Abstract
We report the case of a previously healthy 16‐year‐old male who developed myopericarditis following the second dose of his Pfizer‐BioNTech COVID‐19 vaccine, with no other identified triggers. Adolescents and young adults experiencing chest pain after COVD‐19 vaccination should seek emergent medical care, and emergency providers should have a low threshold to consider and evaluate for myopericarditis. More data are needed to better understand the potential association between COVID‐19 vaccines and myopericarditis. If a true causal link is identified, the risk must also be viewed in context with the millions of patients who have been safely vaccinated and the known morbidity and mortality from COVID‐19 infection. As we see widespread vaccine rollout, it is important that all potential adverse reactions are reported as we continue to monitor for more rare but potentially serious side effects not identified in vaccination trials.
Keywords: COVID‐19, myocarditis
COVID‐19 has infected over 3.9 million children and adolescents in the United States and has resulted in over 3,700 cases of multisystem inflammatory syndrome in children (MIS‐C) and 400 deaths in children 0 to 17.1 Beyond the immediate health impacts, there have also been worsening mental and behavioral health for children and their families, loss of childcare and in‐person education, increased food insecurity, and economic distress.2 Widespread vaccination has been identified as our best hope for ending the pandemic. The Pfizer‐BioNTech COVID‐19 vaccine, Moderna COVID‐19 vaccine, and Janssen COVID‐19 vaccine received emergency authorization use for patients 16 years and older in December 2020. The Pfizer‐BioNTech COVID‐19 vaccine then received emergency authorization us for patients aged 12 to 15 on May 10, 2021.3 The clinical trials data in adolescents age 12 to 17 overall demonstrates a vaccine efficacy rate of 96% and was 100% effective among 12 to 15 year olds.4 The most common side effects reported include headache, fatigue, myalgias, and chills, with no serious safety concerns identified.4 As millions of adolescents in the United States get vaccinated, the Centers for Disease Control and Prevention (CDC) and the U.S. Food and Drug Administration (FDA) have engaged in ongoing safety monitoring. On May 17, 2021, the CDC reported that COVID‐19 Vaccine Safety Technical Work Group identified “several presentations of myocarditis following mRNA vaccines.”5 These cases, which were predominantly seen in adolescent and young adult males, typically occurred within 4 days after receiving the second dose of an mRNA vaccine.5 We present the case of a previously healthy 16‐year‐old male who developed myopericarditis following the second dose of his Pfizer‐BioNTech COVID‐19 vaccine with no other etiology identified.
A previously healthy 16‐year‐old male presented to the emergency department (ED) with a chief complaint of sharp/stabbing chest pain for 36 h. The patient received his second dose of the Pfizer Covid‐19 vaccine approximately 60 h prior to his presentation. Approximately 12 h after vaccination the patient developed myalgias and tactile fevers, which resolved in 1 day. The patient then developed sharp, stabbing midsternal chest pain approximately 24 hours after receiving the vaccine, which was characterized as 6 to 8 on a scale of 1 to 10 and radiating to the left arm. Pain was worse with lying down, with no other associated symptoms or alleviating or exacerbating factors. The pain woke patient from sleep in the middle of the night prompting presentation to the ED. A complete ROS was negative for any signs or symptoms of systemic illness in the 6 weeks prior to his vaccine. A family history was negative for cardiac disease or cardiac risk factors.
