Abstract
Parents of children with autism spectrum disorder (ASD) may be at greater risk for developing anti-vaccine beliefs that lead to vaccine delays and/or refusals for their children. We investigated current parental vaccine hesitancy, parents’ beliefs about causes of children’s developmental delays, and children’s vaccination histories among parents of children with ASD or non-ASD developmental delays. Data were analyzed from 89/511 parents (17.4%) who completed the Parent Attitudes About Childhood Vaccines questionnaire and the Revised Illness Perception Questionnaire; 46.1% had childhood vaccination records available. Overall, 21/89 (23.6%; [95% CI: 15.0, 34.0]) parents were vaccine hesitant (ASD n = 19/21 [90.5%] , non-ASD n = 2/21 [9.5%]). Parents of children with ASD were significantly more likely to agree with “toxins in vaccines” as a cause of their child’s developmental delays (28.4% vs. 5.0%, p = 0.034). The odds of being vaccine hesitant were 11.9 times (95% CI: 2.9, 48.0) greater among parents who agreed versus disagreed that toxins in vaccines caused their children’s developmental delays. Rates of prior vaccine receipt did not differ between hesitant and non-hesitant groups.
Keywords: autism, ASD, developmental delay, vaccines, immunizations, parent perception
Vaccines are one of public health’s greatest successes and have greatly reduced the morbidity and mortality associated with many infectious diseases (Center for Disease Control [CDC], 2011). Although vaccine refusal is relatively uncommon and represents one end of a broad spectrum of vaccine beliefs and behaviors, the number of non-medical vaccine exemptions is steadily increasing in states that permit personal-belief exemptions (Olive, Hotez, Damania, & Nolan, 2018). As a result, several major U.S. cities have now been identified as “hot spots” for vaccine refusals and outbreaks of vaccine-preventable diseases (Olive, Hotez, Damania, & Nolan, 2018; Center for Disease Control [CDC], 2019).
Vaccine-hesitant parents (VHPs) are uncertain about vaccines but are more amenable to vaccination than parents who refuse vaccines entirely (Gust et al., 2005; Gust et al., 2003; Gust, Darling, Kennedy, & Schwartz, 2008; Opel et al., 2013). The prevalence of VHPs varies geographically, with estimates ranging from 9 to 15% (Gust et al., 2008; Opel et al., 2013; Henrickson et al., 2015). Understanding more about cognitive processes related to vaccine hesitancy is key to addressing concerns that lead to vaccine delays and refusals—behaviors with significant public health implications.
Autism spectrum disorder (ASD) is a heterogeneous, behaviorally-defined neurodevelopmental disorder with multiple genetic and epigenetic etiologies, yet a genetic cause can be identified in only about 20% of cases (Schaefer, Mendelsohn, & Professional Practice and Guidelines Committee, 2013). A persistent misconception among many parents, particularly parents of children with ASD, is the erroneous belief that vaccines may have caused their child’s autism (Edwards et al., 2016; Offit, 2008). One study found that almost 20% of parents of children with ASD believed that vaccines were the main cause of their child’s condition, and more than a third of all parents believed that vaccines played some role in their child’s ASD (Goin-Kochel et al., 2015). Research has further demonstrated that the presence of a child with ASD in a family can increase rates of vaccine delay and refusal for that child, as well as his/her younger siblings (Kuwaik et al., 2014; Bazzano, Zeldin, Schuster, Barrett, & Lehrer, 2012; Glickman, Harrison, & Dobkins, 2017; Rosenberg, Law, Anderson, Samango-Sprouse, & Law, 2013; Zerbo et al., 2018). Thus, while a diagnosis of ASD may increase risk for developing antivaccine beliefs and practices, little is known about vaccine hesitancy in this population and how this may be influenced by families’ beliefs about causes of ASD. With this in mind, the objectives of this study were to (a) determine the proportions of VHPs among parents of children with ASD and non-ASD developmental delays (non-ASD-DD), (b) compare beliefs about causes of children’s developmental difficulties between diagnostic (ASD vs. non-ASD-DD) and hesitancy (hesitant vs. not hesitant) groups; (c) identify factors associated with current parental vaccine hesitance; and (d) characterize vaccine receipt among participating children with ASD and non-ASD-DD.
Methods
Data Collection
All families of children seen for evaluation of ASD at the Autism Center at Texas Children’s Hospital are invited to enroll in the Center’s research database, regardless of their final diagnosis (ASD or non-ASD-DD). Parents of children between 2 and 17 years of age who had enrolled in this research database and consented to future contact about additional studies were mailed enrollment paperwork that included a cover letter and questionnaires (described below). Return of completed questionnaires signified a participant’s consent to cooperate; return of blank questionnaires signified a parent’s wish not to participate and not to receive further information about the study. Nonresponsive families were notified up to three times about their opportunity to participate. This study was approved by the Institutional Review Board at Baylor College of Medicine and the TCH Autism Center Database Advisory Board.
Enrollment paperwork included a cover letter, the Parent Attitudes About Childhood Vaccines (PACV, Opel et al., 2011) questionnaire, and the Revised Illness Perception Questionnaire (IPQ-R, Moss-Morris et al., 2002). Briefly, the PACV is a validated 15-item instrument for identifying VHPs (Opel et al., 2013; Opel, Mangione-Smith, et al., 2011; Opel, Taylor, et al., 2011). Parents are dichotomized into hesitant or non-hesitant groups based on their PACV score, with scores ≥ 50 considered hesitant. The commonly-used and modifiable IPQ-R measures perceptions of health-related diagnoses and the impact these perceptions have on coping and subsequent medical decision-making. We relied on the IPQ-R Cause subscale to assess parents’ perceptions of etiological factors contributing to their children’s diagnosis.
