Abstract
Objective:
Understanding the impact of substance use during pregnancy on fetal development and child health is essential for designing effective approaches for reducing prenatal substance exposures and improving child outcomes. Research on the developmental impacts of prenatal substance exposure has been limited by legal, ethical, and practical challenges. This study examined approaches to engage substance-using (with an emphasis on opioids) pregnant persons in research, from multi-stakeholder perspectives.
Methods:
The present study solicited the expertise of 1) an advisory group of community stakeholders, including people with lived experienced of substance/opioid use; and 2) an online survey with content experts. Qualitative analysis examined facilitators and barriers to recruiting and retaining substance-using pregnant persons through a socioecological lens at the individual, interpersonal, organizational, community, and policy levels.
Results:
Stakeholders (N=19) prioritized stigma, loss of confidentiality, legal consequences, and instability (e.g., homelessness and poverty) as important barriers that prevent substance-using persons from enrolling in research studies. Of 70 survey respondents, most self-identified as researchers (n=37), followed by clinicians (n=19), and ‘others’ (n=14). Survey respondents focused on retention strategies that build trusting relationships with participants, including incentives (e.g., transportation and childcare support), participant-friendly study design, and team-related factors, (e.g., attitudes and practices).
Conclusion:
The stakeholder input and survey data offer key insights strengthening our understanding of facilitators and barriers to research participation, and ways to overcome barriers among substance-using pregnant persons. A socioecological framework can be used to identify and address these factors to increase recruitment and long-term retention of high-risk populations.
Keywords: At-Risk Pregnancy, Opioids, Substance Use, Maternal-Infant Research, Recruitment, Retention
Introduction
Research involving pregnant persons and their children can provide unique insights into children’s cognitive, emotional, social and physical development, and may translate into better maternal and child health outcomes. Pregnant persons who use substances or have a substance use disorder (SUD) should be included in longitudinal clinical research because the long-term neurobehavioral impacts of prenatal substance exposure on fetal and child development are still poorly understood.1 Studies are needed to assess early developmental risk and resilience factors. Yet, researchers lack guidance for successfully recruiting and retaining a broadly representative sample of high-risk pregnant participants, particularly individuals with SUD, and their children. Recruiting and retaining this group require intensive and diverse engagement methods responsive to their unique circumstances and barriers. Drawing on a five-level socioecological model (individual, interpersonal, organizational, community, and policy levels), this article proposes that successful recruitment and retention efforts will address participation barriers/facilitators beyond the individual-level. Based on analysis of stakeholders and expert knowledge and beliefs, this work helps fill some knowledge gaps and makes practical recommendations, reflecting factors from every socioecological level, for navigating and mitigating potential barriers to recruitment and retention of persons who use substances during pregnancy.
This article’s recommendations are based on data from stakeholder and expert assessments that initially focused on opioid use during pregnancy. But, consistent with other reports, the data suggested that polysubstance use is frequent among persons who use opioids during pregnancy, and that barriers and facilitators to including persons who use opioids in research are broadly applicable to persons who use other substances.2 Furthermore, there is not always a bright line between the social and legal consequences of using prescribed and other legal substances during pregnancy or using illegal substances. While consumption of alcohol is legal for persons above a statutorily designated age, consuming alcohol during pregnancy can result in pregnant persons or newborns being reported to child protection authorities.3,4 In some states, women who use legally prescribed opioids will be reported to child protection authorities if their infant tests positive for that substance, although their cases may be “screened out” if no (other) risk factors for child abuse are found.5 Thus, this article refers to “pregnant persons who use substances” while recognizing that substance use is a complex, multifaceted phenomenon within which distinctions can be made.
Factors that serve as barriers to research participation may also serve as barriers to engagement with health care. For example, fears of stigmatization and legal repercussions may prevent substance-using pregnant persons from research participation; these fears also serve as barriers to accessing health care, including prenatal care.6–9 Clinical events can influence research participation. For instance, people with SUD may be susceptible to earlier onset of serious medical problems and comorbidities,7 which can negatively affect both pregnancy outcomes and participation in a long-term study.10 Furthermore, people with SUD are more likely to encounter socio-economic obstacles, such as subpar transportation or family responsibilities, that interfere with both research and clinical engagement.9,11,12 Instability-related factors that affect both research participation and clinical engagement, including unsafe or unstable housing, food insecurity, and non-supportive family members, can persist despite sustained SUD recovery.13–16 Because the barriers to research and healthcare overlap, methods to overcome the significant recruitment and retention barriers specific to pregnant persons who use substances are similar to methods for overcoming barriers to clinical care.
Pregnant persons who engage in substance use face legal risks, which pose substantial barriers to research participation and to health care access for themselves and their children. There is state-by-state variation in clinicians’ and researchers’ legal duties to report maternal substance use during pregnancy, or to report the birth of an infant prenatally exposed to substances, to child protection authorities. All states incorporate some reporting requirement into their statutes, regulations, or policies; for instance, some states statutorily define child abuse or neglect to include the birth of a substance-exposed or -affected newborn.3,17 State mandates for reporting prenatal substance exposure generally place this responsibility on clinicians who treat pregnant persons and their newborns. Researchers working with pregnant and newborn participants might also be required to report.18 Such reporting can result in women losing custody of their children, having their parental rights terminated, an sometimes facing criminal charges.
Successful engagement of pregnant persons who use substances will require a nuanced understanding of the barriers they face at the individual, interpersonal, organizational, community, and policy levels. A 2018 report by the Task Force on Research Specific to Pregnant Women and Lactating Women noted that a comprehensive approach and perspective are needed to support research with pregnant persons, especially in the context of substance use.19 Consistent with Brofenbrenner’s ecological systems theory,20 the present study utilized a socioecological framework to examine the multiple determinants that serve as facilitators or barriers to engaging pregnant persons who use substances from multi-stakeholder and content expert perspectives. It is second in a series of publications aimed at providing recommendations for recruitment and retention of pregnant persons in longitudinal research. The first article was a scoping review of birth cohort studies that synthesized the published knowledge on recruitment and retention of pregnant persons.21 Based on the existing body of literature, the scoping review identified more recruitment than retention strategies, and noted a dearth of literature on strategies for engaging persons using substances while pregnant. The focus of the present work was to elicit stakeholder and expert input, including from women with lived experience of opioid use during pregnancy or early motherhood, and to better understand facilitators and barriers to recruiting and retaining pregnant women who use substances (with an emphasis on opioids) during pregnancy.
Through the lens of the socioecological model (SEM),20 we present the complex interplay of challenges and potential solutions. A socioecological framework was selected to better elucidate the range of factors influencing recruitment and retention of a substance-using pregnant person at both the individual and systemic levels. An integrated framework suggests that in order to overcome the challenges of engaging high-risk populations in research, we need to simultaneously and effectively address these barriers across multiple levels.22 SEM is a tool that can be used by others to identify and systematically address these factors in research and other contexts.
Methods
The current study uses qualitative methodology to examine facilitators and barriers to recruiting and retaining substance-using pregnant persons using a 5-factor socioecological model. A two-prong approach was utilized to obtain qualitative data, including responses from a) stakeholders, including women with lived experience who served on the study Stakeholder Advisory Committee; and b) content experts (clinicians and researchers) who were queried via online survey.
