Abstract
Purpose:
Older adults with dementia often rely on both paid caregivers (i.e., home health aides, personal care attendants, and other direct care workers) and family caregivers (i.e., spouses, children, and other unpaid individuals) to remain in the community. This study conceptualizes paid caregivers as part of the collaborative dementia care team and examines the association between receipt of paid care and primary family caregiver experience.
Methods:
Using data from 3 waves (2011, 2015, 2017) of the National Health and Aging Trends Study (NHATS) linked to the National Study of Caregiving (NSOC), we identified community-dwelling Medicare beneficiaries aged ≥67 with advanced dementia (n=338 observations). We compared primary family caregiver experiences among those with zero, part-time (<40 hours/week), and full-time (≥40 hours/week) paid care and used multivariable models to evaluate the associations between full-time paid care and family caregiver strain (e.g., being overwhelmed due to caregiving) and activity restriction (e.g., being unable to work for pay due to caregiving).
Findings:
About half of the community-dwelling older adults with advanced dementia received paid care: 30% had part-time paid care and 18% had full-time paid care. The experiences of family caregivers of those receiving part-time and no paid care were not significantly different. After adjusting for family caregiver and care recipient characteristics, receipt of full-time paid care was associated with a nearly 70% reduced odds of having activity restrictions due to caregiving (OR 0.31, p=0.01) and a reduction in mean caregiver strain score (−0.73, p=0.04). There was no statistically significantly association between the odds of high caregiver strain (score ≥5) and receipt of paid care (OR 0.65, p=0.33).
Implications:
The provision of paid care to individuals with dementia in the community may benefit family caregivers. Future work should acknowledge the important ways that paid caregivers contribute to outcomes for all members of the collaborative dementia care team.
Keywords: Home and community-based care and services, long-term care, workforce issues, caregiver stress, home care, dementia
Introduction
Family caregivers (defined as family members and other unpaid caregivers) perform the bulk of care for those living at home with functional and cognitive impairment 1. As care needs grow, many individuals with dementia and their family caregivers turn to paid caregivers to provide additional help. Paid caregivers (i.e., home health aides, personal care attendants, and other direct care workers) provide functional support and help with health tasks such as observing and reporting problems, providing emotional support, and communicating with families 2. Individuals with the highest levels of functional impairment use the most paid care: 30% of homebound individuals 3 and 50% of those with advanced dementia rely on paid caregivers 4.
As both patient preferences and evidence of cost-effectiveness shift the locus of long-term care from institutions to the community 5,6, awareness of paid caregivers’ important role in home-based care is growing. Yet the bulk of research about paid caregivers to date has adopted a workforce perspective and focuses on issues such as training, turnover, and job satisfaction 7–9. While essential to the field, this literature often fails to connect paid caregivers to the individuals receiving care and the families with whom care is shared. As a result, there is limited understanding of the role that paid caregivers play in the health and well-being of individuals with dementia and their family caregivers.
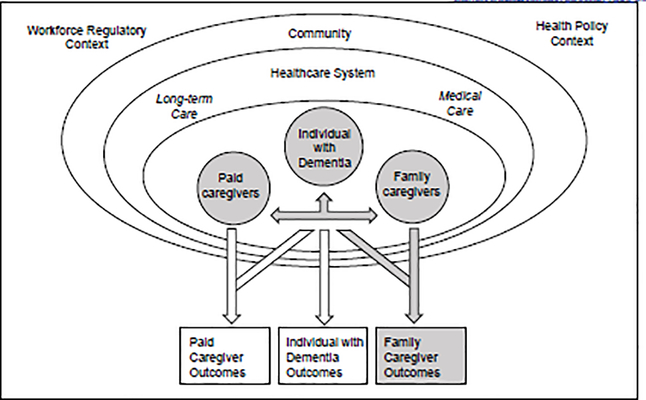
In order to better conceptualize the role of paid caregivers in the care of those with dementia living at home, we developed an integrative framework that highlights how an individual with dementia receives support from a collaborative care team that includes both paid caregivers and family caregivers (Figure 1). We draw significantly on the Convoys of Care 10 model, which suggests that the relationships among assisted living residents and their paid and family caregivers exist in a larger care environment and that characteristics of this “care convoy” impact outcomes for residents, paid caregivers, and family caregivers alike 10. The collaborative care team of paid and family caregivers works with other medical and long-term care providers within the larger healthcare system to make sure needs are met. This team is embedded in the community and interactions are informed by both health policy and workforce regulations. Importantly, paid and family caregivers are involved in active relationships not only with the individual with dementia, but also with each other. Because of the strength of these relationships, outcomes for all caregiving parties are influenced by characteristics of the individuals themselves (e.g. increasing functional impairment of an individual with dementia may lead to institutionalization) and by other care team members.
Figure 1:
Paid Caregivers Within the Collaborative Care Team Supporting Individuals With Dementia in the Community*
*shaded area in figure denotes relationships explored in the current study
The relationship between individuals with dementia and their family caregivers is bidirectional: individuals with dementia impact the outcomes of their family caregivers (e.g., behavioral symptoms of dementia contribute to more family caregiver strain and depression) 11 and family caregivers impact the outcomes of individuals with dementia (e.g., individuals with dementia are more likely to be institutionalized if their caregivers experience burden) 12. We argue that the notion of bidirectionality needs to be extended to paid caregivers, particularly in the context of advanced dementia, as individuals require higher levels of care to meet their functional needs and are more dependent on both paid and family caregivers.
