Abstract
Healthcare systems worldwide were challenged during the COVID-19 pandemic. In Mexico, the public hospitals that perform most transplants were adapted to provide care for COVID-19 patients. Using a nationwide database, we describe the first report of the impact of COVID-19 and related transplantation healthcare policies in a middle-income country by comparing statistics before and during the pandemic (pre-COVID: March 2019–February 2020 vs. COVID era: March 2020–February 2021) and by type of institution (public vs. private). The global reduction in transplantation was higher in public institutions compared with private institutions, 89% versus 62%, respectively, p < .001. When analyzing by organ, kidney transplantation decreased by 89% at public versus 57% at private, p < .001; cornea by 88% at public versus 64% at private, p < .001; liver by 88% at public versus 35% at private, p < .001; and heart by 88% in public versus 67% at private institutions, p = .4. The COVID-19 pandemic along with the implemented health policies were associated with a decrease in donations, waiting list additions, and a decrease in transplantation, particularly at public institutions, which care for the most vulnerable.
KEYWORDS: corneal transplantation / ophthalmology, disparities, ethics and public policy, health services and outcomes research, insurance - private, insurance - public, registry/registry analysis, kidney transplantation / nephrology, liver transplantation / hepatology
Abbreviations: AST, American Society of Transplantation; CENATRA, Centro Nacional de Trasplantes (National Transplant Center); ICU, intensive care unit
1. INTRODUCTION
Over the last year, the COVID-19 pandemic has pushed healthcare systems to their limits worldwide. This has exposed long-standing gaps in public health infrastructure as countries adapted to the challenge.1 As of April 1, 2021, Mexico remains one of the most affected countries by the pandemic, with more than 2.2 million confirmed cases and 200 000 deaths. Furthermore, Mexico has the highest mortality rate among the world’s 20 largest economies, 9.0%2; however, this might be explained by mortality bias because of undertesting, as Mexico has vastly underestimated the severity of the pandemic. During the peak of the pandemic, the positivity rate was as high as 50%.3
As part of the response to the pandemic, Mexico only allocated an additional 0.2% of the GDP to the healthcare sector, a significantly lower expenditure than other Latin American countries.4 For this reason, many of the existing resources were mobilized to guarantee care for infected patients, displacing resources from other healthcare programs, including converting tertiary care centers into COVID-19 units; most noncorneal transplants are performed in these centers, and they belong to the public sector. The need for ventilators and intensive care unit beds has deprived surgical capacity all over the world.5 Solid organ transplantation has not been an exception, and the number of transplants has substantially decreased across the world.6 In addition, there are concerns regarding safety after solid organ transplantation, as recipients could be at an increased risk for severe COVID-19. In April 2020, the American Society of Transplantation (AST) and other transplant societies suggested the suspension of nonurgent transplantations in communities with a high burden of the disease to avoid exposing both the donor and the recipient.6 , 7
In Mexico, all transplant programs are regulated by the government agency Centro Nacional de Transplantes (CENATRA, National Transplant Center). In March 2020, CENATRA agreed with the recommendations of the National Transplant Organization of Spain and the Transplant Society of Latin America and the Caribbean in limiting solid organ transplants to life-saving procedures, such as liver and heart transplants. Elective procedures were canceled during the periods of high transmission to avoid the exposure of patients, donors, and healthcare workers.8 As a result, from March to June 2020, donation and transplantation were greatly reduced in Mexico.
It was until late June 2020 when the plan to reactivate transplantation was launched. A traffic light system with four increasing levels represented by different colors (green, yellow, orange, and red) was implemented in Mexico to regulate public health restrictions. Hospitals with an appropriate number of healthcare workers, hospital, and intensive care unit (ICU) beds, laboratory and imaging services, and COVID-19-free zones could perform transplants with an internal committee approval. As of June 6, 2021, 5831 patients are on the waiting list for a cornea transplant, 16890 for kidney, 48 for heart, and 323 for a liver transplant.8 Our work aims to describe the impact of COVID-19 on Mexico’s liver, kidney, heart, and corneal transplants during March 2020 to February 2021 compared with March 2019 to February 2020. We hypothesized that the implemented COVID-19 policies had more impact on the transplant programs of public institutions than those of private institutions.