2.1. Stakeholder Advisory Committee (SAC)
The SAC was composed of diverse community stakeholders, representing 13 different organizations/groups either engaged or experienced with pregnant persons who use substances (with an emphasis on opioids) (Table 1). SAC members represented local state agencies, professional health care organizations, recovery centers, treatment providers, law enforcement, state legislators, and three women in recovery with lived experience of opioid use disorder (OUD) during pregnancy or early motherhood. SAC members were recruited locally based on their expertise and experience with OUD in pregnant women. The orientation session for SAC members was designed to give participants a clear understanding of their role and prepare them to give feedback to the research team on project processes and materials. The role of SAC members was to use their combined experience, knowledge, and expertise to explore ways for identifying and reducing barriers, and increasing the participation of pregnant persons with OUD/SUD in research.
Table 1.
Stakeholder advisory committee (SAC): Organizations and groups involved with persons who use substances (with an emphasis on opioids) during pregnancy.
| SAC Member Group/Organization | Description/Relevance |
|---|---|
| Clinicians providing obstetrical, pediatric, and general health care | Care for substance-using pregnant persons and their children and families |
| Rural Wisconsin Health Cooperative | Cooperative of Wisconsin rural hospitals aimed at improving rural healthcare |
| Wisconsin Primary Health Care Association | Association of Federally Qualified Health Centers and their partners, aimed at providing high-quality primary health care across the state. |
| ARC Community Services, Maternal Infant Program | Treatment for pregnant and parenting persons with addiction |
| United Community Center / Centro de la Comunidad Unida | Addiction treatment as well as other assistance for the Latinx community members |
| Great Lakes Addiction Technology Transfer Center | Substance use disorder information dissemination, training and technical assistance center |
| Safe Communities | Coalition of public and private sector partners aimed at improving community health, including a reduction of opioid-related harms |
| Wisconsin Voices of Recovery | Statewide peer-run movement and recovery advocacy organization |
| Wisconsin Department Children and Families | Oversees child and family welfare and Child Protective Services (CPS) |
| Wisconsin Department of Health Services | Oversees state Medicaid, peer recovery specialist certification, and opioid use disorder treatment and other health initiatives |
| Wisconsin Perinatal Quality Collaborative | Improves perinatal health outcomes and equity across the continuum for all women and infants in Wisconsin |
| Law Enforcement | Law enforcement, maintaining public order and safety |
| Peer recovery specialists | Persons with lived experience of SUD while pregnant and/or during early motherhood |
Three 90-minute SAC meetings were held within a one-year period. Two in-person and one virtual meetings used a semi-structured interview and moderated discussion format to pose salient questions in a manner consistent with focus group methodology to obtain input from stakeholders on engaging pregnant persons with OUD/SUD in research. At the first meeting (November 2019), 19 SAC members identified and prioritized the top barriers to recruitment and retention of persons using substances during pregnancy or motherhood, and brainstormed possible solutions to overcome these barriers. Each SAC member was asked to answer the question, “What are the biggest barriers that keep pregnant persons from being engaged?” and write down their top three barriers to both recruitment and retention. Each stakeholder then shared one barrier with the group. This process repeated itself until all of the perceived barriers were captured. A total of 30 unique barriers were identified through this process and listed on a large board. SAC member had three votes each which could be assigned to any of the identified barriers to help prioritize them. This prioritization was partly shaped by the barriers most commonly faced by substance using pregnant persons. Finally, members broke into subgroups of four or five individuals to brainstorm ways to overcome the top three barriers.
At the second meeting (February 2020), 17 SAC members explored three pre-designated topics in small group discussions related to recruitment and retention: (i) providing incentives to encourage participation, (ii) alleviating concerns of potential participants; and (iii) presenting controversial, challenging information in a nonthreatening way. At the third SAC meeting (November 2020), 17 SAC members provided feedback on the barriers identified through the survey of experts and prior stakeholder input to ensure that the recommendations compiled by the research team were consistent with the SAC perceptions.
2.2. Survey
A 6-item QualtricsXM survey was developed for experts in the field by the research team (EG, FH, AEZ), which included three close-ended questions about their role and three open-ended questions about relevant resources and experiences supporting the engagement of pregnant persons (especially those from underserved or substance-using groups) and their children/families in research or clinical care (Appendix 1). The survey was emailed to expert-collaborators across the National Institutes of Health (NIH) HEALthy Brain and Child Development (HBCD) initiative23 inviting them to anonymously share their “pearls” of factors that are critically important to the recruitment and retention of pregnant and postpartum persons who use substances or have a SUD. Snowball sampling was used to further issue the survey beyond known individuals selected via purposive sampling by requesting that the recipients forward the description and survey link to their contacts. Openended questions were intended to elicit salient information about factors that promote versus hinder engagement, and ways to overcome barriers to recruiting and retaining substance-using pregnant persons in research.
2.3. Data Analysis
The survey data was collected and stored on QualtricsXM, an online survey platform. Quantitative data on the survey respondent characteristics were described using descriptive statistics. Qualitative data from both the SAC meetings and survey responses were entered into a Microsoft Excel spreadsheet for manual data sorting and coding. Qualitative analysis occurred in several steps. First, data were parsed into meaning units defined as a phrase or sentence representing a unified concept. Second, the meaning units were entered into an excel spreadsheet according to each of the following predetermined categories: (i) recruitment facilitators, (ii) recruitment barriers, (iii) retention facilitators, (iv) retention barriers, (v) incentives and compensation, and (vi) study success factors. Third, a directed approach to content analysis was conducted to identify patterns of meaning within the data.24 The category is a word or concise phrase excerpted directly from the meaning unit, whereas the domain conveys a broader meaning. The theme is the broadest categorization of the meaning unit. Fourth, the socioecological model (SEM) served as a framework to identify five levels of socioecological influence for recruiting and retaining substance-using pregnant persons in research: (i) individual, (ii) interpersonal, (iii) organizational, (iv) community, or (v) policy. Operational definitions were determined for each of the SEM influence levels and applied to each meaning unit. Table 2 shows, as an example of the content analysis, the scheduling-related retention facilitators, which correspond with the organizational level of influence. Validity of the content analysis was achieved by utilizing multiple classifiers to arrive at an agreed upon definition of each specific category. Last, exemplary quotes were selected to highlight key themes for each level of influence.
Table 2.
