Abstract
The emigration of doctors from Nigeria has been on the increase in recent years, with no obvious efforts to manage or mitigate the negative impacts of this growing trend on the already weak health system. This study assessed the emigration intentions of doctors undergoing residency training at the premier tertiary healthcare center in Nigeria and the factors that influence these intentions. This mixed-method study was cross-sectional in design. A semi-structured questionnaire was used to identify the factors that influence the emigration intentions of resident doctors at the University College Hospital, Ibadan, Southwest Nigeria. In-depth interviews (IDIs) were also conducted to further explore the push and pull factors identified from the survey and their migration preferences. A total of 244 resident doctors completed the questionnaires and 10 participated in the IDIs. Overall, 57.4% of the respondents had emigration intentions and 34.8% had made various attempts at emigrating. Major factors that encouraged resident doctors to emigrate to developed countries included better working and living conditions, good salary and the opportunity for career advancement in destination countries. Family ties was the single most important factor that deterred resident doctors from emigrating. The UK was found to be the top preferred destination. Strategic approaches and multisectoral collaborations will be required to address doctors’ emigration from Nigeria. These efforts should be targeted at not just the health sector but should also include the social and economic aspects of the lives of resident doctors, to improve their living conditions.
Keywords: Emigration, Resident doctors, Push and pull factors, Human resource for health, Policy analysis, Nigeria
Introduction
The migration of healthcare professionals is a concern both in developing and developed countries with its negative impact being felt in the reduced number of workers and skilled professionals in the health workforce (Buchan, 2008). It also affects the quality of health services delivered and overall development goals in developing countries (Tankwanchi, 2012).
Current migration patterns as described by the Global Health Workforce Alliance (2014), uncovers an exponentially expanding movement of doctors from low-income nations to high-income countries. The majority of these low-income countries, for example, Nigeria, do not only have a critical healthcare worker shortage, but bear a significant percentage of the world’s disease burden (WHO, 2017a). The prevailing communicable diseases such as malaria, tuberculosis and HIV/AIDS are aggravated by an expanding frequency of chronic diseases like diabetes and hypertension, thus, making the problem of migration even more serious (WHO, 2017b).
Nigeria is one of the ten most populous countries in the world and the most populous country in Africa, hence, contributing to a large volume of African migrants in developed countries (Isiugo-Abanihe & IOM, 2016). Black et al. (2004), observed that even though the immigration processes have become more tedious and time-consuming, it has not deterred Nigerians from migrating to developed countries. Although there is no comprehensive data on the employment of Nigerians in developed countries, the emigration of skilled Nigerians appears to be high (Isiugo-Abanihe & IOM, 2016).
The World Bank projected that global remittances by the end of 2018 would have grown by 10.3% which amounts to 689 billion US dollars with about 528 billion dollars going to developing countries (KNOMAD, 2018). In Africa, remittance has become one of the most significant sources of capital inflow hence contributing to the economic growth and livelihood of the region and Nigeria tops the list of remittance recipient countries in Sub-Saharan Africa (Isiugo-Abanihe & IOM, 2016; KNOMAD, 2018). This has placed Nigeria as an important source country exporting both unskilled and more importantly skilled and professional labor to the developed countries especially from the healthcare sector (Isiugo-Abanihe & IOM, 2016). The effect of this constant emigration of skilled health professionals is the loss of manpower experienced by the healthcare sector and loss of revenue invested by the government in training these professionals (Clemens, 2011). Another effect of this is an increase in the referral of citizens abroad for medical attention where these skilled doctors have relocated to, resulting in a loss of revenue for the healthcare system (Awases et al., 2004).
Both developed and developing countries have a pressing shortage of nurses and doctors, and quite unfortunately, staff shortages, the lack of specialist training in low-and-middle-income (LMIC) countries and the economic downturn in the West have remained some of the reasons for the migration of doctors who are sourced from the most developing countries to the more developed countries (Bidwell et al., 2013). About 30% of doctors in the four largest English-speaking countries (i.e. the USA, UK, Canada and Australia) are overseas trained and about 40–75% of migrants are from developing countries (Arah et al., 2008).
Background
The migration of doctors to developed countries has been linked to staff and skills shortages in the Nigerian health system (Adeloye et al., 2017). There have also been reports in the media focusing on the increasing emigration of doctors (Abang, 2019; Onyekwere & Egenuka, 2019).
According to the latest statistics, there are about 74,543 doctors on the register of the Medical and Dental Council of Nigeria (MDCN) (Ezigbo, 2020). However, only about half of these doctors practice in the country (Muanya, 2020). Nigeria may need more than 300,000 doctors to meet up the WHO’s recommended doctor-to-patient ratio of 1:600 (Muanya, 2020). The poor human resource for health situation in the country is further worsened by the recent COVID 19 pandemic. At the height of the first wave of the pandemic, 20 doctors lost their lives in 1 week in December, 2020 due to complications of COVID 19 which they contacted in the line of duty (Anadolu Agency, 2020).
Furthermore, since the year 2009, Nigeria has been losing an average of 700 doctors annually to Europe, America, Australia and South Africa. Also, the number of Nigeria trained doctors undergoing residency in the USA has doubled in the last 10 years (Tankwanchi, 2012). Likewise, the number of doctors from Nigeria registered with the General Medical Council (GMC) in the UK has doubled from 2006 to 2016 based on available data on the GMC website (GMC, 2018). Furthermore, an online survey conducted in Nigeria, in 2017, revealed that 9 out of every 10 doctors surveyed were seeking work opportunities abroad (NOIPolls, 2018).
The most recent data provided by the World Health Organization (WHO) shows that Nigeria has about 3.8 doctors per 10,000 population (WHO, 2019) as against the recommended minimum threshold of 23 doctors per 10,000 population. Despite the upward trend in emigration and the documented evidence of the deficiencies in the human resources within the Nigerian health system, it appears that little effort has been made to manage the outflow of doctors. This is evidenced by the report of the recent claim by the Nigerian Minister of Labor and Employment that the country had surplus doctors (Akinkuotu, 2019). Moreover, there is no indication of any strategies to ensure the return of health professionals or any policy to ensure an adequate supply or retention of the health workforce to manage the exodus (Adeloye et al., 2017).