Existing evidence demonstrates that paid caregivers develop relationships with both the individuals they care for and their families 13–15. Though this relational care may not be recognized in the formal care plans that describe the responsibilities of paid caregivers in the home, it is an essential part of what paid caregivers do and an important source of job satisfaction and care quality 16. Furthermore, a small but growing body of literature examines how paid caregivers improve care recipients’ health outcomes by doing things like promoting physical activity or helping to coordinate care 17–19. Yet little work examines how paid caregivers may impact the family of those they care for 20, and none, to our knowledge, specifically explores this relationship within the unique context of dementia.
Our study focuses on one particularly underexplored aspect of our larger integrative framework: how outcomes for family caregivers are impacted by characteristics related to paid care (e.g., number of care hours provided) as well as characteristics of the family caregivers themselves (e.g., relationship to the care recipient or hours of care provided) and characteristics of the individual with dementia (e.g., age and degree of functional impairment) (Figure 1, shaded areas). While benefits to caregiving exist, it is long established that the stress of caregiving negatively affects the emotional, social, and physical health of caregivers 21,22. These concerns are particularly important for dementia caregivers, who often provide high levels of care for many years and experience greater caregiving strain 23–25. Therefore, in this study we explore the associations between the primary family caregiver’s caregiving experience (i.e., caregiver strain, activity restriction due to caregiving) and receipt of paid care among those with advance dementia.
In order to do this, we use two linked population studies of older adults and their caregivers, the National Health and Aging Trends Study (NHATS) and the National Study of Caregiving (NSOC). Consistent with our integrative framework, we posit that paid caregivers play an important role in the collaborative care team by providing an additional layer of support that helps relieve some of the stress of family caregiving. Therefore, we hypothesize that receipt of paid care will be associated with fewer negative family caregiving experiences in general and lower strain in particular. While characteristics of individuals with dementia and their family caregivers themselves impact family caregiver outcomes, we expect that paid care exerts an independent effect on the caregiving experience. If present, such an association would support our conceptualization of paid caregivers as an essential part of the collaborative dementia care team.
Methods
Study Population
Our data were drawn from the nationally representative National Health and Aging Trends Study (NHATS) and the linked National Study of Caregiving (NSOC). NHATS is a longitudinal study of late-life disability and function among Medicare beneficiaries ≥65 years old and includes annual in-person cognitive and physical performance tests with participants or proxies. The initial NHATS cohort was recruited in 2011 and the sample was replenished in 2015. NSOC is a companion study to NHATS conducted in 2011, 2015 and 2017 that examines the experiences of up to five family caregivers who assist older NHATS participants with daily activities.
We used data from three waves of NHATS (2011, 2015, 2017). In order to ensure representativeness of the sample, we followed the guidance of NHATS investigators for applying survey weights which included using multiple observations per NHATS participant when applicable and restriction to age ≥67 for consistency across waves 26. Of the 2,060 observations from community-dwelling older adults with probable dementia, 489 came from those with advanced dementia. While 470 of these observations were from individuals with a family caregiver, the final sample included only observations from those who had at least one family caregiver interviewed in NSOC (n=338 observations from 303 unique individuals). Dementia status was determined using criteria for probable dementia established by NHATS 27, which incorporated self-report of dementia, proxy responses to the Alzheimer’s Disease (AD)-8 screening tool, and a cognitive interview that assessed memory, orientation, and function. We categorized individuals who had impairment (as defined below) with dressing, bathing, toileting, and managing medications and finances as having advanced dementia, consistent with a Functional Assessment Staging Tool (FAST) 28 score of 6–7 and as used previously by our study team 4.
Measures
Individuals with Dementia
Sociodemographic, Clinical, and Functional Characteristics
Measures were drawn from NHATS and included a variety of sociodemographic, clinical, and functional variables (Table 1). Chronic conditions were assessed by self-report. We defined impairment in a given activity of daily living (ADL) or instrumental activity of daily living (IADL) based on report that: (1) activity was performed with some or a lot of difficulty, (2) activity was never or rarely done alone, (3) activity was completed with the help of others, (4) activity was not performed because of lack of available assistance, or (5) adverse consequence was experienced because no one was available to help with the activity.
