Abstract
Introduction
The COVID‐19 pandemic is driving unprecedented changes in healthcare services worldwide. This study aimed to quantify the impact of the first wave of the COVID‐19 pandemic on diagnostic imaging services in Australia using an interrupted time series model.
Methods
Monthly data were extracted from the Australian Medicare Benefits Schedule for all diagnostic imaging services performed between January 2016 and December 2019. Holt‐Winters forecasting models were developed for total imaging services as well as for each imaging modality. The models were used to predict monthly data between January 2020 and June 2020 with a 95% confidence interval (P < 0.05). Absolute and percentage residual differences (RD) between observed and predicted services for this time period were calculated.
Results
There were statistically significant reductions in total imaging services performed in March 2020 (RD: −332260, −13.1%, 95% CI: −17.5% to −8.4%), April 2020 (RD: −716957, −32.4%, 95% CI: −36.2% to −28.1%) and May 2020 (RD: −571634, −21.4%, 95% CI: −25.1% to −17.3%). Nuclear medicine and CT services were relatively less impacted than general radiography, ultrasound, and MRI services. There was also a statistically significant increase in nuclear medicine and CT services performed in June 2020 compared to predicted values.
Conclusions
During the first wave of COVID‐19 in Australia, there was a significant reduction in total diagnostic imaging services, with variable impacts on different imaging modalities. These findings may have significant public health implications and can be used to inform evidence‐based strategies in the recovery phase of the pandemic.
Keywords: coronavirus, COVID‐19, health services, public health, radiology, SARS‐CoV‐2
Introduction
The coronavirus disease 2019 (COVID‐19) pandemic is driving unprecedented changes to clinical imaging services worldwide. 1 In Australia, the first case of COVID‐19 was confirmed on the 25th of January 2020. By March 2020, federal and state governments implemented a range of restrictions on healthcare delivery in Australia in order to limit virus transmission and protect hospital capacity. 2 Notably, cancellation of elective surgeries and non‐urgent medical services were implemented on the 25th of March 2020. 3 These restrictions on healthcare delivery combined with stay‐at‐home orders led to an abrupt decline in demand for imaging services in Australia and internationally. 4 , 5 , 6
The potential impact of reduced demand on the radiology sector is multifaceted. Most importantly, radiology plays a central role in healthcare delivery through informing clinical decision‐making, providing or supporting diagnoses, planning surgical interventions, monitoring disease progression and treatment response, and performing diagnostic or therapeutic interventions. A reduction in imaging services has significant public health implications, with a backlog of referrals likely to cause a delay in patient diagnoses and treatments. 7 Other important implications of the COVID‐19 pandemic and decreased demand for imaging services include financial challenges for public and private radiology practices, staffing changes, reduced staff satisfaction, reduced research output, and fewer educational opportunities for radiology trainees. 8 , 9 , 10
Given the potential implications for patients, radiology staff and practices, modelling and analyses are required to quantify the impact of the COVID‐19 pandemic on imaging services. This will in turn assist governments and professional associations in the development of evidence‐based strategies during the recovery phase of the pandemic. As such, we aimed to quantify the impact of the first wave of the COVID‐19 pandemic on diagnostic imaging services in Australia using an interrupted time series model.
Methods
Data source & extraction
Medicare is the publicly funded universal healthcare scheme in Australia. 11 The Medicare Benefits Schedule (MBS) database provides information on the utilisation of a comprehensive range of government subsidised services including diagnostic procedures and investigations, as well as therapeutic interventions. 11 All diagnostic imaging service items are provided in Category 5 of the MBS. Category 5 is divided by Medicare Australia into groups according to imaging modality as follows: (i) ultrasound, (ii) computed tomography (CT), (iii) general radiography, (iv) nuclear medicine, and (v) magnetic resonance imaging (MRI). Monthly data between January 2016 to June 2020 were extracted from Category 5 of the MBS database stratified by imaging modality. Given this study used publicly available data, ethics board approval was not required.