Upon receipt of completed questionnaires, two co-authors independently reviewed children’s diagnostic summaries within the electronic medical record (EMR) to classify them as ASD or non-ASD-DD. Non-ASD-DD were categorized as children who did not meet criteria for ASD but were not neurotypical (i.e., global developmental delay, intellectual disability, speech/language disorders, ADHD). Any discordant results were reviewed and discussed with the child’s provider. Children whose diagnostic status for ASD were unclear were excluded from analyses.
Vaccination Documentation
We attempted to locate vaccine information for all participants through the EMR. Vaccine records were included for children who received primary care at a TCH location within the preceding 18 months. For the purposes of this assessment, vaccine information located within the EMR was assumed to reflect the child’s vaccination status. Children with no routine primary care visits documented within the EMR within the preceding 18 months were excluded from the vaccine assessment.
Receipt of the following six vaccines was categorized according to the Centers for Disease Control and Prevention’s (CDC) Recommended Immunization Schedule for Children and Adolescents (“Resource Library,” 2018), based on the child’s age at the time of study participation: diphtheria, tetanus, and acellular pertussis (DTaP); hepatitis B (HepB); Haemophilus influenzae type b (Hib); inactivated poliovirus (IPV); measles, mumps, and rubella (MMR); and varicella (VAR). These vaccines were selected to afford comparisons with prior research conducted on this topic (see Goin-Kochel et al., 2016). For each vaccine, children were categorized as (a) no evidence of vaccination, (b) not up-to-date for age, or (c) up-to-date for age. Children categorized as “no evidence of vaccination” had no documentation within the EMR of receipt of any dose of vaccine in the series. Doses were considered up-to-date for age when administered within the recommended age range, per the CDC Recommended Immunization Schedule, with a 30-day grace period applied before considering that dose delayed. Changes in vaccine recommendations over the period of retrospective vaccine review were incorporated.
Data Analysis
Participant demographics, vaccine-hesitant status (per the PACV), and IPQ-R responses were summarized by means with standard deviations or frequencies with percentages. Summary statistics were stratified by ASD diagnosis (ASD or non-ASD-DD) and hesitancy group. Demographic characteristics and IPQ-R Cause subscale items were compared between groups using independent, two-sample t-tests or Fisher’s exact test, as appropriate.
The primary outcome of interest was current parental vaccine hesitancy. A logistic regression model was used to estimate the odds ratio of a parent being vaccine hesitant (PACV ≥ 50) in the ASD diagnosis group compared with the non-ASD-DD group. The model included ASD status as well as demographic and IPQ-R variables that were significantly different between diagnostic groups or hesitant groups at the 0.10 level in the univariate analysis. Model results were summarized by odds ratios with 95% confidence intervals, and statistical significance for coefficients of the multiple regression model were assessed at the 0.05 level.
Results
A total of 511 parents enrolled in the Autism Center research database who met inclusion criteria received an invitation to participate and 96 (18.8%) returned completed PACV and IPQ-R questionnaires within a nine-month time period (Figure 1). Of these 96, 7 (7.3%) children had unclear documentation of ASD diagnoses and were subsequently excluded. The remaining 89 participants were included in analyses of vaccine hesitancy (PACV) and illness perception (IPQ-R). Of the 89 participants whose parents completed questionnaires, vaccine records were available for 41 (46.1%).
Figure 1.
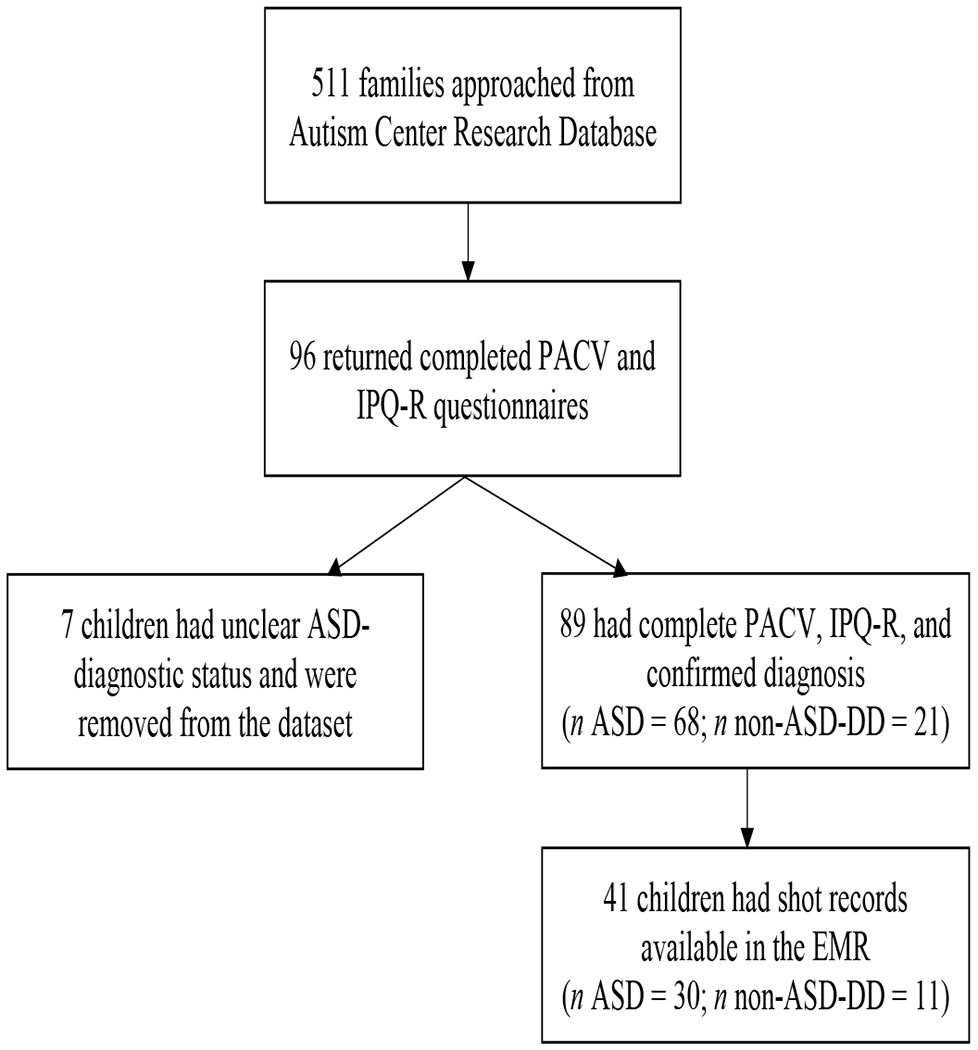
Enrollment Diagram
ASD Diagnostic Status and Vaccine Hesitancy
Overall, 68 parents (76.4%) had a child with ASD and 21 (23.6%) had a child with non-ASD-DD. Parents’ average age was 37.8 years (SD = 7.7); most were non-Hispanic White and had completed at least some college education (Table 1). Children’s average age was 7.3 years (SD = 3.1); the majority were males and half (50.6%) were the first-born.
