ± 1.6 (1.1–7.48) |
| E/e’ ratio | 18 ± 8.6 (6–40) |
| Pulmonary Vascular Resistance [{10(TRvel/PV VTI)+0.16}/80] (WU) | 4.50 ± 2.94 (1.25–15.7) |
| Mitral Regurgitation (III/IV) | 29/61 (48%) |
| Tricuspid Regurgitation (III/IV) | 43/95 (45%) |
| TAPSE < 1.7 cm | 38/85 (45%) |
| Pulmonary Vascular Resistance ≥ 3WU | 45/71 (63%) |
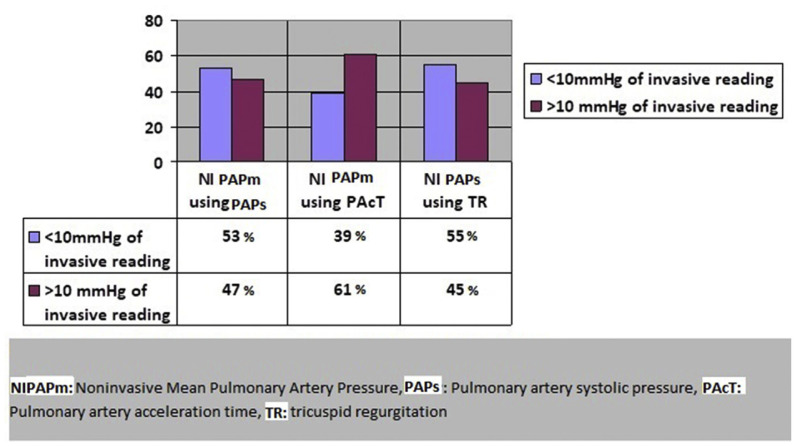
The sensitivity of noninvasive PAPm detection using formula [0.6(PAPs) +2] was 94% with a positive predictive value of 88% and a positive likelihood ratio of 1.5 Table 4. The correlation with invasive measurement of PAPm was 0.43 suggestive of a moderate degree of correlation (Fig. 2B). The correlation (r = 0.51) was better among patients with trace to mild TR and TransAnnular Plane Systolic Excursion (TAPSE) ≥ 1.5 cm compared to patients with moderate to severe TR and TAPSE < 1.5 cm (r: 0.2) (Table 5). Noninvasive PAPm measured in echo using PAPs was within 10 mmHg of the invasive PAPm measured in RHC among 53% of the patients (Fig. 1).
Table 4.
Comparison and correlation of echocardiographic parameters with parameters in right heart catheterization (N = 71).
| Parameters in Echocardiography | Comparison with parameters in right heart catheterization | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Sens | Spec | PPV | NPV | PLR | NLR | Accu | r (P-Value) | |
| Estimation of mPAP on echocardiogram using formula [0.6(PASP)+2 ] | 94% (84.9–98.3) | 38% (13.8–92.1) | 88% (83.1–92.1) | 55.5% (27.9–80.1) | 1.5 (0.9–2.3) | 0.16 (.05–0.52) | 84.6% (74.6–91.7) | 0.43 (<0.01) |
| Estimation of mPAP on echocardiogram using formula [79–0.45(PAcT)] | 89% (78.4–96.0) | 24% (8.22–47.1) | 76% (71.1–80.4) | 45.4% (22.1–70.9) | 1.17 (0.9–1.5) | 0.44 (.15–1.3) | 71.7% (60.4–81.4) | 0.29 (<0.01) |
| Estimation of PASP on echocardiogram using formula [4(TRmax) 2 + RAP] | 86% (75.6–93.5) | 42% (15.1–72.3) | 89% (83.3–92.9) | 35.7% (18.3–57.8) | 1.48 (0.9–2.4) | 0.33 (.13–0.81) | 79.4% (68.8–87.8) | 0.56 (<0.01) |
| Estimation of CO on echocardiogram using formula [Heart rate × 0.785 (dimeter LVOT) 2 × VTI LVOT] | 63% (45.9–78.1) | 48% (32–63.5) | 52% (42.8–61.4) | 58.8% (45.8–70.6) | 1.21 (0.8–1.7) | 0.77 (o.4–1.3) | 55% (43.4–66.1) | 0.19 (0.10) |
| Estimation of E/e’ on echocardiogram and correlation with PCWP | 81% (69.5–89.9) | 28% (9.6–53.4) | 80% (74.5–84.5) | 29.4% (14.4–50.6) | 1.12 (0.8–1.5) | 0.67 (0.2–1.6) | 69.5% (58.3–79.2) | 0.29 (0.01) |
| Estimation of PVR on echocardiogram using formula [{10(TRvel/PV VTI)+0.16}/80] | 75% (60.6–85.4) | 55.6% (37.3–72.4) | 73% (59.0–84.0) | 57.7% (39.0–74.5) | 1.69 (1.4–2.0) | 0.45 (0.3–0.6) | 67.6% (56.1–77.3) | 0.26 (0.02) |
