Abstract
Reformulating severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccines with variant strains is being pursued to combat the global surge in infections. We hypothesize that this may be suboptimal due to immune imprinting from earlier vaccination or infection with the original SARS-CoV-2 strain. New strategies may be needed to improve efficacy of SARS-CoV-2 variant vaccines.
The problem of SARS-CoV-2 variants
Neutralizing antibodies correlate with protective immunity for first generation vaccines against SARS-CoV-2 (see Glossary) [1]. The viral Spike protein is the primary target for neutralizing antibodies and the principal antigen in most vaccines to date. SARS-CoV-2 infection can be prevented in animal models and humans with neutralizing antibodies [2]. Infection or immunization induce a remarkably robust antibody response in which such immunoglobulins bind a range of epitopes specific to Spike. However, most of these antibodies are nonneutralizing, with only a small fraction of recovered monoclonal antibodies effectively neutralizing SARS-CoV-2 [3]. Although both nonneutralizing antibodies (including those with Fc-mediated functions) and T cells play an important role in control of many viral infections, including SARS-CoV-2, effective protection from SARS-CoV-2 appears primarily driven by neutralizing antibodies [1].
Several SARS-CoV-2 variants of concern (VOC) harboring mutations in the receptor binding domain (RBD) have emerged that efficiently escape the neutralizing antibody response raised by infection or by currently approved vaccines [4]. Existing vaccines have lower efficacy in preventing infection with newer or emerging escape variants that suffer neutralization deficits, most notably Beta and Delta variants. Thus, vaccine manufacturers are updating first generation vaccines by replacing the original Spike with the sequence from one or more new variants.
This updated vaccine strategy is logical and rapid as it takes advantage of existing vaccine technologies. Early results suggest this may well be at least partially effective, with an updated mRNA booster vaccine (Moderna) expressing Beta Spike eliciting neutralization against this variant in preprimed individuals [5]. However, boosting with the Beta variant vaccine in the preprimed group resulted in better neutralization of the ancestral SARS-CoV-2 strain than the Beta strain. This suggests that immune imprinting of the response may have occurred. Immune imprinting is a phenomenon whereby initial exposure to one virus strain effectively primes B cell memory and limits the development of memory B cells and neutralizing antibodies against new minor variant strains of the virus [6]. We hypothesize that repeatedly updating SARS-CoV-2 vaccines might not be fully effective because of limitations imposed by prior immune imprinting to ancestral SARS-CoV-2 strains. Although it is hoped that immune imprinting will not be a major problem for SARS-CoV-2 infections, the possibility that immune imprinting will substantially reduce efficacy of future SARS-CoV-2 vaccines requires action now to both define the extent of the problem and begin to devise solutions.
Immune imprinting in influenza virus infection
Imprinting has been widely studied in influenza A virus (IAV) infections. Each year, seasonal infections with circulating IAVs occur, despite widespread prior infection or vaccination. Accumulated mutations in circulating viruses over time result in escape from neutralizing antibodies (antigenic drift), increasing population level susceptibility [7]. While overall IAV vaccine effectiveness is around 60%, effectiveness against the A(H3N2) IAV subtype is only around 33% in seasons in which the vaccine and circulating strain are well-matched antigenically and around 23% in seasons when strains are not well matched [7]. Antigenic drift has been greater among A(H3N2) IAV compared with A(H1N1) IAV and influenza B viruses and, furthermore, vaccination induces substantial ‘back-boosting’ of antibodies against previously circulating A(H3N2) viruses [8]. IAV vaccines recall memory responses against well-conserved epitopes between the vaccine and past strains but are less effective in generating durable new neutralizing antibodies against variant epitopes of the antigenically drifted viral strain [8]. Consequently, the immune response becomes ‘imprinted’ against previous strains, limiting robust neutralizing responses to new strains.
Risks of immune imprinting undermining SARS-CoV-2 vaccine efficacy
Similar to antigenically drifted IAV, SARS-CoV-2 neutralization escape variants have only a few key mutations at neutralization epitopes compared with the ancestral strain [4]. Most antibody responses to Spike are directed against conserved, nonneutralizing epitopes [3]. Reduced effectiveness is observed against neutralization escape strains relative to ancestral strains for all SARS-CoV-2 vaccines studied to date [9], suggesting that nonneutralizing responses might only elicit modest protective value against such new strains.
