Abstract
Background
School-based COVID-19 contacts in England have been asked to self-isolate at home, missing key educational opportunities. We trialled daily testing of contacts as an alternative to assess whether this resulted in similar control of transmission, while allowing more school attendance.
Methods
We did an open-label, cluster-randomised, controlled trial in secondary schools and further education colleges in England. Schools were randomly assigned (1:1) to self-isolation of school-based COVID-19 contacts for 10 days (control) or to voluntary daily lateral flow device (LFD) testing for 7 days with LFD-negative contacts remaining at school (intervention). Randomisation was stratified according to school type and size, presence of a sixth form, presence of residential students, and proportion of students eligible for free school meals. Group assignment was not masked during procedures or analysis. Coprimary outcomes in all students and staff were COVID-19-related school absence and symptomatic PCR-confirmed COVID-19, adjusted for community case rates, to estimate within-school transmission (non-inferiority margin <50% relative increase). Analyses were done on an intention-to-treat basis using quasi-Poisson regression, also estimating complier average causal effects (CACE). This trial is registered with the ISRCTN registry, ISRCTN18100261.
Findings
Between March 18 and May 4, 2021, 204 schools were taken through the consent process, during which three decided not to participate further. 201 schools were randomly assigned (control group n=99, intervention group n=102) in the 10-week study (April 19–May 10, 2021), which continued until the pre-appointed stop date (June 27, 2021). 76 control group schools and 86 intervention group schools actively participated; additional national data allowed most non-participating schools to be included in analysis of coprimary outcomes. 2432 (42·4%) of 5763 intervention group contacts participated in daily contact testing. There were 657 symptomatic PCR-confirmed infections during 7 782 537 days-at-risk (59·1 per 100 000 per week) in the control group and 740 during 8 379 749 days-at-risk (61·8 per 100 000 per week) in the intervention group (intention-to-treat adjusted incidence rate ratio [aIRR] 0·96 [95% CI 0·75–1·22]; p=0·72; CACE aIRR 0·86 [0·55–1·34]). Among students and staff, there were 59 422 (1·62%) COVID-19-related absences during 3 659 017 person-school-days in the control group and 51 541 (1·34%) during 3 845 208 person-school-days in the intervention group (intention-to-treat aIRR 0·80 [95% CI 0·54–1·19]; p=0·27; CACE aIRR 0·61 [0·30–1·23]).
Interpretation
Daily contact testing of school-based contacts was non-inferior to self-isolation for control of COVID-19 transmission, with similar rates of symptomatic infections among students and staff with both approaches. Infection rates in school-based contacts were low, with very few school contacts testing positive. Daily contact testing should be considered for implementation as a safe alternative to home isolation following school-based exposures.
Funding
UK Government Department of Health and Social Care.
Introduction
In the COVID-19 pandemic, disease control in schools has ranged from no controls at one extreme, to school closure at another, the latter largely based on evidence regarding transmission of influenza.1 Between these poles, different degrees of control have been applied, including isolation of suspected or confirmed cases, to isolation of close contacts of cases.2 With widespread availability of SARS-CoV-2 point-of-care testing, daily contact testing has been modelled and piloted as an alternative to compulsory unsupervised isolation of contacts.3, 4, 5 Daily contact testing allows contacts to attend school provided a daily SARS-CoV-2 test is negative. Daily testing with antigen lateral flow devices (LFDs) is feasible,6 with rapid turnaround times, relatively low cost, and good detection of the virus.7, 8, 9 In addition to allowing students and staff to remain at school, daily contact testing might make regular asymptomatic testing more popular and improve contact reporting by removing the social penalty of positive cases triggering isolation in contacts.10 This in turn might improve case detection and therefore might even reduce transmission.3 However, concerns about LFD performance, especially outside of health-care and expert settings, have left uncertainty about whether daily contact testing is appropriate for schools or more widely.11
Research in context.
Evidence before this study
We searched PubMed with no language restrictions for research articles published up to June 26, 2021. We used the terms “SARS-CoV-2” and “school” and “transmission”, as well as “COVID-19” and “school” and “transmission”. We found no clinical trials on interventions to impact SARS-CoV-2 transmission in schools or other educational settings. Evidence synthesis on COVID-19 transmission has found the evidence for school closure relies on extrapolating from studies of influenza transmission. Further data from schools have accrued from observational data and modelling. Public health data after school opening in England in summer, 2020 showed that school-related outbreaks of SARS-CoV-2 were uncommon, and strongly associated with community incidence of infection. A review of all case–contact pairs in the UK Test and Trace system estimated a low chance of transmission following educational contact with SARS-CoV-2 in young people. Modelling studies have suggested that implementing daily contact testing in place of contact isolation might be neutral or advantageous with regards to control of transmission.
Added value of this study
To our knowledge, we report the first randomised, controlled trial of a public health intervention on SARS-CoV-2 transmission in secondary schools and colleges of further education, during a period of low to moderate community incidence, predominantly with the delta (B.1.617.2) variant. Infection in close contacts in these educational settings was uncommon and around 2%. Supervised daily testing with lateral flow devices as an alternative to self-isolation for close contacts was non-inferior for control of SARS-CoV-2 transmission. School absence was reduced where testing was available, but did not demonstrate significant reduction.
Implications of all the available evidence
Safe alternatives to mass isolation for young people in education are crucial to reducing the impact of the COVID-19 pandemic. With low transmission to contacts, in the context of other mitigations, the results here show daily testing of contacts is an acceptable alternative. Further randomised, controlled trials of public health policy interventions can ensure an evidence-based response to the pandemic.
A policy of self-isolation of contacts assumes this reduces the risk of onward transmission in schools. In practice, its impact is unknown: adherence to isolation is incomplete,12 and the number of isolation days required to prevent one onward transmission has not been calculated. Evidence is lacking that the benefit of the policy outweighs the clear social13, 14 and educational15, 16, 17 disadvantages. Contact-tracing data from England suggest that transmission following contact in secondary schools is infrequent, and occurs in less than 3% of contacts of teenagers with SARS-CoV-2 infection.18 Observational reports from England found educational outbreaks are uncommon, and are strongly associated with community incidence.19
We did a cluster-randomised, controlled trial of daily contact testing in students and staff at secondary schools and colleges in England to show whether daily contact testing increases school attendance and to assess the impact of daily contact testing on SARS-CoV-2 transmission within schools.
Methods
Study design and participants
We did an open-label, cluster-randomised, controlled trial to assess the effectiveness of offering daily testing to contacts of COVID-19 cases. The study took place in secondary schools and further education colleges in England. Secondary schools were studied because students at these schools were already participating in asymptomatic screening with LFDs, and so the trial built upon existing infrastructure that was not present in primary schools (students aged ≤11 years). Schools and colleges (hereafter collectively referred to as schools) were eligible to participate if willing to follow the trial procedures and able to operate assisted testing on site. A representative of the institution provided consent electronically. Participation by individual student and staff contacts was voluntary and followed written or electronic completion of a consent form. After random assignment of the school, parents or guardians provided consent for participants younger than 16 years and for those otherwise unable to give consent. The study protocol was reviewed, and ethical approval granted, by Public Health England's Research Ethics and Governance Group (reference R&D 434). The study was done in accordance with the Declaration of Helsinki and national legislation. A nested qualitative process study of acceptability and feasibility for students, parents, and staff is reported separately.20 The study protocol and analysis plan are provided in the appendix (pp 39–102).
Randomisation and masking
Schools were randomly assigned (1:1) to either a policy of offering contacts daily testing over 7 days to allow continued school attendance (intervention group) or to follow usual policy of isolation of contacts for 10 days (control group). Randomisation lists were generated using random number generation provided by Stata version 16 (appendix p 1). Stratification was done according to school type and size, presence of a sixth form, presence of residential students, and proportion of students eligible for free school meals (nine strata: government funded with ages 11–18 years and free school meals ≤17% vs >17%; government funded with ages 11–16 years and free school meals ≤17% vs >17%; residential school; special needs or alternate provision; further education collage with ages ≥16 years; and independent day school ≥500 pupils vs <500 pupils) to ensure schools representative of those in England were balanced between study groups. Randomisation was done by a trial team member (TEAP) who had no role in the enrolment of schools. Group assignment was not masked during study procedures or analysis. During the trial, the trial management team were masked to the combined data recorded for each SARS-CoV-2 infection.
