Abstract
Background and Objectives
Behavioral health issues, such as substance use, depression, and social isolation, are of grave concern during COVID‐19, especially for vulnerable populations. One such population is US veterans, who have high rates of pre‐existing behavioral health conditions and may thus be at‐risk for poorer outcomes. The current study aimed to investigate substance use among US veterans during COVID‐19 as a function of pre‐existing depression, loneliness, and social support.
Methods
We investigated the relationship between pre‐pandemic depression and substance use during COVID‐19 using linear (alcohol) and logistic (cannabis) regression among a large sample of US veterans (N = 1230). We then tested if loneliness and social support moderated these effects.
Results
Though there was a decrease in alcohol and cannabis use among the overall sample, veterans who screened for depression prior to the pandemic exhibited higher levels of substance use after the pandemic's onset. Loneliness compounded the effects of depression on rates of alcohol use. Social support was not protective for the effects of depression on either alcohol or cannabis use.
Discussion and Conclusions
Veterans with pre‐existing depression may be in need of attention for substance use behaviors. Interventions aimed at alleviating loneliness among veterans may be useful in mitigating alcohol use, but not cannabis use, amid COVID‐19.
Scientific Significance
Our findings are among the first to report tangible behavioral health outcomes experienced by US veterans as a result of COVID‐19. Results can help inform treatment efforts for veterans who are struggling with substance use during and post‐pandemic.
INTRODUCTION
In the spring of 2020, the United States implemented lockdown measures to combat the spread of COVID‐19. Consequently, there is increasing worry about the impact of COVID‐19 on behavioral health, with a common liability during the pandemic being loneliness. Many have experienced increased levels of isolation, which can lead to amplified feelings of loneliness and associated negative physical and mental health problems. 1 Specifically, during COVID‐19, lack of social support and loneliness are posited to be major risk factors for mental health consequences and substance use. 2 , 3 Recent research indicates increases in alcohol 4 , 5 and cannabis use, 6 as well as mental health symptomology, 7 , 8 among the general population. Others have noted special consideration for behavioral health (i.e., substance use) may be needed for individuals reporting heightened loneliness and lack or loss of social support, especially in the context of increasing levels of depression during the pandemic. 3 Unfortunately, most COVID‐related behavioral health research has been focused on cross‐sectional studies involving samples of the general population, with little direct attention being given to the long‐term consequences of the pandemic or to particularly vulnerable populations.
Loneliness and social support theory
Existing research conceptualizes loneliness as the perception of unfulfilling relationships resulting in feelings of seclusion, which leads to subsequent wide‐ranging physical and behavioral health issues. 9 Hawkley and Cacioppo's Loneliness Model theory 9 posits that health consequences of loneliness (e.g., depression) may reinforce socially isolating behaviors, thereby exacerbating the experience of loneliness even more. Others have suggested that theories of loneliness are of vital importance in the context of substance use disorders (SUDs) specifically, as those who engage in harmful or problematic substance use are more likely to endorse feelings of loneliness and isolation, and vice versa. 10 Conversely, the stress and coping perspective theory of social support posits that perceived support may help mitigate the adverse effects of stressful events on health outcomes, 11 while lower levels of social support inversely can lead to poorer health outcomes, such as depression. 12
Recent empirical work supports these notions in the context of COVID‐19. Researchers have reported that individuals with higher levels of social support had lower depression levels than those who have less support during COVID‐19. 13 Initial reports also indicate that loneliness is associated with decreased mental health during the pandemic, though research is still growing on this topic, as one study reported loneliness as a risk factor for depression during the pandemic among older adults in the United kingdom. 14 Augmenting this, consistent with Ingram and colleagues' theory, 10 those who experience loneliness or minimal social support amid COVID‐19 may also be more likely to use substances. Substance use has been a major behavioral health concern during COVID‐19, with some calling for specific attention to SUDs during the pandemic. 15 , 16 A predisposition to depression may further increase hazardous substance use during the pandemic, particularly if one has limited social interaction due to restrictions on social gatherings. In one study of US adults in the wake of COVID‐19 lockdowns, loneliness and lack of social connectedness predicted hazardous alcohol use and drug‐related consequences, mediated by anxiety and depression symptoms. 3 Additionally, Bartel et al. 6 reported that social isolation, compounded with depression‐related coping motives, predicted increases in cannabis use during the pandemic, compared with pre‐pandemic levels. Taken together, it is evident that the interaction of depression with loneliness and/or social support may portend additional risk for increased substance use behaviors. Additional research is needed to explore these topics among those most vulnerable to behavioral health consequences.
