Abstract
Well-child visits are protective for child health but underutilized in the United States. The Supplemental Nutrition Assistance Program (SNAP), the largest federal food assistance program in the United States, has been shown to reduce food insecurity and may also promote child health by supporting preventative health care utilization. We examined the relationship between SNAP participation and infant well-child visits using state administrative data from Missouri's Department of Social Services for the period January 2006 to July 2014 for more than 50,000 infant-mother dyads. We find that compared to always receiving SNAP, leaving SNAP or receiving SNAP unstably reduces the likelihood that an infant receives all recommended well-child visits in the first year. These patterns are more pronounced for infants living in urban areas, infants with Black or Hispanic mothers, and infants whose mothers are diagnosed with depression. We also find that stable SNAP participation primarily influences vaccination rates through well-child visits, which is when most infants receive their immunizations. Given the increased public health risk of foregone care, these results may inform policy makers as they consider making permanent policy waivers to reduce the administrative burden of the recertification process and increase the stability of SNAP participation.
Keywords: SNAP participation, Well-child visits, Immunizations, Infants, Maternal depression, Minorities
Highlights
-
•
Leaving SNAP reduces the likelihood an infant receives all recommended well-visits.
-
•
Receiving SNAP unstably reduces the likelihood of infants receiving five well-visits.
-
•
These patterns are larger for Hispanics, Blacks, and infants living in urban areas.
-
•
The “leaving SNAP” pattern is larger for infants with mothers with depression.
-
•
Stable SNAP participation mainly influences vaccinations through well-child visits.
1. Introduction
1.1. Background
Well-child visits are critical for the health of children because they provide preventative health assessments, access to childhood immunizations, and promote maternal education regarding infant health and development (Shumskiy, Richardson et al., 2018). Unfortunately, well-child visits are underutilized in the United States among children on Medicaid. Specifically, among minority children on Medicaid, those living in low-income households and those in Midwest and South regions are less likely to attend the recommend number of well visits (Medicaid, 2020; Ortega, McKenna et al., 2018). Foregone preventative care for children is associated with poorer health outcomes, including an increased risk of hospitalizations among children with chronic disease (Tom, Tseng et al., 2010). Additionally, foregone preventative care, such as routine immunizations, is likely to put children who are already at a higher risk for poor health at increased risk for contracting vaccine-preventable diseases.
Child health and healthcare utilization patterns have many social determinants, including food insecurity. There is a growing body of work that shows a strong linkage between food insecurity and child health (Gundersen & Ziliak, 2015; Thomas, Miller et al., 2019) and between food insecurity and health care use (Berkowitz, Seligman et al., 2017; Cook, Frank et al., 2004). Prior to the COVID-19 pandemic, food insecurity among households with children was declining (Coleman-Jensen September 2013). However, during the recent pandemic, levels of food insecurity in households with children have risen with roughly two in five households with children reporting food insecurity and one in five reporting that their children were experiencing food insecurity (Bauer, 2020; Schanzenbach & Pitts, 2020, pp. 1–15). Food insecurity can affect children's health directly if children do not have enough to eat or if their families choose less nutritious foods to save costs, and indirectly if food insecure parents are more likely to forgo preventative care in order to cope with the added burden of securing immediate food needs for the household.
The Supplemental Nutrition Assistance Program (SNAP), the largest of the federal food assistance programs, provides benefits that can be used to purchase food to be consumed at home for 19 million households in the United States (Food and Nutrition Service, United States Department of Agriculture, 2019). SNAP is the only federal food assistance program with the specifically goal of reducing household food insecurity. Although there are other food and nutrition assistance programs specifically targeted towards mothers and young children, such as WIC, they are intended to improve nutrition but not to address household food insecurity.
SNAP benefits are limited to those with gross household incomes below 130% of the federal poverty line, those that are categorically eligible through their participation in another social program, or the disabled and elderly with net household incomes below 100% of the federal poverty line. While enrollment is open to those eligible of any age, in 2018, prior to the recent economic downturn, the SNAP program served over 8 million families with children per month (Cronquist & Lauffer, 2019).
If SNAP participation weakens the linkage between food insecurity and poor health, then investments in SNAP may translate into lower long-term health care costs. However, empirical evidence regarding the effects of SNAP on child health are limited (Cook, Frank et al., 2004; Hoynes et al., 2015a, Hoynes et al., 2015b; Kreider, Pepper et al., 2012). One possible explanation is SNAP receipt is often interrupted by periods of non-receipt, an experience termed administrative churn, and these interruptions in monthly SNAP benefits may prevent children from receiving the full health benefits of SNAP participation (Heflin, Hodges et al., 2020; Mills, Vericker et al., 2014). We explore this possibility by examining whether SNAP participation dynamics are related to preventative health care utilization in the first year of life using administrative data from the state of Missouri. Prior research has used self-reports of both SNAP participation within the previous 12 months and health care utilization. In contrast, we use administrative records of SNAP participation and healthcare utilization. Missouri is a compelling state to study because rates of infant well-visits and vaccinations are near the fifty-state median (US Department of Health and Human Services, 2015).
1.2. The expected association of SNAP and well-child visits
It is generally thought that, by providing eligible households with the means to purchase food, SNAP promotes child health. However, empirical evidence is limited, both in terms of evidence that there is a health impact and in terms of identifying the mechanisms through which SNAP impacts health care use and by extension health. There is evidence that the introduction of SNAP was associated with positive improvements in child health outcomes (Hoynes et al., 2015a, Hoynes et al., 2015b), and several studies do find that SNAP benefits mediate the negative link between food insecurity and child health outcomes, though the effects are generally smaller than one might expect (Cook, Frank et al., 2004; Kreider, Pepper et al., 2012).
One explanation for the lack of robust evidence that SNAP participation is beneficial for child health is that SNAP benefits are not high enough to make households fully food secure over the entire month (Bronchetti, Christensen et al., 2019). Since SNAP benefits are often exhausted well before the next issuance date, household food consumption may be inconsistent as households deplete their resources (Castellari, Cotti et al., 2017; Castner & Henke, 2011; Dorfman, Gregory et al., 2019; Goldin, Homonoff et al., 2020; Shapiro, 2005; Todd, 2015).
Another consideration is that children in households that experience interruptions in monthly SNAP receipt may not get the full health benefits of SNAP. This consideration is rooted in a 2014 USDA report (Mills, Vericker et al., 2014), which estimated that 17 to 28 percent of the SNAP caseload in six states experienced a break in their SNAP benefits within a 12-month period due to the administrative burden associated with recertification requirements. Further work by Heflin et al. (2020) found that short-term interruptions in SNAP receipt of three months or less, referred to as administrative churn, are associated with changes in health care utilization patterns.
