Abstract
Background
Air pollution has been related to incidence of type 2 diabetes (T2D). We assessed the joint association of various air pollutants with the risk of T2D and examined potential modification by obesity status and genetic susceptibility on the relationship.
Methods and findings
A total of 449,006 participants from UK Biobank free of T2D at baseline were included. Of all the study population, 90.9% were white and 45.7% were male. The participants had a mean age of 56.6 (SD 8.1) years old and a mean body mass index (BMI) of 27.4 (SD 4.8) kg/m2. Ambient air pollutants, including particulate matter (PM) with diameters ≤2.5 μm (PM2.5), between 2.5 μm and 10 μm (PM2.5–10), nitrogen dioxide (NO2), and nitric oxide (NO) were measured. An air pollution score was created to assess the joint exposure to the 4 air pollutants. During a median of 11 years follow-up, we documented 18,239 incident T2D cases. The air pollution score was significantly associated with a higher risk of T2D. Compared to the lowest quintile of air pollution score, the hazard ratio (HR) (95% confidence interval [CI]) for T2D was 1.05 (0.99 to 1.10, p = 0.11), 1.06 (1.00 to 1.11, p = 0.051), 1.09 (1.03 to 1.15, p = 0.002), and 1.12 (1.06 to 1.19, p < 0.001) for the second to fifth quintile, respectively, after adjustment for sociodemographic characteristics, lifestyle factors, genetic factors, and other covariates. In addition, we found a significant interaction between the air pollution score and obesity status on the risk of T2D (p-interaction < 0.001). The observed association was more pronounced among overweight and obese participants than in the normal-weight people. Genetic risk score (GRS) for T2D or obesity did not modify the relationship between air pollution and risk of T2D. Key study limitations include unavailable data on other potential T2D-related air pollutants and single-time measurement on air pollutants.
Conclusions
We found that various air pollutants PM2.5, PM2.5–10, NO2, and NO, individually or jointly, were associated with an increased risk of T2D in the population. The stratified analyses indicate that such associations were more strongly associated with T2D risk among those with higher adiposity.
Xiang Li and co-workers study the potential influence of obesity on associations between air pollutants and incidence of type 2 diabetes.
Author summary
Why was this study done?
Recent evidence has linked ambient air pollution with type 2 diabetes (T2D). However, most of them were mainly focused on 1 or 2 air pollutants separately. In addition, it has been reported that the association between air pollution and T2D was augmented among people with increased adiposity.
Individuals are usually exposed to various air pollutants simultaneously; and the importance of assessing multi-air pollutant exposures as a whole has been increasingly recognized.
Thus, in this study, we aimed to analyze the association between the air pollution score that incorporates various air pollutants with the risk of T2D. We also particularly examined the potential modification by obesity.
What did the researchers do and find?
We built an air pollution score, incorporating PM2.5, PM2.5–10, nitrogen dioxide (NO2), and nitric oxide (NO), and analyzed its association with the risk of T2D among 449,006 participants from UK Biobank. Air pollutants were measured in 2010. During a median follow-up time of 11 years, 18,239 T2D cases were documented.
We found that long-term exposure to various air pollutants, individually or jointly, was associated with an increased risk of T2D. Moreover, such association was more pronounced among people with increased adiposity.
What do these findings mean?
Our findings highlight the importance of comprehensively assessing various air pollutants as a whole in the prevention of T2D.
Given the adverse impact of air pollution on T2D, attention should be paid to reducing and mitigating air pollution.
Our results also emphasize the merit of obesity management.
Introduction
Type 2 diabetes (T2D) is a persistent public threat worldwide. The prevalence of T2D has been increasing, and it is set to rise even further. From the most recent International Diabetes Federation (IDF), it is estimated that there will be more than 700 million adults living with diabetes worldwide by 2045 [1]. While several traditional risk factors, such as poor diet [2,3], low physical activity [4,5], and poor sleep behaviors have been related to T2D [6,7], recent evidence suggests that ambient air pollution may also contribute to the development of the disease [8–10]. However, the relations between air pollution and T2D is a relatively new field, and the previous findings between air pollution and T2D were inconsistent [11,12]. Notably, the prior studies are largely limited by cross-sectional design [13–15], and small sample size [16], while data from large-scale, cohort settings are still scarce. In addition, individuals are usually exposed to a combination of various air pollutants simultaneously, and the importance of assessing multi-air pollutant exposures as a whole has been increasingly recognized [17–19]. However, most previous studies were mainly focused on 1 or 2 air pollutants separately, without considering the joint exposure to various air pollutants [15,20–23]. Recently, we have created and validated a novel air pollution score incorporating various air pollutants, which has been shown to be associated with heart failure [24]. To date, no study has jointly investigated long-term exposure to various air pollutants with the risk of T2D in a cohort study design.
Of note, emerging evidence has also linked air pollutants such as PM2.5, nitrogen dioxide (NO2), and O3 with increased adiposity [25,26], and it was reported that the association between air pollutants and T2D was augmented in obese participants [27]. Therefore, we hypothesized that obesity status might modify the relationship between air pollution and the risk of T2D. In addition, prior evidence suggests that the genetic factors may modify the environment–disease relation, while investigations on the modification effect by the genetic predisposition on the relation between air pollution and T2D risk are scarce [28].
In the present study, we aimed to analyze the associations of various air pollutants and the air pollution score, which comprehensively incorporated PM2.5, PM2.5–10, NO2, and nitric oxide (NO), with the risk of T2D among 449,006 participants from UK Biobank. We particularly examined the potential modification by obesity status (both general and central obesity) and genetic predisposition to obesity or T2D.
Method
Protocol
This research has been conducted using the UK Biobank Resource under Application Number 29256. Our study did not employ a prospective protocol. Analyses were first planned and performed in January 2021. During the peer review, we added a table of Pearson correlations between each of the air pollutant and a map of air pollution levels exposed to study participants at baseline (2010). Minor changes to the manuscript were also made at the request of peer reviewers.
Study population
The UK Biobank is a prospective cohort based in the United Kingdom aimed to improve the prevention, diagnosis, and treatment of a wide range of illnesses. Briefly, over 500,000 middle-aged participants were recruited across 2006 to 2010. Participants provided a wide range of health-related information through touchscreen questionnaires, physical measurements, and biological samples at baseline or follow-up assessment. Details of the study design have been described elsewhere previously [29]. The study was approved by both the National Health Service National Research Ethics Service (Ref: 11/NW/0382) and the Institutional Review Board of Tulane University (2018–1872). All the participants provided written informed consent.
In the current analysis, we excluded participants with T2D (N = 12,185) and those with missing information on residential air pollution (N = 41,302) at baseline, leaving a total of 449,006 participants for the primary analysis. In the joint association of genetic risk and air pollution analysis, to avoid heterogeneity, we only included participants of European descent with complete genotyping data (N = 417,035).