Table 1.
Participant demographics by Diagnostic Group (ASD vs. non-ASD-DD) and Vaccine Hesitancy Group (Hesitant vs. Not Hesitant)
| Diagnostic Status | Vaccine Hesitancy Statusa | ||||||
|---|---|---|---|---|---|---|---|
| Demographic | Total N = 89 | ASD n = 68 (76.4%) | Non-ASD-DD n = 21 (23.6%) | p-value | Vaccine Hesitant n = 21 (23.6%) | Not Vaccine Hesitant n = 68 (76.4%) | p-value |
| Parent age (years), Mean (SD) | 37.8 (7.7) | 37.0 (7.6) | 40.3 (7.7) | 0.09 | 35.8 (6.8) | 38.4 (7.9) | 0.19 |
| Child age (years), Mean (SD) | 7.3 (3.1) | 7.1 (2.9) | 8.0 (3.6) | 0.25 | 6.6 (3.2) | 7.6 (3.1) | 0.20 |
| Child gender, n (%) male | 69 (77.5) | 56 (82.4) | 13 (61.9) | 0.07 | 15 (71.4) | 54 (79.4) | 0.55 |
| Child first born, n (%) | 45 (50.6) | 36 (52.9) | 9 (42.9) | 0.46 | 8 (38.1) | 37 (54.4) | 0.22 |
| Diagnostic status | |||||||
| ASD, n (%) | 68 (76.4) | 19 (90.5) | 49 (72.1) | 0.14 | |||
| Non-ASD-DD, n (%) | 21 (23.6) | 2 (9.5) | 19 (76.4) | ||||
| Parent race, n (%) | 0.93 | 0.08 | |||||
| Asian | 2 (2.2) | 2 (2.9) | 0 (0) | 1 (4.8) | 1 (1.5) | ||
| Black/African American | 6 (6.7) | 5 (7.4) | 1 (4.8) | 2 (9.5) | 4 (5.9) | ||
| White | 64 (71.9) | 47 (69.1) | 17 (81.0) | 12 (57.1) | 52 (76.5) | ||
| Other | 13 (14.6) | 11 (16.2) | 2 (9.5) | 3 (14.3) | 10 (14.7) | ||
| Mixed Race/Ethnicity | 4 (4.5) | 3 (4.4) | 1 (4.8) | 3 (14.3) | 1 (1.5) | ||
| Parent ethnicity, n (%) Hispanic/Latino | 26 (29.2) | 22 (32.4) | 4 (19.0) | 0.28 | 7 (33.3) | 19 (27.9) | 0.78 |
| Annual household income (thousands), n (%) | 0.72 | 0.95 | |||||
| ≤$50 | 38 (44.2) | 31 (46.3) | 7 (36.8) | 9 (42.9) | 29 (44.6) | ||
| $51-100 | 26 (30.2) | 19 (28.4) | 7 (36.8) | 7 (33.3) | 19 (29.2) | ||
| >$100 | 22 (25.6) | 17 (25.4) | 5 (26.3 | 5 (23.8) | 17 (26.2) | ||
| Missing | 3 | 1 | 2 | 0 | 3 | ||
| Highest level of education, n (%) | 0.84 | 0.28 | |||||
| <High school | 5 (5.6) | 3 (4.4) | 2 (9.5) | 1 (4.8) | 4 (5.9) | ||
| High school graduate/GED | 10 (11.2) | 8 (11.8) | 2 (9.5) | 0 (0) | 10 (14.7) | ||
| Some college/Bachelor/AD | 50 (56.2) | 39 (57.4) | 11 (52.4) | 14 (66.7) | 36 (52.9) | ||
| Graduate/Professional degree | 24 (27.0) | 18 (26.5) | 6 (28.6) | 6 (28.6) | 18 (26.5) | ||
Vaccine hesitant = PACV score ≥ 50; not vaccine hesitant = PACV score < 50.
Twenty-one of 89 parents (23.6%; 95% Cl: 15.2%, 33.8%) were vaccine hesitant (PACV score ≥ 50). The median PACV score was 30 (range = 0 to 87), with 17 (19%) scoring between 50 and 69 and 4 (4%) scoring ≥ 70. Nineteen (90.5%) of these VHPs had a child with ASD, whereas 2 (9.5%) had a child with non-ASD-DD.
Univariable analyses are summarized in Table 1. At the 0.10 level, child gender and parent age were significantly different between ASD and non-ASD-DD groups. Male children were more common among parents of children with ASD (82% vs. 62%; p = 0.07), and parents of children with ASD were an average of 3.3 years younger (37.0 vs. 40.3 years; p = 0.09). When comparing hesitant parents to non-hesitant parents, hesitant parents were less likely to be White (57.0% vs. 77.0%, p = 0.08).
