Abstract
Introduction
People with chronic conditions, common among rehabilitation populations, may have risk factors that put them at higher risk for more severe illness due to coronavirus disease 2019 (COVID‐19).
Objective
To describe and compare adherence to public health guidelines, willingness to adhere to public health guidelines (including vaccination), information‐seeking, and perceived trustworthiness of information among people with and without chronic conditions during the early stages of the COVID‐19 pandemic.
Design
National cross‐sectional online survey of people with and without chronic health conditions conducted from April through May 2020.
Participants
Survey respondents were people with and without chronic conditions, ≥18 years old, able to read English, and in the United States since January 2020. In total, 3109 survey responses were received and 2572 complete unique responses were used in the analysis.
Methods
The survey assessed demographics, adherence to public health measures, information‐seeking, and perceived trustworthiness of information sources. Descriptive analyses characterized the sample, and t‐tests and nonparametric tests were used to compare those with and without a chronic condition on the public health measures.
Results
Participants with a chronic condition reported high adherence to public health recommendations and high willingness to adhere to anticipated recommendations across a wide range of chronic conditions and similar to those without a chronic condition despite advised caution for people with underlying health conditions. Of those with a chronic condition, 70.8% reported a willingness to be vaccinated. Participants reported accessing information from varied sources, with perceived trust highest for the health care providers and lowest for social media.
Conclusion
Participants reported high adherence to public health measures, regardless of chronic condition status, during the early phase of the COVID‐19 pandemic. Knowledge of adherence to public health measures, information‐seeking, and trust in information can assist rehabilitation providers and organizations seeking to mitigate disease transmission, particularly for those with chronic conditions.
INTRODUCTION
Preventing the spread of severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection, and its resulting disease, coronavirus disease 2019 (COVID‐19), among at‐risk populations is a key public health concern. The World Health Organization (WHO) declared COVID‐19 a global pandemic on March 11, 2020. 1 Since that time, the number of cases and deaths has grown substantially. Public health organizations around the world have advised special measures to limit the spread of infection.
People with chronic conditions (CCs), including many rehabilitation populations, are more likely to have underlying risk factors that put them at higher risk for more severe illness related to COVID‐19 infection. 2 In the United States, CCs are the leading cause of death and disability; 6 in 10 U.S. adults have a chronic disease. 3 Patients treated by rehabilitation providers, including physiatrists, often have comorbid CCs (eg, diabetes, hypertension, cardiovascular disease) that may place them at greater risk. 4 , 5 , 6
It is important to investigate public health measures to prevent disease transmission, especially for those more vulnerable to hospitalization or death. In addition to vaccines, public health efforts have focused on nonpharmaceutical public health measures. 7 At the time this study was conducted, public health measures advised by the Centers for Disease Control and Prevention (CDC) and WHO included hygiene practices (eg, hand washing), social distancing, and self‐isolation for those exposed to disease. 8 , 9 Individuals at higher risk for experiencing more severe illness from COVID‐19, such as people with CCs, have been strongly advised to adhere to public health measures. 10 , 11 At the time the present study's survey was developed, people who were sick or caring for the sick were advised by the CDC to wear a face mask; however, mask wearing was not recommended by the CDC as a public health measure for the general population. 12
Ultimately, the effectiveness of public health measures depends on the knowledge of and trust in recommendations shared through formal and informal sources. Although information‐seeking has increased in response to COVID‐19, 13 it is not known which sources people with CCs access and trust specifically related to COVID‐19. In general, people in poorer health or with CCs are more likely to seek health information, and those who are middle‐aged (45 to 54 years) are even more likely to seek health information. 14 People with specific health concerns, whether they were diagnosed with a new medical condition, managing an ongoing condition, or helping another deal with health issues, were more likely to seek information online. 15 For people with CCs, the more frequently someone accesses health information on the Internet, the more likely they are to change their health behavior. 16 Gaps between trust and information‐seeking are often identified as key barriers for disseminating health information. People who have experienced health discrimination, including people with CCs and/or disabilities, also often report lower trust ratings in health information sources. 17 Given the strong relationship between health information seeking, trust in health information, and behavior change, better understanding information‐seeking behavior related to COVID‐19 is vital.
Although people living with CCs have been advised to follow public health measures, 11 , 18 it is unknown whether they are adhering to current measures or willing to adhere to anticipated measures, including getting vaccinated. This study aimed to understand how people living with CCs have engaged with public health measures during the initial phase of the COVID‐19 pandemic. Specific aims were to describe the following in people with CCs: (1) rates of adherence to public health measures (hygiene, social distancing); (2) willingness to adhere in the future to anticipated public health measures, including obtaining a COVID‐19 vaccine and wearing face masks; and (3) information‐seeking and perceived trustworthiness of information sources related to COVID‐19. We addressed these aims in a survey of adults with and without self‐identified CCs, conducted early in the COVID‐19 pandemic. Given the novelty of the pandemic and limited previous research on adherence to public health measures for people with chronic or rehabilitation conditions during public health emergencies at the time the survey was conducted, we did not have any a priori hypotheses. Adults without CCs were included to provide context for the results of CC participants. Understanding adherence and information sources may inform future efforts to engage and inform people with CCs, including conditions of relevance to rehabilitation providers, to prevent disease transmission.
METHODS
Sample
The research team developed a cross‐sectional online survey in March and early April 2020 due to the emerging COVID‐19 pandemic. Participants completed the survey online using Research Electronic Data Capture (REDCap), 19 a secure, Health Insurance Portability and Accountablity Act (HIPAA)–compliant, password‐protected web‐based data platform hosted by University of Washington (UW). A human verification service (reCAPTCHA) 20 was enabled to prevent completion by robots or malicious software.
Participants with and without CCs were invited to complete the survey through online research registries (National Institutes of Health [NIH] ResearchMatch), 21 research recruitment websites (Institute of Translational Health Sciences [ITHS] ParticipateinResearch.org), email newsletters by UW, social media (Twitter, Facebook, LinkedIn), and the study team's website. People with CC types identified as higher risk by the CDC at the time were targeted for recruitment via ResearchMatch.