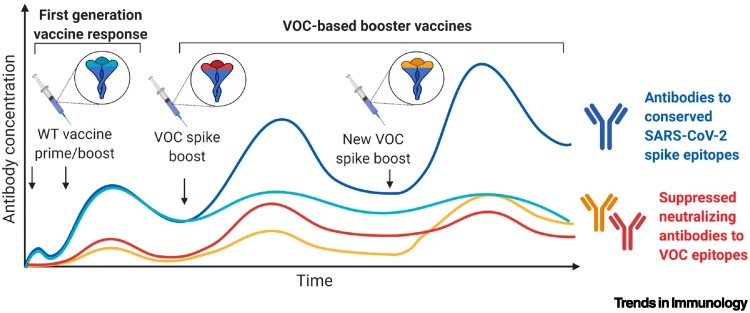
A significant difference in immune imprinting between IAV and SARS-CoV-2 is that adult humans have been exposed to IAVs many times during their lifetime. By contrast, SARS-CoV-2 is a new virus and few humans have yet been exposed to more than one SARS-CoV-2 or vaccine strain. It is possible that serial exposure to several related strains might be required to most effectively ‘imprint’ memory B cell immune responses to ancestral SARS-CoV-2 strains and, consequently, limit neutralizing antibody responses to new strains. Nonneutralizing antibodies and T cell responses to conserved epitopes across SARS-CoV-2 will play a role in immunity to new variants [9], but may be less potently protective than neutralizing antibody responses. As the world grapples with control of SARS-CoV-2 in the coming years, it seems likely that recurrent vaccination or infections will become common and immune imprinting may become an increasingly important issue to consider (Figure 1 ).
Figure 1.
Potential impact of repeated severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spike-based vaccine boosting on antibody responses.
Human antibodies against SARS-CoV-2 epitopes that are conserved across ancestral [wild type (WT)] and variants of concern (VOC) Spike proteins (blue) are elicited by initial WT vaccination and are likely to be boosted in response to subsequent VOC-targeted vaccines. The preferential recall of conserved immune responses imprinted to the WT strain may limit the generation of de novo responses against VOC receptor binding domain (RBD) epitopes (red and yellow) in response to booster vaccine doses. This figure was created using BioRender (https://biorender.com/).
Unknown factors regarding imprinting are the pace at which SARS-CoV-2 variants will emerge, and the magnitude of neutralization escape beyond that currently observed. Optimistically, neutralization escape pathways may be limited and may be already largely exhausted since a few neutralizing epitopes are commonly recognized [10]. Inducing sufficient neutralizing responses to current escape variants might be achievable with reformulated vaccines. Pessimistically, the SARS-CoV-2 Spike exhibits worrying plasticity, suggesting that further neutralization escape variants may emerge.
Evidence for immune imprinting has been suggested by studies of antibody responses against endemic human coronaviruses (hCoV) following SARS-CoV-2 infection [11] or vaccination [3]. For instance, back-boosting was observed for antibodies that were crossreactive to both hCoV-HKU1 or hCoV-OC43 and SARS-CoV-2 in samples from subjects recovering from coronavirus disease 2019 (COVID-19), particularly to the conserved S2 region of Spike [11]. Pre-existing hCoV antibodies were inversely correlated with SARS-CoV-2 de novo antibody responses following COVID-19 [11]; in particular, the responses were directed against the antigenically distinct SARS-CoV-2 Spike RBD, containing most of the key neutralizing epitopes [3]. This suggests that pre-existing crossreactive antibodies to Spike can limit new antibody responses to Spike from different viral strains (i.e., hCoVs and SARS-CoV-2); this is consistent with a potential problem of immune imprinting between ancestral and variant strains of SARS-CoV-2.