Assessment of air pollution and air pollution score
The annual average air pollution, including PM2.5, PM2.5–10, NO2, and NOx, in 2010, were modeled for each address using a Land Use Regression (LUR) model developed as part of the European Study of Cohorts for Air Pollution Effects (ESCAPE, http://www.escapeproject.eu/) [30,31] and linked to participants’ residential addresses given at baseline visit. The LUR models calculated the spatial variations of annual average air pollutant concentration at participants’ home addresses using Geographic Information System (GIS)-derived predictors, such as traffic, land use, and topography. The LUR model is based on ESCAPE monitoring done between January 2010 and January 2011, and air pollution estimates are representative for the year 2010. The ESCAPE estimates for particulates are valid up to 400 km from the monitoring area [30,31]. The concentration of NO is estimated by subtracting NO2 from NOx following the previous study [32].
To capture the joint exposure to various air pollutants, we created an air pollution score by summing up concentrations of 4 ambient air pollutants (PM2.5, PM2.5–10, NO2, and estimated NO), weighted by the multivariable-adjusted risk estimates (β coefficients) on T2D in the present analysis [24]. The β coefficient was from the final model with individual air pollutant as the independent variable, one at a time. The equation was: air pollution score = (βPM2.5 × PM2.5 + βPM2.5–10 × PM2.5–10 + βNO2 × NO2 + βNO × NO) × (4 / sum of the β coefficients). The air pollution score ranges from 31.7 to 140.3, a higher score indicating greater exposure to ambient air pollution. Since PM2.5–10 was not significantly associated with T2D, we also created a weighted air pollution score without PM2.5–10.
Assessment of outcomes
Information on incident T2D was collected through February 8, 2020. Incident T2D was defined by ICD-10 code E11, ascertained by hospital inpatient records containing data on admissions and diagnoses from the Hospital Episode Statistics for England, Scottish Morbidity Record data for Scotland, and the Patients Episode Database for Wales.
Genotype data
Genotyping, imputation, and quality control of the genetic data were performed by the UK Biobank team. The detailed information is available elsewhere (http://www.ukbiobank.ac.uk/scientists-3/genetic-data/) [33]. A genetic risk score (GRS) for T2D was created using 112 independent single nucleotide polymorphisms (SNPs), which passed quality control out of the 128 SNPs recently identified to be associated with T2D at genome-wide significance [34,35]. Information of the 112 independent SNPs is provided in S1 Table. The GRS for T2D was calculated by the weighted method: GRS = (β1 × SNP1 + β2 × SNP2 + … + β112 × SNP112) × (112 / sum of the β coefficients). Each SNP was recoded as 0, 1, and 2 according to the number of risk alleles. The β coefficient was obtained from the reported GWAS meta-analysis [35]. The GRS for T2D in the current analysis ranges from 81.0 to 136.9; a higher score indicates a higher genetic predisposition to T2D. The BMI-GRS was created in the same way as T2D-GRS, using the 97 identified body mass index (BMI)-related SNPs [36]. Information of the BMI-related SNPs is summarized in S2 Table. We determined whether participants were at low, intermediate, or high genetic risk according to the tertile categories of the GRS.
Assessment of other covariates
Age, sex, ethnicity, and Townsend deprivation index (based on the participant’s postcode, higher scores indicate a higher degree of deprivation) were obtained at baseline. Weight, height, and waist circumference (WC) were measured at baseline during the initial assessment center visit. BMI was calculated as weight divided by height squared (kg/m2) during the initial Assessment Centre visit. Overall obesity status was defined as follows: normal weight: 18.5 to less than 25 kg/m2; overweight: 25 to less than 30 kg/m2; obese: 30 kg/m2 and above. Central obesity was defined using the European cutoff points for WC: ≥94 cm for men and ≥80 cm for women. Physical activity was assessed by the International Physical Activity Questionnaire (IPAQ) and metabolic equivalent task (MET) score was calculated using the IPAQ guideline [37,38]. Alcohol intake was assessed by the Touchscreen questionnaire. A healthy diet score was adapted from the American Heart Association Guidelines and defined as adherence to 4 or 5 components of the following: (1) total fruit intake ≥4.5 pieces/week; (2) total vegetable intake ≥4.5 servings/week (3 tablespoons of vegetable considered as 1 serving); (3) total fish intake ≥2 servings/week; (4) processed meat intake less than twice/week; and (5) red meat intake ≤5 times/week [39].
Statistical analysis
Follow-up time was calculated from the recruitment date to the first diagnosis of T2D, lost to follow-up, death, or end of the current follow-up, whichever came first. Cox proportional hazard models were used to estimate the hazard ratios (HRs) and 95% confidence intervals (CIs) for incident T2D associated with the individual air pollutant or the air pollution score. The proportional hazards assumption was tested by creating a time-dependent variable, and no violation was found. Cox regression models were adjusted for age, sex, and ethnicity in model 1. Model 2 was further adjusted for Townsend deprivation index, assessment center, alcohol intake, smoking status, physical activity, sedentary hours, and healthy diet score. In model 3, we additionally adjusted for BMI, systolic blood pressure, antihypertension medication use, high cholesterol, and T2D-GRS. We examined the dose–response relationship between the air pollution score and incident T2D using the restricted cubic spline analysis. We particularly tested whether the association between the air pollution score and risk of T2D was modified by obesity status (overall obesity and central obesity) or genetic predisposition to T2D or obesity, by including an interaction term between the air pollution score and the continuous BMI or WC. To disentangle the temporal concerns regarding the relationship between air pollution and T2D, we further conducted a sensitivity analysis by excluding T2D cases that occurred in the first 2 years of follow-up. In addition, we performed the analyses among participants who have been living in the current address for at least 5 years to assess the long-term effect of air pollution on T2D.
Statistical analyses were performed with SAS version 9.4 (SAS Institute, Cary, NC). All p-values were two-sided, and p < 0.05 was considered statistically significant.
The study was reported as per the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (S1 STROBE checklist).
Results
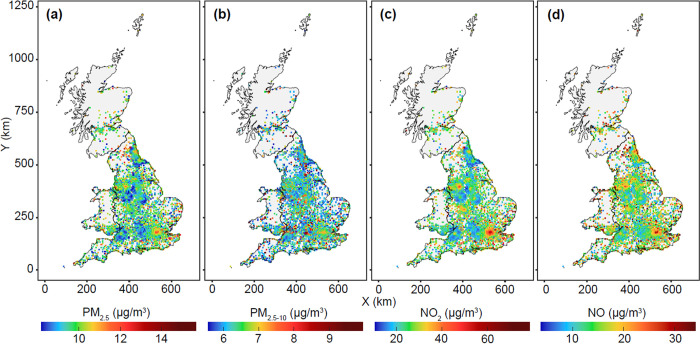
Among the 449,006 participants, a total of 18,239 incident cases of T2D were recorded during a median follow-up time of 11 years. Baseline characteristics of the study participants according to the quintiles of the air pollution score are presented in Table 1. Participants with higher exposure to ambient air pollution were younger, with a greater Townsend deprivation index (indicating a greater degree of deprivation), more likely to be current smokers, and less likely to be physically active. The Pearson correlation coefficients among the individual air pollutants were shown in S3 Table. Air pollution levels in areas where participants lived in 2010 were shown in Fig 1. The distribution patterns of air pollution levels in the current study are comparable to the spatial distribution of air pollutants from the public UK Air Information Resources (https://uk-air.defra.gov.uk/data/pcm-data). The administrative boundary data of UK is sourced from UK Government Open Data portal (https://data.gov.uk/dataset/3fd8d2d2-b591-42ff-b333-c53a6a513e96/countries-december-2017-full-clipped-boundaries-in-great-britain). These data are UK government–released open data.