Content analysis for scheduling-related retention facilitators that correspond with the organizational level of influence.
| Theme | Domain | Category | Meaning Unit |
|---|---|---|---|
| Scheduling | Timing | Weekends / Off hours | Data collection on weekends/off hours |
| Scheduling | Timing | Evenings / Weekends | Be flexible (e.g., evenings, weekends) when research visits take place as the protocol allows and assuming confidentiality can be maintained. |
| Scheduling | Timing | Around school times | Plan around school times |
| Scheduling | Flexibility | Hard-to-reach groups | Flexibility seems to be important to the recruitment/retention of underserved/hard-to-reach groups, including pregnant persons with a substance use disorder. |
| Scheduling | Flexibility | Timing | Help support as many aspects of getting to the study appointment (e.g., flexibility in timing) |
| Scheduling | Flexibility | Multiple options for follow-up | Have multiple options for follow-up visits (in-person, phone, online, after work, etc.) |
| Scheduling | Flexibility | Multiple rescheduling | Create a protocol that allows for multiple rescheduling/cancellations |
| Scheduling | Flexibility | Multiple rescheduling | Be super flexible with visit times and dates (expect multiple reschedules and missed visits) as mums are often working multiple jobs |
| Scheduling | Flexibility | Scheduling appointments | Flexibility on scheduling appointments |
| Scheduling | Flexibility | Not on time (Late) | Recognize that participants will often not be on time for research visits (usually late, but sometimes early) |
| Scheduling | Efficiency | Align assessments with other appointments |
We do struggle with retention, but being mindful of their time (scheduling repeat visits around the time of other scheduled appointments at our institution) |
| Scheduling | Efficiency | Align assessments with other appointments |
Aligning assessments with routine clinic visits is ideal, while not always feasible. |
| Scheduling | Efficiency | Align assessments with childcare | Align study visits with childcare when possible |
| Scheduling | Duration | Under 1.5 hours | Keep an assessment under 1–1.5 hours is also a major factor to consider. Often studies pack so many assessments at each visit (3+ hours of testing) that the patient burden becomes a real concern and deterrent. |
| Scheduling | Duration | Split long visits | Recognize that participants may need to split long visits into two |
Results
The SAC and survey results represent two non-overlapping groups and distinct methods of gathering insight and practical experiences for identifying barriers and facilitators to engage persons who use opioids and/or substances while pregnant. Stakeholders prioritized stigma, loss of confidentiality, legal consequences, and instability (e.g., homelessness and poverty) as important barriers that prevent substance-using persons from enrolling in research studies. Of 70 survey respondents, most self-identified as researchers (n=37), followed by clinicians (n=19), and ‘others’ (n=14). Survey respondents focused on retention strategies that build trusting relationships with participants, including incentives (e.g., transportation and childcare support), participant-friendly study design, and team-related factors, (e.g., attitudes and practices). The following analysis is presented through the lens of the SEM model (Figure 1).
Fig.1.
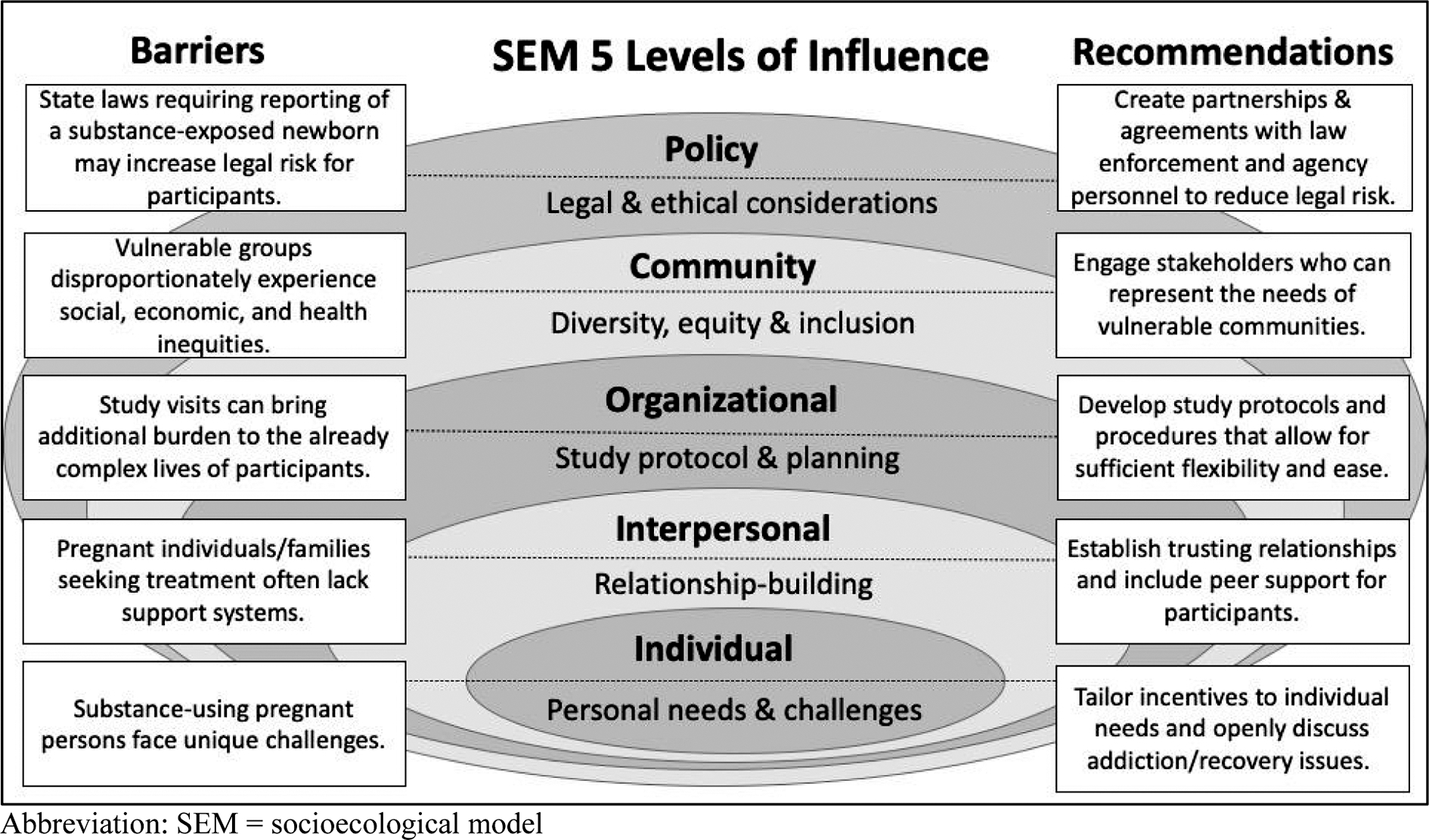
Barriers and recommendations for recruiting and retaining opioid/substance-using pregnant persons in research through the lens of the five levels of socioecological influence.
Abbreviation: SEM = socioecological model
3.1. Individual Level Influences
The individual level refers to the factors directly influencing an individual’s decision to participate in a long-term study. In this section, we identify the incentives that motivate individuals to engage in research and address the unique challenges that opioid/substance-using pregnant persons face.
3.1.1. Stakeholder Advisory Committee
SAC members emphasized the importance of retainment incentives in the form of adequate compensation (e.g., gift cards rather than cash) as well as offering safe transportation to and from study visits and childcare. There was also discussion about incentives beyond monetary ones. Stakeholders described altruism or the “power of wanting to help others” as a motivating factor for persons to enter into a research study, while others wanted to know the direct benefit for participating in the study. SAC members remarked that an emphasis on the health of the child and identifying potential health issues in order to receive early intervention, care, and resources were motivators for joining a study.
Individual level recruitment barriers highlighted by SAC members were categorized as personal apprehensions, study concerns, and health limitations. Examples of personal apprehensions included fears of being reported to Child Protective Services (CPS) and losing custody of their child, subjected to judgement and shame when disclosing substance use during pregnancy, not yet ready for recovery, and/or discovering through the study assessments any potential health/development problems with the fetus/child. Study concerns entailed navigation of the logistics associated with study participation, such as being “too busy,” fear of losing a job if work was missed due to study activities, or feeling intimidated by, or lacking sufficient knowledge about, the study. Personal health limitations, such as cognitive disabilities or persistent mental health problems that could potentially limit study participation, were mentioned as barriers.
