Abstract
Background
The burden of time is often the primary reason why patients discontinue their treatment. Telemedicine may help patients adhere to treatment by offering convenience.
Objective
This study examined the efficacy and safety of telemedicine for the management of hypertension in Japan.
Methods
Patients with uncomplicated hypertension were recruited through web advertising between November 2015 and February 2017. They were then screened, stratified by office systolic blood pressure (SBP), and randomized into two groups: usual care (UC) and telemedicine. The telemedicine group used a 3G network–attached home blood pressure (BP) monitoring device, consulted hypertension specialists from an academic hospital through web-based video visits, and received prescription medication by mail for 1 year. The UC group used the same BP monitoring device but was managed using self-recorded BP readings, which included their diary entries and office BP taken in a community practice setting.
Results
Initial screening was completed by 99 patients, 54% of whom had untreated hypertension. Baseline BP was similar between the groups, but the weekly average SBP at the end of the 1-year study period was significantly lower in the telemedicine group (125, SD 9 mmHg vs 131, SD 12 mmHg, respectively; P=.02). SBP in the telemedicine group was 3.4 mmHg lower in the morning and 5.8 mmHg lower in the evening. The rate of SBP control (135 mmHg) was better in the telemedicine group (85.3% vs 70.0%; P=.01), and significant adverse events were not observed.
Conclusions
We present evidence suggesting that antihypertensive therapy via home BP telemonitoring and web-based video visits achieve better BP control than conventional care and is a safe treatment alternative that warrants further investigation.
Trial Registration
UMIN-CTR UMIN000025372; https://tinyurl.com/47ejkn4b
Keywords: blood pressure management, digital health, web-based medicine, prospective study, telemonitoring, blood pressure, monitoring, telemedicine, telehealth, efficacy, hypertension, video conference, safety, Japan
Introduction
Antihypertensive therapy has advanced over the years to enable lowering of blood pressure (BP) in most patients with hypertension if they receive proper treatment. Nevertheless, in Japan, only 12 million of 43 million individuals with hypertension receive treatment and have their BP controlled [1]. This phenomenon, termed the “hypertension paradox,” must be resolved to improve public health [2]. Among the reasons why individuals do not take action to control their hypertension, the burden of time takes precedence for discontinuation or noninitiation of antihypertensive treatment. Telemedicine using internet-based communication may lower the hurdle for starting and adhering to hypertension treatment, eventually leading to the prevention of cardiovascular disease. This approach may also result in higher satisfaction among patients by allowing better use of their time rather than having them spend much of it waiting at clinics or hospitals. Technical difficulty and anxiety associated with telemedicine hence need to be managed sufficiently.
Achieving target BP levels in the treatment of hypertension requires patients’ adherence to and persistence in taking their medication. Self-measurement of home BP (SMBP) helps improve adherence to treatment and aids in BP control [3,4]. Adjusting antihypertensive medication based on self-measured home BP (HBP) for long periods is feasible, and HBP self-monitoring with self-titration of antihypertensive medication in accordance with an individualized predetermined protocol has been reported to result in better BP control than that with usual care (UC) [5].
In Japan, telemedicine without face-to-face communication has been permitted since early 2015. We developed an integrated web-based telemedicine platform to manage appointments, medical care, and payment without patients visiting a clinic. However, clinical evidence concerning the efficacy and safety of telemedicine remains scarce. In this study, we attempted to demonstrate the advantages of telemedicine over traditional care in the management of hypertension. The Paradigm of Antihypertensive Therapy along with Telemedicine Randomized (POATRAND) trial was designed and performed as a prospective, randomized, open-label, 2-arm study of patients with uncontrolled, uncomplicated hypertension to test the effectiveness and safety of BP telemonitoring as well as hypertension telemedicine.