Table 1. Baseline characteristics of the UK Biobank participants according to the quintiles of air pollution score (N = 449,006).
| Air Pollution Score | |||||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | |
| Age, year | 57.2 (7.8) | 56.9 (8.0) | 56.7 (8.1) | 56.1 (8.2) | 55.4 (8.3) |
| White | 85,814 (95.2) | 83,849 (93.6) | 82,394 (92.2) | 79,749 (89.7) | 74,540 (84.1) |
| Male | 40,524 (45.1) | 40,443 (45.0) | 40,483 (45.1) | 40,514 (45.1) | 41,078 (45.7) |
| PM2.5, μg/m3 | 8.7 (0.4) | 9.5 (0.3) | 9.9 (0.3) | 10.4 (0.4) | 11.5 (0.9) |
| PM2.5–10, μg/m3 | 6.2 (0.8) | 6.2 (0.8) | 6.3 (0.8) | 6.5 (0.9) | 6.9 (1.0) |
| NO2, μg/m3 | 17.3 (2.8) | 22.8 (2.7) | 26.3 (2.8) | 29.8 (2.9) | 37.0 (6.4) |
| NO, μg/m3 | 9.4 (2.8) | 13.4 (3.6) | 16.0 (3.7) | 18.9 (3.9) | 29.1 (11.9) |
| BMI, kg/m2 | 27.0 (4.4) | 27.3 (4.6) | 27.4 (4.7) | 27.5 (4.8) | 27.5 (5.0) |
| WC, cm | 89.2 (13.0) | 89.9 (13.1) | 90.3 (13.3) | 90.5 (13.4) | 90.4 (13.6) |
| Systolic blood pressure, mm Hg | 138.8 (18.5) | 138.2 (18.5) | 138.1 (18.4) | 137.4 (18.4) | 136.2 (18.3) |
| Townsend deprivation index | −3.2 [−4.2–−2.1] | −2.9 [−4.1–−1.3] | −2.4 [−3.7–−0.30] | −1.4 [−3.0–1.0] | 0.9 [−1.6–3.6] |
| Total MET | 2,466.0 [1,048.5–3,155.0] | 2,435 [996.0–2,979.0] | 2,493.0 [1,010.0–2,946.0] | 2,559.0 [1,022.0–2,932.0] | 2,506.5 [1,032.0–2,882.5] |
| Healthy diet score | 2.1 (0.9) | 2.1 (0.9) | 2.1 (0.9) | 2.1 (0.9) | 2.1 (0.9) |
| Sedentary time | 4.0 [3.0–6.0] | 4.0 [3.0–6.0] | 4.0 [3.0–6.0] | 4.0 [3.0–6.0] | 4.0 [3.0–6.0] |
| Smoking status | |||||
| Never | 52,165 (58.3) | 50,860 (56.9) | 49,428 (55.4) | 48,503 (54.4) | 44,740 (50.2) |
| Previous | 30,835 (34.5) | 30,926 (34.6) | 30,944 (34.7) | 30,458 (34.1) | 31,140 (35.0) |
| Current | 6,501 (7.3) | 7,597 (8.5) | 8,902 (10.0) | 10,251 (11.5) | 13,200 (14.8) |
| Alcohol intake | |||||
| Daily or almost daily | 22,284 (24.8) | 18,132 (20.2) | 17,114 (19.1) | 16,624 (18.6) | 18,330 (20.5) |
| 3–4 times/week | 23,211 (25.9) | 21,628 (24.1) | 20,492 (22.9) | 19,924 (22.3) | 18,832 (21.1) |
| 1–2 times/week | 22,442 (25.0) | 23,985 (26.8) | 24,009 (26.8) | 23,404 (26.2) | 21,626 (24.2) |
| 1–3 times/month | 8,929 (10.0) | 10,198 (11.4) | 10,379 (11.6) | 10,413 (11.6) | 9,728 (10.9) |
| Special occasions only | 7,932 (8.8) | 9,650 (10.8) | 10,612 (11.9) | 11,280 (12.6) | 11,520 (12.9) |
| Never | 4,905 (5.5) | 6,035 (6.7) | 6,967 (7.8) | 7,867 (8.8) | 9,268 (10.4) |
| Hypertension, yes | 47,228 (52.6) | 47,418 (52.8) | 47,391 (52.8) | 45,971 (51.2) | 43,542 (48.5) |
| Antihypertension meds, yes | 16,572 (18.5) | 17,633 (19.8) | 18,015 (20.2) | 17,939 (20.2) | 17,245 (19.4) |
| Cholesterol lowering meds, yes | 12,826 (14.4) | 13,935 (15.6) | 14,648 (16.4) | 14,894 (16.7) | 14,602 (16.5) |
Data are mean (SD), Median [IQR], or N (%).
BMI, body mass index; MET, metabolic equivalent task; NO, nitric oxide; NO2, nitrogen dioxide; PM, particulate matter; WC, waist circumference.
Fig 1. Map of air pollutions (PM2.5, PM2.5–10, NO2, and NO) of areas where participants lived in 2010.
(a) PM2.5, (b) PM2.5–10, (c) NO2, and (d) NO. The administrative boundary data of the UK are sourced from UK Government Open Data portal (https://data.gov.uk/dataset/3fd8d2d2-b591-42ff-b333-c53a6a513e96/countries-december-2017-full-clipped-boundaries-in-great-britain). These data are UK government–released open data. NO, nitric oxide; NO2, nitrogen dioxide; PM2.5, particulate matter with aerodynamic diameter ≤2.5 μm; PM2.5–10, particulate matter with an aerodynamic diameter between 2.5 and 10 μm.
The associations between individual air pollutants and the risk of T2D are shown in Table 2. We found that PM2.5, NO2, and NO were each associated with an increased risk of T2D in the multivariate-adjusted models, while a positive and marginal association was found for PM2.5–10. Compared to individuals exposed to the lowest quintile of air pollutant, the HR for T2D for those exposed to the highest quintile was 1.12 (95% CI: 1.05 to 1.18, p = 0.002) for PM2.5, 1.11 (1.04 to 1.18, p < 0.001) for NO2, and 1.12 (1.06 to 1.18, p < 0.001) for NO, respectively.
Table 2. HRs of T2D by individual air pollutant concentration among 461,191 UK Biobank participants.
| HR (95% CI) per SD increase | Air pollutant concentration in quintiles | P for trend | |||||
|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | |||
| PM2.5 | 1.04 (1.02, 1.05) | Ref. | 1.08 (1.02, 1.14) | 1.06 (1.01, 1.12) | 1.06 (1.01, 1.12) | 1.12 (1.05, 1.18) | 0.002 |
| PM2.5–10 | 1.01 (0.99, 1.03) | Ref. | 1.02 (0.97, 1.07) | 1.04 (0.98, 1.09) | 1.01 (0.96, 1.06) | 1.06 (1.00, 1.11) | 0.081 |
| NO2 | 1.05 (1.02, 1.07) | Ref. | 1.04 (0.99, 1.10) | 1.07 (1.01, 1.13) | 1.11 (1.05, 1.17) | 1.11 (1.04, 1.18) | <0.001 |
| NO | 1.04 (1.02, 1.05) | Ref. | 1.06 (1.00, 1.11) | 1.06 (1.01, 1.12) | 1.12 (1.06, 1.18) | 1.12 (1.06, 1.18) | <0.001 |
CI, confidence interval; GRS, genetic risk score; HR, hazard ratio; NO, estimated nitric oxide; NO2, nitrogen dioxide; PM2.5, particulate matter with aerodynamic diameter ≤2.5 μm; PM2.5–10, particulate matter with an aerodynamic diameter between 2.5 and 10 μm; T2D, type 2 diabetes.