Veterans amid COVID‐19
Veterans are disproportionately at‐risk for behavioral health problems, including depression and heavy substance use. 17 , 18 As current research points to such pre‐existing health conditions as a risk factor for consequences related to poorer mental health and substance use during COVID‐19, 19 veterans with pre‐existing mental health problems may struggle with exacerbated mental health and substance use difficulties throughout the pandemic. Reports indicate veterans are at‐risk for loneliness and social isolation prior to 20 and during the pandemic, 21 which has been found to further intensify behavioral health problems. 22 Further, consistent with social support theory, 11 veterans who have lower levels of social support are more likely to partake in heavy drinking, with high social support being protective against excessive drinking. 23
Though an at‐risk group for behavioral health conditions, there is little research that investigates behavioral health outcomes of the pandemic on U.S. veterans. Most pandemic‐related behavioral health research on veterans focuses on the use of telehealth within Veterans Affairs (VA) systems to develop recommendations for its expansion during COVID‐19. 24 The tangible effects of the pandemic on veterans' mental health has remained largely unexplored. The present study investigated the associations between loneliness, social support, and pre‐pandemic depression on veterans' substance use behaviors during the first 6 months of the pandemic in the United States. Specifically, we looked at the impacts on alcohol and cannabis use, as these substances are two of the most often used among veteran populations. 25 Further, in line with theories of isolation and social support, we aimed to understand how loneliness and limited social support during the pandemic influenced the relationship between depression and substance use, hypothesizing that those with greater reported loneliness and limited social support would be engaging in the heaviest substance use, particularly if they reported pre‐pandemic depression.
METHODS
Participants and procedures
Veterans were eligible to participate if they were aged 18–40 and previously served in one of the following branches of the US Armed Forces: Air Force, Army, Marine Corps, or Navy. Potential participants were recruited in February 2020 (Time 1) from social media websites (e.g., Facebook, RallyPoint) as part of a larger survey effort to examine substance use and mental health symptoms among a sample of veterans recruited outside of VA settings. A general sample of veterans was sought for the study; thus, there were no eligibility criteria related to substance use or mental health. There were no other exclusion criteria. Data collection was completed in February 2020, which was approximately one month prior to the declaration of a national emergency in the United States in March 2020. 26 A total of 1855 individuals responded to the survey, of which 1230 participants were screened as eligible, consented to participate, and passed a series of internal validation checks. Such checks were used to ensure individuals were not misrepresenting themselves (e.g., giving participants “insider knowledge” items about military service to verify veteran status, endorsing consistent responses between items), repeatedly completing the survey to collect multiple incentives (e.g., checking for duplicate IP addresses), or carelessly responding to items and making data invalid (e.g., checking time stamps to verify they completed the survey in a possible length of time, including “check items” to make sure participants were paying attention to item wording). Participants received a $20 Amazon gift card for completing a 30‐min online survey.
The same participants were recontacted by email 6 months after the baseline survey in August 2020 (Time 2) to complete a follow‐up survey about substance use and mental health, with additional items assessing their experiences with COVID‐19. Of the 1230 invited, 1025 completed the follow‐up survey and passed internal validation checks (83%). Participants received a $30 Amazon gift card for completing the follow‐up 30‐min online survey. All procedures were approved by the local Institutional Review Board at the university where the study was conducted.