We call interruptions in SNAP participation unstable SNAP in this study and we identify other patterns of SNAP participation: always on SNAP, leaving SNAP, and never on SNAP. We hypothesize that receiving SNAP on a regular basis in the first year of a child's life (always on SNAP) might increase well-child visits by addressing household food insecurity. For example, prior work by Ma et al. (2008) found that food insecurity was associated with inadequate health care access in low-income children and, specifically, that food insecurity was associated with not receiving the recommended number of well-child visits. We hypothesize that unstable SNAP might have detrimental effects on health investments (Bahadur, Pai et al., 2018). For example, a temporary disruption in SNAP benefits may make it difficult for new mothers to make and keep well-child appointments due to increased stress, cognitive burden, and fewer resources for food, which forces a tradeoff between time spent on obtaining preventative care and time spent on securing food (Conger, Wallace et al., 2002).
Although prior work has distinguished between short-term disruptions in benefits (lasting less than four months) followed by returns to the SNAP program and long-term disruptions in benefits (lasting more than four months) (Heflin et al., 2020), other research suggests that the majority of those who are eligible who leave SNAP do it due to paperwork issues and very few do it voluntarily (Ribar & Edelhoch, 2008). Therefore, the leaving SNAP group could represent two subgroups: 1) those who are no longer eligible, and we expect this group to be better off; and 2) those who remain eligible but face difficulties completing the recertification process, and we expect this group to be worse off. If subgroup 2 dominates subgroup 1, then leaving SNAP and unstable SNAP may have a similar patterns of infants’ health care utilization.
Families never receiving SNAP in the year prior to birth, but receiving SNAP in earlier or later periods, may also reflect two different groups: those who remain eligible but have become disconnected from the system and are at greater risk of foregone preventative care or those that have experienced increases in household income that have made them ineligible for benefits. If mothers in the never SNAP group mainly fall into the latter category, i.e., better off economically, then we might expect a positive association with preventative health care utilization (well visits). However, this expectation is attenuated by concerns that working mothers with infants may face additional hurdles to keeping well-child visits.
The risk of forgone care due to SNAP participation dynamics may be augmented by racial-ethnic disparities, urbanicity, and maternal mental well-being. Racial-ethnic disparities in health and health care utilization have been widely studied (Chen, Martin et al., 2006; Williams & Sternthal, 2010) and findings suggest that Black children are less likely to receive recommended doses of vaccines against preventable diseases than white children and Hispanic children are less likely than white children to have had a well-child visit in the past year (Agency for Healthcare Research and Quality, 2018). Environment also plays a role in child health, with children living in urban areas at increased risk of contracting vaccine-preventable communicable diseases (Flanagan, Hallisey et al., 2018). On the other hand, children living in rural areas often live in poorer communities where health services are limited (Health Resources and Services Administration, 2015). We hypothesize that SNAP could work as a protective factor for minorities and participants in urban areas. Finally, we hypothesize that new mothers who are dealing with depression may struggle to keep well-child appointments when SNAP benefits are interrupted, due to the increased cognitive burden of food insufficiency (Conger et al., 2002). We take these factors into consideration by examining patterns of SNAP receipt and infant healthcare utilization separately by race and ethnicity, by urban and rural residence, and by maternal diagnosis of depression.
2. Methods
2.1. Data & sample
We use administrative data containing SNAP participation linked to Medicaid claims data from Missouri's Department of Social Services (Family Support Division) for the period January 2006 to July 2014. Our analytic sample is comprised of first-born children of low-income mothers aged 18 and older who participated in SNAP and Medicaid. We focus on first-born children because mothers may learn to navigate the complex enrollment and recertification processes of SNAP and Medicaid over time which could influence the stability of their program participation.
We have monthly SNAP participation data for 83,062 first-born children born during the study period; almost all of them (98 percent) were Medicaid insured at some point during the study period, making them adjunctively eligible for WIC. Because our measure of maternal depression and our outcomes of interest rely upon Medicaid claims data, we exclude children if the mother did not receive Medicaid both in the three months prior to and preceding birth, or if the child received Medicaid for less than 12 months after birth. Our final analytic sample includes 51,551 children (infant-mother dyads). The demographic characteristics of children and their mothers for the main analytical sample are shown in Appendix Table 1 and for the full sample and the excluded groups in Appendix Table 2. There are differences between the final analytic sample of first-borns and the initial full sample. The main driver seems to be the excluded group of teenage mothers. This is expected as we limit our sample to mothers who are over the age of 18 and teenage mothers are systematically different from other mothers.
2.2. Key measures
2.2.1. Well-child visits
We use International Classification of Disease, Ninth Revision, (ICD-9) diagnosis code V202 and date of service associated with the Medicaid claims to construct a binary indicator of whether a child receives at least five well-child visits in the year after birth. The American Academy of Pediatrics recommends that infants have six well-child visits in the first year: at one, two, four, six, nine, and twelve months (American Academy of Pediatrics, 2018). While our data contains month and year of birth, due to privacy considerations we are not able to observe exact date of birth. Because there is uncertainty around the exact timing of birth in our data, we define our outcome of interest as the completion of five or more well-visits within what we estimate is their first year of life. We observe at least one well-child visit for more than 97 percent of children in our sample. However, only about half had five or more visits within what we estimate is the first 12 months. See Appendix Table 3.
2.2.2. Immunizations
We use ICD-9 diagnosis codes to identify whether a child received immunizations that are typically administered at least once in the first 12 months. We focus on hepatitis B (HepB; diagnosis code V053 and procedure codes 90723, 90740, 90744 , 90747, 90748, and G0010); diptheria, tetanus, & acellular pertussis (DTaP; diagnosis code V061 and procedure codes 90698, 90700–90703, 90714, 90715, 90718–90721, and 90723); and haemophilus influenza type B (Hib; diagnosis code V0381 and procedure codes 90644–90648, 90698, 90721, and 90748). The Centers for Disease Control and Prevention Advisory Committee on Immunization Practices annually releases a schedule of recommended vaccinations for children from birth to 15 months. Our ideal measure for each immunization would be whether the child was up to date for that vaccine series at twelve months according to this schedule. However, because there is some uncertainty around the timing of the birth, we construct a less restrictive indicator of whether the child received at least one dose of the recommended vaccine in the first year.
The first dose of HepB is administered in the hospital at birth, and we observe at least one dose of HepB for 84 percent of children in our sample. The first doses of DTaP and Hib are typically administered at the two-month well-child visit, and we observe at least one dose of DTaP and one dose of Hib for 80 percent of children in our sample. See Appendix Table 3.