Statistical analysis
Holt‐Winters modelling is a commonly used forecasting technique that utilises past values in a time series to predict future values. Holt‐Winters modelling utilises additive triple exponential smoothing in order to account for three key components in a time series: average values, trend over time, and seasonality (for example, declines in services associated with school and major holiday periods). 12 In the present study, a Holt‐Winters model was built using monthly data between January 2017 and December 2019 in order to predict expected monthly diagnostic imaging services between January 2020 and June 2020 with a 95% confidence interval. Observed monthly services between January 2020 and June 2020 were compared with predicted monthly services over the same time period to calculate residual differences (RD). A residual difference was considered statistically significant if the observed data point was outside of the 95% confidence interval of the model’s prediction (P < 0.05). A total of six models were developed. This comprised one model for each imaging modality (ultrasound, computed tomography, general radiography, nuclear medicine and magnetic resonance imaging) as well as one for total imaging services. All statistical analyses were performed using SPSS version 22 (IBM SPSS, Amronk, NY, USA) and LKS‐CHART Forecasting Tool (St. Michael’s Hospital, Toronto, ON, Canada).
To determine the accuracy of fit of the model, the mean absolute percentage error (MAPE) between observed and modelled monthly services between January 2017 and December 2019 was calculated. The MAPE is one of the most commonly used metrics of model fit and predictive accuracy. 13 To determine the six‐monthly predictive accuracy of the model, cross‐validation was performed by using observed monthly services between January 2016 and December 2018 to predict monthly services between January 2019 and June 2019. The predicted monthly services were then compared with the observed monthly services for this same time period in order to determine the MAPE in the model’s prediction. Model fit and predictive accuracy was calculated for all six models.
Results
Model fit and predictive accuracy
All six models demonstrated excellent model fit and six‐monthly predictive accuracy. The range of MAPEs for all models was 1.65–2.31%. The range of MAPEs for the cross‐validation models was 2.17–4.42% (Table 1).
Table 1.
Summary of model fit and predictive accuracy for all models
| Model | MAPE for model fit† (%) | MAPE for predictive accuracy‡ (%) |
|---|---|---|
| Total Imaging Services | 1.71 | 3.16 |
| Ultrasound | 1.65 | 3.15 |
| Computed Tomography | 1.72 | 2.17 |
| General Radiography | 2.05 | 4.24 |
| Nuclear Medicine | 2.25 | 2.33 |
| Magnetic Resonance Imaging | 2.31 | 4.42 |
MAPE, mean absolute percentage error.
Calculated on observed and modelled data between January 2017 and December 2019.
Calculated on observed and predicted data between January 2019 and June 2019 using January 2016–December 2018 data.
Total diagnostic imaging services