Models were adjusted for age, ethnicity, sex, Townsend deprivation index, center, alcohol intake, smoking status, physical activity, sedentary hour, healthy diet score, BMI, systolic blood pressure, antihypertension meds, high cholesterol, and T2D GRS.
When jointly considering the 4 air pollutants by the air pollution score, we found that participants exposed to higher levels of the score were significantly associated with a higher risk of T2D (Table 3). In the age, ethnicity, and sex-adjusted model (model 1), individuals within the fifth quintile (Q5) of air pollution score had a 71% increased risk of developing T2D, compared to those in Q1 (p < 0.001). After further adjustment for assessment center, Townsend deprivation index, alcohol intake, smoking status, total physical activity, sedentary hours, and healthy diet score, the association between air pollution score and risk of T2D attenuated but remained significant (HR for extreme quintiles was 1.16 (1.10 to 1.22, p < 0.001) in model 2). Additional adjustment for BMI, systolic blood pressure, antihypertension medication use, high cholesterol, and GRS of T2D did not appreciably change the result (HR for extreme quintiles was 1.12 (1.06 to 1.109, p < 0.001) in model 3). Also, the results were stable when we excluded PM2.5–10 in the air pollution score (S4 Table). Sensitivity analysis excluding T2D cases developed within the first 2 years of follow-up yielded similar results (S5 Table). Moreover, the results were robust when only participants living in the current address for at least 5 years were included (S6 Table).
Table 3. Associations between air pollution score and incident T2D among 461,191 UK Biobank participants.
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| HR (95% CI) | p-value | HR (95% CI) | p-value | HR (95% CI) | p-value | |
| Air pollution score per SD | 1.17 (1.16, 1.19) | <0.001 | 1.05 (1.03, 1.07) | <0.001 | 1.04 (1.02, 1.06) | <0.001 |
| Q1 | ref | - | ref | - | ref | - |
| Q2 | 1.20 (1.14, 1.27) | <0.001 | 1.07 (1.02, 1.13) | 0.007 | 1.05 (0.99, 1.10) | 0.11 |
| Q3 | 1.34 (1.28, 1.41) | <0.001 | 1.11 (1.05, 1.16) | <0.001 | 1.06 (1.00, 1.11) | 0.051 |
| Q4 | 1.51 (1.44, 1.58) | <0.001 | 1.15 (1.09, 1.21) | <0.001 | 1.09 (1.03, 1.15) | 0.002 |
| Q5 | 1.71 (1.63, 1.80) | <0.001 | 1.16 (1.10, 1.22) | <0.001 | 1.12 (1.06, 1.19) | <0.001 |
Model 1: adjusted for age, ethnicity, and sex.
Model 2: Model 1+ Townsend deprivation index, center, alcohol intake, smoking status, physical activity, sedentary hour, and healthy diet score.
Model 3: Model 2+ BMI, SBP, antihypertension meds, high cholesterol, and T2D-GRS.
BMI, body mass index; CI, confidence interval; GRS, genetic risk score; HR, hazard ratio; SBP, systolic blood pressure; T2D, type 2 diabetes.
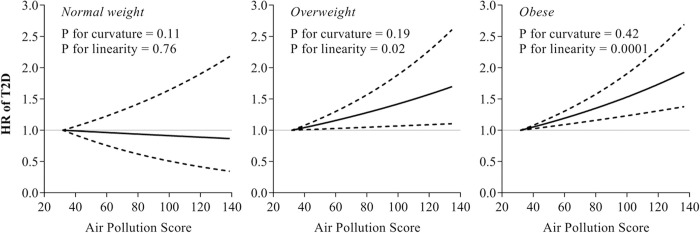
Intriguingly, we found significant interactions between the air pollution score and BMI on the risk of T2D (S7 Table; p-interaction < 0.001). In the stratified analysis according to the obesity status (normal-weight, overweight, and obesity), the associations between air pollution score and T2D risk appeared to be stronger among overweight and obese participants, while no association was found among those with normal-weight (Fig 2). The spline analysis showed a significant linear relationship between air pollution score and the risk of T2D among overweight and obese participants (p for curvature was 0.19 and 0.42, p for linearity was 0.02 and 0.0001, respectively, in the overweight and obese group). A similar interaction pattern was observed between air pollution score and central obesity status (S1 Fig and S7 Table; p-interaction = 0.015). We also further tested the interaction between air pollution score and obesity GRS on the risk of T2D. However, we did not find a significant modification effect by the obesity GRS, though the relationship was statistically significant among participants with a high genetic risk of obesity (S2 Fig).
Fig 2. Dose-responsive relationship of air pollution score with T2D incidence according to obesity status.
Dashed lines represent the 95% CIs of the HR. Multivariable models were adjusted for age, sex, Townsend deprivation index, center, alcohol intake, smoking status, physical activity, sedentary hours, healthy diet score, systolic blood pressure, antihypertension meds, high cholesterol, and T2D GRS. Sample size for normal weight, overweight, and obese subgroup were 149,945, 193,492, and 105,569, respectively. CI, confidence interval; GRS, genetic risk score; HR, hazard ratio; T2D, type 2 diabetes.
We did not observe a significant interaction between the air pollution score and the genetic risk of T2D, suggesting that such association was consistent regardless of participants’ genetic predisposition to T2D (S3 Fig). We noted that the relationship between air pollution score and T2D were stronger among those with intermediate/high genetic predisposition to T2D, though the test for interaction was not significant.
Discussion
In this large-scale cohort, we found that long-term exposure to various ambient air pollutants including PM2.5, PM2.5–10, NO2, and NO, individually or jointly as an air pollution score, was significantly associated with an increased risk of T2D in the whole population in a dose-responsive fashion, independent of the traditional risk factors. In addition, we found that the association was significantly modified by obesity status, with more pronounced associations observed among overweight/obese individuals than in normal-weight individuals.
The relationship between air pollution and T2D has only been recently investigated. Our findings on the relations between individual air pollutants and T2D are in line with the results from several cohort studies assessing the long-term exposure to air pollutants [16,20–23,27,40]. A study conducted in Hong Kong (N = 57,053) among an elder population (aged 65+) with a mean follow-up of 9.8 years demonstrated that PM2.5 was associated with an increased risk of T2D [40]. NO2 and NOx were also found to be associated with an increased risk of T2D [16,20,22]. The association between PM2.5–10 and T2D was less studied, and the results were inconsistent [14,23,41]. The conflicting findings from the limited body of previous studies are partly accounted for by the varies in study design, population, sample size, air pollutants measurement, as well as exposure duration.