Measures
Demographics and military characteristics
Participants reported their age, race/ethnicity, gender, branch of service, marital status (married/unmarried), and whether they had children living at home with them.
Depression
Depression symptom severity was assessed at Time 1 and Time 2 using the 8‐item Patient Health Questionnaire (PHQ‐8), 27 where participants indicated how often they experienced eight symptoms of depression (e.g., feeling down, depressed, or hopeless). Symptoms were rated over the past two weeks from not at all (0) to (3) nearly every day; yielding a sum score between 0 and 24 (α = .85). Participants who scored at or above a cutoff score of 10 27 were classified with a positive screen for possible depression.
Alcohol and cannabis use
At Time 1 and Time 2, participants completed items for past 30‐day alcohol use using the daily drinking questionnaire (DDQ), 28 which assesses the typical number of drinks consumed on each day of a typical week and yields a total drink per week variable. Pictures of standard drinks preceded the DDQ (e.g., 12 oz. beer, 5 oz. wine, 0.5 oz hard liquor). Participants also reported any use of cannabis in any form (e.g., smoking, vaping, edible) over the past 30 days.
Loneliness and social support
At Time 2, loneliness was measured with the 20‐item UCLA Loneliness Scale, 29 which assessed how often the participant felt feelings related to loneliness, such as “How often do you feel alone,” “How often do you feel close to people,” and “How often do you feel left out” (1 = never to 4 = always). A sum score was calculated ranging from 20 to 80 (α = .63). Social support was assessed at Time 2 with the RAND Social Support Survey from the Medical Outcomes Study, 30 which consisted of 18 items assessing social support in areas of emotional/informational (e.g., someone to confide in), tangible (e.g., someone to help you if sick), affectionate (e.g., someone who sows you love), positive social interaction (e.g., someone to have a good time with), and an additional item regarding having someone to do things with to get your mind off things. The scale yields a mean score across items (1 = none of the time to 5 = all of the time) on how often each kind of support is available (α = .78).
Analytic plan
The first aim of this study was to investigate the association between pre‐existing depression and substance use behaviors during the pandemic. To do this, we predicted Time 2 past month drinks per week (linear regression) and any past month cannabis use (logistic regression) in separate models with pre‐pandemic depression screens on the PHQ‐8 as the predictor, controlling for Time 1 substance use and demographic and military characteristics. The second aim of our study was to examine whether loneliness and social support during the pandemic moderated the relationship between depression and substance use. To do this, we added Time 2 loneliness and social support to drinks per week and any cannabis models as independent predictors. Next, we included depression screen × loneliness and depression screen × social support interactions in the models to test for moderation. Significant interactions were plotted for interpretation using low and high values of the moderator (+1 to −1 standard deviations from the mean) and all continuous variables were grand mean‐centered to facilitate interpretation.
RESULTS
Sample description
A description of the analytic sample can be found in Table 1. Participants were 34.6 (SD = 3.5) years old, and the majority of participants were white (82.9%) and male gender (89.5%). Participants were primarily veterans separated from the Army (70.4%). Most were married (92.2%) and had children living at home (63.1%). Nearly one‐third (31.9%) met the criteria for depression at Time 1. Participants reported a mean of 48.8 on the UCLA loneliness scale (range 20 to 80) and a mean of 3.17 on the MOS Social Support Survey (range, 1–5).
Table 1.