3.1.2. Survey
Survey respondents recommended individualizing and tailoring of the study incentives to the needs of the participants. By doing this, researchers can “learn from the source population what questions are of interest, what the motivating factors for participation will be, and what the best incentives/rewards for retention will be, i.e., what are we offering these persons and families that is helpful and will make participation meaningful or at least worthwhile and at the very least not harmful?” For example, studies can offer “free, good quality housing and food services for pregnant [persons] with significant/dire financial need; especially pregnant with children” and prioritize recipients based on their socioeconomic needs and number of dependents.
Adequate financial incentives were identified by the vast majority of respondents as a key retention strategy. Among approaches discussed, compensation by cash, stipends or gift cards were mentioned. In addition, bonus compensation for completing all assessments and/or a progressing compensation schedule for participation in longitudinal studies were deemed as worthwhile retention strategies. One participant cautioned, “Offer fair compensation for research visits and don’t assume that persons with SUDs will respond for less because many are low socioeconomic status.” Transportation and childcare were equally important. While transportation and budgeting for cabs and ride share programs as well as providing childcare during the study appointments were widely acknowledged, specific needs of participants with low socioeconomic status (SES) were emphasized. For example, “Low SES participants often have less control over their time due to transportation issues and limited childcare”.
The diverse social circumstances of study participants require reimbursement to be customized, since researchers have “found that checks or other incentives that were mailed to them were not feasible as many could not cash the checks nor had reliable permanent mailing addresses,” often due to the lack of a bank account and housing stability. Instead, compensation in the form of care items for mother and/or child were recommended, including baby products, such as diapers and food packets. Additionally, other proposed means of compensation included “providing participants with well-vetted and up-to-date community resources, including facilitating their access to these when appropriate (e.g., with phone calls)” as well as access to medical and supplemental services that provide meaningful information to the family, including ongoing feedback on their child’s development. One survey respondent stated that, “Incorporating tests which can provide meaningful feedback to families on child development (as opposed to ‘experimental assessments’ only) is a major incentive. Thus, allocating budgets not just for research activities, but for developmental specialists/clinical psychologists available to cohort participants, would be crucial. Access to services (beyond a simple ‘referral’) is also crucial. Nobody will bring children for 10 years if they don’t get a sense that they are getting something tangible out of this (compensation is not an adequate motivator).”
3.2. Interpersonal Level Influences
The interpersonal level is focused on creating trusting relationships between researchers and participants, enhancing social relationships with family members, and building rapport with providers, clinics, and other study partners. In this section, we elaborate on what constitutes a trusting relationship and how to maintain that trust in the context of a research study with opioid/substance-using participants.
3.2.1. Stakeholder Advisory Committee
SAC members identified that participants may fear that their involvement in the study could negatively impact relationships with partners, family, or friends. There was also concern about the potential lack of a personal or trusting relationship with the researcher. SAC members discussed ways to provide support for participants, including having a study advocate, a social worker, or peer support person. Several topics that stakeholders felt should be discussed with participants during the consent process included confidentiality and privacy (e.g., CPS reporting), study duration, impact on work or school, and specific details of any possible negative effects from testing (e.g., imaging studies, biospecimens, behavioral assessments). They also felt that the approach to reporting incidental findings and/or false negatives/positives test results should also be addressed early. SAC members emphasized communication and relationship building. Areas of emphasis included expressing how valuable a participant’s participation is while acknowledging any concerns and compassionately presenting potentially stressful information.
3.2.2. Survey Results
At the interpersonal level, one concept emphasized by the respondents was the importance of selecting appropriately matched study personnel to facilitate recruitment and, later on, retention. Specifically, it was stated that research staff should have adequate time for recruitment, and ideally should come from the same community and the same racial/ethnic background as the targeted study population. Recruitment by a trusted healthcare professional was also advised as effective. Respondents recommended having multiple ways to contact study participants, including requesting several alternate contacts, such as family or friends. Establishing a relationship with family members was also recommended to encourage continued participation. One respondent advised “providing referrals/other support for families under stress” as a way to build rapport and promote retention.
Respondents shared many general comments on study success factors, of which the predominant theme was building an authentic, personal relationship with study participants. They elaborated on the essential qualities of the study staff, such as their relational impact and attitudes describing staff attitudes of being welcoming, respectful, non-judgmental, positive, and compassionate. Continuity among study staff was also deemed as important. Additionally, hiring support staff (e.g., to provide transportation) who come to know the families can be considered. One respondent noted, “We eventually ended up with one cab driver who knew us and also became a familiar person to the families.” Practices to maintain strong positive relationships with study participants included personalized birthday, holiday or congratulation cards after a birth, or study “scrap books” documenting child’s milestones and progress during the study. Others advised monthly or end of the year newsletters sent to the participants.
3.3. Organizational Level Influences
In this section, we focus on approaches to allow for flexibility and ease of implementation, including timing of recruitment; coordinating research and clinical activities; communicating clearly crucial information in the consent and other study materials; ensuring availability and ease of referrals to services; allowing for flexibility with assessment timing and settings; reducing overall ‘participant burden’, and providing availability of different types of communication methods.
3.3.1. Stakeholder Advisory Committee
Stakeholders identified several organizational level barriers and challenges related to preserving confidentiality, including presenting clear, comprehensible, and comprehensive information in the consent and other study materials; maintaining contact with participants over a decade; and addressing potential concerns and risks associated with planned evaluations (e.g., magnetic resonance imaging). Providing an adequate description of procedures, such as biosampling (e.g., purpose of analysis, specific targets of interest, invasiveness) and neuroimaging procedures (e.g., safety, incidental findings) were of particular importance.
SAC members also advised that presenting stressful information to potential participants can be overcome by offering clear and explicit information about assessments, including potential risks and how they will be mitigated; addressing safety concerns in advance; and providing more support and additional services and resources for participants. For example, informed consent should require inclusion of the standard language about risk-benefit assessment for all procedures and mandatory reporting requirements, and such language needs to be supplemented with the support infrastructure and resources available to study participants. Availability of referrals to services (e.g., medical, social, legal) for study participants were highlighted as a “must have”. For higher-risk participants, assistance with access and coordination of often fragmented medical services, treatment and recovery coaching, finding housing, childcare, and other social services are paramount. Early identification of developmental delays and other health issues, with an adequate referral base for services, was identified as an important motivator for joining a study.
3.3.2. Survey
Recruitment facilitators included a discussion about optimal timing of recruitment during pregnancy with somewhat divergent opinions. Some respondents noted that recruitment during the hospital stay after labor and delivery might be both logistically easier and will reduce selection biases due to varying access to prenatal care and referral patterns. Other respondents suggested that mid-pregnancy may be the best time to obtain consent from participants for research studies. The same respondent suggested avoiding recruiting patients within six weeks before delivery or six weeks postpartum stating that, “This time is stressful, and they will be less engaged in non-essential tasks. Maximize patient convenience.” Recruitment at the scheduled prenatal care appointments rather than at a separate visit was identified as a major facilitator. Engagement of community organizations serving pregnant persons as well as recovery organizations were identified as additional facilitators.