In addition, we purposefully recruited a subsample of people with multiple sclerosis (MS) for a secondary study on psychological distress in that population. Toward this effort, the survey was posted publicly on the National MS Society (NMSS) website and shared via recruitment emails to research registries and a UW listserv of people with MS. Of those included in this survey, 512 (19.9%) reported having MS. Two other studies, with research questions different from the present study, have been published reporting the results for the MS subsample. 22 , 23
Eligible participants self‐reported they were ≥18 years old, able to read English, and in the United States at some point since the first identified COVID‐19 case in the United States: January 20, 2020. 24 Data collection began on April 10, 2020, and ended on May 26, 2020. Participants included all those completing the survey during this time. This study was approved by the UW Human Subjects Division.
Measures
Demographics
Demographic questions assessed age, gender, race, ethnicity, marital status, education level, and geographic location.
Chronic conditions
Participants were given a list of underlying conditions or other risk factors that were defined by the CDC 25 as being associated with more severe illness related to COVID‐19. The total number of CCs per participant was generated by summing all conditions endorsed.
COVID‐19 disease
Participants indicated whether they had any symptoms of COVID‐19 (based on CDC guidance) since the date of the first identified COVID‐19 case in the United States (January 20, 2020), 26 had been tested for COVID‐19, and their test result.
Adherence to public health measures
Participants reported their adherence to public health measures in the past week based on CDC and WHO recommendations at the time. 8 , 9 , 27 Participants indicated how much they changed the way they live their life in response to COVID‐19. 28 They were also asked how much they followed two other public health measures: hygiene (eg, washing your hands; disinfecting commonly used surfaces; avoiding touching your mouth, eyes, and nose; covering your coughs and sneezes; and other similar practices) and social distancing during the past week on a scale of 1 (not at all) to 5 (extremely).
Willingness to adhere to public health measures
We modified previously developed measures designed to assess willingness to adhere to public health measures during influenza pandemics 28 , 29 , 30 to assess whether participants would be willing to adhere in the future to public health measures not yet recommended (eg, wearing face masks, getting vaccinated) or that an individual may not have experienced (eg, COVID‐19 testing or self‐isolation). Participants reported how willing they would be to receive vaccination, isolate from others if needed, wear a face mask, and get tested for COVID‐19 on a scale of 1 (not at all willing) to 5 (extremely willing). To describe the proportion of the sample willing to obtain a COVID‐19 vaccine when available, we categorized the vaccine item's responses as “willing” to receive a vaccine (4 [very willing] or 5 [extremely willing]), “moderately willing” (3), and “not willing” (1 [not at all willing] or 2 [a little willing]).
Sources of information accessed and perceived trustworthiness of information sources
We modified a measure used in prior pandemics 31 to assess how often participants accessed nine sources of information on a scale of 0 (not at all) to 4 (a lot) and perceived trustworthiness of that information on scale of 1 (do not trust at all) to 4 (totally trust). Participants also indicated how much they trusted various government officials/agencies (local elected officials such as mayor, county commissioner; state government officials such as governor, state or local public health officials, CDC, U.S. Secretary of Health and Human Services, U.S. Secretary of Homeland Security, U.S. President Donald Trump).
Analysis
Data analyses were conducted for both respondents with and without CCs. The focus of this study was on CCs; results from those without CCs provide context for the findings about people with CCs. Prior to conducting study analyses, data were examined to attend to outliers and missing data. Incomplete responses (participants who discontinued the survey prior to indicating their CC status) were removed; sample sizes for each variable described are included in related tables. Most participants (>90%) had five or fewer items missing, a few participants (<1%) were retained with 10+ items missing. All responses were verified for validity by cross‐checking identifiable information. Where duplicate responses were identified, the first response was retained. Completion time was reviewed to identify surveys in which participants completed the questionnaire faster than a human could read; none were identified.
Any participant who endorsed at least one CC was included in the CC category. Descriptive statistics were performed to characterize the sample and to describe current adherence, willingness to adhere to future measures, information sources accessed, and perceived trustworthiness of information sources and government officials/agencies. Independent group t‐tests (for continuous variables) and chi‐square analysis (for categorical variables) were used to compare those with and without a CC on the public health adherence measures (current adherence and future willingness) and the demographics, with a Bonferroni adjusted alpha level of .003 per test (.05/17). We were primarily interested in whether those with and without a CC differed in terms of demographics and adherence to public health measures. We did not conduct statistical comparisons between the two groups for the COVID‐19 information sources and trustworthiness items; inspection of the means for these items suggests that any differences, even if statistically significant, would not be clinically meaningful.
RESULTS
Participants
In total, 3109 survey responses were received. Of those responses, 153 (4.9%) discontinued at the information statement, 19 (0.6%) were duplicates, and 32 (1.0%) were ineligible (3 [0.1%] <18 years old, 29 [0.9%] not in United States). Of the 2727 (87.2%) eligible unique responses, 155 (5.0%) were excluded because they were incomplete. In all, 2572 (82.7%) of all surveys were complete and used for analysis. Overall, 1180 participants (45.9%) were recruited from NIH ResearchMatch.org, 437 (17.0%) from email newsletters, 264 (10.3%) from ITHS ParticipateinResearch.org, 262 (10.2%) from university research participant pools, 181 (7.0%) from social media, 49 (1.9%) from the NMSS, 162 (6.3%) from other sources, and 37 (1.4%) did not indicate a source.
Overall, 55.4% of participants reported having one of more 1 CC (range = 0–8). Table 1 summarizes types of CC in detail. Participants with one or more CCs were predominantly female, White, and an average of 56.5 years old (SD = 15.34 years.). Approximately half of the CC sample was married or lived with a partner (51.8%), under one‐third were employed full time (30.6%), and almost all had education beyond high school (95.5%). Participants with CCs included residents of all 50 states and the District of Columbia (DC), with 330 (23.1%) participants from Washington state, 114 (8.0%) from Ohio, 87 (6.1%) from California, 78 (5.5%) from New York, and the other 48 states and DC contributing less than 5.0% of the sample each. In total, 337 (23.8%) of participants with CCs reported experiencing symptoms associated with COVID‐19 not related to an underlying condition, 97 (6.8%) had been tested for COVID‐19, and only 5 (0.4%) had tested positive for COVID‐19. Relative to participants without CCs, those with CCs were significantly more likely to be older and married; more people without CCs were employed full‐time and had received graduate/professional education. Table 2 describes detailed demographic data for the subsample with CCs as well as the sample as a whole and those without CCs.