Methods
Study Design and Participant Recruitment
The POATRAND trial was a multicenter, open-label randomized controlled trial performed at Tokyo Women’s Medical University Clinic and private clinics in Japan. Potentially eligible participants with hypertension were recruited through web advertising. The inclusion criteria were age over 20 years, elevated systolic BP (SBP) or diastolic BP (DBP), ability to visit the Tokyo Women’s Medical University Clinic for the initial screening, willingness to receive hypertension care through telemedicine, and ability to self-measure HBP. The exclusion criteria were inability to use a smartphone, pregnancy, presence of major cardiovascular events and diabetes mellitus, an estimated glomerular filtration rate lower than 30 mL/min/1.73 m2 determined using the modified Modification of Diet in Renal Disease formula for Japanese patients [6], and presence of secondary hypertension excluding primary aldosteronism without surgical indication. The study protocol was approved by the Tokyo Women’s Medical University Research Ethics Committee (approval 160603) and registered in the UMIN Clinical Trials Registry under accession number UMIN000025372. All patients provided their written informed consent to participate in the study.
Randomization
Potentially eligible patients were invited to Tokyo Women’s Medical University Clinic between November 2015 and February 2017 for screening. After eligibility screening and provision of informed consent, each patient’s office BP was measured with the patient sitting quietly alone in a room. Before measurement, an experienced staff member instructed the patient on the procedure, placed a cuff with an appropriately sized bladder on the patient’s upper left arm, and left the room. BP was measured 3 times at 3-min intervals. Office BP was measured using the same validated BP monitor as the one used for home BP measurements (HEM-7252G-HP; Omron) [7], and the values were not concealed from the participants. At the second baseline visit, screening results were communicated to the participants, and the participants were stratified by the average of the second and third office SBP readings at the first visit and randomly assigned at a 1:1 ratio into the UC or telemedicine group, using an Excel-based random sampling number system.
Procedures
HBP was measured using a 3G network–equipped automatic sphygmomanometer (HEM-7252G-HP; Omron) [7]. The device was based on the cuff–oscillometric principle and validated to meet the criteria of the Association for the Advancement of Medical Instrumentation. The device recorded and transmitted SBP and DBP values, heart rate, and the date and time of each measurement. Registered patients were instructed on how to use the device and asked to take their HBP reading in a sitting position twice every morning within 1 h of waking before taking a meal or medication and after more than 2 minutes of rest. Participants were also asked to measure their HBP twice every evening before going to bed. The telemedicine group used this device, consulted a physician through web-based visits in consideration of their transmitted BP values, and received prescription medication by mail for 1 year. The UC group used the same BP monitoring device but was managed with actual office visits using self-recorded BP readings, such as their diary entries. After randomization, baseline HBP was measured in both groups without changes in treatment. The standard visit-to-visit interval was set at 6 weeks for the telemedicine group and was unspecified for the UC group, leaving it to the physician’s discretion.
Primary and Secondary Outcomes
The primary outcome was the average home SBP during the last week of the 12-month study period. Secondary outcomes included other measures of office BP and HBP including morning and evening SBP, DBP, and BP control rates, adverse events (eg, side effects and cardiovascular events), medication prescription (ie, number and defined daily dose), body weight, and laboratory measures.
Statistical Analysis
We initially estimated that 260 patients were required for screening per group to detect a 4-mmHg difference in home SBP values between the 2 groups, with a 2-sided P value of .05 and 80% power. However, the study was prematurely terminated at the end of March 2018 because the health insurance policy in Japan changed, requiring a face-to-face visit at least every 3 months. SPSS (version 21, IBM Corp) was used for statistical analyses. All P values were 2-sided, and P≤.05 was considered statistically significant. Data are presented as mean (SD) values unless otherwise indicated.
Results
Baseline Participant Characteristics
In total, 159 patients were screened for the study (Figure 1). Their baseline characteristics are shown in Table 1. The groups did not show significant differences in age, female-to-male ratio, BMI, home SBP, home DBP, pulse rate, plasma aldosterone concentration, plasma renin activity, estimated glomerular filtration rate, hemoglobin A1c level, and low-density-lipoprotein cholesterol (LDL-C) level. At the end of the study, we assessed 46 individuals from the UC group and 48 from the telemedicine group. Dropout rates and adverse events are discussed subsequently.
Figure 1.