Analytic sample characteristics
| All participants (N = 1025) | ||
|---|---|---|
| N/mean | %/SD | |
| Age | 34.6 | 3.5 |
| Race/ethnicity | ||
| Hispanic/Latinx | 90 | 8.8% |
| Black/African American | 62 | 6.0% |
| Asian | 12 | 1.2% |
| White | 850 | 82.9% |
| Multiracial/other | 11 | 1.1% |
| Gender | ||
| Male | 917 | 89.5% |
| Female | 96 | 9.4% |
| Other | 12 | 1.2% |
| Branch | ||
| Air force | 123 | 12.0% |
| Army | 722 | 70.4% |
| Marine corps | 94 | 9.2% |
| Navy | 86 | 8.4% |
| Marital status | ||
| Unmarried | 80 | 7.8% |
| Married | 945 | 92.2% |
| Children in home | ||
| Yes | 647 | 63.1% |
| No | 378 | 36.9% |
| Depression (PHQ‐8) screen | 327 | 31.9% |
| Loneliness (UCLA) sum score | 48.8 | 7.1 |
| Social support mean score | 3.17 | 0.56 |
Note: Depression screen represents those with a score of 10 or higher on the Patient Health Questionnaire 8‐item at Time 1. Loneliness is the composite score from the UCLA Loneliness Scale at Time 2. Social support is the mean score on the MOS Social Support Survey.
Abbreviation: PHQ‐8, 8‐item Patient Health Questionnaire.
Alcohol outcome
Table 2 contains the final model for drinks per week. Participants reported drinking 6.34 (SD = 9.65) drinks per week at Time 2, which was approximately 5.8 drinks less than they reported drinking at Time 1, t (1022) = 18.43, p < .001. Though participants reported less drinking over time, those participants who screened positive for depression at Time 1 reported drinking significantly more at Time 2 than participants who did not screen positive for depression. In the model controlling for demographics and Time 1 drinks per week, a positive screen for depression at Time 1 was associated with more drinks per week at Time 2 (β = 3.52, SE = 0.69, p < .001; b = 0.17), such that a standard deviation increase in Time 1 depression is associated with a 0.17 standard deviation increase in drinks per week at Time 2 (5.2 drinks compared with 8.7 drinks; see Figure 1, top).
Table 2.
Final model predicting drinks per week and any cannabis use at Time 2
| Drinks per week (past month), b (95% CI) | Cannabis use (past month), OR (95% CI) | |
|---|---|---|
| Constant | 5.01 (2.94, 7.08) | 0.01 (–) |
| Drinks per week at Time 1 | 0.40 (0.34, 0.46) | – |
| Any cannabis use at Time 1 | – | 5.18 (3.01, 8.92) |
| Depression screen at Time 1 | 3.43 (2.06, 4.79) | 2.49 (1.46, 4.25) |
| Loneliness | 0.02 (−0.09, 0.12) | 1.01 (0.96, 1.07) |
| Loneliness × depression | 0.24 (0.62, 0.41) | 0.98 (0.92, 1.06) |
| Social support | 0.01 (−1.29, 1.31) | 1.08 (0.56, 2.09) |
| Social support × depression | 1.83 (−0.38, 4.03) | 2.14 (0.90, 5.09) |
Note: Loneliness is the composite score from the UCLA Loneliness Scale at Time 2. Social support is the mean score on the MOS Social Support Survey. Analyses controlled for age, gender (male gender reference group), race/ethnicity (White race/ethnicity reference group), branch of service (Army reference group), marital status, and children living in the home. Bold values indicate p < .05.
Abbreviations: b, unstandardized coefficient; CI, confidence interval; OR, odds ratio.
Figure 1.