The development of specialist manpower in the medical field for healthcare delivery services is dependent on residency training, including the quality of healthcare and medical research (Esan et al., 2014). In addition to the provision of specialist training at a high level and appropriate to the needs of the Nigerian population, residency training was also established formally in 1974 to reduce the brain drain taking place from the non-return of specialists after being trained abroad (Yusufu et al., 2010).
Resident doctors are important because they form a crucial aspect of the health workforce in most teaching hospitals. In addition, they contribute to the pool of medical specialists and also function in medical student training and teaching. Therefore, this study assessed the emigration intentions of resident doctors at the University College Hospital (UCH), Ibadan, and the factors that influence such intentions.
Methods
Study Design and Setting
The mixed-method study, carried out between August and November 2018, was cross-sectional in design. The quantitative study was conducted first followed by the qualitative aspect of the study. The study population consisted of resident doctors currently in the employment of UCH, Ibadan, southwestern Nigeria.
University College Hospital, Ibadan, is Nigeria’s premier teaching hospital and one of the foremost tertiary hospitals in West Africa and a top choice for specialist healthcare services. The hospital runs residency programs in nearly all specialties of internal medicine, surgery, obstetrics and gynecology, pediatrics, otorhinolaryngology, ophthalmology, anesthesia, radiotherapy, radiology, laboratory medicine, psychiatry, community medicine and, dentistry. The hospital, established in 1952, has about 1000 beds for in-patient care.
Sampling, Data Collection and Analysis
For the quantitative component of the study, stratified random sampling was done to recruit participants from different specializations. Proportional allocation using number of residents and required sample size for each of the specialties was first calculated followed by systematic random sampling for subject selection in each specialty. The sampling frame used was the list of doctors on the payroll of the hospital which was obtained from the Human Resources Department. At the time of the study, there were 465 resident doctors and a minimum sample size of 234 was derived using the Leslie Kish formula (1965).
A semi-structured paper questionnaire modified from previous studies on doctors’ migration (NOIPolls, 2018; Otubu, 2008; Sibasis, 2016) was used to collect data for the quantitative study. Information on sociodemographic variables such as age, gender, marital status, specialty and average monthly income was assessed. The questionnaire was self-administered and it established different factors (such as personal and professional) in a push and pull framework. It contained items in several formats, including Likert type scales and multiple-choice questions. Data entry and analysis was done using SPSS 20. Frequencies, proportions, percentages and, means were generated. Cross-tabulations were done and chi-square test was used to test associations between variables at 5% level of significance.
Participants for the in-depth interviews (IDIs) were recruited via purposive sampling based on availability and willingness to discuss their emigration intentions. Participants were enlisted for the IDIs irrespective of their emigration intentions. The interviews were conducted in English using a guide and they provided in-depth insights, specifically about emigration intentions, the factors influencing these intentions and their preferred emigration destination. Each interview lasted between 30 min and 1 h. Although the interviews were held within the hospital premises, the location and time were determined by respondents. All interviews were conducted by the first author who is a physician, as well as the second author. Interviews were audio-recorded, transcribed and, thematic analysis done using NVIVO 10. Coding was done independently by both authors, these were later compared and merged. Individual interviews were preferable to focus group discussions because it was not practical to form a group of resident doctors, especially as many were from different specialties, involved in emergency duties and had different work schedules. The number of IDIs conducted was based on the principle of saturation (Fusch & Ness, 2015), when no new information is being obtained from respondents. The SRQR guidelines for qualitative studies (O’Brien et al., 2014) were used in developing this manuscript.
The authors were drawn to this particular research by a genuine and personal interest in issues related to doctors’ emigration and by the fact that they, as doctors too, are also affected as they know colleagues who have emigrated.
Ethics
Approval to conduct the study was sought and obtained from the Joint University of Ibadan/University College Hospital, Ibadan Ethical Committee. Informed verbal and written consent was also obtained from all participants in the study. No personal identifiers were used to ensure participants’ anonymity and confidentiality.
Results
Sociodemographic Characteristics of Respondents
There were 244 respondents, 149 (61.1%) of which were males. Slightly more than half (51.6%) were 35 years or older and the mean age was 34.9 ± 3.9 years. More than three-quarters (77.9%) of the respondents were married and about 61% had children. Majority (81.1%) of the resident doctors had spent 5 years or less in the residency training program, while the remaining 18.9% had spent 6 years or more. The average monthly salary of resident doctors in UCH was 300,000 Naira (about US$ 983), with slightly above half (54.9%) of the resident doctors earning < 304,000 Naira (about US$ 996). See Table 1. For the IDI, there were 10 participants; Majority were male (70.0%) and married (80.0%). Most of the participants (70.0%) were Senior registrars and based on their broad category of specialties 4 (40.0%) were from medical specialties, 2 (20.0%) from surgical specialties, 2 (20.0%) from laboratory medicine specialties, 1 (1.0%) from radiology and radiotherapy, and 1 (1.0%) from dentistry. Half of the participants (50.0%) were aged 34 years or older and the mean age was 33.9 ± 2.3 years.
Table 1.