Parent Report of Causes for Developmental Differences
Differences were observed in parents’ perceived causes of their child’s developmental delay by both diagnostic (ASD vs. non-ASD-DD) and hesitancy groups (Table 2). Parents of children with ASD were more likely to agree with the statement that “toxins found in vaccines/immunizations” are a possible cause of their children’s delays compared with parents of children with non-ASD-DD (28.4% vs. 5.0%, p = 0.034). Parents of children with ASD were also less likely to agree that “parental age” is a possible cause of their children’s delays (7.5% vs. 25.0%, p = 0.046).
Table 2.
Factorsa Believed to Cause Child’s Developmental Delays by Diagnostic Status (ASD vs. non-ASD-DD) and Vaccine Hesitancy Status (Hesitant vs. Not Hesitant)
| Diagnostic Status | Vaccine Hesitancy Statusb | ||||||
|---|---|---|---|---|---|---|---|
| Factor Believed to Cause Developmental Delays | Total N = 89 | ASD n = 68 (76.4%) | Non-ASD-DD n = 21 (23.6%) | p-value | Vaccine Hesitant n = 21 (23.6%) | Not Vaccine Hesitant n = 68 (76.4%) | p-valuec |
| General Life Stress | 31/87 (35.6%) | 21/67 (31.3%) | 10/20 (50.0%) | 0.18 | 10/21 (47.6%) | 21/66 (31.8%) | 0.20 |
| Genetics | 62/86 (72.1%) | 47/66 (71.2%) | 15/20 (75.0%) | 1.00 | 13/20 (65.0%) | 49/66 (74.2%) | 0.41 |
| A Germ or Virus | 8/86 (9.3%) | 8/66 (12.1%) | 0/20 (0%) | 0.19 | 2/21 (9.5%) | 6/65 (9.2%) | 1.00 |
| Diet or Eating Habits | 15/86 (17.4%) | 10/66 (15.2%) | 5/20 (25.0%) | 0.33 | 6/20 (30.0%) | 9/66 (13.6%) | 0.10 |
| Chance or Bad Luck | 17/87 (19.5%) | 15/67 (22.4%) | 2/20 (10.0%) | 0.34 | 2/21 (9.5%) | 15/66 (22.7%) | 0.22 |
| Poor Medical Care in Past | 9/87 (10.3%) | 5/67 (7.5%) | 4/20 (20.0%) | 0.20 | 1/21 (4.8%) | 8/66 (12.1%) | 0.45 |
| Environmental Pollution | 19/87 (21.8%) | 16/67 (23.9%) | 3/20 (15.0%) | 0.54 | 8/21 (38.1%) | 11/66 (16.7%) | 0.07 |
| My Own Behavior or Decisions | 15/87 (17.2%) | 10/67 (14.9%) | 5/20 (25.0%) | 0.32 | 5/21 (23.8%) | 10/66 (15.2%) | 0.34 |
| In Utero Stress or Accident | 35/88 (39.8%) | 27/67 (40.3%) | 8/21 (38.1%) | 1.00 | 9/21 (42.9%) | 26/67 (38.8%) | 0.80 |
| Mental Attitude/Negative Views | 7/85 (8.2%) | 6/65 (9.2%) | 1/20 (5.0%) | 1.00 | 2/19 (10.5%) | 5/66 (7.6%) | 0.65 |
| Family Worries About Developmental Difficulties | 12/87 (13.8%) | 7/67 (10.4%) | 5/20 (25.0%) | 0.14 | 3/21 (14.3%) | 9/66 (13.6%) | 1.00 |
| Will of God | 32/87 (36.8%) | 25/67 (37.3%) | 7/20 (35.0%) | 1.00 | 12/21 (57.1%) | 20/66 (30.3%) | 0.04 |
| My Own Emotional State | 19/85 (22.4%) | 15/66 (22.7%) | 4/19 (21.1%) | 1.00 | 8/21 (38.1%) | 11/64 (17.2%) | 0.07 |
| My or My Partner’s Age | 10/87 (11.5%) | 5/67 (7.5%) | 5/20 (25.0%) | 0.05 | 4/21 (19.0%) | 6/66 (9.1%) | 0.25 |
| My Own Alcohol Consumption | 4/87 (4.6%) | 3/67 (4.5%) | 1/20 (5.0%) | 1.00 | 1/21 (4.8%) | 3/66 (4.5%) | 1.00 |
| My Own Tobacco Consumption | 2/86 (2.3%) | 1/66 (1.5%) | 1/20 (5.0%) | 0.41 | 0/21 (0%) | 2/65 (3.1%) | 1.00 |
| Accident or Injury | 6/87 (6.9%) | 5/67 (7.5%) | 1/20 (5.0%) | 1.00 | 1/21 (4.8%) | 5/66 (7.6%) | 1.00 |
| My Child’s Brain Structure | 49/87 (56.3%) | 38/67 (56.7%) | 11/20 (55.0%) | 1.00 | 12/21 (57.1%) | 37/66 (56.1%) | 1.00 |
| Deterioration of My Child’s Immunity | 12/86 (14.0%) | 11/66 (16.7%) | 1/20 (5.0%) | 0.28 | 5/20 (25.0%) | 7/66 (10.6%) | 0.14 |
| Toxins Found in Vaccines/Immunizations | 20/87 (23.0%) | 19/67 (28.4%) | 1/20 (5.0%) | 0.03 | 13/21 (61.9%) | 7/66 (10.6%) | <0.0001 |
| Stress at Birth | 33/86 (38.4%) | 25/66 (37.9%) | 8/20 (40.0%) | 1.00 | 10/20 (50.0%) | 23/66 (34.8%) | 0.29 |
Note. Factors believed to cause developmental delays are from the IPQ-R.
Denotes Agreement or Strong Agreement with specified factor as a cause for children’s developmental delays/differences.
Vaccine hesitant = PACV score ≥ 50; not vaccine hesitant = PACV score < 50.