Sens: Sensitivity, Spec: Specificity, PPV: Positive Predictive Value, NPV: Negative Predictive Value, PLR: Positive likelihood Ratio, NLR: Negative Likelihood Ratio, Accu: Accuracy, r: Spearman correlation coefficient, mPAP: mean Pulmonary artery pressure, PASP: Pulmonary artery systolic pressure, RAP: Right atrial pressure, TRmax: Tricuspid regurgitation maximum, LVOT: Left ventricle outflow tract, PCWP: Pulmonary capillary wedge pressure, PV: Pulmonary valve.
Fig. 2.
Correlation of echocardiographic and right heart catheterization (RHC) parameter. A: Correlation between mean pulmonary artery pressure (MPAP) in echo using PASP and RHC. B: Correlation between mean pulmonary artery pressure (MPAP) in echo using PAcT and RHC. C: Correlation between pulmonary artery systolic pressure (PASP) in echo and RHC. D: Correlation between Cardiac Output (CO) in echo and RHC. E: Correlation between pulmonary capillary wedge pressure (PCWP) in echo and Echo. F: Correlation between pulmonary vascular resistance (PVR) in echo and RHC.
Table 5.
Correlation of echocardiographic parameters with right heart catheterization parameters among patients with right sided heart failure.
| Echocardiographic variables | TR grade 3 or 4 | TR grade 3 or 4 and TAPSE<1.5 cm | TR grade 1 or 2 | TR grade 1 or 2 and TAPSE ≥1.5 cm |
|---|---|---|---|---|
| Pulmonary artery systolic pressure(PASP) (4TR2+RAP) | Correlation with PASP on right heart catheterization | |||
| 0.51 | 0.31 | 0.59 | 0.61 | |
| Mean Pulmonary artery pressure(MPAP) [0.6(PSAP)+2] | Correlation with MPAP on right heart catheterization | |||
| 0.22 | 0.24 | 0.54 | 0.54 | |
| Mean Pulmonary artery pressure(MPAP) [79–0.45(AcT)] | Correlation with MPAP on right heart catheterization | |||
| 0.34 | 0.42 | 0.25 | 0.26 | |
| Pulmonary Vascular Resistance (PVR) [{10(TRv/PV VTI)+0.16}/80] | Correlation with PVR on right heart catheterization | |||
| 0.37 | 0.35 | 0.23 | 0.17 | |
| E/e’ ratio | Correlation with PCWP on right heart catheterization | |||
| 0.29 | 0.57 | 0.32 | 0.28 | |
| Cardiac Output | Correlation with cardiac output on right heart catheterization | |||
| 0.05 | −0.36 | 0.28 | 0.24 | |
Fig. 1.
Proximity of noninvasive measurement with invasive measurement.
The sensitivity of noninvasive PAPm using formula [79–0.45(PAcT)] was 89% with a positive predictive value of 76% and a positive likelihood ratio of 1.17 Table 4. Accuracy was 72% and correlation with invasive measurement of PAPm was 0.29 suggestive of a weak correlation (Fig. 2C). Noninvasive PAPm measured in echo using PAcT was within 10 mmHg of the invasive PAPm measured in RHC among 39% of the patients (Fig. 1). There was a moderate correlation (r: 0.42) among patients with moderate to severe tricuspid regurgitation and TAPSE < 1.5 cm (Table 5).