On arrival to the ED, vital signs included a temperature of 37.5°C, heart rate 80 beats/min, blood pressure of 112/70 mmHg, respiratory rate 18, and pulse oximetry 98% on room air. Physical examination was normal, including normal cardiac and respiratory exam. Electrocardiogram (ECG) revealed normal sinus rhythm with diffuse ST elevation in V2 to V6 and I and aVL (Figure 1). Laboratory evaluation was notable for troponin T elevated to 1,018 ng/L, creatinine kinase elevated to 699 U/L, and CK‐MB elevated at 47.7 µg/L. B‐type natriuretic peptide was slightly above normal at 111 pg/mL. His creatinine was elevated to 1.17 with otherwise normal comprehensive metabolic panel. He had a normal complete blood count, but C‐reactive protein and erythrocyte sedimentation rate were both elevated at 7.6 mg/dL and 28 mm/h, respectively. Thyroid function testing, triglycerides, and ferritin sent as a part of the MIS‐C workup were all normal; however, his D‐dimer was slightly elevated at 233 ng/mL. Rapid COVID‐19 and influenza tests were both negative. Cardiology was consulted in the setting of ST elevation on ECG and chest pain. They performed a bedside point‐of‐care ultrasound, which showed subjectively normal systolic function, no wall motion abnormalities, and no pericardial effusions. His chest radiograph showed no acute cardiopulmonary abnormality. He was diagnosed with suspected myopericarditis and admitted to the pediatric intensive care unit (ICU) due to risk of cardiovascular collapse and shock requiring telemetry and close monitoring of his vitals while ongoing workup and treatment were completed.
FIGURE 1.
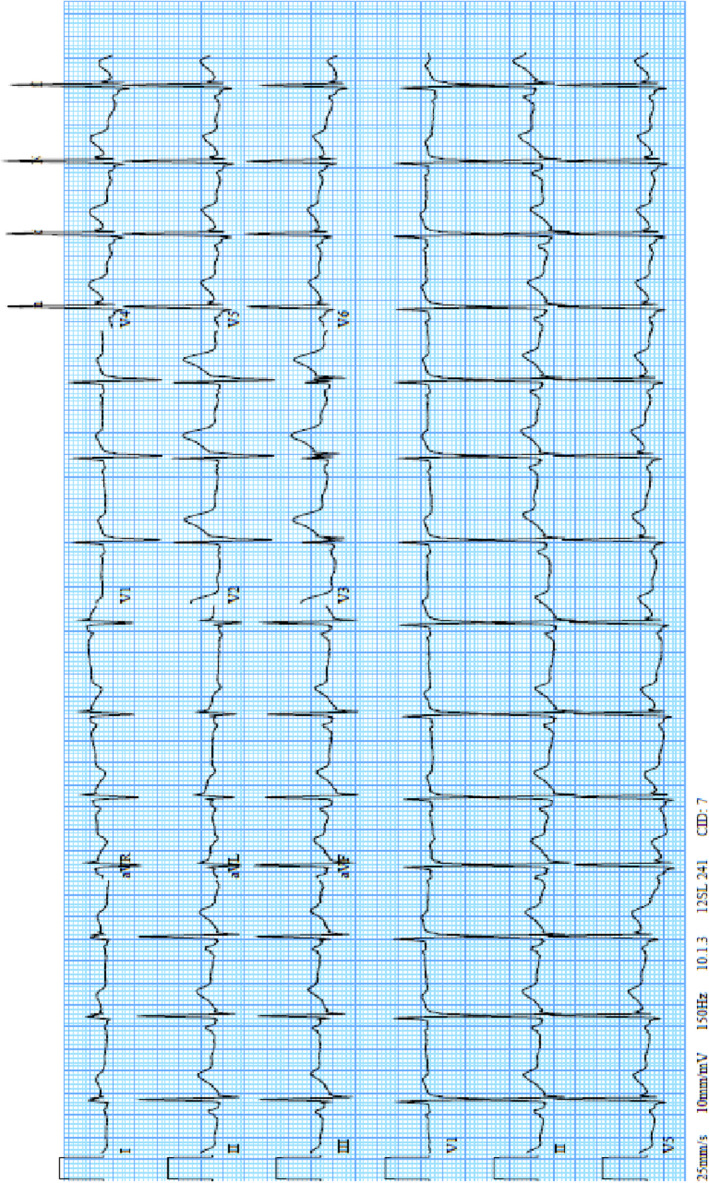
Myocarditis case
His hospital workup included a formal pediatric echocardiogram, which demonstrated normal anatomy, normal systolic function (61%), and no pericardial effusion. The right coronary artery was not well visualized. Computed tomography angiogram of the heart revealed minimal lateral wall subepicardial hyperenhancement, suggestive of myocarditis. He was also noted to have an incidental benign coronary artery anomaly believed to be unrelated to his illness. Cardiac magnetic resonance imaging showed normal biventricular volumes, morphology, and systolic function. However, there were signs of myocardial fibrosis, myocardial hyperemia, and a small pericardial effusion consistent with myopericarditis.