Procedures
All schools in the intervention and control groups followed the national policy of offering twice weekly asymptomatic testing with LFDs. Individuals with positive LFD results were required to self-isolate immediately and requested to obtain a confirmatory PCR test within 2 days.21 Those with indicator symptoms of possible COVID-19 (new cough, fever, loss or change in taste or smell) were required to self-isolate along with their household and obtain an urgent PCR test.
If a student or staff member tested positive by LFD or PCR, close contacts (hereafter referred to as contacts) were identified by schools using national guidelines (appendix p 2). Those in close contact with a case less than 48 h before symptom onset (or a positive test if asymptomatic) were required to self-isolate for 10 days.22
At schools in the intervention group, contacts were offered daily contact testing as an alternative to self-isolation, provided the contact was school-based (ie, with a staff member or student), the contact did not have indicator symptoms of COVID-19, and contacts were able to attend for on-site testing at school. Contacts were excluded from daily contact testing if they had a household member who was isolating following a positive SARS-CoV-2 test. Contacts who did not consent to daily contact testing were required to self-isolate for 10 days.22
Participants in schools in the intervention group who agreed to daily contact testing swabbed their own anterior nose; swabs were tested by school staff using a SARS-CoV-2 antigen LFD (Orient Gene, Huzhou, China).23 Participants who tested negative were informed and released from isolation that day to attend education, but were asked to self-isolate after school and on non-testing days (weekends and holidays). Those with five negative tests over 7 or more days were released from self-isolation, allowing for no testing at weekends. When a school-based close contact tested positive, they were instructed to self-isolate along with their household, their school-based contacts were identified, and the process repeated for those contacts.
A study worker was funded at each participating school. Schools provided a list of all students and staff, including personal identifiers and demographics. For consented, randomly assigned schools that stopped active participation, where available, a list of students was provided by the UK Government Department for Education.
Schools reported the numbers of staff and students present on each school day, absent for COVID-19-related reasons, and absent for other reasons. Where available, data from schools who stopped participating were obtained from the Department for Education.
Schools recorded each SARS-CoV-2 infection (index case) brought to their attention, including PCR-positive cases and LFD-positive cases without a subsequent PCR test. LFD-positive-PCR-negative individuals were not considered cases. The school-based contacts of each index case, whether the contact consented to study procedures, and the LFD results were recorded.
Results of routine SARS-CoV-2 PCR tests done outside of the study in staff and students were obtained from national public health data (National Health Service [NHS] Test and Trace). Dedicated study PCR testing was also done in consenting contacts in both study groups on day 2 and 7 of the testing or isolation period. In addition, study PCR tests were obtained from consenting LFD-positive or PCR-positive individuals for later analysis (appendix pp 2–3).
Outcomes
The coprimary outcomes, across all students and staff, were (1) the number COVID-19-related school absences among those otherwise eligible to be in school and (2) the extent of in-school SARS-CoV-2 transmission. Non-inferiority in transmission was considered appropriate, as the intervention was hypothesised to produce beneficial increases in attendance. Transmission was estimated from rates of symptomatic PCR-positive infections recorded by NHS Test and Trace, after controlling for community case rates. Both these endpoints were assessed using study data for actively participating schools and using national administrative data on student attendance and student and staff lists for non-participating, randomly assigned schools. Rates of symptomatic PCR-positive community tests were compared because the incidence of these tests was not expected to be affected by the study intervention, whereas more intensive sampling of asymptomatic contacts in intervention schools might have detected more asymptomatic infection. Twice weekly asymptomatic LFD testing was not reliably reported, so results were not compared between groups.
Secondary outcomes were the estimated rate of symptomatic and asymptomatic SARS-CoV-2 infections outside of first order contacts; daily contact testing participation rates in the intervention group; the proportion of contacts testing positive on asymptomatic study PCR tests and symptomatic routine PCR tests; the performance characteristics of LFD testing versus PCR testing; participation in weekly active COVID-19 case finding; behavioural outcomes for pupils, parents, and staff; and the estimated number of infections acquired in schools and transmission cluster sizes, refined by genomic data. The latter three will be reported separately.
Statistical analysis
The challenge with setting a non-inferiority margin for transmission events is that the margin's meaning is highly dependent on the control group event rate. It was not possible to determine the transmission event rate in the control group before the trial started, and it is subject to ongoing change. However, it was considered at the time of writing the study protocol that with an example infection rate in contacts of 20%, an upper bound of the CI of an absolute increase of 10%—ie, relative increase in transmission of up to 50%—would be acceptable. Given the uncertainties in the absolute rates of transmission events in each group, we powered the trial to detect a difference in school attendance (details are in the appendix p 7).
Rates of COVID-19-related absences and symptomatic PCR-positive SARS-CoV-2 infections were compared on an intention-to-treat basis using quasi-Poisson regression to account for over-dispersion, considering each school as the unit of analysis. We adjusted for randomisation strata groups and participant type (student vs staff) and accounted for repeated measurements from the same school over time (see appendix p 3 for details and for following analyses). Infection incidence models were also adjusted for community SARS-CoV-2 case counts at the lower tier local authority level in the previous week. To account for incomplete participation in daily contact testing, we present complier average causal effects (CACE) estimates for both primary outcomes, which estimate the effect of the intervention among those actively participating.
We report daily contact testing uptake in participants in the intervention group, on a per day and per participant basis. We used Poisson regression to investigate factors associated with per individual participation rates, including the randomisation stratification groups, participant type, age, sex, and ethnicity.
The proportion of close contacts testing positive on an asymptomatic study PCR test or symptomatic community PCR test was compared between study groups using logistic regression. Given there were relatively few PCR-positive contacts, adjustment was made only for randomisation strata groups and local case counts in the previous week.
We compared the performance of LFD testing versus PCR testing in participants tested by both methods on the same day, or up to 2 days later for those testing LFD-positive, regarding PCR testing as the reference standard.
All analyses were performed using R version 4.1 (appendix p 7). This trial is registered with the ISRCTN registry, ISRCTN18100261.
Role of the funding source
The sponsor of the study was involved in study design, matching of NHS Test and Trace data with study records, data curation, and interim monitoring. Otherwise, the study sponsor had no role in data analysis, data interpretation, or writing of the report.
Results
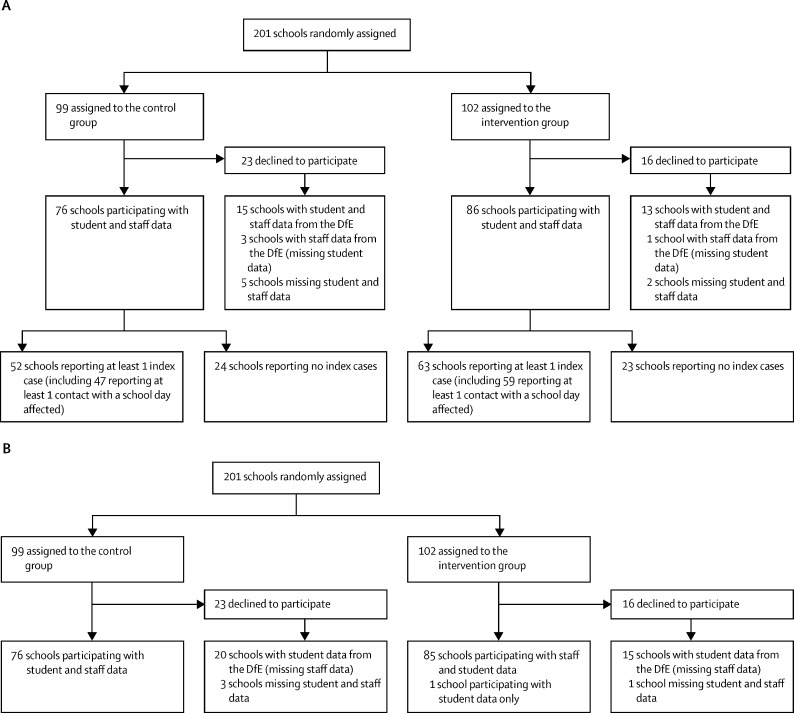
Between March 18 and May 4, 2021, 2000 schools were notified of the study by email and 226 attended webinars to learn more about the study. Of these schools, 204 were taken through the consent process, during which three decided not to participate further. 201 schools were randomly assigned (control group n=99, intervention group n=102; appendix pp 9–14, 34), started participating in the 10-week study (from April 19 to May 10, 2021), and continued until the pre-appointed stop date (June 27, 2021). 76 (77%) of 99 schools in the control group and 86 (84%) of 102 in the intervention group actively participated, returning student and staff lists and attendance data (figure 1 ).