The sensitivity of noninvasive PAPs measured using formula [4(TRmax)2+RAP] was 86% with a positive predictive value of 89% and a positive likelihood ratio of 1.48 Table 4. Accuracy was 79% and correlation with invasive measurement of PAPs was 0.56 suggestive of a moderate correlation (Fig. 2A). The correlation further improved to strong correlation (r = 0.61) among patients with trace to mild TR and TAPSE ≥ 1.5 cm (Table 5). Noninvasive PAPs measured in echo was within 10 mmHg of the invasive PAPs measured in RHC among 55% of the patients (Fig. 1).
Pulmonary hypertension was confirmed in RHC among 94% of the patients who had PAPs ≥37 mmHg in echo. However, 61% of patients with PAPs <37 mmHg in echo also had confirmed PH in RHC. Among patients with pulmonary hypertension confirmed in RHC, 88% had PAPs ≥37 mmHg in echo. 56% of patients with normal PA pressure in RHC had PAPs <37 mmHg on echo.
The sensitivity of noninvasive CO measurement using formula [Heart rate × 0.785 (dimeterLVOT)2xVTILVOT] in echowas 63% with a positive predictive value of 52% and a positive likelihood ratio of 1.21 Table 4. Accuracy was 55% and correlation with invasive measurement of CO was 0.19 suggestive of a weak correlation (Fig. 2D). Among patients with moderate to severe TR and TAPSE <1.5 cm correlation with invasive measurements of CO became worse (Table 5).
E/e’ ratio in echo of ≥10 cm/s was used as a marker of elevated PCWP. The sensitivity of noninvasive measurement of E/e’ ratio in echo for detecting PCWP ≥15 mmHg was 81% with a positive predictive value of 80% and a positive likelihood ratio of 1.12 Table 4. Accuracy was 70% and correlation with invasive measurement of PCWP was 0.28 suggestive of a weak correlation (Fig. 2F). Among patients with moderate to severe TR and TAPSE <1.5 cm correlation improved to 0.5 suggestive of a moderate correlation (Table 5).
Echocardiographic measurement of PVR was weakly correlated (r = 0.26) with the measurement of PVR in RHC (Fig. 2E). Among patients with moderate to severe TR and TAPSE <1.5 cm correlation of measurement in echo with invasive measurement of PVR remained poor (Table 5).
4. Discussion
Echocardiography plays an important role in assessing the probability of pulmonary hypertension and recommendations for further workup. Tricuspid regugitaion velocity >2.8 and other associated features such as right ventricle dilatation, flattening of interventricular septum, dilatation of pulmonary artery, presence of pulmonary regurgitation, increase pulmonary acceleration velocity, and dilatated and non-collapsing inferior venacava suggest intermediate or high probability of PH [2]. Most of the patients enrolled in our study had high or intermediate probability of pulmonary hypertension. In our study echo measurements of PAPm using formulas incorporating PAPs or PAcT were sensitive with high positive predictive value (sensitivity 89–94% and PPV 76–88%). Higher sensitivity in our study is in line with the previous study [6] and suggests that echo is better at identifying PH among patients with PH. Good correlation was found between echo and RHC parameters of PAPm and PAPs in a study conducted earlier along with excellent sensitivity and specificity [6], similarly, in our study 53% of the patients had PAPm measured in echo using formula incorporating PAPs was within 10 mmHg of PAPm measured in RHC and mean of both values were also comparable. Conversely, lower specificity in our study suggests that echo is not good at identifying individuals without PH. The absence of PH on echocardiogram doesn’t rule out PH and if clinically suggested then RHC should be requested. According to a recent meta-analysis, pooled sensitivity and specificity of echo for diagnosis of PH was 85% and 74% respectively [12]. Echo can’t replace RHC which is considered as a gold standard [12]. Reveal registry concluded that echo had a reasonable correlation with RHC at one time but lack correlation in precise measurement of serial changes in pulmonary hemodynamics [13]. In our study echo had little impact on the pretest probability of PH. Our finding was in agreement with another study suggesting an insufficient role of echo to rule out PH among patients with high pretest probability [9].