2.2.3. Months of SNAP participation
Using administrative data on SNAP participation, we identify the number of months that the child's household participated in SNAP in the year after birth. The distribution of total months of SNAP is bimodal, with observations concentrated around zero and 12 months. See Appendix Table 3. We use a continuous measure of months of SNAP participation in our main analysis and we check the sensitivity of our results to the distribution of the variable using a categorical measure (never SNAP, one to seven months, eight to ten months, and 11 to 12 months).
While we expect a positive association between number of months in SNAP and infant's health care utilization, we believe that it does not account for SNAP dynamics and therefore, its association with infants’ health care utilization may be weaker.
2.2.4. Patterns of SNAP participation
Our administrative data on SNAP participation details monthly SNAP receipt in the year after birth, which we categorize as follows:
Always SNAP: Mothers received SNAP in year prior to birth and received SNAP in 11 or 12 months in the year after birth.
Onto SNAP: Mothers did not receive SNAP in the year prior to birth and then enrolled in SNAP in the year after birth.
Off SNAP: Mothers continuously received SNAP for at least three months after the birth month followed by four or more months of no SNAP receipt in the year after birth. See Appendix Table 4.
Unstable SNAP: Mothers received SNAP intermittently during the first year of birth. The majority of mothers with unstable SNAP received SNAP in the 6 months prior to the child's birth. For many, unstable participation may be due to administrative churn, which occurs when households receive benefits for several months, do not receive benefits for up to four months, and then receive benefits again (Heflin, Hodges et al., 2020). Administrative churn frequently occurs around the recertification period (Mills, Vericker et al., 2014).
Never SNAP: Mothers did not receive SNAP in the year after birth, but received SNAP in the year prior to birth.
2.2.5. Covariates
To control for potential confounders of the relationship between SNAP dynamics and infant's health care utilization, we control for child, mother, household, and geographic characteristics. We control for the characteristics of the child, the mother, and the household at or around the time of birth, including child's sex, maternal race and ethnicity (Non-Hispanic White, Non-Hispanic Black, Hispanic, Multiple/Other/Unknown), maternal education (less than high school diploma, high school diploma or GED, more than high school diploma, unknown), geographic location (rural vs. urban area), maternal age, a proxy for maternal income prior to birth (income below 19% FPL, income above 185% FPL), maternal citizenship status, and presence of another adult in the household. We also construct a binary indicator for diagnosed maternal depression in the year after birth using ICD-9 codes of major depressive disorder (311), complications in anti or postpartum period due to mental disorders of the mother (648.40, 648.41, 648.42, 648.43, and 648.44), depressive episode (296.2, 296.20–296.25, 296.3, 396.30–296.35, 296.5, 296.51–296.56, 296.6), or other depression-related diagnosis (296.82, 300, 300.4, 301.12, 305.8, 305.81–305.83, 309, 309.1, 309.28). Diagnosed maternal depression may underestimate true rates of maternal depression among our sample (Horowitz & Cousins, 2006).
2.3. Approach
Our analytic approach is primarily descriptive with the aim of documenting dynamics in SNAP participation for the children in our sample and using multivariate regression analysis to examine how these dynamics are related to patterns in preventative care. We begin by estimating the average likelihood of having five or more well-child visits in the year after birth as a function of the total number of months of household SNAP receipt in the first year of life controlling for maternal and child sociodemographic characteristics (model 1). Then, to investigate if movements on and off SNAP influence health care utilization, we replace months of SNAP with binary indicators of SNAP participation pattern including always SNAP, never SNAP, onto SNAP, off SNAP, and unstable SNAP (model 2). We cannot include patterns of SNAP participation and monthly SNAP participation together in the same regression as both variables are highly correlated. We then replicate this analysis with immunizations as our outcomes of interest.
Finally, to better understand the role of SNAP in supporting access to preventative care services for groups of special concern, we stratify our models by geographic area, maternal race and ethnicity and mother's diagnosis of depression in the year after birth.
All models are estimated using probit regression analysis. To allow for comparisons across models, we present estimates of average marginal effects (AME). The AME can be interpreted as the change in the predicted probability of the outcome due to a discrete change in the value of the independent variable averaged across all observations in the sample.
3. Results
3.1. Well visits
3.1.1. Overall
We observe that an additional month of SNAP participation increases the likelihood of attending five or more well-child visits. See Table 1, Model 1. While the magnitude of the relationship is quite small on a monthly basis (0.2 percentage points), an increase in 10 months of SNAP participation results in a more sizable 2 percentage point increase. We also observe that relative to those always receiving SNAP, the likelihood of having five or more well-child visits is 1.4 percentage points lower for those never receiving SNAP and 4.8 percentage points lower for those transitioning off SNAP and those with unstable participation. See Table 1, Model 2. The similarities between the off SNAP and unstable SNAP groups suggest that SNAP participation dynamics may be more strongly related to patterns in preventative care than the total number of months of participation. For both models, consistent with prior research on completion of well-child visits, we observe that having a mother who identifies as Black Non-Hispanic and having a mother with a diagnosis of depression reduces the likelihood of having all well-child visits, while living in an urban area, mother's education level, and mother's age increase the likelihood (Minkovitz, Strobino et al., 2005; Agency for Healthcare Research and Quality, 2018; Flanagan, Hallisey et al., 2018).
Table 1.
Probit model, dependent variable: Attending five or more well-child visits in year after birth.