Sociodemographic information of survey respondents (N = 244)
| Variable | Frequency (n) |
Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 149 | 61.1 |
| Female | 95 | 38.9 |
| Age (years) | ||
| ≤ 34 | 118 | 48.4 |
| ≥ 35 | 126 | 51.6 |
| Mean | 34.9 ± 3.9 | |
| Marital status | ||
| Married | 190 | 77.9 |
| Unmarried | 54 | 22.1 |
| Number of children | ||
| None | 96 | 39.3 |
| 1 or more | 148 | 60.7 |
| Number of years spent in residency training | ||
| ≤ 5 | 198 | 81.1 |
| ≥ 6 | 46 | 18.9 |
| Residency specialty | ||
| Surgicala | 79 | 32.4 |
| Medicalb | 98 | 40.1 |
| Laboratoryc | 27 | 11.1 |
| Radiology & radiotherapy | 18 | 7.4 |
| Dentistry | 22 | 9.0 |
| Monthly salary (in Naira) | ||
| ≤ 304,000 | 134 | 54.9 |
| ≥ 305,000 | 110 | 45.1 |
| Median salary | 300,000d | |
aAnaesthesia, Obstetrics and Gyneacology and all other Surgical subspecialties including General Surgery, Orthopaedics, Neurosurgery
bCommunity Medicine, Clinical Pharmacology, Internal Medicine, Family Medicine, Paediatrics and Psychiatry
cHaematology, Medical Microbiology, Chemical Pathology and Histopathology
dAbout US$ 983
Factors Encouraging Emigration
When asked about factors that they perceived encouraged resident doctors to emigrate, most selected better living conditions (93.4%); better working conditions (93.9%) and increased income (91.8%) as important factors. The desire to join family members already abroad as a factor that encouraged emigration was considered important by less than half (43.9%) of the respondents and unimportant by 30.3%. Table 2 below highlights other factors perceived by respondents to encourage the emigration of resident doctors.
Table 2.
Perception of factors likely to encourage resident doctors’ emigration
| Statements | Important | Somewhat important | Unimportant |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Pull factors | |||
| Better working conditions | 229 (93.9) | 4 (1.6) | 11 (4.5) |
| Better living conditions | 228 (93.4) | 8 (3.3) | 8 (3.3) |
| Increased income | 224 (91.8) | 10 (4.1) | 10 (4.1) |
| More advanced technology for patient care | 217 (88.9) | 14 (5.7) | 13 (5.3) |
| Availability of research opportunities | 200 (82.0) | 30 (12.3) | 14 (5.7) |
| Good rapport with senior colleagues—availability of mentorship | 197 (80.7) | 31 (12.7) | 16 (6.6) |
| Opportunity for career advancement e.g. Masters, PhD | 197 (80.7) | 31 (12.7) | 16 (6.6) |
| Job opportunities for family members e.g. spouse | 182 (74.6) | 46 (18.9) | 16 (16.6) |
| Personal desire to live in another country | 147 (60.2) | 56 (23.0) | 41 (16.8) |
| Opportunity for residency training in rare specialties | 139 (56.5) | 49 (20.1) | 57 (23.4) |
| Family desire to live in another country | 138 (56.6) | 60 (24.6) | 46 (18.9) |
| Desire to join family members already abroad | 107 (43.9) | 63 (25.8) | 74 (30.3) |
| Push factors | |||
| Recognition given to residency training done abroad | 187 (76.6) | 31 (12.7) | 26 (10.7) |
| Insecurity (in Nigeria) | 181 (74.2) | 41 (16.8) | 22 (9.0) |
Push and Pull Factors Leading to Resident Doctors’ Emigration
The major factors that were identified by the interview participants that “pushed” resident doctors to emigrate and in the same vein attracted them to the destination countries included remuneration, working and living conditions (Table 3). The general view was that the challenges in the health sector extended to the general population and corruption, with poor political will were some of the challenges pointed out by some of the participants. Our findings also show that some resident doctors plan to relocate to developed countries due to the fear that they might not secure employment after their fellowship training in Nigeria. Similarly, some respondents believe it is better to emigrate early since a fellowship qualification in Nigeria might not confer any additional benefit internationally. However, some residents experienced family pressure to emigrate as shown in the quotes in Table 3.
Table 3.
Push and pull factors influencing emigration of resident doctors
| Quotes | |
|---|---|
| Push factors | |
| Inadequate mentorship | “Another thing is the lack of mentorship and the fact that you are always compared to the experience you get from other people here that they have a good working relationship, there are mentor mentee relationship with their teachers there, we don’t have that here. Your teachers feel like demi-gods. If you have somewhere that you have an easier working relationship you will go” (Dr. H, female, married) |
| Poor relationship with teachers and trainers | |
| Poor work environment | |
| Pressure from family members |
“They (family members) think that I’m shortchanging myself, ‘what are you really doing? What are you really doing in this country?’…” (Dr. H, female, married) “They (family members) are encouraging me, they are pushing me to emigrate” (Dr. I, female, single) |
| Corruption | “The problem that is making all these residents to leave the country is not solely due to the challenges faced within the health sector … let’s say from the government political will, corruption because when we look at it, we can’t take health in isolation, academics the university poorly funded, poorly trained people, people don’t have access to maybe internet, researches, the health facilities there too is there” (Dr. H, female, married.) |
| Poorly funded educational institutions | |
| Poor infrastructures | |
| Fear of unemployment | “Most of the people in training have this fear that there is no job for them after training so they feel ‘the earlier I leave the country the better for me’ or at least write these exams in preparation for leaving the country after the residency training and many are not even concluding their residency training before leaving” (Dr. G, married male) |
| Non-recognition of fellowship qualification internationally | “I was talking to a friend who emigrated last week and he was telling me even our fellowship in Nigeria is worthless, they don’t recognize it, it’s not recognized, it’s just like a waste of time, just as if you waste your time in the country doing all these training so a lot of people just want to travel as early as possible so as to avoid staying this long and venturing into a program that it can only be used in Nigeria” (Dr. C, male, married) |
| Pull factors | |
| Better condition of service | “The thing I believe is driving a lot of people out of the country include there is better condition of service, there is better reward and again there are better chance of them even getting postgraduate training though might not be in a choice field…” (Dr. C, male, married) |
| Renumeration | |
| Training opportunities | |
Factors That May Discourage Emigration Among Resident Doctors
Factors considered likely to discourage resident doctors from emigrating as selected by respondents include the non-recognition of the residency training done in Nigeria by other countries (57.8%); the cost of examinations and other processes involved in emigrating (54.9%) and the uncertainty of securing residency placement in another country (51.6%). Less than half of respondents considered the inability to pass required English exams like the International English Language Testing System (IELTS), Test of English as a Foreign Language (TOEFL) (48.4%) and the ability to adapt to the new culture of another country (41.0%) as unimportant. See Table 4.
Table 4.