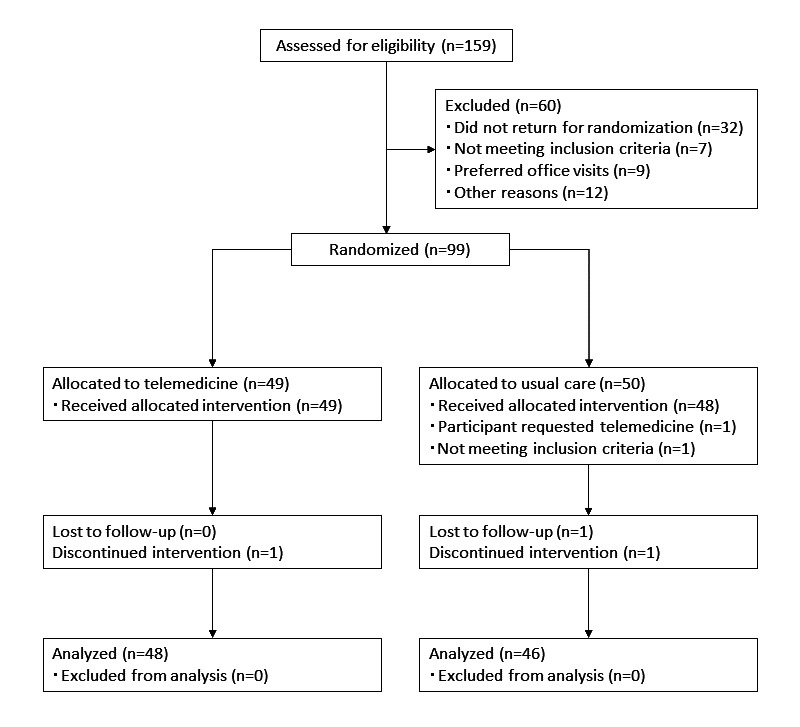
CONSORT (Consolidated Standards of Reporting Trials) flowchart for the study. TM: telemedicine, UC: usual care.
Table 1.
Baseline characteristics of the study participants (N=97).
| Parameters | All participants | Usual care group (n=48) | Telemedicine group (n=49) |
| Female, n (%) | 58 (60%) | 30 (63%) | 28 (57%) |
| Age (years), mean (SD) | 53 (9) | 53 (9) | 53 (9) |
| BMI (kg/m2), mean (SD) | 24.2 (3.9) | 24.3 (4.3) | 24.2 (3.4) |
| Home systolic blood pressure (mmHg), mean (SD) | 136 (13) | 136 (11) | 136 (15) |
| Home diastolic blood pressure (mmHg), mean (SD) | 91 (9) | 91 (8) | 90 (10) |
| Home pulse rate (bpm), mean (SD) | 73 (9) | 74 (9) | 73 (9) |
| Antihypertensive treatment, n (%) | 55 (57) | 29 (60) | 26 (53) |
| Estimated glomerular filtration rate (mL/min/1.73 m2), mean (SD) | 75.9 (14.0) | 77.3 (13.3) | 74.4 (14.4) |
| Low-density-lipoprotein cholesterol (mg/dL), mean (SD) | 121.1 (28.8) | 119.2 (28.9) | 123.0 (28.3) |
| Hemoglobin A1c (%), mean (SD) | 5.7 (0.3) | 5.6 (0.3) | 5.7 (0.3) |
| Plasma aldosterone (pg/mL), median (IQR) | 155 (119-216) | 150 (112-199) | 167 (136-232) |
| Plasma renin activity (ng/mL/h), median (IQR) | 1.1 (0.6-1.9) | 0.9 (0.5-1.8) | 1.2 (0.9-2.0) |
Changes in HBP and Laboratory Data Before and After the Study
Home SBP and DBP significantly decreased after 1 year in both groups (Tables 2 and 3). Plasma renin activity was significantly increased in the UC group (P=.02) but not in the telemedicine group.
Table 2.