| Model 1 | Model 2 | |
|---|---|---|
| Months of SNAP Participation (Continuous) | 0.002** | |
| SNAP Participation Pattern | ||
| Onto SNAP | −0.012 | |
| Off of SNAP | −0.048*** | |
| Unstable SNAP | −0.048*** | |
| Never SNAP | −0.014* | |
| Child is Female | 0.009* | 0.008 |
| Mother's Race (Relative to White Non-Hispanic) | ||
| Black Non-Hispanic | −0.045*** | −0.043*** |
| Hispanic | −0.028 | −0.027 |
| Multiple/Other/Unknown/Missing | −0.011 | −0.010 |
| Mother is not a US citizen | 0.035 | 0.033 |
| Other Adult in Household (Relative to No) | 0.004 | 0.014** |
| Mother's Education | ||
| HS Diploma/GED | 0.049*** | 0.048*** |
| More Than HS | 0.064*** | 0.064*** |
| Unknown | 0.046*** | 0.045*** |
| Mother's Age (Relative to 18 to 20) | ||
| 20 to 24 | 0.023*** | 0.024*** |
| 25 to 29 | 0.050*** | 0.051*** |
| 30 and older | 0.020 | 0.020 |
| Mother's Income Prior to Birth (Relative to Low Income, 19%–185% FPL) | ||
| Very Low Income (<19% FPL) | −0.033*** | −0.034*** |
| Other | −0.062*** | −0.064*** |
| Child's Year of Birth (Relative to 2007) | ||
| 2008 | 0.008 | 0.007 |
| 2009 | 0.094*** | 0.093*** |
| 2010 | 0.143*** | 0.143*** |
| 2011 | 0.109*** | 0.110*** |
| 2012 | 0.109*** | 0.113*** |
| 2013 | 0.060*** | 0.068*** |
| Geography | ||
| Urban | 0.055*** | 0.056*** |
| Missing/Unknown | −0.000 | 0.003 |
| Maternal Depression ( any diagnosis in YAB) | −0.035*** | −0.035*** |
| Number of observations | 51,551 | 51,551 |
SOURCE Authors’ analysis of Missouri administrative data for SNAP and Medicaid, 2006–2014. NOTE Numbers reported are average marginal effects***p<0.001, **p<0.01, *p<0.05.
We tested the sensitivity of our findings to the distribution of months of SNAP receipt in the first year by using a categorical measure in place of our continuous measure. We also tested the robustness of our results by changing the number of well-child visits attended (i.e., four or more rather than five or more). Overall, our results remain consistent and robust to different specifications. See Appendix Tables 5 and 6
3.1.2. Subgroup analysis
Rural/Urban. Given the differential access to both SNAP offices and health care providers in urban and rural counties in Missouri, as well as the significant coefficients found in the main analysis, we re-estimated our main models stratifying the sample by urban and rural county of residence. For children living in urban areas, an extra month of SNAP receipt is associated with a 0.3 percentage point increase in the likelihood of receiving five or more well-child visits. However, for children living in rural areas, the coefficient on months of SNAP is not statistically significant. See Appendix Table 5.
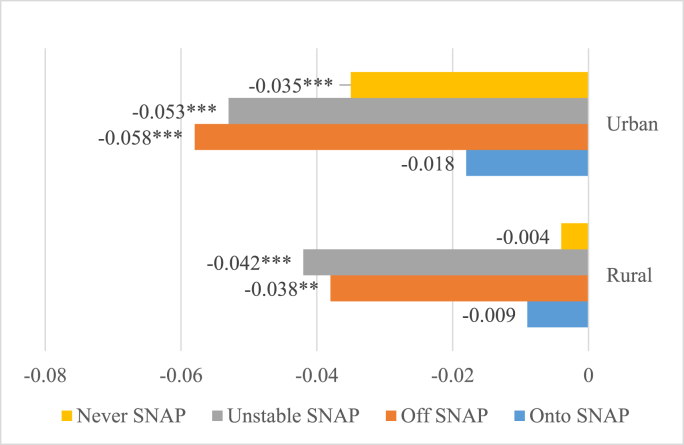
In terms of SNAP dynamics, children in rural and urban areas that transition off SNAP and that have unstable SNAP participation are less likely to have five or more well visits compared to children with stable SNAP participation. See Fig. 1. For children in rural areas, relative to those always receiving SNAP, the likelihood of having five or more well-child visits is 4 percentage points lower for those moving off SNAP (p<0.001) and for those receiving SNAP unstably (p<0.01). For children in urban areas, the differences are greater. Relative to those who always participate in SNAP, the likelihood is 6 percentage points lower for those moving off SNAP (p<0.001), 5 percentage points lower for those receiving SNAP unstably (p<0.001), and 3.5 percentage points lower for those never receiving SNAP (p<0.01). See appendix Fig. 1. When we tested for differences in the average marginal effects between groups, the difference between urban and rural areas estimates was not statistically significant for unstable SNAP or off SNAP, but it was for never SNAP (p<0.05).
Fig. 1.
Average Marginal Effects of Five or More Well Visits in the Year after Birth by SNAP participation pattern and geography (regression adjusted)
SOURCE Authors’ analysis of Missouri administrative data for SNAP and Medicaid, 2006–2014.
NOTE We used probit models (model 2) and report average marginal effects. Our model includes all covariates except for living in urban area. ***p<0.001, **p<0.01, *p<0.05 indicates statistically different from reference category (Always SNAP).
Race and ethnicity. Next, we examine if the marginal return associated with SNAP participation differs by maternal race and ethnicity. Using the continuous measure of SNAP, an extra month of SNAP receipt is associated with a 0.4 percentage point increase in having at least five well visits for children with Black non-Hispanic mothers but not statistically significant for children with White non-Hispanic and Hispanic mothers. See Appendix Table 5.
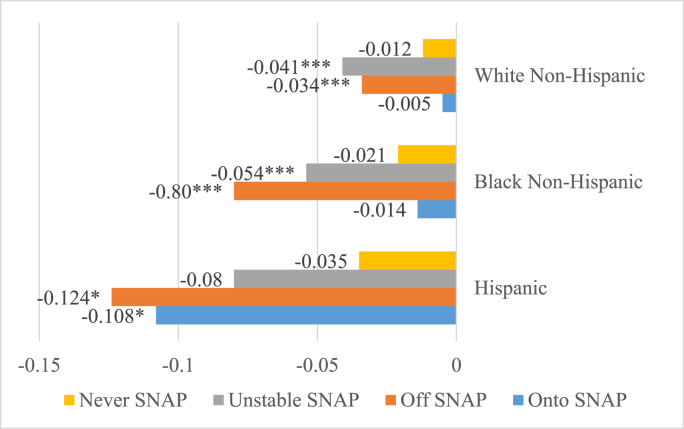
Then we measure SNAP dynamics and observe that the risk of not receiving at least five well visits is quite different across race and ethnicity. See Fig. 2. Among children with White non-Hispanic mothers, relative to those always participating in SNAP, the likelihood of attending five or more well-child visits is 3 percentage points lower for those transitioning off SNAP (p<.0001) and 4 percentage points lower for those receiving SNAP unstably (p<.0001). Among children with Black non-Hispanic mothers, relative to those always participating in SNAP, the likelihood of having five or more well-child visits is 8 percentage points lower for those transitioning off SNAP (p<0.001) and 5 percentage points lower for those with unstable participation (p<0.001). When we tested for differences in the average marginal effects between groups, the difference in the Off SNAP estimates between White non-Hispanics and Black non-Hispanic was statistically significant (p<0.05).
Fig. 2.