Perception of factors likely to discourage resident doctors’ emigration
| Statements | Important | Somewhat important | Unimportant |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Non-recognition of residency training done in Nigeria by other countries | 141 (57.8) | 37 (15.2) | 65 (26.6) |
| Cost of examinations and other processes involved in emigration | 134 (54.9) | 59 (24.2) | 50 (20.5) |
| Uncertainty of securing residency placement in another country | 126 (51.6) | 64 (26.2) | 53 (21.7) |
| Personal desire to live in Nigeria | 125 (51.2) | 60 (24.6) | 59 (24.2) |
| Age | 114 (46.7) | 58 (23.8) | 72 (29.5) |
| Inability to pass licensing examinations e.g. PLAB, USMLE | 108 (44.3) | 53 (21.7) | 82 (33.6) |
| Family desire to live in Nigeria | 106 (43.4) | 58 (23.8) | 80 (32.8) |
| Racism in destination country | 103 (42.2) | 82 (33.6) | 59 (24.2) |
| Children | 102 (41.8) | 54 (22.1) | 88 (36.1) |
| Disconnection from other family members | 97 (39.8) | 76 (31.1) | 71 (29.1) |
| Opportunity to improve the health system of Nigeria | 82 (33.6) | 80 (32.8) | 81 (33.2) |
| Ability to adapt to new culture of another country | 74 (30.3) | 70 (28.7) | 100 (41.0) |
| Inability to pass English Language examinations e.g. IELTS, TOEFL | 74 (30.3) | 51 (20.9) | 118 (48.4) |
| Opportunity to improve Nigerian society | 73 (29.9) | 77 (31.6) | 94 (38.5) |
| Ability to adapt to the weather and terrain of another country | 67 (27.5) | 82 (33.6) | 95 (38.9) |
Participants were also asked about their views on reasons why some residents may decide to stay back in Nigeria. From their responses, possible family ties, the huge cost of emigrating and the presence of racism in the destination countries among others discouraged some resident doctors from emigrating. Also, some resident doctors decided to stay back in the country out of a sense of patriotism and the desire to contribute to society.
However, beyond family ties and a sense of patriotism, another reason given as to why some resident doctors might decide against emigrating included the tedious processes involved in relocating out of the country. Some respondents believed that it might not be prudent to leave the known for the unknown or to truncate their professional progression in the country to start all over elsewhere. Table 5 summarizes these issues with verbatim quotes.
Table 5.
Why some resident doctors might not be interested in emigrating
| Themes | Quotes |
|---|---|
| Family ties | “Majorly many of the doctors in the country now are in the country because of family or because they are trying to raise funds to run away too. There are some that actually have strong family ties, maybe only child of the family” (Dr. C, male, married) |
| Huge cost of emigrating | |
| Patriotism | “When you are at home you already know the rules and regulations, you know what you can do, what you can’t do; there is no issue of racism and it’s your country you know everything and then a number of people still believe in Nigeria, so they believe they have to contribute their quota into the system and well for some others they have family ties, and all that might prevent them from leaving the system” (Dr. I, female, single) |
| Racism in destination countries | |
| Desire to give back to the system | |
| Difficulty with relocating | “I think the most important thing that will make them want to stay back in Nigeria is the difficulty of leaving. Let me explain: if it was quite easy to go a lot of people would have left. The other thing is that some people have in-depth family ties, roots but I really don’t think those are the things that hold people these days. A very few maybe 1–2% of people who believe in patriotism and say they want to stay back to fix the country and there are those who believe that they will be better off here as kings or at the top of their profession than going there to just be lost in the crowd” (Dr. F, male, married) |
| Professional progression |
Emigration Intentions and Preferred Destinations
When asked if they had intentions to emigrate, 140 (57.4%) respondents said yes, 28 (11.5%) said no and 76 (31.1%) were not sure (Fig. 1). Of the 140 respondents that indicated that they had emigration intentions, their top three preferred destinations were the United Kingdom (UK) (45.0%), Canada (26.4%) and the United States of America (USA) (20.0%). See Fig. 2 below.
Fig. 1.
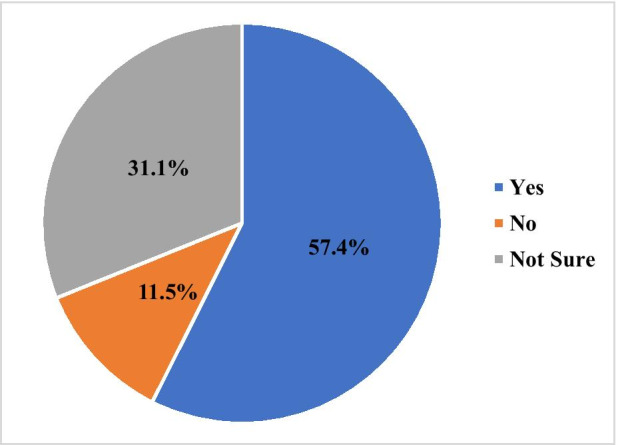
Emigration intentions of resident doctors
Fig. 2.
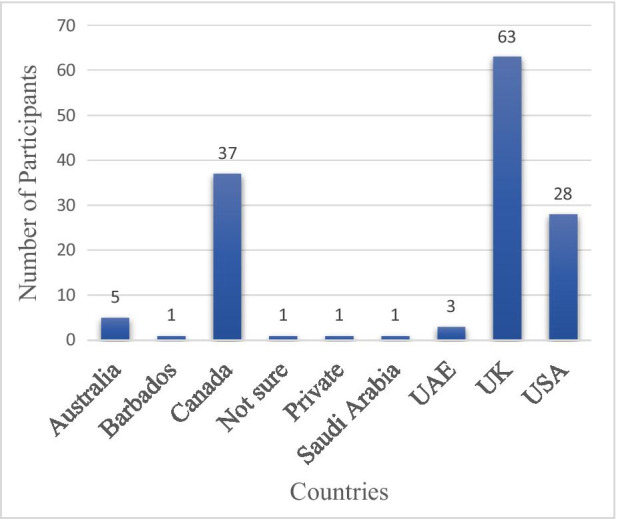
Preferred emigration destinations among UCH resident doctors
The association between emigration intentions and other variables was also explored and there was a relationship between emigration intentions and satisfaction with work environment with a P-value of 0.001 where P-value was set to be significant at < 0.05. See Tables 6 and 7.