Figure 1.
Consort diagram of participating schools for the two coprimary outcomes: COVID-19-related school absence and symptomatic PCR-positive infection
(A) Flow diagram for COVID-19-related school absence, which depends on availability of daily school attendance data for students and staff aggregated at school level. (B) Flow diagram for symptomatic PCR-positive infection, which depends on provision of student and staff lists to enable matching of identifiers with National Health Service Test and Trace national community testing data. School participation was defined on the basis of submission of student and staff lists and attendance data for at least part of the study. 39 schools stopped active participation between random assignment and the study starting, 26 of which provided reasons: 20 stated resource constraints (15 in the control group; five in the intervention group), three schools in the intervention group cited concerns about the protocol, two schools in the control group did not wish to be in the control group, and one school in the intervention group stopped active participation on local authority public health advice. DfE=UK Government Department for Education.
Baseline characteristics of the randomly assigned schools are shown in table 1 . Ages, sex, and ethnic groups in students and staff were similar between the study groups and most students were aged 11–18 years (table 2 ).
Table 1.
School level baseline characteristics by study group
| Control group (n=99) | Intervention group (n=102) | ||
|---|---|---|---|
| Strata | |||
| Government-funded, ages 11–18 years, free school meals ≤17% | 32 (32%) | 34 (33%) | |
| Government-funded, ages 11–16 years, free school meals ≤17% | 8 (8%) | 8 (8%) | |
| Government-funded, ages 11–18 years, free school meals >17% | 22 (22%) | 24 (24%) | |
| Government-funded, ages 11–16 years, free school meals >17% | 19 (19%) | 18 (18%) | |
| Any residential school | 5 (5%) | 6 (6%) | |
| Special needs or alternate provision | 5 (5%) | 5 (5%) | |
| Further education college, ages ≥16 years | 3 (3%) | 2 (2%) | |
| Independent day school ≥500 pupils | 3 (3%) | 3 (3%) | |
| Independent day school <500 pupils | 2 (2%) | 2 (2%) | |
| Students attending school | 1014 (529–1376) | 1025 (682–1359) | |
| Missing data | 3 (3%) | 1 (1%) | |
| School staff | 142 (91–189) | 125 (91–173) | |
| Missing data | 23 (23%) | 17 (17%) | |
Data are n (%) or median (IQR). The number of students and staff at each school are based on participant lists provided as part of the study and for students from the UK Government Department for Education for schools not actively participating after random assignment. Four schools had missing student lists because schools stopped participating before these were provided and the school had not submitted student lists to the Department for Education previously. 40 schools had missing staff lists because schools stopped participating before these were provided and only student data were available from the Department for Education.
Table 2.
Student and staff level baseline characteristics by study group
|
Students |
Staff |
|||
|---|---|---|---|---|
| Control group (n=102 859) | Intervention group (n=111 693) | Control group (n=11 798) | Intervention group (n=12 229) | |
| Ethnicity | ||||
| Asian | 14 735 (14·3%) | 12 885 (11·5%) | 562 (4·8%) | 522 (4·3%) |
| Black | 6240 (6·1%) | 5772 (5·2%) | 239 (2·0%) | 204 (1·7%) |
| Chinese | 491 (0·5%) | 703 (0·6%) | 12 (0·1%) | 20 (0·2%) |
| Mixed | 4975 (4·8%) | 4565 (4·1%) | 120 (1·0%) | 96 (0·8%) |
| Other | 2137 (2·1%) | 2123 (1·9%) | 65 (0·6%) | 57 (0·5%) |
| Prefer not to say | 8709 (8·5%) | 9948 (8·9%) | 3411 (28·9%) | 3502 (28·6%) |
| White | 65 339 (63·5%) | 75 470 (67·6%) | 7389 (62·6%) | 7828 (64·0%) |
| Missing data | 233 (0·2%) | 227 (0·2%) | 0 | 0 |
| Age group | ||||
| 11–14 years | 48 396 (47·1%) | 50 400 (45·1%) | .. | .. |
| 15–18 years | 49 461 (48·1%) | 52 185 (46·7%) | 16 (0·1%) | 5 (<0·1%) |
| 19–34 years | 3602 (3·5%) | 6974 (6·2%) | 3453 (29·3%) | 3411 (27·9%) |
| 35–44 years | 744 (0·7%) | 1232 (1·1%) | 2807 (23·8%) | 3015 (24·7%) |
| 45–54 years | 418 (0·4%) | 672 (0·6%) | 2865 (24·2%) | 3145 (25·7%) |
| 55–64 years | 143 (0·1%) | 209 (0·2%) | 2215 (18·8%) | 2193 (17·9%) |
| ≥65 years | 95 (<0·1%) | 21 (<0·1%) | 442 (3·7%) | 460 (3·8%) |
| Sex | ||||
| Female | 49 502 (48·1%) | 58 148 (52·1%) | 8092 (68·6%) | 8395 (68·7%) |
| Male | 53 356 (51·9%) | 53 545 (47·9%) | 3706 (31·4%) | 3834 (31·4%) |
| Missing data | 1 (<0·1%) | 0 | 0 | 0 |
Data are n (%). Note students aged ≥19 years attended further education colleges providing courses for students at any age. Data based on 96 control group schools and 101 intervention group schools with data on student demographics and 76 and 86 schools respectively with data on staff.
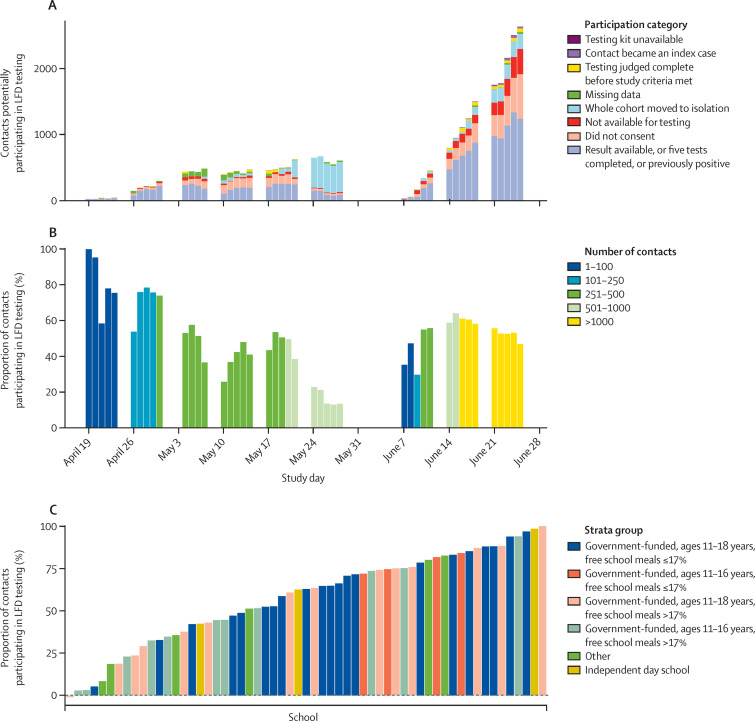
The 76 actively participating schools in the control group reported 338 index cases (students or staff), resulting in 5097 recorded school-based contact events in 4400 individuals. The 86 actively participating schools in the intervention group reported 450 index cases (students or staff), resulting in 6721 recorded school-based contact events in 5797 individuals. 247 index cases in the control group and 343 in the intervention group had at least one contact for whom the 10 days following the contact event included at least 1 study school day. The remaining index cases had no reported close contacts—eg, having tested positive during a weekend or holiday. The 4463 contacts in 47 schools in the control group involved 22 466 school days on which students and staff were asked to isolate at home. The 5763 contacts in 59 schools in the intervention group involved 27 973 school days on which, without the intervention, students and staff would have been asked to isolate at home. In the intervention group, this represented a theoretical maximum of 27 973 (0·68%) of 4 105 826 school days for which daily contact testing could potentially prevent COVID-19-related absences. On 13 846 (49·5%) of 27 973 days an LFD result was recorded (or the contact had already completed follow-up—ie, recorded five or more tests or a positive test). In 1241 contact episodes, the contact declined to participate in daily contact testing (5598 [19·9%] person-school-days) and on 2600 (9·2%) person-school-days a participating contact was unavailable for testing (ie, did not attend school or declined testing). Testing on 4457 (15·8%) person-school-days did not occur after the whole cohort of contacts or school was sent home to isolate, following either school or public health agency intervention (figure 2A ). These participation pauses occurred at 14 schools: five due to school capacity issues, six following school or public health agency concern about the delta (B.1.617.2) variant, and three after public health concern about cases in the school arising from community transmission. No pause was instituted because of excess transmission attributed to the intervention.
