Abstract
Paracaecal hernia is a rare type of internal hernia usually presenting with a picture of small bowel obstruction. In this report we present a 68-year-old woman who was admitted with colicky lower abdominal pain, vomiting and abdominal distention. A computed tomography scan of her abdomen and pelvis demonstrated multiple dilated small bowel loops with a transition point in the right iliac fossa. After a trial of conservative treatment, the patient was taken to theatre where she underwent laparoscopic reduction of a strangulated paracaecal hernia. The patient had an uneventful post-operative recovery and was discharged home.
Despite being a rare cause for small intestinal obstruction, this should be part of the differential diagnosis especially in the absence of previous abdominal operations. Early recognition and prompt surgical treatment is the key to prevent complications. A laparoscopic approach is feasible if expertise is available.
INTRODUCTION
Paracaecal hernia is a rare cause of small bowel obstruction and it accounts for ~0.1% to 6.6% of all internal herniae [1]. Patients usually present with a picture of small bowel obstruction, with colicky abdominal pain, bilious vomiting and constipation. A computed tomography (CT) scan with contrast is the diagnostic modality of choice, however in most cases the definitive diagnosis is made intraoperatively. Surgery is the mainstay of treatment, using either an open or minimally invasive laparoscopic approach. To our knowledge, in the literature, there are only 11 reported cases that have been managed laparoscopically [2].
CASE REPORT
A 68-year-old woman presented to the surgical assessment unit with a 1-day history of colicky lower abdominal pain, distention and vomiting. She had a background of diverticular disease, and no previous abdominal surgery. On examination, her initial observations were normal, she was mildly dehydrated, tender over the right lower quadrant of her abdomen with mild abdominal distension. Admission blood tests showed leucocytosis (WBC 15.9), but the remainder was otherwise within normal limits. Initial differential diagnoses were appendicitis and diverticulitis. Contrast-enhanced CT of the abdomen and pelvis (Fig. 1) showed a small bowel obstruction, with multiple dilated small bowel loops in the pelvis and a transition point in the right iliac fossa. Initial management with NG tube, intravenous fluid and bowel rest was started. The patient underwent a diagnostic laparoscopy on the assumption that this could be a congenital band adhesion. Intraoperatively, a loop of terminal ileum was entrapped in the lateral paracaecal recess (Fig. 2). This recess was opened with laparoscopic scissors to release the entrapped segment. The released small bowel loop appeared viable on intraoperative assessment, so no resection was needed (Fig. 3). The recess was then opened completely along the ascending colon by dividing the lateral peritoneal reflection to prevent recurrence. Post-operatively, the patient recovered uneventfully, and she was discharged on day four.
Figure 1 .
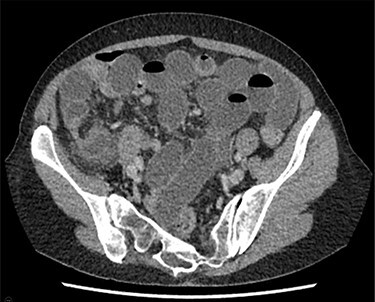
CTAP showing multiple loops of dilated small bowel with transition point in the right iliac fossa.
Figure 2 .

Paracaecal recess with a loop of obstructed small bowel trapped within.
Figure 3 .

Bruised but viable released small bowel loop.
DISCUSSION
Paracaecal hernia has been reported in the literature since the 1950s [3]. It is a rare type of internal hernia that can cause small bowel obstruction and should be diagnosed promptly to prevent complications. It accounts for only 0.1 to 6.6% of all internal herniae [1]. Internal herniae are either naturally occurring (congenital or acquired) or iatrogenic and can be classified into six types: para- duodenal, foramen of Winslow, paracaecal, inter-sigmoid, trans-mesenteric or trans-mesocolic and retro-anastomotic accounting for almost 0.5–3% of all cases of intestinal obstruction [4].
There are currently two main classification systems for paracaecal herniae published in the literature. Meyer et al. [1] classify paracaecal herniae into four subtypes: internal, retrocecal recess, lateral and unclassifiable (caecal recess type).
Endo et al.’s [5] classification system, used in Japan and North America, includes four subtypes: superior ileocecal, inferior ileocecal, appendicular fossa and retrocecal recess (in which the superior and inferior ileocecal types are equivalent to the internal type in Meyer’s classification).
The anatomy of the caecal and paracaecal peritoneum is the end result of ileocecal migration that occurs during rotation of the midgut in the fifth month of gestation. At that stage, four distinct peritoneal recesses of various depths occur in the paracaecal area, namely the superior and inferior ileocecal recess, retrocecal recess and paracolic sulci, all of which may become hernial orifices [6]. This is one of the embryology-anatomy theories behind the development of this hernia.
Yokota et al. [2] performed a PubMed search of the literature published from January 1980 to August 2019 using the keywords ‘paracaecal hernia’, ‘retrocecal hernia’, ‘pericaecal hernia’ and ‘ileocecal hernia’, identifying 27 English language reports, describing 33 surgical cases of paracaecal hernias. The data from these cases are summarized in Table 1. The most common variant was the lateral one, as in our case and most of the patients had had no previous operations.
Table 1.