Table 6.
Association between emigration intentions and selected sociodemographic information
| Emigration intention | |||||||
|---|---|---|---|---|---|---|---|
| Yes (%) |
No (%) |
Not sure (%) |
Total (%) |
X2 | df | P-value | |
| Gender | |||||||
| Male | 93 (62.4) | 21 (14.1) | 35 (23.5) | 149 (61.1) | 11.185 | 2 | 0.004* |
| Female | 47 (49.5) | 7 (7.4) | 41 (43.2) | 95 (38.9) | |||
| Total (%) | 140 (57.4) | 28 (11.5) | 76 (31.1) | 244 (100.0) | |||
| Age | |||||||
| ≤ 34 | 62 (52.5) | 15 (12.7) | 41 (34.7) | 118 (48.6) | 2.425 | 2 | 0.297 |
| ≥ 35 | 78 (62.4) | 13 (10.4) | 34 (27.2) | 125 (51.4) | |||
| Total (%) | 140 (57.6) | 28 (11.5) | 75 (30.9) | 243 (100.0) | |||
| Religion | |||||||
| Christianity | 128 (59.5) | 21 (9.8) | 66 (30.7) | 215 (88.1) | 10.529 | 6 | 0.104 |
| Islam | 12 (46.2) | 6 (23.1) | 8 (30.8) | 26 (10.7) | |||
| Traditional worshipper | 0 (0.0) | 0 (0.0) | 1 (100.0) | 1 (0.4) | |||
| Others | 0 (100.0) | 1 (50.0) | 1 (50.0) | 2 (0.8) | |||
| Total (%) | 140 (57.4) | 28 (11.5) | 76 (31.1) | 244 (100.0) | |||
| Marital status | |||||||
| Married | 116 (61.1) | 23 (12.1) | 51 (26.8) | 190 (77.9) | 7.428 | 2 | 0.024* |
| Unmarried | 24 (44.4) | 5 (9.3) | 25 (46.3) | 54 (22.1) | |||
| Total (%) | 140 (57.4) | 28 (11.5) | 76 (31.1) | 244 (100.0) | |||
| Number of children | |||||||
| None | 49 (51.0) | 11 (11.5) | 36 (37.5) | 96 (39.3) | 3.158 | 2 | 0.206 |
| 1 or more | 91 (61.5) | 17 (11.5) | 40 (27.0) | 148 (60.7) | |||
| Total (%) | 140 (57.4) | 28 (11.5) | 76 (31.1) | 244 (100.0) | |||
*P-value is significant < 0.05
Table 7.
Association between emigration intentions and selected professional information
| Emigration intention | ||||||||
|---|---|---|---|---|---|---|---|---|
| Yes (%) |
No (%) |
Not sure (%) |
Total (%) |
X2 | df | P-value | ||
| Years post medical school graduation | ||||||||
| ≤ 5 | 16 (59.3) | 4 (14.8) | 7 (25.9) | 27 (11.1) | 1.712 | 4 | 0.788 | |
| 6–10 | 91 (55.5) | 20 (12.2) | 53 (32.3) | 164 (67.2) | ||||
| ≥ 11 | 33 (62.3) | 4 (7.5) | 16 (30.2) | 53 (21.7) | ||||
| Total (%) | 140 (57.4) | 28 (11.5) | 76 (31.1) | 244 (100.0) | ||||
| Years in residency training | ||||||||
| ≤ 5 | 112 (56.9) | 23 (11.7) | 62 (31.5) | 197 (81.1) | 0.056 | 2 | 0.972 | |
| ≥ 6 | 27 (58.7) | 5 (10.9) | 14 (30.4) | 46 (18.9) | ||||
| Total (%) | 139 (57.2) | 28 (11.5) | 76 (31.1) | 243 (100.0) | ||||
| Residency specialty | ||||||||
| Anaesthesia | 12 (70.6) | 1 (5.9) | 4 (23.5) | 17 (7.0) | 27.886 | 22 | 0.180 | |
| Clinical pharmacology | 2 (100.0) | 0 (0.0) | 0 (0.0) | 2 (0.8) | ||||
| Community medicine | 8 (44.4) | 5 (27.8) | 5 (27.8) | 18 (7.4) | ||||
| Dentistry | 14 (63.8) | 1 (4.5) | 7 (31.8) | 22 (9.0) | ||||
| Family medicine | 11 (55.0) | 2 (10.0) | 7 (35.0) | 20 (8.2) | ||||
| Internal medicine | 12 (50.0) | 1 (4.2) | 11 (45.8) | 24 (9.8) | ||||
| Obstetrics and gynaecology | 7 (58.3) | 2 (16.7) | 3 (25.0) | 12 (4.9) | ||||
| Paediatrics | 9 (42.9) | 4 (19.0) | 8 (38.1) | 21 (8.6) | ||||
| Pathology | 12 (44.4) | 2 (7.4) | 13 (48.1) | 27 (11.1) | ||||
| Psychiatry | 7 (53.8) | 0 (0.0) | 6 (46.2) | 13 (5.3) | ||||
| Radiology and radiotherapy | 12 (66.7) | 4 (22.2) | 2 (11.1) | 18 (7.4) | ||||
| Surgery | 34 (68.0) | 6 (12.0) | 10 (20.0) | 50 (20.5) | ||||
| Total (%) | 140 (57.4) | 28 (11.5) | 76 (31.1) | 244 (100.0) | ||||
| Monthly salary (in Naira) | ||||||||
| ≤ 304,000 | 77 (57.5) | 16 (11.9) | 41 (30.6) | 134 (54.9) | 0.085 | 2 | 0.958 | |
| ≥ 305,000 | 63 (57.3) | 12 (10.9) | 35 (31.8) | 110 (45.1) | ||||
| Total (%) | 140 (57.4) | 28 (11.5) | 76 (31.1) | 244 (100.0) | ||||
| Satisfied with work environment | ||||||||
| Yes | 12 (31.6) | 11 (28.9) | 15 (39.5) | 38 (15.6) | 20.876 | 4 | 0.001* | |
| No | 110 (63.2) | 16 (9.2) | 48 (27.6) | 174 (71.6) | ||||
| Indifferent | 17 (54.8) | 1 (3.2) | 13 (41.9) | 31 (12.8) | ||||
| Total (%) | 139 (57.2) | 28 (11.5) | 76 (31.1) | 243 (100.0) | ||||
*P-value is significant at < 0.05
The interview participants also listed the UK as their most preferred emigration destination due to the affordable cost of emigration. They also claimed that it was easier to use the UK as a stepping stone to other preferred destinations like Canada. The US ranked low on their choice destinations due to the cost and perceived difficulty in passing the licensing examinations. Some of the participants responded thus:
As it is today it’s not very easy to actually emigrate to US because of the rigor of the exams, finance involved. Thus, if you meet an average Nigerian doctor emigrating the choice is actually UK. It's faster cheaper and again he can use it as a stepping stone for better placement later. If you are in UK you can start writing your licensing board exam all those things, you can even work towards moving to Canada of which Canada has better condition than UK, but UK affords you the opportunity to start to gain experience while making money and that is far far far better than Nigeria (Dr. C, male, married).