Retention facilitators, such as home visits and study procedure flexibility, were identified as the most common among numerous experts, such as “budget for outreach to do home visits if lost to follow-up” and, “help support as many aspects of getting to the study appointment (e.g., home visits)”. Respondents emphasized that the study team needs to anticipate missed visits and create protocols for multiple rescheduled visits/cancellations. Providing a variety of options for follow-up visits, e.g., in-person, by phone, online, weekends and evenings, was viewed as a key facilitator. One respondent emphasized that this is particularly pertinent to vulnerable populations, stating, “flexibility seems to be important to the recruitment/retention of underserved/hard-to-reach groups, including pregnant [persons] with a substance use disorder”. Alignment of study visits with other clinic appointments, such as well child visits, and keeping them under 1–1.5 hours were mentioned as other key considerations. Taking into account potential custody changes (“Many studies lose all of their children placed in foster care”) and allowing for flexibility with biospecimen collection, (“Allowing [participants] to refuse collection of certain specimens or specific assessments, which are concerning to them, also allows for more flexibility with the design (can be accomplished by checkboxes on the consent”) were identified as additional retention facilitators.
Other study success factors included annual study meetings with a reception for nursing staff involved in research activities. Involvement of a physician prescribing medication for opioid use disorder, who can help to facilitate recruitment, and on-site “engagement specialists” were also mentioned. “These specialists were typically those with prior SUD and from the local community. This immediate warm hand-off was very effective in getting persons into treatment and could be helpful in getting persons engaged in research.” In addition, the need for trauma-informed care training for staff was identified due to the high incidence of posttraumatic stress disorder among individuals with SUD. Specific communication strategies with study participants emphasized the availability of different types of communication modes, e.g., in-person, phone, text, and electronic, access to the study team, and use of language that participants can understand, such as “not too difficult, not upper-class”.
3.4. Community Level Influences
The community level addresses the economic and social conditions that influence individual and group differences by designing studies that promote diversity, equity, and inclusion. In this section, we explore the social environment and inequities that certain groups and communities face. For example, there are factors specific to vulnerable and underserved, (e.g., opioid/substance-using, minority and low-income) populations that should be considered when designing a research study.
3.4.1. Stakeholder Advisory Committee
SAC members identified poverty (specifically housing instability and homelessness) as a key community level barrier for enrollment of pregnant persons, especially those underserved or with SUD. Other important enrollment barriers highlighted lack of access, cost of medical resources, and incarceration status as resulting in inconsistency of treatment. Additionally, having a minority identity can lead to stress from potential stigma and discrimination associated with one’s language and/or culture, citizenship status, and/or sexual orientation and gender identity. Other community-level motivators were engaging single mothers to participate in imaging, testing, and studying of their infant or young children. Suggestions included an awareness of networks, which could assist with housing or child safety, financial incentives, and the use of common, inclusive and specific language to explain study details.
3.4.2. Survey
Survey respondents recommended recruitment facilitators at the community level that were focused on “doing community outreach in the form of free informational classes on topics of interest to the participant population,” or by making “sure the community knows about this study, and have the proper information to be able to support it.” It is also beneficial to engage community organizations, which have already built trusting relationships with potential study participants, and members representing the targeted vulnerable or at-risk population. Examples of these community organizations included: addiction treatment programs; recovery houses; social service nonprofit agencies that offer housing, counseling, or job services; pregnancy specific organizations, such as Planned Parenthood; or park and recreation agencies offering programs and activities to multicultural, racial or ethnic communities, members of the LGBTQ+ community or refugee and immigrant communities. Social impediments of recruitment largely focused on poverty and housing instability, including homelessness.
The reported retention-related challenges were similar to those identified for research recruitment. Distrust in research and the academic system can hinder participants from remaining in a study (“[there are] significant challenges with gaining the trust of our native families and tribal leadership (for good reason, as I am a white physician).” Suggestions at the community level for study success focused on navigating health literacy and language barriers. For example, one respondent suggested that, “having research staff available in the clinic waiting rooms to help persons with literacy issues (‘would you rather I asked you the questions or you can complete yourself?’)” and hiring multilingual research staff are critical components of study success. Additionally, when needed, providing language support through an in-person rather than using telephone interpreter services was emphasized.
3.5. Policy Level Influences
The policy level identifies and confronts the legal and ethical concerns related to pregnancy and opioid/substance use issues and the barriers that these may present to a pregnant person who is potentially interested in joining a long-term study. In this section, we emphasize the need to work across sectors to increase the support for and access to services that pregnant persons in this situation may need, and how researchers can help minimize the impact of these issues.
3.5.1. Stakeholder Advisory Committee
Stakeholders identified “the fear of legal consequences” and “the fear of being reported to Child Protective Services” as two significant policy-level barriers that may prevent persons from participating in the study. Stakeholders emphasized the importance of building relationships with local criminal justice officials, including police officers and sheriffs, prosecutors, judges, and parole departments, and agreed that partnering with these professionals would be motivating for persons by potentially offering deferred prosecution options. However, it is important to be realistic with both treatment accessibility and overpromising legal benefits, which could become a coercive method for encouraging research participation. Peer support can also be helpful to assist persons with navigating the law. Stakeholders emphasized the importance of confidentiality in alleviating a person’s concerns about reporting substance-use and consequently losing custody of one’s children. Another stakeholder suggested informing participants that disclosures are “sacred information” that no one outside of the study will have access to, which may encourage persons to be more truthful. These concerns should be directly addressed during the recruitment and consent process and require building a strong foundation of trust between research staff and study participants.
3.5.2. Survey
Survey responses at the policy level focused on how local policies and protocols of government agencies, such as CPS, impact the participation of substance-using pregnant persons. During the recruitment stage of the study, the state- and local-level punitive approaches to substance use may dissuade pregnant persons from enrolling in a study, especially when the study evaluates substance use. One respondent compared their experience between working in communities with supportive versus punitive policies noted that, “[having] practiced in the past in a state that did not report [persons] for substance abuse and use was not grounds for civil commitment. These policies [e.g., mandatory reporting, the possibility of losing custody] are a critical hindrance to [a person’s] self-disclosure.” Furthermore, study retention can be hindered by the involvement of CPS. One respondent noted that stringent CPS reporting protocol presented a barrier to retention stating, “I have struggled with CPS and their unwillingness to engage with us on removing mandatory prenatal reporting of SUD as prenatal child abuse.” In order to overcome this barrier, one respondent recommended building a partnership with CPS that can help studies navigate reporting requirements or child custody changes.
Discussion
The present study extended beyond the published literature by soliciting the expertise of community stakeholders via an advisory group, including persons in recovery with lived experience of SUD during pregnancy or motherhood, and health care practitioner and researcher experts via a survey. The perspectives of stakeholders and content experts offered key insights and actionable strategies for recruiting and retaining opioid/substance-using pregnant persons in long-term research studies. Expert input provided more information on retention strategies when compared to the published literature, which focused more on the recruitment methods. A synthesis of stakeholder and survey responses of content experts that highlights critical concerns and obstacles and how to overcome them, for effective recruitment and retention of opioid/substance-using pregnant persons, is presented in the discussion below.
4.1. Tailoring incentives to individualized needs and addressing personal challenges (individual level influences)
The conundrum for researchers at this influence level is twofold; one, to incentivize and appeal to what is personally motivating for individuals and two, to help them overcome actual and perceived limitations that may prevent them from entering into a study. Some of these issues can be best addressed by tailoring incentives to meet the basic needs of individuals. Stakeholders, who are representative of and well-versed in understanding the target population, can assist with identifying priority needs. Conveying an empathetic understanding to potential participants of the difficulties that are likely to accompany substance use will be crucial in meeting them where they are at. In addition, providing adequate (yet not coercive) reimbursement for study participation should promote rather than hinder recovery and wellness.