Average Marginal Effects of Five or More Well Visits in the Year after Birth by SNAP participation pattern and mother's race and ethnicity (regression adjusted)
SOURCE Authors’ analysis of Missouri administrative data for SNAP and Medicaid, 2006–2014. NOTE We used probit models (model 2) and report average marginal effects. Our model includes all covariates except for mother's race and ethnicity.
***p<0.001, **p<0.01, *p<0.05 indicates statistically different from reference category (Always SNAP).
For the children with Hispanic mothers, SNAP dynamics appear to have a different relationship to well-child visits. Like children whose mothers identified as White and Black, the likelihood of having five or more well-child visits is lower for those transitioning off SNAP, relative to always SNAP (12 percentage points; p<0.001). However, for this group, those transitioning onto SNAP had much lower likelihoods of having at least five visits (11 percentage points), while having unstable SNAP does not result in a statistically significant difference in well-visit attendance. When we tested for differences in the average marginal effects between groups, the difference in the Onto SNAP estimates between White Non-Hispanics with Hispanics was significant (p<0.05).
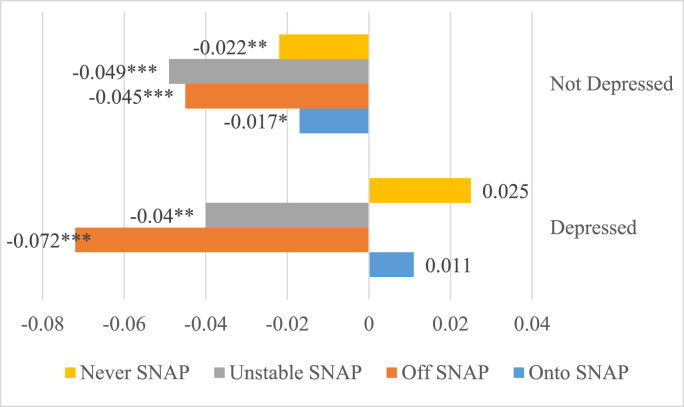
Mothers with diagnosed depression. We also examined the possibility that SNAP participation patterns may be differentially related to well-child visits for mothers diagnosed with maternal depression relative to those without. The estimate on the continuous measure of SNAP receipt for mothers without depression essentially mirrors that for the full sample while the estimates for mothers with depression is not statistically significant. See Appendix Table 5. We also observe that transitions off SNAP and unstable SNAP receipt are negatively associated with well-child visits for both groups. See Fig. 3. For children whose mothers who have been diagnosed with depression, 47% of those always participating in SNAP have at least five well-child visits compared to 40% of those transitioning off SNAP and 43% of those with unstable participation (See Appendix Fig. 1).
Fig. 3.
Average Marginal Effects of Five or More Well Visits in the Year after Birth by SNAP participation pattern and maternal depression (regression adjusted)
SOURCE Authors’ analysis of Missouri administrative data for SNAP and Medicaid, 2006–2014. NOTE We used probit models (model 2) and report average marginal effects. Our model includes all covariates except for mothers diagnosed with depression.
***p<0.001, **p<0.01, *p<0.05 indicates statistically different from reference category (Always SNAP).
3.2. Immunizations
Additionally, we explored the relationship between SNAP participation and the likelihood of receiving an immunization dose in the first year (Table 2). We find that the continuous measure of SNAP participation is a strong and consistent predictor of receiving specific vaccinations, whereas there are fewer statistically significant differences by SNAP participation pattern. Relative to those always receiving SNAP, those never receiving SNAP are less likely to have HepB, DTaP, and Hib vaccinations in the first year; those who move off SNAP are less likely to have a vaccination for DTaP. Importantly, whether our key predictor is months of SNAP or SNAP participation pattern, it appears that the main way in which SNAP is associated with vaccinations is by increasing the likelihood of well-child visits and these findings are consistent when the sample is stratified by geography, and by race and ethnicity (See Appendix Table 7). When we control for well-child visits in the model directly, the coefficients on months of SNAP and SNAP participation pattern attenuate and most are no longer statically significant.
Table 2.
Probit Models, Dependent Variable: Immunizations (any dose) in the Year after Birth.
| Immunizations (any dose = 1) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hep B |
DTaP |
HiB |
||||||||||
| Model 1 | Model 1 + Well visits | Model 2 | Model 2 +Well visits) | Model 1 | Model 1 + Well visits | Model 2 | Model 2 +Well visits) | Model 1 | Model 1 + Well visits | Model 2 | Model 2 +Well visits) | |
| Total Months of SNAP Participation | 0.002*** | 0.001* | 0.002*** | 0.001 | 0.001*** | 0.000 | ||||||
| SNAP Participation Pattern | ||||||||||||
| Onto SNAP | −0.004 | −0.000 | −0.008 | −0.004 | −0.008 | −0.004 | ||||||
| Off of SNAP | −0.005 | 0.004 | −0.013* | −0.003 | −0.009 | 0.002 | ||||||
| Unstable SNAP | −0.002 | 0.006 | 0.000 | 0.009 | −0.001 | 0.008 | ||||||
| Never SNAP | −0.022*** | −0.012* | −0.020*** | −0.009 | −0.016** | −0.005 | ||||||
| Total Number of Well-visits, YAB | ||||||||||||
| 1 | 0.352*** | 0.352*** | 0.340*** | 0.340*** | 0.336*** | 0.336*** | ||||||
| 2 | 0.491*** | 0.491*** | 0.492*** | 0.492*** | 0.494*** | 0.494*** | ||||||
| 3 | 0.516*** | 0.516*** | 0.512*** | 0.512*** | 0.519*** | 0.519*** | ||||||
| 4 | 0.525*** | 0.526*** | 0.518*** | 0.518*** | 0.524*** | 0.524*** | ||||||
| 5 or more | 0.557*** | 0.558*** | 0.569*** | 0.569*** | 0.579*** | 0.579*** | ||||||
| Observations | 51,551 | 51,551 | 51,551 | 51,551 | 51,551 | 51,551 | 51,551 | 51,551 | 51,551 | 51,551 | 51,551 | 51,551 |
SOURCE Authors’ analysis of Missouri administrative data for SNAP and Medicaid, 2006–2014.
NOTE Numbers reported are average marginal effects. All regressions control for child's sex, mother's race, other adult in household, mother's citizenship status, mother's education, mother's age, mother's income, living in urban area, maternal depression, and child's year of birth.
