Dear Editor
The first case of COVID‐19 was identified in December 2019 with progression to the declaration of a worldwide pandemic announced in March 2020 by the World Health Organisation. It has had an impact on medical practice and patient behaviours globally. Australians have been spared the large number of cases seen overseas, with 28 947 cumulative cases as of 26 February 2021 compared with more than 28 million cases in the United States.1 As such the experience of dermatology departments in Australia has differed from those reported in Europe and the United States.2, 3, 4, 5, 6
At St George Hospital Dermatology Department, a tertiary referral centre in Sydney, New South Wales (NSW) Australia, we have prospectively collected data on inpatient and emergency department consultations as part of routine departmental quality assurance. Here, we present the trends of dermatology consults from the period of February to November 2020 compared with these months in 2018. Differences in means were measured by two‐sample T‐test. As expected, there was a 16% reduction in consults in 2020 (n = 265) compared with 2018 (n = 315). The reduction in mean consults per month was by 5 (31.5 in 2018, 26.5 in 2020, t = 1.97, P = 0.06). The largest reduction was in the month of March, correlating with the initial rise of COVID‐19 cases seen in the state of NSW (Fig. 1). The number of referrals from the emergency department was similar in both years (2018, n = 80; 2020, n = 82). The top five reasons for referral in both years are summarised in Table 1. Drug eruption was still the main reason for inpatient dermatology consultation (2018: n = 51, 16.2% and 2020: n = 44, 16.6%). There was a decline in referrals for non‐melanoma skin cancers (NMSC) from 21 (6.7%) in 2018 to 13 (4.9%) in 2020. There was a mean monthly reduction in biopsies by 2.3 (P = 0.04), with an overall 22% reduction in the selected months. Only six inpatients were assessed via teledermatology in April 2020, when the case was deemed suitable (awaiting COVID swab or non‐urgent consult).
Figure 1.
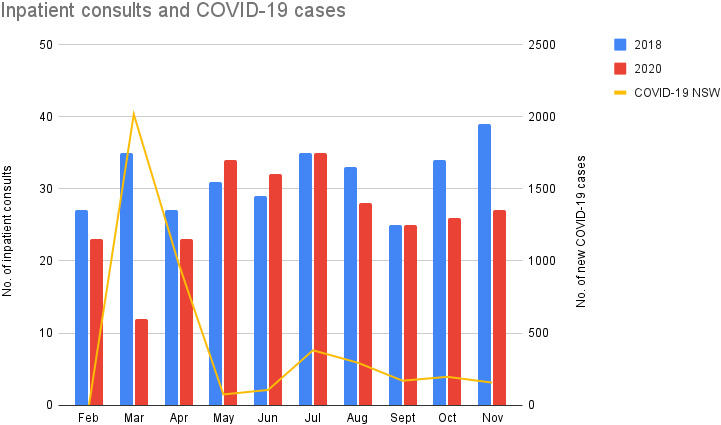
Number of referrals received by St George dermatology department in the years 2018 (blue bar) and 2020 (red bar) for the months of February to November; COVID‐19 cases in New South Wales highlighted in yellow line.
Table 1.
Top five reasons for inpatient dermatology referral in the years 2018 and 2020 (Feb‐Nov)
| 2018 | N (% of total no. of referrals) | 2020 | N (% of total no. of referrals) |
|---|---|---|---|
| 1. Drug Eruption | 51 (16.2) | 1. Drug eruption | 44 (16.6) |
| 2. Non‐melanoma skin cancer | 21 (6.7) | 2. Atopic Dermatitis | 23 (8.7) |
| 3. Atopic Dermatitis | 14 (4.4) | 3. Contact dermatitis | 17 (6.4) |
| 4. Venous stasis dermatitis | 11 (3.5) | 4. Scabies | 15 (5.7) |
| 5. Acute urticaria | 10 (3.2) | 5. Acute urticaria | 14 (5.3) |
Discussion
Several pivotal announcements were made by the NSW government in March, including universal self‐isolation for returned travellers (March 15th), a sequence of restrictions on non‐essential activities and gatherings, and a spike in cases due to the Ruby Princess cruise ship first announced on 20th March. The initial reduction in consults was not sustained, as the expansion of testing eligibility and easing of some restrictions occurred at the end of April. A ‘catch‐up’ phenomenon potentially explains the surge in consults seen in the months of May and June. As case numbers stabilised, the difference in consults between 2018 and 2020 narrowed but remained lower in 2020.