Estimation of PAcT can be difficult and subject to error depending upon sampling site, RV function, poor doppler signals, and heart rate. Among both the formulas used for measurement of PAPm in our study, formula incorporating PAPs had a better negative likelihood ratio (0.16 vs. 0.44), accuracy (85% vs.72%), and correlation with invasive measurement (0.42 vs. 0.29) than formula utilizing PAcT. Another study had also validated the formula incorporating PAPs for calculating PAPm in echo [5] and our study also suggested higher sensitivity and accuracy for PAPm measurement using PAPs. In our study among patients with moderate to severe tricuspid regurgitation and TAPSE <1.5 cm, PAPm measurement utilizing PAcT had a better correlation with invasive measurement and may be the preferred method among such patients.
PAPs estimation by echo was sensitive with high positive predictive value. Maximum tricuspid valve regurgitation velocity is usually feasible for measurement and need to be assess in multiple views for optimum value.
In our study, 88% of patients with PH (mean PAP ≥ 25 mmHg in RHC) had PAPs ≥37 mmHg on echo (True Positive) and 44% of patients with normal PAP (mean PAP < 25 mmHg in RHC) had PASP ≥ 37 mmHg on echo (false positive). The findings in our study reiterate the finding of earlier studies suggesting that absence or presence of pulmonary arterial systolic hypertension on echocardiogram doesn’t rule out or rule in PH conclusively and require invasive studies for further evaluation among clinically indicated patients [9,14].
The modest correlation was found between invasive and echocardiographic assessment of PAPs among the different subset of patients using higher PAPs cutoff in echo [15,9]. In our study sensitivity and specificity were 86% and 48% for the diagnosis of PH at PAPs cutoff of 37 mmHg in echo and could have been different if higher PASP cutoff was used. In our study among all the echo variables studied, PAPs measurement using tricuspid valve regurgitation has the best correlation and accuracy, 55% of patients had differences between invasive and echo reading of PAPs within 10 mmHg and mean values measured by both modalities were also comparable. Similarly to our study good sensitivity, specificity, and correlation of PAPs measurement by echo was noted in earlier studies [16,17], and in Reveal registry 43% of the patients had a difference of less than 10 mmHg in PAPs measured by echo and RHC [13].
In our study echo estimation of CO had the least sensitivity, specificity, and correlation. Positive and negative likelihood ratios were also close to 1 suggesting that it did not add much to the pretest probability. Multiple factors were responsible for low accuracy of noninvasive measurement of cardiac output. Measurement of LVOT is critical because a minimal error will be duplicated and lead to a huge difference [7]. Sampling of LVOT and calculating Velocity time integral can also induce errors. Our finding is similar to a previous study stating inaccuracy in measuring cardiac output using echocardiographic parameters [7].
Estimation of LVEDP (Left ventricle end diastolic pressure) is critical in the management of patients with heart failure and pulmonary hypertension. PCWP measurement in RHC is a reliable estimation of LVEDP and can be measured by placing a wedge catheter in the pulmonary artery. Noninvasive measurement of E/e’ ratio by echo was found helpful for estimating LVEDP. E/e’ ratio of <8 and >15 in echo is suggestive of normal and abnormal LVEDP respectively [18,19]. Among patients with advanced systolic heart failure, E/e’ showed poor correlation with LVEDP especially in presence of resynchronization therapy [20]. Cardiac resynchronization therapy has effect on RV function and it was proposed to check baseline RV function with stress test during preimplant evaluation, however cadidates shouldn’t be denied of CRT based on RV function [21]. E/e’ ratio was recommended to be supplemented by other echo parameters for proper estimation of LVEDP [22]. Quantitative PCWP in echo was measured using multiple variables in a validated formula and showed good correlation, sensitivity, and specificity when compared with PCWP measurement in RHC[23]. In our study, E/e’ of ≥10 cm/s in echo was 81% sensitive with PPV of 80% for the detection of PCWP ≥15mmHg in RHC. E/e’ in echo had a better correlation with invasive PCWP measurement among patients with moderate to severe TR and TAPSE <1.5 cm. E/e’ > 10 cm/s measured in echo demonstrated good accuracy for detection of PCWP >15 mmHg in RHC. However it lacked quantitative correlation with PCWP in RHC because E/e’ is a echo variable which provides information regarding left ventricle diastolic function, left ventricle end diastolic pressure, and PCWP instead of measuring the PCWP itself. A study which measured PCWP using echo variables showed good quantitative correlation with PCWP measured in RHC [23].