Over 12.9 million diagnostic imaging services were performed between January 2020 and June 2020. There was a statistically significant reduction in total imaging services performed in March 2020 (−13.1%), April 2020 (−32.4%) and May 2020 (−21.4%) (Table 2). In absolute numbers, this equates to a total reduction of over 1.6 million imaging services performed between March and May 2020 compared to predicted (Figure 1).
Table 2.
Monthly absolute and percentage differences between observed and predicted number of MBS imaging services items stratified by imaging modality
| Date | Ultrasound | Computed tomography | General radiography | Nuclear medicine | Magnetic resonance imaging | Total imaging services | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Absolute difference | Percentage difference (95% CI) | Absolute difference | Percentage difference (95% CI) | Absolute difference | Percentage difference (95% CI) | Absolute difference | Percentage difference (95% CI) | Absolute difference | Percentage difference (95% CI) | Absolute Difference | Percentage difference (95% CI) | |
| Jan‐2020 | −3 329 | −0.4 (−5.8, 5.7) | 4 761 | 1.6 (−3.9, 7.7) | 30 056 | 3.6 (−3.7, 12.0) | 3 038 | 5.4 (−2.9, 15.2) | −1 072 | −1.1 (−8.3, 7.4) | 25 565 | 1.2 (−4.6, 7.6) |
| Feb‐2020 | −12 640 | −1.3 (−6.2, 4.1) | 5 862 | 1.8 (−3.3, 7.5) | 14 999 | 1.7 (−5.0, 9.3) | 18 | 0.0 (−7.0, 8.2) | 3 358 | 3.0 (−3.8, 11.0) | 15 191 | 0.6 (−4.6, 6.5) |
| Mar‐2020 | −139 709 | −13.3 (−17.4, −8.9) | −39 576 | −11.6 (−15.8, −6.9) | −134 380 | −14.2 (−19.7, −8.0) | −6 914 | −10.1 (−16.0, −3.3) | −8 781 | −7.2 (−12.9, −0.8) | −332 260 | −13.1 (−17.5, −8.4) |
| Apr‐2020 | −278 436 | −30.5 (−34.3, −26.4) | −74 829 | −24.9 (−28.9, −20.4) | −313 258 | −37.8 (−42.4, −32.5) | −14 586 | −24.6 (−30.3, −17.9) | −37 479 | −33.0 (−37.4, −28.0) | −716 957 | −32.4 (−36.2, −28.1) |
| May‐2020 | −245 307 | −22.3 (−25.8, −18.5) | −48 787 | −13.7 (−17.7, −9.3) | −234 789 | −23.2 (−27.9, −17.8) | −8 709 | −12.3 (−17.9, −5.9) | −32 782 | −24.3 (−28.4, −19.5) | −571 634 | −21.4 (−25.1, −17.3) |
| Jun‐2020 | 227 | 0.0 (−5.0, 5.6) | 19 783 | 6.2 (0.8, 12.2) | 30 700 | 3.5 (−3.8, 11.9) | 6 812 | 11.0 (3.0, 20.4) | −3 648 | −3.0 (−8.9, 3.7) | 53 451 | 2.3 (−3.2, 8.3) |
Bold values indicates statistical significance (P < 0.05).
Fig. 1.
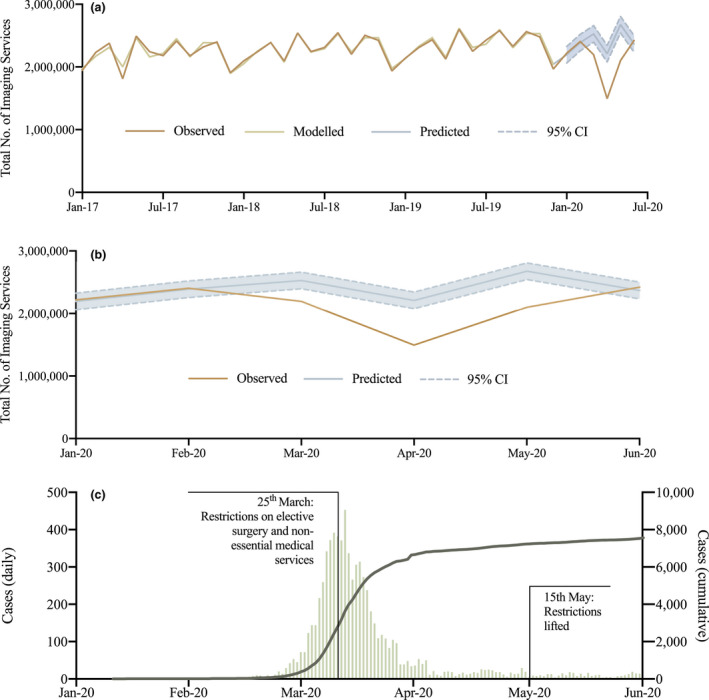
Total imaging services performed in Australia during the COVID‐19 pandemic. (a) Observed total imaging services between January 2017 and June 2020, modelled total imaging services between January 2017 and December 2019 with predicted (with 95% confidence interval) total imaging services between January 2020 and June 2020. (b) Observed and predicted (with 95% confidence interval) total imaging services between January 2020 and June 2020. (c) Daily (left axis) and cumulative (right axis) COVID‐19 cases in Australia with key time points for restrictions on healthcare delivery indicated.
Ultrasound
Compared to predicted, there was a statistically significant reduction in ultrasound services performed in March 2020 (−13.3%), April 2020 (−30.5%) and May 2020 (−22.3%) (Figure 2).
Fig. 2.