***p<0.001, **p<0.01, *p<0.05.
4. Discussion
Using SNAP and Medicaid linked administrative data from Missouri, we find that an additional month of SNAP participation is positively associated with the likelihood that an infant received five or more well-child visits in the first 12 months of life. These results are consistent with a recent study that used self-reported SNAP participation within the last 12 months and found that increased in SNAP benefits provided by the American Recovery and Reinvestment Act was associated with a decrease in 1.52 percentage points in delayed care and a decrease in 4.4 percentage point in the number of unmet medical needs (Morrissey & Miller, 2020).
However, when we control for dynamics of SNAP participation, we find that leaving SNAP or receiving SNAP unstably, which may be a consequence of administrative churn in some cases, reduces the likelihood that the infant receives all five recommended well-child visits. While some households who exit SNAP are presumably economically better off and may have more resources to support their completion of their well-child visits, we find that the negative relationship dominates for this group. It may be that households that leave SNAP become ineligible but have more demanding work obligations that limit flexibility to keep appointments. It may also be that or households that leave SNAP remain eligible but find it difficult to comply with the administrative burden associated with recertification. When these households lose SNAP, they may be forced to deal with immediate food needs that take priority over well-child visits. Importantly, the negative association between SNAP dynamics and well-child visits are larger for children living in urban areas (in comparison to children living in rural areas), and black and Hispanic children (in comparison to white children), suggesting several groups for targeted intervention.
In addition, we explored the potential role that maternal depression may play in this relationship. Maternal depression is consistently related to a lower likelihood of an infant receiving all five well-child visits in our base models and this finding is replicated in both urban and rural counties. We find that maternal depression is associated with a reduction in the likelihood of receiving all five well-child visits for non-Hispanic White women but not for non-Hispanic Black or Hispanic women, groups in which maternal depression may be under-diagnosed (Burwell, 2011; Kozhimannil, Trinacty et al., 2011; Liu & Tronick, 2013; Wei, Greaver et al., 2008). When we stratify the sample by depression, we find that there is no relationship with our continuous measure of SNAP for the sample with diagnosed maternal depression but that the coefficient for off SNAP is larger than that found in the sample without diagnosed maternal depression.
Finally, we explored the relationship between SNAP receipt and the likelihood of receiving vaccinations, another important marker of preventative infant care. We find that stable SNAP participation primarily influences vaccination behavior through the likelihood of attending well-child visits, which is when most infants receive their immunizations. This is supported by literature that suggests that well-child visits improve infants’ likelihood of immunization (Gill, Saldarriaga et al., 2002), and literature that describes the negative associations of food insecurity with well-child visits (Palakshappa, Khan et al., 2016). Our results demonstrate that once well-child visits are controlled for, food hardships might not directly affect immunizations.
We acknowledge several limitations of this study. First, our estimates likely contain omitted variable bias, as we do not have access to administrative records of participation in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). WIC participation is relevant for well-child visits since this program focuses on health and nutrition in early childhood including vaccination compliance and our sample of Medicaid covered children are adjunctively eligible for WIC. However, WIC food packages provide specific food items that are tailored to meet the nutritional needs of participants. Unlike SNAP benefits, WIC is not designed to fully address household food insecurity but to address specific nutritional inadequacies. However according to USDA (USDA, 2017) and our own analyses of the Early Childhood Longitudinal Study-Birth cohort data (Tourangeau, Nord, et al., 2006), more than 90% of infants who participate in SNAP are also enrolled in WIC. Given that our study sample is composed of mother-child dyads who were observed in SNAP and therefore were likely jointly enrolled in WIC, we expect that accounting for WIC participation directly would not substantially change our results. In additional sensitivity analyses, we created a variable that randomly assigned 95% of mother-child dyads in the sample to one group (the hypothetical WIC participant group). Including this variable in our models in Table 1 did not change the results.
Second, because our analyses are descriptive, we are not able to explore the mechanisms through which SNAP may affect child-well visits. However, we hypothesize that SNAP benefits, especially when received without interruption, could reduce maternal food insecurity which in turn could reduce her stress to get food and allow her to focus on long-term investments in infant health. This in turn could influence parental practices such as taking children to their well-visits as prior research has shown (McLennan & Kotelchuck, 2000, Perry, 2008).
Third, our analytical sample is not representative of all first-time mothers in Missouri, which may limit generalizability. We expected some selection given our sample exclusion criteria. Our findings reflect the relationship for a specific population first-time mothers receiving Medicaid at the time of their child's birth who are over the age of 18 and who ever received SNAP during our study period.
Additionally, because our analyses are descriptive, we cannot rule out the possibility that mothers who are able to navigate the recertification process and remain connected to the SNAP program are also better able to make and keep preventative care appointments for their children. However, our findings point to an important direction for future research on how to best support mothers who struggle with both and can help with targeting policy interventions designed to simplify the SNAP recertification processes and policy interventions designed to help mothers and their infants access preventative care. Along these lines, we note that the US Department of Agriculture provided State agencies with the option to modify certification and recertification periods during the beginning of the Covid-19 emergency. How the temporary policy waivers changed the stability of SNAP participation, especially for mothers with young children, is an important area for future research.
5. Conclusion
To our knowledge, our study is the first study that examines the relationship between SNAP dynamics and infant preventive care. The recent spike in food insecurity along with evidence of a decline in preventative health care during the COVID-19 pandemic is a major public health concern. Foregone primary care is associated with poorer health outcomes (Tom et al., 2010). Furthermore, well-visits are the primary way in which children receive vaccinations, so foregone routine care is likely to put children who are already at a higher risk for poor health and their communities at increased risk for outbreaks of vaccine-preventable diseases (CDC, 2020). A recent study found a 25 percent decline in up-to-date status for recommended vaccines among infants in Michigan (5 months) (Bramer, Kimmins, et al., 2020). Given the long-term health benefits associated with well-child visits and immunizations, the public health benefits associated with stable SNAP participation, particularly among households with young children, deserves continued attention.
Disclaimer
The findings and conclusions in this publication are those of the authors and should not be construed to represent any official USDA or U.S. government determination or policy or views of the sponsoring institutions.
Funding
Funding for this project was provided by Tufts University/University of Connecticut RIDGE program (Sub-award # AG9002-Arteaga) with funding from ERS-USDA (PTE federal award # 59-5000-6-0070).
CRediT authorship contribution statement
Irma Arteaga: Conceptualization, Methodology, Supervision, Writing – original draft, Project administration, Funding acquisition. Leslie Hodges: Software, Validation, Data curation, Formal analysis, Writing – review & editing. Colleen Heflin: Conceptualization, Writing – review & editing.
Declaration of competing interest
Each of the authors has no financial interest or conflict of interest to report. During the duration of the project, Leslie Hodges was a postdoctoral associate at the University of Wisconsin-Madison.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2021.100910.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Agency for Healthcare Research and Quality Maternal and child health care: Effectiveness measures. 2018. https://www.ahrq.gov/research/findings/nhqrdr/chartbooks/healthyliving/mcheff-measures.html from.