2. MATERIALS AND METHODS
We conducted a retrospective review of the publicly available database of Mexico’s National Transplant Registry.9 The database includes information from all transplants performed in Mexico from January 1, 2007 to February 28, 2021. Transplant centers register patients to CENATRA, who approves and assigns procured organs to public and private institutions. Organs will be exclusive to the type of institution (public or private) where they were procured. Allocation is prioritized at the local level to patients in life-threatening situations. If there are no recipients at the local level, CENATRA looks for a recipient at the state level and lastly, at the federal level. Transplants can only be performed if patients are registered on the CENATRA database. The database includes the following information: sex, institution, state of registration, hospital, procurement institution, state of donation procurement, place of birth of the recipient, state of residency, blood group, age, date of registration to the waiting list (waitlist addition), date of transplantation, type of transplantation, relationship between donor and recipient, and transplant result at 24 h. We included all the kidney, cornea, liver, and heart transplants from March 2019 to February 2021. These organs were selected as they have the highest number of procedures per year. March was chosen as the starting point as it was the first month when public health measures against the COVID-19 pandemic were implemented in 2020. The analysis was stratified in two time periods: pre-COVID included patients undergoing transplantation from March 1, 2019, to February 29, 2020, and COVID-era included patients undergoing transplantation from March 1, 2020, to February 28, 2021 (during COVID-19 pandemic). Demographic variables of interest were age, sex, type of institution where the transplant was performed (public or private), organ (kidney, liver, heart, or cornea), date of transplantation, and type of donor (living or deceased).
Public institutions depend on the federal budget and do not receive recovery fees for the care of patients. Private institutions are those in which patients themselves or a private medical insurance covers the cost of patient care.
Data regarding COVID-19 cases were extracted from the database of the Mexican Secretaria de Salud (Ministry of Health).10 This database is an open source and is updated daily with suspected COVID-19 cases that have been confirmed with a positive test for SARS-CoV-2. We included all ambulatory and hospitalized COVID-19 patients from March 1, 2020, to February 28, 2021.
Because data were publicly available, the Ethics Committee of the Instituto Nacional de Nutrición y Ciencias Médicas Salvador Zubirán deemed this study exempt from ethics approval.
2.1. Statistical analysis
Categorical variables are presented as frequencies and percentages and numerical variables as median and interquartile range. The proportion of transplants in the pre-COVID and COVID-era were compared by the type of institution using a Pearson’s chi-square or a Fisher’s exact test for independence as appropriate, overall and by the type of organ. The proportional reduction in the number of transplants from the pre-COVID to the COVID-era was computed for each transplant center, and their distributions between public and private institutions were compared using a Mann–Whitney U test, overall and by type of organ. The tendencies over time for the number of transplants per week by organ, type of institution (public or private) and period were assessed with locally weighted scatterplot smoothing (LOWESS) curves superimposed to their corresponding true number of transplants per week. Additionally, the number of COVID-19 cases and hospitalizations per week were also superimposed to the numbers of transplants per week during the COVID-era. The statistical analysis was performed using R version 4.0.2.
3. RESULTS
3.1. General characteristics
From March 2019 to February 2021, a total of 8593 transplants were performed in Mexico. Cornea was the most performed transplant (n = 4729, 55%), followed by kidney (n = 3551, 41.3%), liver (n = 273, 3.2%), and heart (n = 40, 0.5%). Most of the transplants were performed during the pre-COVID era (n = 7136, 83%), whereas only a minor proportion were from the COVID-era (n = 1457, 17%). The global reduction in the transplant volume from the pre-COVID era to the COVID-era was 80%. Overall, age and sex were similar among patients undergoing kidney, corneal, liver, and heart transplantation during both time periods.