Outcomes.
|
|
Usual care group | Telemedicine group | P value | ||||||
|
|
Preintervention (n=48) | Postintervention (n=46) | P value | Preintervention (n=49) | Postintervention (n=48) | P value |
|
||
| BMI (kg/m2), mean (SD) | 24.2 (4.3) | 3.9 (4.1) | .86 | 24.2 (3.4) | 23.9 (3.3) | .29 | .10 | ||
| Home systolic blood pressure (mmHg), median (95% CI) | 136 (133-139) | 131 (128-134) | .01 | 136 (132-140) | 125 (122-128) | <.001 | .02 | ||
| Home diastolic blood pressure (mmHg), median (95% CI) | 91 (89-93) | 87 (85-89) | .02 | 90 (87-93) | 83 (81-85) | <.001 | .07 | ||
| Home pulse rate (bpm), mean (SD) | 74 (9) | 71 (7) | .46 | 73 (9) | 71 (8) | .08 | .08 | ||
| Systolic blood pressure control rate (%) | 41.3 | 70.0 | <.001 | 47.7 | 85.4 | <.001 | .01 | ||
| Estimated glomerular filtration rate (mL/min/1.73 m2), mean (SD) | 77.3 (13.3) | 76.8 (11.9) | .16 | 74.4 (14.4) | 72.4 (14.4) | .30 | .05 | ||
| Potassium (mEq/L), mean (SD) | 4.1 (0.3) | 4.1 (0.3) | .81 | 4.1 (0.3) | 4.1 (0.3) | .65 | .93 | ||
| Low-density-lipoprotein cholesterol (mg/dL), mean (SD) | 119.2 (28.9) | 110.3 (22.7) | .53 | 123.0 (28.3) | 123.8 (28.6) | .11 | .04 | ||
| Hemoglobin A1c (%), mean (SD) | 5.6 (0.3) | 5.7 (0.3) | .74 | 5.7 (0.3) | 5.7 (0.4) | .60 | .53 | ||
| Plasma aldosterone (pg/mL), median (IQR) | 150 (112-199) | 151 (115-226) | .07 | 167 (136-232) | 171 (139-229) | .54 | .49 | ||
| Plasma renin activity (ng/mL/h), median (IQR) | 0.9 (0.5-1.8) | 1.1 (0.6-3.6) | .02 | 1.2 (0.9-2.0) | 1.9 (1.1-4.8) | .07 | .57 | ||
Table 3.
Home blood pressure change from baseline till the end of the 1-year study period.
|
|
Usual care group | Telemedicine group | P value |
| Change in systolic blood pressure (mmHg), mean (SD) | –5.4 (11.3) | –9.2 (14.3) | .23 |
| Change in diastolic blood pressure (mmHg), mean (SD) | –3.5 (8.1) | –5.5 (8.7) | .33 |
Differences in HBP Between the Participant Groups
The average home SBP during the last week of the study was significantly lower (by 6 mmHg) in the telemedicine group than in the UC group (Table 2). Home DBP after the 1-year study period tended to be lower in the telemedicine group, but the difference was not significant. The average SBP and DBP reached the therapeutic targets of less than 135 mmHg and 85 mmHg, respectively, at the time of measurement in the telemedicine group only.
When morning (4-10:59 AM) and evening (6 PM to 3:59 AM) BPs were analyzed separately (Table 4), the telemedicine group showed significantly lower evening SBP and DBP readings. The average morning SBP and DBP readings were also lower in the telemedicine group, but the difference was not significant.
Table 4.
Average morning and evening home blood pressure readings during the last week of the 1-year study period.
|
|
Usual care group (n=46), mean (SD) | Telemedicine group (n=48), mean (SD) | P value | |
| Morning | ||||
|
|
Home systolic blood pressure (mmHg) | 134.0 (8.6) | 130.6 (10.3) | .09 |
|
|
Home diastolic blood pressure (mmHg) | 90.6 (7.2) | 88.3 (7.7) | .14 |
|
|
Home pulse rate (bpm) | 71.6 (8.0) | 69.7 (7.5) | .25 |
| Evening | ||||
|
|
Home systolic blood pressure (mmHg) | 131.6 (8.7) | 125.8 (11.5) | .007 |
|
|
Home diastolic blood pressure (mmHg) | 87.2 (7.5) | 82.5 (7.5) | .003 |
|
|
Home pulse rate (bpm) | 76.3 (9.4) | 74.2 (8.5) | .27 |
The number of BP measurements per week for the whole study period was significantly higher in the telemedicine group (17.8, SD 11.5) than in the UC group (12.1, SD 11.0) (P=.02).