- American Academy of Pediatrics H.C. 2018. AAP Schedule of Well-child Care Visits.https://www.healthychildren.org/English/family-life/health-management/Pages/Well-Child-Care-A-Check-Up-for-Success.aspx from. [Google Scholar]
- Bahadur K., Pai S., Thoby E., Petrova A. Frequency of food insecurity and associated health outcomes in pediatric patients at a federally qualified health center. Journal of Community Health. 2018;43(5):896–900. doi: 10.1007/s10900-018-0499-8. [DOI] [PubMed] [Google Scholar]
- Bauer L. About 14 million of children in the US are not getting enough to eat. Up Front blog. 2020 https://www.brookings.edu/blog/up-front/2020/07/09/about-14-million-children-in-the-us-are-not-getting-enough-to-eat/ from. [Google Scholar]
- Berkowitz S.A., Seligman H.K., Basu S. 2017. Impact of Food Insecurity and SNAP Participation on Healthcare Utilization and Expenditures. [Google Scholar]
- Bramer C.A., Kimmins L.M., Swanson R., Kuo J., Vranesich P., Jacques‐Carroll L., Shen A.K. Decline in child vaccination coverage during the COVID‐19 pandemic—Michigan Care Improvement Registry, May 2016‐May 2020. American Journal of Transplantation. 2020;20(7):1930. doi: 10.1111/ajt.16112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronchetti E.T., Christensen G., Hoynes H.W. Local food prices, SNAP purchasing power, and child health. Journal of Health Economics. 2019;68:102231. doi: 10.1016/j.jhealeco.2019.102231. [DOI] [PubMed] [Google Scholar]
- Burwell T. 2011. Postpartum depression and race: What we all should know.https://psychologybenefits.org/2016/06/21/postpartum-depression-in-women-of-color/ Retrieved from. [Google Scholar]
- Castellari E., Cotti C., Gordanier J., Ozturk O. Does the timing of food stamp distribution matter? A panel‐data analysis of monthly purchasing patterns of US households. Health Economics. 2017;26(11):1380–1393. doi: 10.1002/hec.3428. [DOI] [PubMed] [Google Scholar]
- Castner L., Henke J. Mathematica Policy Research; 2011. Benefit redemption patterns in the supplemental nutrition assistance program. [Google Scholar]
- Chen E., Martin A.D., Matthews K.A. Understanding health disparities: The role of race and socioeconomic status in children’s health. American Journal of Public Health. 2006;96(4):702–708. doi: 10.2105/AJPH.2004.048124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman-Jensen A., Nord M., Singh A. September 2013. Household food security in the United States in 2012 economic research report. U. S. D. o. A. Economic research service. ERR-155. [Google Scholar]
- Conger R.D., Wallace L.E., Sun Y., Simons R.L., McLoyd V.C., Brody G.H. J.D.p. Economic pressure in African American families: A replication and extension of the family stress model. 2002;38(2):179. [PubMed] [Google Scholar]
- Cook J.T., Frank D.A., Berkowitz C., Black M.M., Casey P.H., Cutts D.B., Meyers A.F., Zaldivar N., Skalicky A., Levenson S. Food insecurity is associated with adverse health outcomes among human infants and toddlers. Journal of Nutrition. 2004;134(6):1432–1438. doi: 10.1093/jn/134.6.##. [DOI] [PubMed] [Google Scholar]
- Cronquist K., Lauffer S. Report prepared for U.S. Department of Agriculture, Food and Nutrition Service, Office of Policy Support, by Mathematica Policy Ressearch; 2019. Characteristics of supplemental nutrition assistance program households: Fiscal Year 2017. [Google Scholar]
- Dorfman J.H., Gregory C., Liu Z., Huo R. Re-examining the SNAP benefit cycle allowing for heterogeneity. Applied Economic Perspectives and Policy. 2019;41(3):404–433. [Google Scholar]
- Flanagan B.E., Hallisey E.J., Adams E., Lavery A. Measuring community vulnerability to natural and anthropogenic hazards: The centers for disease control and prevention’s social vulnerability index. Journal of Environmental Health. 2018;80(10):34. [PMC free article] [PubMed] [Google Scholar]
- Food and Nutrition Service, United States Department of Agriculture Persons, households, benefits, and average monthly benefit per person & household, FY16- FY20. 2019. https://www.fns.usda.gov/pd/supplemental-nutrition-assistance-program-snap from.
- Gill J.M., Saldarriaga A., Mainous A., Unger D. Does continuity between prenatal and well-child care improve childhood immunizations? FAMILY MEDICINE-KANSAS CITY- 2002;34(4):274–280. [PubMed] [Google Scholar]
- Goldin J., Homonoff T., Meckel K. National Bureau of Economic Research; 2020. Issuance and incidence: Snap benefit cycles and grocery prices. [Google Scholar]
- Gundersen C., Ziliak J.P. Food insecurity and health outcomes. Health Affairs. 2015;34(11):1830–1839. doi: 10.1377/hlthaff.2015.0645. [DOI] [PubMed] [Google Scholar]
- Health Resources and Services Administration . 2015. The health and well-being of children in rural areas: A portrait of the nation, 2011–2012.https://mchb.hrsa.gov from. [Google Scholar]
- Heflin C., Hodges L., Ojinnaka C. Administrative churn in SNAP and health care utilization patterns. Medical Care. 2020;58(1):33–37. doi: 10.1097/MLR.0000000000001235. [DOI] [PubMed] [Google Scholar]
- Horowitz J.A., Cousins A. Postpartum depression treatment rates for at-risk women. Nursing Research. 2006;55(2):S23–S27. doi: 10.1097/00006199-200603001-00005. [DOI] [PubMed] [Google Scholar]
- Hoynes H., McGranahan L., Schanzenbach D. In: Snap and food consumption. SNAP matters: How food stamps affect health and well being. Bartfeld J., Gundersen C., Smeeding T., Ziliak J., editors. Stanford University Press; 2015. [Google Scholar]
- Hoynes H.W., McGranahan L., Schanzenbach D.W. 2015. "SNAP and food consumption." SNAP matters: How food stamps affect health and well being; pp. 107–133. [Google Scholar]
- Kozhimannil K.B., Trinacty C.M., Busch A.B., Huskamp H.A., Adams A.S. Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatric Services. 2011;62(6):619–625. doi: 10.1176/appi.ps.62.6.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreider B., Pepper J.V., Gundersen C., Jolliffe D. Identifying the effects of SNAP (Food Stamps) on child health outcomes when participation is endogenous and misreported. Journal of the American Statistical Association. 2012;107(499):958–975. [Google Scholar]