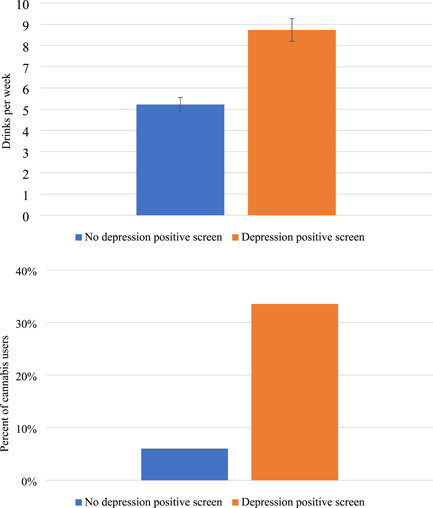
Drinks per week and percent of cannabis users at Time 2 by Time 1 depression screening. Figure 1 (top) contains estimated marginal means and 95% confidence intervals. Models controlled for age, race, gender, marital status, children living at home, and the Time 1 outcome
Next, we added the main effects of loneliness and social support to the model. Results indicated loneliness was associated with more drinks per week at Time 2 (β = 0.07, SE = 0.04, p = .025; b = 0.10). There was no significant main effect for social support. When adding the depression × loneliness and the depression × social support interaction terms (see final model in Table 2), results only indicated a significant interaction effect for loneliness and depression (β = 0.10, SE = 0.09, p = .008; b = 0.24). Figure 2 shows the prototypical plots. We can see that participants with a positive depression screen at Time 1 who reported more loneliness at Time 2 reported drinking the most at Time 2. Tests of simple slopes revealed a significant slope for high loneliness (slope gradient = 5.10, t = 5.46, p < .001), but not for low loneliness (slope gradient = 1.76, t = 1.86, p = .064). There was no significant interaction between depression and social support.
Figure 2.
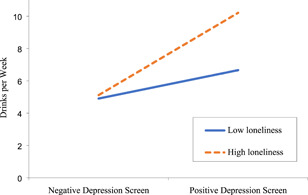
Interaction between depression screen at Time 1 and loneliness at Time 2 for the cannabis outcome
Cannabis outcome
At Time 1, 16.7% of the sample reported using any cannabis in the past 30 days, while at Time 2, 14.8% of the sample reported any use. Factoring in Time 1 depression screening, 33.5% of those who screened positive for depression at Time 1 used any cannabis in the past 30 days at Time 2, compared with 6.0% of those who did not screen positive (see Figure 1, bottom). In the model predicting any use of cannabis at Time 2, a positive screen for depression at Time 1 significantly predicted any Time 2 past 30‐day cannabis use (odds ratio [OR] = 2.63, p < .001). When we added loneliness and social support to the model, there was no significant effect for loneliness (p = .742), but there was a significant effect for social support (OR = 1.61, p = .035). However, when the interaction terms were added to the model, the effect for social support was no longer significant, likely due to the interaction taking much of the variance of the main effect when the interaction was not included. There were no significant depression × loneliness or depression × social support interaction effects. Table 2 contains the final model for the cannabis outcome.
DISCUSSION
While COVID‐19 has had substantial consequences on public health, little is known about the effects it may have on at‐risk populations who are already susceptible to behavioral health problems, such as American military veterans. 17 , 18 The current study investigated substance use during the first six months of the COVID‐19 pandemic in the United States, as it relates to loneliness, social support, and depression among a large national sample of US veterans. While substance use decreased overall among the full sample from 1‐month pre‐pandemic to 6 months post, those who screened positive for depression prior to COVID‐19 had higher rates of both alcohol and cannabis use during the pandemic, with those with pre‐pandemic depression who experienced high levels of loneliness during the first six months of the pandemic drinking most heavily.
The overall decrease in alcohol and cannabis use was contrary to other reports noting substance use increases during COVID‐19. 4 , 15 , 16 This may be due to a dearth of opportunities to use substances, such as decreased ability to use in certain settings (e.g., not being able to drink at a bar with friends), and potential financial barriers to obtaining substances. 31 This may suggest a social component to cannabis use over and above any coping‐related motivations, though further research is needed to fully parse out the interaction of cannabis use and social mechanisms during COVID‐19. However, veterans with existing depression were more likely to use alcohol and cannabis, which is consistent with hypotheses and prior work that those with pre‐existing behavioral health conditions may be at risk for poorer behavioral health outcomes throughout the pandemic. 19 Mental health providers serving veterans, such as the Veterans Healthcare System (VA) and veteran service organizations, may thus need to emphasize treatment outreach during and after the pandemic to those with pre‐existing conditions such as depression.