Variables that were significantly different between diagnostic groups or hesitancy groups at the 0.10 level in the univariate analysis were simultaneously included in a multiple logistic regression.
VHPs were more likely to agree that “will of God” (57.1% vs. 30.3%, p = 0.038) and “toxins found in vaccines/immunization” (61.9% vs. 10.6%, p < 0.0001) were causes of their children’s delays compared to non-hesitant parents.
Measures of Association
The primary purpose of this study was to estimate the association between ASD-diagnostic status (ASD or non-ASD-DD) and parental vaccine hesitancy. The unadjusted odds of a parent being vaccine hesitant was 3.7 (95% Cl: 0.8, 17.4; p = 0.10) times greater among parents of a child diagnosed with ASD compared with parents of a child with non-ASD-DD. The adjusted odds ratio was 3.2 (95% Cl: 0.37, 27.3; p = 0.29) after adjusting for child gender, race (White vs. Other), and parent age, as well as IPQ-R items for agreement with “parental age,” “toxins in vaccines,” “environmental pollution,” “will of god,” and “parental emotional state” as causes for ASD. Only agreement with “toxins in vaccines” was statistically significant at the 0.05 level in the final multiple logistic regression model; all other variables crossed unity. The adjusted odds of a parent being vaccine hesitant were 11.9 (95% Cl: 2.9, 48.0) times greater among parents who agreed that “toxins in vaccines” contributed to their child’s ASD compared with parents who did not agree (see Figure 2).
Figure 2.
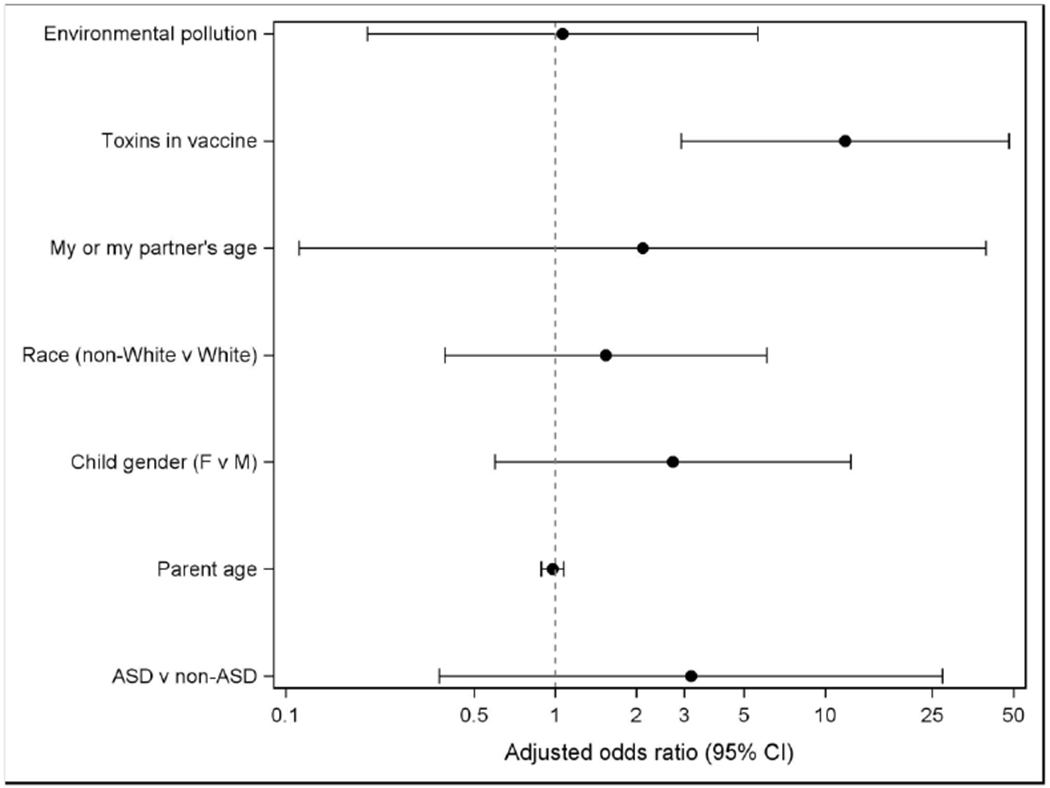
Adjusted Odds of Being Vaccine Hesitant by Demographic Factors and Beliefs About Causes
Vaccine Receipt and Vaccine Hesitancy
Among the 41 children for whom immunization records were available (80% male, M age = 6.8 [SD = 2.8]; 70.7% with ASD), 11 (26.8%) of the parents were vaccine hesitant. Of those who were hesitant, 10 (90.9%) had a child with ASD and five (45%) were non-White. Participants for whom vaccine records were available reported higher annual incomes than those without vaccine records (p = 0.03). Overall, 15 (36.6%) participants with vaccine records reported an annual income >$100,000, 14 (34.1%) reported an income between $51,000- −$100,000, and 13 (31.7%) reported an income <= $50,000.
Distributions of actual vaccine receipt (no evidence of vaccination, not up-to-date for age, and up-to-date for age) did not significantly differ between VHPs and non-hesitant parents (p ≥ 0.55); proportions of children in different categories of vaccine receipt by hesitancy status can be found in Table 3.
Table 3.