3.2. Type of institution
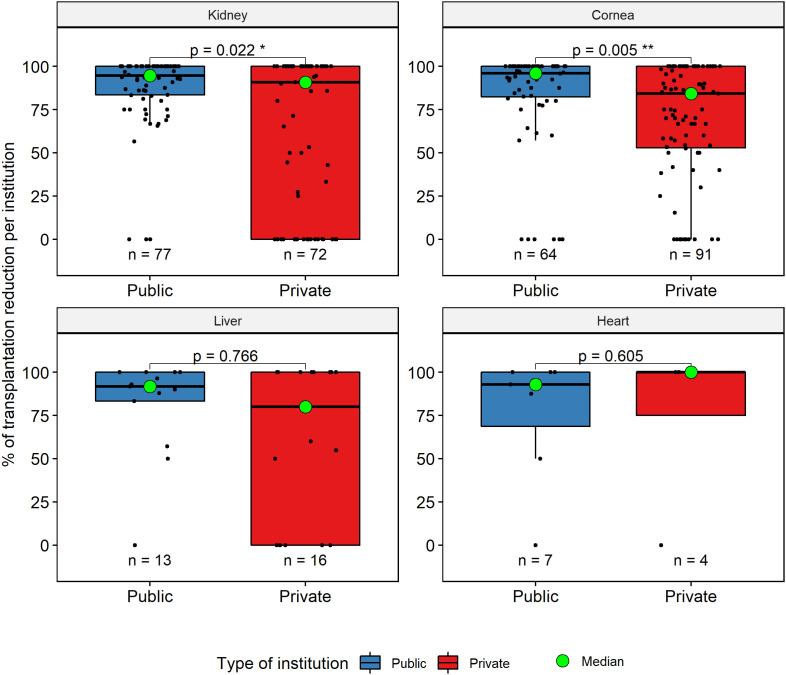
During pre-COVID time, for all organs, most transplants were performed at public institutions (n = 4646, 65%) compared with private institutions (n = 2490, 35%). The opposite occurred during the COVID-era; most transplants were from private institutions (n = 935, 64%), and public institutions performed a minor amount (n = 522, 36%). Despite that both types of institutions suffered a decrease in the number of transplants, the reduction was more marked at the public ones (public n = –4124, –89% vs. private n = –1555, –62%, p < .001) ( Figure 1). The median reduction in the number of transplants from pre-COVID to COVID-era was –95% in public institutions and –86% in private institutions, p < .001. These findings were consistent across all types of organs; specific differences are summarized in Table 1 and Figure 1.
FIGURE 1.
Impact of the COVID-19 pandemic across institutions. This figure shows the reduction in the number of transplants in public and private institutions by organ, the n = below each boxplot represents the number of centers. Each dot represents a transplant center [Color figure can be viewed at wileyonlinelibrary.com]
TABLE 1.
Comparison of organ transplantation by the type of institution between pre-COVID and COVID-era
| Organa | Public institutions n = 102 |
Private institutions |
p-value* | ||||
|---|---|---|---|---|---|---|---|
|
n = 162 | |||||||
| Pre-COVID | COVID-era | Reduction (%) | Pre-COVID | COVID-era | Reduction (%) | ||
| Kidney | 2387 | 251 | –89% | 639 | 274 | –57% | <.001 |
| Cornea | 2063 | 250 | –88% | 1780 | 636 | –64% | <.001 |
| Liver | 164 | 17 | –90% | 68 | 24 | –35% | <.001 |
| Heart | 32 | 4 | –88% | 3 | 1 | –67% | .4 |
| Global | 4646 | 522 | –89% | 2490 | 935 | –62%a | <.001 |
Pre-COVID: March 2019 to February 2020; COVID-era: March 2020 to February 2021.
The number for each organ represents the total number of transplanted patients during a specific era.
p-value obtained with a chi-square test for independence.
3.3. Type of donor
At public institutions, live donor kidney transplantation decreased by 8% while live donor liver transplantation increased by 20%, from the pre-COVID to the COVID-era. The type of donor was similar between both eras at private institutions. The distributions of live and deceased donors for kidney, cornea, liver, and heart transplants are displayed in Table 2 and Table 3.
TABLE 2.
Comparison of demographic variables and the type of donor by the type of institution between the pre-COVID and COVID-era for kidney and cornea transplants
| Public institutions |
Private institutions |
|||
|---|---|---|---|---|
| Pre-COVID | COVID-era | Pre-COVID | COVID-era | |
| Kidney | N = 2387 | N = 251 | N = 639 | N = 274 |
| Number of centers | 77 | 72 | ||
| Age (yr), median (IQR) | 30 (25, 43) | 30 (25, 42) | 40 (28, 56) | 37 (28, 54) |
| Sex, n (%) | ||||
| Female | 871 (36) | 100 (40) | 203 (32) | 86 (31) |
| Male | 1516 (64) | 151 (60) | 436 (68) | 188 (69) |
| Type of donor, n (%) | ||||
| Deceased | 841 (35) | 109 (43) | 102 (16) | 39 (14) |
| Live | 1546 (65) | 142 (57) | 537 (84) | 235 (86) |
| Cornea | N = 2063 | N = 250 | N = 1780 | N = 636 |
| Number of centers | 64 | 91 | ||
| Age (yr), median (IQR) | 55 (36, 69) | 53 (32, 66) | 56 (33, 70) | 52 (32, 68) |
| Sex, n (%) | ||||
| Female | 976 (47) | 111 (44) | 859 (48) | 300 (47) |
| Male | 1087 (53) | 139 (56) | 921 (52) | 336 (53) |
| Type of donor, n (%) | ||||
| Deceased | 2063 (100) | 250 (100) | 1780 (100) | 636 (100) |
Abbreviation: IQR, interquartile range.