Figure 2.
Study participation during 27 973 potential isolation school days in 5763 intervention group contacts
The school half-term holiday was May 31 to June 4, 2021. (A) The number of contacts in the intervention group by study day, by participation or reason for non-participation. (B) The proportion of contacts in the intervention group participating, by study day; bars are coloured according to the number of contacts under follow-up on a given day. (C) The proportion of contacts participating in LFD testing in 59 intervention group schools reporting at least one contact affecting school days. For each contact event, return of three or more LFD results or a positive LFD result is used to summarise participation in the intervention. The bars are coloured by strata group, which summarises the nine strata used for randomisation. Schools with no contacts participating are shown with a small negative value on the y-axis to aid visualisation. LFD=lateral flow device.
Per-day daily contact testing participation was highest at the start of the study and lowest in the week before the half-term holiday (May 31–June 4, 2021) when participation decreased, predominately due to school-wide participation pauses (figure 2A–B).
Using the reporting of three or more LFD results or an LFD-positive result to summarise participation per contact rather than per day, 2432 (42·4%) of 5763 contacts participated, with differing rates by school (figure 2C). Median participation across the 59 schools was 63% (IQR 40–79). Staff were more likely to participate than students (adjusted rate ratio 1·40 [95% CI 1·09–1·80]; p=0·0094). Among schools with up to 17% of students receiving free school meals, participation rates were higher in schools with students aged 11–16 years compared with 11–18 years (table 3 ).
Table 3.
Associations with participation in lateral flow testing in 5763 contacts in intervention group schools where the 10 days following the positive test in the index case included at least 1 school day
|
Descriptive |
Univariable |
Multivariable |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Did not participate (n=3331) | Participated (n=2432) | Rate ratio | 95% CI | p value | Rate ratio | 95% CI | p value | ||
| Study week of first contact test | |||||||||
| 1 | 7 (17%) | 34 (83%) | 1·10 | 0·77–1·58 | 0·60 | 1·45 | 0·92–2·27 | 0·11 | |
| 2 | 70 (25%) | 213 (75%) | .. | .. | .. | .. | .. | .. | |
| 3 | 147 (43%) | 195 (57%) | 0·76 | 0·58–0·99 | 0·041 | 0·81 | 0·60–1·09 | 0·17 | |
| 4 | 138 (41%) | 200 (59%) | 0·79 | 060–1·02 | 0·075 | 0·96 | 0·68–1·36 | 0·82 | |
| 5 | 306 (72%) | 118 (28%) | 0·37 | 0·14–0·95 | 0·038 | 0·43 | 0·20–0·95 | 0·036 | |
| 6 | 412 (93%) | 30 (7%) | 0·09 | 0·02–0·43 | 0·0025 | 0·12 | 0·03–0·49 | 0·0031 | |
| 8 | 206 (42%) | 280 (58%) | 0·77 | 0·59–0·99 | 0·041 | 0·82 | 0·62–1·09 | 0·17 | |
| 9 | 332 (31%) | 755 (69%) | 0·92 | 0·79–1·08 | 0·32 | 1·03 | 0·84–1·28 | 0·75 | |
| 10 | 1713 (74%) | 607 (26%) | 0·35 | 0·24–0·50 | <0·0001 | 0·39 | 0·25–0·60 | <0·0001 | |
| Strata group | |||||||||
| Government-funded, ages 11–18 years, free school meals ≤17% | 1018 (51%) | 979 (49%) | .. | .. | .. | .. | .. | .. | |
| Government-funded, ages 11–16 years, free school meals ≤17% | 70 (22%) | 252 (78%) | 1·60 | 1·17–2·19 | 0·0035 | 1·44 | 1·06–1·95 | 0·020 | |
| Government-funded, ages 11–18 years, free school meals >17% | 987 (66%) | 501 (34%) | 0·69 | 0·39–1·22 | 0·20 | 0·71 | 0·45–1·11 | 0·13 | |
| Government-funded, ages 11–16 years, free school meals >17% | 904 (67%) | 439 (33%) | 0·67 | 0·31–1·44 | 0·30 | 0·76 | 0·47–1·23 | 0·26 | |
| Other | 209 (58%) | 154 (42%) | 0·87 | 0·51–1·47 | 0·59 | 0·82 | 0·49–1·36 | 0·45 | |
| Independent day school | 143 (57%) | 107 (43%) | 0·87 | 0·64–1·19 | 0·39 | 1·00 | 0·68–1·47 | >0·99 | |
| Ethnicity | |||||||||
| White | 2320 (57%) | 1764 (43%) | .. | .. | .. | .. | .. | .. | |
| Asian | 394 (63%) | 236 (37%) | 0·87 | 0·49–1·53 | 0·62 | 1·06 | 0·85–1·31 | 0·61 | |
| Black | 167 (61%) | 106 (39%) | 0·90 | 0·62–1 ·30 | 0·57 | 1·03 | 0·82–1·30 | 0·82 | |
| Chinese | 12 (23%) | 40 (77%) | 1·78 | 1·18–2·69 | 0·0063 | 1·72 | 1·15–2·55 | 0·0076 | |
| Mixed | 134 (64%) | 75 (36%) | 0·83 | 0·61–1·13 | 0·24 | 0·93 | 0·79–1·10 | 0·39 | |
| Other | 76 (77%) | 23 (23%) | 0·54 | 0·31–0·92 | 0·024 | 0·69 | 0·48–0·98 | 0·037 | |
| Prefer not to say | 228 (55%) | 188 (45%) | 1·05 | 0·70–1·57 | 0·83 | 0·94 | 0·70–1·28 | 0·71 | |
| Age group | |||||||||
| 11–14 years | 1840 (65%) | 984 (35%) | .. | .. | .. | .. | .. | .. | |
| 15–18 years | 1400 (53%) | 1258 (47%) | 1·36 | 0·91–2·03 | 0·14 | .. | .. | .. | |
| >18 years | 91 (32%) | 190 (68%) | 1·94 | 1·26–2·99 | 0·0026 | .. | .. | .. | |
| Sex | |||||||||
| Female | 1619 (54%) | 1390 (46%) | .. | .. | .. | .. | .. | .. | |
| Male | 1712 (62%) | 1042 (38%) | 0·82 | 0·72–0·93 | 0·0025 | 0·92 | 0·82–1·03 | 0·14 | |
| Participant type | |||||||||
| Student | 3257 (59%) | 2253 (41%) | .. | .. | .. | .. | .. | .. | |
| Staff | 74 (29%) | 179 (71%) | 1·73 | 1·33–2·25 | <0·0001 | 1·40 | 1·09–1·80 | 0·0094 | |
| School size, students and staff, rate ratio per 100 | 1274 (958–1410) | 1070 (801–1506) | 0·99 | 0·97–1·01 | 0·35 | 0·99 | 0·98–1·00 | 0·18 | |
Data are n (%) or median (IQR), except where otherwise stated. Participant age is omitted from the multivariable model due to colinearity with participant type. Results from Poisson regression, with robust variance estimation, adjusting variance to account for repeated measurements from the same school (for univariable and multivariable models). Week 7 is the school half-term holiday, when school-based lateral flow testing was not done. Participation in the final week of the study is lower than in figure 2, as participation is summarised as completion of three or more lateral flow tests, and contacts in the final week might not have completed testing before the end of the study.