Table 1:
Characteristics of Individuals with Advanced Dementia Living at Home and Their Primary Caregivers Categorized by Amount of Paid Care Received (n=338 observations)a
| Full Sample | No Paid Care | Part-time Paid Care: <40 Hours/week | Full-time Paid Care: ≥40 Hours/week | |
|---|---|---|---|---|
| Sample, N Observations (% of sample) | 338 | 177 (52%) | 101 (30%) | 60 (18%) |
| Individual with Dementia | ||||
| Sociodemographic, Clinical, and Functional Characteristics | ||||
| Age, Mean (SD) | 83.1 (8.5) | 83.5 (7.8) | 82.1 (9.1) | 83.7 (9.3) |
| Female, % | 62.8 | 65.9 | 54.4 | 68.1 |
| White Non-Hispanic, % | 67.4 | 61.7 | 75.0 | 69.3 |
| ≥ High School Education, % | 61.1 | 51.9** | 75.6** | 61.0 |
| Income, 2015 Median | 19,656 | 19,300.0 | 19,418.3 | 21,726 |
| Medicaid, % | 35.7 | 36.7 | 32.1 | 39.1 |
| Long-term Care Insurance, % | 15.4 | 12.8 | 13.8 | 24.4 |
| Living Children, Mean (SD) | 3.4 (2.3) | 3.9*†† (2.5) | 3.1* (2.0) | 2.7†† (1.9) |
| Married, % | 38.4 | 37.5 | 39.0 | 39.6 |
| Interview Conducted with Proxy, % | 74.0 | 70.4 | 75.9 | 79.5 |
| ADLb Impairment, Mean (SD) | 5.5 (0.8) | 5.4†† (0.9) | 5.5‡ (0.7) | 5.8††‡ (0.5) |
| IADLc Impairment, Mean (SD) | 4.9 (0.5) | 4.8 (0.5) | 4.9 (0.5) | 4.9 (0.4) |
| Medical Conditions, Mean (SD) | 5.3 (2.2) | 5.7 (2.3) | 5.1 (2.0) | 5.0 (1.9) |
| Hospital Stay in Last Year, % | 54.6 | 56.7 | 46.0 | 62.7 |
| Caregiving Arrangements | ||||
| Total Caregivers, Mean (SD) | 3.3 (1.7) | 2.6**†† (1.5) | 3.8** (1.5) | 4.2†† (1.7) |
| Family Caregivers, Mean (SD) | 2.4 (1.4) | 2.5 (1.5) | 2.4 (1.4) | 2.3 (1.3) |
| Paid Caregivers, Mean (SD) | 0.8 (0.9) | n/a | 1.3‡‡ (0.5) | 1.9‡‡ (1.0) |
| Hours/week Total Care, Mean (SD) | 122.6 (79.8) | 112.2†† (71.8) | 111.7‡‡ (84.0) | 163.9††‡‡ (78.7) |
| Hours/week Paid Care, Mean (SD) | 23.7 (43.3) | n/a | 14.0‡‡ (11.4) | 94.9‡‡ (49.6) |
| Paid Caregiver Paid by Self/family | 25.2 | n/a | 49.9 | 55.3 |
| Primary Caregiver | ||||
| Age, Mean, (SD) | 62.2 (12.0) | 60.7 (12.8) | 63.1 (10.2) | 64.6 (12.1) |
| Female, % | 72.6 | 74.8 | 70.8 | 70.1 |
| Worked for Pay in the Last Month, % | 27.6 | 23.6 | 31.5 | 31.1 |
| Self-report Health Fair/poor, % | 23.4 | 28.2 | 21.5 | 15.1 |
| Child of Individual With Dementia | 60.0 | 65.8 | 55.6 | 52.8 |
| Co-resides With Individual With Dementia | 74.7 | 77.3 | 77.7 | 64.2 |
| Hours/week Care Provided, Mean (SD) | 49.2 (42.7) | 58.0*†† (45.8) | 44.6* (36.0) | 35.8†† (40.6) |
Significance of group-wise comparisons:
No paid care versus part-time paid care:
p<0.05
p<0.01
No paid care versus full-time paid care:
p<0.05
p<0.01
Part-time paid care versus full-time paid care:
p<0.05
p<0.01
Six ADLs evaluated: eating, getting out of bed, showering, toileting, dressing, getting around inside
Caregiving Arrangements
The paid and family caregivers supporting individuals with advanced dementia in their homes were identified using NHATS self-report. If NHATS participants or proxies note that help is needed to perform a particular functional task (eating, getting out of bed, showering, toileting, dressing, laundry, shopping, meal preparation, medication management, getting around outside, bills and banking, addressing money matters, and going to the doctor) in the last month, the individual providing care is identified. The following information about the caregiver is subsequently obtained: 1) relationship to study participant, 2) hours of help provided, 3) whether care was paid or unpaid, 4) if paid, sources of payment (e.g., self or family, a government program).
Based on NHATS reports, we calculated total weekly hours of care received from all caregivers (paid and family) and hours of paid care received by all individuals with advanced dementia included in our sample. In order to capture the wide range of paid care hours received by individuals with dementia in a clinically meaningful way, we stratified paid caregiver hours as zero, part-time (<40 hours/week paid care ), and full-time (≥40 hours/week paid care) paid care and reported if paid caregivers were paid directly by the individual with dementia or their family. We also determined total number of caregivers, number of family caregivers, and number of paid caregivers.
Family Caregivers
We defined the primary family caregiver as the family or other unpaid caregiver who reported spending the most hours providing care based on their own self-report in NSOC. We reported the total weekly hours spent providing care for each primary family caregiver. Characteristics for primary family caregivers were drawn from NSOC and included sociodemographic variables and information about the caregiving context.
Family Caregiver Outcomes
NSOC asks a wide range of questions about how the caregiving experience impacts the lives and well-being of caregivers. Drawing on previous reports using NSOC data 29,30 and our own review of NSOC questions, we identified two groups of questions that explored negative family caregiving experiences. We chose not to include variables (e.g., depression, self-rated health) that described family caregivers’ more general experience and instead focused on variables that were directly tied to caregiving both in the wording of the question and in the published literature.