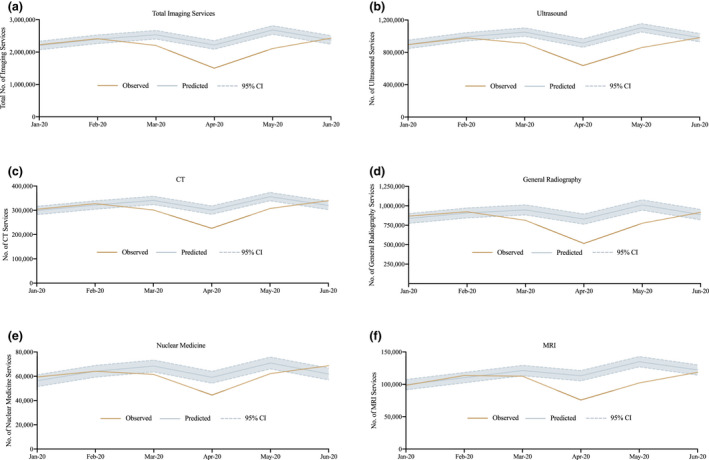
Observed and predicted (with 95% confidence interval) imaging services performed in Australia during the COVID‐19 pandemic stratified by imaging modality. (a) Total imaging services. (b) Ultrasound. (c) Computed tomography. (d) General radiography. (e) Nuclear medicine. (f) Magnetic resonance imaging.
Computed tomography
Compared to predicted, there was a statistically significant reduction in CT services performed in March 2020 (−11.6%), April 2020 (−24.9%) and May 2020 (−13.7%), followed by a statistically significant increase in June 2020 (+6.2%) (Figure 2).
General radiography
Compared to predicted, there was a statistically significant reduction in general radiography services performed in March 2020 (−14.2%), April 2020 (−37.8%) and May 2020 (−23.2%) (Figure 2). Out of all imaging modalities, general radiography had the greatest percentage reductions in each of March, April and May 2020.
Nuclear medicine
Compared to predicted, there was a statistically significant reduction in nuclear medicine services performed in March 2020 (−10.1%), April 2020 (−24.6%) and May 2020 (−12.3%), followed by a statistically significant increase in June 2020 (+11.0%) (Figure 2).
Magnetic resonance imaging
Compared to predicted, there was a statistically significant reduction in MRI services performed in March 2020 (−7.2%), April 2020 (−33.0%) and May 2020 (−24.3%) (Figure 2).
Discussion
The COVID‐19 pandemic has had profound impacts on healthcare delivery worldwide. Using interrupted time series modelling to quantify the impact of COVID‐19 on diagnostic imaging services in Australia, our models accounted for long‐term trends as well as seasonality and achieved predictive errors of less than 5% in cross‐validation testing. We demonstrated that total imaging services were 13.1%, 32.4% and 21.4% lower than expected for March, April and May 2020, respectively, corresponding with the peak of the first wave of the COVID‐19 pandemic in Australia. 14 In absolute numbers, this equates to a total reduction of 1 620 851 imaging services performed between March and May 2020 compared to predicted. Total imaging services rebounded in June 2020, aligning with the flattening of the first wave. 14 For comparison, a number of single institution studies in the United States of America (US) demonstrated reductions in imaging volumes of 40–70%. 4 , 6 , 15 , 16 Australia’s relatively lower reduction in imaging services may be related to its lower burden of COVID cases compared to the US. 14
The decreases in imaging services observed in March, April and May 2020 were likely the result of a number of factors. First, the Australian Government implemented nationwide restrictions on healthcare delivery starting on the 25th of March 2020. This included the cancellation of elective surgeries and non‐urgent medical services in order to protect hospital capacity, preserve personal protective equipment, and reduce the risk of infection to patients and healthcare workers. 3 Further, national stay‐at‐home orders combined with public anxiety led to a reduction in healthcare attendances. 17 While general practice and many specialties have transitioned to telehealth and remote provision of healthcare services, this is not feasible in the delivery of imaging services, which requires in‐person attendance for image acquisition. Lastly, referring practitioners may be intentionally delaying referrals for imaging services due to concerns of overburdening the healthcare system or risk of their patients being exposed to COVID‐19 infection. 18 Similarly, referrers may also be more judicious in only requesting imaging services that are genuinely clinically indicated. The combination of these pandemic‐related factors likely resulted in the significant reduction of imaging services performed between March and May 2020.