Childhood Vaccination Status by Vaccine Hesitancy Status (Hesitant vs. Not Hesitant)
| Vaccine Record Available N =41 of 89 (46.1%) | Vaccine Hesitanta n = 11 (27%) | Not Vaccine Hesitanta n = 30 (73%) | |||
|---|---|---|---|---|---|
| N | % | N | % | P-valueb | |
| DTaP | 1.00 | ||||
| No evidence of immunization | 0 | 0 | 0 | 0 | |
| Not up to date | 0 | 0 | 2 | 6.7 | |
| Up to date | 11 | 100 | 28 | 93.3 | |
| IPV | 0.55 | ||||
| No evidence of immunization | 0 | 0 | 0 | 0 | |
| Not up to date | 0 | 0 | 3 | 10.0 | |
| Up to date | 11 | 100 | 27 | 90.0 | |
| Hib | 0.55 | ||||
| No evidence of immunization | 0 | 0 | 0 | 0 | |
| Not up to date | 0 | 0 | 3 | 10.0 | |
| Up to date | 11 | 100 | 27 | 90.0 | |
| HepB | 1.00 | ||||
| No evidence of immunization | 0 | 0 | 0 | 0 | |
| Not up to date | 0 | 0 | 1 | 3.3 | |
| Up to date | 11 | 100 | 29 | 96.7 | |
| MMR | 1.00 | ||||
| No evidence of immunization | 0 | 0 | 1 | 3.3 | |
| Not up to date | 0 | 0 | 1 | 3.3 | |
| Up to date | 11 | 100 | 28 | 93.3 | |
| Varicella | 0.62 | ||||
| No evidence of immunization | 1 | 9.1 | 1 | 3.3 | |
| Not up to date | 0 | 0 | 1 | 3.3 | |
| Up to date | 10 | 90.9 | 28 | 93.3 | |
Note.
Vaccine hesitant = PACV score ≥ 50; not vaccine hesitant = PACV score < 50.
All values are based on Fisher’s exact test.
Discussion
The overall rate of current vaccine hesitancy in this sample was 23.6%, which is higher than previously reported rates of vaccine hesitancy in other parent samples (Gust et al., 2008; Henrikson et al., 2015). While there are no comparative data on current vaccine hesitancy among parents of toddlers or school-age children in the general population of Houston, Texas, a recent study examining vaccine hesitancy with the PACV among 610 expectant mothers in the Texas Children’s Pavilion for Women found that 8.2% were vaccine hesitant (Cunningham et al., 2018). This is similar to the 9.5% seen in the non-ASD-DD group and other estimates (Henrikson et al., 2015) but remarkably lower than the 27.9% seen in the ASD group. The assessment of vaccine records for a subset of our population did not demonstrate a difference between the ASD and non-ASD-DD groups in rates of vaccine delay or refusal for vaccines recommended during the first two years of life, suggesting that the vast majority of parents were not vaccine hesitant to the degree of refusal at that time. This is consistent with previous findings of high rates of parent-reported vaccine receipt for children with ASD (Goin-Kochel et al., 2016). It is worth noting that the majority of children who were not currently up to date on their vaccines were in the “not vaccine hesitant” group, and there are a variety of factors that could explain delayed receipt or nonreceipt of vaccines in families who are generally accepting of vaccines (e.g., missed well-child visit, child illness at the time the vaccine would have been offered).
While there were few differences observed between the ASD and non-ASD-DD groups with respect to perceived causes of children’s developmental delays, our data suggest that these beliefs may influence vaccine hesitancy. Among study participants, “will of God” and “toxins found in vaccines/immunizations” were more frequently endorsed as causes of their child’s developmental delays by VHPs. Two additional causes—“environmental pollution” and “my own emotional state”—were more frequently endorsed by VHPs compared to non-hesitant parents, albeit the differences did not reach statistical significance. However, in each of these cases, the proportions of parents agreeing with these factors as causes for their children’s delays were more than doubled among VHPs compared to non-hesitant parents. Collectively, these findings reflect a gravitation toward external explanations (i.e., environmental, metaphysical) for their children’s delays as opposed to internal explanations (e.g., biological, genetic) among VHPs. These results further underscore the importance of both educating parents about evidence-based causes of their children’s developmental conditions and addressing parental vaccine concerns to ensure that children of VHPs are vaccinated on time.
It is important to note, however, that the connection between cognition (i.e., vaccine hesitancy, beliefs about causes of ASD) and behavior (i.e., vaccinating their child) may shift over time. Despite a relatively high rate ~24%) of current parental vaccine hesitancy, overall rates of vaccine receipt in the subsample who had vaccine records on file were high, with the proportions across vaccines ranging from 90% to 100% (see Table 3). The fact that such a large proportion of parents are currently vaccine hesitant is consistent with earlier reports of changes in vaccine acceptance among families of children with ASD (Kuwaik et al., 2014; Rosenberg et al., 2013, Zerbo et al., 2018). The question remains as to exactly when and how these concerns develop, especially among parents whose children have been previously well-vaccinated.
Limitations and Future Directions
This study had several important limitations. First, the overall response rate was low at 18.8%, which may have resulted in response bias. It is well established that the topic of vaccines and autism is polarizing, particularly in the autism population (Taylor et al. 2014), and the sample may be skewed toward those feeling more strongly one way or the other. Therefore, our results may not be generalizable. Second, when the overall sample was divided into ASD and non-ASD-DD groups, resulting subsamples were small and some differences observed did not reach statistical significance, possibly because of reduced power. This is particularly reflected in the small subgroup of non-ASD-DD, non-hesitant parents. Third, only a portion (46.1%) of children had vaccine records available in the EMR. It is very likely that those children without vaccine information received doses elsewhere. Additionally, we had limited statistical power to formally assess potential differences between those with and without vaccine records available. Finally, age at diagnosis of ASD or non-ASD-DD was not available, so it was impossible to determine the potential influence of diagnostic-evaluation proximity on current vaccine hesitancy.
Considering evidence that children with ASD are reportedly well-vaccinated for recommended vaccines offered during the first two years of life (Goin-Kochel et al., 2016), and that the average age of ASD diagnosis is now 4.5 years (Christensen, 2016), future studies should compare rates of vaccine receipt pre- and post-ASD diagnostic evaluation among ASD and non-ASD-DD groups to clearly delineate the impact and immediacy of the ASD diagnosis on risk for decreased vaccine acceptance and adherence. Previous studies demonstrate the potential for vaccine behaviors to change for younger siblings of a child with ASD (Kuwaik et al., 2014; Bazzano et al., 2012; Rosenberg et al., 2013). Further evidence (i.e., Zerbo et al., 2018) suggests that after receiving an ASD diagnosis, affected children are significantly undervaccinated for their remaining scheduled vaccines compared to neurotypical controls, and their younger counterparts are significantly undervaccinated at all ages. Understanding how this shift in vaccine acceptance occurs may improve educational efforts targeted toward families affected by ASD.
