Abstract
Paroxysmal finger hematoma, also known as Achenbach syndrome, is an underdiagnosed condition that causes apprehension in patients owing to the alarming appearance. It usually presents as a blue-purple discoloration of the volar aspect of one or more digits and can be associated with pain and paresthesia. This condition is benign and is usually self-limiting.
Keywords: Achenbach Syndrome, Cyanotic finger, Paroxysmal finger hematoma
A purple or blue finger or fingers can present a diagnostic dilemma for the vascular medicine and surgery specialist. Raynaud disease is a common cause of pale and blue digits. Unusual causes such as vasculitis, acrocyanosis, trauma, and subclavian artery aneurysm with thrombi should be considered in the differential diagnosis. Achenbach syndrome, also known as paroxysmal finger hematoma, is exceedingly rare and can be diagnosed by clinical suspicion, confirmed with a dampened arterial waveform. In this case series, we described three patients with Achenbach syndrome. All three included patients provided written informed consent for the report of their case.
Case report
Patient 1
A nonsmoking 48-year-old woman with a medical history of hyperlipidemia had presented to an outpatient clinic with a 7-day history of complete volar discoloration of her left index finger. She stated she had awoken with blue-purple discoloration on the digit and had presented to urgent care where she was prescribed prednisone. She denied injury or exposure to cold temperatures at the time of onset. On resolution of the original symptoms, she had developed a small spot of discoloration on the left third finger associated with point tenderness. The patient had no neurologic symptoms associated with the discoloration. Physiologic testing with arterial Doppler waveforms demonstrated results within the normal limits for the bilateral upper extremities, with a dampened Doppler waveform of the right first three digits and left fourth digit. The patient was treated with 30 days of 75 mg clopidogrel (Plavix). The patient was followed up by telephone and reported resolution of her symptoms.
Patient 2
A 68-year-old woman with a medical history of hyperlipidemia had presented to the clinic with a 3-day history of discoloration of the entire volar aspect of her left middle finger. It was associated with paresthesia and pain. She denied any weakness in the hand. The patient was a former smoker and had quit smoking <10 years before her presentation. A dampened arterial Doppler waveform was demonstrated in the right second, right third, and right fourth fingers. She was recommended to take 81 mg of aspirin daily. The patient was followed up by telephone and reported resolution of her symptoms.
Patient 3
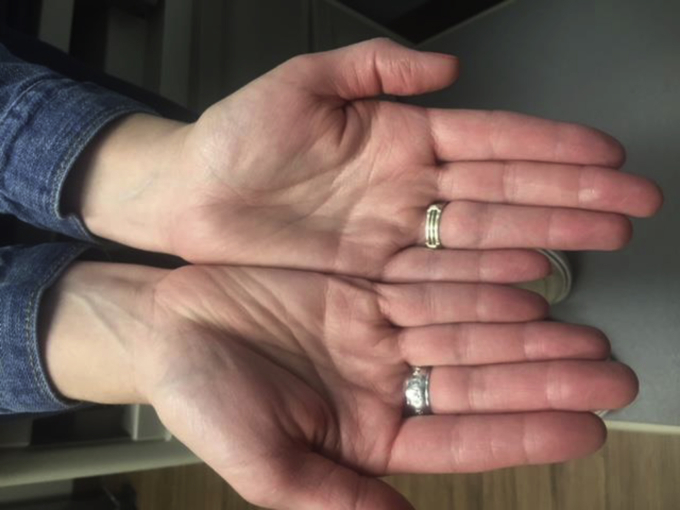
A nonsmoking, 34-year-old woman with a medical history of rheumatoid arthritis, inflammatory bowel disease, and lupus erythematosus had presented to the clinic with a 3-day duration of bruising of the volar aspect of her left third finger (Fig 1), associated with pain and tingling. She had had experienced three similar episodes in the past with complete resolution within 72 hours of onset. The physical examination revealed blue-purple color changes on the left third finger. Physiologic testing demonstrated dampening of the arterial Doppler digital waveform (Fig 2). A cold immersion test was performed, which was negative for any changes. The patient was prescribed 75 mg clopidogrel (Plavix) and was followed up 3 weeks later. Her symptoms had resolved at that time (Fig 3).
Fig 1.
Physical examination findings at presentation for patient 3.
Fig 2.
Physical examination findings at the 3-week follow-up visit for patient 3.
Fig 3.
Dampened waveform for the left third digit compared with the right for patient 3.
The clinical presentation of our three patients was not suggestive of thoracic outlet syndrome or vasculitis. The erythrocyte sedimentation rate, antinuclear antibody, antithrombin III, anticardiolipin antibodies, C-reactive protein, complete blood count, platelet count, and basic metabolic panel were normal in all three patients, negating any concerns for vasculitis. Also, none of our three patients had a history of trauma or signs of thoracic outlet syndrome.