Pre-COVID: March 2019 to February 2020; COVID-era: March 2020 to February 2021.
TABLE 3.
Comparison of demographic variables and type of donor by the type of institution between the pre-COVID and COVID-era for liver and heart transplants
| Public institutions |
Private institutions |
|||
|---|---|---|---|---|
| Pre-COVID | COVID-era | Pre-COVID | COVID-era | |
| Liver | N = 164 | N = 17 | N = 68 | N = 24 |
| Number of centers | 13 | 16 | ||
| Age (yr), median (IQR) | 47 (29, 56) | 41 (3, 52) | 58 (52, 62) | 60 (36, 65) |
| Sex, n (%) | ||||
| Female | 92 (56) | 11 (65) | 30 (44) | 10 (42) |
| Male | 72 (44) | 6 (35) | 38 (56) | 14 (58) |
| Type of donor, n (%) | ||||
| Deceased | 157 (96) | 13 (76) | 62 (91) | 21 (88) |
| Live | 7 (4) | 4 (24) | 6 (9) | 3 (12) |
| Heart | N = 32 | N = 4 | N = 3 | N = 1 |
| Number of centers | 7 | 4 | ||
| Age (yr), median (IQR) | 46 (41, 56) | 26 (17, 36) | 41 (30, 52) | 65 (65, 65) |
| Sex, n (%) | ||||
| Female | 8 (25) | 1 (25) | ||
| Male | 24 (75) | 3 (75) | 3 (100) | 1 (100) |
| Type of donor, n (%) | ||||
| Deceased | 32 (100) | 4 (100) | 3 (100) | 1 (100) |
Abbreviation: IQR, interquartile range.
Pre-COVID: March 2019 to February 2020; COVID-era: March 2020 to February 2021.
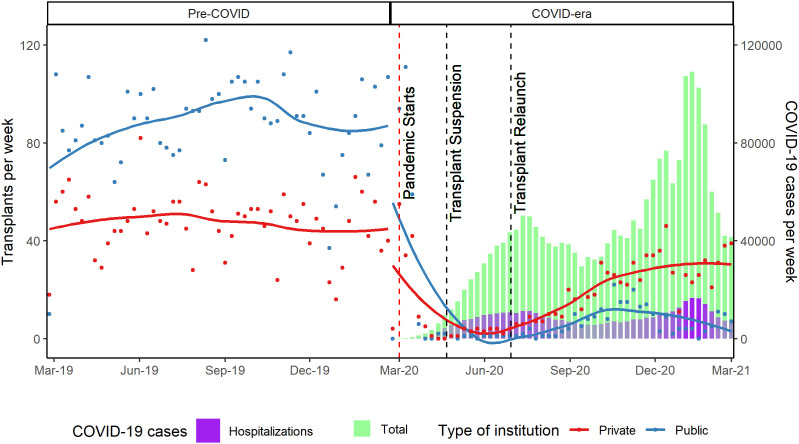
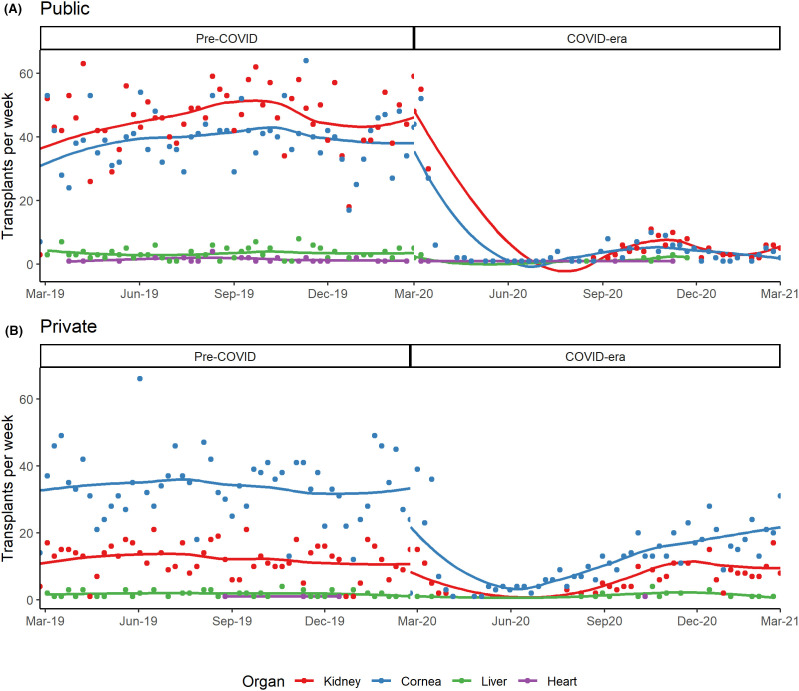
3.4. Transplant tendencies over time
Transplant trends are shown in Figure 2. During the pre-COVID era, the number of transplants per week remained stable across all organs, with most transplants occurring at public institutions ( Figure 3). During the COVID-era, a steep decline in transplantation was noted in March 2020 and remained low after CENATRA suspended donation and transplant programs in April 2020. The number of transplants started to rise slightly after the relaunch of the transplant program in June 2020 with a more marked increase at private institutions despite the rise in COVID-19 cases (Figure 2).
FIGURE 2.