First, we evaluated components of caregiver strain using a previously published 6-item caregiver strain measure 31,32 that included three items related to difficulty providing care (financial, emotional, and/ or physical difficulty arising from caregiving) and three items related to role overload (exhausted when going to bed, more things to do than you can handle, not having time for oneself). Following previous literature, we then calculated a composite caregiving strain score using the components of caregiver strain described above. If respondents reported that helping was difficult in any domain (physical, emotional, and financial), they were asked to rate the level of difficulty. Responses were scored as 0 (no difficulty), 1 (some difficulty, rating of 1, 2, or 3), or 2 (a lot of difficulty, rating of 4 or 5). Respondents who reported having no time for themselves, being overwhelmed, or being exhausted scored a 1 if they answered yes to any of the questions and 0 if they answered no. These answers were then summed to form an index from 0 to 9. High caregiver strain was defined as a strain score of ≥5, a cut off previously found to have clinical relevance 33.
Second, we examined whether or not caregiving caused the caregiver to restrict seven specific activities: visiting people not living with you, attending religious services, participating in club meetings or group activities, going out for enjoyment, working for pay, doing volunteer work, and/or caring for a child or other adult. We then created a binary variable to indicate if the caregiver reported caregiving-related restriction in any of these seven activities.
Analysis
We used Chi-square and Student’s t-test to examine differences in characteristics of individuals with advanced dementia and their primary family caregiver among those receiving no, part-time, and full-time paid care. We also compared the percentage of those reporting affirmative responses to any of the negative family caregiving experiences described above among those receiving no, part-time, and full-time paid care. We report imputed values for income that are provided by NHATS. Because no other single reported variable had ≥5% missing data with the exception of receipt of long-term care insurance (6.2% missing), univariate results are presented with missing values dropped.
We used multivariable logistic and linear regression as appropriate to examine the relationship between full-time paid care and 1) high caregiver strain, 2) mean caregiver strain score, and 3) caregiving-related restriction in any activity. Seven observations had components of the strain score missing and fewer than 5 observations had missing information about caregiving-related activity restriction; missing components were considered “zero” for construction of the caregiver strain score and “no restriction” for the “any activity restriction” outcome. Drawing from relationships described in our conceptual model (Figure 1, shaded areas), we conducted regression models controlling for other factors that may also influence family caregiver outcomes: characteristics of the individual with dementia (age, gender, ADL impairment, IADL impairment, Medicaid) and primary family caregiver characteristics (gender, co-resides with individual with dementia, child caring for parent, hours of care from primary caregiver). When multiple variables described complementary aspects of a single concept (e.g., total hours of care and hours from primary caregiver both describe care received) we chose the variables we believed to be most relevant based on clinical experience and review of the literature. Because 10% (n= 33) of observations had some missing data element and in order to retain a full sample for analysis, we used Multiple Imputation by Chained Equations (MICE) for missing variables for all multivariable models. Results were similar for sensitivity-test regressions on complete cases only.
We applied survey weights to all variables 26. All analyses were completed using Stata 16 (College Station, TX, n.d.).
Results
Of the 338 observations from community-dwelling older adults with advanced dementia included in our study, 177 (52%) did not receive paid care. One hundred and one (30%) had part-time paid care (<40 hours/ week) and 60 (18%) had full-time paid care (≥40 hours/ week). There were few statistically significant differences in sociodemographic, clinical, and functional characteristics among individuals with dementia based on receipt of paid care, though those who received part-time paid care were more likely to have at least a high school education as compared to those with no paid care (75.6% vs. 51.9%, p<0.01); those with full-time paid care were more likely to have greater ADL impairment as compared to those with no paid care (mean ADL impairment 5.8 ADLs versus 5.4, p<0.01) or part-time paid care (mean ADL impairment 5.8 ADLs versus 5.5, p=0.04); and those with no paid care were more likely to have more living children compared to both those with part-time paid care (3.9 vs 3.1, p=0.03) and full-time paid care (3.9 vs. 2.7, p<0.01) (Table 1).
All three groups had similar mean numbers of family caregivers involved in their care (2.5, 2.4, and 2.3 caregivers for those with no paid care, part-time paid care, and full-time paid care respectively). While those with part-time paid care received a mean of 14.0 hours/ week paid care, those with full-time paid care received 95.9 hours/ week paid care. Accordingly, total hours of care received from all caregivers (paid and family) were similar for those with no paid care and part-time paid care (112.2 vs 111.7, p=0.97) but much higher for those with full-time paid care as compared to those with no paid care (163.9 vs. 112.2, p<0.01) or part-time paid care (163.9 vs. 111.7, p<0.01). Approximately half of all paid care was paid for privately by individuals with dementia and/or their families regardless of whether paid care was part-time or full-time (49.9 vs 55.3 respectively, p=0.63). Primary family caregivers of individuals with dementia receiving no paid care provided more hours of care per week as compared to those with full-time paid care (58.0 vs 35.8, p<0.01) or part-time paid care (58.0 vs 44.6, p=0.02); the difference in caregiving hours per week for primary caregivers of individuals with part-time and full-time paid care was not significant (p=0.29) (Table 1).