We observed significant associations of the joint exposure to various air pollutants, evaluated by an air pollution score, with the risk of T2D. Evaluating the health impact of multiple air pollutants has been recognized as a priority in the US Environmental Protection Agency’s integrated, cross-disciplinary research planning [17,19]. The recent assessment of public health consequences of air pollution has been encouraged to move toward a multipollutant approach [42]. Indeed, humans are simultaneously exposed to a complex mixture of air pollutants. The air pollution score could reflect a more comprehensive exposure to various air pollutants and acknowledge the importance of assessing the health burden from simultaneous exposure to multiple air pollutants. This simple algorithm is also easy to interpret and facilitate public health protection from air pollution. Our study indicates that various air pollutants, when exposed together, may jointly influence the T2D risk.
Although the underlying mechanisms linking various air pollutants and increased risk of T2D are still unclear, several mechanisms have been proposed. PM is among the most studied air pollutant on the risk of T2D. A main working hypothesis is that PM may induce oxidative stress and subsequent visceral adipose tissue inflammation, which further leads to insulin resistance [43–46]. Other possible mechanisms explaining the association between air pollution and T2D include the disturbed autonomic nervous system [47], epigenetic changes [48,49], mitochondrial dysfunction [50], as well as alterations in the composition and function of the human gut microbiome [51].
Interestingly, we found that being overweight/obese significantly amplified the association between air pollution score and the risk of T2D, while no association was observed among normal-weight participants. Previous evidence in the Danish Nurse Cohort Study also showed that the association between PM2.5 and T2D was augmented among obese women [27]. Notably, the increased susceptibility of obesity to the adverse effect of air pollution has also been seen with regard to other diseases, including cardiovascular events [52], chronic obstructive pulmonary disease [53], and hypertension [54], lending support to the modification effects of metabolic status on the relations between air pollution and T2D. Our finding on the interaction between air pollution and obesity status is biologically plausible. A previous study has shown that obesity may enhance associations between air pollution and systemic inflammation [55]. As obesity is a proinflammatory state, being overweight/obese may predispose to a heightened inflammatory response and oxidative stress. When both conditions (air pollution and obesity) are present, there is a multiplicative effect [53,55]. Furthermore, several hormones such as adiponectin, leptin, and resistin, which are inversely related to adiposity, may accentuate the adverse effect of air pollution [25,56,57]. Moreover, changes in respiratory physiology among obese individuals may also explain the enhanced susceptibility to air pollution. Previous particle deposition studies and a weight loss trial have shown an association between obesity and enlarged tidal volume, which lead to a greater dose of inhaled particles among obese participants [58–60].
We did not observe the modification effects by the genetic predisposition to obesity or diabetes on the relationship between air pollution and risk of T2D. The null results were partly due to the small variation of BMI or T2D risk explained by the discovered genetic loci [36]. Further studies with a large sample size and prospective design are warranted to replicate our findings.
To the best of our knowledge, this is the first study to investigate the joint associations of various ambient air pollutants with the risk of T2D. The major strengths of our study include a large sample size, prospective study design of UK Biobank, and comprehensive incorporation of various air pollutants in the air pollution score. However, we acknowledge the current analysis has several potential limitations. First, although we have comprehensively considered various air pollutants, some of the previously reported air pollutants were not available in UK Biobank, such as O3, sulfur dioxides, and carbon monoxide. Second, the participants of UK Biobank are mainly of European descent. Whether the observed association could be applied to other ethnic groups and areas warrants further investigation. Third, the observational nature of the study precludes conclusions about causality. Fourth, although we have comprehensively considered typical risk factors and potential confounders, because of the observational study design, residual confounding is inevitable. Lastly, we do not have air pollution data during follow-up.
In conclusion, we found that long-term exposure to various air pollutants, individually or jointly, was associated with an increased risk of T2D, and that the association was more pronounced among overweight/obese participants and central obese participants. Our findings highlight the importance to comprehensively assess the various air pollutants and body weight management in the prevention of T2D.
Supporting information
(DOCX)
EA, effect allele; NEA, noneffect allele; OR, odds ratio; SE, standard error; SNP, single nucleotide polymorphism; T2D, type 2 diabetes.
(DOCX)
β, beta coefficient; BMI, body mass index; Chr, chromosome; EA, effect allele; NEA, noneffect allele; SE, standard error; SNP, single nucleotide polymorphism.
(DOCX)
*Indicates p < 0.001.
(DOCX)
Model 1: adjusted for age, ethnicity, and sex; Model 2: Model 1+ Townsend deprivation index, center, alcohol intake, smoking status, physical activity, sedentary hour, healthy diet score; Model 3: Model 2+ BMI, SBP, antihypertension meds, high cholesterol, and T2D-GRS. BMI, body mass index; GRS, genetic risk score; SBP, systolic blood pressure; T2D, type 2 diabetes.
(DOCX)
Model 1: adjusted for age, ethnicity, and sex; Model 2: Model 1+ Townsend deprivation index, center, alcohol intake, smoking status, physical activity, sedentary hour, healthy diet score; Model 3: Model 2+ BMI, SBP, antihypertension meds, high cholesterol, and T2D-GRS. BMI, body mass index; GRS, genetic risk score; SBP, systolic blood pressure; T2D, type 2 diabetes.
(DOCX)
Model 1: adjusted for age, ethnicity, and sex; Model 2: Model 1+ Townsend deprivation index, center, alcohol intake, smoking status, physical activity, sedentary hour, healthy diet score; Model 3: Model 2+ BMI, SBP, antihypertension meds, high cholesterol, and T2D-GRS. BMI, body mass index; GRS, genetic risk score; SBP, systolic blood pressure; T2D, type 2 diabetes.
(DOCX)
Multivariable models were adjusted for age, sex, Townsend deprivation index, center, alcohol intake, smoking status, physical activity, sedentary hours, healthy diet score, systolic blood pressure, antihypertension meds, high cholesterol, and T2D GRS. GRS, genetic risk score; T2D, type 2 diabetes.
(DOCX)
Dashed lines represent the 95% CIs of the HR. Multivariable models were adjusted for age, sex, Townsend deprivation index, center, alcohol intake, smoking status, physical activity, sedentary hours, healthy diet score, systolic blood pressure, antihypertension meds, high cholesterol, and T2D GRS. Sample size for noncentral obese and central obese subgroup were 177,791 and 271,215, respectively. CI, confidence interval; GRS, genetic risk score; HR, hazard ratio; T2D, type 2 diabetes.
(TIF)
Stratified analyses were performed by tertiles of obesity GRS. Multivariable models were adjusted for age, sex, Townsend deprivation index, center, alcohol intake, smoking status, physical activity, sedentary hours, healthy diet score, BMI, systolic blood pressure, antihypertension meds, and high cholesterol. BMI, body mass index; CI, confidence interval; GRS, genetic risk score; HR, hazard ratio; T2D, type 2 diabetes.
(TIF)
Stratified analyses were performed by tertiles of T2D GRS. Multivariable models were adjusted for age, sex, Townsend deprivation index, center, alcohol intake, smoking status, physical activity, sedentary hours, healthy diet score, BMI, systolic blood pressure, antihypertension meds, and high cholesterol. BMI, body mass index; CI, confidence interval; GRS, genetic risk score; HR, hazard ratio; T2D, type 2 diabetes.
(TIF)
Acknowledgments
The authors appreciate the participants in UK Biobank for their participation and contribution to the research. The study has been conducted using the UK Biobank Resource under Application 29256.