TABLE 1.
Chronic conditions by type
| Chronic condition/risk factor type a | Description b | N (%) |
|---|---|---|
| Neurological disorders | Disorders of the brain, spinal cord, peripheral nerve, and muscle such as cerebral palsy, epilepsy (seizure disorders), stroke, intellectual disability, moderate to severe developmental delay, muscular dystrophy, or spinal cord injury | 609 (23.7%) |
| Lung disease | Asthma or chronic obstructive pulmonary disease (eg, chronic bronchitis or emphysema, or other chronic conditions associated with impaired lung function or that require home oxygen) | 433 (16.8%) |
| Endocrine disorders | For instance, diabetes mellitus | 417 (16.2%) |
| Compromised immune system/immunosuppression | Seeing a doctor for cancer and treatment such as chemotherapy or radiation, receiving an organ or bone marrow transplant, taking high doses of corticosteroids or other immunosuppressant medications, HIV or AIDS | 403 (15.7%) |
| Heart disease | Congenital heart disease, congestive heart failure, or coronary artery disease | 234 (9.1%) |
| Blood disorders | Sickle cell disease or on blood thinners | 211 (8.2%) |
| Chronic kidney disease | Patients who have been told to avoid or reduce the dose of medications due to kidney disease, or who are under treatment for kidney disease, including receiving dialysis | 81 (3.1%) |
| Metabolic disorders | Inherited metabolic disorders and mitochondrial disorders | 55 (2.1%) |
| Chronic liver disease | Cirrhosis, chronic hepatitis, or patients who have been told to avoid or reduce the dose of medications because of liver disease or are under treatment for liver disease | 39 (1.5%) |
Participants may endorse more than one one chronic condition. Due to this, the total number of conditions endorsed is greater than the sample size and the percentage does not equal 100%.
Descriptions of chronic conditions are based on CDC descriptions. 18
TABLE 2.
Participant characteristics, including comparisons between those with and without chronic conditions
| Demographic variable | Entire sample (n = 2572) | No chronic conditions (n = 1146) | One or more chronic conditions (n = 1426) | p a |
|---|---|---|---|---|
| Mean (SD) or N (%) | Mean (SD) or N (%) | Mean (SD) or N (%) | ||
| Age (y) | 53.7 (16.8), range 18–90 | 50.3 (17.8), range 18–89 | 56.5 (15.3), range 18–90 | <.001 * 95% CI [−7.44, −4.86] |
| 18–29 | 299 (11.6%) | 202 (17.6%) | 97 (6.8%) | |
| 30–39 | 353 (13.7%) | 197 (17.2%) | 156 (10.9%) | |
| 40–49 | 330 (12.8%) | 143 (12.5%) | 187 (13.1%) | |
| 50–59 | 468 (18.2%) | 183 (16.0%) | 285 (20.0%) | |
| 60–69 | 629 (24.5%) | 229 (20.0%) | 400 (28.1%) | |
| 70–79 | 399 (15.5%) | 154 (13.4%) | 245 (17.2%) | |
| 80+ | 65 (2.5%) | 27 (2.4%) | 38 (2.7%) | |
| No response | 29 (1.1%) | 11 (1.0%) | 18 (1.3%) | |
| Gender | .273 | |||
| Woman | 1919 (74.6%) | 876 (76.4%) | 1043 (73.1%) | |
| Man | 596 (23.2%) | 246 (21.5%) | 350 (24.5%) | |
| Non–binary | 27 (1.0%) | 13 (1.1%) | 14 (1.0%) | |
| Transgender man | 6 (0.2%) | 2 (0.2%) | 4 (0.3%) | |
| Transgender woman | 3 (0.1%) | 0 (0.0%) | 3 (0.2%) | |
| Other/prefer not to say/no response | 21 (0.8%) | 9 (0.8%) | 12 (0.9%) | |
| Race | .247 | |||
| White | 2246 (87.3%) | 983 (85.8%) | 1263 (88.6%) | |
| More than one race | 107 (4.2%) | 50 (4.4%) | 57 (4.0%) | |
| Black or African American | 69 (2.7%) | 24 (2.1%) | 45 (3.2%) | |
| Asian | 65 (2.5%) | 48 (4.2%) | 17 (1.2%) | |
| Other | 38 (1.5%) | 19 (1.7%) | 19 (1.3%) | |
| Prefer not to say | 33 (1.3%) | 16 (1.4%) | 17 (1.2%) | |
| American Indian/Alaskan Native | 10 (0.4%) | 3 (0.3%) | 7 (0.5%) | |
| No response | 4 (0.2%) | 3 (0.3%) | 1 (0.1%) | |
| Ethnicity | .265 | |||
| Not Hispanic or Latino | 2372 (92.2%) | 1059 (92.4%) | 1313 (92.1%) | |
| Hispanic or Latino | 90 (3.5%) | 49 (4.3%) | 41 (2.9%) | |
| No response | 59 (2.3%) | 14 (1.2%) | 45 (3.2%) | |
| Prefer not to say | 38 (1.5%) | 19 (1.7%) | 19 (1.3%) | |
| Unknown | 13 (0.5%) | 5 (0.4%) | 8 (0.6%) | |
| Employment | <.001* | |||
| Employed full‐time | 965 (37.5%) | 529 (46.2%) | 436 (30.6%) | |
| Retired | 790 (30.7%) | 285 (24.9%) | 505 (35.4%) | |
| Unable to work | 250 (9.7%) | 36 (3.1%) | 214 (15.0%) | |
| Employed part‐time | 217 (8.4%) | 107 (9.3%) | 110 (7.7%) | |
| Unemployed due to COVID‐19 | 143 (5.6%) | 71 (6.2%) | 72 (5.0%) | |
| Unemployed unrelated to COVID‐19 | 100 (3.9%) | 50 (4.4%) | 50 (3.5%) | |
| Student | 99 (3.8%) | 66 (5.8%) | 33 (2.3%) | |
| No response | 8 (0.3%) | 2 (0.2%) | 6 (0.4%) | |
| Education | <.001 * | |||
| Ninth grade or less | 2 (0.1%) | 0 (0.0%) | 2 (0.1%) | |