Discussion
Paroxysmal finger hematoma (Achenbach syndrome) is an underdiagnosed vascular syndrome. Achenbach syndrome usually presents as recurring episodes of unexplained, sudden onset of painful swelling associated with deep ecchymosis of the volar aspect of the finger.1, 2 First described by Achenbach in 1955, it usually affects women aged 40 to 60 years. The exact etiology remains unclear. However, the hypothesis of a vasomotor disorder is widely favored. An association exists between Raynaud phenomenon and a history of chilblains.3 Hormonal factors can also play a role in the causation of this underreported condition.4 Most patients will seek medical attention owing to the alarming purple discoloration that occurs with this condition. Owing to the self-limiting nature of this disease, invasive studies are not necessary, although would be negative if preformed.5 Multiple capillary hematomas have been described with this condition. An association with acrocyanosis, gastrointestinal disorders, migraines, and gallbladder disease has been reported.2 Achenbach syndrome is a self-limiting condition in which the skin discoloration resolves within an average of 4 days.6
Achenbach syndrome can be confused with other conditions, including embolic digital artery occlusion, dermatitis artefacta, and Raynaud disease. Embolic digital artery occlusion will frequently involve multiple digits. A common cause is arterial thoracic outlet syndrome in a relatively healthy young patient. It is usually associated with post-stenotic dilation or aneurysm formation in the subclavian artery, commonly due to a cervical rib. The diagnostic workup of a patient presenting with purplish discoloration of a finger or fingers with or without a diminished radial pulse, should include a Doppler arterial study and duplex ultrasound scan of the subclavian artery to exclude a subclavian artery aneurysm in association with thoracic outlet syndrome, as demonstrated in Khaira et al.7
Dermatitis artefacta will usually present as a superficial erosion or a hyperpigmented macule on the face or hand in patients with chronic dermatitis such as acne or alopecia.8 These patients will frequently have an underlying depression or anxiety disorder, and the lesions will be self-inflicted by the patient. The appearance of a digit with intact skin is not consistent with the diagnosis of dermatitis artefacta.
Raynaud disease will typically present with episodes of the patient's fingers turning pale, followed by a purple discoloration. It will be accompanied by a cold sensation and numbness and will usually be bilateral. The fingers will then turn warm and red as the vasospasm subsides.
We have described three patients with a similar presentation of Achenbach syndrome. Two of our three patients did not have a history of smoking. Physiologic testing was performed for each patient at their presentation, with each showing dampened digital waveforms corresponding to the respective fingers. In the third patient, a cold immersion test was performed, with negative findings. Achenbach syndrome can be confused with Raynaud disease; however, implementation of a cold immersion test can help differentiate the two disorders. Each of our patients was treated using an antiplatelet agent, and all symptoms pertaining to finger discoloration subsequently resolved. Although not previously reported, a short course of an antiplatelet agent, such as clopidogrel or aspirin, could be beneficial for patients presenting with a purple or blue finger, possibly improving arterial flow and preventing thrombosis to the respective digits. Because the symptoms will resolve spontaneously, the benefit of antiplatelet agents could not be ascertained with certainty. Two of our patients were treated with clopidogrel, and one was treated with aspirin owing to lack of coverage of clopidogrel by insurance. The diagnosis requires a high clinical suspicion and a knowledge of other diagnoses with presentations similar to that of Achenbach syndrome. A possible diagnostic approach to a patient with a purple digit or digits is shown in Fig 4.9
Fig 4.
Diagnostic approach to a patient with purple digit or digits.
Conclusions
Achenbach syndrome is a rare condition that can be confused with other more concerning disorders.10 It is important to be familiar with this syndrome because most cases will be diagnosed clinically, and invasive studies are not necessary for diagnosis.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Eikenboom J.C., Cannegieter S.C., Briet E. Paroxysmal finger haematoma: a neglected syndrome. Thromb Hemost. 1991;66:266. [PubMed] [Google Scholar]
- 2.Kampfen S., Santa D.D., Fusetti S.C. A painful blue thumb: a case of Achenbach's syndrome. EJVES Extra. 2005;10:84–85. [Google Scholar]
- 3.Frerix M., Richter K., Muller-Ladner U., Hermann W. Achenbach's syndrome (paroxysmal finger hematoma) with capillaroscopic evidence of microhemorrhages. Arthritis Rheumatol. 2015;67:1073. doi: 10.1002/art.39003. [DOI] [PubMed] [Google Scholar]
- 4.Carpentier P.H., Maricq H.R., Biro C., Jiguet M., Seinturier C. Paroxysmal finger haematoma—a benign acrosyndrome occurring in middle-aged women. Vasa. 2016;45:57–62. doi: 10.1024/0301-1526/a000496. [DOI] [PubMed] [Google Scholar]
- 5.Robertson A., Liddington M.I., Kay S.P. Paroxysmal finger haematomas (Achenbach's syndrome) with angiographic abnormalities. J Hand Surg Br. 2002;27:391–393. doi: 10.1054/jhsb.2001.0726. [DOI] [PubMed] [Google Scholar]
- 6.Kordzadeh A., Caine P.L., Jones A., Rhodes K.M., Panayiotopolous Y.P. Is Achenbach’s syndrome a surgical emergency? A systematic review. Eur J Trauma Emerg Surg. 2016;42:439–443. doi: 10.1007/s00068-015-0610-0. [DOI] [PubMed] [Google Scholar]
- 7.Khaira H.S., Rittoo D., Vohra R.K., Smith S.R. The non-ischaemic blue finger. Ann R Coll Surg. 2001;83:154–157. [PMC free article] [PubMed] [Google Scholar]
- 8.Mohandas P., Bewley A., Taylor R. Dermatitis artefacta and artefactual skin disease: the need for a psychodermatology multidisciplinary team to treat a difficult condition. J Derm. 2013;169:600–606. doi: 10.1111/bjd.12416. [DOI] [PubMed] [Google Scholar]
- 9.Achenbach W. Das paroxysmale Handhematoma. Medizinische. 1958;52:2138–2140. [PubMed] [Google Scholar]
- 10.Deliss L.J., Wilson J.N. Acute blue fingers in women. J Joint Bone Surg. 1982;72:121. doi: 10.1302/0301-620X.64B4.7096422. [DOI] [PubMed] [Google Scholar]