Abbreviations
- BMI
body mass index
- CI
confidence interval
- ESCAPE
European Study of Cohorts for Air Pollution Effects
- GIS
Geographic Information System
- GRS
genetic risk score
- HR
hazard ratio
- IDF
International Diabetes Federation
- IPAQ
International Physical Activity Questionnaire
- LUR
Land Use Regression
- MET
metabolic equivalent task
- NO
nitric oxide
- NO2
nitrogen dioxide
- PM
particulate matter
- SNP
single nucleotide polymorphism
- T2D
type 2 diabetes
- WC
waist circumference
Data Availability
Requests to access the dataset from qualified researchers trained in human participants confidentiality protocols may be sent to UK Biobank (https://www.ukbiobank.ac.uk/researchers/). The current study has been conducted using the UK Biobank Resource under Application 29256.
Funding Statement
LQ received awards from National Heart, Lung, and Blood Institute (Award # HL071981, HL034594, HL126024, URL: https://www.nhlbi.nih.gov/); the National Institute of Diabetes and Digestive and Kidney Diseases (Awards # DK115679, DK091718, DK100383, URL: https://www.niddk.nih.gov/), the Fogarty International Center (award # TW010790, URL: https://www.fic.nih.gov/), and Tulane Research Centers of Excellence Awards (URL: https://sph.tulane.edu/). XL received award from the American Heart Associatioion (award #: 19PRE34380036; URL: https://professional.heart.org/en/research-programs/application-information/predoctoral-fellowship). The funders have no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.International Diabetes Federation. IDF Diabetes Atlas, Ninth Edition 2019 (IDF, 2019). 2019.
- 2.Hu Y, Ding M, Sampson L, Willett WC, Manson JE, Wang M, et al. Intake of whole grain foods and risk of type 2 diabetes: results from three prospective cohort studies. BMJ. 2020;370:m2206. doi: 10.1136/bmj.m2206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Qian F, Liu G, Hu FB, Bhupathiraju SN, Sun Q. Association Between Plant-Based Dietary Patterns and Risk of Type 2 Diabetes: A Systematic Review and Meta-analysis. JAMA Intern Med. 2019;179:1335–44. doi: 10.1001/jamainternmed.2019.2195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Umpierre D, Ribeiro PAB, Kramer CK, Leitao CB, Zucatti ATN, Azevedo MJ, et al. Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: a systematic review and meta-analysis. JAMA. 2011;305:1790–9. doi: 10.1001/jama.2011.576 [DOI] [PubMed] [Google Scholar]
- 5.Avery L, Flynn D, Van Wersch A, Sniehotta FF, Trenell MI. Changing physical activity behavior in type 2 diabetes: a systematic review and meta-analysis of behavioral interventions. Diabetes Care. 2012;35:2681–9. doi: 10.2337/dc11-2452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shan Z, Ma H, Xie M, Yan P, Guo Y, Bao W, et al. Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care. 2015;38:529–37. doi: 10.2337/dc14-2073 [DOI] [PubMed] [Google Scholar]
- 7.Wang M, Zhou T, Li X, Ma H, Liang Z, Fonseca VA, et al. Baseline Vitamin D Status, Sleep Patterns, and the Risk of Incident Type 2 Diabetes in Data From the UK Biobank Study. Diabetes Care. 2020;43: 2776 LP– 2784. doi: 10.2337/dc20-1109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang B-Y, Fan S, Thiering E, Seissler J, Nowak D, Dong G-H, et al. Ambient air pollution and diabetes: A systematic review and meta-analysis. Environ Res. 2020;180:108817. doi: 10.1016/j.envres.2019.108817 [DOI] [PubMed] [Google Scholar]
- 9.Li Y, Xu L, Shan Z, Teng W, Han C. Association between air pollution and type 2 diabetes: an updated review of the literature. Ther Adv Endocrinol Metab. 2019;10:2042018819897046. doi: 10.1177/2042018819897046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rajagopalan S, Brook RD. Air pollution and type 2 diabetes: mechanistic insights. Diabetes. 2012;61:3037–45. doi: 10.2337/db12-0190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coogan PF, White LF, Yu J, Burnett RT, Seto E, Brook RD, et al. PM2. 5 and diabetes and hypertension incidence in the Black Women’s Health Study. Epidemiology. 2016;27:202. doi: 10.1097/EDE.0000000000000418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coogan PF, White LF, Yu J, Burnett RT, Marshall JD, Seto E, et al. Long term exposure to NO2 and diabetes incidence in the Black Women’s Health Study. Environ Res. 2016;148:360–6. doi: 10.1016/j.envres.2016.04.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li X, Tang K, Jin X-R, Xiang Y, Xu J, Yang L-L, et al. Short-term air pollution exposure is associated with hospital length of stay and hospitalization costs among inpatients with type 2 diabetes: a hospital-based study. J Toxicol Environ Heal Part A. 2018;81:819–29. doi: 10.1080/15287394.2018.1491912 [DOI] [PubMed] [Google Scholar]
- 14.Strak M, Janssen N, Beelen R, Schmitz O, Vaartjes I, Karssenberg D, et al. Long-term exposure to particulate matter, NO(2) and the oxidative potential of particulates and diabetes prevalence in a large national health survey. Environ Int. 2017;108:228–36. doi: 10.1016/j.envint.2017.08.017 [DOI] [PubMed] [Google Scholar]
- 15.Pearson JF, Bachireddy C, Shyamprasad S, Goldfine AB, Brownstein JS. Association between fine particulate matter and diabetes prevalence in the US. Diabetes Care. 2010;33:2196–201. doi: 10.2337/dc10-0698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Krämer U, Herder C, Sugiri D, Strassburger K, Schikowski T, Ranft U, et al. Traffic-related air pollution and incident type 2 diabetes: results from the SALIA cohort study. Environ Health Perspect. 2010;118:1273–9. doi: 10.1289/ehp.0901689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.U.S. EPA. Air, Climate, and Energy Strategic Research Action Plan 2012–2016. 2012; 601/R–12/00. Available from: www.epa.gov/research
- 18.U.S. EPA. Air, Climate, and Energy: Strategic Research Action Plan 2016–2019. 2015.
- 19.U.S. EPA. Air and Energy Strategic Research Action Plan FY 2019–2022. 2020.