Right heart disease is associated with a poor correlation of PAPs measurement between echo and RHC. Conversely, left heart pathology was associated with higher correlation and less differences between echo and catheterization measurements [24]. In our study, 45% of the study participants had evidence of right-sided dysfunction evident by reduced TAPSE and moderate to severe TR. Right ventriculoarterial coupling derived through variables measured in both RHC and echo showed good correlation with right ventricular function [25]. A reduced TAPSE was positively associated with impaired right ventriculoarterial coupling [25]. Correlation between echocardiographic and invasive measurement of PAPm using TR velocity and estimation of CO became poor among patients with moderate to severe tricuspid regurgitation and TAPSE <1.5 cm. Echo measurement of PAPm using PAcT had a better correlation with invasive measurement among patients with moderate to severe TR and TAPSE <1.5 cm and may be a preferred method among such patients. The presence of a significant number of patients with right-sided dysfunction in our study can explain the weak correlation found between echo and right heart catheterization assessment of pulmonary hypertension.
4.1. Strength and limitation
Echo and RHC were done within 1 week. Echo was performed before the RHC. 36, 33, 11, 8 and 6 patients had echo 1, 2, 4, 5, and 6 days before RHC respectively. Majority of the patients had echo within 2 days of RHC and it is unlikely that clinical condition would have changed drastically within 2 days to have a significant impact on the result. However, for our future studies will try to conduct echo on the same day as of RHC to minimize the chances of variation.
Chances of error in calculation of variables in echo such as cardiac output, PAPm is high due to complex formulas, difficult windows and poor Doppler signals. We minimized these errors by using contrast when required, capturing multiple views such as parasternal, long axis and nonstandard views according to the need, and competent, well-trained staff performing and reading the echoes.
We minimized the chances of error in measurement obtained in RHC by calculating during end expiration and keeping zero reference line at the level of mid thoracic line for best estimation of PCWP.
5. Conclusion
Echo parameters had high sensitivity for detecting pulmonary hypertension and estimating left ventricular end-diastolic pressure. Among all the echocardiographic variables measured in our study estimation of pulmonary artery systolic pressure has the highest correlation with right heart catheterization measurement. Estimation of mean pulmonary pressure in echo using tricuspid valve regurgitation has a better correlation with invasive measurements than using pulmonary artery acceleration time except among patients with moderate to severe tricuspid regurgitation and TAPSE <1.5 cm. Noninvasive assessment of cardiac output using echo variables had the least sensitivity. Invasive assessment of pulmonary hypertension is required among patients with possible or definite pulmonary hypertension on echocardiogram for further evaluation and stratification.
Acknowledgement
I acknowledge the support of “Zainab Jaffery” and “Ashwaq Alhumrani” in coordinating with research and ethical board of our hospital.
Abbreviations and acronyms
- Echo
Echocardiography
- RHC
Right heart catheterization
- TR
Tricuspid Regurgitation
- PAcT
Pulmonary artery acceleration time
- PAPs
Pulmonary artery systolic pressure
- PAPm
Mean pulmonary artery pressure
- RAP
Right atrial pressure
- CO
Cardiac Output
- PVR
Pulmonary vascular resistance
- PH
Pulmonary hypertension
- IVC
Inferior VenaCava
- LVOT
Left Ventricle outflow tract
- PCWP
Pulmonary capillary wedge pressure
- TAPSE
Trans Annular Plane Systolic Excursion
- LVEDP
Left ventricle end diastolic pressure
Footnotes
Author contribution
Conception and design of Study, Research coordination and management: Muhammad Adil Soofi, Muhammad Azam Shah. Literature review, Drafting of manuscript, Revising and editing the manuscript critically for important intellectual contents: Muhammad Adil Soofi, Muhammad Azam Shah, Ammar Mohammed AlQadhi, Abdulla Mofareh AlAnazi, Waleed M Alshehri, Amir Umair. Acquisition of data, Data preparation and presentation: Muhammad Adil Soofi, Amir Umair. Analysis and interpretation of data, Research investigation and analysis: Muhammad Adil Soofi, Muhammad Azam Shah, Amir Umair. Data collection: Ammar Mohammed AlQadhi, Abdulla Mofareh AlAnazi, Waleed M Alshehri. Supervision of the research: Muhammad Adil Soofi.