Transplantation in Mexico during the pre-COVID and COVID-era. The number of transplants per week are displayed in public and private institutions during the two eras. The vertical lines indicate important events during the pandemic in Mexico. Each dot represents hospital variation [Color figure can be viewed at wileyonlinelibrary.com]
FIGURE 3.
Transplantation by organ and the type of institution during the pre-COVID and COVID-era: behavior of organ transplantation in (A) public institutions and (B) private institutions. Each dot represents hospital variation [Color figure can be viewed at wileyonlinelibrary.com]
3.5. Donations and waiting list additions
A marked decrease in organ procurement from deceased donors occurred during the study period. In the pre-COVID era, there were a total of 7222 organ donations, whereas in the COVID-era there were only 981. This represents a reduction of 86% when comparing both periods. Waiting list additions were also reduced by 70% during the pandemic. This was driven by a decrease in the addition of patients needing a kidney (pre-COVID n = 3671 vs. COVID-era n = 657, difference = –3014, –82%, p < .001) and a cornea (pre-COVID n = 1212 vs. COVID-era n = 747, difference = –465, –38%, p < .001) transplant. Donations and waiting list additions by the type of organ are summarized in Table 4.
TABLE 4.
Comparison of organ donation and waiting list additions between pre-COVID and COVID-era
| Organ | Donations |
Waiting list additions |
||||||
|---|---|---|---|---|---|---|---|---|
| Pre-COVID | COVID-era | Reduction (%) | p-value | Pre-COVID | COVID-era | Reduction (%) | p-value* | |
| Kidney | 3030 | 523 | –83% | <.001 | 3671 | 657 | –82% | <.001 |
| Cornea | 3932 | 412 | –90% | <.001 | 1212 | 747 | –38% | <.001 |
| Liver | 226 | 41 | –82% | <.001 | 75 | 68 | –9.3% | .5 |
| Heart | 34 | 5 | –83% | <.001 | 13 | 12 | –7.6% | .8 |
| Global | 7222 | 981 | –86% | <.001 | 4971 | 1484 | –70% | <.001 |
Pre-COVID: March 2019 to February 2020; COVID-era: March 2020 to February 2021.
p-value obtained with a chi-square test for independence.