- Liu C.H., Tronick E. Rates and predictors of postpartum depression by race and ethnicity: Results from the 2004 to 2007 New York city PRAMS survey (pregnancy risk assessment monitoring system) Maternal and Child Health Journal. 2013;17(9):1599–1610. doi: 10.1007/s10995-012-1171-z. [DOI] [PubMed] [Google Scholar]
- Ma C.T., Gee L., Kushel M.B. Associations between housing instability and food insecurity with health care access in low-income children. Ambulatory Pediatrics. 2008;8(1):50–57. doi: 10.1016/j.ambp.2007.08.004. [DOI] [PubMed] [Google Scholar]
- McLennan J.D., Kotelchuck M. Parental prevention practices for young children in the context of maternal depression. Pediatrics. 2000;105(5):1090–1095. doi: 10.1542/peds.105.5.1090. [DOI] [PubMed] [Google Scholar]
- Medicaid . 2020. Well-visits in the First 15 Months of Life. [Google Scholar]
- Mills G., Vericker T., Koball H., Lippold K., Wheaton L., Elkin S. United States Department of Agriculture, Food and NutriCtion Service, Office …; 2014. Understanding the rates, causes, and costs of churning in the supplemental nutrition assistance program (snap) [Google Scholar]
- Minkovitz C.S., Strobino D., Scharfstein D., Hou W., Miller T., Mistry K.B., Swartz K. Maternal depressive symptoms and children's receipt of health care in the first 3 years of life. Pediatrics. 2005;115(2):306–314. doi: 10.1542/peds.2004-0341. [DOI] [PubMed] [Google Scholar]
- Morrissey T.W., Miller D.P. Supplemental nutrition assistance program participation improves children's health care use: An analysis of the American Recovery and reinvestment Act's natural experiment. Academic pediatrics. 2020;20(6):863–870. doi: 10.1016/j.acap.2019.11.009. [DOI] [PubMed] [Google Scholar]
- Ortega A.N., McKenna R.M., Chen J., Alcalá H.E., Langellier B.A., Roby D.H. Insurance coverage and well-child visits improved for youth under the Affordable Care Act, but Latino youth still lag behind. Academic Pediatrics. 2018;18(1):35–42. doi: 10.1016/j.acap.2017.07.006. [DOI] [PubMed] [Google Scholar]
- Palakshappa D., Khan S., Feudtner C., Fiks A.G. Acute health care utilization among food-insecure children in primary care practices. Journal of Health Care for the Poor and Underserved. 2016;27(3):1143–1158. doi: 10.1353/hpu.2016.0127. [DOI] [PubMed] [Google Scholar]
- Perry C.D. Does treating maternal depression improve child health management? The case of pediatric asthma. Journal of Health Economics. 2008;27(1):157–173. doi: 10.1016/j.jhealeco.2007.03.005. [DOI] [PubMed] [Google Scholar]
- Ribar D.C., Edelhoch M. Income volatility and food assistance in the United States. WE Upjohn Institute for Employment Research; Kalamazoo, MI: 2008. Earnings volatility and the reasons for leaving the food stamp program; pp. 63–102. [Google Scholar]
- Schanzenbach D., Pitts A. Institute for Policy Research; 2020. Food insecurity in the census household pulse survey data tables; pp. 1–15. [Google Scholar]
- Shapiro J.M. Is there a daily discount rate? Evidence from the food stamp nutrition cycle. Journal of Public Economics. 2005;89(2–3):303–325. [Google Scholar]
- Shumskiy I., Richardson T., Brar S., Hall M., Cox J., Crofton C., Peltz A., Samuels-Kalow M., Alpern E.R., Neuman M.I. Well-child visits of Medicaid-insured children with medical complexity. The Journal of Pediatrics. 2018;199:223–230. doi: 10.1016/j.jpeds.2018.04.003. e222. [DOI] [PubMed] [Google Scholar]
- Thomas M.M., Miller D.P., Morrissey T.W. Food insecurity and child health. Pediatrics. 2019;144(4) doi: 10.1542/peds.2019-0397. [DOI] [PubMed] [Google Scholar]
- Todd J.E. Revisiting the Supplemental Nutrition Assistance Program cycle of food intake: Investigating heterogeneity, diet quality, and a large boost in benefit amounts. Applied Economic Perspectives and Policy. 2015;37(3):437–458. [Google Scholar]
- Tom J.O., Tseng C.-W., Davis J., Solomon C., Zhou C., Mangione-Smith R. Missed well-child care visits, low continuity of care, and risk of ambulatory care–sensitive hospitalizations in young children. Archives of Pediatrics & Adolescent Medicine. 2010;164(11):1052–1058. doi: 10.1001/archpediatrics.2010.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tourangeau K., Nord C., Lê T., Pollack J.M., Atkins-Burnett S. Early Childhood Longitudinal Study, Kindergarten Class of 1998–99 (ECLS-K), Combined User’s Manual for the ECLS-K Fifth-Grade Data Files and Electronic Codebooks (NCES 2006–032) U.S. Department of Education. Washington, DC: National Center for Education Statistics; 2006. [Google Scholar]
- US Department of Health and Human Services Performance rates on frequently reported health care quality measures in the CMS Medicaid/CHIP Child and Adult Core Sets, for FFY 2014 reporting. 2015. https://www.medicaid.gov/medicaid/quality-of-care/performance-measurement/adult-and-child-health-care-quality-measures/childrens-health-care-quality-measures/index.html from.
- USDA . Food and Nutrition Service, Office of Policy Support. National- and State-Level Estimates of Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) Eligibles and Program Reach in 2014, and Updated Estimates for 2005–2013, by Paul Johnson, David Betson, Lorraine Blatt, and Linda Giannarelli. Project Officer: Grant Lovellette. Alexandria, VA: September 2017. USDA; 2017. [Google Scholar]
- Wei G., Greaver L.B., Marson S.M., Herndon C.H., Rogers J. Postpartum depression: Racial differences and ethnic disparities in a tri-racial and bi-ethnic population. Maternal and Child Health Journal. 2008;12(6):699–707. doi: 10.1007/s10995-007-0287-z. [DOI] [PubMed] [Google Scholar]
- Williams D.R., Sternthal M. Understanding racial-ethnic disparities in health: Sociological contributions. Journal of Health and Social Behavior. 2010;51(1_suppl):S15–S27. doi: 10.1177/0022146510383838. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.