The decreased provision of imaging services in March, April and May 2020 may have concerning impacts on downstream patient care. Radiology plays a central role in healthcare through informing clinical decision‐making, providing or supporting diagnoses, planning surgical interventions, monitoring disease progression and treatment response, and performing diagnostic or therapeutic interventions. 7 The reduction in imaging services is likely to lead to backlogs of referrals and, consequently, to delayed diagnoses and treatments. This has the potential to lead to suboptimal clinical outcomes. 7 As such, it is essential that evidence‐based recovery strategies are implemented to reduce the severity of backlogs as well as the impact of cancelled or delayed imaging services on patient care. In the US, the American College of Radiology guidelines recommend appropriate prioritisation of referrals to ensure equitable access for the patients most in need for imaging services. 19 Ultimately, decisions to render a radiology service should be made on the balance between service urgency and the risk of COVID‐19 transmission. 19
Each of the imaging modalities demonstrated a statistically significant reduction in services performed in March, April and May 2020. However, the magnitude of these reductions was variable between different modalities. Notably, nuclear medicine services had the lowest percentage reductions in both April and May 2020. Further, nuclear medicine services demonstrated the largest rebound in June 2020, with a statistically significant increase in the number of services performed compared to predicted. Interestingly, nuclear medicine services, in particular positron emission tomography (PET) imaging, has been consistently the least impacted modality among other international studies. 15 , 20 , 21 This is likely related to the key role PET imaging plays in diagnosing and staging cancer as well as monitoring treatment response and cancer recurrence. 22 A range of guidelines were implemented nationally in Australia to ensure cancer treatment was not delayed due to COVID‐19. 23 The relative preservation of nuclear medicine services noted in this study is reassuring of the success of these efforts.
Similar to nuclear medicine services, CT services were less impacted than other modalities, particularly in April and May 2020. There was also a statistically significant increase in CT services in June 2020 compared to predicted. The impact of the COVID‐19 pandemic on CT services reported in other studies has been variable. 4 , 6 , 15 , 16 , 24 , 25 As many specialities have adopted telehealth to replace face‐to‐face consultations, referrers may be preferentially requesting CT services as a replacement for physical examination. 26 If this is the case, it is important to be mindful of the risks of unnecessary radiation exposure. Additionally, the increase in CT services in June may reflect a build‐up of demand for CT imaging for preoperative planning following recommencement of elective surgeries in Australia in May 2020. 27
The decrease in imaging services may impact radiology research and education. Academic centres and universities have halted scientific research activities to comply with social distancing measures and to reallocate resources to create capacity to handle a surge in COVID‐19 cases. 9 It has been estimated that a three‐month pandemic‐related shutdown in radiology research will result in up to two years of lost research productivity. 9 The sequestering of senior radiologists and trainees to maintain social distancing will reduce opportunities for the traditional shoulder‐to‐shoulder training that enables experiential learning and timely feedback. 28 To address the closures of radiology reading rooms, teaching institutions have implemented web conferencing to facilitate readouts. 28 Strategies like this may help to maintain research and education during the COVID‐19 era.
It is important to consider the economic and financial implications of the COVID‐19 pandemic for both public and private radiology practices. 8 , 29 It is expected that practices that perform predominantly outpatient imaging services will be most impacted by the decrease in demand and reductions in revenue. 29 High equipment and overhead costs make radiology practices particularly vulnerable relative to other medical services. It is integral that private practices proactively ensure their financial resiliency, 8 given that their sustainability is essential in protecting the public system from overload. 7
Ideally, the decreases observed in March, April and May 2020 will be matched with increases in imaging services during the post‐wave period. 4 This may be a contributing factor to the statistically significant increase in nuclear medicine and CT services performed in June 2020, corresponding with the end of the first wave of the COVID‐19 pandemic in Australia. Radiology service providers have implemented various measures to address safety concerns and to prepare for the impending increased demand as restrictions on healthcare services are gradually lifted. 19 Some radiology departments have used staff repurposing to assist with the increased patient rescheduling workload. Uptake of new technologies and software can assist with use of remote and home workstations, enabling maintenance of social distancing measures. 19 Many hospitals are continuing screening of staff and patients at entry with risk questionnaires and temperature checks, 30 and comprehensive disinfection practices have been introduced for cleaning of radiological equipment between patients. 31 It is important that radiology department administrators continually review and adapt their operational practices in order to deliver the maximum imaging services that is safely possible.