4. DISCUSSION
Our study reveals the impact of the COVID-19 pandemic in the national transplant program in Mexico. This is the first report of this type in a middle-income country using a nationwide database. There was an overall nationwide reduction in the number of transplants performed during the first year of the COVID-19 pandemic in Mexico across the organs studied: Cornea, kidney, liver, and heart. The reduction in transplant volume occurred in both public and private institutions; however, the impact in public institutions was greater than the one seen in private institutions. This may be explained by the COVID-19 transplant policy implemented by CENATRA and by different government policies directed at the restructuring of the healthcare system.8 , 11
Tertiary public centers perform most of the organ procurement and transplantation activities in Mexico. The government plan mandated the restructuring of all public hospitals prioritize care for patients with COVID-19.12 This policy made public institutions more vulnerable by depriving them of the resources required to perform solid organ transplantation. From March to July 2020, Mexico increased its ICU capability from 1.9 to 9.1 beds per 100 000 population.11 Despite this, hospitals were quickly overwhelmed. The lack of COVID-19-free zones limited organ procurement and made transplants unviable due to the risk of infection to recipients, donors, and healthcare workers. In contrast, because private institutions played a lesser role in the coordinated care of COVID-19 patients,13 most of their elective surgeries remained active. This allowed private institutions to comply with CENATRA requirements at the local level to reactivate transplantation procedures, which might explain the relative increase despite the high rates of infection and hospitalizations during the last months of 2020.
Healthcare workers represented another essential element to reactivate the transplant program; however, they have faced several problems during the pandemic in Mexico. In the first months, there was a shortage of personal protective equipment and poor working conditions leading to a high rate of SARS-CoV-2 infections, the highest rate among healthcare workers in the world.14 In June 2020, they represented 21% of all individuals with laboratory-confirmed SARS-CoV-2 infection,15 and some institutions had to close due to COVID-19 outbreaks.14 Afterward, vulnerable personnel were removed, reducing the workforce in public institutions, and increasing the workload and psychological burden of the remaining personnel.16 These factors limited the availability of healthcare workers for the care of transplant patients in the public setting. Private institutions faced less burden and thus their transplant programs did not have this limitation.17 There are also important differences in material resources between both types of institutions, the availability of SARS-CoV-2 testing for donors and recipients, facilitates program reactivation in private centers.13
The strategy of the Mexican government has been heavily criticized.11 , 18During the initial stage of the COVID-19 pandemic, there was a lack of consistency among the case definitions and algorithms between institutions, and to make matters worse, access to diagnostic tests was also heavily restricted.16 The government focused on increasing hospital capacity, mass communications for hygiene measures and social distancing.19 A limited testing strategy and the lack of contact tracing along with an early reopening of the economy led to an accelerated transmission of the virus during the following months.11 , 18 , 20Another obstacle to resuming transplantation in Mexico was the burden of the disease in the community.8 Hence, the high number of cases seen during the pandemic in Mexico limited the transplant procedures to only life-threatening situations.
During the first month of the pandemic, other countries with high rates of community viral transmission such as the United States and France faced reductions in transplantation rates of 51.1% and 90.6%, respectively.21 Indeed, countries that implemented early policies such as aggressive testing among donors, extension of intensive care capacity on already strong structural healthcare systems with high ICU capacity and well-organized transplant centers were able to maintain stable numbers of transplantation despite high infection rates among their population.22 , 23 The lack of such existing centers and tailored policy design at public institutions in Mexico has limited the possibility of maintaining transplant numbers stable despite a high number of patients on the waiting list, which might not represent the real number of patients, as many have not been evaluated to enter the waiting list.
The public healthcare institutions in Mexico care for the most vulnerable population of patients,24 while private institutions care for the wealthiest patients; it is estimated that only 1% of the population has access to them through private insurance of personal funds.25 COVID-19 has increased and exposed existing healthcare disparities among patients with high and low socioeconomic status.26 In 2012, 49% of Mexican population had no access to healthcare under the former Seguro Popular,27 a government program aimed to guarantee universal access to healthcare, particularly in vulnerable populations. According to a study, the population living in marginalized regions have lesser access to healthcare and a lower number of physicians compared with regions with higher income (fewer than 5 vs. nearly 20 physicians per 100 000 inhabitants, respectively).28 To complicate things further, a new health system was implemented a few months before the pandemic to substitute Seguro Popular with no intentions of including private institutions; increasing the fragmentation of the Mexican health system.29 These disparities were also observed in the transplant program of Mexico, limiting the accessibility of solid organ transplantation among vulnerable patients.
The main limitation of this study is that we used an administrative database. Although the CENATRA database contains the information of every transplant performed in the country, it lacks important clinical variables that could add relevant information such as outcomes and follow-up of transplanted patients and of those in the waiting list. We consider that CENATRA should improve data collection to answer these questions and should demand transplant centers to provide long-term patient outcomes.