Summary of the data collected by Yokota et al. [2].
| Total number of cases (33) | |
|---|---|
| Age | <60 (20) |
| ≥60 (13) | |
| Sex | |
| Male | 15 |
| Female | 18 |
| Previous abdominal operation | |
| 1-Yes | 5 |
| 2-No | 21 |
| 3-Not known | 7 |
| Type | |
| 1-Retrocæcal | 8 |
| 2-Lateral | 17 |
| 3-Internal | 3 |
| 4-Unclassifiable | 5 |
| Approach | |
| 1-Laparoscopic | 11 |
| 2-Laparotomy | 22 |
| Bowel resection | |
| 1-Yes | 5 |
| 2-No | 28 |
| Hernial orifice management | |
| 1-Closed | 11 |
| 2-Opened widely | 13 |
| 3-N/A | 7 |
| 4-Ileocæcal resection | 2 |
Usually the presentation is a typical picture of small bowel obstruction with abdominal pain, bilious vomiting and constipation [2, 7]. Those symptoms are not specifically diagnostic or pathognomonic for paracaecal hernia and the definitive diagnosis is usually confirmed radiologically or intraoperatively.
Some patients may develop a closed loop small bowel obstruction and can develop complications quickly if not diagnosed promptly and treated in a timely manner.
Some fatal cases of paracaecal hernia have been reported, therefore surgery must be performed expeditiously if small bowel strangulation is suspected [8].
CT is the diagnostic modality of choice, however most of the time the definite diagnosis is only made intraoperatively [9, 10]. Direction of caecal shift may give an indication of the type of the paracaecal hernia, for example it will be shifted anteriorly in a retrocaecal type or laterally in an internal type (inferior and superior ileocaecal type) [2, 11]. In our case, the caecum was mobilized and displaced medially as the hernia was of the lateral variant.
Surgery is the only treatment option to resolve the small bowel obstruction and to prevent the complication and consequences. The surgical approach is either open or laparoscopic, depending on patient presentation and surgeon preference/expertise [12].
The surgical management follows the principles of managing any hernia, dealing first with the entrapped bowel, having released it from the hernial orifice. The controversial part is how to deal with the hernial orifice or recess as there is no consensus about which is better, closing it or opening it widely, which we did in our case [2].
In conclusion, this case report highlights paracaecal hernia as a rare cause for small bowel obstruction, outlining the classification systems available and treatment options. In particular, this case report demonstrated that this can be successfully managed with laparoscopic surgery.
CONFLICT OF INTEREST STATEMENT
Authors have no conflict of interest to declare.
Contributor Information
Mahmoud Al-Ardah, Department of General Surgery, Royal Cornwall Hospital, Cornwall, UK.
Heena Sisodia, Department of General Surgery, Royal Cornwall Hospital, Cornwall, UK.
Hannah Rottenburg, Department of General Surgery, Royal Cornwall Hospital, Cornwall, UK.
Michael Clarke, Department of General Surgery, Royal Cornwall Hospital, Cornwall, UK.
References
- 1.Meyers MA. Internal abdominal hernias. In: Meyers MA (ed). Dynamic radiology of the abdomen, Vol. 5. New York: Springer, 2000, 711–48. [Google Scholar]
- 2.Yokota T, Otani K, Yoshida J, et al. Paracecal hernia due to membranous adhesion of the omentum to the right paracolic gutter. Surg Case Rep 2019;5:183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tidler HS, Miller JM. Retrocecal Hernia. Am J Surg 1957;94:829–31. [DOI] [PubMed] [Google Scholar]
- 4.Rivkind AI, Shiloni E, Muggia-Sullam M, Weiss Y, Lax E, Freund HR. Paracecal hernia: a cause of intestinal obstruction. Dis Colon Rectum 1986;29:752–4. [DOI] [PubMed] [Google Scholar]
- 5.Endo T. Kimoto S supervised. Gendai-gekagakutaikei, Vol. 34. Tokyo: Nakayama Shoten, 1993, 92–3 (in Japanese). [Google Scholar]
- 6.Hirokawa T, Hayakawa T, Tanaka M, Okada Y, Sawai H, Takeyama H, et al. Laparoscopic surgery for diagnosis and treatment of bowel obstruction: case report of paracecal hernia. Med Sci Monit 2007;13:CS79–82. [PubMed] [Google Scholar]
- 7.Otani H, Makihara S. Laparoscopic Surgery for Small Bowel Obstruction due to Paracecal Hernia. Acta Med Okayama 2018;72:81–4. [DOI] [PubMed] [Google Scholar]
- 8.Zimmerman LM, Laufman H. Intraabdominal hernias due to developmental and rotational anomalies. Ann Surg 1953;138:82–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jang EJ, Cho SH, Kim DD. A case of small bowel obstruction due to a paracecal hernia. J Korean Soc Coloproctol 2011;27:41–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Osadchy A, Keidar A, Zissin R. Small bowel obstruction due to a paracecal hernia: computerized tomography diagnosis. Emerg Radiol 2005;11:239–41. [DOI] [PubMed] [Google Scholar]
- 11.Suyama M, Yasuno M, Takahashi H, Wakayama T. A case report of lateral paracecal hernia. Journal of Japan Surgical Association 2013;74:833–7. [Google Scholar]
- 12.Inukai K, Tsuji E, Uehara S. Paracecal hernia with intestinal ischemia treated with laparoscopic assisted surgery. Int J Surg Case Rep 2018;44:20–3. [DOI] [PMC free article] [PubMed] [Google Scholar]