Rates of student and staff COVID-19-related absence, due to known or suspected COVID-19 or as a contact, were compared. Student attendance data were available for part or all of the study from 91 (92%) control schools and 99 (97%) intervention schools; with data for 3551 (86%) of 4146 possible school and school day combinations in the control group and 3836 (90%) of 4261 in the intervention group (appendix p 35). Similarly, staff attendance was available from 94 (95%) control schools for 3767 (91%) of 4146 days and from 100 (98%) intervention group schools for 3925 (92%) of 4261 days. 95 545 students and 14 687 staff in the control group and 102 134 students and 14 811 staff in the intervention group were reported in attendance data (total numbers of students and staff in aggregate attendance data differ from totals from student and staff identifier lists used to identify symptomatic cases [table 2], reflecting different underlying data sources and different schools with available data).
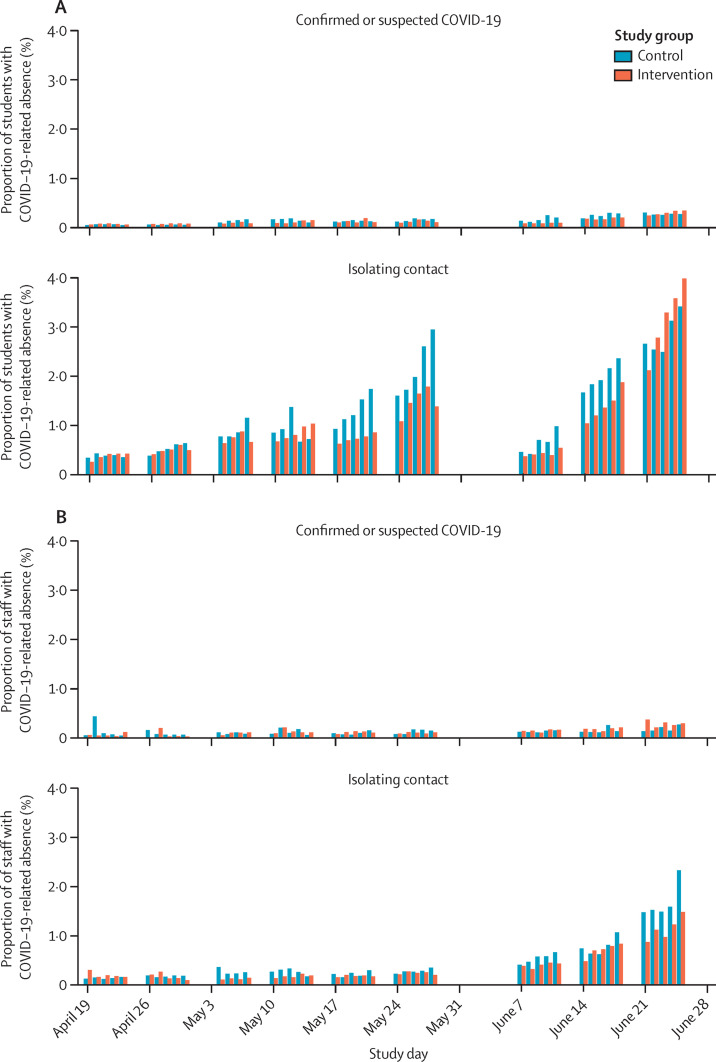
Students had 55 718 (1·80%) COVID-19-related absences during 3 092 515 person-school-days in the control group, and 48 609 (1·47%) during 3 305 403 person-school-days in the intervention group (figure 3 ). Rates of staff COVID-19-related absences were 3704 (0·65%) of 566 502 person-school-days in control schools and 2932 (0·54%) of 539 805 person-school-days in intervention schools.
Figure 3.
Proportion of participants with COVID-19-related absences in the control and intervention groups (coprimary outcome)
The school half-term holiday was May 31 to June 4, 2021. (A) Students absent for COVID-19-related reasons as a proportion of all those not absent for other reasons by study day. (B) Staff absent for COVID-19-related reasons as a proportion of all those not absent for other reasons by study day.
On an intention-to-treat basis, adjusting for the randomisation strata group and participant type, the adjusted incidence rate ratio (aIRR) for COVID-19-related absence in the intervention group was 0·80 (95% CI 0·54–1·19; p=0·27; table 4 ; appendix p 15). Overall, staff were less likely to be absent for COVID-19-related reasons than students across both groups (aIRR 0·39 [95% CI 0·31–0·48]; p<0·0001), but there was no evidence of a difference in the effect of the intervention between students and staff (heterogeneity p=0·98). As no covariate changed with time, the originally proposed approach has a more conservative CI than required. We repeated the analysis aggregating the data per school and participant type, yielding an aIRR of 0·80 (95% CI 0·62–1·03; p=0·085; appendix p 16).
Table 4.
Coprimary and secondary endpoints
|
Intention to treat |
Complier average causal effect |
||||
|---|---|---|---|---|---|
| aIRR or aOR* | 95% CI | p value | Effect | 95% CI | |
| Primary endpoints | |||||
| Rate of COVID-19-related absence | 0·80 | 0·54–1·19 | 0·27 | 0·61 | 0·30–1·23 |
| Rate of COVID-19-related absence (aggregated dataset) | 0·80 | 0·62–1·03 | 0·085 | 0·62 | 0·29–1·33 |
| Rate of symptomatic PCR-confirmed infection | 0·96 | 0·75–1·22 | 0·72 | 0·86 | 0·55–1·34 |
| Secondary endpoints | |||||
| Rate of any absence | 0·97 | 0·82–1·16 | 0·77 | 0·89 | 0·71–1·18 |
| Rate of any community testing PCR-confirmed infection | 0·96 | 0·76–1·20 | 0·71 | 0·88 | 0·57–1·41 |
| Proportion of asymptomatic contacts testing PCR-positive on a research PCR test | 0·73 | 0·33–1·61 | 0·44 | .. | .. |
| Proportion of contacts testing PCR-positive while symptomatic on a routine community test | 1·21 | 0·82–1·79 | 0·34 | .. | .. |
aIRR=adjusted incidence rate ratio. aOR=adjusted odds ratio.
aIRRs are reported for rates, aORs are reported for proportions.
As per day participation in the intervention group was 49·5%, we estimated the impact of the intervention among those participating; the point estimate showed a greater reduction in absences (CACE aIRR 0·61 [95% CI 0·30–1·23]; appendix p 15). Applying this point estimate (with the caveat the range of uncertainty is wide) to COVID-19-related absence in students in the control group (1·80%), would equate to a 39% relative and 0·70% absolute reduction in school days missed due to COVID-19. CACE estimates were relatively unaffected by the choice of imputation strategy for schools with no contacts and therefore no participation data (appendix p 17). Separate intention-to-treat and CACE results for students and staff are shown in the appendix (pp 18–19).
There was no evidence of an impact on all-cause absence rates (intention-to-treat aIRR 0·97 [95% CI 0·82–1·16]; p=0·77), with non-COVID-19-related reasons responsible for most absences (appendix p 20).