To our knowledge, this is the first study to use interrupted time series modelling to quantify the impacts of the COVID‐19 pandemic on imaging services at a national level. However, these findings should be interpreted in the context of a number of limitations. First, MBS data do not include imaging services provided to inpatients at public hospitals or imaging services that are 100% private, i.e. services that do not attract a Medicare rebate. 11 Further, the MBS does not cover services qualifying for benefit under the Department of Veterans’ Affairs, Work Cover or the Transport Accident Commission. 11 Second, our study only assessed nationwide data. Future modelling should assess service disruptions in different states and territories given the variability in outbreaks of COVID‐19 and lockdown measures from the second half of 2020 onwards. With the ongoing risk of future waves of COVID‐19 and reimposition of restrictions on healthcare delivery, modelling must be continually updated in order to provide the most accurate and up‐to‐date information. Lastly, our study only quantified the impact of COVID‐19 on the volume of imaging services. Further studies are required to quantify the direct and indirect impacts of temporary reductions in imaging services on clinical, research, economic and educational outcomes.
In conclusion, the COVID‐19 pandemic has had profound impacts on imaging services worldwide. The present study utilised interrupted time series modelling based on nationwide data and demonstrated reductions in total imaging services of 13.1%, 32.4% and 21.4% in March, April and May 2020, respectively. Nuclear medicine and CT services were relatively preserved during the peak of the first wave and rebounded stronger in June compared to general radiography, ultrasound and MRI services. This modelling can inform evidence‐based decision‐making and planning by governments and professional associations for the recovery phase of the COVID‐19 pandemic as well as for potential future public health crises.
Funding
No funding sources.
S Sreedharan MD, M Mian MD, BDS, DJT McArdle MBBS, MPsych, A Rhodes MBBS, FRANZCR, EBIR, MClinEd.
Conflict of interest: The authors disclose no conflict of interest.
References
- 1. Rosen MP, Norbash A, Kruskal J et al. Impact of coronavirus disease 2019 (COVID‐19) on the practice of clinical radiology. J Am Coll Radiol 2020; 17: 1096–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Australian Government . Australian Health Sector Emergency Response Plan for Novel Coronavirus (COVID‐19) Canberra ACT2020 [cited 2020 October]. Available from: https://www.health.gov.au/sites/default/files/documents/2020/02/australian‐health‐sector‐emergency‐response‐plan‐for‐novel‐coronavirus‐covid‐19_2.pdf
- 3. Negopdiev D, Hoste E, Collaborative C . Elective surgery cancellations due to the COVID‐19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg 2020; 107: 1440–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Parikh KD, Ramaiya NH, Kikano EG et al. COVID‐19 pandemic impact on decreased imaging utilization: a single institutional experience. Acad Radiol. 2020; 27: 1204–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Freudenberg LS, Paez D, Giammarile F et al. Global impact of COVID‐19 on nuclear medicine departments: an international survey in April 2020. J Nucl Med 2020; 61: 1278–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Naidich JJ, Boltyenkov A, Wang JJ et al. Coronavirus disease 2019 (COVID‐19) pandemic shifts inpatient imaging utilization. J Am Coll Radiol 2020; 17: 1289–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. The Royal Australian and New Zealand College of Radiologists . Impact of COVID‐19 Pandemic on Availability of Clinical Radiology Position Statement from RANCZR Board of Directors, 2020. [cited 2020 October]. Available from: https://www.ranzcr.com/fellows/clinical‐radiology/professional‐documents/position‐statement‐on‐the‐impact‐of‐covid‐19‐pandemic‐on‐availability‐of‐clinical‐radiology‐in‐australia
- 8. Sharpe RE, Kuszyk BS, Mossa‐Basha M et al. Special report of the RSNA COVID‐19 task force: the short‐and long‐term financial impact of the COVID‐19 pandemic on private radiology practices. Radiology 2021; 298: E11–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vagal A, Reeder SB, Sodickson DK et al. The impact of the COVID‐19 pandemic on the radiology research Enterprise: radiology scientific expert panel. Radiology 2020; 296: E134–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Alvin MD, George E, Deng F et al. The impact of COVID‐19 on radiology trainees. Radiology 2020; 296: 246–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Australian Government . Medicare Group Statistics Reports 2020 [cited 2020 October]. Available from: http://medicarestatistics.humanservices.gov.au/statistics/mbs_group.jsp