| 10th–12 grade | 8 (0.3%) | 2 (0.2%) | 6 (0.4%) | |
| High school graduate or GED | 78 (3.0%) | 28 (2.4%) | 50 (3.5%) | |
| Vocational or Technical School | 98 (3.8%) | 36 (3.1%) | 62 (4.3%) | |
| Some college | 437 (17.0%) | 162 (14.1%) | 275 (19.3%) | |
| College graduate | 905 (35.2%) | 387 (33.8%) | 518 (36.3%) | |
| Graduate or professional school | 1035 (40.2%) | 527 (46.0%) | 508 (35.6%) | |
| No response | 9 (0.3%) | 4 (0.3%) | 5 (0.4%) | |
| Marital status | <.001 * | |||
| Married | 1271 (49.4%) | 532 (46.4%) | 739 (51.8%) | |
| Never Married | 581 (22.6%) | 320 (27.9%) | 261 (18.3%) | |
| Divorced | 412 (16.0%) | 172 (15.0%) | 240 (16.8%) | |
| Domestic partner | 134 (5.2%) | 63 (5.5%) | 71 (5.0%) | |
| Widowed | 126 (4.9%) | 42 (3.7%) | 84 (5.9%) | |
| Legally Separated | 31 (1.2%) | 11 (1.0%) | 20 (1.4%) | |
| Annulled | 8 (0.3%) | 4 (0.3%) | 4 (0.3%) | |
| No response | 9 (0.3%) | 2 (0.2%) | 7 (0.5%) | |
| COVID‐19 symptoms | .069 | |||
| Yes | 645 (25.1%) | 308 (26.9%) | 337 (23.8%) | |
| No | 1918 (74.6%) | 837 (73.1%) | 1081 (76.2%) | |
| No response | 9 (0.3%) | 1 (0.1%) | 8 (0.6%) | |
| COVID‐19 test | .247 | |||
| I have been tested. | 153 (5.9%) | 56 (4.9%) | 97 (6.8%) | |
| I have not tried to get tested. | 2113 (82.2%) | 946 (82.5%) | 1167 (81.8%) | |
| I tried to get tested and was unable to. | 108 (4.2%) | 45 (3.9%) | 63 (4.4%) | |
| I have an appointment to get tested. | 25 (1.0%) | 11 (1.0%) | 14 (1.0%) | |
| No response | 173 (6.7%) | 88 (7.7%) | 85 (6.0%) | |
| COVID‐19 test result | .673 | |||
| Positive for COVID‐19 | 9 (0.3%) | 4 (0.3%) | 5 (0.4%) | |
| Negative for COVID‐19 | 139 (5.4%) | 51 (4.5%) | 88 (6.2%) | |
| Waiting on result | 24 (0.9%) | 7 (0.6%) | 17 (1.2%) | |
| No response | 6 (0.2%) | 5 (0.4%) | 1 (0.0%) | |
| Not applicable | 2394 (93.1%) | 1079 (94.1%) | 1315 (92.2%) |
Value significant at p < .01.
t‐tests were conducted for continuous variables and chi‐squared tests were conducted for categorical variables. p Values pertain to comparisons between those with none or one or more chronic conditions.
Adherence to public health measures
People with CCs reported high adherence to recommendations regarding hygiene and social distancing in the week before completing the survey (Table 3). Participants with and without CCs reported that they had changed their lives moderately due to COVID‐19. Reported adherence to public health guidelines was high and comparable for those with and without CCs.
TABLE 3.
Adherence to public health measures in the past week a,c
| Behavior | Entire sample | No chronic conditions | One or more chronic conditions | t b | p | 95% CI |
|---|---|---|---|---|---|---|
| How much have you changed the way you live your life (n = 2474) | 3.8 (1.0) | 3.8 (0.9) | 3.8 (1.0) | 1.05 | .293 | [−.035, .117] |
| Followed hygiene recommendations (n = 2511) | 4.1 (0.8) | 4.0 (0.8) | 4.1 (0.8) | −1.38 | .167 | [−.112, .019] |
| Practiced social distancing (n = 2515) | 4.4 (0.7) | 4.4 (0.7) | 4.4 (0.7) | −1.19 | .235 | [−.091, .022] |
Data are mean (SD) for the adherence to public health measures items, possible responses ranged from 1 (not at all) to 5 (extremely).
t‐tests were conducted between those with none or one or more chronic conditions.
Data were collected prior to widespread mask mandates and recommendations.
Willingness to adhere to public health measures
Participants with CCs reported they were very willing to adhere to potential future public health measures, including receiving a COVID‐19 vaccination, isolating from others, wearing a face mask, and getting tested for COVID‐19, with mean scores for those with CCs ranging from 4.0 (SD = 1.2) to 4.6 (SD = 0.8; 1–5 scale; see Figure 1). Although overall willingness to receive a vaccination was high for people with CCs, people were less willing to obtain a vaccination, when available, than other public health measures. Nearly 6.2% of those with CCs said that they were not at all willing, and 8.2% said they were only a little willing to obtain a vaccination when available; 14.8% were moderately willing and 70.8% were willing to obtain a vaccination. Furthermore, participants with at least one CC were significantly more likely to report a willingness to obtain the vaccine when available (4.15 ± 1.09) as compared to those without a CC (3.95 ± 1.22), t (2542) = 4.21, p = <.001, d = 1.162, 95% CI [0.104, 0.286]. The two groups did not differ statistically in their willingness to adhere to the other hypothetical public health measures, specifically wearing a mask (p = .161), getting tested for COVID‐19 (p = .570), and isolating from others (p = .227).