Clinical Parameters at the End of the Study
At the end of the study, LDL-C was significantly lower in the UC group than in the telemedicine group. Plasma renin activity was not significantly different between the 2 groups at baseline, but significantly increased at the endpoint only in the UC group. The endpoint plasma renin activity was not significantly different between the 2 groups. Other laboratory data were not significantly different between the 2 groups.
Prescription Data for Antihypertensive Medications
Percentages of antihypertensive treatment are shown in Table 5.
Table 5.
Prescription data.
|
|
Usual care group | Telemedicine group | |
|
|
Preintervention (n=48), n (%) | Preintervention (n=49), n (%) | Postintervention (n=48), n (%) |
| No medication | 29 (60.0) | 26 (54.2) | 7 (14.6) |
| Calcium channel blocker only | 11 (23.0) | 13 (27.1) | 8 (16.7) |
| Angiotensin II receptor blocker only | 0 (0) | 2 (4.2) | 3 (6.3) |
| Mineralocorticoid receptor blocker only | 2 (4.0) | 0 (0) | 3 (6.3) |
| Angiotensin II receptor blocker/angiotensin converting enzyme inhibitor + calcium channel blocker | 5 (10.0) | 7 (14.6) | 22 (45.8) |
| Mineralocorticoid receptor blocker + calcium channel blocker | 1 (2.0) | 1 (2.1) | 3 (6.3) |
| Angiotensin II receptor blocker + diuretic | 0 (0) | 0 (0) | 0 (0) |
| Angiotensin II receptor blocker/angiotensin converting enzyme inhibitor + calcium channel blocker + diuretic | 0 (0) | 0 (0) | 2 (4.2) |
Dropout Rates and Adverse Events
Of the 50 and 49 participants allocated to the UC and telemedicine groups, respectively, we assessed 46 from the UC group and 48 from the telemedicine group. In the UC group, a participant requested telemedicine, another did not meet the inclusion criteria, and another was lost to follow-up; hence, all 3 were excluded from the study. One participant from the UC group experienced a mild subarachnoid hemorrhage with no neurological deficits or hospitalization and dropped out of the study. In the telemedicine group, 1 participant experienced angina pectoris and discontinued the intervention. Medication-related complaints upon initiation or change of antihypertensive drugs included urticaria (n=1) and concerns of having considerably low BP (n=3). No discontinuation owing to drug side effects or difficulty using the telemedicine interface was recorded.
Discussion
Principal Findings
This study, for the first time in Japan, conducted hypertension treatment using telemonitoring and telemedicine without face-to-face visits for 1 year and revealed 2 major findings. First, telemedicine without actual office visits was determined to be relatively safe in managing hypertension for 1 year. Second, the telemedicine group achieved a lower BP than the UC group. Although the BP difference from baseline was not significantly different between the groups, the telemedicine group demonstrated a reduction in SBP of 9.2 mmHg, whereas the reduction in the UC group was 5.4 mmHg.
In a previous study that investigated the safety of telemedicine without office visits, the number of adverse events was not significantly different from that of UC. In the Telemonitoring and Self-management of Hypertension (TASMINH2) Trial, the frequency of side effects, such as swelling of legs, stiff joints, fatigue, and cough, was similar between the telemedicine and UC groups [5]. In our study, 2 patients dropped out owing to cardiovascular events during the study: 1 from the telemedicine group for new-onset angina pectoris and 1 from the UC group for subarachnoid hemorrhage. No significant difference in the laboratory findings was observed between the 2 groups at the end of the study, except for lower LDL-C in the UC group. Medication-related complaints were successfully managed through web-based consultations. The results of this and previous studies suggest that telemedicine is reasonably safe for use in controlling BP in uncomplicated hypertension.