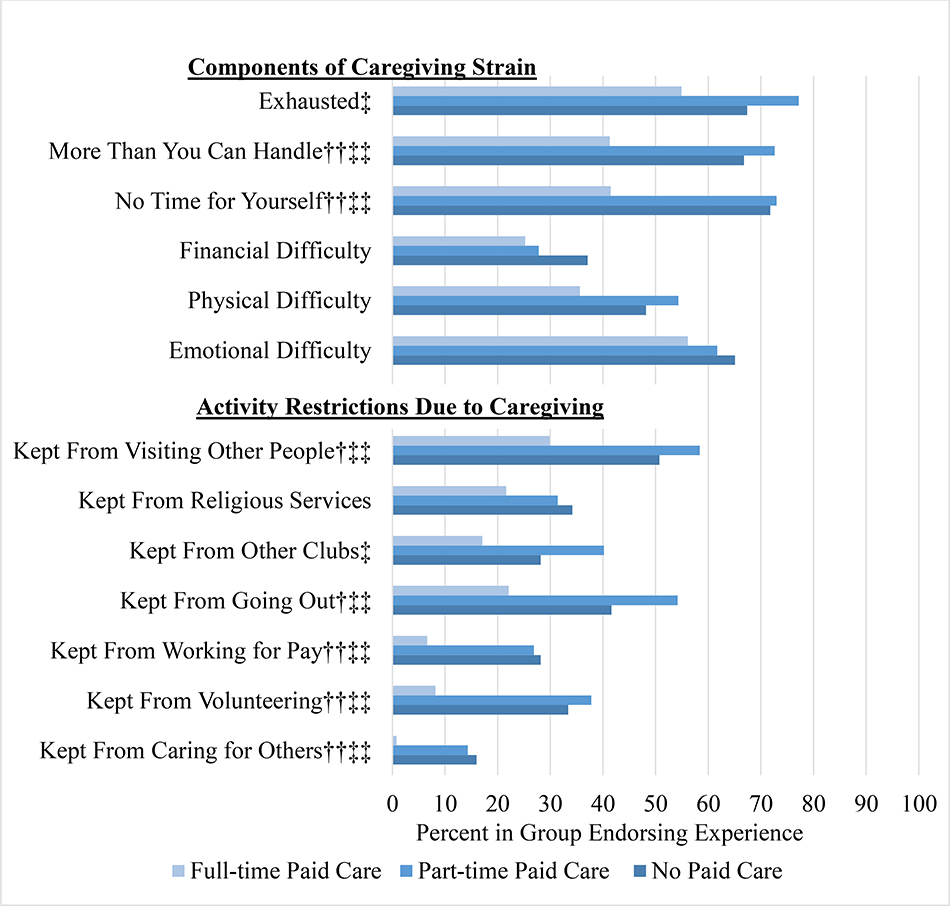
Figure 2 presents the percentage of family caregivers reporting negative caregiving experiences grouped by whether or not the individual with dementia for whom they cared received no paid care, part-time paid care, and full-time paid care. Compared to those with no paid care or part-time paid care, those with full-time paid care were significantly less likely to report negative caregiving experiences in several domains, especially those related to role overload and activity restrictions due to caregiving. For example, over 70% of those caring for an individual with dementia who had no paid care or part-time paid care reported they did not have time for themselves compared to just 42% of those caring for an individual with dementia with full-time paid care. Only 22% of those caring for an individual with dementia with full-time care reported that caregiving kept them from going out for enjoyment, while 42% and 54% of those caring for an individual with dementia with no paid care and part-time paid care respectively reported this. No statistically significant differences in reported negative family caregiving experiences existed between caregivers of those who had no paid care vs. part-time paid care.
Figure 2:
Negative Family Caregiver Experiences by Receipt of Paid Care a
a Significance of group-wise comparisons:
No paid care versus part-time paid care: *p<0.05, **p<0.01
No paid care versus full-time paid care: †p<0.05, †† p<0.01
Part-time paid care versus full-time paid care: ‡p<0.05, ‡‡ p<0.01
Full-time paid care was not significantly associated with being in the high caregiver strain group (28.9% vs 43.0% in the full-time and non-full-time groups respectively, p=0.134) and findings did not change after adjusting for characteristics of individuals with dementia and their primary family caregivers (OR 0.65, p=0.33) (Table 2). However, full-time paid care was associated with a lower mean caregiver strain score (3.1 vs 4.1 in the full-time and non-full-time groups respectively, p<0.01) and the relationship persisted in the fully adjusted model (−0.73, p=0.04). In addition, those with full-time paid care were less likely to report any caregiving-related activity restriction (45.1% vs. 69.4% in the full-time and non-full-time groups respectively, p<0.01) and the relationship persisted in the fully adjusted model (OR 0.31, p=0.01) (Table 2).