FIGURE 1.
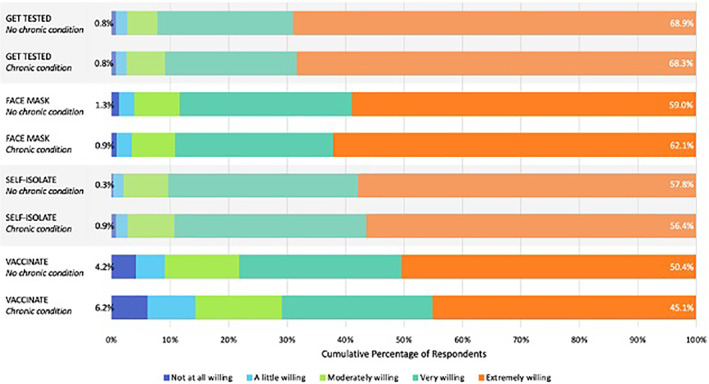
Willingness to adhere to public health measures for those with no chronic conditions versus those with one or more chronic conditions†. †For the willingness to adhere to public health measures items, possible responses ranged from 1 (not at all willing) to 5 (extremely willing). Missing responses were removed prior to calculating percentage; percentages were calculated based on completed responses only. Missing responses accounted for less than 1% of all responses. Sample size for participants without chronic conditions ranged from 1133 to 1138 and for participants with one or more chronic conditions ranged from 1410 to 1415
Sources of information accessed and perceived trustworthiness of information sources
Participants with CCs reported accessing information from many different sources, most often by reading news on a news website or in print and least often from local radio stations. Information from family and friends, social media, TV news, and government or other Internet websites was all accessed at similar rates with little variation based on whether the participant had a CC. Participants with CCs were only slightly more likely than those without CCs to access information from health care providers (Table 4).
TABLE 4.
Information sources accessed a
| Information source | Entire sample | No chronic conditions | One or more chronic conditions |
|---|---|---|---|
| Watching TV news (n = 2550) | 2.7 (1.2) | 2.5 (1.2) | 2.8 (1.2) |
| Reading news on a news website or in print (n = 2547) | 3.2 (0.9) | 3.3 (0.9) | 3.2 (0.9) |
| Government website (n = 2533) | 2.3 (1.0) | 2.3 (1.0) | 2.3 (1.0) |
| Social media (n = 2518) | 2.3 (1.8) | 2.4 (1.1) | 2.3 (1.1) |
| Other Internet website (n = 2485) | 2.3 (1.0) | 2.3 (1.0) | 2.3 (1.0) |
| National Public Radio (n = 2520) | 2.0 (1.1) | 2.1 (1.1) | 1.9 (1.1) |
| Local radio stations (n = 2492) | 1.6 (0.9) | 1.6 (0.9) | 1.6 (0.9) |
| Health care provider (n = 2506) | 1.8 (1.0) | 1.7 (0.9) | 1.9 (1.0) |
| Family and friends (n = 2518) | 2.4 (0.9) | 2.4 (0.9) | 2.4 (0.9) |
Data are mean (SD) for the information sources accessed items, possible responses ranged from 1 (not at all) to 4 (a lot).
Participants with CCs reported the lowest rate of perceived trustworthiness in social media, followed by other Internet websites. Of note, perceived trustworthiness of information from family and friends was similar to that of watching TV news. Health care providers had the highest perceived trustworthiness with similar perceptions of trustworthiness among people with and without CCs (Table 5).
TABLE 5.
Perceived trustworthiness of information sources a
| Information source | Entire sample | No chronic conditions | One or more chronic conditions |
|---|---|---|---|
| Watching TV news (n = 2402) | 2.2 (0.7) | 2.2 (0.7) | 2.3 (0.8) |
| Reading news on a news website or in print (n = 2475) | 2.4 (0.7) | 2.5 (0.7) | 2.4 (0.7) |
| Government website (n = 2400) | 2.6 (0.8) | 2.7 (0.8) | 2.5 (0.8) |
| Social media (n = 2419) | 1.5 (0.6) | 1.5 (0.6) | 1.5 (0.6) |
| Other Internet website (n = 2197) | 1.9 (0.7) | 1.9 (0.7) | 1.9 (0.7) |
| National Public Radio (n = 2069) | 2.7 (1.0) | 2.8 (0.9) | 2.6 (1.0) |
| Local radio stations (n = 1924) | 2.0 (0.7) | 2.1 (0.7) | 2.0 (0.7) |
| Health care provider (n = 2219) | 3.3 (0.7) | 3.3 (0.7) | 3.3 (0.7) |
| Family and friends (n = 2382) | 2.3 (0.7) | 2.2 (0.7) | 2.3 (0.7) |
Data are mean (SD) for the perceived trustworthiness of information sources items, possible responses ranged from 1 (do not trust at all) to 4 (totally trust). Participants were able to respond N/A to trustworthiness of information sources items. N/A responses were set to missing to calculate descriptive statistics.
Participants with CCs reported high rates of perceived trustworthiness in state government officials (mean = 2.50, SD = 0.89) and state or local public health officials (mean = 2.74, SD = 0.77), with the highest rate of perceived trustworthiness in the CDC (mean = 2.90, SD = 0.79) and the lowest level of perceived trust in U.S. President Donald Trump (mean = 1.42, SD = 0.81). Participants reported similar rates of perceived trustworthiness in sources of information and government officials/agencies regardless of CC/risk factor type, number of CCs, or presence of a CC.