Superior BP control in the telemedicine group than that in the UC group could be attributed to several factors, one being the intensity of the intervention. Sheppard et al [8] demonstrated that intense interventions, such as pharmacotherapeutic intervention managed by a pharmacist, with frequent telemonitoring, were more effective than low-intensity interventions, such as telemonitoring only, in patients with obesity. In this study, the telemedicine group received team-based care from physicians specializing in hypertension, and the participants were able to ask questions using the app. Therefore, the effects of antihypertensive intervention could have been enhanced by the more intensive interventions and greater expertise that the telemedicine group received. Several studies found that telemonitoring of BP improves BP control [3,4]. On the other hand, other studies showed that telemonitoring by itself does not significantly improve it [9]. Pellegrini et al [10] recently reported that self-monitoring of BP at home with co-interventions, such as telecounseling, favorably controlled BP more than self-monitoring of BP alone did. Nevertheless, regardless of their effects on BP control, advances in internet technology and data technology should accelerate the dissemination of BP telemonitoring and telemedicine, which would make retrospective analysis of BP management interventions in the future much easier than those in the past, when such analysis depended on a paper-based approach. In our previous study, an electronic sphygmomanometer with an automated 3G data transfer and room temperature monitor was used for daily SMBP [11]. BP variability based on SMBP can predict cardiovascular outcome in patients with hypertension [12,13]. Room temperature at the time of SMBP significantly correlates with variability of SBP [14,15]. Therefore, an HBP monitor equipped with various sensors, serving as the “Internet of Things,” may be used to monitor environmental conditions to maintain the optimal BP in future studies.
Regarding adherence, the frequency of HBP measurements was much higher in the telemedicine group than in the UC group. We do not have data on medication adherence, but Ogedegbe and Schoenthaler [16] demonstrated that HBP self-monitoring significantly improved medication adherence and reported that the telemedicine group self-monitored their BP more frequently.
Limitations
This study has several limitations. First, this study was limited by its design in that the physicians’ level of expertise differed for the telemedicine and UC groups. Second, although the rate of treated hypertension at baseline was not different between the groups, changes in prescription were precisely tracked only in the telemedicine group. Third, the number of visits for the UC group was not determined, and the average number of visits could not be compared. In Japan, regular face-to-face visits for hypertension management in clinics generally occur at 2- to 8-week intervals. Fourth, because the study was terminated prematurely, it did not reach its intended sample size, making the power of the study insufficient for some analyses. Nevertheless, our finding of a significantly lower HBP at the end of the study period in the telemedicine group despite a smaller-than-intended sample size is promising for the improvement of BP control through telemedicine. Fifth (related to the first limitation), although the participants in the UC group were referred to primary care physicians with a letter asking them to target an HBP of less than 135/85 mmHg, it is not clear whether the physicians actually adhered to this request [17]. Although this study cannot delineate the effects of telemonitoring, telemedicine, and specialist intervention compared with UC, ours is a real-world study providing pilot data on hypertension telemedicine in Japan, which can be used to design future studies.
Conclusions
Our results suggest that antihypertensive telemedicine using HBP telemonitoring and web-based video visits is safe. The telemedicine group of patients with uncomplicated hypertension achieved better BP control than the group assigned to conventional care. Further investigations are required to elucidate the benefits of telemedicine in treating hypertension on a larger scale.
Acknowledgments
This study was conducted at Tokyo Women’s Medical University. This study was supported in part by the PORT Corporation. We gratefully acknowledge the excellent technical assistance of Erina Yamaguchi, who participated in data collection and analysis.
Abbreviations
- BP
blood pressure
- DBP
diastolic blood pressure
- HBP
home blood pressure
- LDL-C
low-density-lipoprotein cholesterol
- POATRAND
Paradigm of Antihypertensive Therapy Along With Telemedicine Randomized Trial
- SBP
systolic blood pressure
- SMBP
self-measurement of home blood pressure
- UC
usual care
CONSORT-eHEALTH checklist (V 1.6.1).
Footnotes
Authors' Contributions: JY and MSY contributed to the design of the study and performed data collection and analysis. JY, MSY, RO, and AI drafted, critically revised, and approved the final version of the paper for submission.
Conflicts of Interest: JY and MSY are directors of General Incorporated Association TelemedEASE, which aims to facilitate safe and effective telemedicine.