Strategies to limit immune imprinting from SARS-CoV-2 vaccines
Findings on IAV immune imprinting offer some guidance on strategies to limit the problem of immune imprinting but also suggest caution since, despite extensive research, a universal IAV vaccine remains unavailable. We propose that one strategy may be to immunize individuals only with minimal antigen content needed to induce effective neutralizing antibodies, rather than with the entire protein, which may contain additional ‘distracting’ epitopes that might potentially side-track the immune response [12]. The stem of the IAV hemagglutinin (HA) protein has been widely studied in this regard. The HA stem is relatively poorly immunogenic on its own, likely due to eliciting low affinity antibodies and weakly inducing T cell help [13]. However, when the HA stem has been engineered into a full-length HA protein derived from an irrelevant avian IAV strain, vaccination with this chimeric protein has induced robust immune responses in human trials and provided protective immunity in ferret models [14]. From this rationale, engineering SARS-CoV-2 variant RBDs into heterologous scaffolds such as hCoV Spike proteins might avoid the risk of imprinting with SARS-CoV-2 full-length Spike. Similarly, multimerizing the IAV HA stem and/or presenting it as an ordered array on a nanoparticle can partially overcome the weak immunogenicity of the HA stem [15]. The SARS-CoV-2 RBD is also relatively weakly immunogenic alone [12] but multimerization might ameliorate this. Noteworthy, priming with full-length Spike and then boosting with only the SARS-CoV-2 RBD ‘immuno-focuses’ neutralizing antibody responses to the RBD protein in mice and macaques [12] and might represent an approach to redirect immunity against SARS-CoV-2 variants.
Testing the imprinting hypothesis
Randomized trials are needed to evaluate the impact of immune imprinting on SARS-CoV-2 vaccine designs. We suggest that unvaccinated subjects could be randomized to receive active ancestral vaccines or placebo and then all subjects be later immunized with the reformulated variant Spike vaccine. Field efficacy could be assessed in a scenario where a given variant is circulating. If imprinting is a substantial problem, one would expect that efficacy would be reduced in the preimmunized group. An indication of the extent of the problem might be gleaned from neutralization data and parallel animal studies.
Experience from the IAV field indicates that multiple serial exposures to variant IAV strains might imprint (focus) the immune response to a narrow array of well-conserved viral epitopes relative to emerging subsequent strains and this might eventually reduce vaccine effectiveness. Randomizing multiple cohorts over time to either serial or partial immunization might also yield important neutralization data, although powering such studies for efficacy would be challenging. Larger observational studies of cohorts receiving serial immunizations might therefore also prove useful.
Concluding remarks
We hypothesize that updated vaccines against SARS-CoV-2 variants might primarily boost ‘imprinted’ immune responses to conserved regions of the Spike protein to the detriment of new neutralizing responses to antigenically altered sites within new variants. We argue that this ‘updated strain’ vaccine strategy can still yield partial efficacy against the new variants, particularly for vaccines that induce potent neutralizing responses. However, robust long-term control of COVID-19 may require the development of strategies that avoid primarily boosting imprinted immune responses and instead focus neutralizing antibody immunity on the novel RBD epitopes evolving in emerging VOC.
Acknowledgments
Acknowledgments
This work was supported by the Victorian government, the Medical Research Future Fund, and the National Health and Medical Research Council of Australia.
Author contributions
S.K. drafted the paper. All authors contributed ideas and concepts and revised the paper.
Declaration of interests
We declare no competing interests.
Glossary
- Ancestral SARS-CoV-2 strain
(wild type strain) original strain of SARS-CoV-2 that emerged in Wuhan, China, in late 2019. All current vaccines express this strain of SARS-CoV-2.
- Antigenic drift
here, mutations in influenza virus antigens over many years can result in escape from neutralizing antibodies.
- Back-boosting
phenomenon related to immune imprinting where infection with closely related strains or viruses boosts crossreactive responses primed to the previous strain, often to the detriment of generating new responses specific to the current strain.
- Beta and Delta variants
common variants of concern eliciting high neutralization escape.
- Endemic human coronaviruses (hCoV)
coronaviruses that cause common colds in humans, including viruses hCoV-HKU1 and hCoV-OC43. hCoV can share epitopes that crossreact with SARS-CoV-2, including in the S2 region of Spike.
- HA stem
part of the surface influenza virus (IAV) protein hemagglutinin (HA); conserved between strains and less susceptible to antigenic drift; a common target for universal IAV vaccine approaches that do not require yearly updates.
- Immune imprinting
phenomenon whereby initial exposure to one virus strain limits the development of immunity against new minor variant strains of the virus. Also commonly called original antigenic sin.
- Influenza A virus (IAV)
common respiratory virus that also mutates over time to escape neutralizing antibody responses.
- Neutralizing antibodies
block infection. Most neutralizing antibodies to SARS-CoV-2 bind to the RBD.