Funding
This research was funded by research department of King Fahad Medical City and grant number was 018–065. Funding has no impact on analysis and interpretation of data or on any aspect of manuscript.
Conflicts of interest
There were no financial, personal or professional interests that could have influced the manuscript.
References
- 1. Rodríguez-Roisin R, Krowka MJ, Hervé P, Fallon MB. ERS task force pulmonary-hepatic vascular disorders (PHD) scientific committee pulmonary-hepatic vascular disorders (PHD) Eur Respir J. 2004;24:861–80. doi: 10.1183/09031936.04.00010904. [DOI] [PubMed] [Google Scholar]
- 2. Galiè N, Humbert M, Vachieryc JL, Gibbs S, Lang I, Torbicki A, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. 2016;37:67–119. doi: 10.1093/eurheartj/ehv317. [DOI] [PubMed] [Google Scholar]
- 3. Hoeper MM, Lee SH, Voswinckel R, Palazzini M, Jais X, Marinelli A, et al. Complications of right heart catheterization procedures in patients with pulmonary hypertension in experienced centers. J Am Coll Cardiol. 2006;48:2546–52. doi: 10.1016/j.jacc.2006.07.061. . Epub 2006 Nov 28. [DOI] [PubMed] [Google Scholar]
- 4. Sathish P, Seamus W, Brodie LL, Nicholas DG, Andrew MW, Crystal L, et al. Assessment of pulmonary artery pressure by echocardiography—a comprehensive review. Int J Cardiol Heart Vasc. 2016;12:45–51. doi: 10.1016/j.ijcha.2016.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Steckelberg RC, Tseng AS, Nishimura R, Ommen S, Sorajja P. Derivation of mean pulmonary artery pressure from noninvasive parameters. J Am Soc Echocardiogr. 2013;26(5):464–8. doi: 10.1016/j.echo.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 6. Sohrabi B, Kazemi B, Mehryar A, Teimouri-Dereshki A, Toufan M, Aslanabadi N. Correlation between pulmonary artery pressure measured by echocardiography and right heart catheterization in patients with rheumatic mitral valve stenosis (A prospective study) Echocardiography. 2016;33(1):7–13. doi: 10.1111/echo.13000. [DOI] [PubMed] [Google Scholar]
- 7. Fisher MR, Forfia PR, Chamera E, Housten-Harris T, Champion HC, Girgis RE, et al. Accuracy of Doppler Echocardiography in the hemodynamic assessment of pulmonary hypertension. Am J Respir Crit Care Med. 2009;179(7):615–21. doi: 10.1164/rccm.200811-1691OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Colle IO, Moreau R, Godinho E, Belghiti J, Ettori F, Chohensolal A, et al. Diagnosis of portopulmonary hypertensionin candidates for liver transplantation: a prospective study. Hepatology. 2003;37(2):401–9. doi: 10.1053/jhep.2003.50060. [DOI] [PubMed] [Google Scholar]
- 9. Mukerjee D, St George D, Knight C, Davar J, Wells AU, Du Bois RM, et al. Echocardiography and pulmonary function as screening tests for pulmonary arterial hypertension in systemic sclerosis. Rheumatology. 2004;43(4):461–6. doi: 10.1093/rheumatology/keh067. [DOI] [PubMed] [Google Scholar]
- 10. Chemla D, Castelain V, Humbert M, Hébert JL, Simonneau G, Lecarpentier Y, et al. New formula for predicting mean pulmonary artery pressure using systolic pulmonary artery pressure. Chest. 2004;126:1313–7. doi: 10.1378/chest.126.4.1313. [DOI] [PubMed] [Google Scholar]
- 11. Lafarge CG, Miettinen OS. The estimation of oxygen consumption. Cardiovasc Res. 1970;4(1):23–30. doi: 10.1093/cvr/4.1.23. [DOI] [PubMed] [Google Scholar]
- 12. Jin-Rong N, Pei-Jing Y, Shi-Dong L, Yuan H, Ke-Hu Y, Bing S, et al. Diagnostic accuracy of transthoracic echocardiography for pulmonary hypertension: a systematic review and meta-analysis. BMJ Open. 2019;9(12):e033084. doi: 10.1136/bmjopen-2019-033084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Farber HW, Foreman AJ, Miller DP, McGoon MD. REVEAL Registry: correlation of right heart catheterization and echocardiography in patients with pulmonary arterial hypertension. Congest Heart Fail. 2011;17:56–63. doi: 10.1111/j.1751-7133.2010.00202.x. [DOI] [PubMed] [Google Scholar]