References
- 1.Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, Horio T, Hoshide S, Ikeda S, Ishimitsu T, Ito M, Ito S, Iwashima Y, Kai H, Kamide K, Kanno Y, Kashihara N, Kawano Y, Kikuchi T, Kitamura K, Kitazono T, Kohara K, Kudo M, Kumagai H, Matsumura K, Matsuura H, Miura K, Mukoyama M, Nakamura S, Ohkubo T, Ohya Y, Okura T, Rakugi H, Saitoh S, Shibata H, Shimosawa T, Suzuki H, Takahashi S, Tamura K, Tomiyama H, Tsuchihashi T, Ueda S, Uehara Y, Urata H, Hirawa N. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019) Hypertens Res. 2019 Sep;42(9):1235–1481. doi: 10.1038/s41440-019-0284-9.10.1038/s41440-019-0284-9 [DOI] [PubMed] [Google Scholar]
- 2.Chobanian AV. Shattuck Lecture. The hypertension paradox--more uncontrolled disease despite improved therapy. N Engl J Med. 2009 Aug 27;361(9):878–887. doi: 10.1056/NEJMsa0903829.361/9/878 [DOI] [PubMed] [Google Scholar]
- 3.Duan Y, Xie Z, Dong F, Wu Z, Lin Z, Sun N, Xu J. Effectiveness of home blood pressure telemonitoring: a systematic review and meta-analysis of randomised controlled studies. J Hum Hypertens. 2017 Jul;31(7):427–437. doi: 10.1038/jhh.2016.99.jhh201699 [DOI] [PubMed] [Google Scholar]
- 4.Omboni S, Gazzola T, Carabelli G, Parati G. Clinical usefulness and cost effectiveness of home blood pressure telemonitoring: meta-analysis of randomized controlled studies. J Hypertens. 2013 Mar;31(3):455–467. doi: 10.1097/HJH.0b013e32835ca8dd. [DOI] [PubMed] [Google Scholar]
- 5.McManus R, Mant J, Bray E, Holder R, Jones MI, Greenfield S, Kaambwa B, Banting M, Bryan S, Little P, Williams B, Hobbs FDR. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomised controlled trial. Lancet. 2010 Jul 17;376(9736):163–172. doi: 10.1016/S0140-6736(10)60964-6.S0140-6736(10)60964-6 [DOI] [PubMed] [Google Scholar]
- 6.Horio M, Imai E, Yasuda Y, Watanabe T, Matsuo S. Modification of the CKD epidemiology collaboration (CKD-EPI) equation for Japanese: accuracy and use for population estimates. Am J Kidney Dis. 2010 Jul;56(1):32–38. doi: 10.1053/j.ajkd.2010.02.344.S0272-6386(10)00592-5 [DOI] [PubMed] [Google Scholar]
- 7.Takahashi H, Yoshika M, Yokoi T. Validation of two automatic devices: Omron HEM-7252G-HP and Omron HEM-7251G for self-measurement of blood pressure according to the European Society of Hypertension International Protocol revision 2010. Blood Press Monit. 2015 Oct;20(5):286–290. doi: 10.1097/MBP.0000000000000127. [DOI] [PubMed] [Google Scholar]
- 8.Sheppard J, Tucker K, Davison W, Stevens R, Aekplakorn W, Bosworth HB, Bove A, Earle K, Godwin M, Green BB, Hebert P, Heneghan C, Hill N, Hobbs FDR, Kantola I, Kerry SM, Leiva A, Magid DJ, Mant J, Margolis KL, McKinstry B, McLaughlin MA, McNamara K, Omboni S, Ogedegbe O, Parati G, Varis J, Verberk WJ, Wakefield BJ, McManus RJ. Self-monitoring of Blood Pressure in Patients With Hypertension-Related Multi-morbidity: Systematic Review and Individual Patient Data Meta-analysis. Am J Hypertens. 2020 Mar 13;33(3):243–251. doi: 10.1093/ajh/hpz182. http://europepmc.org/abstract/MED/31730171 .5626378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tucker KL, Sheppard JP, Stevens R, Bosworth HB, Bove A, Bray EP, Earle K, George J, Godwin M, Green BB, Hebert P, Hobbs FDR, Kantola I, Kerry SM, Leiva A, Magid DJ, Mant J, Margolis KL, McKinstry B, McLaughlin MA, Omboni S, Ogedegbe O, Parati G, Qamar N, Tabaei BP, Varis J, Verberk WJ, Wakefield BJ, McManus RJ. Self-monitoring of blood pressure in hypertension: A systematic review and individual patient data meta-analysis. PLoS Med. 2017 Sep;14(9):e1002389. doi: 10.1371/journal.pmed.1002389. https://dx.plos.org/10.1371/journal.pmed.1002389 .PMEDICINE-D-16-03401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pellegrini D, Torlasco C, Ochoa JE, Parati G. Contribution of telemedicine and information technology to hypertension control. Hypertens Res. 2020 Jul;43(7):621–628. doi: 10.1038/s41440-020-0422-4.10.1038/s41440-020-0422-4 [DOI] [PubMed] [Google Scholar]