Our findings reinforced the importance of using non-stigmatizing language and recognizing that SUD-related self-shame and stigma are common for pregnant persons who are using substances.25 This is consistent with the literature, which documents stigma toward people with SUD as an endemic societal problem and causes those affected to internalize self-shame.26 Substance use during pregnancy can heighten internalized self-shame due to the realization of being unable to stop using substances while carrying the fetus. Stigma, self-shame and apprehension of being harshly judged can cause those affected not to seek appropriate health care and may hinder recruitment in long-term studies. Providing training for research staff that promotes sensitivity to addiction/recovery issues could help reduce the impact of stigma and unconscious biases among research team members and facilitate recruitment and retention.
4.2. Building relationships (interpersonal level influence)
Building and maintaining strong relationships with participants is paramount for retention. Both stakeholders and survey respondents shared similar views that establishing an authentic, personal connection that communicates respect and non-judgement, and honors each participant as an individual is key. Investigators should carefully select research staff who can relate to participants and provide the warm, personal attention, which, in turn, can promote continued research engagement of participants. Ideally, research staff are individuals, who are trusted in the community, and knowledgeable about the community as well as research. Similar to clinical care, the interaction between research staff and participants should be gender- and trauma-informed and person-centered. Organizers should also consider the interpersonal impact that participation may incur by creating systems to deal with specific barriers (e.g., complex informed consent procedures; anxiety about the impact of study participation on social/family relationships or employment). Establishing relationships with other family members and including peer support persons and study advocates to assist participants with navigating the study as well as recovery processes can help to counter potential barriers.
4.3. Designing flexible study protocols (organizational level influence)
Concordant with the literature, integration of research activities into the daily practices and activities of a busy clinical practice can be challenging.27 Some of these barriers include the coordination of research and clinical assessments as well as securing support and buy-in from clinic staff and leadership. Identifying designated liaisons among clinical personnel who can coordinate recruitment activities along with research staff or paying an honorarium to clinical staff can be helpful.28,29 It is also important to work closely with clinic administrators to ensure that the study does not increase burden for clinic staff and providers. Eliciting input early on in the study design as to what would work best for the clinic and to adjust the study ongoing to better align with the clinic flow is recommended.
For pregnant and postpartum persons, often a major barrier is balancing the increasing demands of a growing family with multiple study visits. These concerns are even more pertinent to vulnerable groups who may lack reliable transportation, housing, social support, and access to health care and community resources. In addition, flexibility in the work schedule to accommodate study visits, legal challenges (e.g., incarcerations, change in custody) and medical needs (e.g., increased unplanned hospital visits due to medical conditions of the mother and/or infant) present additional barriers.
Thus, developing study protocols and procedures that allow for sufficient flexibility both for research personnel and study participants is crucial. Such flexibility can be achieved by utilizing different forms of study visits (e.g., at the clinic, at home, on-line, by phone), broader evaluation windows, which can accommodate the need for multiple rescheduled visits and shorter, less burdensome assessments, and availability of the study team outside normal working hours to contact the participants and conduct certain evaluations. A study design would benefit from a priori planning for the approach to custody changes for children-participants, and referrals and/or access to medical, legal, and social services. Assurance of confidentiality, adequate compensation, and assistance with transportation and childcare are equally crucial. From the research team perspective, allocating sufficient resources and time for ongoing training and recognition of research and clinical staff are important for long-term study success.
4.4. Promoting diversity, equity, and inclusion (community level influence)
The community level of the socioecological model promotes diversity, equity and inclusion through deliberate strategies, which account for the needs of individual members of a given community. The inequities arising from social, economic, environmental, and structural disparities that disproportionately affect certain groups and communities include socioeconomic status, health literacy, and food insecurities, to name a few.30 To overcome these barriers, the approach should be individualized and focused on increasing access to health care and resources. This can be accomplished by engaging community stakeholders from diverse sectors, including persons with lived experience of SUD during pregnancy or early motherhood, and trusted community organization representatives that have already established positive, trusting relationships with substance-using pregnant persons. For example, stakeholder partners connected to addiction and obstetric treatment programs, and recovery, harm reduction or advocacy groups can assist with engaging vulnerable populations to join the study. Incorporation of community stakeholder feedback should be sought early on – ideally from the study inception and design phase – so that the study methods and execution can meet the needs of the target population rather than applying “one-size fits all” strategies. This targeted approach can include provision of resources in multiple languages, referral and/or access to medical, legal and social services, or incentives that meet the needs of vulnerable and underserved groups historically underrepresented in research.
4.5. Navigating legal and ethical considerations of opioid/substance use (policy level influence)
A nationwide study aiming to include persons who may face drastic legal and social risks should their substance use during pregnancy be discovered requires effective, well-articulated ethical-legal guidance to help prevent and minimize potential harms to participants. Unless researchers incorporate legal knowledge into the study design and governance, pregnant participants who use opioids and/or other substances could be put at substantial risk of civil commitment, arrest, losing custody of newborns and other children, having their parental rights terminated or even facing criminal prosecution. Pregnant persons who use substances are already vulnerable and at risk for negative legal and social repercussions, however study participation should not exacerbate these risks.
Adequately protecting participants against legal risks may require researchers to execute agreements (e.g., memoranda of understanding) with state and local authorities. Such agreements should be executed in advance of study recruitment. They clarify when and whether state statutes will apply to researchers and their participants and, in may exempt the research from enforcement of some state statutes. Appropriate agreements could minimize the possibility that participants who are in treatment would be arrested for drug-related crimes. Some jurisdictions offer deferred prosecution agreements (DPA) to persons arrested for drug crimes. Under a DPA, if a person fulfills the promise to live by a certain set of rules or conditions for a specified period, the prosecution is dropped and the case is dismissed.31 Local prosecutors usually have discretion regarding DPAs. When possible researchers and their institutions would be well-advised to educate local prosecutors concerning the study and negotiate agreements favoring DPAs for research participants.32 However, a study cannot ensure or guarantee that participation would lead to a DPA, or use the possibility of a DPA as a recruitment incentive, as doing so could unduly influence a person’s decision to participate in the study and therefore violate federal regulations for the protection of human participants in research (the Common Rule).33
Protecting participants’ privacy and confidentiality has instrumental value for minimizing risks, demonstrates respect for participants, and is required by the Common Rule. In any National Institutes of Health (NIH)-funded study that gathers data about substance use during pregnancy, the participant’s privacy would be protected by an automatically granted certificate of confidentiality (CoC).34,35 The CoC prohibits researchers from disclosing identifiable, sensitive study information to persons “not connected with the research”, unless the disclosure is required by law or participants consent to disclosure of information about themselves.36
Privacy and confidentiality must be balanced against other important values, such as preventing harm to participants or others, or providing a benefit such as a medical referral. For instance, as an ethical matter a study involving participants who use substances during pregnancy should refer such persons for treatment and other needed services, if participants are not already receiving these services. To make such referrals, study personnel might need to disclose a participant’s name and some substance use information. Alternatively, if participants screen at high risk as a danger to themselves, e.g., as high risk for suicide, researchers have ethical obligations to refer them for help. Referrals for treatment and services generally are not mandated by law, and therefore to comply with the CoC law while undertaking the ethically preferred action, researchers need to obtain consent from participants to disclose some identifiable, sensitive information should the need arise.