Conclusion
This study suggests that there may be differences in vaccine hesitancy in parents of children with ASD compared with parents of children with non-ASD developmental delays. Prospective, longitudinal research focused on identifying how and when vaccine concerns emerge with respect to beliefs in an ASD-vaccine connection is critical to the development of effective vaccine-safety education and overall public health. Without this information, fears about an ASD-vaccine connection may persist, contributing to increasing vaccine hesitancy, lack of confidence in the U.S. vaccination program, and a potential increase in underimmunized/unimmunized children who are susceptible to vaccine-preventable diseases.
Acknowledgements:
This work was partially supported by a gift from the William Stamps Farish Foundation. A portion of Dr. Goin-Kochel’s effort was also supported by the NICHD-funded Baylor Intellectual and Developmental Disabilities Research Centers, Core B Clinical Translation Core (U54HD083092-02; Zoghbi [PI]). We are grateful to all the families who participated in this study, as well as all providers, administrators, and staff within TCH system who helped facilitate this work.
Footnotes
Disclosure: Dr. Goin-Kochel has consulted with Yamo Pharmaceuticals in the design of clinical trials. All other authors have no relationships to disclose.
References
- Bazzano A, Zeldin A, Schuster E, Barrett C, Lehrer D. Vaccine-related beliefs and practices of parents of children with autism spectrum disorders. Am J Intellect Dev Disabil. 2012;117(3):233–242. doi: 10.1352/1944-7558-117.3.233 [DOI] [PubMed] [Google Scholar]
- Benin AL. Qualitative analysis of mothers’ decision-making about vaccines for infants: The importance of trust. PEDIATRICS. 2006; 117(5):1532–1541. doi: 10.1542/peds.2005-1728 [DOI] [PubMed] [Google Scholar]
- Brunson EK. How parents make decisions about their children’s vaccinations. Vaccine. 2013a;31(46):5466–5470. doi: 10.1016/j.vaccine.2013.08.104 [DOI] [PubMed] [Google Scholar]
- Brunson EK. The impact of social networks on parents’ vaccination decisions. PEDIATRICS. 2013b;131(5):e1397–e1404. doi: 10.1542/peds.2012-2452 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control. Great Public Health Achievements--United States, 2011–2010. Morbidity and Mortality Weekly Report. 2011;60(19):619–623. [PubMed] [Google Scholar]
- Centers for Disease Control. Increase in measles cases—United States, January 1—April 26, 2019. Morbidity and Mortality Weekly Report. 2019;68(17):402–404. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control. Measles cases and outbreaks. Centers for Disease Control and Prevention. https://www.cdc.gov/measles/cases-outbreaks.html.Published May 3, 2018. Accessed June 15, 2018. [Google Scholar]
- Christensen DL, Baio J, Braun KVN, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years — Autism and developmental disabilities monitoring network, 11 sites, united states, 2012. MMWR Surveill Summ. 2016;65(3):1–23. doi: 10.15585/mmwr.ss6503a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Minard CG, Guffey D, Swaim LS, Opel DJ, Boom JA. Prevalence of vaccine hesitancy among expectant mothers in Houston, Texas. Academic Pediatrics. 2018;18(2):154–160. doi: 10.1016/j.acap.2017.08.003 [DOI] [PubMed] [Google Scholar]
- DeStefano F, Chen RT. Autism and measles-mumps-rubella vaccination: Controversy laid to rest? CNS Drugs. 2001;15(11):831–837. doi: 10.2165/00023210-200115110-00002 [DOI] [PubMed] [Google Scholar]
- Edwards KM, Hackell JM, THE COMMITTEE ON INFECTIOUS DISEASES, THE COMMITTEE ON PRACTICE AND AMBULATORY MEDICINE. Countering vaccine hesitancy. PEDIATRICS. 2016;138(3):e20162146–e20162146. doi: 10.1542/peds.2016-2146 [DOI] [PubMed] [Google Scholar]
- Fombonne E, Chakrabarti S. No evidence for a new variant of measles-mumps-rubella-induced autism. PEDIATRICS. 2001;108(4):e58–e58. doi: 10.1542/peds.108.4.e58 [DOI] [PubMed] [Google Scholar]
- Glickman G, Harrison E, Dobkins K. Vaccination rates among younger siblings of children with autism. NEngl JMed. 2017;377(11):1099–1101. doi: 10.1056/NEJMc1708223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goin-Kochel RP, Mire SS, Dempsey AG. Emergence of autism spectrum disorder in children from simplex families: Relations to parental perceptions of etiology. J Autism Dev Disord. 2015;45(5):1451–1463. doi: 10.1007/s10803-014-2310-8 [DOI] [PubMed] [Google Scholar]
- Goin-Kochel RP, Mire SS, Dempsey AG, et al. Parental report of vaccine receipt in children with autism spectrum disorder: Do rates differ by pattern of ASD onset? Vaccine. 2016;34(11):1335–1342. doi: 10.1016/j.vaccine.2016.02.008 [DOI] [PubMed] [Google Scholar]
- Goin-Kochel RP, Myers BJ. Congenital versus regressive onset of autism spectrum disorders: Parents’ beliefs about causes. Focus Autism Other Dev Disabl. 2005;20(3):169–179. doi: 10.1177/10883576050200030501 [DOI] [Google Scholar]
- Gust DA, Woodruff R, Kennedy A, Brown C, Sheedy K, Hibbs B. Parental perceptions surrounding risks and benefits of immunization. Seminars in Pediatric Infectious Diseases. 2003;14(3):207–212. doi: 10.1016/S1045-1870(03)00035-9 [DOI] [PubMed] [Google Scholar]