Greater loneliness was associated with heavier drinking, and those with pre‐existing depression and greater loneliness during the pandemic reported the most drinking, in line with the theory that loneliness can lead to poorer health outcomes. 9 The association between loneliness and alcohol use was evident despite controlling for social support, which is not consistent with theories of social support 11 , 12 or other COVID‐related studies that reported social support being protective against such outcomes. 13 , 32 This suggests that, for veterans during COVID‐19, experiencing loneliness may have a larger role than social support in predicting substance use outcomes such as alcohol use. Even if social support is available to individuals at home during the pandemic (e.g., family members), loneliness related to not spending time with other groups outside the home (e.g., friends, coworkers, other veterans/military personnel) may impact cannabis or alcohol use and undermine protective effects. Although veterans who screened positive for depression were more likely to report any cannabis use during the pandemic than those who did not screen positive, loneliness was not associated with cannabis use, which is inconsistent with prior research on self‐isolation and cannabis use during COVID‐19 among other populations. 6 Social support, however, was positively associated with any cannabis use, which could imply a social component to cannabis use beyond a coping reason (i.e., using to manage depressive symptoms). These results seem to indicate that veterans have different motivations for using alcohol and cannabis during the pandemic, though additional research on use motives is needed to fully understand the differences.
Given the differences in predictors of alcohol and cannabis use, interventions aimed at reducing harmful substance use among veterans during and after the pandemic may thus benefit from different approaches depending on what substances an individual is using. For instance, emphasizing healthy ways to cope with feelings of isolation may be an important component of treatment targeting alcohol use, but not cannabis use, for veterans during COVID‐19. Forthcoming interventions to help mitigate the effects of isolation may also consider approaches aimed at correcting negative social cognition, as outlined by existing theory. 9 As we explored alcohol and cannabis use separately in the current study, research on polysubstance use is also needed to expand upon these findings. Co‐occurring SUDs are indeed common among veterans, 17 so further studies that assess co‐use of substances could enhance understanding of how using alcohol and cannabis together may have affected behavioral health outcomes for veterans amid and post‐COVID‐19.
Limitations and future directions
Findings should be taken in light of the current study's limitations. First, data were collected through self‐report measures and may be subject to certain biases as a result (e.g., social desirability, recall), though there is evidence to support the validity of self‐reported substance use. 33 Second, our sample is comprised primarily of white male Army veterans recruited online through a nontreatment setting. Though the Army is the military's largest branch, our sample recruited Army participants at a proportionally higher rate (~70%) than the general veteran population (~50%), perhaps due to the Army's representation on the social media sites we recruited from. Further, although our sample is proportional in terms of gender representation compared to veterans as a whole, generalizability is still limited. We also did not have a large enough sample with specific racial/ethnic groups to draw meaningful comparisons across these groups. The majority of the US veteran population is White, as reflected by our sample; however, current reports indicate that racial and ethnic minorities in the United States experience poorer outcomes from COVID‐19 due to systemic socioeconomic barriers and racism embedded within systems of healthcare. 34 Being able to look further at race and ethnicity differences is vital to understanding the full behavioral health and substance use impacts of the pandemic on veterans, especially as ethnic minority representation increases among US armed forces. Participants who completed the Time 1 survey only and not the Time 2 survey (about 17% attrition) were more likely to be women, non‐White, and reported higher depression and cannabis use at Time 1, indicating that better engagement efforts to retain these veterans in longitudinal research efforts are needed. Changes in the original sample may thus not be fully captured due to attrition bias, and results should be interpreted with this in mind. Future work can expand upon these findings through recruitment of a more diverse sample in terms of gender, race/ethnicity, and branch of service, as well as through recruiting clinical samples from a treatment/VA setting. Next, regarding our study's measurement, we only measured loneliness and social support at Time 2; studies that can directly compare these constructs to pre‐pandemic data are needed. Lastly, despite our study being longitudinal in nature, causation cannot be completely characterized, as there may be other variables not included in analyses that influence our study's outcomes of interest.