I think it’s easier for me to go to the UK. I would love to be in America for example also but it is easier to go to UK, there are many channels through which you can go to UK that is why. The remuneration there are not as high as in the US obviously or even some other parts of the western world but it is easier, the exams are easier and cheaper compared to USMLE for example. (Dr. G, male, married).
Close to three-quarters (71.3%) of the respondents reported that they were not satisfied with their work environment (Fig. 3), while only 15.6% of the respondents indicated that they were satisfied and 12.7% responded as indifferent.
Fig. 3.
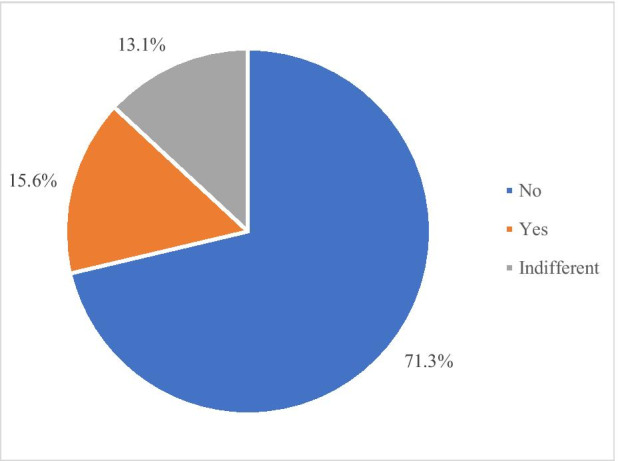
Respondents’ satisfaction with work environment
Discussion
More than half of the respondents had emigration intentions and about a third of those with emigration intentions had made various attempts at emigrating ranging from taking tests of English language to writing licensing exams. This finding is similar to those of the NOIPolls (2018), where 88.0% of the Nigerian doctors who responded to the web survey were considering work opportunities abroad. However, the lower proportion reported in this study may be explained by the difference in the study population as the NOIPolls (2018) sampled various categories of Nigerian doctors whereas this study was conducted only among doctors undergoing residency training.
Better income, improved working conditions and enhanced living conditions were the top factors listed by respondents that attracted them to destination countries and encouraged them to emigrate. This is in keeping with findings by previous studies (NOIPolls, 2018; Otubu, 2008). The interview findings also established the role of financial factors (poor remuneration) in influencing the emigration intentions of resident doctors. This confirms findings by previous studies in Nigeria as well as other developing countries. For example, the NOIPolls (2018) revealed that 91.0% of the Nigerian doctors who participated in their web survey listed poor salaries and emoluments as a major challenge faced by doctors in Nigeria which encouraged them to emigrate. In addition, a five-country study carried out by Astor et al. (2005) in Colombia, Nigeria, India, Pakistan and the Philippines revealed that poor salary was reported as the most influential factor promoting international migration by about 91% of the participating doctors. Another study conducted by the WHO found that poor income played a dominant role in motivating health workers in the African region to migrate overseas (Awases et al., 2004).
More than half of the respondents in this study earn below US$1000 (≤ 304,000 Naira) per month with an average annual salary of about 3.9 million Naira, which is equivalent to US$12,700 or £9800 based on the current official exchange rate from the Central Bank of Nigeria (CBN) (2019) at the time of this study. However, their counterparts in the UK earn up to £36,000 or more annually (BDI Resourcing, 2018), while those in the USA earn an average of US$59,000 annually (Levy, 2018). Although the cost of living and the economic situation vary, there is an obvious discrepancy in these values which might explain why the UK and the USA are choice destination countries of respondents as well as resident doctors they know to have emigrated.
Other reasons that were adduced for the emigration of resident doctors which have been confirmed by previous studies among doctors in Nigeria include insecurity, availability of opportunity for career advancement, research opportunities and more advanced technology for patient care in destination countries (Hagopian et al., 2005; NOIPolls, 2018; Otubu, 2008; Tankwanchi, 2012).
This study also found that majority of the respondents expressed dissatisfaction with their work environment and an important association was found between emigration intention and satisfaction with work environment. About three-quarters of the respondents agreed that they had enormous workload, which can be linked to the prevailing shortage of doctors already being experienced in Nigeria with a low doctor–patient ratio reported by the WHO (2019). Similar results were found by Esan et al. (2014) in their study conducted to assess psychological distress among resident doctors at the same study site; more than half of the respondents described the intensity of their work as heavy or excessive.