The patient's hospital course consisted of a negative infectious workup including viral testing for influenza A/B, respiratory syncytial virus, parainfluenza, coronavirus (not 2019 pandemic virus), human metapneumovirus, rhino/enterovirus, adenovirus, Chlamydia pneumoniae, Mycoplasma pneumoniae, parvovirus, enterovirus, herpesvirus 6, coxsackie B virus, and adenovirus antibody. Urine drug screen was also sent to investigate other potential sources of troponin leak, which was negative. No alternative etiology of the myopericarditis identified beyond the temporal association with COVID‐19 vaccination.
The patient was treated with a four‐dose series of intravenous immunoglobulin and provided ibuprofen for symptomatic relief with resolution of chest pain. He otherwise did not require any cardiovascular or respiratory supportive measures and did not have other interventions during his admission. His ECG showed resolution of ST elevation on hospital day 3. He was discharged home on hospital day 6 with a troponin of 45 ng/L, which was down trending from a peak of 1,693 ng/L. He was sent home on a 7‐day course of schedule ibuprofen and famotidine, and 2‐week follow‐up with pediatric cardiology was arranged.
Myocarditis and pericarditis are inflammatory processes involving the myocardium, pericardium, or both. The primary etiology in the United States is thought to be viral, but other etiologies include other infections, systemic disease, drugs, and toxins.6, 7 Presentations may be acute, defined by direct viral cytotoxicity and focal or diffuse necrosis of the myocardium; subacute, defined by an increase in auto‐immune mediated injury; or chronic, defined by diffuse myocardial fibrosis and cardiac dysfunction that may lead to dilated cardiomyopathy and its sequelae.7 Presenting symptoms vary based on age of the patient, with infants and toddlers often presenting with fatigue, respiratory distress, fever, poor appetite, and tachycardia, while older children more often present with chest pain, abdominal pain, myalgias, fatigue, cough, and edema.8 In one study, the most common presenting symptoms in the ED in cases of pediatric myocarditis were respiratory distress, tachycardia, lethargy, hepatomegaly, abnormal heart sound, and fever.9 The incidence of myocarditis has been reported as approximately 1.5 million cases worldwide per year and is estimated between 10 to 20 cases per 100,000 persons.7 However, it is thought to be underdiagnosed as many cases are subclinical. While the disease course is unpredictable and variable, higher levels of troponin (greater than 3× the upper limit of the reference range) likely correlate with more myocardial damage.7 The prognosis of patients with myocarditis varies. Those with severe disease (decreased systolic function or development of dilated cardiomyopathy) have a poor prognosis without a transplant, but patients with mild disease typically have good outcomes. The mortality rate is as high as 20% at 1 year and 50% at 5 years.7
While the disease process in our patient appears related to this vaccine and has been previously reported with other vaccines, we highlight that current evidence only supports a causal relationship secondary to timing. There have been case reports of pericarditis following influenza vaccine10, 11 and hepatitis B vaccination,12 myopericarditis after DTaP,13 and more widespread instances of myopericarditis following smallpox vaccination (0.05%).6 Outside of the association with smallpox vaccination, most myocarditis or pericarditis cases following vaccinations are very rare and reported as unique cases. In the wake of widespread COVID‐19 vaccination that is occurring nationally and internationally, there are emerging cases of myopericarditis reported after vaccination.14, 15, 16 As more cases arise we will better understand the mechanism of myocardial infiltration, the true incidence of potential vaccine‐associated myopericarditis, and the long‐term sequela and burden of this disease.