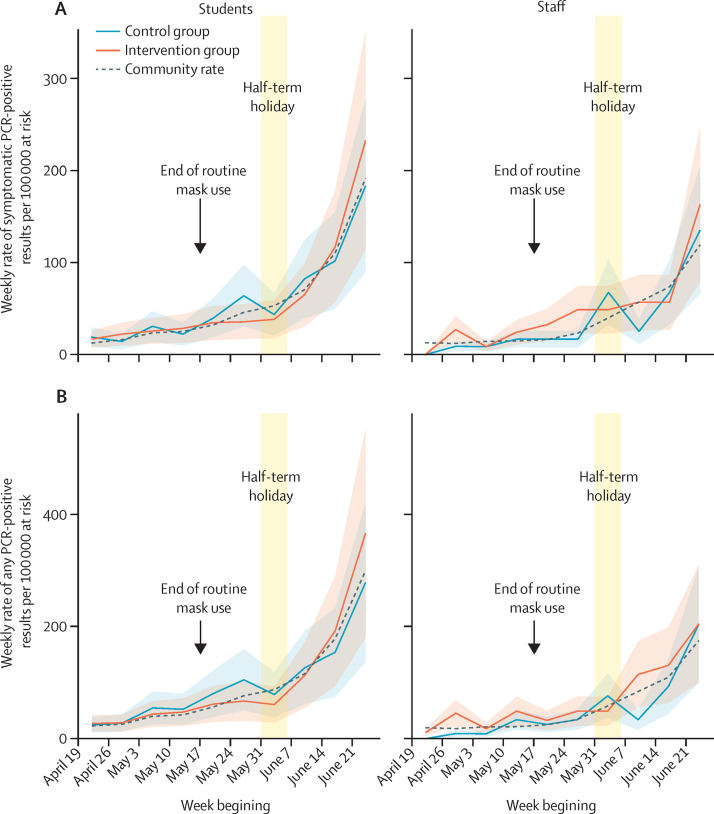
PCR results from symptomatic SARS-CoV-2 infections in students were available for 96 (97%) of 99 control schools and 101 (99%) of 102 intervention schools; staff results were available for 76 (76%) control schools and 85 (83%) intervention schools. 614 students at control schools tested PCR-positive and reported symptoms during 6 966 653 days-at-risk (61·7 cases per 100 000 population per week). 683 students at intervention schools tested PCR-positive and reported symptoms during 7 541 525 days-at-risk (63·4 cases per 100 000 population per week). Rates in staff were 43 per 790 219 days-at-risk (38·1 cases per 100 000 population per week) in the control group and 57 per 819 487 days-at-risk (48·7 cases per 100 000 population per week) in the intervention group. Incidence increased during the study, as the delta variant spread nationally,24 similarly in each group (figure 4A ). Incidence was higher than the number of index cases reported by schools, partly because not all randomly assigned schools actively reported cases and in active schools not all community-diagnosed infections were reported or recorded (appendix p 21).
Figure 4.
Incidence of symptomatic PCR-positive results (coprimary outcome) and incidence of all PCR-positive results (secondary outcome)
(A) Incidence of symptomatic PCR-positive results in students and staff by study group. (B) Incidence of all PCR-positive results in students and staff by study group. Weekly incidence is shown per 100 000 at risk. The shaded area is the mean rate plus or minus 1 SE using a negative binomial model to account for overdispersion (θ=0·28).
Adjusting for the randomisation strata, participant type, and the community rate of SARS-CoV-2 infection in the previous week, there was no evidence of difference between study groups in symptomatic PCR-confirmed infection (intention-to-treat aIRR 0·96 [95% CI 0·75–1·22]; p=0·72; table 4; appendix p 22). Overall rates of infection were lower in staff than students across both groups (aIRR 0·75 [95% CI 0·61–0·92]; p=0·0060), but there was no evidence that the effect of the intervention differed in staff and students (heterogeneity p=0·41). Infection rates in students were approximately linearly related to local case counts, plateauing as community incidence increased (appendix p 36); estimates were similar with varying plausible lags between community case counts and student and staff infections (appendix p 23).
A CACE analysis allowing the impact of the intervention to be estimated given theoretical full participation, also showed no evidence of difference between study groups in symptomatic PCR-confirmed infection (aIRR 0·86 [95% CI 0·55–1·34]). CACE estimates were relatively unaffected by the choice of imputation strategy for schools with missing participation data (appendix p 24).
Similar results were obtained in a secondary analysis of any positive PCR result from routine community-based testing (intention-to-treat aIRR 0·96 [95% CI 0·76–1·20]; p=0·71 and CACE aIRR 0·88 [95% CI 0·57–1·41]; figure 4B; appendix p 25). There was no evidence of a difference in the effect of the intervention for students and staff (intention-to-treat model, heterogeneity p=0·21). Separate analyses for students and staff for symptomatic and any PCR-positive infection are shown in the appendix (pp 26–29).
PCR testing of asymptomatic contacts was done in 886 non-overlapping contact episodes in the control group: 14 (1·6%) tested PCR-positive, one (0·1%) was indeterminate, and 871 (98·3%) tested negative. In 2981 intervention group contacts, 44 (1·5%) tested positive, 14 (0·5%) were indeterminate, and 2923 (98·1%) tested negative. Adjusting for randomisation stratification group and community case counts in the previous week, there was no evidence that the proportion of contacts testing positive varied between study groups (adjusted odds ratio [aOR] 0·73 [95% CI 0·33–1·61]; p=0·44; appendix p 30). Of control and intervention group contacts testing positive or indeterminate, four (27%) of 15 and 19 (33%) of 58 went on to have a positive symptomatic test (exact p=0·76).
We also compared the proportion of contacts with a symptomatic PCR-positive test, which included those initially testing positive while asymptomatic who went on to have a symptomatic test. This analysis was contingent on schools reporting contacts, with several control group schools with higher incidence not actively participating and reporting contacts (appendix p 37). In the control group, 44 (0·9%) of 4665 contacts tested PCR-positive within 10 days, compared with 79 (1·3%) of 5955 in the intervention group. Adjusting for randomisation strata groups and community case counts, there was no evidence that the proportion of contacts testing positive differed between groups (aOR 1·21 [95% CI 0·82–1·79]; p=0·34; appendix p 31).
Across the study, and the non-randomised pilot phase, 4757 contacts completed at least one LFD during daily contact testing, generating 20 289 LFD results overall. For 3226, a paired PCR test was available from the same day, or up to 2 days later for those testing LFD-positive. 3166 were PCR-negative and 60 were PCR-positive. Specificity was 3164 (99·93% [exact binomial 95% CI 99·77–99·99]) of 3166 and sensitivity was 32 (53% [40–66]) of 60 (appendix p 32). These results largely reflect performance in students (appendix p 33), as 3003 (93·1%) of 3226 participants with paired tests were students. PCR-positive cycle threshold values were lower in those testing LFD-positive (median 18·5 [IQR 16·3–22·0]) than LFD-negative (median 25·3 [21·6–28·5]; Kruskal-Wallis p<0·0001; appendix p 38).
Discussion
Daily LFD testing of school-based SARS-CoV-2 contacts was trialled as a voluntary alternative to 10 days of self-isolation. Although daily contact testing avoids students and staff missing school while isolating, at the conception of the trial there was uncertainty whether it would substantially increase SARS-CoV-2 transmission—eg, via infections missed by LFD testing.3 This trial provides evidence this was not the case.
We investigated the incidence of symptomatic infection as an unbiased outcome measure that could be ascertained across nearly all schools, because national public health policy was that all symptomatic children and adults, whether or not they had an LFD test, should obtain a PCR test for SARS-CoV-2. Because the intervention was not expected to affect the relative incidence of asymptomatic versus symptomatic infection, this measure should also indicate the effect on all infections. On the basis of a non-inferiority margin of ensuring any relative increase in symptomatic infection, as a proxy for transmission, did not exceed 50%, we show that allowing student and staff contacts to remain in school after a negative LFD test was non-inferior to routine isolation. On an intention-to-treat basis (ie, implementing daily contact testing at participation rates in the trial, using data for students from 197 of 201 schools and staff data from 161 of 201 schools), we can be 97·5% confident that any increase in the rate of symptomatic infection in the intervention group did not exceed 22% more than in the control group. If all those eligible to participate did so, then, based on a CACE model, we can be 97·5% confident that any increase does not exceed 34%. In both analyses, the point estimate favours a slight to modest reduction in incidence with the intervention.
The range of absolute changes in symptomatic infection rates potentially shown in the intervention group depends on prevailing incidence. At the average incidence in the control group during the study (0·06% students per week; figure 4), the range of uncertainty in the effect of the intervention (based on the CACE estimate shown in table 4) was equivalent to 1·2 fewer to 0·9 more infections per 1000 students per month, or 3·6 fewer to 2·7 more infections per 1000 students per month at the highest weekly rate seen (0·18% students per week). Throughout the study, cases in both groups remained well below the more than 1% level seen in 2020 when schools remained open.25 Staff had lower rates of infection than students. There was no evidence of a difference in the effect of the intervention for students and staff.