CONCLUSIONS
The present study has a number of unique strengths that supply vital contributions to the existing literature. This study is among the few currently published that have addressed changes over time in substance use and behavioral health, with data available both immediately prior to and during COVID‐19. Moreover, this study addresses an understudied group in the literature on the impacts of COVID‐19, being among the first to report behavioral health consequences faced by US veterans. We therefore provide preliminary results that may help inform imminent additional research as well as behavioral health interventions for this vulnerable population.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
ACKNOWLEDGMENTS
This research was funded by grant R01AA026575 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA), supplement R01AA026575‐02S1, and a Keck School of Medicine COVID‐19 Research Funding Grant awarded to Eric R. Pedersen.
Fitzke RE, Wang J, Davis JP, Pedersen ER. Substance use, depression, and loneliness among American veterans during the COVID‐19 pandemic. Am J Addict. 2021;30:552‐559. 10.1111/ajad.13211
REFERENCES
- 1. Hwang T‐J, Rabheru K, Peisah C, Reichman W, Ikeda M. Loneliness and social isolation during the COVID‐19 pandemic. Int Psychogeriatr. 2020;32(10):1217‐1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Liu CH, Zhang E, Wong GTF, Hyun S, Hahm HC. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID‐19 pandemic: clinical implications for U.S. young adult mental health. Psychiatry Res. 2020;290:113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Horigian VE, Schmidt RD, Feaster DJ. Loneliness, mental health, and substance use among US young adults during COVID‐19. J Psychoact Drugs. 2020;53:1‐9. [DOI] [PubMed] [Google Scholar]
- 4. Pollard MS, Tucker JS, Green HD Jr. Changes in adult alcohol use and consequences during the COVID‐19 pandemic in the US. JAMA Netw Open. 2020;3(9):e2022942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Vanderbruggen N, Matthys F, Van Laere S, et al. Self‐reported alcohol, tobacco, and cannabis use during COVID‐19 lockdown measures: results from a web‐based survey. Eur Addict Res. 2020;26(6):309‐315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bartel SJ, Sherry SB, Stewart SH. Self‐isolation: a significant contributor to cannabis use during the COVID‐19 pandemic. Subst Abus. 2020;41:1‐4. [DOI] [PubMed] [Google Scholar]
- 7. Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID‐19 pandemic. JAMA Netw Open. 2020;3(9):e2019686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rajkumar RP. COVID‐19 and mental health: a review of the existing literature. Asian J Psychiatr. 2020;52:102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40(2):218‐227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ingram I, Kelly PJ, Deane FP, et al. Loneliness among people with substance use problems: a narrative systematic review. Drug Alcohol Rev. 2020;39(5):447‐483. [DOI] [PubMed] [Google Scholar]
- 11. Lakey B, Cohen S. Social support theory and measurement. In: Social Support Measurement and Intervention: A Guide for Health and Social Scientists. Oxford, UK: Oxford University Press; 2000:29‐52. [Google Scholar]
- 12. Lakey B, Cronin A. Chapter 17—Low social support and major depression: research, theory and methodological Issues. In: Dobson KS, Dozois DJA, eds. Risk Factors in Depression. San Diego: Elsevier; 2008:385‐408. [Google Scholar]