- 11.Yatabe J, Yatabe MS, Morimoto S, Watanabe T, Ichihara A. Effects of room temperature on home blood pressure variations: findings from a long-term observational study in Aizumisato Town. Hypertens Res. 2017 Aug;40(8):785–787. doi: 10.1038/hr.2017.18.hr201718 [DOI] [PubMed] [Google Scholar]
- 12.Stevens SL, Wood S, Koshiaris C, Law K, Glasziou P, Stevens RJ, McManus RJ. Blood pressure variability and cardiovascular disease: systematic review and meta-analysis. BMJ. 2016 Aug 09;354:i4098. doi: 10.1136/bmj.i4098. http://www.bmj.com/lookup/pmidlookup?view=long&pmid=27511067 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Juhanoja EP, Niiranen TJ, Johansson JK, Puukka PJ, Thijs L, Asayama K, Langén VL, Hozawa A, Aparicio LS, Ohkubo T, Tsuji I, Imai Y, Stergiou GS, Jula AM, Staessen JA, International Database on Home Blood Pressure in Relation to Cardiovascular Outcome (IDHOCO) Investigators Outcome-Driven Thresholds for Increased Home Blood Pressure Variability. Hypertension. 2017 Apr;69(4):599–607. doi: 10.1161/HYPERTENSIONAHA.116.08603.HYPERTENSIONAHA.116.08603 [DOI] [PubMed] [Google Scholar]
- 14.Iwahori T, Miura K, Obayashi K, Ohkubo T, Nakajima H, Shiga T, Ueshima H. Seasonal variation in home blood pressure: findings from nationwide web-based monitoring in Japan. BMJ Open. 2018 Jan 05;8(1):e017351. doi: 10.1136/bmjopen-2017-017351. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=29306878 .bmjopen-2017-017351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hanazawa T, Asayama K, Watabe D, Tanabe A, Satoh M, Inoue R, Hara A, Obara T, Kikuya M, Nomura K, Metoki H, Imai Y, Ohkubo T, HOMED‐BP (Hypertension Objective Treatment Based on Measurement by Electrical Devices of Blood Pressure) Investigators Association Between Amplitude of Seasonal Variation in Self-Measured Home Blood Pressure and Cardiovascular Outcomes: HOMED-BP (Hypertension Objective Treatment Based on Measurement By Electrical Devices of Blood Pressure) Study. J Am Heart Assoc. 2018 May 04;7(10):e008509. doi: 10.1161/JAHA.117.008509. https://www.ahajournals.org/doi/10.1161/JAHA.117.008509?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .JAHA.117.008509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ogedegbe G, Schoenthaler A. A systematic review of the effects of home blood pressure monitoring on medication adherence. J Clin Hypertens (Greenwich) 2006 Mar;8(3):174–180. doi: 10.1111/j.1524-6175.2006.04872.x. https://onlinelibrary.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=1524-6175&date=2006&volume=8&issue=3&spage=174 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nishigaki N, Shimasaki Y, Yoshida T, Hasebe N. Physician and patient perspectives on hypertension management and factors associated with lifestyle modifications in Japan: results from an online survey. Hypertens Res. 2020 May;43(5):450–462. doi: 10.1038/s41440-020-0398-0. http://europepmc.org/abstract/MED/31996815 .10.1038/s41440-020-0398-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
CONSORT-eHEALTH checklist (V 1.6.1).