- 14. Arcasoy SM, Christie JD, Ferrari VA, Sutton MS, Zisman DA, Blumenthal NP, et al. Echocardiographic assessment of pulmonary hypertension in patients with advanced lung disease. Am J Respir Crit Care Med. 2003;167(5):735–40. doi: 10.1164/rccm.200210-1130OC. [DOI] [PubMed] [Google Scholar]
- 15. Habash F, Gurram P, Almomani A, Duarte A, Hakeem A, Vallurupalli S, et al. Correlation between echocardiographic pulmonary artery pressure estimates and right heart catheterization measurement in liver transplant candidates. J Cardiovasc Imaging. 2018;26(2):75–84. doi: 10.4250/jcvi.2018.26.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wang B, Feng Y, Jia LQ, Wu XL, Li DD, Zhou HX, et al. Accuracy of Doppler Echocardiography in the assessment of pulmonary arterial hypertension in patients with congenital heart disease. Eur Rev Med Pharmacol Sci. 2013;17(7):923–8. doi: 10.3389/fped.2019.00421. [DOI] [PubMed] [Google Scholar]
- 17. Lanzarini L, Fontana A, Lucca E, Campana C, Klersy C. Noninvasive estimation of both systolic and diastolic pulmonary artery pressure from Doppler analysis of tricuspid regurgitant velocity spectrum in patients with chronic heart failure. Am Heart J. 2002;144(6):1087–94. doi: 10.1067/mhj.2002.126350. [DOI] [PubMed] [Google Scholar]
- 18. Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Red-field MM, et al. Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: a comparative simultaneous Doppler-catheterization study. Circulation. 2000;102:1788–94. doi: 10.1161/01.cir.102.15.1788. [DOI] [PubMed] [Google Scholar]
- 19. Nagueh SF, Mikati I, Kopelen HA, Middleton KJ, Quiñones MA, Zoghbi WA. Doppler estimation of left ventricular filling pressure in sinus tachycardia. A new application of tissue Doppler imaging. Circulation. 1998;98:1644–50. doi: 10.1161/01.cir.98.16.1644. [DOI] [PubMed] [Google Scholar]
- 20. Mullens W, Borowski AG, Curtin RJ, Thomas JD, Tang WH. Tissue Doppler imaging in the estimation of intracardiac filling pressure in decompensated patients with advanced systolic heart failure. Circulation. 2009;119:62–70. doi: 10.1161/CIRCULATIONAHA.108.779223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ricci F, Mele D, Bianco F, Bucciarelli V, De Caterina R, Gallina S. Right heart-pulmonary circulation unit and cardiac resynchronization therapy. Am Heart J. 2017;185:1–16. doi: 10.1016/j.ahj.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 22. Park JH, Marwick TH. Use and limitations of E/e’ to Assess Left Ventricular Filling Pressure by Echocardiography. J Cardiovasc Ultrasound. 2011;19(4):169–73. doi: 10.4250/jcu.2011.19.4.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chubuchny V, Pugliese NR, Taddei C, Poggianti E, Spini V, Barison A, et al. A novel echocardiographic method for estimation of pulmonary artery wedge pressure and pulmonary-vascular resistance. ESC Heart Failure. 2021;8:1216–29. doi: 10.1002/ehf2.13183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Finkelhor RS, Lewis SA, Pillai D. Limitations and strengths of Doppler/echo pulmonary artery systolic pressure-right heart catheterization correlations: a systematic literature review. Echocardiography. 2015;32(1):10–8. doi: 10.1111/echo.12594. [DOI] [PubMed] [Google Scholar]
- 25. Bianco F, Bucciarelli V, Ammirati E, Occhi L, Musca F, Tonti G, et al. Assessment of right ventricular function in advanced heart failure with nonischemic dilated cardiomyopathy: insights of right ventricular elastance. J Cardiovasc Med. 2020;21(2):134–43. doi: 10.2459/JCM.0000000000000921. [DOI] [PubMed] [Google Scholar]