The COVID-19 pandemic health policies in Mexico were associated with an important nationwide reduction across all types of solid organ transplantation. Hospital reconversion, shortage of healthcare workers, low ICU capacity, uncontrolled viral transmission in the community, and the lack of exclusive transplantation and donation centers were important factors that limited the number of transplants at public institutions. Better resource allocation and tailored health care policies are required to maintain transplantation during times of crisis at public institutions. Absence of such interventions leaves the most vulnerable population unable to access lifesaving procedures.
ACKNOWLEDGMENT
The authors would like to thank Dr Alice Gallo De Moraes for her help with style corrections.
DISCLOSURE
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
OPEN RESEARCH BADGE STATEMENT
This article earned the Open Data Badge for transparent practices. The data are publicly available at https://datos.gob.mx/busca/organization/cenatra.
DATA AVAILABILITY STATEMENT
The data that support the findings of our study are openly available in Datos Abiertos CENATRA at http://cenatra.salud.gob.mx/transparencia/datos-abiertos/datos_abiertos_trasplantes.html, reference number.9
REFERENCES
- 1.Lal A, Erondu NA, Heymann DL, Gitahi G, Yates R. Fragmented health systems in COVID-19: rectifying the misalignment between global health security and universal health coverage. Lancet. 2021;397(10268):61–67. doi: 10.1016/S0140-6736(20)32228-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johns Hopkins Coronavirus Resource Center. MORTALITY RATE. https://coronavirus.jhu.edu/data/mortality. Accessed March 23, 2021.
- 3.Ritchie H, Ortiz-Ospina E, Beltekian D, et al. Mexico: coronavirus pandemic country profile. https://ourworldindata.org/coronavirus/country/mexico. Accessed June 1, 2021.
- 4.Hannan S, Honjo K, Raissi M. Mexico needs a fiscal twist. IMF Work Pap. 2020;20(215) doi: 10.5089/9781513559018.001. [DOI] [Google Scholar]
- 5.Søreide K, Hallet J, Matthews JB, et al. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br J Surg. 2020;107(10):1250–1261. doi: 10.1002/bjs.11670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Azzi Y, Bartash R, Scalea J, Loarte-Campos P, Akalin E. COVID-19 and solid organ transplantation: a review article. Transplantation. 2021;105(1):37–55. doi: 10.1097/TP.0000000000003523. [DOI] [PubMed] [Google Scholar]
- 7.American Society of Transplantation. 2019-nCoV (Coronavirus): FAQs for organ transplantation. https://www.myast.org/sites/default/files/COVID19FAQTxCenters10.26.2020.pdf. Accessed February 15, 2021.
- 8.Centro Nacional de Trasplantes. CENATRA. https://www.gob.mx/cenatra. Accessed May 15, 2021.
- 9.CENATRA Datos Abiertos CENATRA. http://cenatra.salud.gob.mx/transparencia/datos-abiertos/datos_abiertos_trasplantes.html. Published 2021. Accessed February 15, 2021.
- 10.Secretaria de Salud Datos Abiertos Dirección General de Epidemiología. https://www.gob.mx/salud/documentos/datos-abiertos-152127. Published 2021. Accessed June 1, 2021.
- 11.Taylor L. Covid-19: How denialism led Mexico’s disastrous pandemic control effort. BMJ. 2020;371:1–2. doi: 10.1136/bmj.m4952. [DOI] [PubMed] [Google Scholar]
- 12.Secretaria de Gobernacion ACUERDO por el que el Consejo de Salubridad General reconoce la epidemia de enfermedad por el virus SARS-CoV2 (COVID-19) en México, como una enfermedad grave de atención prioritaria, así como se establecen las actividades de preparación y respuest. http://dof.gob.mx/nota_detalle.php?codigo = 5590161&fecha = 23/03/2020. Published 2020. Accessed May 20, 2021.