DISCUSSION
People with CCs are at greater risk for adverse outcomes due to COVID‐19. Given the higher prevalence of CCs among people cared for in rehabilitation settings, as well as the various sources making recommendations or sharing information about COVID‐19, it is crucial to understand how people living with CCs have engaged with public health measures during the COVID‐19 pandemic. In this study conducted early in the pandemic, people with CCs reported that they had significantly changed their behavior as a result of public health recommendations. They reported high levels of adherence to public health measures and of willingness to adhere to a variety of potential future public health measures, including wearing masks, as did those without CCs. For those with CCs, participants reported lower rates of willingness to obtain a COVID‐19 vaccination once available compared to other behaviors; however, willingness to obtain vaccination for those with CCs was higher than those without CCs. We also found that participants with CCs obtained information about SARS‐CoV‐2 and COVID‐19 from many sources, and many of the most frequently accessed sources were not those that they rated as most trustworthy.
Participants with CCs reported high rates of adherence to public health measures, including social distancing. Similar to one other recent study in the general population, 32 participants with CCs expressed a high degree of future willingness to wear a face mask, to self‐isolate, and to get a COVID‐19 test if indicated. High reported adherence could be related to the timing of the survey, conducted early in the pandemic when almost all states had stay‐at‐home orders and novelty of the virus and uncertainty regarding its effects contributed to high willingness to adhere. 10 Whether adherence will be maintained over time is not known and an important area for future research, as people may become habituated to risk over time, as has been found in past pandemics and as initial evidence suggests. 33 Future research to better identify those unwilling or unable to adhere and the related rationale can help inform public health and clinical interventions addressing barriers to adherence.
Relative to other public health measures, participants were least willing to obtain a future vaccination, regardless of whether they had a CC. Of those with a CC, 14.4% were unwilling, 14.8% were moderately willing, and 70.8% were willing to vaccinate. A few studies in other populations without a CC have examined COVID‐19 vaccine acceptability and found similar rates of vaccine willingness. 34 , 35 Given that vaccination will be a key strategy to prevent COVID‐19, these findings have concerning implications for people with CCs. These findings as well as those from other recent studies on vaccine hesitancy in the general population suggest that rehabilitation providers should not assume that their patients are willing to receive the COVID‐19 vaccine just because of their health status. 35 , 36 , 37 Health care providers, including rehabilitation providers, and public health organizations will need to provide education on vaccine safety and efficacy specific to the benefits and risks for people with CCs to reduce morbidity and mortality, particularly as other studies have found willingness to vaccinate has further decreased over time. 36
Participants with CCs reported accessing information from a wide range of sources, with varying degrees of trust. Participants most commonly reported obtaining information from news websites or print (eg, newspapers), although they rated them as only moderately trustworthy. Respondents with CCs frequently obtained information from not only the typical sources such as TV news, social media, and websites (all rated as only moderately trustworthy, on average), but also from family and friends. Reliance on family and friends as a major information source suggests the potential for social contacts as a means to disseminate information about COVID‐19 with important implications for public health organizations. Reliance on social media as an information source is noteworthy due to the varying quality of information available through social media, emphasizing that public health organizations must not only disseminate accurate information but also combat and correct misinformation. 38
The gap between trust and accessing information is a major barrier to individual health behavior change. Although participants reported rarely accessing information from health care providers, they also described health care providers as one of the most trustworthy sources of information. Given that many individuals with CCs are followed by rehabilitation providers, it would be valuable for rehabilitation providers to offer relevant information about COVID‐19 to their patients, such as information about adherence to public health recommendations based on CDC guidance and the latest information about the state of the pandemic. This will be particularly important given potential risks and benefits associated with vaccination against COVID‐19 for people with CCs who may have special considerations based on health status. Health care providers and public health organizations must identify information sources that are highly trusted and partner with these sources to share evidence‐based information, particularly for people and communities at greater risk for severe outcomes from COVID‐19. 39 Limited accessing of information from providers, despite high trust, underscores the importance of providing trusted information through other means, including government sources, public health agencies, and other organizations, including condition‐specific organizations (eg, Amputee Coalition, National MS Society, and American Diabetes Association). Although government websites were accessed at rates similar to those of other sources, perceived trustworthiness of government information varied widely by source, with the CDC as the most trusted and the U.S. President Donald Trump as the least trusted. During the 2009 H1N1 pandemic, the CDC was also the most trusted government source; however, perceived trustworthiness of President Barack Obama was similar to that of other government sources. 31
Future research in this field could benefit greatly from use of a model of human behavior change and health promotion in order to better understand individual adherence to public health guidelines. 40 Use of an ecological systems model, 41 , 42 in which broader governmental and organizational factors are related to interpersonal influences and individual decisions, could be a valuable tool to understand and implement public health efforts to encourage adherence. The health belief model, 43 which examines individuals' health beliefs, perceived benefits of and barriers to health behaviors, and self‐efficacy for engaging in health‐promoting behaviors, is another empirically supported model for health behavior change that could be applied in future research on adherence to public health measures during pandemics by people with CCs.
Several limitations should be noted. Foremost, findings are based upon self‐reported behaviors and may be affected by social desirability bias, leading to the under‐reporting of undesirable behavior. However, a study during the COVID‐19 pandemic found the effect of social desirability bias on self‐reported social distancing to be less prevalent than expected. 44 As the survey was cross‐sectional early in the pandemic, it is likely that behaviors, such as mask wearing, have changed over time. Similarly, as scientists learn more about COVID‐19 and vaccines become more readily available, increased knowledge regarding risk factors may change risk perception and adherence. In the future, studies may better elucidate factors affecting adherence based on relevant health behavior theory. Although we obtained a large sample from multiple and diverse sources, the sample was not randomly selected and may not be representative. We purposefully sampled people with CCs, including oversampling people with MS. More highly educated people were disproportionately represented in this sample, which should be kept in mind while considering this study's results. Finally, findings are based on categorizing participants as having CCs or not; there is considerable variability within CCs in terms of disease severity.