Asymptomatic and symptomatic infections were uncommon in school-based contacts in both study groups: in the control group, 1·6% of students and staff participating in study PCRs tested positive while asymptomatic versus 1·5% in the intervention group; in the control group, 0·9% of students and staff tested positive in symptomatic testing versus 1·3% in the intervention group. Around a third of asymptomatic PCR-positive participants went on to develop symptoms, and therefore are also included in the symptomatic percentage testing positive. Thus, the overall proportion of contacts testing positive, with or without symptoms, in both study groups was around 2%. These figures are similar to the estimates for school-age children from national contact-tracing data.18 Therefore, given precautions in place in schools during the trial (routine mask use was discontinued during the trial on May 17, 2021, but other precautions were maintained), the overall risks to students and staff following exposure to a contact at school are low. Whether the extent of transmission and performance of LFDs is sufficient to make contact testing necessary and cost-effective will require careful discussion and might vary with changes in incidence, virus transmissibility, or the prevalence of any vaccine evasive strains. Participation in study PCR testing in control schools was lower than in the intervention schools, in part because participation in daily contact testing facilitated intervention group PCR-testing and because of the greater awareness of the study in intervention schools. It is unclear whether this introduced bias in the results for the study PCR tests; however, we also found no evidence of difference in symptomatic infection rates in contacts.
We did not clearly show superiority of the intervention for avoiding student and staff COVID-19-related school absences. This possibly reflects that the trial was underpowered given the large extent of variation in absence rates over time and between schools, requiring overdispersion to be accounted for in regression models fitted. Pooling data on a per school basis, in an intention-to-treat analysis, our point estimate showed a 20% decrease in COVID-19-related absences, but with a broad range of uncertainty (95% CI 0·62–1·03), similarly in the CACE analysis among those who participated, the point estimate was a 38% reduction, but with broader uncertainty (95% CI 0·29–1·33).
Reductions in COVID-19-related absences were not greater because not all those eligible participated, and not all absences were amenable to the intervention (eg, household contacts were ineligible). However, despite the lack of statistical evidence from the trial, in the absence of increased transmission it is reasonable to assume that a policy allowing students and staff to remain in school would lead to increased attendance, but this might be more limited than initially anticipated.
Daily contact testing participation rates in intervention group contacts were 42·4% on a per-person basis, with marked variation between schools (range 0–100%). Staff were more likely to participate than students. Although contacts at government-funded schools with students 11–16 years old with a low proportion of free school meals were most likely to participate, other school types were similar, such that differences in participation related to factors other than school type. A qualitative analysis of interviews with participants to understand why some participated and others did not, will be reported separately.20 Additionally, at some stages, schools paused the intervention because of capacity limitations or public health officials' concerns about the delta lineage or increasing transmission in the community. No local public health teams reported concern that transmission increased because of this study. We did not formally assess compliance with isolation in the control group, although it was school policy that known cases and contacts did not attend school. However, it is still possible that in both study groups there was incomplete compliance with isolation at home outside of school hours and during school hours in the control group, particularly as lockdown restrictions eased.
Previous estimates for the performance of antigen LFDs compared with PCR testing have varied markedly.7, 9, 26 We estimated the overall sensitivity of school-based LFD testing in largely asymptomatic individuals as 53%—ie, within the range of previously reported rates. It is worth noting that our findings on transmission in this study are in the context of this level of performance. Specificity was 99·93%. As LFD performance varies by viral load,27 performance can change as the population viral load distribution changes. Consistent with previous reports,7 we find higher viral loads (ie, lower PCR cycle threshold values), are associated with increased sensitivity, and therefore LFDs are more likely to detect those who are most infectious.18
This study has several limitations. Schools and colleges, despite provision of dedicated resources, were not always able to participate due to competing pressures. As a result, it is also likely that data capture was imperfect—eg, it is possible that not all PCR-positive cases were reported to schools, and not all contacts were documented for all index cases. However, our primary outcomes are robust to this. We used the incidence of symptomatically driven testing as a primary endpoint as this was least likely to be affected by the two testing strategies; in fact, there was little difference in the incidence of all community PCR tests between the study groups. Relying on linkage to Test and Trace data is a potential weakness, as it depended on imperfectly recorded identifiers; however, this would not be expected to differ between study groups. Furthermore, using incidence data means we did not directly measure within-school transmission, rather we estimated it by controlling for the rate of community infections, as a proxy for the extent of introductions into the school. The trial was done during periods of low to moderate SARS-CoV-2 incidence. We, therefore, did not estimate the impact of daily contact testing in high incidence settings; monitoring of the impact of daily contact testing might be needed if it is deployed when incidence is high. Changes in incidence might relate to new variants, which might impact LFD performance, and so ongoing assessment of LFD performance would be needed as well. High incidence might also pose logistical challenges: in the last 2 weeks of the study, community incidence increased, making the daily contact testing protocol unwieldy for some schools given the space and staff required to do testing. We did not have sufficient power to study if the intervention had different impacts across different school types and settings.
Future work includes whole-genome sequencing of positive samples from school members and from the community, which might help analyse transmission networks in schools, including during periods of higher incidence, in a manner successfully achieved for SARS-CoV-228, 29 and a number of health-care-associated pathogens.30, 31 This study included staff and students from secondary schools and colleges of further education but most of the participants were students aged 11–18 years. Therefore, it is unclear the extent to which it can be generalised to other settings, and other context-specific studies are required.
Our findings have implications for policy makers seeking to balance control of COVID-19 with student wellbeing, education, and avoiding social inequalities. We show daily contact testing is a safe alternative to home isolation for school-based contacts, which has potential to facilitate increased school attendance and therefore to reduce the wider long-term negative consequences of the pandemic.
Overall, this study shows that in secondary schools and colleges of further education, student and staff infection following contact with an individual with COVID-19 at school occurs in only around 2% of contacts. We found switching from isolation at home to daily contact testing, at least in the settings of the schools studied, kept rates of symptomatic COVID-19 in students and staff at similar levels. Daily contact testing is a safe alternative to home isolation in school-based contacts and should be considered an alternative to routine isolation of close contacts following school-based exposures.
Data sharing
Data from the trial will be available within the Office for National Statistics Secure Research Service. Applications for access can be made by accredited researchers. For more details please see https://cy.ons.gov.uk/aboutus/whatwedo/statistics/requestingstatistics/approvedresearcherscheme.
Declaration of interests
DWE reports lecture fees from Gilead outside the submitted work. VB, RO, and DC are consultants employed by Department of Health and Social Care as part of Deloitte's broader project work supporting the delivery of NHS Test and Trace. TF reports honoraria from Qatar National Research Fund outside the submitted work. All other authors declare no competing interests.
Acknowledgments
Acknowledgments
We acknowledge all the students and staff at participating schools, as well as ten pilot schools, for contributing to the study, and in particular the study workers at each of the schools. We are thankful to the Microbiology Department of Oxford University Hospitals NHS Foundation Trust for doing PCR testing. Additionally, we acknowledge the support in conducting the study of the Department of Health and Social Care daily contact testing project management team, especially Nichole Solomon, and the Office for National Statistics daily contact testing team. We thank Department for Education colleagues, particularly Sara Cooper, Matt Mawer, and Richard Lumley for their assistance. We thank Sarah Walker for insightful advice. This study was funded by the UK Government Department of Health and Social Care and supported by the UK Government Department for Education and Office for National Statistics. The work was also supported by the National Institute for Health Research (NIHR) Health Protection Research Unit (HPRU) in Healthcare Associated Infections and Antimicrobial Resistance at Oxford University in partnership with Public Health England (NIHR200915) and the NIHR Biomedical Research Centre, Oxford. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR, the Department of Health and Social Care, the Department for Education, the Office for National Statistics, or Public Health England. BCY is an NIHR clinical lecturer. BCY, TEAP, and LY received grants from the Department of Health and Social Care to fund this work. DWE is a Robertson Foundation Fellow. LY is an NIHR Senior Investigator and her research programme is partly supported by NIHR Applied Research Collaboration–West, NIHR HPRU for Behavioural Science and Evaluation, and the NIHR Southampton Biomedical Research Centre.
Contributors
FI, JH, ST, VB, RO, DC, PM, NH, TF, SH, LY, and TEAP contributed to the protocol and design of the study. BCY, SK, CW, SS, IDi, ER, FD, IDa, LD, PS, AL, JM, FJ, JK, SO, and UB contributed to the implementation of the study or data collection. BCY, DWE, GB, TN, FI, IDa, and TEAP accessed and verified the data. DWE, BCY, and TEAP analysed the data and wrote the manuscript. All authors contributed to revising the manuscript, had full access to all the data in the study, and had final responsibility for the decision to submit for publication.