- Gust D, Brown C, Sheedy K, Hibbs B, Weaver D, Nowak G. Immunization attitudes and beliefs among parents: Beyond a dichotomous perspective. Am J Health Behav. 2005;29(1):81– 92. doi: 10.5993/AJHB.29.1.7 [DOI] [PubMed] [Google Scholar]
- Gust DA, Darling N, Kennedy A, Schwartz B. Parents with doubts about vaccines: Which vaccines and reasons why. Pediatrics. 2008;122(4):718–725. doi: 10.1542/peds.2007-0538 [DOI] [PubMed] [Google Scholar]
- Henrikson NB, Opel DJ, Grothaus L, et al. Physician communication training and parental vaccine hesitancy: A randomized trial. PEDIATRICS. 2015;136(1):70–79. doi: 10.1542/peds.2014-3199 [DOI] [PubMed] [Google Scholar]
- Kuwaik GA, Roberts W, Zwaigenbaum L, et al. Immunization uptake in younger siblings of children with autism spectrum disorder: Autism. October2012;18(2):148–155. doi: 10.1177/136236131245911 [DOI] [PubMed] [Google Scholar]
- Larson HJ, Jarrett C, Eckersberger E, Smith DMD, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine. 2014;32(19):2150–2159. doi: 10.1016/j.vaccine.2014.01.081 [DOI] [PubMed] [Google Scholar]
- Mackintosh V, Myers B, Goin-Kochel R. Sources of information and support used by parents of children with autism spectrum disorders. J on Dev Dis. 2005;12:41–51. [Google Scholar]
- Madsen KM, Hviid A, Vestergaard M, et al. A population-based study of measles, mumps, and rubella vaccination and autism. N Engl J Med. 2002;347(19):1477–1482. doi: 10.1056/NEJMoa021134 [DOI] [PubMed] [Google Scholar]
- Miller VA, Schreck KA, Mulick JA, Butter E. Factors related to parents’ choices of treatments for their children with autism spectrum disorders. Research in Autism Spectrum Disorders. 2012;6(1):87–95. doi: 10.1016/j.rasd.2011.03.008 [DOI] [Google Scholar]
- Moss-Morris R, Weinman J, Petrie K, Horne R, Cameron L, Buick D. The revised illness perception questionnaire(IPQ-R). Psychology & Health. 2002; 17(1):1–16. doi: 10.1080/08870440290001494 [DOI] [Google Scholar]
- Offit PA. Autism’s False Prophets: Bad Science, Risky Medicine, and the Search for a Cure. New York: Columbia University Press; 2008. [Google Scholar]
- Olive JK, Hotez PJ, Damania A, Nolan MS. The state of the antivaccine movement in the United States: A focused examination of nonmedical exemptions in states and counties. PLoS Med. 2018;15(6):e1002578. doi: 10.1371/journal.pmed.1002578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opel DJ, Mangione-Smith R, Taylor JA, et al. Development of a survey to identify vaccine-hesitant parents: The parent attitudes about childhood vaccines survey. Human Vaccines. 2011;7(4):419–425. doi: 10.4161/hv.7.4.14120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opel DJ, Taylor JA, Mangione-Smith R, et al. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine. 2011;29(38):6598–6605. doi: 10.1016/j.vaccine.2011.06.115 [DOI] [PubMed] [Google Scholar]
- Opel DJ, Taylor JA, Zhou C, Catz S, Myaing M, Mangione-Smith R. The relationship between parent attitudes about childhood vaccines survey scores and future child immunization status: a validation study. JAMA Pediatr. 2013;167(11):1065. doi: 10.1001/jamapediatrics.2013.2483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker SK. Thimerosal-containing vaccines and autistic spectrum disorder: a critical review of published original data. PEDIATRICS. 2004;114(3):793–804. doi: 10.1542/peds.2004-0434 [DOI] [PubMed] [Google Scholar]
- Resource Library: Vaccine schedule-related resources ∣ CDC. https://www.cdc.gov/vaccines/schedules/hcp/schedule-related-resources.html.Published February 16, 2018. Accessed June 15, 2018.
- Rosenberg RE, Law JK, Anderson C, Samango-Sprouse C, Law PA. Survey of vaccine beliefs and practices among families affected by autism spectrum disorders. Clin Pediatr (Phila). 2013;52(9):871–874. doi: 10.1177/0009922812438435 [DOI] [PubMed] [Google Scholar]
- Schaefer GB, Mendelsohn NJ, Professional Practice and Guidelines Committee. Clinical genetics evaluation in identifying the etiology of autism spectrum disorders: 2013 guideline revisions. Genet Med. 2013;15(5):399–407. doi: 10.1038/gim.2013.32 [DOI] [PubMed] [Google Scholar]
- Taylor B, Miller E, Lingam R, Andrews N, Simmons A, Stowe J. Measles, mumps, and rubella vaccination and bowel problems or developmental regression in children with autism: Population study. BMJ. 2002;324(7334):393–396. doi: 10.1136/bmj.324.7334.393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor LE, Swerdfeger AL, Eslick GD. Vaccines are not associated with autism: An evidence- based meta-analysis of case-control and cohort studies. Vaccine. 2014;32(29):3623–3629. doi: 10.1016/j.vaccine.2014.04.085 [DOI] [PubMed] [Google Scholar]
- Zerbo O, Modaressi S, Goddard K, et al. Vaccination patterns in children after autism spectrum disorder diagnosis and in their younger siblings. JAMA Pediatr. 2018;172(5):469. doi: 10.1001/jamapediatrics.2018.0082 [DOI] [PMC free article] [PubMed] [Google Scholar]