CONCLUSION
As the COVID‐19 pandemic continues, it is clear that ongoing adherence to public health measures will be paramount to mitigate disease transmission and people with CCs will continue to be at increased risk. Given recommendations to account for health status when making decisions about illness prevention, 2 it is not surprising this study found that those with CCs reported high levels of adherence particularly, since the survey occurred during the beginning of the pandemic when stay‐at‐home orders were in effect and vigilance was high. Understanding peoples' behaviors related to public health recommendations can help health care providers, governments, and other organizations encourage adherence, particularly for those at greater risk, as public health recommendations to curb the spread of infection evolve. Although high rates of adherence have been reported, longitudinal research is needed to understand changes over time. As current knowledge evolves, it is critical that people are able to access and trust information about the pandemic and the nature of the scientific process. Although people highly trust information from their health care providers, they more often access information from news and government sources, or even from their family and friends. Maintaining high trust in government sources and utilizing both frequently accessed and highly trusted sources, such as providers, to share reputable information will ultimately aid adherence to public health measures and thereby mitigate disease transmission.
ACKNOWLEDGMENTS
This study was partially supported by the Nancy and Buster Alvord Endowed Professorship in Multiple Sclerosis Research held by Dawn M. Ehde, PhD. We have no conflicts of interest to report. Study data were collected and managed using REDCap electronic data capture tools hosted at the Institute of Translational Health Sciences (ITHS), which is supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH) under Award Number UL1 TR002319. This same award also provides the research recruitment website, ParticipateinResearch.org, which was one of the sources for participants in this study. Recruitment for the study included ResearchMatch. ResearchMatch is funded in part by the National Institutes of Health Clinical and Translational Science Award (CTSA) program and is funded by grants UL1TR000445, U24TR00157 9, and 5 U24 TR001579‐02. The CTSA program is led by the NIH's National Center for Advancing Translational Sciences (NCATS). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of NIH.
Roberts MK, Ehde DM, Herring TE, Alschuler KN. Public health adherence and information‐seeking for people with chronic conditions during the early phase of the COVID‐19 pandemic. PM&R. 2021;13(11):1249‐1260. 10.1002/pmrj.12668
Funding information Nancy and Buster Alvord Endowment; National Institutes of Health (NIH) Clinical and Translational Science Award (CTSA) program, Grant/Award Numbers: 5 U24 TR001579‐02, U24TR00157 9, UL1TR000445; National Center for Advancing Translational Sciences of the National Institutes of Health, Grant/Award Number: UL1 TR002319
Contributor Information
Michelle K. Roberts, Email: mkrob@uw.edu.
Dawn M. Ehde, Email: ehde@uw.edu.
Tracy E. Herring, Email: teh7@uw.edu.
Kevin N. Alschuler, Email: kalschul@uw.edu.
REFERENCES
- 1. Ghebreyesus TA. WHO Director General's opening remarks at the media briefing on COVID‐19 [Transcript]. 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020. Accessed November 10, 2020.
- 2. National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases . People with certain medical conditions. Centers for Disease Control and Prevention. 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed November 10, 2020.
- 3. National Center for Chronic Disease Prevention and Health Promotion . About chronic diseases. Centers for Disease Control and Prevention. 2019. https://www.cdc.gov/chronicdisease/about/index.htm. Accessed November 10, 2020.
- 4. DiPiro ND, Murday D, Corley EH, Krause JS. Prevalence of chronic health conditions and hospital utilization in adults with spinal cord injury: an analysis of self‐report and South Carolina administrative billing data. Spinal Cord. 2019;57(1):33‐40. 10.1038/s41393-018-0185-9 [DOI] [PubMed] [Google Scholar]
- 5. Hammond FM, Corrigan JD, Ketchum JM, et al. Prevalence of medical and psychiatric comorbidities following traumatic brain injury. J Head Trauma Rehabil. 2019;34(4):E1‐E10. 10.1097/HTR.0000000000000465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jiang X, Wang L, Morgenstern LB, Cigolle CT, Claflin ES, Lisabeth LD. A new index for multiple chronic conditions predicts functional outcome in ischemic stroke. Neurology. 2020;96(1):e42‐e53. 10.1212/WNL.0000000000010992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hartley DM, Perencevich EN. Public health interventions for COVID‐19: emerging evidence and implications for an evolving public health crisis. JAMA. 2020;323(19):1908. 10.1001/jama.2020.5910 [DOI] [PubMed] [Google Scholar]
- 8. National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases . How to protect yourself & others. Centers for Disease Control and Prevention. 2019. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fprepare%2Fprevention.html. Accessed November 10, 2020.
- 9. World Health Organization . Coronavirus disease (COVID‐19) advice for the public. 2019. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public. Accessed November 10, 2020.
- 10. Moreland A, Herlihy C, Tynan MA, et al. Timing of state and territorial COVID‐19 stay‐at‐home orders and changes in population movement — United States, march 1–may 31, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(35):1198‐1203. 10.15585/mmwr.mm6935a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases . People at increased risk. Centers for Disease Control and Prevention. 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/index.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fneed-extra-precautions%2Fpeople-at-increased-risk.html. Accessed November 10, 2020.
- 12. Centers for Disease Control and Prevention . Recommendation regarding the use of cloth face coverings, especially in areas of significant community‐based transmission. 2020. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover.html. Accessed May 5, 2020.
- 13. Bento AI, Nguyen T, Wing C, Lozano‐Rojas F, Ahn Y‐Y, Simon K. Evidence from internet search data shows information‐seeking responses to news of local COVID‐19 cases. Proc Natl Acad Sci U S A. 2020;117(21):11220‐11222. 10.1073/pnas.2005335117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rooks RN, Kapral CG, Mathis AL. Chronic conditions may be more important than race or ethnicity in relation to health information seeking and use. J Aging Health. 2019;31(4):611‐630. 10.1177/0898264317744643 [DOI] [PubMed] [Google Scholar]
- 15. Rice RE. Influences, usage, and outcomes of internet health information searching: multivariate results from the pew surveys. Int J Med Inform. 2006;75(1):8‐28. 10.1016/j.ijmedinf.2005.07.032 [DOI] [PubMed] [Google Scholar]
- 16. Ayers SL, Kronenfeld JJ. Chronic illness and health‐seeking information on the internet. Health (London). 2007;11(3):327‐347. 10.1177/1363459307077547 [DOI] [PubMed] [Google Scholar]
- 17. Ipsen C, Myers A, Sage R. A cross‐sectional analysis of trust of information and COVID‐19 preventative practices among people with disabilities. Disabil Health J. 2021;14(2):101062. 10.1016/j.dhjo.2021.101062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mayo Clinic . COVID‐19: who's at higher risk of serious symptoms? 2020. https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/coronavirus-who-is-at-risk/art-20483301. Accessed November 10, 2020.