- 20.Coogan PF, White LF, Jerrett M, Brook RD, Su JG, Seto E, et al. Air Pollution and Incidence of Hypertension and Diabetes Mellitus in Black Women Living in Los Angeles. Circulation. 2012;125:767–72. doi: 10.1161/CIRCULATIONAHA.111.052753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen H, Burnett RT, Kwong JC, Villeneuve PJ, Goldberg MS, Brook RD, et al. Risk of incident diabetes in relation to long-term exposure to fine particulate matter in Ontario. Canada Environ Health Perspect. 2013;121:804–10. doi: 10.1289/ehp.1205958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andersen ZJ, Raaschou-Nielsen O, Ketzel M, Jensen SS, Hvidberg M, Loft S, et al. Diabetes Incidence and Long-Term Exposure to Air Pollution. Diabetes Care. 2012;35:92LP–98. doi: 10.2337/dc11-1155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Renzi M, Cerza F, Gariazzo C, Agabiti N, Cascini S, Di Domenicantonio R, et al. Air pollution and occurrence of type 2 diabetes in a large cohort study. Environ Int. 2018;112:68–76. doi: 10.1016/j.envint.2017.12.007 [DOI] [PubMed] [Google Scholar]
- 24.Wang M, Zhou T, Song Y, Li X, Ma H, Hu Y, et al. Joint exposure to various ambient air pollutants and incident heart failure: a prospective analysis in UK Biobank. Eur Heart J. 2021. doi: 10.1093/eurheartj/ehaa1031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li W, Dorans KS, Wilker EH, Rice MB, Schwartz J, Coull BA, et al. Residential proximity to major roadways, fine particulate matter, and adiposity: The framingham heart study. Obesity. 2016;24:2593–9. doi: 10.1002/oby.21630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li M, Qian Z, Vaughn M, Boutwell B, Ward P, Lu T, et al. Sex-specific difference of the association between ambient air pollution and the prevalence of obesity in Chinese adults from a high pollution range area: 33 communities Chinese health study. Atmos Environ. 2015;117:227–33. [Google Scholar]
- 27.Hansen AB, Ravnskjær L, Loft S, Andersen KK, Bräuner EV, Baastrup R, et al. Long-term exposure to fine particulate matter and incidence of diabetes in the Danish Nurse Cohort. Environ Int. 2016;91:243–50. doi: 10.1016/j.envint.2016.02.036 [DOI] [PubMed] [Google Scholar]
- 28.Eze IC, Imboden M, Kumar A, von Eckardstein A, Stolz D, Gerbase MW, et al. Air pollution and diabetes association: Modification by type 2 diabetes genetic risk score. Environ Int. 2016;94:263–71. doi: 10.1016/j.envint.2016.04.032 [DOI] [PubMed] [Google Scholar]
- 29.Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:e1001779–9. doi: 10.1371/journal.pmed.1001779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Beelen R, Hoek G, Vienneau D, Eeftens M, Dimakopoulou K, Pedeli X, et al. Development of NO2 and NOx land use regression models for estimating air pollution exposure in 36 study areas in Europe–The ESCAPE project. Atmos Environ. 2013;72:10–23. doi: 10.1016/j.atmosenv.2013.02.037 [DOI] [Google Scholar]
- 31.Eeftens M, Beelen R, de Hoogh K, Bellander T, Cesaroni G, Cirach M, et al. Development of Land Use Regression models for PM(2.5), PM(2.5) absorbance, PM(10) and PM(coarse) in 20 European study areas; results of the ESCAPE project. Environ Sci Technol. 2012;46:11195–205. doi: 10.1021/es301948k [DOI] [PubMed] [Google Scholar]
- 32.Cyrys J, Eeftens M, Heinrich J, Ampe C, Armengaud A, Beelen R, et al. Variation of NO2 and NOx concentrations between and within 36 European study areas: Results from the ESCAPE study. Atmos Environ. 2012;62:374–90. doi: 10.1016/j.atmosenv.2012.07.080 [DOI] [Google Scholar]
- 33.Bycroft C, Freeman C, Petkova D, Band G, Elliott LT, Sharp K, et al. Genome-wide genetic data on ~500,000 UK Biobank participants. bioRxiv. 2017. doi: 10.1101/166298 [preprint] [DOI] [Google Scholar]
- 34.Vetter C, Dashti HS, Lane JM, Anderson SG, Schernhammer ES, Rutter MK, et al. Night shift work, genetic risk, and type 2 diabetes in the UK biobank. Diabetes Care. 2018;41:762–9. doi: 10.2337/dc17-1933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scott RA, Scott LJ, Mägi R, Marullo L, Gaulton KJ, Kaakinen M, et al. An Expanded Genome-Wide Association Study of Type 2 Diabetes in Europeans. Diabetes. 2017;66:2888–902. doi: 10.2337/db16-1253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Locke A, Kahali B, Berndt S, Justice A, Pers T. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518:197–206. doi: 10.1038/nature14177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.IPAQ Research Committee. Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ)-short and long forms. 2005. Available from: http//wwwipaqkise/scoring pdf.
- 38.Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB [DOI] [PubMed] [Google Scholar]
- 39.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The american heart association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703 [DOI] [PubMed] [Google Scholar]
- 40.Qiu H, Schooling CM, Sun S, Tsang H, Yang Y, Lee RS-Y, et al. Long-term exposure to fine particulate matter air pollution and type 2 diabetes mellitus in elderly: a cohort study in Hong Kong. Environ Int. 2018;113:350–6. doi: 10.1016/j.envint.2018.01.008 [DOI] [PubMed] [Google Scholar]
- 41.Puett RC, Hart JE, Schwartz J, Hu FB, Liese AD, Laden F. Are particulate matter exposures associated with risk of type 2 diabetes? Environ Health Perspect. 2011;119:384–9. doi: 10.1289/ehp.1002344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dominici F, Peng RD, Barr CD, Bell ML. Protecting human health from air pollution: shifting from a single-pollutant to a multipollutant approach. Epidemiology. 2010;21:187–94. doi: 10.1097/EDE.0b013e3181cc86e8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sun Q, Yue P, Deiuliis JA, Lumeng CN, Kampfrath T, Mikolaj MB, et al. Ambient air pollution exaggerates adipose inflammation and insulin resistance in a mouse model of diet-induced obesity. Circulation. 2009;119:538–46. doi: 10.1161/CIRCULATIONAHA.108.799015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brook RD, Rajagopalan S, Pope CA III, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. 2010;121:2331–78. doi: 10.1161/CIR.0b013e3181dbece1 [DOI] [PubMed] [Google Scholar]
- 45.Hoffmann B, Moebus S, Dragano N, Stang A, Möhlenkamp S, Schmermund A, et al. Chronic residential exposure to particulate matter air pollution and systemic inflammatory markers. Environ Health Perspect. 2009;117:1302–8. doi: 10.1289/ehp.0800362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hennig F, Fuks K, Moebus S, Weinmayr G, Memmesheimer M, Jakobs H, et al. Association between source-specific particulate matter air pollution and hs-CRP: local traffic and industrial emissions. Environ Health Perspect. 2014;122:703–10. doi: 10.1289/ehp.1307081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen J-C, Stone PH, Verrier RL, Nearing BD, MacCallum G, Kim J-Y, et al. Personal Coronary Risk Profiles Modify Autonomic Nervous System Responses to Air Pollution. J Occup Environ Med 2006;48. Available from: https://journals.lww.com/joem/Fulltext/2006/11000/Personal_Coronary_Risk_Profiles_Modify_Autonomic.7.aspxdoi: 10.1097/01.jom.0000245675.85924.7e [DOI] [PubMed] [Google Scholar]