- 12. Gelper S, Fried R, Croux C. Robust forecasting with exponential and Holt‐Winters smoothing. J Forecast 2010; 29: 285–300. [Google Scholar]
- 13. Bowerman BL, O'Connell RT, Forecasting KAB. Time Series, and Regression. , 4th edn. Duxbury Press, South West College, 2005. [Google Scholar]
- 14. Johns Hopkins University . COVID‐19 Dashboard 2020 [cited 2020 October]. Available from: https://coronavirus.jhu.edu/map.html
- 15. Norbash AM, Van Moore JA, Recht MP et al. Early‐stage radiology volume effects and considerations with the coronavirus disease 2019 (COVID‐19) pandemic: adaptations, risks, and lessons learned. J Am Coll Radiol 2020; 17: 1086–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Vagal A, Mahoney M, Allen B et al. Rescheduling nonurgent care in radiology: implementation during the coronavirus disease 2019 (COVID‐19) pandemic. J Am Coll Radiol 2020; 17: 882–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wong LE, Hawkins JE, Murrell KL. Where are all the patients? Addressing Covid‐19 fear to encourage sick patients to seek emergency care, 2020. [cited 2020 October]. Available from: https://catalyst.nejm.org/doi/pdf/ 10.1056/CAT.20.0193 [DOI]
- 18. The Royal Australian and New Zealand College of Radiologists . Position Statement: Patient Access to Imaging Services in New Zealand – During and After COVID‐19. Social Distancing 2020. [cited 2020 October]. Available from: https://www.ranzcr.com/our‐work/coronavirus/position‐statements‐and‐guidance
- 19. Davenport MS, Bruno MA, Iyer RS et al. ACR statement on safe resumption of routine radiology care during the coronavirus disease 2019 (COVID‐19) pandemic. J Am Coll Radiol 2020; 17: 839–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wong WL, Ross P, Peters K et al. The coronavirus disease pandemic 2019 [COVID‐19]: impact on NHS England PET‐CT Scanning, 2020. 10.21203/rs.3.rs-77635/v1 [DOI]
- 21. Maurea S, Mainolfi CG, Bombace C et al. FDG‐PET/CT imaging during the Covid‐19 emergency: a southern Italian perspective. Eur J Nucl Med Mol Imaging 2020; 47: 2691–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kostakoglu L, Agress H Jr, Goldsmith SJ. Clinical role of FDG PET in evaluation of cancer patients. Radiographics 2003; 23: 315–40. [DOI] [PubMed] [Google Scholar]
- 23. Weinkove R, McQuilten ZK, Adler J et al. Managing haematology and oncology patients during the COVID‐19 pandemic: interim consensus guidance. Med J Aust 2020; 212: 481–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Houshyar R, Tran‐Harding K, Glavis‐Bloom J et al. Effect of shelter‐in‐place on emergency department radiology volumes during the COVID‐19 pandemic. Emerg Radiol 2020; 27: 781–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Madhuripan N, Cheung HM‐C, Cheong LHA et al. Variables influencing radiology volume recovery during the next phase of the COVID‐19 pandemic. J Am Coll Radiol 2020; 17: 855–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Azam SA, Myers L, Fields BK et al. Coronavirus disease 2019 (COVID‐19) pandemic: Review of guidelines for resuming non‐urgent imaging and procedures in radiology during Phase II. Clin Imaging 2020; 67: 30–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Australian Government . Elective surgery restrictions eased, 2020. [cited 2020 October]. Available from: https://www.health.gov.au/ministers/the‐hon‐greg‐hunt‐mp/media/elective‐surgery‐restrictions‐eased
- 28. Chertoff JD, Zarzour JG, Morgan DE et al. The early influence and effects of the Coronavirus disease 2019 (COVID‐19) pandemic on resident education and adaptations. J Am Coll Radiol 2020; 17: 1322–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cavallo JJ, Forman HP. The economic impact of the COVID‐19 pandemic on radiology practices. Radiology 2020; 296: E141–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Azam SA, Myers L, Fields BKK et al. Coronavirus disease 2019 (COVID‐19) pandemic: review of guidelines for resuming non‐urgent imaging and procedures in radiology during Phase II. Clin Imaging 2020; 67: 30–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Deng M. The prevention and management of the coronavirus disease 2019 (COVID‐19) outbreak in radiology departments in epidemic areas. Jpn J Radiol 2020; 38: 483–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