- 13. Grey I, Arora T, Thomas J, Saneh A, Tohme P, Abi‐Habib R. The role of perceived social support on depression and sleep during the COVID‐19 pandemic. Psychiatry Res. 2020;293:113452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Creese B, Khan Z, Henley W, et al. Loneliness, physical activity, and mental health during COVID‐19: a longitudinal analysis of depression and anxiety in adults over the age of 50 between 2015 and 2020. Int Psychogeriatr. 2020;33:1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jemberie WB, Stewart Williams J, Eriksson M, et al. Substance use disorders and COVID‐19: multi‐faceted problems which require multi‐pronged solutions. Front Psychiatry. 2020;11:714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Volkow ND. Collision of the COVID‐19 and addiction epidemics. Ann Intern Med. 2020;173(1):61‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Seal KH, Cohen G, Waldrop A, Cohen BE, Maguen S, Ren L. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: Implications for screening, diagnosis and treatment. Drug Alcohol Depend. 2011;116(1):93‐101. [DOI] [PubMed] [Google Scholar]
- 18. Seal KH, Metzler TJ, Gima KS, Bertenthal D, Maguen S, Marmar CR. Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs health care, 2002–2008. Am J Public Health. 2009;99(9):1651‐1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Alonzi S, La Torre A, Silverstein MW. The psychological impact of preexisting mental and physical health conditions during the COVID‐19 pandemic. Psychol Trauma Theory Res Pract Policy. 2020;12(S1):S236‐S238. [DOI] [PubMed] [Google Scholar]
- 20. Wilson G, Hill M, Kiernan MD. Loneliness and social isolation of military veterans: systematic narrative review. Occup Med. 2018;68(9):600‐609. [DOI] [PubMed] [Google Scholar]
- 21. Austin G, Calvert T, Fasi N, et al. Soldiering on only goes so far: how a qualitative study on Veteran loneliness in New Zealand influenced that support during COVID‐19 lockdown. J Mil Veteran Fam Health. 2020;6(S2):60‐69. [Google Scholar]
- 22. Teo AR, Marsh HE, Forsberg CW, et al. Loneliness is closely associated with depression outcomes and suicidal ideation among military veterans in primary care. J Affect Disord. 2018;230:42‐49. [DOI] [PubMed] [Google Scholar]
- 23. Fuehrlein BS, Kachadourian LK, DeVylder EK, et al. Trajectories of alcohol consumption in US military veterans: results from the National Health and Resilience in Veterans Study. Am J Addict. 2018;27(5):383‐390. [DOI] [PubMed] [Google Scholar]
- 24. Sciarrino NA, Myers US, Wangelin BC. When chaos is the norm: how some veterans with PTSD are continuing to engage in trauma‐focused treatments during the COVID‐19 pandemic. Psychol Trauma Theory Res Pract Policy. 2020;12(S1):S69‐S70. [DOI] [PubMed] [Google Scholar]
- 25. Substance Abuse and Mental Health Services Administration . 2018 National Survey on Drug Use and Health: Veterans, Rockville, MD; 2020.
- 26. AJMC . A timeline of COVID‐19 developments in 2020. Am J Manag Care. 2020. Accessed December 9, 2020. https://www.ajmc.com/view/a-timeline-of-covid19-developments-in-2020
- 27. Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokdad AH. The PHQ‐8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1‐3):163‐173. [DOI] [PubMed] [Google Scholar]
- 28. Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self‐administration of alcohol. J Consult Clin Psychol. 1985;53:189‐2000. [DOI] [PubMed] [Google Scholar]
- 29. Russell DW. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess. 1996;66(1):20‐40. [DOI] [PubMed] [Google Scholar]
- 30. Sherbourne CD, Stewart A. The MOS Social Support Survey. Santa Monica, CA: RAND Corporation; 1993.
- 31. Rehm J, Kilian C, Ferreira‐Borges C, et al. Alcohol use in times of the COVID 19: implications for monitoring and policy. Drug Alcohol Rev. 2020;39(4):301‐304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bu F, Steptoe A, Fancourt D. Loneliness during a strict lockdown: trajectories and predictors during the COVID‐19 pandemic in 38,217 United Kingdom adults. Soc Sci Med. 2020;265:113521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Simons JS, Wills TA, Emery NN, Marks RM. Quantifying alcohol consumption: self‐report, transdermal assessment, and prediction of dependence symptoms. Addict Behav. 2015;50:205‐212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gray DM, Anyane‐Yeboa A, Balzora S, Issaka RB, May FP. COVID‐19 and the other pandemic: populations made vulnerable by systemic inequity. Nat Rev Gastroenterol Hepatol. 2020;17(9):520‐522. [DOI] [PMC free article] [PubMed] [Google Scholar]