- 19. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377‐381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Google reCAPTCHA . reCAPTCHA. https://www.google.com/recaptcha/about/. Accessed September 18, 2020.
- 21. ResearchMatch . ResearchMatch.org. https://www.researchmatch.org. Accessed September 18, 2020.
- 22. Alschuler KN, Roberts MK, Herring TE, Ehde DM. Distress and risk perception in people living with multiple sclerosis during the early phase of the COVID‐19 pandemic. Mult Scler Relat Disord. 2020;47(102618). 10.1016/j.msard.2020.102618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ehde DM, Roberts MK, Herring TE, Alschuler KN. Willingness to obtain COVID‐19 vaccination in adults with multiple sclerosis in the United States. Mult Scler Relat Disord. 2021;49(102788). 10.1016/j.msard.2021.102788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Harcourt J, Tamin A, Lu X, et al. Severe acute respiratory syndrome coronavirus 2 from patient with coronavirus disease, United States. Emerg Infect Dis. 2020;26(6):1266‐1273. 10.3201/eid2606.200516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases . Seattle‐King, Pierce and Snohomish, Washington community mitigation. Centers for Disease Control and Prevention. 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/washington-seattle.html. Accessed March 19, 2020.
- 26. National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases . Symptoms of Coronavirus. Centers for Disease Control and Prevention. 2020. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html. Accessed March 19, 2020.
- 27. Michie, S. , Rubin, J. , Amlôt, R. Behavioural science must be at the heart of the public health response to covid‐19. BMJ Opinion. 2020. https://blogs.bmj.com/bmj/2020/02/28/behavioural-science-must-be-at-the-heart-of-the-public-health-response-to-covid-19/. Accessed March 19, 2020. [Google Scholar]
- 28. Barr M, Raphael B, Taylor M, et al. Pandemic influenza in Australia: using telephone surveys to measure perceptions of threat and willingness to comply. BMC Infect Dis. 2008;8(1). 10.1186/1471-2334-8-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Maguire PA, Reay RE, Looi JC. A sense of dread: affect and risk perception in people with schizophrenia during an influenza pandemic. Australas Psychiatry. 2019;27(5):450‐455. 10.1177/1039856219839467 [DOI] [PubMed] [Google Scholar]
- 30. Taylor M, Raphael B, Barr M, Agho K, Stevens G, Jorm L. Public health measures during an anticipated influenza pandemic: factors influencing willingness to comply. Risk Manag Healthc Policy. 2009;2:9‐20. 10.2147/RMHP.S4810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Quinn SC, Parmer J, Freimuth VS, Hilyard KM, Musa D, Kim KH. Exploring communication, Trust in Government, and vaccination intention later in the 2009 H1N1 pandemic: results of a National Survey. Biosecur Bioterror. 2013;11(2):96‐106. 10.1089/bsp.2012.0048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Park CL, Russell BS, Fendrich M, Finkelstein‐Fox L, Hutchison M, Becker J. Americans' COVID‐19 stress, coping, and adherence to CDC guidelines. J Gen Intern Med. 2020;35:2296‐2303. 10.1007/s11606-020-05898-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Johnson BB, Mayorga M. Temporal shifts in Americans' risk perceptions of the Zika outbreak. Hum Ecol Risk Assess Int J. 2020;27(5):1242‐1257. 10.1080/10807039.2020.1820852 [DOI] [Google Scholar]
- 34. Dror AA, Eisenbach N, Taiber S, et al. Vaccine hesitancy: the next challenge in the fight against COVID‐19. Eur J Epidemiol. 2020;35:775‐779. 10.1007/s10654-020-00671-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Reiter PL, Pennell ML, Katz ML. Acceptability of a COVID‐19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine. 2020;38(42):6500‐6507. 10.1016/j.vaccine.2020.08.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tyson A, Johnson C, Funk C. U.S. public now divided over whether to get COVID‐19 vaccine. Pew Research Center. 2020. https://www.pewresearch.org/science/2020/09/17/u-s-public-now-divided-over-whether-to-get-covid-19-vaccine/. Accessed November 5, 2020.
- 37. Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS‐CoV‐2 vaccine: a survey of U.S. adults. Ann Intern Med. 2020;173(12):964‐973. 10.7326/M20-3569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Pazzanese C. Battling the ‘pandemic of misinformation.’ The Harvard Gazette. 2020. https://news.harvard.edu/gazette/story/2020/05/social-media-used-to-spread-create-covid-19-falsehoods/. Accessed November 5, 2020.
- 39. Richardson A, Allen JA, Xiao H, Vallone D. Effects of race/ethnicity and socioeconomic status on health information‐seeking, confidence, and trust. J Health Care Poor Underserved. 2012;23(4):1477‐1493. 10.1353/hpu.2012.0181 [DOI] [PubMed] [Google Scholar]
- 40. Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annu Rev Public Health. 2010;31(1):399‐418. 10.1146/annurev.publhealth.012809.103604 [DOI] [PubMed] [Google Scholar]
- 41. Bronfenbrenner U. The Ecology of Human Development. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- 42. McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351‐377. 10.1177/109019818801500401 [DOI] [PubMed] [Google Scholar]
- 43. Becker MH. The health belief model and sick role behavior. Health Educ Monogr. 1974;2(4):409‐419. 10.1177/109019817400200407 [DOI] [Google Scholar]
- 44. Jensen UT. Is self‐reported social distancing susceptible to social desirability bias? Using the crosswise model to elicit sensitive behaviors. J Behav Public Admin. 2020;3(2):1‐11. 10.30636/jbpa.32.182 [DOI] [Google Scholar]