On the other hand, statutes in nearly all states require researchers to report child abuse (not involving prenatal substance exposure) to CPS, and such reporting requirements would supersede the protections of the CoC. Nonetheless, as a matter of respect and to fully inform prospective participants of the study’s risks, the informed consent process and forms should clearly indicate that researchers would be required to report child abuse.
Despite the research project’s attempts to decrease participants‟ research-related legal risks, participants who use substances during pregnancy might still be reported to CPS by persons not associated with the study (e.g., participants‟ health care providers or social workers). Such reporting might be required by law or institutional policy or might reflect the reporter’s personal conscience in situations where reporting is legally permitted but not required. To minimize such risks, researchers might work with institutions to educate non-research personnel about when the law requires versus merely permits reporting, about options other than reporting, and about the research project’s mechanisms for treatment referrals. If a hospital or other institution’s policy requires reporting even when the law does not, researchers might negotiate with the institution to suspend its policy with respect to research participants.
Some state legislators, agency personnel (e.g., CPS or department of health agencies), law enforcement, and penal officials are involved in developing or implementing policies, programs, task forces, or legislation related to substance use and recovery. These individuals may be supportive of research to develop an evidence base on which they could draw. Project sites could include some such individuals as advisors or board members, as they can aid the project in navigating relationships with governmental actors and executing legal agreements, which will minimize risk to research participants.
A robust yet “user-friendly” consent and permission process will be crucial for any complex, longitudinal study involving persons who use substances during pregnancy and their infants. The study processes and informational materials should promote participants’ comprehension of the nature of the research, including the wide variety of study assessments and activities, and of the risks and burdens associated with study participation. Consent form text should be readable and comprehensible for all participants. To the extent possible, consent methods and formats should be evidence-based. Videos that describe study processes, and econsenting should be considered and tested. Study personnel must understand the study’s social and legal risks, the project’s methods for mitigating them, and any limitations on participants’privacy and confidentiality. Study personnel must be able to explain these points during the consent process and any time thereafter. Truthfully and comprehensibly explaining the projects’ data gathering activities, and its risks and burdens, will be crucial for operationalizing the principle of respect for persons and the ethical value of trustworthiness.
Limitations
Limitations of this study may constrain generalizability of our results. A convenience sample that represented responses from the content experts, predominantly clinicians and researchers, was used to obtain survey responses. The racial/ethnic composition of respondents was not assessed. Further, the relatively small sample size (N = 70) limited our ability to compare and contrast responses from different groups of survey respondents (e.g., clinicians versus researchers). Additionally, SAC members were selected from one state and, while they represented diverse expertise, their recommendations could be influenced by local context and state laws and frameworks specific to that clinical population. Another possible limitation is one inherent to qualitative data analysis. To increase objectivity and limit bias, we involved multiple people from diverse backgrounds (e.g., sociology of law, medicine, behavioral health) who worked collaboratively to develop the coding themes and achieve agreement between the coders. In addition, the findings were reviewed with SAC members for their input prior to finalizing the recommendations. Although the focus of our advisory group and expert survey was to gather input based on their experience and expertise working with persons who primarily use opioids during pregnancy, there is some overlap of the concerns and challenges that pregnant persons with broader substance use disorder may face.37 Further, it is common for people with addiction to use more than one substance.38 Still, there may be substance-specific considerations for the recruitment and retention of pregnant persons that constitute an important area for future research.
Conclusion
Findings from this study can strengthen our understanding of the barriers that can deter opioid/substance-using pregnant persons from research engagement in long-term studies. We should design studies in a way that meets the fundamental needs of this vulnerable population and facilitates participation by investing time and resources in creating a viable protocol that retains participants. Moreover, study protocols that are tailored to individual needs and preferences can promote successful oversampling of high-risk populations. Getting to know the target population by partnering with the communities and vital stakeholders, who are well-versed in the needs of substance-using pregnant persons, appear to be crucial ingredients of effective recruitment and retention. Additionally, it is critical to partner with legal advisors and social services for assistance with negotiating complex legal and ethical situations, which are commonly encountered by opioid/substance-using pregnant persons. Finally, peer support partners can assist participants to navigate and prevent potential pitfalls and to prepare researchers for the unforeseen challenges at every socioecological level of influence that, in turn, can improve overall engagement and retention efforts. A socioecological lens can be an especially helpful tool in strategically planning for a long-term birth cohort study focused on substance-using pregnant persons.
Acknowledgments
We would like to express our gratitude to the members of the stakeholder advisory committee and the survey respondents who generously provided guidance and expertise during this study.
Funding:
Research reported in this publication was supported by the HEALthy Brain and Child Development (HBCD) Study funded by the National Institutes of Health (NIH) Helping to End Addiction Long-term (HEAL) Initiative (https://heal.nih.gov/) and (National Institute on Drug Abuse (NIDA) and National Institute of Neurological Disorders and Stroke (NINDS)) under award numbers: R34DA050237, R34DA050254, R34DA050263, R34DA050270 and R34DA050341. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations:
- SEM
Socioecological Model
- SUD
Substance Use Disorder
Appendix 1. Survey of the Experts in the Field
Do you have suggestions for published articles and other resources that we should not miss when compiling the recommendations for engaging pregnant persons (especially those from underserved or drug using groups) and their children/families in a decade-long birth cohort study? If yes, please list these articles / resources.
Please list your clinical or research related “pearls” for supporting engagement of pregnant persons (especially those from underserved or substance-using groups) and their children/families in research or clinical care. Factors that promote versus hinder engagement, and ways to overcome barriers to engagement, are often similar in research and clinical care. Please share with us anything that may help guide the “blueprint” recommendations (for example: “I found [this approach] useful.” “I quickly learned that [this approach] can negatively impact recruitment or retention.”).
Please describe your background, from which you drew to offer your suggestions and “pearls”.
In addition, please mark all that apply:
-
I am a researcher Y/N
-
a.a.
working with pregnant persons who use drugs Y/N
-
a.b.
working with children whose parent(s)/guardian(s) use drugs Y/N
-
a.c.
working with individuals with addiction Y/N
-
a.d.
other:
-
a.a.
-
I am a professional working with individuals affected by drug use Y/N
-
I am a health care professional Y/N
-
i.a.
working with pregnant persons who use drugs Y/N
-
i.b.
working with children whose parent(s)/guardian(s) use drugs Y/N
-
i.c.
working with individuals with addiction Y/N
-
i.d.
other:
-
i.a.
I am a law enforcement or criminal justice field professional Y/N
I am a public health agency professional Y/N
-
I am an advocacy organization member Y/N
Please specify the name of this organization:
-
I am a person with a lived experience (e.g., personal or close family member) of addiction recovery Y/N
Footnotes
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ross EJ, Graham DL, Money KM, Stanwood GD. Developmental consequences of fetal exposure to drugs: what we know and what we still must learn. Neuropsychopharmacology. 2015;40(1):61–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roth D, Loudin S, Andrews L, Evans J, Davies TH. Inclusion of Positive Self-reporting by Mothers of Substance Exposed Neonates Increases the Predictability of NAS Severity Over Toxicology Alone. Matern Child Health J. 2020;24(3):340–350. [DOI] [PubMed] [Google Scholar]
- 3.Child Welfare Information Gateway. Parental substance use as child abuse. 2020; https://www.childwelfare.gov/pubPDFs/parentalsubstanceuse.pdf.Accessed November 16, 2020.