COVID‐19 caries a serious health burden for pediatric patients. While pediatric patients have had lower incidences of COVID‐19 compared to older populations,17 about one in three children hospitalized with COVID‐19 in the United States were admitted to the ICU, similar to the rate among adults.18 Also similar to adults, these children with severe disease may develop respiratory failure and multiorgan dysfunction and failure. Myocarditis has also been reported among patients with COVID‐19 infection, with a rate estimated at less than 5% in adults.19 At least two pediatric patients have been diagnosed with COVID‐19–associated myocarditis, although one was coinfected with adenovirus.20, 21
As we consider the health consequences of COVID‐19 infections, we are beginning to see more cases of “long‐haul” COVID‐19 among pediatric patients with symptoms of fatigue, shortness of breath, body aches, chest pain, headaches, depression, and brain fog.22 The burden and incidence of serious COVID‐19 infections, long‐haul symptoms, and MIS‐C in pediatric populations continue to be defined, as do the social, emotional, economic, and academic repercussions brought on by more than 12 months of isolation and societal shutdowns and the devastating impact of racial disparities.
Several important implications should be considered in light of this case and other recent reports in the media and literature while awaiting further data and conclusions from the CDC. First, while chest pain usually has a benign etiology in pediatric populations,23 as more children, adolescents, and young adults become vaccinated against COVID‐19, even young patients experiencing chest pain after COVD‐19 vaccination should seek emergent evaluation. Also, health care providers should have a low threshold to consider and evaluate for myopericarditis among patients presenting with chest pain in the postvaccine period. This and other emerging cases also help to illustrate the important role that emergency medicine providers can play in identifying, treating, and reporting potential vaccine‐associated conditions. It is important that any cases of myopericarditis and other potential adverse reactions occurring after COVID‐19 vaccination are reported to vaccine manufacturers and governing vaccine event reporting systems as we continue to monitor for more rare but serious side effects that were not identified in vaccination trials.
More data are needed to better understand the potential association between COVID‐19 vaccines and myopericarditis as well as more long‐term follow‐up to better characterize prognosis and sequelae. If a true causal link is identified, it must also be viewed in context with the millions of patients who have been safely vaccinated and the known morbidity and mortality from COVID‐19 infection.
McLean K, Johnson TJ. Myopericarditis in a previously healthy adolescent male following COVID‐19 vaccination: A case report. Acad Emerg Med. 2021;28:918–921. 10.1111/acem.14322
Supervising Editor: John H. Burton, MD.
REFERENCES
- 1.Health Department‐Reported Cases of Multisystem Inflammatory Syndrome in Children (MIS‐C) in the United States . Centers for Disease Control and Prevention website. 2021. Accessed May 25, 2021. https://www.cdc.gov/mis‐c/cases/index.html
- 2.Patrick SW, Henkhaus LE, Zickafoose JS, et al. Well‐being of parents and children during the COVID‐19 pandemic: a national survey. Pediatrics. 2020;146(4):e2020016824. [DOI] [PubMed] [Google Scholar]
- 3.Commissioner of the Coronavirus (COVID‐19) Update: FDA Authorizes Pfizer‐BioNTech COVID‐19 Vaccine for Emergency Use in Adolescents in Another Important Action in Fight Against Pandemic . U.S. Food and Drug Administration website. 2021. Accessed May 26, 2021. https://www.fda.gov/news‐events/press‐announcements/coronavirus‐covid‐19‐update‐fda‐authorizes‐pfizer‐biontech‐covid‐19‐vaccine‐emergency‐use
- 4.A PHASE 1/2/3, PLACEBO‐CONTROLLED, RANDOMIZED, OBSERVER‐BLIND, DOSE‐FINDING STUDY TO EVALUATE THE SAFETY, TOLERABILITY, IMMUNOGENICITY, AND EFFICACY OF SARS‐COV‐2 RNA VACCINE CANDIDATES AGAINST COVID‐19 IN HEALTHY INDIVIDUALS . 2020. Accessed May 26, 2021. https://cdn.pfizer.com/pfizercom/2020‐11/C4591001_Clinical_Protocol_Nov2020.pdf
- 5.COVID‐19 VaST Technical Report May 17, 2021 . Centers for Disease Control and Prevention website. 2021. Accessed May 25, 2021. https://www.cdc.gov/vaccines/acip/work‐groups‐vast/technical‐report‐2021‐05‐17.html
- 6.Casey CG. Adverse events associated with smallpox vaccination in the United States, January‐October 2003. JAMA. 2005;294(21):2734. 10.1001/jama.294.21.2734 [DOI] [PubMed] [Google Scholar]
- 7.Kang M, An J. Viral Myocarditis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459259/. 2021. Accessed May 25, 2021.