- 13.Najera H, Ortega-Avila AG. Health and institutional risk factors of COVID-19 mortality in Mexico, 2020. Am J Prev Med. 2021;60(4):471–477. doi: 10.1016/j.amepre.2020.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Caldera-Villalobos C, Garza-Veloz I, Martínez-Avila N, et al. The coronavirus disease (COVID-19) challenge in Mexico: a critical and forced reflection as individuals and society. Front Public Health. 2020;8(June):26–29. doi: 10.3389/fpubh.2020.00337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guerrero-Torres L, Caro-Vega Y, Crabtree-Ramírez B, Sierra-Madero JG. Clinical characteristics and mortality of health-care workers with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in Mexico city. Clin Infect Dis. 2021;73(1):e199–e205. doi: 10.1093/cid/ciaa1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bautista-González E, Werner-Sunderland J, Pérez-Duarte Mendiola P, et al. Health-care guidelines and policies during the COVID-19 pandemic in Mexico: a case of health-inequalities. Health Policy OPEN. 2020;2021(2):100025. doi: 10.1016/j.hpopen.2020.100025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arizpe-Bravo D, Arizpe-Bravo A, Leon RB, et al. Experience with Covid-19 critically Ill patients in a private community hospital in Puebla city, Mexico. Chest. 2020;158(4):A2482–A2483. doi: 10.1016/j.chest.2020.09.057. [DOI] [Google Scholar]
- 18.Ibarra-Nava I, Cardenas-De La Garza JA, Ruiz-Lozano RE, Salazar-Montalvo RG. Mexico and the COVID-19 Response. Disaster Med Public Health Prep. 2020;14(4):E17–E18. doi: 10.1017/dmp.2020.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Secretaria de Salud. Lineamiento Estandarizado para la Vigilancia Epidemiológica y por Laboratorio de la enfermedad respiratoria viral. https://www.gob.mx/salud/documentos/lineamiento-estandarizado-para-la-vigilancia-epidemiologica-y-por-laboratorio-de-la-enfermedad-respiratoria-viral. Accessed February 15, 2021.
- 20.Bernal-Serrano D, Carrasco H, Palazuelos L, Mubiligi JM, Oswald C, Mukherjee JS. Health Policy Issue Brief: COVID-19 in Mexico, an imperative to test, trace, and isolate. OSF Prepr; 2020.
- 21.Loupy A, Aubert O, Reese PP, Bastien O, Bayer F, Jacquelinet C. Organ procurement and transplantation during the COVID-19 pandemic. Lancet. 2020;395(10237):e95–e96. doi: 10.1016/S0140-6736(20)31040-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hugo C, Strassburg C, Stecher M, Rahmel A. Stable and safe organ procurement and transplantation during SARS-CoV-2 pandemic in Germany. Transpl Int. 2020;33(10):1335–1336. doi: 10.1111/tri.13704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reddy S, Dumbill R, Akhtar MZ, et al. Transplant programmes in areas with high SARS-CoV-2 transmission. Lancet. 2020;396(10260):1395–1396. doi: 10.1016/S0140-6736(20)32209-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Frenk J, González-Pier E, Gómez-Dantés O, Lezana MÁ, Knaul FM. Reforma integral para mejorar el desempeño del sistema de salud en México. Salud Publica Mex. 2007;49(SUPPL. 1):23–36. doi: 10.1590/s0036-36342007000700007. [DOI] [PubMed] [Google Scholar]
- 25.Fajardo-Dolci G, Gutiérrez JP, García-Saisó S. Acceso efectivo a los servicios de salud: operacionalizando la cobertura universal en salud. Salud Publica Mex. 2015;57(2):180. doi: 10.21149/spm.v57i2.7415. [DOI] [PubMed] [Google Scholar]
- 26.Lopez L, Hart LH, Katz MH. Racial and ethnic health disparities related to COVID-19. JAMA. 2021;2019:8–9. doi: 10.1001/jama.2020.26443. [DOI] [PubMed] [Google Scholar]
- 27.Gutiérrez JP, García-Saisó S, Dolci GF, Ávila MH. Effective access to health care in Mexico. BMC Health Serv Res. 2014;14(1):1–9. doi: 10.1186/1472-6963-14-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barraza-Lloréns M, Bertozzi S, González-Pier E, Gutiérrez JP. Addressing inequity in health and health care in Mexico. Health Aff. 2002;21(3):47–56. doi: 10.1377/hlthaff.21.3.47. [DOI] [PubMed] [Google Scholar]
- 29.Reich MR. Restructuring health reform, Mexican style. Health Syst Reform. 2020;6(1):1–11. doi: 10.1080/23288604.2020.1763114. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of our study are openly available in Datos Abiertos CENATRA at http://cenatra.salud.gob.mx/transparencia/datos-abiertos/datos_abiertos_trasplantes.html, reference number.9