Table 2:
Analysis of Adjusted and Unadjusted Associations Between Full-time Paid Care (≥40 hours/ week) and Negative Caregiver Experience Outcomes (n= 338 observations)
| High Caregiver Strain (Strain Score ≥5) | Mean Caregiver Strain Score | Caregiving Caused ny Activity Restriction | ||||
|---|---|---|---|---|---|---|
| Odds Ratio | p-value | Coefficient | p-value | Odds Ratio | p-value | |
| Unadjusted | 0.54 | 0.14 | −1.08 | 0.01 | 0.36 | 0.01 |
| Adjusted for Individual Characteristics a | 0.52 | 0.12 | −1.14 | 0.01 | 0.25 | <0.01 |
| Adjusted for Individual a and Family Caregiver b Characteristics | 0.65 | 0.33 | −0.73 | 0.04 | 0.31 | 0.01 |
Individual with Dementia Characteristics: Age, Female Gender, ADL Impairment (evaluated eating, getting out of bed, showering, toileting, dressing, getting around inside), IADL Impairment (evaluated laundry, shopping, meal preparation, medication management, bills and banking), Medicaid
Primary Family Caregiver Characteristics: Age, Female Gender, Co-resides with Individual with Dementia, Family Caregiver is Child of Individual with Dementia, Mean Hours of Care Per Week Provided
Discussion
Our findings suggest that receipt of paid care may be beneficial for family caregivers among a nationally representative sample of older adults with advanced dementia living in the community. Family caregivers caring for someone with full-time paid care were less likely than others to have negative caregiving experiences such as being exhausted or being unable to work for pay due to caregiving responsibilities. Full-time paid care was significantly associated with a lower mean caregiver strain score and fewer caregiving-related activity restrictions after controlling for characteristics of both the individual with dementia and the primary family caregiver that may also impact caregiver experience.
Ongoing research to understand and improve the experiences of family caregivers of those with dementia should consider the important contribution paid caregivers make to the well-being of family caregivers. In particular, there is a need to identify specific care arrangements or settings where paid caregiving may provide the greatest benefit. For example, family caregivers of individuals with dementia who experience behavioral symptoms experience disproportionate levels of strain and may uniquely benefit from additional paid caregiver support. Similarly, people caring for aging parents, particularly long-distance caregivers coordinating care from afar or sandwich generation caregivers balancing the needs of their parents and young children, may gain particular benefit from sharing caregiving responsibilities with paid caregivers.
It is important to note that the benefit of paid care for family caregivers in our study was only evident in those receiving full-time paid care, who received more than six times as many paid care hours per week compared to those receiving part-time care (14.0 hours versus 95.9 hours of care provided per week for those with part-time and full-time paid care respectively.) In general, there was little difference between those receiving no or part-time paid care. One possible explanation is that part-time and full-time paid care serve different functions in the community-based care of individuals with dementia. Whereas part-time paid care likely focuses on completing specific tasks, full-time paid caregivers are more globally involved in care. As a result, full-time paid caregivers may be more likely to work collaboratively over time to support both individuals with dementia and their family caregivers.
While the finding that higher amounts of paid care are associated with improved family caregiver experiences is not surprising, it is important. Much of the existing health literature that examines paid care fails to capture paid caregiving hours and the presence of any paid care is simply dichotomized. Without considering the amount of paid care, one could erroneously conclude that having paid care made no difference for care recipients or their families when in fact the “dose” was too small to expect such an impact.
Our work also helps to underscore individual aspects of the family caregiving experience which may be most impacted by paid care. The presence of full-time paid care seemed to afford family caregivers the additional time to engage more fully (e.g., with less exhaustion) in other aspects of their life (e.g., working for pay or volunteering), but did not significantly decrease the financial, emotional, or physical difficulty they experienced as a result of providing care. This finding, along with a small sample size, likely contributed to the fact that full-time paid care did not significantly reduce the odds of being in the high strain category. Of note, receipt of paid care does not mean family caregivers stop caregiving. We found that the number of family caregivers involved remained similar regardless of receipt of paid care. Yet when individuals with dementia received more paid care hours, family caregivers provided significantly fewer hours of care.
However, the relationship between full-time paid care and family caregiver experience is only partly explained by reduced hours spent caring. Controlling for weekly hours of family caregiving somewhat attenuated the association between full-time paid care and negative caregiving experiences, but a significant relationship remained. This suggests that paid care both substitutes for and complements family care. Furthermore, the roles and relationships among caregivers on the care team are likely unique for each individual with dementia. Because training and supervision of paid caregivers (even those employed by home care agencies) are often minimal, paid and family caregivers must negotiate complex caregiving dynamics on their own 7,34. When individuals have dementia, this may lead to significant stress for family caregivers who take on a managerial role for which they are often unprepared.
Importantly, our finding that paid care is associated with improved family caregiver experience supports our broader conceptualization of paid caregivers not as interchangeable members of an abstract workforce, but instead, as members of a collaborative care team where individuals with dementia, paid caregivers, and family caregivers may each impact outcomes for the others. While this study specifically examines the association between paid care and family caregiver experience, future work should explore other aspects of this collaborative team care (e.g., associations between paid caregiver training and care outcomes for individuals with dementia and their family caregivers).
Such research will require collection of more robust data about paid caregivers themselves including primary language, race and ethnicity, language concordance and cultural similarities with others on the team, presence of agency-based nursing supervision, and general and dementia-specific training. Because community-based paid care in the United States is essentially part of a patchwork of long-term services and supports that vary significantly from state to state (e.g., minimum training requirements, thresholds for Medicaid funding for paid care in the home) 7 and community to community (e.g. workforce shortages, cost of privately hired paid caregivers)35, detailed information about these contextual factors is also critical to building upon this research.