Other countries have experienced more significant COVID‐related impacts on their dermatology services. In Turkey, there has been a reduction in outpatient referrals by 77% from January to May 2020,4 and another centre in southwest Poland experienced a reduction in dermatology admissions by 71.9% between the years of 2019 and 2020.5 In the United States, one centre reported a reduction of 29% in inpatient dermatology consults from March to May 2019 and 2020.6 42% of these consults were done by teledermatology.5 We used teledermatology at the beginning of April for a select few patients in order to minimise in‐person consults due to limitations of personal protective equipment (PPE); however, hospital supplies were subsequently assured and local policies changed. Fortunately, we were able to avoid reliance on teledermatology and its associated limitations that may miss important diagnoses.6
Acute dermatitis featured more in 2020, similar to findings from other countries,5 and as expected subacute referrals reduced (e.g. NMSC). Interestingly, there was a rise in scabies presentations, which was experienced by other local private practices. This is contrary to the expectation that lockdown and social distancing would reduce opportunities for intimate or close contact. Similar observations have been made regarding sexually transmitted diseases, wherein delayed diagnosis can have more serious implications.4, 5, 7 It is thus important to encourage testing for STIs despite COVID‐19. Unlike our international counterparts, we did not experience a sustained significant reduction in consults and have not needed to dramatically change our practice. However, the long‐term consequences of potentially delayed diagnosis of subacute conditions in Australian dermatology practice need to be further evaluated, including trends in private and primary care practices. Our experience also shows that demand for hospital dermatology services continues and departments should learn from the experiences of international counterparts for better preparedness for future pandemics.
Ethical
Ethical committee review was not sought as guided by the 2014 NHMRC Guidelines for Quality Assurance and Evaluation Activities, and this was a clinical audit.
Financial Support
No funding was acquired or utilised for this report.
Conflicts of interest
The authors have no conflicts of interest to declare.
References
- 1.World Health Organisation . WHO Coronavirus Disease (COVID‐19) Dashboard [online]. 2021. [Accessed 27 February 2021]. Available from http://covid19.who.int/ [Google Scholar]
- 2.Uzuncakmak TK, Bayazit S, Askin Oet al. Inpatient dermatology consultations during COVID 19 pandemic in a tertiary referral center. Dermatol. Ther. 2020; 33: e13883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tanacan E, Aksoy Sarac G, Emeksiz MAet al. Changing trends in dermatology practice during COVID‐19 pandemic: A single tertiary center experience. Dermatol. Ther. 2020; 33: e14136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kartal SP, Çelik G, Sendur Net al. Multicenter study evaluating the impact of COVID‐19 outbreak on dermatology outpatients in Turkey. Dermatol. Ther. 2020; 2: e14485. [DOI] [PubMed] [Google Scholar]
- 5.Białynicki‐Birula R, Siemasz I, Otlewska Aet al. Influence of COVID‐19 pandemic on hospitalizations at the tertiary dermatology department in south‐west Poland. Dermatol. Ther. 2020; 33: e13738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rogers MC, Wallace MM, Wheless Let al. Impact of the COVID‐19 pandemic on inpatient dermatology consult patterns at a tertiary care hospital: A retrospective cohort study. J. Am. Acad. Dermatol. 2021; 84: 156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Balestri R, Magnano M, Rizzoli Let al. STIs and the COVID‐19 pandemic: the lockdown does not stop sexual infections. J. Eur. Acad. Dermatol. Venereol. 2020; 34: e766–e768. 10.1111/jdv.16808. [DOI] [PMC free article] [PubMed] [Google Scholar]