An important push factor identified by this study is the non-recognition of the residency training done in Nigeria by developed countries. Majority of the respondents listed the recognition of residency training done abroad as one of the factors that encouraged resident doctors to emigrate. In contrast, this factor also served to discourage some residents from emigrating as they would have to start residency training all over again in their destination countries. This might explain why some of the interview participants said resident doctors were emigrating without completing their training program in Nigeria, which they viewed as a waste of time. This confirms the submission by Okonofua (2018) in his analysis of the residency training program in Nigeria. He identified that the degrees offered by both the National Postgraduate Medical College of Nigeria (NPMCN) and the West African Postgraduate Medical College (WAPMC) on the completion of the residency program were neither accredited nor recognized in developed countries and this would continue to pose a challenge to the Nigerian healthcare system. In contrast, a previous study showed that the inability to secure a placement for residency training was listed as a reason for emigrating among doctors who were yet to commence residency training (NOIPolls, 2018). It can, therefore, be concluded that getting a residency placement in Nigeria alone, will not prevent doctors from emigrating.
This study also explored factors that might deter resident doctors from emigrating and the presence of family ties was identified in the interviews as one of the most important reasons why some resident doctors have decided not to emigrate. This is corroborated by Tankwanchi (2012) and Sibasis (2016), where interview participants expressed that family ties and responsibilities to members of their extended family such as aged parents were part of their reasons for not emigrating. However, this study also identified that family ties was a factor that might encourage resident doctors to emigrate. Majority of the respondents considered the availability of job opportunities for their family members in destination countries as an important factor likely to encourage emigration. In addition, some interview participants reported that their family members encouraged them to emigrate. This is similar to the findings by Sibasis (2016), where respondents also reported that their concerns for the future of their immediate family members, especially their children and spouse and the encouragement received from family and friends were part of the reasons they intended to emigrate. Therefore, family ties can be seen as a factor that can both encourage or deter doctors from emigrating.
The UK was the most preferred emigration destination of respondents both for the survey and interviews. This corroborates the findings by NOIPolls where 93.0% of the respondents listed the UK as a known destination for Nigerian doctors seeking work opportunities abroad. The reason for this choice was explored during the interviews and participants generally agreed that the cost of emigrating to the UK in terms of examination fees and other expenses was more affordable compared to other countries. Another plausible explanation might be that the medical school and training curriculum was primarily tailored towards that of the UK which may make it easier for doctors from Nigeria to adapt quickly to the system over there (Malu, 2010).
Limitations of the Study
Data for this study were obtained from resident doctors only. Key informant interviews with administrative and management level cadres may have provided additional information from the perspective of managers on possible strategies or efforts to address the emigration of resident doctors. However, this study provides important data from the key stakeholders in the doctors’ emigration issue which may help policymakers and health system managers better respond to the challenge. In addition, UCH is just one tertiary center in Nigeria and results from it may not be reflective of the intentions of all resident doctors in the country.
Conclusion
The emigration of resident doctors from Nigeria portends a serious problem in the Nigerian healthcare system. This is not just because Nigeria already has a shortage of physicians and poor health statistics but it may result in a shortage of specialists which may force Nigerians to seek specialist healthcare outside the country. Although both push and pull factors were identified, it appears that the push factors were more central. Certainly, pull factors exert their influence and need to be addressed, but it seems logical that Nigerian resident doctors would be less likely to emigrate if they were comfortable in their home country.
Resident doctors in this survey cited poor work and living conditions and a desire for increased income as major push factors. For these problems to be addressed, the government will need to invest more in the health system as well as basic infrastructure and build a more equitable and egalitarian society. Policymakers and health system managers should also be mindful of creating a conducive work environment, providing equitable remuneration given the context and other non-monetary motivation.
Acknowledgements
This research was made possible by a grant to the first author from the Embassy of France in Nigeria and Institut Français de Recherche en Afrique (IFRA) in Nigeria. The funders however did not have any role in conceptualization of the research, design, data collection or in the manuscript writing.
Funding
Funding was provided by Council for the Development of Social Science Research in Africa (SN).
Declarations
Conflict of interest
The authors hereby declare that there are no conflicts of interest in this study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Abang, M. (2019). Nigeria’s medical brain drain: Healthcare woes as doctors flee. https://www.aljazeera.com/indepth/features/nigeria-medical-brain-drain-healthcare-woes-doctors-flee-190407210251424.html
- Adeloye, D., David, R. A., Olaogun, A. A., Auta, A., Adesokan, A., Gadanya, M., … Iseolorunkanmi, A. (2017). Health workforce and governance: the crisis in Nigeria. Human Resources for Health, 15(1), 32. 10.1186/s12960-017-0205-4 [DOI] [PMC free article] [PubMed]
- Akinkuotu, E. (2019). Doctors free to leave Nigeria, we have enough—Ngige. The Punch Newspaper. Retrieved from https://punchng.com/doctors-free-to-leave-nigeria-we-have-enough-ngige/
- Anadolu Agency. (2020). 20 Nigerian doctors die in one week from COVID-19. Africa, Latest on Coronavirus Outbreak. Retrieved from https://www.aa.com.tr/en/africa/20-nigerian-doctors-die-in-one-week-from-covid-19/2089037
- Arah OA, Ogbu UC, Okeke CE. Too poor to leave, too rich to stay: Developmental and global health correlates of physician migration to the United States, Canada, Australia, and the United Kingdom. American Journal of Public Health. 2008;98(1):148–154. doi: 10.2105/AJPH.2006.095844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Astor A, Akhtar T, Matallana MA, Muthuswamy V, Olowu FA, Tallo V, Lie RK. Physician migration: Views from professionals in Colombia, Nigeria, India, Pakistan and the Philippines. Social Science & Medicine. 2005;61(12):2492–2500. doi: 10.1016/j.socscimed.2005.05.003. [DOI] [PubMed] [Google Scholar]
- Awases, M., Gbary, A., Nyoni, J., & Chatora, R. (2004). Migration of Health Professionals in Six Countries: A Synthesis Report. Retrieved from https://www.afro.who.int/sites/default/files/2017-06/hrh%20migration_en.pdf
- BDI Resourcing. (2018). A doctor’s pay within the NHS. Retrieved from https://bdiresourcing.com/news/a-doctors-pay-within-the-nhs/119
- Bidwell P, Humphries N, Dicker P, Thomas S, Normand C, Brugha R. The national and international implications of a decade of doctor migration in the Irish context. Health Policy. 2013;110(1):29–38. doi: 10.1016/j.healthpol.2012.10.002. [DOI] [PubMed] [Google Scholar]
- Black, R., Ammassari, S., Mouillesseaux, S., & Rajkotia, R. (2004). Migration and Pro-Poor Policy in West Africa. Retrieved from http://www.sussex.ac.uk/Units/SCMR/drc/publications/working_papers/WP-C8.pdf
- Buchan, J. (2008). How can the migration of health service professionals be managed so as to reduce any negative effects on supply? [Policy brief]. Retrieved from https://www.euro.who.int/__data/assets/pdf_file/0006/75453/E93414.pdf
- CBN. (2019). CBN Exchange Rates. Retrieved from https://www.cbn.gov.ng/rates/ExchRateByCurrency.asp
- Clemens MA. The financial consequences of high-skill emigration: Lessons from African doctors abroad. In: Plaza S, Dilip R, editors. Diaspora for development in Africa. The World Bank; 2011. pp. 165–182. [Google Scholar]
- Esan, O., Adeoye, A., Onakoya, P., Opeodu, O., Owonikoko, K., Olulana, D., … Idowu, O. (2014). Features of residency training and psychological distress among residents in a Nigerian teaching hospital. South African Journal of Psychiatry, 20(2), 46–50.