- 8.Blauwet LA, Cooper LT. Myocarditis. Prog Cardiovasc Dis. 2010;52(4):274‐288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Amabile N. Outcome of acute fulminant myocarditis in children. Heart. 2006;92(9):1269‐1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Meester A , Luwaert R, Chaudron JM. Symptomatic pericarditis after influenza vaccination. Chest. 2000;117(6):1803‐1805. [DOI] [PubMed] [Google Scholar]
- 11.Streifler JJ, Dux S, Garty M, Rosenfeld JB. Recurrent pericarditis: a rare complication of influenza vaccination. BMJ. 1981;283(6290):526‐527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bensaid J, Denis F. Péricardite aiguë bénigne après vaccination contre l'hépatite B [Benign acute pericarditis after vaccination against hepatitis B]. Presse Med. 1993;22(6):269. [PubMed] [Google Scholar]
- 13.Boccara F, Benhaiem‐Sigaux N, Cohen A. Acute myopericarditis after diphtheria, tetanus, and polio vaccination. Chest. 2001;120(2):671‐672. 10.1378/chest.120.2.671 [DOI] [PubMed] [Google Scholar]
- 14.Albert E, Aurigemma G, Saucedo J, Gerson DS. Myocarditis following COVID‐19 vaccination. Radiol Case Rep. 2021;16(8):2142–2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mandavilli A. C.D.C. Is Investigating a Heart Problem in a Few Young Vaccine Recipients. The New York Times website. 2021. Accessed May 26, 2021. https://www.nytimes.com/2021/05/22/health/cdc‐heart‐teens‐vaccination.html
- 16.James S, Washington Co. Teen's Parents Warning about Myocarditis, Rare Condition Possibly Linked to COVID‐19. WPXI website. 2021. Accessed May 26, 2021. https://www.wpxi.com/news/top‐stories/local‐teen‐rushed‐hospital‐with‐trouble‐breathing‐following‐2nd‐dose‐covid‐19‐vaccine/MRSTITDZXBCKBCIRQCIUKNOBAQ/
- 17.CDC COVID Data Tracker . Centers for Disease Control and Prevention website. 2021. Accessed May 25, 2021. https://covid.cdc.gov/covid‐data‐tracker/#datatracker‐home
- 18.Information for Pediatric Healthcare Providers . Centers for Disease Control and Prevention website. 2021. Accessed May 25, 2021. https://www.cdc.gov/coronavirus/2019‐ncov/hcp/pediatric‐hcp.html
- 19.Kawakami R, Sakamoto A, Kawai K, et al. Pathological evidence for SARS‐CoV‐2 as a cause of myocarditis. J Am Coll Cardiol. 2021;77(3):314‐325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Trogen B, Gonzalez FJ, Shust GF. COVID‐19‐associated myocarditis in an adolescent. Pediatr Infect Dis J. 2020;39(8):e204–e205. [DOI] [PubMed] [Google Scholar]
- 21.Lara D, Young T, Del Toro K, et al. Acute fulminant myocarditis in a pediatric patient with COVID‐19 infection. Pediatrics. 2020; 146(2):e20201509. [DOI] [PubMed] [Google Scholar]
- 22.Post‐COVID Conditions . Centers for Disease Control and Prevention website. 2021. Accessed May 25, 2021. https://www.cdc.gov/coronavirus/2019‐ncov/long‐term‐effects.html
- 23.Kocis KC. Chest pain in pediatrics. Pediatr Clin North Am. 1999;46(2):189‐203. [DOI] [PubMed] [Google Scholar]