- Nonneutralizing antibodies
bind to a virus (or pathogen) but do not block the initial infection.
- Receptor binding domain (RBD)
part of the Spike protein used to bind receptors on infected cells. Antibodies blocking this interaction can neutralize the virus.
- S2 region of Spike
part of the Spike protein that forms the stalk of the protein and is primarily involved in mediating virus–cell fusion. The SARS-CoV-2 S2 shares some immunological crossreactivity with endemic human coronaviruses.
- SARS-CoV-2
severe acute respiratory syndrome coronavirus 2; cause of the COVID-19 pandemic.
- Spike protein
main surface protein of SARS-CoV-2; used for cell entry.
- Variants of concern (VOC)
strains of SARS-CoV-2 that escape neutralizing antibody responses to the wild type strain and/or are more transmissible. The strains contain mutations in the Spike protein.
References
- 1.Khoury D.S., et al. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat. Med. 2021;27:1205–1211. doi: 10.1038/s41591-021-01377-8. [DOI] [PubMed] [Google Scholar]
- 2.Weinreich D.M., et al. REGN-COV2, a neutralizing antibody cocktail, in outpatients with Covid-19. N. Engl. J. Med. 2021;384:238–251. doi: 10.1056/NEJMoa2035002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Amanat F., et al. The plasmablast response to SARS-CoV-2 mRNA vaccination is dominated by non-neutralizing antibodies that target both the NTD and the RBD. medRxiv. 2021 doi: 10.1101/2021.03.07.21253098. Published online May 1, 2021. [DOI] [Google Scholar]
- 4.Wall E.C., et al. Neutralising antibody activity against SARS-CoV-2 VOCs B.1.617.2 and B.1.351 by BNT162b2 vaccination. Lancet. 2021;397:2331–2333. doi: 10.1016/S0140-6736(21)01290-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu K., et al. Preliminary analysis of safety and immunogenicity of a SARS-CoV-2 variant vaccine booster. medRxiv. 2021 doi: 10.1101/2021.05.05.21256716. Published online May 6, 2021. [DOI] [Google Scholar]
- 6.Davenport F.M., Hennessy A.V. Predetermination by infection and by vaccination of antibody response to influenza virus vaccines. J. Exp. Med. 1957;106:835–850. doi: 10.1084/jem.106.6.835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Belongia E.A., et al. Variable influenza vaccine effectiveness by subtype: a systematic review and meta-analysis of test-negative design studies. Lancet Infect. Dis. 2016;16:942–951. doi: 10.1016/S1473-3099(16)00129-8. [DOI] [PubMed] [Google Scholar]
- 8.Fonville J.M., et al. Antibody landscapes after influenza virus infection or vaccination. Science. 2014;346:996–1000. doi: 10.1126/science.1256427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cromer D., et al. SARS-CoV-2 variants: neutralizing antibodies required for protective immunity. medRxiv. 2021 doi: 10.1101/2021.08.11.21261876. Published online August 13, 2021. [DOI] [Google Scholar]
- 10.Dejnirattisai W., et al. The antigenic anatomy of SARS-CoV-2 receptor binding domain. Cell. 2021;184:2183–2200. doi: 10.1016/j.cell.2021.02.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aydillo T., et al. Antibody immunological imprinting on COVID-19 patients. Nat. Commun. 2021;12:3781. doi: 10.1038/s41467-021-23977-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tan H.X., et al. Immunogenicity of prime-boost protein subunit vaccine strategies against SARS-CoV-2 in mice and macaques. Nat. Commun. 2021;12:1403. doi: 10.1038/s41467-021-21665-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tan H.X., et al. Subdominance and poor intrinsic immunogenicity limit humoral immunity targeting influenza HA stem. J. Clin. Invest. 2019;129:850–862. doi: 10.1172/JCI123366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nachbagauer R., et al. A chimeric hemagglutinin-based universal influenza virus vaccine approach induces broad and long-lasting immunity in a randomized, placebo-controlled phase I trial. Nat. Med. 2021;27:106–114. doi: 10.1038/s41591-020-1118-7. [DOI] [PubMed] [Google Scholar]
- 15.Yassine H.M., et al. Hemagglutinin-stem nanoparticles generate heterosubtypic influenza protection. Nat. Med. 2015;21:1065–1070. doi: 10.1038/nm.3927. [DOI] [PubMed] [Google Scholar]