- 48.Bind M-A, Baccarelli A, Zanobetti A, Tarantini L, Suh H, Vokonas P, et al. Air pollution and markers of coagulation, inflammation and endothelial function: Associations and epigene-environment interactions in an elderly cohort. Epidemiology. 2012;23:332. doi: 10.1097/EDE.0b013e31824523f0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Carmona JJ, Sofer T, Hutchinson J, Cantone L, Coull B, Maity A, et al. Short-term airborne particulate matter exposure alters the epigenetic landscape of human genes associated with the mitogen-activated protein kinase network: a cross-sectional study. Environ Health. 2014;13:94. doi: 10.1186/1476-069X-13-94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Xu X, Liu C, Xu Z, Tzan K, Zhong M, Wang A, et al. Long-term exposure to ambient fine particulate pollution induces insulin resistance and mitochondrial alteration in adipose tissue. Toxicol Sci. 2011;124:88–98. doi: 10.1093/toxsci/kfr211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fouladi F, Bailey MJ, Patterson WB, Sioda M, Blakley IC, Fodor AA, et al. Air pollution exposure is associated with the gut microbiome as revealed by shotgun metagenomic sequencing. Environ Int. 2020;138:105604. doi: 10.1016/j.envint.2020.105604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Miller KA, Siscovick DS, Sheppard L, Shepherd K, Sullivan JH, Anderson GL, et al. Long-Term Exposure to Air Pollution and Incidence of Cardiovascular Events in Women. N Engl J Med. 2007;356:447–58. doi: 10.1056/NEJMoa054409 [DOI] [PubMed] [Google Scholar]
- 53.McCormack MC, Belli AJ, Kaji DA, Matsui EC, Brigham EP, Peng RD, et al. Obesity as a susceptibility factor to indoor particulate matter health effects in COPD. Eur Respir J. 2015;45:1248 LP–1257. doi: 10.1183/09031936.00081414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dong G-H, Wang J, Zeng X-W, Chen L, Qin X-D, Zhou Y, et al. Interactions Between Air Pollution and Obesity on Blood Pressure and Hypertension in Chinese Children. Epidemiology 2015;26. Available from: https://journals.lww.com/epidem/Fulltext/2015/09000/Interactions_Between_Air_Pollution_and_Obesity_on.18.aspxdoi: 10.1097/EDE.0000000000000336 [DOI] [PubMed] [Google Scholar]
- 55.Dubowsky SD, Suh H, Schwartz J, Coull BA, Gold DR. Diabetes, Obesity, and Hypertension May Enhance Associations between Air Pollution and Markers of Systemic Inflammation. Environ Health Perspect. 2006;114:992–8. doi: 10.1289/ehp.8469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chen W, Han Y, Wang Y, Chen X, Qiu X, Li W, et al. Associations between changes in adipokines and exposure to fine and ultrafine particulate matter in ambient air in Beijing residents with and without pre-diabetes. BMJ Open Diabetes Res Care. 2020;8:e001215. doi: 10.1136/bmjdrc-2020-001215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wolf K, Popp A, Schneider A, Breitner S, Hampel R, Rathmann W, et al. Association Between Long-term Exposure to Air Pollution and Biomarkers Related to Insulin Resistance, Subclinical Inflammation, and Adipokines. Diabetes. 2016;65:3314 LP–3326. doi: 10.2337/db15-1567 [DOI] [PubMed] [Google Scholar]
- 58.Graham DR, Chamberlain MJ, Hutton L, King M, Morgan WK. Inhaled particle deposition and body habitus. Br J Ind Med. 1990;47:38–43. doi: 10.1136/oem.47.1.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bennett WD, Zeman KL. Effect of body size on breathing pattern and fine-particle deposition in children. J Appl Physiol. 2004;97:821–6. doi: 10.1152/japplphysiol.01403.2003 [DOI] [PubMed] [Google Scholar]
- 60.Matos CMP, Moraes KS, França DC, Tomich GM, Farah MW, Dias RC, et al. Changes in breathing pattern and thoracoabdominal motion after bariatric surgery: a longitudinal study. Respir Physiol Neurobiol. 2012;181:143–7. doi: 10.1016/j.resp.2012.02.009 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
EA, effect allele; NEA, noneffect allele; OR, odds ratio; SE, standard error; SNP, single nucleotide polymorphism; T2D, type 2 diabetes.
(DOCX)
β, beta coefficient; BMI, body mass index; Chr, chromosome; EA, effect allele; NEA, noneffect allele; SE, standard error; SNP, single nucleotide polymorphism.
(DOCX)
*Indicates p < 0.001.
(DOCX)
Model 1: adjusted for age, ethnicity, and sex; Model 2: Model 1+ Townsend deprivation index, center, alcohol intake, smoking status, physical activity, sedentary hour, healthy diet score; Model 3: Model 2+ BMI, SBP, antihypertension meds, high cholesterol, and T2D-GRS. BMI, body mass index; GRS, genetic risk score; SBP, systolic blood pressure; T2D, type 2 diabetes.
(DOCX)
Model 1: adjusted for age, ethnicity, and sex; Model 2: Model 1+ Townsend deprivation index, center, alcohol intake, smoking status, physical activity, sedentary hour, healthy diet score; Model 3: Model 2+ BMI, SBP, antihypertension meds, high cholesterol, and T2D-GRS. BMI, body mass index; GRS, genetic risk score; SBP, systolic blood pressure; T2D, type 2 diabetes.
(DOCX)
Model 1: adjusted for age, ethnicity, and sex; Model 2: Model 1+ Townsend deprivation index, center, alcohol intake, smoking status, physical activity, sedentary hour, healthy diet score; Model 3: Model 2+ BMI, SBP, antihypertension meds, high cholesterol, and T2D-GRS. BMI, body mass index; GRS, genetic risk score; SBP, systolic blood pressure; T2D, type 2 diabetes.
(DOCX)
Multivariable models were adjusted for age, sex, Townsend deprivation index, center, alcohol intake, smoking status, physical activity, sedentary hours, healthy diet score, systolic blood pressure, antihypertension meds, high cholesterol, and T2D GRS. GRS, genetic risk score; T2D, type 2 diabetes.
(DOCX)
Dashed lines represent the 95% CIs of the HR. Multivariable models were adjusted for age, sex, Townsend deprivation index, center, alcohol intake, smoking status, physical activity, sedentary hours, healthy diet score, systolic blood pressure, antihypertension meds, high cholesterol, and T2D GRS. Sample size for noncentral obese and central obese subgroup were 177,791 and 271,215, respectively. CI, confidence interval; GRS, genetic risk score; HR, hazard ratio; T2D, type 2 diabetes.
(TIF)
Stratified analyses were performed by tertiles of obesity GRS. Multivariable models were adjusted for age, sex, Townsend deprivation index, center, alcohol intake, smoking status, physical activity, sedentary hours, healthy diet score, BMI, systolic blood pressure, antihypertension meds, and high cholesterol. BMI, body mass index; CI, confidence interval; GRS, genetic risk score; HR, hazard ratio; T2D, type 2 diabetes.
(TIF)
Stratified analyses were performed by tertiles of T2D GRS. Multivariable models were adjusted for age, sex, Townsend deprivation index, center, alcohol intake, smoking status, physical activity, sedentary hours, healthy diet score, BMI, systolic blood pressure, antihypertension meds, and high cholesterol. BMI, body mass index; CI, confidence interval; GRS, genetic risk score; HR, hazard ratio; T2D, type 2 diabetes.
(TIF)
Data Availability Statement
Requests to access the dataset from qualified researchers trained in human participants confidentiality protocols may be sent to UK Biobank (https://www.ukbiobank.ac.uk/researchers/). The current study has been conducted using the UK Biobank Resource under Application 29256.