As is common in secondary data analysis, our ability to characterize individuals with dementia, paid caregivers, and family caregivers in the collaborative care team was constrained by the variables available in the NHATS and NSOC datasets and important variables (e.g., family caregiver use of other respite services, emotional valence of paid and family caregiver relationship) were not available. In particular, caregivers were defined and hours of help were calculated based on reports of help with a series of functional tasks, but this did not include other forms of help such as the emotional and psychological support that both family and paid caregivers are known to provide 2,16. In addition, our focus on primary family caregivers did not evaluate if or how paid care affects the broader network of family caregivers that support individuals with dementia in the community.
Despite these limitations, this study provides foundational information about the important ways that family caregivers may benefit from the paid care that their family members with dementia receive and suggests that interventions to improve the family caregiver experience 36 should consider the impact of paid care. By providing evidence for an innovative approach to conceptualizing the role of paid caregivers in community-based dementia care, our work should prompt researchers, clinicians, and policy makers to consider the interdependence of the collaborative care team in dementia care. It is in the interest of those working to support family caregivers to engage more deeply and advocate more vocally around issues important to the strength of the paid caregiver workforce (e.g., competency-based paid caregiver training, living wages) 35. Likewise, as members of the long-term services and supports team 37 the needs of family caregivers should be prioritized in discussions of what contributes to quality paid care in the home.
Conclusions
The provision of paid care to individuals with dementia in the community may benefit family caregivers. Future work should acknowledge the important ways that paid caregivers contribute to outcomes for all members of the collaborative dementia care team.
Highlights:
Half of those with advanced dementia living in the community received paid care.
Family experiences were similar for those with no and part-time paid care.
Families of those with full-time paid care had fewer negative caregiving effects.
Paid caregivers play an important role in the collaborative dementia care team.
Acknowledgments
Disclosure of Funding Support
This work was supported by the National Institute on Aging [R03AG060092 and K23AG066930 to JR, R01AG060967 to KO]. The study sponsors had no role in study design; collection, analysis, and interpretation of the data; wiring of the manuscript; or the decision to submit the manuscript for publication.
Sponsor Role: The study sponsors had no role in study design; collection, analysis, and interpretation of the data; writing of the manuscript; or the decision to submit the manuscript for publication.
Footnotes
Declaration of Interest: The authors have no conflicts to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Wolff JL, Spillman BC, Freedman VA, Kasper JD. A National Profile of Family and Unpaid Caregivers Who Assist Older Adults With Health Care Activities. JAMA Intern Med. 2016;176(3):372–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reckrey JM, Tsui EK, Morrison RS, et al. Beyond Functional Support: The Range Of Health-Related Tasks Performed In The Home By Paid Caregivers In New York. Health Aff (Millwood). 2019;38(6):927–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reckrey JM, Federman AD, Bollens-Lund E, Morrison RS, Ornstein KA. Homebound Status and the Critical Role of Caregiving Support. J Aging Soc Policy. 2019:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reckrey JM, Morrison RS, Boerner K, et al. Living in the Community With Dementia: Who Receives Paid Care? J Am Geriatr Soc. 2020;68(1):186–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kitchener M, Ng T, Miller N, Harrington C . Medicaid home and community-based services: national program trends. Health Aff (Millwood). 2005;24(1):206–212. [DOI] [PubMed] [Google Scholar]
- 6.Samus QM, Black BS, Bovenkamp D, et al. Home is where the future is: The BrightFocus Foundation consensus panel on dementia care. Alzheimers Dement. 2018;14(1):104–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kelly CM, Morgan JC, Jason KJ. Home care workers: interstate differences in training requirements and their implications for quality. J Appl Gerontol. 2013;32(7):804–832. [DOI] [PubMed] [Google Scholar]
- 8.Ejaz FK, Noelker LS, Menne HL, Bagaka’s JG. The impact of stress and support on direct care workers’ job satisfaction. Gerontologist. 2008;48 Spec No 1:60–70. [DOI] [PubMed] [Google Scholar]
- 9.Stone R, Wilhelm J, Bishop CE, Bryant NS, Hermer L, Squillace MR. Predictors of Intent to Leave the Job Among Home Health Workers: Analysis of the National Home Health Aide Survey. Gerontologist. 2017;57(5):890–899. [DOI] [PubMed] [Google Scholar]
- 10.Kemp CL, Ball MM, Perkins MM. Convoys of care: theorizing intersections of formal and informal care. J Aging Stud. 2013;27(1):15–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Feast A, Moniz-Cook E, Stoner C, Charlesworth G, Orrell M. A systematic review of the relationship between behavioral and psychological symptoms (BPSD) and caregiver well-being. Int Psychogeriatr. 2016;28(11):1761–1774. [DOI] [PubMed] [Google Scholar]