- 4. Minn. Stat. Ann. §260E.31 (West 2021).
- 5.Wood KE, Smith P, Krasowski MD. Newborn drug testing practices in Iowa birthing hospitals. J Neonatal Perinatal Med. 2017;10(4):445–450. [DOI] [PubMed] [Google Scholar]
- 6.Stone R Pregnant women and substance use: fear, stigma, and barriers to care. Health Justice. 2015;3:2. [Google Scholar]
- 7.Louw K-A. Substance use in pregnancy: The medical challenge. Obstet Med. 2018;11(2):54–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Friedman SH, Heneghan A, Rosenthal M. Characteristics of women who do not seek prenatal care and implications for prevention. J Obstet Gynecol Neonatal Nurs. 2009;38(2):174–181. [DOI] [PubMed] [Google Scholar]
- 9.Wu M, Lagasse LL, Wouldes TA, et al. Predictors of inadequate prenatal care in methamphetamine-using mothers in New Zealand and the United States. Matern Child Health J. 2013;17(3):566–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benningfield MM, Arria AM, Kaltenbach K, et al. Co-occurring psychiatric symptoms are associated with increased psychological, social, and medical impairment in opioid dependent pregnant women. Am J Addict. 2010;19(5):416–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Substance Abuse and Mental Health Services Administration. Substance Abuse Treatment: Addressing the Specific Needs of Women. Treatment Improvement Protocol (TIP) Series, No. 51. HHS Publication No. (SMA) 13–4426. Rockville, MD: Substance Abuse and Mental Health Services Administration;2009. [Google Scholar]
- 12.Brady TM, Ashley OS. Women In Substance Abuse Treatment: Results from the Alcohol and Drug Services Study (ADSS). (HHS Publication No. SMA 04–3968, Analytic Series A26). Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies;2005. [Google Scholar]
- 13.Koegel P, Sullivan G, Burnam A, Morton SC, Wenzel S. Utilization of mental health and substance abuse services among homeless adults in Los Angeles. Med Care. 1999;37(3):306–317. [DOI] [PubMed] [Google Scholar]
- 14.Robertson MJ, Zlotnick C, Westerfelt A. Drug use disorders and treatment contact among homeless adults in Alameda County, California. Am J Public Health. 1997;87(2):221–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Havens JR, Simmons LA, Shannon LM, Hansen WF. Factors associated with substance use during pregnancy: results from a national sample. Drug Alcohol Depend. 2009;99(13):89–95. [DOI] [PubMed] [Google Scholar]
- 16.Schempf AH, Strobino DM. Illicit drug use and adverse birth outcomes: is it drugs or context? J Urban Health. 2008;85(6):858–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guttmacher Institute. Substance Use During Pregnancy. 2020; https://www.guttmacher.org/state-policy/explore/substance-use-during-pregnancy.Accessed November 16, 2020.
- 18.Resnik DB, Randall DC. Reporting suspected abuse or neglect in research involving children. J Med Ethics. 2018;44(8):555–559. [DOI] [PubMed] [Google Scholar]
- 19.Task Force on Research Specific to Pregnant Women and Lactating Women: Report to Secretary, Health and Human Services Congress. September2018; https://www.nichd.nih.gov/sites/default/files/2018-09/PRGLAC_Report.pdf.Accessed Oct 16, 2020.
- 20.Bronfenbrenner U, ed Making human beings human: Bioecological perspectives on human development 106–173 ed: Sage Publications Ltd; 1992. [Google Scholar]
- 21.Goldstein E, Bakhireva LN, Nervik K, et al. Recruitment and retention of pregnant women in prospective birth cohort studies: A scoping review and content analysis of the literature. Neurotoxicol Teratol. 2021:106974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Salihu HM, Wilson RE, King LM, Marty PJ, Whiteman VE. Socio-ecological Model as a Framework for Overcoming Barriers and Challenges in Randomized Control Trials in Minority and Underserved Communities. Int J MCH AIDS. 2015;3(1):85–95. [PMC free article] [PubMed] [Google Scholar]
- 23.National Institutes of Health. HEALthy Brain and Child Development Study. https://heal.nih.gov/research/infants-and-children/healthy-brain.Accessed Nov 5, 2020.
- 24.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. [DOI] [PubMed] [Google Scholar]
- 25.Zgierska AE, Miller MM, Rabago DP, et al. Language Matters: It Is Time We Change How We Talk About Addiction and its Treatment. J Addict Med. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hammarlund R, Crapanzano KA, Luce L, Mulligan L, Ward KM. Review of the effects of self-stigma and perceived social stigma on the treatment-seeking decisions of individuals with drug- and alcohol-use disorders. Subst Abuse Rehabil. 2018;9:115–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Verhoef MJ, Mulkins A, Kania A, Findlay-Reece B, Mior S. Identifying the barriers to conducting outcomes research in integrative health care clinic settings--a qualitative study. BMC Health Serv Res. 2010;10:14–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Manca DP, O’Beirne M, Lightbody T, et al. The most effective strategy for recruiting a pregnancy cohort: a tale of two cities. BMC Pregnancy Childbirth. 2013;13:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Monk AR, Tracy SK, Foureur M, Tracy M. Evaluating midwifery units (EMU): lessons from the pilot study. Midwifery. 2013;29(8):845–851. [DOI] [PubMed] [Google Scholar]
- 30.National Academies of Sciences of Engineering Medicine. Communities in Action: Pathways to Health Equity. The Root Causes of Health Inequity 2017; https://www.ncbi.nlm.nih.gov/books/NBK425845/.
- 31.American Law Institute. Model Penal Code. Federal Sentencing Reporter 2018;30(4–5): 326–347. [Google Scholar]
- 32.Biro KEM, Blum G, Bourdeau J. Admission of Accused to Diversion or Deferral Program, American Jurisprudence 2d: Criminal Law, 21A, §840. 2020. [Google Scholar]
- 33.Office for Human Research Protections (OHRP). 45 CFR Part 46: Basic HHS Policy For Protection of Human Subjects. 2018; https://www.hhs.gov/ohrp/sites/default/files/revised-common-rule-reg-text-unofficial2018-requirements.pdf.Accessed November 16, 2020.
- 34.42 U.S.C. §241 (d) (2021).
- 35.National Institutes of Health Central Resource for Grants and Funding Information. Certificates of Confidentiality (CoC) - Human Subjects. https://grants.nih.gov/policy/humansubjects/coc.htm.Accessed April 5, 2021.
- 36.42 USC §241 (d)(1)(B) and (C) (2021).
- 37.Stone R Pregnant women and substance use: fear, stigma, and barriers to care. Health & Justice. 2015;3(2):1–15. [Google Scholar]
- 38.Connor JP, Gullo MJ, White A, Kelly AB. Polysubstance use: diagnostic challenges, patterns of use and health. Curr Opin Psychiatry. 2014;27(4):269–275. [DOI] [PubMed] [Google Scholar]