Supplementary Material
References
- 1.Viner RM, Russell SJ, Croker H, et al. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc Health. 2020;4:397–404. doi: 10.1016/S2352-4642(20)30095-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.UK Government Guidance for schools: coronavirus (COVID-19) 2020. https://www.gov.uk/government/collections/guidance-for-schools-coronavirus-covid-19
- 3.Scientific Pandemic Influenza Group on Modelling. Operational sub-group (SPI-M-O) SPI-M-O: statement on daily contact testing. 3 March 2021. https://www.gov.uk/government/publications/spi-m-o-statement-on-daily-contact-testing-3-march-2021
- 4.Leng T, Hill EM, Thompson RN, Tildesley MJ, Keeling MJ, Dyson L. Assessing the impact of secondary school reopening strategies on within-school COVID-19 transmission and absences: a modelling study. medRxiv. 2021 doi: 10.1101/2021.02.11.21251587. published online Feb 12. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Quilty BJ, Clifford S, Hellewell J, et al. Quarantine and testing strategies in contact tracing for SARS-CoV-2: a modelling study. Lancet Public Health. 2021;6:e175–e183. doi: 10.1016/S2468-2667(20)30308-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Love N, Ready D, Turner C, et al. The acceptability of testing contacts of confirmed COVID-19 cases using serial, self-administered lateral flow devices as an alternative to self-isolation. medRxiv. 2021 doi: 10.1101/2021.03.23.21254168. published online March 26. (preprint). [DOI] [PubMed] [Google Scholar]
- 7.Peto T, Affron D, Afrough B, et al. COVID-19: rapid antigen detection for SARS-CoV-2 by lateral flow assay: a national systematic evaluation of sensitivity and specificity for mass-testing. EClinicalMedicine. 2021;36 doi: 10.1016/j.eclinm.2021.100924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pekosz A, Parvu V, Li M, et al. Antigen-based testing but not real-time polymerase chain reaction correlates with severe acute respiratory syndrome coronavirus 2 viral culture. Clin Infect Dis. 2021 doi: 10.1093/cid/ciaa1706. published online Jan 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leber W, Lammel O, Siebenhofer A, Redlberger-Fritz M, Panovska-Griffiths J, Czypionka T. Comparing the diagnostic accuracy of point-of-care lateral flow antigen testing for SARS-CoV-2 with RT-PCR in primary care (REAP-2) EClinicalMedicine. 2021;101011 doi: 10.1016/j.eclinm.2021.101011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martin AF, Denford S, Love N, et al. Engagement with daily testing instead of self-isolating in contacts of confirmed cases of SARS-CoV-2. BMC Public Health. 2021;21 doi: 10.1186/s12889-021-11135-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scientific Advisory Group for Emergencies SAGE 83 minutes: coronavirus (COVID-19) response. 11 March 2021. https://www.gov.uk/government/publications/sage-83-minutes-coronavirus-covid-19-response-11-march-2021
- 12.Smith LE, Potts HWW, Amlôt R, Fear NT, Michie S, Rubin GJ. Adherence to the test, trace, and isolate system in the UK: results from 37 nationally representative surveys. BMJ. 2021;372:n608. doi: 10.1136/bmj.n608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Crawley E, Loades M, Feder G, Logan S, Redwood S, Macleod J. Wider collateral damage to children in the UK because of the social distancing measures designed to reduce the impact of COVID-19 in adults. BMJ Paediatr Open. 2020;4 doi: 10.1136/bmjpo-2020-000701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burgess S, Sievertsen HH. Schools, skills, and learning: the impact of COVID-19 on education. April 1, 2020. https://voxeu.org/article/impact-covid-19-education
- 16.Centre for Education Policy and Equalising Opportunities Briefing note: school absences and pupil achievement. 2021. https://repec-cepeo.ucl.ac.uk/cepeob/cepeobn1.pdf
- 17.Education Endowment Fund School closures rapid evidence assessment. 2020. https://educationendowmentfoundation.org.uk/evidence-summaries/evidence-reviews/school-closures-rapid-evidence-assessment/
- 18.Lee LYW, Rozmanowski S, Pang M, et al. SARS-CoV-2 infectivity by viral load, S gene variants and demographic factors and the utility of lateral flow devices to prevent transmission. Clin Infect Dis. 2021 doi: 10.1093/cid/ciab421. published online May 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ismail SA, Saliba V, Lopez Bernal J, Ramsay ME, Ladhani SN. SARS-CoV-2 infection and transmission in educational settings: a prospective, cross-sectional analysis of infection clusters and outbreaks in England. Lancet Infect Dis. 2021;21:344–353. doi: 10.1016/S1473-3099(20)30882-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Denford S, Yardley L. Feasibility and acceptability of daily testing at school as an alternative to self-isolation following close contact with a confirmed cases of COVID19: a qualitative process analysis (preprint) http://www.hprubse.nihr.ac.uk/EasysiteWeb/getresource.axd?AssetID=90034&servicetype=Attachment [DOI] [PMC free article] [PubMed]
- 21.Department for Education Schools COVID-19 operational guidance. https://www.gov.uk/government/publications/actions-for-schools-during-the-coronavirus-outbreak/schools-covid-19-operational-guidance
- 22.Public Health England Guidance for contacts of people with confirmed coronavirus (COVID-19) infection who do not live with the person. https://www.gov.uk/government/publications/guidance-for-contacts-of-people-with-possible-or-confirmed-coronavirus-covid-19-infection-who-do-not-live-with-the-person/guidance-for-contacts-of-people-with-possible-or-confirmed-coronavirus-covid-19-infection-who-do-not-live-with-the-person
- 23.Department of Health and Social Care Lateral flow device performance data. July 7, 2021. https://www.gov.uk/government/publications/lateral-flow-device-performance-data
- 24.Public Health England SARS-CoV-2 variants of concern and variants under investigation in England, technical briefing 18. July 9, 2021. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1001358/Variants_of_Concern_VOC_Technical_Briefing_18.pdf
- 25.Office for National Statistics COVID-19 schools infection survey round 4, England. March 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/covid19schoolsinfectionsurveyround4england/march2021
- 26.Dinnes J, Deeks JJ, Adriano A, et al. Rapid, point-of-care antigen and molecular-based tests for diagnosis of SARS-CoV-2 infection. Cochrane Database Syst Rev. 2020;8 doi: 10.1002/14651858.CD013705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fernandez-Montero A, Argemi J, Rodríguez JA, Ariño AH, Moreno-Galarraga L. Validation of a rapid antigen test as a screening tool for SARS-CoV-2 infection in asymptomatic populations. Sensitivity, specificity and predictive values. EClinicalMedicine. 2021;37 doi: 10.1016/j.eclinm.2021.100954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lumley SF, Constantinides B, Sanderson N, et al. Enhancing epidemiological investigation of nosocomial SARS-CoV-2 infection with whole genome sequencing: a retrospective cohort study across four hospitals in the UK. medRxiv. 2021 doi: 10.1101/2021.06.28.21259028. published online July 2. (preprint). [DOI] [Google Scholar]
- 29.Meredith LW, Hamilton WL, Warne B, et al. Rapid implementation of SARS-CoV-2 sequencing to investigate cases of health-care associated COVID-19: a prospective genomic surveillance study. Lancet Infect Dis. 2020;20:1263–1271. doi: 10.1016/S1473-3099(20)30562-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eyre DW, Sheppard AE, Madder H, et al. A Candida auris outbreak and its control in an intensive care setting. N Engl J Med. 2018;379:1322–1331. doi: 10.1056/NEJMoa1714373. [DOI] [PubMed] [Google Scholar]
- 31.Price JR, Cole K, Bexley A, et al. Transmission of Staphylococcus aureus between health-care workers, the environment, and patients in an intensive care unit: a longitudinal cohort study based on whole-genome sequencing. Lancet Infect Dis. 2017;17:207–214. doi: 10.1016/S1473-3099(16)30413-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data from the trial will be available within the Office for National Statistics Secure Research Service. Applications for access can be made by accredited researchers. For more details please see https://cy.ons.gov.uk/aboutus/whatwedo/statistics/requestingstatistics/approvedresearcherscheme.