- 12.Eska K, Graessel E, Donath C, Schwarzkopf L, Lauterberg J, Holle R. Predictors of institutionalization of dementia patients in mild and moderate stages: a 4-year prospective analysis. Dement Geriatr Cogn Dis Extra. 2013;3(1):426–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kemp CL, Ball MM, Morgan JC, Doyle PJ, Burgess EO, Perkins MM. Maneuvering Together, Apart, and at Odds: Residents’ Care Convoys in Assisted Living. J Gerontol B Psychol Sci Soc Sci. 2018;73(4):e13–e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kemp CL, Ball MM, Perkins MM, Hollingsworth C, Lepore MJ. “I get along with most of them”: direct care workers’ relationships with residents’ families in assisted living. Gerontologist. 2009;49(2):224–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ayalon L, Roziner I. Satisfaction with the relationship from the perspectives of family caregivers, older adults and their home care workers. Aging Ment Health. 2016;20(1):56–64. [DOI] [PubMed] [Google Scholar]
- 16.Franzosa E, Tsui EK, Baron S. “Who’s Caring for Us?”: Understanding and Addressing the Effects of Emotional Labor on Home Health Aides’ Well-being. Gerontologist. 2019;59(6):1055–1064. [DOI] [PubMed] [Google Scholar]
- 17.Dean KM, Hatfield LA, Jena AB, et al. Preliminary Data on a Care Coordination Program for Home Care Recipients. J Am Geriatr Soc. 2016;64(9):1900–1903. [DOI] [PubMed] [Google Scholar]
- 18.Luz CC, Hanson KV, Hao Y, Spurgeon E . Improving Patient Experiences and Outcomes Through Personal Care Aide Training. J Patient Exp. 2018;5(1):56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muramatsu N, Yin L, Lin TT. Building Health Promotion into the Job of Home Care Aides: Transformation of the Workplace Health Environment. Int J Environ Res Public Health. 2017;14(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim EY, Yeom HE. Influence of home care services on caregivers’ burden and satisfaction. J Clin Nurs. 2016;25(11–12):1683–1692. [DOI] [PubMed] [Google Scholar]
- 21.Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA. 1999;282(23):2215–2219. [DOI] [PubMed] [Google Scholar]
- 22.Schulz R, O’Brien AT, Bookwala J, Fleissner K. Psychiatric and physical morbidity effects of dementia caregiving: prevalence, correlates, and causes. Gerontologist. 1995;35(6):771–791. [DOI] [PubMed] [Google Scholar]
- 23.Ory MG, Hoffman RR 3rd, Yee JL, Tennstedt S, Schulz R. Prevalence and impact of caregiving: a detailed comparison between dementia and nondementia caregivers. Gerontologist. 1999;39(2):177–185. [DOI] [PubMed] [Google Scholar]
- 24.Kim Y, Schulz R. Family caregivers’ strains: comparative analysis of cancer caregiving with dementia, diabetes, and frail elderly caregiving. J Aging Health. 2008;20(5):483–503. [DOI] [PubMed] [Google Scholar]
- 25.Kasper JD, Freedman VA, Spillman BC, Wolff JL. The Disproportionate Impact Of Dementia On Family And Unpaid Caregiving To Older Adults. Health Aff (Millwood). 2015;34(10):1642–1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Freedman VA, Hu M, DeMatteis J, Kasper JD. Accounting for Sample Design in NHATS and NSOC Analyses: Frequently Asked Questions. 2020. https://www.nhats.org/sites/default/files/inlin-efiles/Accounting_for_the_NHATS_NSOC_Design_in_Analyses_FAQ_0.pdf.
- 27.Kasper JD, Freedman VA, Spillman BC. Classification of Persons with Dementia Status in the National Helath and Aging Trends Study: Technical Paper #5. In. Baltimore: Johns Hopkins University School of Public Health; 2013. [Google Scholar]
- 28.Sclan SG, Reisberg B. Functional assessment staging (FAST) in Alzheimer’s disease: reliability, validity, and ordinality. Int Psychogeriatr. 1992;4 Suppl 1:55–69. [DOI] [PubMed] [Google Scholar]
- 29.Halpern MT, Fiero MH, Bell ML. Impact of caregiver activities and social supports on multidimensional caregiver burden: analyses from nationally-representative surveys of cancer patients and their caregivers. Qual Life Res. 2017;26(6):1587–1595. [DOI] [PubMed] [Google Scholar]
- 30.Pristavec T The Burden and Benefits of Caregiving: A Latent Class Analysis. Gerontologist. 2019;59(6):1078–1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vick JB, Ornstein KA, Szanton SL, Dy SM, Wolff JL. Does Caregiving Strain Increase as Patients With and Without Dementia Approach the End of Life? J Pain Symptom Manage. 2019;57(2):199–208 e192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wolff JL, Mulcahy J, Huang J, Roth DL, Covinsky K, Kasper JD. Family Caregivers of Older Adults, 1999–2015: Trends in Characteristics, Circumstances, and Role-Related Appraisal. Gerontologist. 2018;58(6):1021–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wolff JL, Mulcahy J, Roth DL, et al. Long-Term Nursing Home Entry: A Prognostic Model for Older Adults with a Family or Unpaid Caregiver. J Am Geriatr Soc. 2018;66(10):1887–1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schulz R, Eden J. Families Caring for an Aging America. Washington (DC)2016. [PubMed] [Google Scholar]
- 35.Spetz J, Stone RI, Chapman SA, Bryant N. Home And Community-Based Workforce For Patients With Serious Illness Requires Support To Meet Growing Needs. Health Aff (Millwood). 2019;38(6):902–909. [DOI] [PubMed] [Google Scholar]
- 36.Walter E, Pinquart M. How Effective Are Dementia Caregiver Interventions? An Updated Comprehensive Meta-Analysis. The Gerontologist. 2019. [DOI] [PubMed] [Google Scholar]
- 37.Qualls SH. Caregiving families within the long-term services and support system for older adults. Am Psychol. 2016;71(4):283–293. [DOI] [PubMed] [Google Scholar]