- Ezigbo, O. (2020, 4 March). Population of Doctors in Nigeria Hits 74,543. This Day. Retrieved from https://www.thisdaylive.com/index.php/2020/03/04/population-of-doctors-in-nigeria-hits-74543/#
- Fusch PI, Ness LR. Are we there yet? Data saturation in qualitative research. The Qualitative Report. 2015;20(9):1408. [Google Scholar]
- GHWA. (2014). The Global Health Workforce Alliance 2013 Annual Report: Rising to the grand challenge of human resources for health. Retrieved from https://www.who.int/workforcealliance/knowledge/resources/ghwa_anual_report_2013.pdf?ua=1
- GMC. (2018). The medical register over time. Retrieved 18/02/2019, from General Medical Council, UK. https://data.gmc-uk.org/gmcdata/home/#/reports/The%20Register/Stats/report
- Hagopian A, Ofosu A, Fatusi A, Biritwum R, Essel A, Gary Hart L, Watts C. The flight of physicians from West Africa: Views of African physicians and implications for policy. Social Science & Medicine. 2005;61(8):1750–1760. doi: 10.1016/j.socscimed.2005.03.027. [DOI] [PubMed] [Google Scholar]
- Isiugo-Abanihe, U. C., & IOM. (2016). Migration in Nigeria: A country profile 2014. Retrieved from https://publications.iom.int/system/files/pdf/mp_nigeria.pdf
- Kish L. Survey sampling. Willey; 1965. [Google Scholar]
- KNOMAD. (2018). Migration and Remittances: Recent Developments and Outlook Migration and Development Brief 30. Retrieved from https://www.knomad.org/sites/default/files/2018-12/Migration%20and%20Development%20Brief%2030.pdf
- Levy, S. (2018). Medscape Residents Salary & Debt Report 2018. Retrieved from https://www.medscape.com/slideshow/2018-residents-salary-debt-report-6010044
- Malu A. Universities and medical education in Nigeria. Nigeria Medical Journal. 2010;51(2):84–88. [Google Scholar]
- Muanya, C. (2020, 24 September). Nigerian medical doctors among least paid globally. The Guardian. Retrieved from https://guardian.ng/news/nigerian-medical-doctors-among-least-paid-globally/
- NOIPolls. (2018). Emigration of Nigerian Medical Doctors. Retrieved from https://noi-polls.com/2018/wp-content/uploads/2019/06/Emigration-of-Doctors-Press-Release-July-2018-Survey-Report.pdf
- O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: A synthesis of recommendations. Academic Medicine. 2014;89(9):1245–1251. doi: 10.1097/ACM.0000000000000388. [DOI] [PubMed] [Google Scholar]
- Okonofua FE. Postgraduate medical education in Nigeria: Past, present, and future. Tropical Journal of Obstetrics Gynaecology. 2018;35(1):1–13. doi: 10.4103/TJOG.TJOG_54_16. [DOI] [Google Scholar]
- Onyekwere, J., & Egenuka, N. (2019). Nigeria groans as medical professionals’ emigration worsens. Guardian Newspapers. Retrieved from https://guardian.ng/news/nigeria-groans-as-medical-professionals-emigration-worsens/
- Otubu, O. (2008). Physician Migration from Nigeria: A Look at the Influential Factors and Suggested Policy Options (Master's Dissertation). (Master of Public Health), University of North Carolina, Chapel Hill. Retrieved from https://cdr.lib.unc.edu/concern/masters_papers/bc386n56b
- Sibasis, H. (2016). Intention to Migrate to Australia: a Mixed-Method Study of Indian Physicians and Nurses (Doctoral Dissertation). (Doctor of Philosophy), Queensland University of Technology, Australia.
- Tankwanchi, S. (2012). Doctors beyond borders: Data trends and medical migration dynamics from Sub-Saharan Africa to the United States (Doctoral Dissertation). (Doctor of Philosophy), Vanderbilt University, Nashville.
- WHO. (2017a). Achieving the health-related MDGs. It takes a workforce! Retrieved from https://www.who.int/hrh/workforce_mdgs/en/
- WHO. (2017b). World Health Statistics 2017: Monitoring Health for the Sdgs, Sustainable Development Goals . Geneva: World Health Organization; 2017. Retrieved from http://apps.who.int/iris/bitstream/10665/255336/1/9789241565486-eng.pdf?ua=1
- WHO. (2019). Global Health Observatory Data Repository. Retrieved from http://apps.who.int/gho/data/node.country.country-NG
- Yusufu LMD, Ahmed A, Odigie VI, Delia IZ, Mohammed AA. Residency training program: Perceptions of residents. Annals of African Medicine. 2010;9(2):91. doi: 10.4103/1596-3519.64745. [DOI] [PubMed] [Google Scholar]


